Abstract
Water insecurity (WI) is a serious and worsening problem worldwide, but its role in health outcomes among people living with HIV or pregnant women is unknown. We assessed experiences of WI in a cohort of 323 pregnant Kenyan women of mixed HIV status. The majority (77.7%) had at least one experience of WI in the previous month; it was associated with negative economic, nutrition, disease, and psychosocial outcomes. A standardized cross-culturally valid household WI scale would facilitate assessment of the prevalence and consequences of WI, and increased attention to WI could reveal an overlooked, but modifiable, cause of adverse HIV outcomes.
Keywords: HIV, Kenya, water insecurity, women
INTRODUCTION
Water insecurity (WI), i.e., insufficient and uncertain access to adequate water for an active and healthy lifestyle (Stevenson et al. 2012) is a serious and worsening problem globally (Webb & Iskandarani 1998; Wutich & Brewis 2014). The region of the world with the greatest HIV prevalence is also most severely affected by water scarcity: sub-Saharan Africa (WHO/UNICEF 2014). As such, we posit that WI and HIV may be syndemic, in much the same way that household food insecurity and HIV are (Weiser et al. 2011). Given that women bear the psychological and physical responsibility of water acquisition as well as water-intensive chores (Webb & Iskandarani 1998; Stevenson et al. 2012), household water security is also likely to be fundamental to their well-being, as well as to that of their infants and children.
However, the relationships between household WI, HIV, and maternal and child health have received scant attention. Given the many pathways by which household WI may impact HIV disease, especially among women, we explored experiences with WI in an ongoing observational cohort study of 323 pregnant women of mixed HIV status in Nyanza, Kenya.
METHODS
Participants were recruited from seven clinical sites in Nyanza province, Kenya between September 2014 and June 2015. They were enrolled at <30 weeks gestation, with a 1:1 ratio of HIV-infected to HIV-uninfected.
Although there is no validated scale for measuring household WI in Kenya, all 323 women who attended the second study visit were surveyed about their experiences with WI at approximately 33 weeks of pregnancy. Specifically, they were asked about water acquisition and use, and perceived consequences of insufficient water using questions adapted from a UNICEF WASH questionnaire (UNICEF & World Health Organization 2006) and a WI study in Ethiopia (Stevenson et al. 2012). The frequencies of WI experiences in the last month were queried, with possible responses being ‘never’, ‘rarely’ (1–2 times), ‘sometimes’ (3–10 times), or ‘often’ (>10 times). Basic descriptive analyses (Student’s t-tests, chi-square) were performed using STATA 14 (StataCorp, College Station, TX, USA).
This study was approved by the Kenya Medical Research Institute and Cornell University Institutional Review Board.
RESULTS
Of the 323 study participants, 38.9% used an unimproved primary water source, e.g., an unprotected dug well or spring, or surface water (WHO/UNICEF 2014). The majority (71.2%) did not have a source of water within their households. Among households without a source of water in their compound, respondents (i.e., women) bore the primary responsibility of acquiring water in 77.5% of households, even while in late pregnancy (mean (SD) gestational age of 33.1 (2.1) weeks). Those women without water in the compound spent, on average, 4.5 (6.7) hours per week acquiring water.
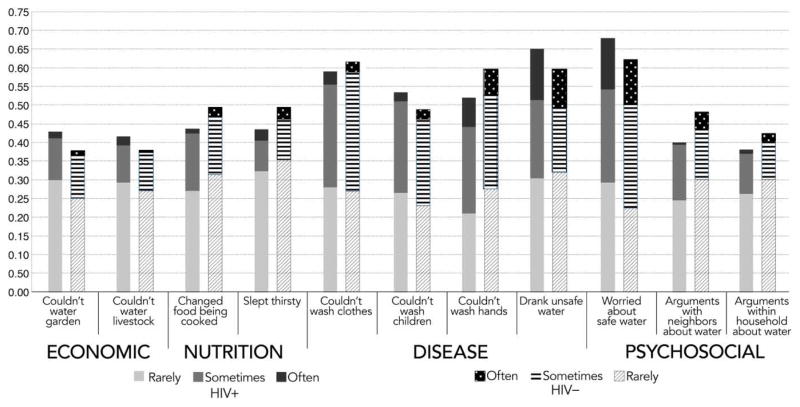
Participants reported experiencing four types of negative impacts of WI: in economic, nutritional, disease, and psychosocial domains (Figure 1). Economic consequences included decreased agricultural productivity (experienced by 42.3% of study participants) and livestock productivity (39.9%). Nutritional consequences of WI included changes in food being cooked (46.4%) and going to sleep thirsty (46.4%). WI impacted disease transmission by preventing a number of sanitation and hygiene behaviors, including the inability to wash clothes (60.4%), bathe children (51.3%), and wash one’s own hands after contact with fecal material (55.7%). Further, 64.1% reported drinking unsafe water. Psychosocial impacts included worrying about accessing sufficient water (65.3%), and arguments about water with neighbors (43.9%) and within one’s own households (40.3%). The majority of women (77.7%) had at least one experience of WI in the prior month. Water acquisition also posed both psychological stress and physical risk, with 77.3% stating that they felt ‘somewhat or strongly concerned’ for their physical safety during these trips. In bivariate analyses, there were no significant differences by HIV status in any of the indicators assessed (Figure 1).
