Abstract
Between 2001 and 2012, the number of unrelated donors registered worldwide increased from 7 to 21 million, and the number of public cord blood units increased to over 500,000. We addressed the question of whether this expansion resulted in higher percentages of patients reaching transplantation. Unrelated donor searches were evaluated for 3,124 eligible patients in the Netherlands in two cohorts (2001–2006, n=995; 2007–2012, n=2129), comparing results for patients of Northwestern European and non-Northwestern European origin. Endpoints were ‘donor found’ and ‘transplantation reached’. The substantial growth of the donor inventory over the period studied did not increase the median number of potential unrelated donors (n=7) for non-Northwestern European patients, but almost doubled the number for Northwestern European patients from 42 to 71. Before and after 2007, an unrelated donor or cord blood was identified for 91% and 95%, respectively, of Northwestern European patients and for 65% and 82% of non-Northwestern European patients (P<0.0001). Non-Northwestern European patients more often needed a cord blood transplant. The degree of HLA matching was significantly lower for non-Northwestern European patients (P<0.0006). The time needed to identify a donor decreased for both populations. The percentage of Northwestern European patients reaching transplantation increased from 77% to 83% and for non-Northwestern European patients from 57% to 72% (P=0.0003). The increase of the global inventory resulted in more transplants for patients lacking a family donor, although the quality and quantity of (potential) haematopoietic cell grafts for patients of a non-Northwestern European descent remained inferior, indicating the need for adaptation of recruitment.
Introduction
Allogeneic hematopoietic progenitor cell transplantation plays an important role in treatment of hemato-oncological diseases. For patients lacking a matched related donor, an unrelated donor (UD) or cord blood unit (CBU) may provide a valuable alternative. Alternative donors are identified through registries of volunteer unrelated donors or public cord blood banks. In the past decade, the identification and availability of UD and UCB have improved. Bone Marrow Donors Worldwide (BMDW), the file of registered unrelated donors, almost tripled (from 7.4 million donors in 2001 to over 21 million in December 2012), while the inventory of unrelated CBU grew from 87,000 in 2001 to over 500,000.1 To date (2016) the number of registered donors has increased to over 27 million, and currently over 650.000 CBU are registered. Increased knowledge of the HLA system, more well-typed donors, and the availability of several search-related software tools2–5 have facilitated and speeded up the efficiency of the search process.6–8 Simultaneously searching for a back-up donor can minimize the delay if a donor is unexpectedly not fit or unavailable to donate.9 Given these recent improvements, we set out to address the questions of whether a higher percentage of patients in need of an UD/CBU may actually reach transplantation nowadays, whether the time needed to identify an UD/CBU has decreased, and whether possible factors can be identified for potential improvement. We addressed the questions in a large cohort of 3,365 consecutive UD searches performed between 2001–2012 in the Netherlands, including searches for Dutch patients of Northwestern European (NWE) and non-Northwestern European (non-NWE) descent.
Methods
The patients and donor searches
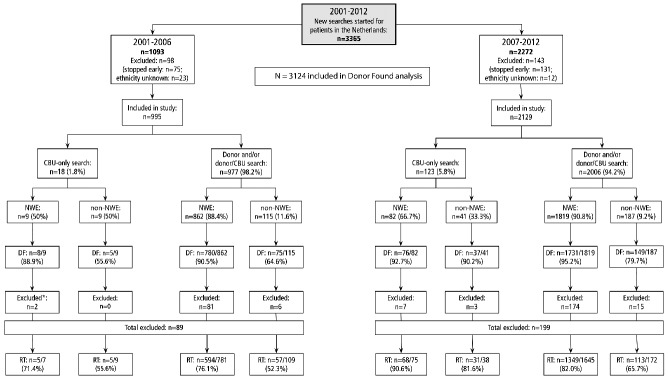
Europdonor Foundation, the Dutch Stem cell donor registry, coordinates the UD searches in the Netherlands, serving a population of 16.8 million inhabitants. There were eight adult and two pediatric stem cell transplantation units in 2012 in the Netherlands, and the number of new searches increased to approximately 500 annually. All UD and CBU searches performed from 2001 until 2012 for the patients of all Dutch transplantation centers were included (n=3,365, Figure 1) for the initial ‘donor found’ analysis, and divided into two periods: cohort I, 2001–2006 (n=1,093) and cohort II, 2007–2012 (n=2,272). Patients for whom a search was cancelled in less time than the median search time for the given year, and for whom no donor was yet identified were excluded for the ‘donor found’ analysis (cohort I, n=75; cohort II, n=131), leaving 3,124 evaluable search cases. Each cohort was split according to NWE and non-NWE descent. Patients were assigned to NWE or non-NWE background based upon self-identified descent.10 Descendants from the Netherlands, Germany, Belgium, Luxembourg, Great Britain, Ireland, and Scandinavia were considered NWE. The non-NWE group consisted of patients with self-reported genetic ancestry in Northern Africa (n=51), Sub-Saharan Africa (n=22), Turkey (n=87), Asia (n=54), Eastern Europe (n=4), Hispanic (n=9), or mixed (n=125). Patients with unknown ethnic background (n=35, of whom 14 reached transplantation) were excluded. Searches for combined donor/CBU and CBU-only and searches for NWE and non-NWE patients were analyzed separately.
