Abstract
Background
The diagnosis of ventilator-associated pneumonia (VAP) remains time-consuming and costly, the clinical tools lack specificity and a bedside test to exclude infection in suspected patients is unavailable. Breath contains hundreds to thousands of volatile organic compounds (VOCs) that result from host and microbial metabolism as well as the environment. The present study aims to use breath VOC analysis to develop a model that can discriminate between patients who have positive cultures and who have negative cultures with a high sensitivity.
Methods/design
The Molecular Analysis of Exhaled Breath as Diagnostic Test for Ventilator-Associated Pneumonia (BreathDx) study is a multicentre observational study. Breath and bronchial lavage samples will be collected from 100 and 53 intubated and ventilated patients suspected of VAP. Breath will be analysed using Thermal Desorption – Gas Chromatography – Mass Spectrometry (TD-GC-MS). The primary endpoint is the accuracy of cross-validated prediction for positive respiratory cultures in patients that are suspected of VAP, with a sensitivity of at least 99% (high negative predictive value).
Discussion
To our knowledge, BreathDx is the first study powered to investigate whether molecular analysis of breath can be used to classify suspected VAP patients with and without positive microbiological cultures with 99% sensitivity.
Trial registration
UKCRN ID number 19086, registered May 2015; as well as registration at www.trialregister.nl under the acronym ‘BreathDx’ with trial ID number NTR 6114 (retrospectively registered on 28 October 2016).
Keywords: Ventilator-associated pneumonia, Breath analysis, Volatile organic compounds, Metabolomics, Sensitivity, Specificity
Background
Ventilator-associated pneumonia (VAP) is a frequent complication of mechanical ventilation in the Intensive Care Unit (ICU) [1–3] and the associated morbidity results in substantial healthcare costs [4, 5]. The diagnosis of VAP remains challenging as clinical, laboratory and radiological parameters are sensitive but non-specific for VAP and suffer from high inter-rater variability [6, 7]. A lower respiratory tract sample [bronchoalveolar lavage (BAL), endotracheal aspirate or protected specimen brush sample] is recommended for microbiological confirmation of clinically suspected VAP [8], but these results take days to become available and the procedures cannot be repeated frequently due to their invasiveness. As a result of this delay, patients are overtreated with antibiotics, as empiric antibiotic treatment is initiated immediately after obtaining a lower respiratory tract sample. Subsequent microbiological results help to tailor and deescalate antibiotic treatment [9], so the lower respiratory tract sample continues to be of crucial importance for diagnosing VAP.
There is need for a less invasive and more time-efficient diagnostic technique that ultimately reduces the amount of antibiotics used to treat suspected VAP. Clinical scoring systems, like the Clinical Pulmonary Infection Score (CPIS) [10] and biomarkers have been studied as means to exclude VAP, but so far these attempts have not resulted in a test that is suitable for current ICU practice [11–15].
Exhaled breath contains volatile organic compounds (VOCs); small volatile molecules that result from host or bacterial metabolism or are contaminants from the environment [16, 17]. Exhaled VOC profiles have been shown to differentiate between many different disease states and may therefore qualify as non-invasive biomarkers [18–21]. Capture of VOCs and exhaled breath analysis has proven to be safe and reliable in mechanically ventilated critically ill patients [22–24]. Data from in-vitro experiments suggest that the presence of bacteria may be detected based on a small panel of VOCs [17]. This concept was recently translated in vivo: ventilated patients with and without positive bacterial cultures of endotracheal aspirate could be discriminated based on exhaled VOCs [24].
The aim of this study is to determine whether molecular analysis of breath can be used to discriminate between patients that are suspected of VAP who have positive cultures and who have negative cultures with high sensitivity, thus having the potential to limit antibiotic use. Secondly, we hypothesize that molecular analysis of breath can be used to specifically detect the causative pathogen in patients that are suspected of VAP, offering the possibility of more targeted antibiotic therapy.
Methods
Design
‘BreathDx – Molecular Analysis of Exhaled Breath as Diagnostic Test for Ventilator–Associated Pneumonia’ is an international European multicentre observational cohort study in intubated and ventilated ICU patients suspected of VAP. Six ICUs of university hospitals in the Netherlands, the United Kingdom, Spain and Portugal are involved: the Academic Medical Centre (AMC) in Amsterdam; University Hospital South Manchester (UHSM), Salford Royal and Central Manchester University Hospitals in Manchester; Parc Tauli Hospital in Sabadell; and Sao Francisco Hospital/Nova Medical School in Lisbon. Patients are expected to be recruited from all six sites over an 18 to 24-month time period. The project is funded by the European Union (BreathDx – 611951).