Figure 1.
The frequency of experiences of household WI in the prior month among 323 pregnant Kenyan women, by domain and HIV status.
DISCUSSION
In this first study of the associations between WI, HIV, and maternal health, a large proportion of participants experienced a variety of deleterious consequences of insufficient household water. These data, together with the plausibility of the role of WI in adverse economic, nutritional, disease, and psychosocial outcomes, suggest that WI merits further exploration. Below we outline two next important steps to better understand the role of WI in public health: the development of a cross-culturally valid scale, and greater attention to WI in the HIV program and research communities.
While the experiences related to household WI that we queried participants on is an important starting point, a cross-culturally valid and reliable scale is needed to properly assess the multi-dimensional consequences of household-level WI. Although there is a burgeoning literature in which scales to assess household water security are presented (e.g. Stevenson et al. 2012; Jepson 2014; Wutich & Brewis 2014; Tsai et al. 2016), few are validated, and none are suitable for cross-cultural use. The development of a short and easy-to-administer cross-culturally valid scale would facilitate data collection on household WI globally and promote harmonized assessments of the consequences of WI.
Further, we hope the HIV community begins to pay more attention to issues of water scarcity because of the greater water needs of people living with HIV (PLHIV) (Lule et al. 2005). Indeed, we had expected that the frequency of WI would be greater among HIV-infected women for this very reason. Water is essential for maximizing efficacy and minimizing toxic side effects of anti-retroviral medicines (ARVs); some ARVs require an additional 2 L of water (Lesho & Gey 2003) above the 2.5–3 L average daily water intake required for survival. During bouts of mouth ulcers or oral thrush, extra water may also be needed to soften foods (Lesho & Gey 2003). Further, as HIV progresses, the amount of water needed to preserve health and hygiene increases. Compared with the usual minimum requirement of 2–6 L per day for basic hygiene, an additional 80 L/day during diarrheal episodes may be needed to maintain hygiene for PLHIV and their caregivers (WaterAID 2014). In spite of greater water needs, it is worth noting that water may be more difficult for PLHIV to access, due to stigma or the physical inability to haul water during advanced disease progression (WaterAID 2014).
A second reason for the HIV community to pay attention to WI is that WI may have more severe consequences for PLHIV. For example, consuming unsafe water is more dangerous for PLHIV, given their greater susceptibility to waterborne opportunistic infections (Lule et al. 2005). Diarrheal illnesses can in turn lead to dehydration, decreased immunity, increased viral load, and poor intestinal absorption of essential nutrients and therapeutic dosages of medicines (Lule et al. 2005). Furthermore, water acquisition can exacerbate energy deficits. Drawing and carrying water is calorically very costly. Given the 10% increased resting energy expenditure associated with HIV infection (Kosmiski 2011), such exertion can exacerbate already existing energy deficits, contributing to weight loss. Finally, the energy and time demands of water acquisition and/or dehydration may decrease the duration of exclusive breastfeeding, which increases the risk of vertical transmission of HIV. Measurements of HIV disease status by WI, including viral load and CD4 count, would be helpful for testing the hypothesis that WI exacerbates HIV disease progression.
CONCLUSION
In sum, our understanding of the role of food insecurity has been transformative of our understanding of HIV acquisition and disease progression (Weiser et al. 2011); WI may be as valuable for understanding both HIV and maternal and child health outcomes. A thorough understanding of the prevalence and sequelae of WI will make it possible to intervene where valuable resources are most needed, to measure the impacts of those interventions on household WI, and ultimately, to reduce the deleterious consequences of household WI on the health of vulnerable populations everywhere.