Figure 1.
Overview of inclusion/exclusion in different stages of the search process. NWE: Northwestern European; non-NWE: non-Northwestern European; DF: donor found; CB: cord blood; RT: reached transplantation with unrelated donor or CB. *Patients for whom the procedure was cancelled for reasons not related to the search process were excluded (see Methods section).
Diagnoses were described in broad groups (Table 1). Overall, a donor was found for 2,861 (91%) of the patients (Table 2). For the subsequent analysis of ‘reaching transplantation’ we excluded 288 patients from the original cohorts I (n=89/995) and II (=199/2,129) for whom a donor was found but transplantation was cancelled for reasons not related to the search process (Figure 1). These reasons included never having reached remission/refractory disease (n=100), alternative therapy chosen (e.g. anti-thymocyte globulin for severe aplastic anemia, or randomized to a non-transplant arm in a study, n=88), autologous hematopoietic stem cell transplant (n=5), (extended) family donor available (n=23), indication changed/good clinical condition (n=27), and patient withdrawal (n=45). This left 2,836 patients for whom a successful search was performed (788 NWE and 118 non-NWE patients in cohort I, and 1,720 NWE and 210 non-NWE patients in cohort II).
Table 1.
Baseline characteristics of 2772 NWE and 352 non-NWE patients in the two search periods.
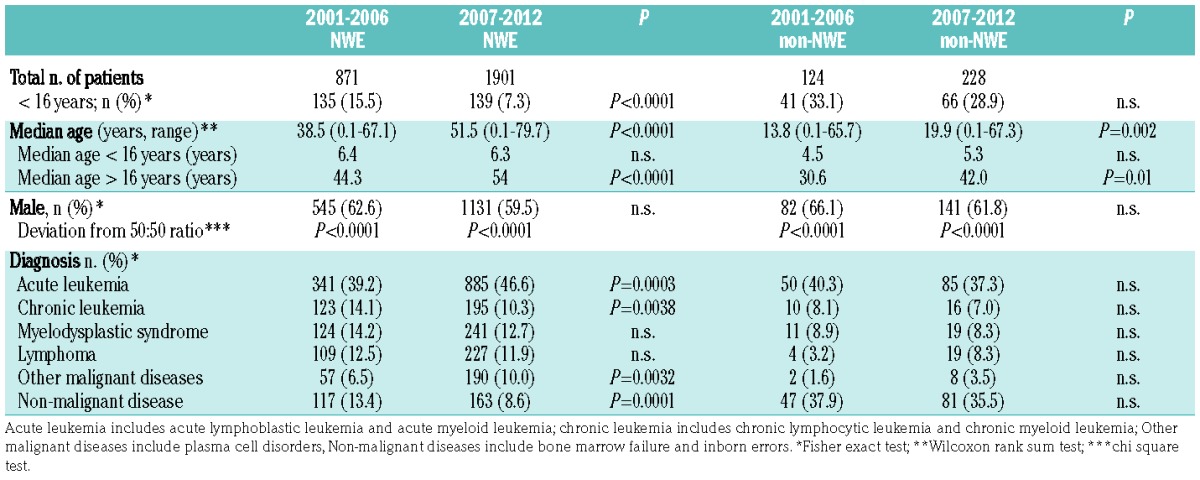
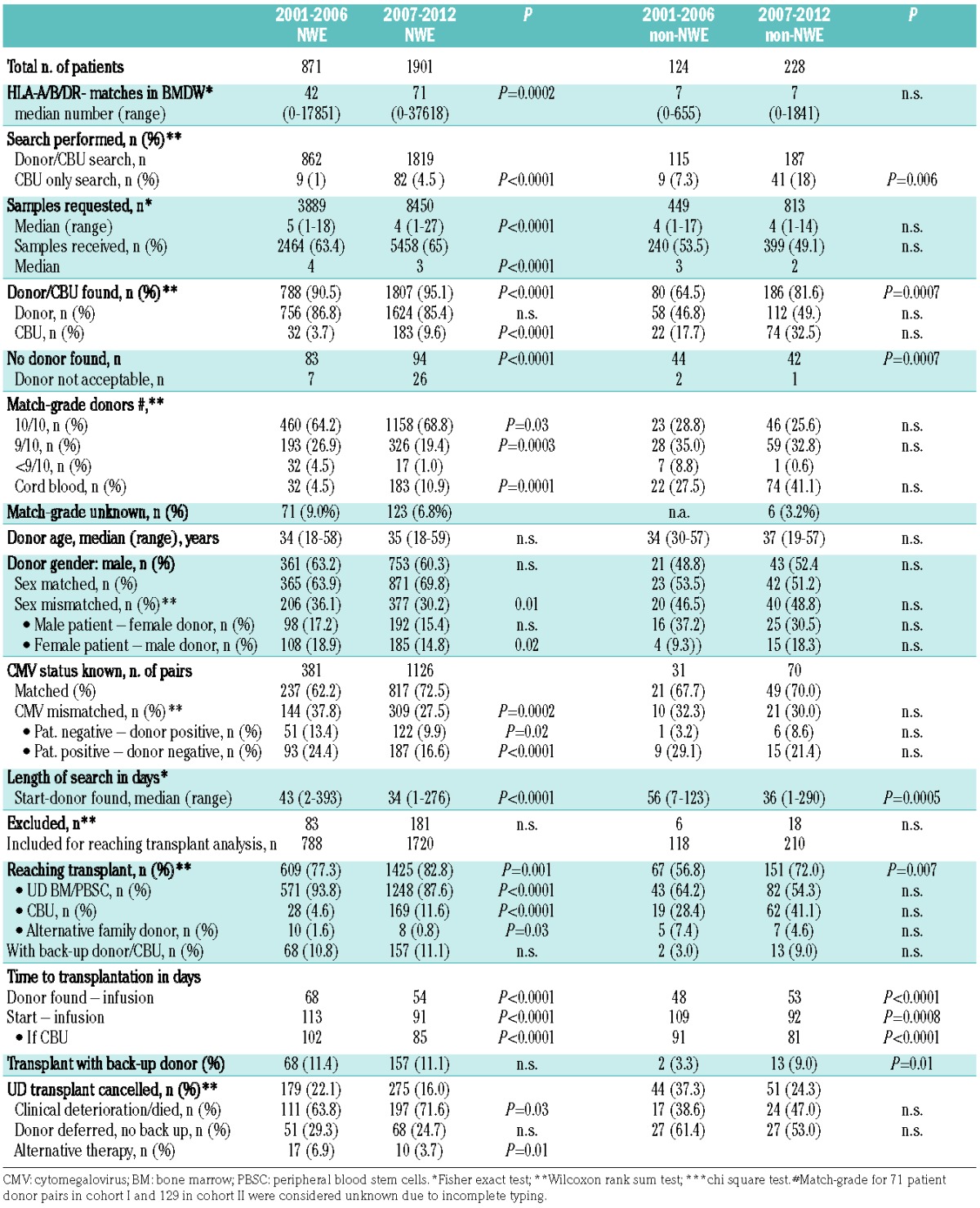
Table 2.
Characteristics of the search process and reaching transplantation for NWE and non-NWE patients in the two periods.
Search strategies
The basis for the UD/CBU search has been described elsewhere11,12 and was adjusted to new insights and better quality of the donor pool. Each new search, irrespectively of whether it was for an UD or CBU, started with estimation of the likelihood of finding an acceptable donor, taking into consideration the match-grade or haematopoietic cell source preferences of a center. These results were communicated to the center so that, in cases for which it was unlikely that an acceptable donor would be found, search strategies or treatment options could be adjusted to avoid unnecessary delay.