Study population
Patients at one of the six involved ICUs that are clinically suspected of having VAP are eligible for the study. VAP is defined by (1) systemic changes [temperature >38 or <36.5 °C; white blood cell count <4,000 or >12,000/mm3]; and (2) chest abnormalities [new infiltrates on chest X-ray, purulent tracheal secretions]; and (3) positive microbiology results [25]. Inclusion criteria are (1) 18 years and older and (2) intubation and mechanical ventilation for > 48 h and (3) clinical suspicion of VAP (aforementioned systemic changes combined with chest abnormalities). Exclusion criteria include patients who: (1) are deemed clinically inappropriate to collect samples from (e.g. if they are receiving end-of-life care); or (2) are in strict isolation (e.g. Middle East Respiratory Syndrome, Ebola or resistant tuberculosis).
Study procedures
Patients will be recruited and samples collected within 24 h of the clinical suspicion of VAP. First breath samples will be collected, followed by bronchoscopy and bronchial lavage. Standard Operating Procedures (SOPs) will be in place at all sites in order to ensure samples are collected equally. Breath samples will be shipped within days after collection and shall be analysed within 2 weeks upon arrival. Previous results have shown breath samples can be stored for at least 14 days without loss of data [26]. The (mini) BAL samples are processed and frozen immediately after recruitment. When all (mini) BAL samples are collected they will be shipped on dry ice to remain conserved.
Breath sampling
Breath samples will be collected once (at time of recruitment) using a breath gas sampler (BGS, see Fig. 1) consisting of a pump (NMS020B 6VDC Micro Membranegas pump), a mass flow controller (Horiba STEC Z500), battery and charger (Panasonic LC-RA1212PG and IDEAL POWER PC170-2) all combined in a metal casing with operating display (Brooks Instrument 0254). Using this BGS and PTFE (PolyTetraFluoroEthylene) tubing (Swagelok, Warrington, UK), the exhaled breath is drawn from the sidearm of a T-piece connector inserted in the ventilator circuit distal of the HME filter and through a stainless steel sorbent tube (Markes International, Llantrisant, UK; and Gerstel, Mülheim an der Ruhr, Germany), adapted from Bos et al [23]. Subsequently the sorbent tubes will be transported for off-site analysis. The samples will be link-anonymised. Two pairs will be collected per patient and will be sent to two different laboratory locations for analysis (one pair to Philips Research, Eindhoven, the Netherlands and the other to Manchester Institute of Biotechnology, University of Manchester, Manchester, United Kingdom). For analysis at Philips Research the exhaled breath is collected using sorbent tubes packed with 300 mg Carbograph 5TD (Markes International, Llantrisant, UK) and 90 mg Tenax GR (Sigma-Aldrich Chemie B.V., Zwijndrecht, the Netherlands). The samples to be analysed at the Manchester Institute of Biotechnology are collected using sorbent tubes packed with 200 mg Tenax GR (Markes International, Llantrisant, UK). All samples are taken in duplicate. Breath samples are stored in a cold room immediately after collection. This sampling setup has shown to be safe and adequate for sample collection in ventilated ICU patients [18, 23, 27].
Fig. 1.

The breath gas sampler
Bronchoalveolar lavage
A (mini)-BAL sample will be obtained for microbiological analysis as soon as possible after collecting the breath samples (see Fig. 2). A syringe is connected to a bronchoscope or a 50 cm suctioning catheter and 20 mL 0.9% saline is injected in the airway. At least 4 mL is aspirated of which 1 mL is sent to the medical microbiology for routine cultures, leading to a semi-quantitative bacterial count with a cut-off of 104 colony forming units/mL defining a positive culture. An aliquot of the (mini)-BAL sample will be processed and stored for future analysis.
Fig. 2.
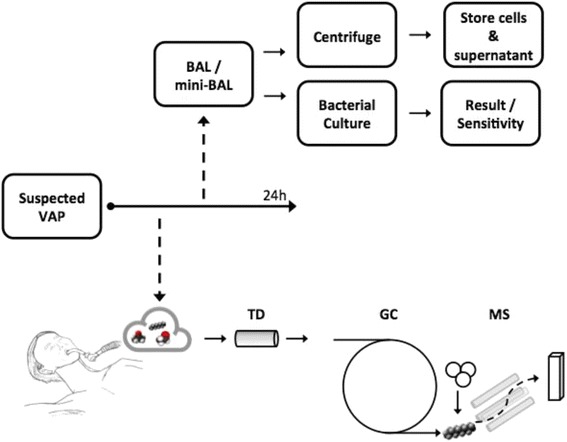
Overview of the sample collection
Gas chromatography and mass-spectrometry
The exhaled breath sample will be analysed using Thermal Desorption – Gas Chromatography – Mass-Spectrometry (TD-GC-MS). In order to separate, quantify and identify a wide range of volatiles in breath, different chromatographic set-ups at Eindhoven and Manchester are used. Both GC-MS analyses will result in a list of detected volatiles and their relative concentrations.