Acknowledgments
We very warmly thank the mothers and children who have taken their valuable time to participate in the Pith Moromo/Pii en Ngima studies. We gratefully acknowledge the assistance of Ann Lei, Sarah Obaje, Benter Ogwano, Joyce Bonke, Teresa Owade, Joy China, and Tobias Odwar with data collection. This work was supported by K01 MH098902 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Contributor Information
Natalie R. Krumdieck, Weill Cornell Medical College, 1300 York Avenue, New York, NY 10021, USA
Shalean M. Collins, Program in International Nutrition, Cornell University, Ithaca, NY 14853, USA and Department of Population Medicine and Diagnostic Sciences, Cornell University, Ithaca, NY 14853, USA
Pauline Wekesa, Kenya Medical Research Institute, Centre for Microbiology Research, Mbagathi Road, Nairobi, Kenya.
Patrick Mbullo, Kenya Medical Research Institute, Centre for Microbiology Research, Mbagathi Road, Nairobi, Kenya.
Godfred O. Boateng, Program in International Nutrition, Cornell University, Ithaca, NY 14853, USA and Department of Population Medicine and Diagnostic Sciences, Cornell University, Ithaca, NY 14853, USA
Maricianah Onono, Kenya Medical Research Institute, Centre for Microbiology Research, Mbagathi Road, Nairobi, Kenya.
Sera L. Young, Program in International Nutrition, Cornell University, Ithaca, NY 14853, USA and Department of Population Medicine and Diagnostic Sciences, Cornell University, Ithaca, NY 14853, USA. Department of Anthropology, Northwestern University, Evanston, IL 60208, USA
References
- Jepson W. Measuring ‘no-win’ waterscapes: experience-based scales and classification approaches to assess household water security in colonias on the US–Mexico border. Geoforum. 2014;51:107–120. [Google Scholar]
- Kosmiski L. Energy expenditure in HIV infection. American Journal of Clinical Nutrition. 2011;94(6):1677S–1682S. doi: 10.3945/ajcn.111.012625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesho E, Gey D. Managing issues related to antiretroviral therapy. American Family Physician. 2003;68(4):675–686. [PubMed] [Google Scholar]
- Lule J, Mermin J, Ekwaru J, Malamba S, Downing R, Ransom R, Nakanjako D, Wafula W, Hughes P, Bunnell R, Kaharuza F, Coutinho A, Kigozi A, Quick R. Effect of home-based water chlorination and safe storage on diarrhea among persons with human immunodeficiency virus in Uganda. The American Journal of Tropical Medicine and Hygiene. 2005;73(5):926–933. [PubMed] [Google Scholar]
- Stevenson E, Greene L, Maes K, Ambelu A, Tesfaye Y, Rheingans R, Hadley C. Water insecurity in 3 dimensions: an anthropological perspective on water and women’s psychosocial distress in Ethiopia. Social Science & Medicine. 2012;75(2):392–400. doi: 10.1016/j.socscimed.2012.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A, Kakuhikire B, Mushavi R, Vořechovská D, Perkins J, McDonough A, Bangsberg D. Population-based study of intra-household gender differences in water insecurity: reliability and validity of a survey instrument for use in rural Uganda. Journal of Water and Health. 2016;14(2):280–292. doi: 10.2166/wh.2015.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF & World Health Organization. Joint Monitoring Programme for Water Supply and Sanitation. WHO; Geneva, Switzerland: 2006. Core Questions on Drinking Water and Sanitation for Household Surveys. [Google Scholar]
- WaterAID. Integrated Approach to HIV and Water, Sanitation, and Hygiene in Southern Africa: A Gap and Needs Assessment. SAfAIDS; Harare, Zimbabwe: Anglo-American Group Foundation; London, UK: 2014. p. 50. [Google Scholar]
- Webb P, Iskandarani M. Water Insecurity and the Poor: Issues and Research Needs. Discussion Papers on Development Policy. ZEF, University of Bonn; Bonn, Germany: 1998. [Google Scholar]
- Weiser S, Young S, Cohen C, Kushel M, Tsai A, Tien P, Hatcher A, Frongillo E, Bangsberg D. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. The American Journal of Clinical Nutrition. 2011;94(6):1729S–1739S. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO/UNICEF. Joint Water Supply and Sanitation Monitoring Programme. WHO; Geneva, Switzerland: 2014. Progress on Drinking Water and Sanitation. [Google Scholar]
- Wutich A, Brewis A. Food, water, and scarcity: toward a broader anthropology of resource insecurity. Current Anthropology. 2014;55(4):444–468. [Google Scholar]