The search profile for an UD was based upon confirmed HLA-typing of the patient (HLA-A, B, C, DRB1, DQB1 high resolution), including a review of family typing, haplotype frequencies, allele frequencies, HLA-B/C-associations, and HLA-DRB1/DQB1 associations. Ethnic background and results of the BMDW regular match (mismatch runs if applicable) were taken into consideration. When appropriate, advice for a concurrent donor search within the extended family search was given.12 A 10/10 or 9/10 HLA-matched donor was usually preferred; however, in some transplant protocols (e.g. with reduced intensity conditioning) mismatched donors were not acceptable.
The search profile for a CBU was based on HLA-A, -B serological (split) level, and -DRB1 at high resolution and the minimum total nucleated cell count based on the recipient’s body weight, in accordance with local protocols.13 If no 6/6 or 5/6 mismatched units with sufficient total nucleated cells were identified, a run for two mismatches was performed, for both single and double CBU searches.
In the selection of donors for verification typing, non-HLA factors (age, gender, ABO group, cytomegalovirus status, previous donation) were considered. Verification typing of a prospective UD was performed for HLA-A, B, C, DRB1, DQB1 high resolution by the center; for the selection of a CBU the minimum HLA typing requirements were HLA-A and –B on a serological split level and HLA-DRB1 at high resolution, usually performed upon request by the cord blood bank. In this study, for a number of patients, HLA-C was not typed due to local policies. Match-grade for these pairs (71 in cohort I and 129 in cohort II) were considered ‘unknown’.
Definitions
Donor found means that there was a donor or CBU meeting the valid HLA matching criteria of the center at that time. Length of search refers to the interval in days from the start of the search to the time of identifying an acceptable donor or CBU. If a search was cancelled after the median time necessary for a search in that particular year, the outcome was considered No donor found: the search remained included in the No donor found-group.
Statistical analysis
Statistical analyses were performed using R version 2.15.1 (R Foundation for Statistical Computing). We used the chi square test, Fisher exact test (two-tailed) and Wilcoxon rank sum test to measure association and differences and the Pearson product-moment to determine correlations. A P-value of 0.05 or less was considered statistically significant.