At Philips Research, the sorbent tubes are thermally desorbed at 225 °C (TDSA, Gerstel, Mülheim an der Ruhr, Germany) into the GC capillary column. Solvent venting mode is used to transfer the sample without loss to the packed liner (filled with Tenax TA) held at −55 °C which is subsequently heated to 280 °C. A cold trap (CTS2, Gerstel, Mülheim an der Ruhr, Germany) is used to minimize band broadening (initial temperature −150 °C, after 1.6 min heated to 220 °C). A capillary gas chromatograph (6890 N GC, Agilent, SantaClara, CA, USA) using a VF1-MS column (length 30 m × internal diameter 0.25 mm, film thickness 1 μm, 100% dimethyl-polysiloxane, Varian Chrompack, Middelburg, the Netherlands) is used with the following temperature program: 30 °C-hold 3.5 min, ramp 5 °C/min to 50 °C, hold 0 min, ramp 10 °C/min to 90 °C, ramp 15 °C/min to 130 °C, ramp 30 °C/min to 180 °C, ramp 40 °C/min to 280 °C, hold 1 min. A Time-of-Flight Mass Spectrometer (Pegasus 4D system, LECO, St. Joseph, Mi, USA) is used in the electron ionization mode at 70 eV, with a scan range of m/z 29–400 Da, scanning rate 20 scans/s. Gaseous calibration standards (10 ppmv acetone-D8, hexane-D14, toluene-D8, xylene-D10 in nitrogen, Air Products, Amsterdam, the Netherlands) are made by use of a home-built dilution system and loaded on adsorption tubes as an internal standard.
At Manchester Institute of Biotechnology sorbent tubes filled with Tenax GR are thermally desorbed at 280 °C (TD100, Markes International, Llantrisant, UK) into a cold trap to minimize band broadening (initial temperature −0 °C, after 2 min heated again to 280 °C). This will then be fed into a capillary gas chromatograph (7890B GC, Agilent, SantaClara, CA, USA) using a HP-5 ms Ultra Inert column (length 30 m × internal diameter 0.25 mm, film thickness 0.25 μm, (5%-Phenyl)-methylpolysiloxane, Agilent, SantaClara, CA, USA) with the following temperature program: 40 °C - hold 0 min, ramp 6 °C/min to 170 °C, hold 0 min, ramp 15 °C/min to 190 °C for a total time of 23 min. A Triple-Quad mass spectrometer (7010, Agilent, SantaClara, CA, USA) will be used in the electron ionization mode at 70 eV, with a scan range of m/z 40–500 Da, scanning rate 4 scans/s. A gaseous calibration standard (1 ppmv, 4-Bromofluorobenzene in nitrogen, Thames Restek, UK) will be loaded on adsorption tubes as an internal standard for 1 min at 20 ml/min. Additionally, to aid in retention time correction, an external standard containing a mixture of laboratory standard VOC chemicals (Sigma Aldrich, UK) will be sampled on separate tubes, either side of a breath sample.
Clinical data
Clinical data regarding patient characteristics, primary and secondary diagnoses, comorbidities, drug history, measures of disease severity such as Acute Physiology and Chronic Health Evaluation (APACHE) IV [28] and Simplified Acute Physiology Score (SAPS) II [29] ventilation data, CPIS [10], culture data, outcome variables (ICU/hospital length of stay, mortality) and adverse events will be collected.
Study outcomes
The primary endpoint is the accuracy of cross-validated prediction for positive respiratory cultures in patients that are suspected of VAP, with a sensitivity of at least 99% (high negative predictive value).
The secondary endpoints are: (1) the accuracy of cross-validated prediction for growth of a specific pathogen with a specificity of at least 90%; (2) GC-MS identified molecular markers that can distinguish between patients with and without microbiologically confirmed VAP with p <0.05 and a false discovery rate <0.05; (3) GC-MS identified molecular markers that can distinguish between patients with and without growth of specific pathogens during bacterial culture with p <0.05 and a false discovery rate <0.05; (4) accuracy of prediction within the subgroup of patients with and without a previous respiratory infection; (5) accuracy of prediction within the subgroup of patients intubated for less and more than 1 week.
Sample size calculation
The sample size calculation has been performed based on binomial distributions instead of normal approximations to this distribution [30]. With an expected sensitivity of 99% (almost 100% negative predictive value) we require the lower 95% confidence limit to be larger than 90% with 95% probability. 90% sensitivity is the absolute minimal in a discovery study such as this, for a lower sensitivity is clinically irrelevant and would not be clinically useful. With these figures, the required number of cases is estimated to be 61 [30]. Assuming a prevalence of 40% of positive cultures of bronchoalveolar lavage in patients that are clinically suspected of VAP [24], the total study sample size should be 153 subjects.
