Short abstract
Following the launch by the BMJ and others of the campaign to promote academic medicine, a working party of 20 medical academics from all over the world was convened to develop a plan of action
Editorials published in several of the world's leading journals in the past few months have heralded the launch of a global campaign to promote and revitalise academic medicine.1 The campaign is a response to a widely held view that academic medicine is in crisis.2
In June 2004 the BMJ Publishing Group and others (www.bmj.com/academicmedicine) convened a working party of medical academics to discuss the challenges facing academic medicine. This paper summarises the results of the meeting, and outlines how the working party will conduct its business in the next 12 months.
What are the roles of academic medicine?
Academic medicine is traditionally conceived of having three roles: teaching, research, and service. These roles are changing: academic medicine still has the primary responsibility for training doctors; research remains a core role but more is being done in institutes of biotechnology and biomedicine; and, most clinical service, even in academic centres, is now provided by non-academic doctors.
We strongly feel that it is the “added value” or the synergy that should exist between these three roles—when they are brought effectively together—that defines academic medicine. Traditionally focused on tertiary hospitals, academic medicine must now extend more into primary care and public health. The traditional “clinical service” should be reframed more broadly as “service to the health system and the patient.”
How well is academic medicine carrying out its roles?
We feel that currently academic medicine
Undervalues our teaching role
Tolerates the imbalance and lack of communication between basic research and clinical or applied research
Fails to drive innovation and excellence in clinical practice resulting in indefensible variations in practice and outcome
Ignores the essential values of social and global responsibility.
The growth and imbalance of biomedical research institutes creates a challenge. How much of this research will bear a dividend in our health systems, and when? Who will translate this research into health benefit? Communication between basic and clinical and health systems researchers seems to have become increasingly difficult. We seem not to have learned that the greatest health benefits come from applying what we already know to more people. We continue to try to make basic scientists of our best and brightest clinicians: trainees enrolled in PhD programmes are typically seeking another new gene instead of working on clinical safety, quality, and health outcomes. Have we got the balance right?
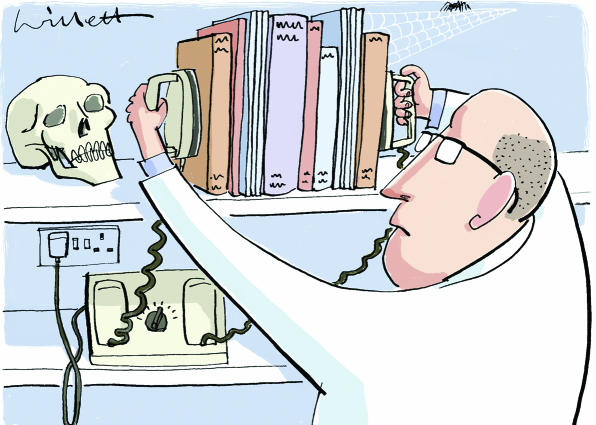
Figure 1.
Box 1: Task groups
Analysing the evidence—This group is collecting and appraising systematically the available evidence on academic medicine and its problems3
Careers and training—This group aims to explore the issues of mentoring and recruitment with a special emphasis on women and marginalised groups, and to set up student and trainee international advisory groups to help explore problems and to propose possible solutions
Communication and dissemination—This group is responsible for internal and external communication strategies and management of publication policies
Stakeholder liaisons and operations—This group is outlining how the working party will operate and is establishing collaborative relationships with relevant regional bodies such as governments, professional associations and universities
Vision and values—This group is developing a discussion paper that seeks to explore current values and then propose a new vision and set of values for academic medicine
Another great failing is the lack of focus on the health needs of populations not normally supported by academic medicine due to race, ethnic origin, social class, gender, or geographical location.
What needs to be done to permit academic medicine to fulfil its roles?
Firstly, we need this campaign, and we need a great global debate. We need to acknowledge that there is a crisis and there is a need for change. So, the campaign is underway and we want your participation.
We need a new vision for academic medicine. We need a clear definition of the roles of academic medicine and we need a clear iteration of our values—what we stand for and what we want to achieve. We need to clarify the place of academic medicine within medicine, the health system, and civil society. We need to articulate and demonstrate the economic and social value that academic medicine provides. And we need a global perspective.
Box 2: Regional and stakeholder advisory groups
Regional advisory groups are being created for:
Australasia (East Asia and Pacific)
Europe
Latin America and the Caribbean
Middle East and North Africa
North America
South Asia
Sub-Saharan Africa
Stakeholder advisory groups are being created to represent the following constituents:
Academics
Business and industry
Government and policy makers
Journal editors
Patients
Professional associations
Students and trainees
Summary points
Academic medicine worldwide is perceived to be in crisis
An international working party has been convened with the aim of revitalising academic medicine
A series of task groups and regional and stakeholder advisory groups have been formed to inform the working party through wide consultation
Expected outputs include a report with recommendations and a series of peer reviewed published papers
We cannot do this alone. We need partnerships within academic medicine itself and beyond medicine, partnerships that cut across traditional disciplinary and institutional boundaries. We also need partnerships with others in the health system, and of course—perhaps more than anything else—we need partnerships with patients, policy makers, and the public.
Next steps
During the meeting the working party analysed these problems and together agreed to work more on several topics:
Proposing how academic medicine could listen better and improve its relationships with its “customers,” including patients, policy makers, and practitioners
Exploring/examining what the values of academic medicine should be
Building capacity in academic medicine, including better career paths
Developing a vision of how academic medicine should look in 2020
Planning how to ensure that the campaign achieves change.
Five task groups have been formed (box 1). A member of the working party convenes each task group, and the convenors meet by teleconference monthly.
We are developing a series of regional and stakeholder advisory groups (box 2) to inform and advise the working party through as broad a range of consultations as possible. The regional advisory groups will provide global geographic coverage for the consultations, and the stakeholder advisory groups will represent the interests of the various “customers” of academic medicine. Out of this we see a series of working papers being developed to further stimulate and inform the debate. These working papers will lead to a series of peer reviewed publications. The whole working group will meet in mid-2005 with international policy makers to complete a final report, which will include recommendations for reform in academic medicine and a platform for action.
We are aware that this effort could easily lead to a lot of discussion and little action, with a report produced in 12 months that has minimal impact. Our challenge is to ensure a different outcome. We hope to do this through the task groups outlined here and a range of other consultation processes that we are currently establishing. We invite all of you to join with us in changing the face and future of academic medicine.
Supplementary Material
References
- 1.Tugwell P. Campaign to revitalise academic medicine kicks off. BMJ 2004;328: 597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clark J, Smith R. BMJ Publishing Group to launch an international campaign to promote academic medicine BMJ 2003;327: 1001-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Working Party to Promote and Revitalise Academic Medicine. Academic medicine: the evidence base. BMJ 2004:329: 789-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 Members of the working party are listed on
Members of the working party are listed on