Institutional Review Board approval
Dutch Transplant Centers are responsible for obtaining informed consent for (anonymized) data analysis and data exchange from all patients referred for UD searches. Additional Institutional Review Board approval to perform this study was not necessary.
Results
The baseline characteristics of NWE (n=2,772) and non-NWE (n=352) patients are presented in Table 1. The distribution of NWE and non-NWE patients did not differ significantly over time between the two cohorts (13% non-NWE in cohort I, and 11% non-NWE in cohort II). Data for non-NWE and mixed background patients were also analyzed separately, but showed similar outcome results and no significant differences between groups. The median age of patients increased significantly over time, mainly due to more elderly NWE patients. Non-NWE patients remained significantly younger than NWE patients in both periods (P<0·0001). Indications for transplantation changed over time. The proportion of NWE patients with chronic myeloid leukemia (P=0.0001) and inborn errors (P=0.0003) decreased while the proportion of (elderly) NWE patients with acute myeloid leukemia (P<0.0001) and plasma cell malignancies (P=0.002) increased significantly. The distribution of ethnic backgrounds of non-NWE patients in cohorts I and II was similar.
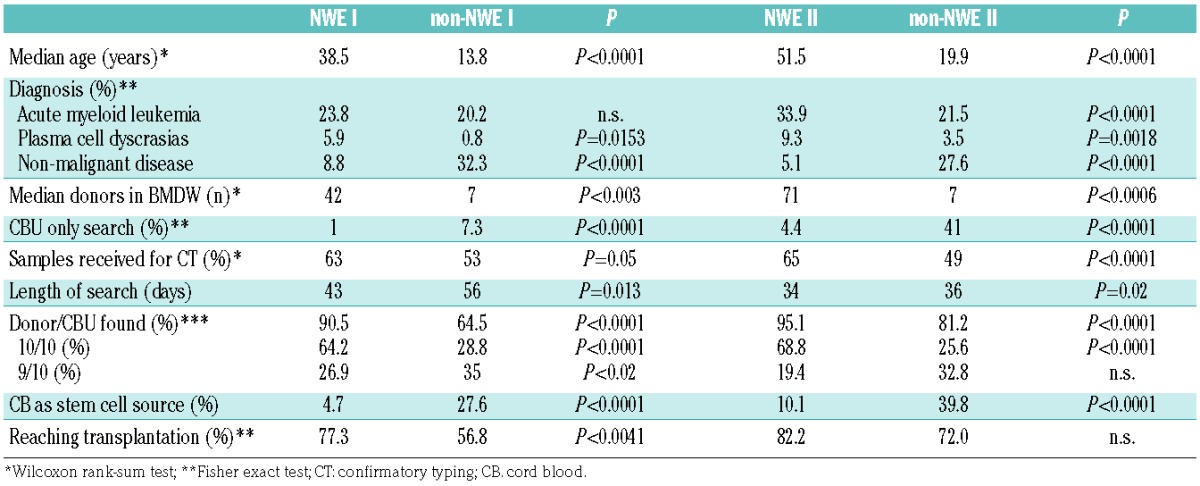
The characteristics of the search process are reported in Table 2. The median number of potential donors increased from 42 to 71 only for NWE patients (P=0.004) and remained at seven for non-NWE patients. A preferred CBU-only search was significantly more often performed for non-NWE patients (P<0·0001, Table 3).
Table 3.
Major differences between results for NWE and non-NWE patients in the two periods (I: 2001–2006, II: 2007–2012).
Donor found
A donor was found for 2,861 patients (91%). Significantly more UD/CBU were found in cohort II (P<0.0001) for both NWE and non-NWE patients (Table 2). In cohort I, an UD/CBU was identified for 91% of NWE patients and 65% of non-NWE patients. In cohort II, an UD/CBU was identified for 95% of NWE and 82% of non-NWE patients. Cord blood as an alternative haematopoietic cell source was needed more frequently for non-NWE patients in both cohorts (P<0.0001), although better matched (6/6) units were more often found for NWE patients (P<0.002, Online Supplementary Data). The amount of CBU identified for non-NWE patients almost doubled over time (18%–33%).
Grade of HLA-matching and aspects of non-HLA-matching
Major differences in match-grade were observed between NWE and non-NWE patients. As far as concerns non-NWE patients, fewer 10/10 HLA-matched or 9/10 HLA-matched donors were identified in cohort II than in cohort I. A ≥9/10 donor was found for at least 91% of NWE patients in cohort I and 88% in cohort II, compared to 64% of non-NWE patients in cohort I and 58% non-NWE patients in cohort II (Table 2).
The median time to identify a donor in a combined donor/CBU search for NWE patients was 43 days in cohort I and 34 days in cohort II. The same improvement was also seen for non-NWE patients (median of 56 and 36 days in cohort I and II, respectively, Table 3).