Statistical analysis
The GC-MS data are three-dimensional in nature, with ion counts for every combination of m/z value and retention time. The chromatogram represents the total ion count (TIC) measured by GC-MS as a function of retention time. The first step in pre-processing consists of correcting the chromatographic baseline, required for proper estimation of ion intensities and accurate molecule identification based on the mass spectra. Subsequently the data will be visually inspected to exclude contaminated samples. Contamination of the sampling tubes (e.g. due to loose fittings during transport) can severely distort the stored breath content. These tubes will be excluded from further analysis.
For peak detection we will use the method described by Smith et al. [31] implemented in the R-package XCMS [31–33]. It is currently the most cited pre-processing tool in the metabolomics literature [34]. The settings for peak detection will be determined as described by Smith et al. [31], using model peak widths that are considerably larger than the signal peak (1.5 – 4 times) for consistent signal-to-noise improvement [35].
The intensity of the internal standards toluene-d8 and 4-bromofluorobenzene will be used to normalize all other peaks in the GC-MS data of the two laboratories, respectively.
The retention time alignment in the XCMS package works very well for relatively small retention time shifts. For large shifts this method becomes inaccurate resulting in the loss of peaks in the final table and erroneous alignment of the samples. In our experiment the samples will be measured over a time span of at least 18 months. Therefore rather large retention time shifts can be expected. To account for the retention time shifts the following approach will be applied, which consists of two steps [27]. First the major part of the time shifts will be corrected by using anchor points (marker molecules), i.e. molecules with clearly identifiable mass spectra distributed over the full retention time window. Examples are isoprene, toluene and compounds from the internal standards. These molecules will be identified by comparing the measured mass spectra to the spectra published in the National Institute of Standards and Technology (NIST) chemistry web book database [36] using the dot-product function as similarity measure. According to Stein and Scott [37], this algorithm gives the best similarity estimate between mass spectra. The first raw retention time correction will be performed using a linear or quadratic fit to the retention times of the marker molecules. The second step in the approach will consist of fine alignment using the regular retention time correction of the XCMS package, as described by Smith et al. [31].
All the steps above will result in an ion-fragment peak table. Each row in the table corresponds with a sample. The first few columns will contain sample and patient data, such as sample data, age, gender and illnesses. The remaining columns will contain the abundances of the peaks or ion-fragments; typically there are a few thousand. This table will serve as input for extra quality checks and subsequent statistical analysis.
One of the quality checks will consist of comparing the two pairs of samples successively collected from each patient. The content of these duplicates should be equivalent, especially when compared to the content of other, arbitrary samples. Cosine similarity measures will be plotted into the histograms for duplicate samples and arbitrary samples. The equalities of the distributions in the histograms will be tested with the two-sided Kolmogorov–Smirnov test. Additionally the intensity of several common molecules between replicate samples will be analysed using Bland-Altman plots.
Samples measured on different GC-MS instruments are rarely identical due to multiple differing technical characteristics. Previous attempts to align data from different GC-MS machines have proved to be very complicated. Therefore the samples from different GC-MS machines will be aligned separately. For each GC-MS machine fragment averaging over the two consecutive samples will summarize peak intensities. In this way the number of breath features becomes roughly twice as large. Newly added features will be correlated to the existing features, since they are sequentially sampled from the same patient. The dependence between the features and the higher number of features puts higher strain on the statistical analysis.
The data can now be used for (1) data discovery, (2) untargeted analysis and (3) targeted analysis. Data discovery will consist of principle component analysis (PCA) on the log-transformed and scaled data, and Ward clustering on the 100 most abundant peaks eluting at least one second apart, as well as on the most relevant principle components.
Untargeted analysis will consist of building predictive models based on the data. The models will reduce the dimensionality of the dataset: the number of features is many times higher than the number of patients, increasing the risk of over-fitting. Additionally the features are not independent: several ion fragments originate from the same molecule. The statistical model needs to be able to deal with this. Finally breath data typically shows large variation in VOC abundance between, but also within individuals. Considering these characteristics of the data, we have chosen sparse partial least squares models to analyse the log-transformed data [38]. The small number of included patients will not allow data to be split into a training set and a validation set, although this is the preferred method. Instead permutation tests will be used to estimate the performance of the model.
In the targeted approach existing literature will be searched for potential biomarkers for VAP. The abundance of such molecules will be compared between patient groups using student t-tests or Mann–Whitney-Wilcoxon tests for normally and non-normally distributed data respectively. The important advantage of this approach is the low likelihood on false discoveries. The amount of comparisons is limited and previous findings will be validated.
In order to assess the influence of possible confounders (e.g. comorbidities, ventilator settings, medications) on the association between exhaled breath and the VAP the log odds ratios will be compared between a logistic regression model with the VOCs of interest as dependent variables and VAP (yes/no) as independent variable and the same model with the inclusion of the potential confounder as co-variate. When the log odds ratio shows a change of more than 10% the co-variate will be considered a confounder.
End of study definition
The study will end when the required sample size is reached.
Reporting
The results will be reported strictly following Standards for Reporting Diagnostic Accuracy (STARD) guidelines [39].
Discussion
This manuscript describes the protocol for a multicentre prospective observational study that aims to develop a diagnostic tool for discriminating between patients that are suspected of VAP who have positive cultures and who have negative cultures through breath analysis using TD-GC-MS. Additionally, we aim to describe patterns of VOCs in exhaled breath that are predictive of the presence of specific pathogens. Ultimately we strive for a diagnostic test with 99% sensitivity for culture positive VAP, which is required in an ICU setting where delayed initiation of adequate antibiotic therapy is unacceptable.
Several clinical challenges can be recognized for this study a priori. First, the reported incidence of VAP has declined over the last decade [40]. As recruitment depends on the clinical suspicion of VAP, this could slow the inclusion rate. The clinical definition for inclusion into the study could also be seen as a weakness of the study as clinical practice may vary from hospital to hospital. However, we have tried to include hospitals from a wide variety of settings and countries throughout Europe to cover the heterogeneity in clinical practice. This geographical variation may also introduce noise into the data collected by breath analysis as the environment contributes to exhaled VOCs [41, 42]. Another challenge concerns the secondary aim of this study to identify patterns of VOCs that are predictive of the presence of specific causative pathogens. A number of VOCs are already associated with certain pathogens. There is a large number of pathogens that can cause VAP [43] and the groups of patients are not likely to be infected with the same pathogen. This is a risk that is inherent to a prospective clinical study. We expect to find sufficiently large groups of patients for at least the most important pathogens in VAP: Pseudomonas aeruginosa, Staphylococcus aureus and Enterobacteriaceae [43].
There are also multiple analytical challenges. Patients will be recruited over a minimum 18-month period. As a result, the GC-MS platforms will have to be stable over this period of time when there is potential for column degradation that can change the retention time of VOCs. Several members of the consortium previously performed studies over similarly long periods of time and have developed statistical tools to correct for this shift in retention time [27]. The sensitivity of the mass spectrometer may also drift. This was a problem in previous studies and therefore an internal standard was included in the present protocol. As in any study that focuses on breath analysis there is always the challenge of statistical overfitting [44]. We expect to find several hundreds of VOCs in the breath of patients. These will be used as predictors for the presence of VAP. Such a high dimensional predictor matrix easily results in false discovery and therefore sufficient internal validation measures must be taken [45]. There, we suggest two approaches in this protocol. First, we aim to validate previously found markers. This limits the number of statistical comparisons and increases the changes on valid discoveries. Second, novel biomarkers are discovered using cross-validation and permutation tests.
The described protocol also has several strengths and is pragmatic in nature. The studied population is clinically very relevant as a treatment decision may be influenced by the outcome of the test. Using an unbiased approach, with patient recruitment in multiple European countries and breath analysis on multiple GC-MS platforms, this study allows for the development of a test that is applicable in a wide variety of hospitals. Special attention was given to analytical versatility; multiple sorbent beds are used and breath is analysed on two separate platforms that have complementary analytical strengths. There is also additional intellectual benefit; the results may be translated to other patients; the identified markers may also be studied in patients suspected of community- or hospital-acquired pneumonia. Another possibility for value within the results is the development of a continuous breath test that can warn the clinician that a patient is about to develop pneumonia.
The results from this study will have direct clinical implications. If the sensitivity of 99% is reached while maintaining a moderate to good specificity, antibiotic treatment can be withheld from a large proportion of VAP-suspected patients. With a prevalence of culture positive VAP of 40%, 48 out of every 100 patients would benefit in the scenario that a sensitivity of 99% and a specificity of 80% is obtained. Antibiotic therapy could be withheld in four patients in such a case. These figures improve with increased specificity at the pre-selected sensitivity and a lower prevalence of culture positive VAP.
In conclusion, we hypothesize that breath analysis can be used for discrimination between VAP suspected patients with and without microbiological positive cultures with a high sensitivity, and can be used to specifically detect the causative strain of bacteria.
Trial status
Patient recruitment for the BreathDx study is currently ongoing.
Acknowledgements
+A list of all members of the BreathDx Consortium: Waqar Ahmed, Antonio Artigas, Lieuwe D. J. Bos, Marta Camprubi, Luis Coelho, Paul Dark, Alan Davie, Emili Diaz, Gemma Goma, Timothy Felton, Stephen J. Fowler, Royston Goodacre, Hugo Knobel, Oluwasola Lawal, Jan-Hendrik Leopold, Ignacio Martin-Loeches, Tamara Nijsen, Pouline M. P. van Oort, Pedro Povoa, Craig Portsmouth, Nicholas J. W. Rattray, Guus Rijnders, Marcus J. Schultz, Ruud Steenwelle, Peter J. Sterk, Jordi Valles, Fred Verhoeckx, Anton Vink, Hans Weda, Tineke Winters, Tetyana Zakharkina.