A CBU-only search was performed upon request of the centers for 18 patients in cohort I (2%) and 123 patients in cohort II (6%). Preferred CBU-only searches were performed significantly more often for non-NWE patients in both cohorts. A preferred CBU search, despite the availability of a fully matched UD, was performed for a few non-NWE patients (1 and 2 patients in cohort I and II, respectively) and some NWE patients (5 and 17 patients in cohort I and II, respectively).
Other characteristics that may affect transplant outcome, such as donor-recipient gender disparity, reduced over time for NWE patients but not for non-NWE patients in cohort II. Cytomegalovirus status mismatches between the recipient-donor pairs decreased significantly for NWE patients but not for non-NWE patients.
The donor searches for the patients excluded from the ‘reached transplantation’ analysis (89 in cohort I and 199 in cohort II, see Methods section) did not differ in length (median 42 days and 35 days, respectively). No acceptable UD/CBU was identified for 127/995 patients (13%) in cohort I and 136/2124 (6%) patients in cohort II. The median search time was longer for these patients than those in the ‘donor found’ group (P<0·0001, data not shown).
Reaching transplantation
Despite a successful donor search, Transplant Centers cancelled procedures for 89 patients in cohort I and 199 patients in cohort II, because the patients clinically deteriorated or died (Table 2). There was no correlation between length of search and whether or not a transplant was actually performed. The time from starting the search to transplantation was significantly shorter for patients receiving a cord blood graft in cohort II (P=0.0001). The percentage of transplanted patients increased significantly over time, with NWE patients more often reaching their intended transplantation. In total 77% (609/788) NWE and 57% (67/118) non-NWE eligible patients in cohort I and 82% (1,425/1,720) NWE and 72% (144/210) non-NWE eligible patients in cohort II reached transplantation. The increase in reaching transplantation was statistically significant for both NWE and non-NWE patients (P=0.001 and P=0.007, respectively) in the two cohorts, but not between NWE and non-NWE patients in cohort II. Overall NWE patients were transplanted with better matched donors (Figure 2), and cord blood as the source of hematopoietic cells was significantly more frequent in non-NWE patients. Fifteen patients in both cohorts were transplanted with a mismatched family donor (haploidentical), because the chosen donor (and back-up donor if identified) was no longer available. Overall, 240 patients received hematopoietic cells from a back-up donor (n=234) or a back-up cord blood unit (n=6), because the initial chosen donor was no longer available: 70 patients in cohort I (9.3% of NWE and 5.5% of non-NWE patients) and 170 patients in cohort II (9.8% of NWE and 7.8% of non-NWE patients).
Figure 2.
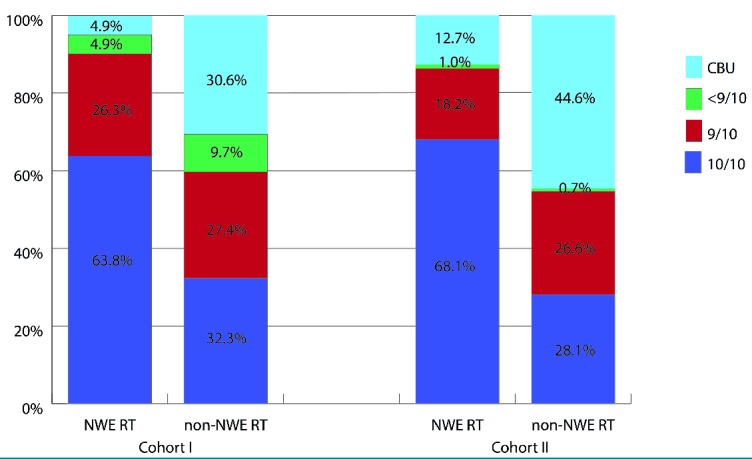
Match-grade of donors for NWE and non-NWE patients reaching transplantation (RT). Match-grade was unknown for 52 (8.7%) NWE patients in cohort I (2001-2006), 84(5.9%) NWE patients in cohort II (2007–2012), and 5 (3.5%) non-NWE patients in cohort II (2007–2012).
Discussion
In the last decade, substantial investments14 resulted in an increase of the worldwide hematopoietic progenitor cell donor pool and improvement of the quality of donor HLA typing. However, the availability of alternative donors, especially for patients of non-European descent15,16 remains concerning. Currently, for a Dutch NWE patient a median number of 71 potentially matched donors are listed, often allowing selection for non-HLA characteristics (e.g., age, gender, cytomegalovirus status) that may improve transplant outcome. In contrast, we found that the number of potentially matched donors for our non-NWE patients remained low: a median number of seven UD per patient. We addressed the question of whether the above-mentioned developments resulted in a higher percentage of transplants for Dutch patients. Overall, we observed that the percentages of patients reaching transplantation among both NWE and non-NWE patients in the period 2007–2012 were higher than those in the search period before 2007. However, the probability of identifying a 10/10 matched donor for non-NWE patients has not improved, while a significant advantage for NWE patients has become apparent (Table 3). The probability of finding a CBU with at least a 4/6 match increased over time for non-NWE patients, but here also the degree of matching appeared significantly less optimal than that for the NWE patients in our study. Thirty percent of non-NWE patients received cord blood grafts, compared to 10% of NWE patients. Cord blood is currently increasingly used in patients with very poor risk, acute leukemia, needing an immediate transplant after having obtained remission, or children with inborn errors, other than hemoglobinopathies.12,17 CBU are almost instantly available and require less stringent HLA matching criteria, but are associated with a higher rate of graft failure and delayed hematopoietic recovery.18,19 Studies have suggested that the outcome of cord blood grafting is better when the CBU contains higher numbers of cells, or when double CBU grafts, and/or better HLA-C matched grafts are used.20–24 While allele level matching was recently found to be associated with better transplant outcomes, high resolution typing for HLA-A-B-C and DRB1 would probably show 8/8 matching in only 10% of recipient/cord blood pairs.25 Requiring a higher level of matching for cord blood will result in fewer matching units, in particular for non-NWE patients.