Funding
This study is an investigator-initiated trial part of a project funded by the European Union: BreathDx – 611951. The funder has no role in the study design, data collection, analysis and design of the manuscript.
Availability of data and material
The detailed clinical data set will not be publically available to protect research subject privacy and confidentiality, in line with the ethical approval and patient consent obtained for this study.
Authors’ contributions
LDJB, SJF, PD and MJS designed the study. LDJB, TN and SJF wrote the study protocol. PMPvO, TN, HK, PD, TF, NJWR, OL, WA, CP, MJS, TZ, SJF and LDJB advised on study design and participated in the study protocol. All authors approved the study design. LDJB performed the power calculation. HW and SJF designed the statistical analysis plan. PMPvO and LDJB prepared the initial draft of this manuscript. All authors approved the submitted version of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The patient information letters, informed consent forms and the study protocol were approved by the institutional review boards (IRBs) of the individual institutions (IRB of the Academic Medical Centre Amsterdam, IRB of Parc Tauli Hospital in Sabadell; and the IRB of Sao Francisco Hospital/Nova Medical School in Lisbon) and for the three UK-based centres, by the National Research Ethics Service Committee North West – Greater Manchester South (REC reference 15/NW/0393) and the local Research and Development (R&D) offices at the different sites. As this study concerns patients lacking capacity, at time of inclusion formal assent will be sought with a designated consultee who is independent of the BRAVo study: this is likely to be the consultant directly responsible for the care of this particular patient. The independency of this physician enables the decision for recruitment to be solely in the patient’s best interest. Where the patient regains capacity, deferred consent will be obtained. In case the patient does not regain capacity, samples will not be discarded and can be used for research purposes.
Abbreviations
- AMC
Academic Medical Centre
- APACHE
Acute physiology and chronic health evaluation
- BAL
Bronchoalveolar lavage
- BGS
Breath gas sampler
- CPIS
Clinical Pulmonary Infection Score
- eV
electron volt
- GC
Gas Chromatography
- ICU
Intensive Care Unit
- m/z
Mass-to-charge ratio
- MS
Mass Spectrometry
- NIST
National Institute of Standards and Technology
- PCA
Principle component analysis
- ppmv
Parts per million by volume
- PTFE
PolyTetraFluoroEthylene
- SAPS
Simplified Acute Physiology Score
- STARD
Standards for reporting diagnostic accuracy
- TD-GC-MS
Thermal Desorption – Gas Chromatography – Mass Spectrometry
- TIC
Total ion count
- UHSM
University Hospital South Manchester
- UKCRN
United Kingdom Clinical Research Network
- VAP
Ventilator-associated pneumonia
- VOC
Volatile organic compound
Contributor Information
Pouline M. P. van Oort, Email: pouline.vanoort@gmail.com
on behalf of the BreathDx Consortium:
Waqar Ahmed, Antonio Artigas, Lieuwe D. J. Bos, Marta Camprubi, Luis Coelho, Paul Dark, Alan Davie, Emili Diaz, Gemma Goma, Timothy Felton, Stephen J. Fowler, Royston Goodacre, Hugo Knobel, Oluwasola Lawal, Jan-Hendrik Leopold, Ignacio Martin-Loeches, Tamara Nijsen, Pouline M. P. van Oort, Pedro Povoa, Craig Portsmouth, Nicholas J. W. Rattray, Guus Rijnders, Marcus J. Schultz, Ruud Steenwelle, Peter J. Sterk, Jordi Valles, Fred Verhoeckx, Anton Vink, Hans Weda, Tineke Winters, and Tetyana Zakharkina
References
- 1.Koenig SM, Truwit JD. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clin Microbiol Rev. 2006;19(4):637–657. doi: 10.1128/CMR.00051-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis KA. Ventilator-associated pneumonia: a review. J Intensive Care Med. 2006;21(4):211–226. doi: 10.1177/0885066606288837. [DOI] [PubMed] [Google Scholar]
- 3.Ego A, Preiser J-C, Vincent J-L. Impact of diagnostic criteria on the incidence of ventilator-associated pneumonia. Chest. 2014:1–28. doi:10.1378/chest.14-0610. [DOI] [PubMed]
- 4.Zimlichman E, Henderson D, Tamir O, et al. Health care–associated infections. JAMA Intern Med. 2013;173(22):2039. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 5.Bassetti M, Taramasso L, Giacobbe D, Pelosi P. Management of ventilator-associated pneumonia: epidemiology, diagnosis and antimicrobial therapy. Expert Rev Anti Infect Ther. 2012;10(5):585–596. doi: 10.1586/eri.12.36. [DOI] [PubMed] [Google Scholar]
- 6.Chastre J, Fagon J. State of the Art ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(23):867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 7.Bos LDJ, Martin-Loeches I, Artigas A. Innovations that could improve early recognition of ventilator-associated pneumonia. Intensive Care Med. 2014;40(9):1352–1354. doi: 10.1007/s00134-014-3356-y. [DOI] [PubMed] [Google Scholar]
- 8.Society AT. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 9.Woodhead MA, Arrowsmith J, Chamberlain-Webber R, Wooding S, Williams I. The value of routine microbial investigation in community-acquired pneumonia. Respir Med. 1991;85(4):313–317. doi: 10.1016/S0954-6111(06)80103-4. [DOI] [PubMed] [Google Scholar]
- 10.Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143(5 Pt 1):1121–1129. doi: 10.1164/ajrccm/143.5_Pt_1.1121. [DOI] [PubMed] [Google Scholar]
- 11.Palazzo SJ, Simpson T, Schnapp L. Biomarkers for ventilator-associated pneumonia: review of the literature. Hear Lung J Acute Crit Care. 2011;40(4):293–298. doi: 10.1016/j.hrtlng.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin-Loeches I, Bos LD, Povoa P, et al. Tumor necrosis factor receptor 1 (TNFRI) for ventilator-associated pneumonia diagnosis by cytokine multiplex analysis. Intensive Care Med Exp. 2015;3(1):26. doi: 10.1186/s40635-015-0062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conway Morris A, Kefala K, Wilkinson TS, et al. Diagnostic importance of pulmonary interleukin-1 and interleukin-8 in ventilator-associated pneumonia. Thorax. 2010;65:201–207. doi: 10.1136/thx.2009.122291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hellyer TP, Conway Morris A, McAuley DF, et al. Diagnostic accuracy of pulmonary host inflammatory mediators in the exclusion of ventilator-acquired pneumonia. Thorax. 2015;70(1):41–47. doi: 10.1136/thoraxjnl-2014-205766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilkinson TS, Conway Morris A, Kefala K, et al. Ventilator-associated pneumonia is characterized by excessive release of neutrophil proteases in the lung. Chest. 2012;142(December):1425–1432. doi: 10.1378/chest.11-3273. [DOI] [PubMed] [Google Scholar]
- 16.Schnabel RM, Boumans MLL, Smolinska A, et al. Electronic nose analysis of exhaled breath to diagnose ventilator-associated pneumonia. Respir Med. 2015. doi:10.1016/j.rmed.2015.09.014. [DOI] [PubMed]
- 17.Bos LDJ, Sterk PJ, Schultz MJ. Volatile metabolites of pathogens: a systematic review. PLoS Pathog. 2013;9(5):e1003311. doi: 10.1371/journal.ppat.1003311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bos LDJ, Schultz MJ, Sterk PJ. Exhaled breath profiling for diagnosing acute respiratory distress syndrome. BMC Pulm Med. 2014;14(1):72. doi: 10.1186/1471-2466-14-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fens N, Zwinderman AH, Van Der Schee MP, et al. Exhaled breath profiling enables discrimination of chronic obstructive pulmonary disease and asthma. Am J Respir Crit Care Med. 2009;180(11):1076–1082. doi: 10.1164/rccm.200906-0939OC. [DOI] [PubMed] [Google Scholar]
- 20.Paff T, van der Schee MP, Daniels JMA, et al. Exhaled molecular profiles in the assessment of cystic fibrosis and primary ciliary dyskinesia. J Cyst Fibros. 2013;12(5):454–460. doi: 10.1016/j.jcf.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 21.Bruins M, Rahim Z, Bos A, van de Sande WWJ, Endtz HP, van Belkum A. Diagnosis of active tuberculosis by e-nose analysis of exhaled air. Tuberculosis. 2013;93(2):232–238. doi: 10.1016/j.tube.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Schubert JK, Miekisch W, Birken T, Geiger K, Noldge-Schomburg GF. Impact of inspired substance concentrations on the results of breath analysis in mechanically ventilated patients. Biomarkers. 2005;10(2–3):138–152. doi: 10.1080/13547500500050259. [DOI] [PubMed] [Google Scholar]
- 23.Bos L, Schultz M, Sterk P. A simple breath sampling method in intubated and mechanically ventilated critically ill patients. Respir Physiol Neurobiol. 2014;191:67–74. doi: 10.1016/j.resp.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Fowler SJ, Basanta-Sanchez M, Xu Y, Goodacre R, Dark PM. Surveillance for lower airway pathogens in mechanically ventilated patients by metabolomic analysis of exhaled breath: a case–control study. Thorax. 2015:320–325. doi:10.1136/thoraxjnl-2014-206273. [DOI] [PubMed]
- 25.Croce MA, Swanson JM, Magnotti LJ, et al. The futility of the clinical pulmonary infection score in trauma patients. J Trauma. 2006;60(3):523–527. doi: 10.1097/01.ta.0000204033.78125.1b. [DOI] [PubMed] [Google Scholar]