Matching for HLA-DPB1 is currently not mandatory in Dutch transplant protocols. The likelihood of being DPB1-matched is approximately 20%, while approximately 50% permissive HLA-DPB1 mismatches would lower transplant mortality.26 DPB1 selection might be considered in the future, but will be less feasible for non-NWE patients given the restricted numbers of available donors allowing no choices.
Gragert et al. described a theoretical model based on population genetics for calculating the likelihood of finding a well-matched UD or CBU for patients of different ethnic background in the USA.15 Donor availability, inconsistent typing results and donor medical eligibility were taken into account. Their model is based on donor and cord blood data in the BeTheMatch registry itself, representing approximately 50% of the global inventory. They calculated a more than 95% likelihood of identifying an UD/CBU for both white and African-American patients, which is possibly an overestimate. Using 100% of the global inventory,1 we found an acceptable UD/CBU with a match-grade of at least 7/8 for 95% of NWE patients and 82% of non-NWE patients in the Netherlands. The clinical “real life” nature of our study may explain the difference, in that we searched for actual patients instead of conducting a theoretical exercise. The assumption that the donor population represents a true reflection of the patient population might overestimate the probability of finding an acceptable UD/CBU, in particular for patients with different ethnic backgrounds.
Population heterogeneity is present across the continents, but there are also unique HLA combinations at a national level, probably originating from former colonialism and more recent global migration. Cord blood offers the opportunity for a reasonable alternative as a less mismatched graft, and ethnic minorities are generally willing to donate cord blood to a public bank. However, a mismatched donor or CBU is not always an acceptable alternative. In this light, preliminary results of recent and ongoing studies indicate that the role of extended family (or haploidentical) donors could become clearer in the future.
All patients for whom no donor was found in our study had one or more rare alleles, uncommon HLA-B-C/DRB1-DQB1 associations, or a combination of these, often originating from a mixed racial background. A similar observation was reported by Testi et al.,27 who identified a 9/10-or 10/10-matched donor for 75% of their 315 patients, who had a high frequency allele. In contrast Grubic et al.28 reported having found a 9/10- or 10/10-matched donor for 95% of 105 Croatian patients, but their cohort only consisted of patients who were actually transplanted. The genetic heterogeneity of a population apparently also plays a role.
A weakness of our study is that the proportions of non-NWE patients in both cohorts (13% and 11%) were small and so confounding factors are possible. However, we have no indication that the findings were influenced by factors such as relapse, untimely referral, more withdrawals, or financial aspects. Unfortunately, the proportion of donors from ethnic minorities in the various donor registries is not recorded.29
In more recent years, the significantly shorter search time, observed for both NWE and non-NWE patients, may be a reason for fewer cancellations. The cancellation rate, due to clinical deterioration of the patient after a donor had been found, preventing the patient from undergoing transplantation, was approximately 30% in the period 1991–2000,12 and only 10% in the years after 2007. This demonstrates the importance of time, in particular in adult patients with high-risk leukemia.30–32 Future complete, high-resolution HLA typing and provision of additional donor characteristics could theoretically minimize the length of a search to a single day,33,34 and probably further reduce the rate of transplant cancellations due to relapsed malignancies. This, however, may not help non-NWE patients, since the limited number of registered, available and suitable non-NWE donors in the national and international registries35–38 highlights the need for strategic recruitment of both UD and CBU,39 and for methods to prevent untimely opt-out of donors, in particular those from ethnic minorities.40 Targeted donor recruitment, with personal and written native speaker support, and through social media, is being increasingly practiced.41 Furthermore, addressing misconceptions about donation add to donor commitment, and improve chances for all patients, but in particular non-NWE patients, to receive optimal allogeneic stem cell grafts.40 The subject is on the agenda of registries united in the World Marrow Donor Association.
Conclusions
Improved efficiency of searches for hematopoietic stem cell donors is associated, overall, with more NWE and non-NWE patients reaching their intended transplantation. However, we conclude from this large retrospective study that the increase of the global inventory and the major efforts and investments to improve the search process have resulted in a strong benefit mainly for NWE patients. For non-NWE patients, the probability of identifying a well-matched UD has not increased over time and non-NWE patients more often rely on CBU as an alternative source of hematopoietic stem cells. In addition, the match-grade for both UD and CBU is less optimal for non-NWE patients. In concordance with others, our findings in successive cohorts of non-NWE patients are strong confirmation of the need to expand the global inventory, focusing on donors and grafts from underrepresented ethnicities.