- 26.van der Schee MP, Fens N, Brinkman P, et al. Effect of transportation and storage using sorbent tubes of exhaled breath samples on diagnostic accuracy of electronic nose analysis. J Breath Res. 2013;7(1):16002. doi: 10.1088/1752-7155/7/1/016002. [DOI] [PubMed] [Google Scholar]
- 27.Bos LDJ, Weda H, Wang Y, et al. Exhaled breath metabolomics as a noninvasive diagnostic tool for acute respiratory distress syndrome. Eur Respir J. 2014;44(1):188–197. doi: 10.1183/09031936.00005614. [DOI] [PubMed] [Google Scholar]
- 28.Knaus W, Draper E, Wagner D, Zimmerman J. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13(10). doi:10.1097/00003465-198603000-00013. [PubMed]
- 29.Le Gall J, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA J Am Med Assoc. 1993;270(24):2957–2963. doi: 10.1001/jama.1993.03510240069035. [DOI] [PubMed] [Google Scholar]
- 30.Flahault A, Cadilhac M, Thomas G. Sample size calculation should be performed for design accuracy in diagnostic test studies. J Clin Epidemiol. 2005;58(8):859–862. doi: 10.1016/j.jclinepi.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Smith C, Elizabeth J, O’Maille G, Abagyan R, Siuzdak G. XCMS: processing mass spectrometry data for metabolite profiling using nonlinear peak alignment, matching, and identification. ACS Publ. 2006;78(3):779–787. doi: 10.1021/ac051437y. [DOI] [PubMed] [Google Scholar]
- 32.Benton HP, Want EJ, Ebbels TMD. Correction of mass calibration gaps in liquid chromatography-mass spectrometry metabolomics data. Bioinformatics. 2010;26(19):2488–2489. doi: 10.1093/bioinformatics/btq441. [DOI] [PubMed] [Google Scholar]
- 33.Tautenhahn R, Bottcher C, Neumann S. Highly sensitive feature detection for high resolution LC/MS. BMC Bioinformatics. 2008;9(1):504. doi: 10.1186/1471-2105-9-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coble JB, Fraga CG. Comparative evaluation of preprocessing freeware on chromatography/mass spectrometry data for signature discovery. J Chromatogr A. 2014;1358:155–164. doi: 10.1016/j.chroma.2014.06.100. [DOI] [PubMed] [Google Scholar]
- 35.Danielsson R, Bylund D, Markides KE. Matched filtering with background suppression for improved quality of base peak chromatograms and mass spectra in liquid chromatography-mass spectrometry. Anal Chim Acta. 2002;454(2):167–184. doi: 10.1016/S0003-2670(01)01574-4. [DOI] [Google Scholar]
- 36.Lindstrom P, Mallard W. NIST Chemistry WebBook, NIST Standard Reference Database Number 69. 69. http://webbook.nist.gov. Accessed Mar 18 2016.
- 37.Stein SE, Scott DR. Optimization and testing of mass spectral library search algorithms for compound identification. J Am Soc Mass Spectrom. 1994;5(9):859–866. doi: 10.1016/1044-0305(94)87009-8. [DOI] [PubMed] [Google Scholar]
- 38.Chun H, Keleş S. Sparse partial least squares regression for simultaneous dimension reduction and variable selection. J R Stat Soc Ser B Stat Methodol. 2010;72(1):3–25. doi: 10.1111/j.1467-9868.2009.00723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasiou PP.Irwig LM et al.Towards complete and accurate reporting of studies of diagnostic accuracy : the STARD initiative.BMJ 2003 ; 326 : 41–44 . (This is also available from Annals o. 2003;1968(1):41–44. [DOI] [PMC free article] [PubMed]
- 40.Guillamet CV, Kollef MH. Ventilator associated pneumonia in the ICU: where has it gone? Curr Opin Pulm Med. 2015;21(3):226–231. doi: 10.1097/MCP.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 41.van de Kant KD, van der Sande LJ, Jöbsis Q, van Schayck OC, Dompeling E. Clinical use of exhaled volatile organic compounds in pulmonary diseases: a systematic review. Respir Res. 2012;13(1):117. doi: 10.1186/1465-9921-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cao W. Breath analysis: potential for clinical diagnosis and exposure assessment. Clin Chem. 2006;52(5):800–811. doi: 10.1373/clinchem.2005.063545. [DOI] [PubMed] [Google Scholar]
- 43.Kalanuria AA, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014;18(2):208. doi: 10.1186/cc13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leopold JH, Bos LDJ, Sterk PJ, et al. Comparison of classification methods in breath analysis by electronic nose. J Breath Res. 2015;9(4):046002. doi: 10.1088/1752-7155/9/4/046002. [DOI] [PubMed] [Google Scholar]
- 45.Broadhurst DI, Kell DB. Statistical strategies for avoiding false discoveries in metabolomics and related experiments. Metabolomics. 2006;2(4):171–196. doi: 10.1007/s11306-006-0037-z. [DOI] [Google Scholar]