Supplementary Material
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/102/1/176
References
- 1.BMDW.org [Internet]. Leiden: Bone Marrow Donors Worldwide; [updated 25 January 2016; cited 1 February 2016]. BMDW Statistics, Cord Blood Registries, and Stem Cell Donor Registries. Available from: https://www.bmdw.org/bmdw/news [Google Scholar]
- 2.Mori M, Graves M, Milford EL, Beatty PG. Computer program to predict likelihood of finding an HLA-matched donor: methodology, validation, and application. Biol Blood Marrow Transplant. 1996;2(3): 134–144. [PubMed] [Google Scholar]
- 3.Spellman S, Setterholm M, Maiers M, et al. Advances in the selection of HLA-compatible donors: refinements in HLA typing and matching over the first 20 years of the National Marrow Donor Program Registry. Biol Blood Marrow Transplant. 2008;14(9 Suppl):37–44. [DOI] [PubMed] [Google Scholar]
- 4.Bochtler W, Beth M, Eberhard HP, Mueller CR. OptiMatch® - a universally configurable HLA matching framework. [abstract P-094]. Tissue Antigens. 2008;71:265–398.18325010 [Google Scholar]
- 5.Eberhard HP, Feldmann U, Gerlach A, Bochtler W, Mueller CR. Demonstrating the accuracy of the OptiMatch® prognostic system for donor selection. [abstract]. International Donor Registry Conference; 2008 Apr 18–19; Bern, Switzerland. [Google Scholar]
- 6.Lown R, Shaw BE. Beating the odds: factors implicated in the speed and availability of unrelated haematopoietic cell donor provision. Bone Marrow Transplant. 2013;48(2):210–219. [DOI] [PubMed] [Google Scholar]
- 7.Tiercy J-M, Nicoloso G, Passweg J, et al. The probability of identifying a 10/10 HLA allele-matched unrelated donor is highly predictable. Bone Marrow Transplant. 2007;40(6):515–522. [DOI] [PubMed] [Google Scholar]
- 8.Gourraud PA, Balère ML, Faucher C, et al. HLA phenotypes of candidates for HSCT: comparing transplanted versus non-transplanted candidates, resulting in the predictive estimation of the probability to find a 10/10 HLA matched donor. Tissue Antigens. 2014;83(1):17–26. [DOI] [PubMed] [Google Scholar]
- 9.Van Walraven SM, Heemskerk MB, Lie JL, et al. The importance of identifying a back-up donor for unrelated stem cell transplantation. Bone Marrow Transplant. 2005;35(5): 437–440. [DOI] [PubMed] [Google Scholar]
- 10.Sankar P, Cho MK. Toward a new vocabulary of human genetic variation. Science. 2002;298(5597):1337–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heemskerk MB, van Walraven SM, Cornelissen JJ, et al. How to improve the search for an unrelated haematopoietic stem cell donor. Faster is better than more! Bone Marrow Transplant. 2005;35(7):645–652. [DOI] [PubMed] [Google Scholar]
- 12.Oudshoorn M, Cornelissen JJ, Fibbe WE, et al. Problems and possible solutions in finding an unrelated bone marrow donor. Results of consecutive searches for 240 Dutch patients. Bone Marrow Transplant. 1997;20(12):1011–1017. [DOI] [PubMed] [Google Scholar]
- 13.Somers JA, Brand A, van Hensbergen Y, et al. Double umbilical cord blood transplantation: a study of early engraftment kinetics in leukocyte subsets using HLA-specific monoclonal antibodies. Biol Blood Marrow Transplant. 2013;19(2):266–273. [DOI] [PubMed] [Google Scholar]
- 14.Bart T. Cost effectiveness of cord blood versus bone marrow and peripheral blood stem cells. Clinicoecon Outcomes Res. 2010:2; 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gragert L, Eapen M, Williams E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371(4):339–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barker JN, Byam CE, Kernan NA, et al. Availability of cord blood extends allogeneic hematopoietic stem cell transplant access to racial and ethnic minorities. Biol Blood Marrow Transpant. 2010;16(11):1541–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boelens JJ, Aldenhoven M, Purtill D, et al. Outcomes of transplantation using various hematopoietic cell sources in children with Hurler syndrome after myeloablative conditioning. Blood. 2013;121(19):3981–3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barker JN, Scaradavou A, Stevens CE. Combined effect of total nucleated cell dose and HLA match on transplantation outcome in 1061 cord blood recipients with hematologic malignancies. Blood. 2010;115(1):1843–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brunstein CG, Gutman JA, Weisdorf DJ, et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood. 2010;116(22):4693–4699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danby R, Rocha V. Improving engraftment and immune reconstitution in umbilical cord blood transplantation. Front Immunol. 2014;5:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ballen K, Gluckman E, Broxmeyer H. Umbilical cord blood transplantation: the first 25 years and beyond. Blood. 2013;122(4):491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eapen M, Klein JP, Ruggeri A, et al. Impact of allele-level HLA matching on outcomes after myeloablative single unit umbilical cord blood transplantation for haematologic malignancy. Blood. 2014;123(1):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Somers JA, Braakman E, van der Holt B, et al. Rapid induction of single donor chimerism after double umbilical cord blood transplantation preceded by reduced intensity conditioning: results of the HOVON 106 phase II study. Haematologica. 2014;99(11): 1753–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Bourgeois A, Mohr C, Guillaume T, et al. Comparison of outcomes after two standards-of-care reduced-intensity conditioning regimens and two different graft sources for allogeneic stem cell transplantation in adults with hematologic diseases: a single-center analysis. Biol Blood Marrow Transplant. 2013;19(6):934–939. [DOI] [PubMed] [Google Scholar]
- 25.Oran B, Cao K, Saliba RM, et al. Better allele-level matching improves transplant-related mortality after double cord blood transplantation. Haematologica. 2015;100(10):1361–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fleischhauer K, Fernandez-Viña MA, Wang T, et al. Risk associations between HLA-DPB1 T-cell epitope matching and outcome of unrelated hematopoietic cel transplantation are independent of HLA-DPA1. Bone Marrow Transplant. 2014;49(9):1176–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Testi M, Andreani M, Locatelli F, et al. Influence of the HLA characteristics of Italian patients on donor search outcome in unrelated hematopoietic stem cell transplantation. Tissue Antigens. 2014;84(2): 198–205. [DOI] [PubMed] [Google Scholar]
- 28.Grubic Z, Jankovic KS, Maskalan M, et al. HLA allele and haplotype polymorphisms among Croatian patients in an unrelated hematopoietic stem cell donor search program. Transpl Immunol. 2014;31(3):119–124. [DOI] [PubMed] [Google Scholar]
- 29.Hollenbach JA, Saperstein A, Albrecht M, et al. Race, ethnicity and ancestry in unrelated transplant matching for the National Marrow Donor Program: a comparison of multiple forms of self-identification with genetics. PlosOne. 2015;10(8):e0135960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Confer DL, Abress LK, Navarro W, Madrigal A. Selection of adult unrelated hematopoietic stem cell donors: beyond HLA. Biol Blood Marrow Transplant. 2010;16(1 Suppl): S8–S11. [DOI] [PubMed] [Google Scholar]
- 31.Gratwohl A, Baldomero H, Aljurf M, et al. Hematopoietic stem cell transplantation. A global perspective. JAMA. 2010;303(16): 1617–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mawad R, Gooley TA, Sandhu V, et al. Frequency of allogeneic hematopoietic cell transplantation among patients with high-or intermediate-risk acute myeloid leukemia in first complete remission. J Clin Oncol. 2013;31(31):3883–3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gabriel C, Fuerst D, Fae I, et al. HLA typing by next-generation sequencing – getting closer to reality. Tissue Antigens. 2014;83(2):65–75. [DOI] [PubMed] [Google Scholar]
- 34.Lind C, Ferriola D, Mackiewicz K, Papazoglou A, Sasson A, Monos D. Filling the gaps – the generation of full genomic sequences for 15 common and well-documented HLA class I alleles using next-generation sequencing technology. Hum Immunol. 2013;74(3):325–329. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt AH, Stahr A, Baier D, Schumacher S, Ehninger G, Rutt C. Selective recruitment of stem cell donors with rare human leukocyte antigen phenotypes. Bone Marrow Transplant. 2007;40(9):823–830. [DOI] [PubMed] [Google Scholar]
- 36.Majhail NW, Nayyar S, Burton Santibanez ME, Murphy EA, Denzen EM. Racial disparities in hematopoietic cell transplantation in the United States. Bone Marrow Transplant. 2012;47(11):1385–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lown RN, Marsh SGE, Switzer GE, Latham KA, Madrigal JA, Shaw BE. Ethnicity, length of time on the register and sex predict donor availability at the confirmatory typing stage. Bone Marrow Transplant. 2014;49(4):525–531. [DOI] [PubMed] [Google Scholar]
- 38.Dehn J, Arora M, Spellman S, et al. Unrelated donor hematopoietic cell transplantation: factors associated with a better HLA match. Biol Blood Marrow Transplant. 2008;14(12):1334–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dehn J, Buck K, Maiers M, et al. 8/8 and 10/10 high-resolution match rate for the Be The Match Unrelated Donor Registry. Biol Blood Marrow Transplant. 2015;21(1): 137–141. [DOI] [PubMed] [Google Scholar]
- 40.Switzer GE, Bruce JE, Myaskovsky L, et al. Race and ethnicity in decisions about unrelated hematopoietic stem cell donation. Blood. 2013;121(8):1469–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmidt AH, Solloch UV, Baier D, et al. Criteria for initiation and evaluation of minority donor programs and application to the example of donors of Turkish descent in Germany. Bone Marrow Transplant. 2009; 44(7):405–412. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.