Abstract
Background
Insurance status affects access to care, which may affect health outcomes. The objective was to determine whether patients without insurance or with government‐sponsored insurance had worse quality of care or in‐hospital outcomes in acute ischemic stroke.
Methods and Results
Multivariable logistic regressions with generalized estimating equations stratified by age under or at least 65 years were adjusted for patient demographics and comorbidities, presenting factors, and hospital characteristics to determine differences in in‐hospital mortality and postdischarge destination. We included 589 320 ischemic stroke patients treated at 1604 US hospitals participating in the Get With The Guidelines‐Stroke program between 2012 and 2015. Uninsured patients with hypertension, high cholesterol, or diabetes mellitus were less likely to be taking appropriate control medications prior to stroke, to use an ambulance to arrive to the ED, or to arrive early after symptom onset. Even after adjustment, the uninsured were more likely than the privately insured to die in the hospital (<65 years, OR 1.33 [95% CI 1.22‐1.45]; ≥65 years OR 1.54 [95% CI 1.34‐1.75]), and among survivors, were less likely to go to inpatient rehab (<65 OR 0.63 [95% CI 0.6‐0.67]; ≥65 OR 0.56 [95% CI 0.5‐0.63]). In contrast, patients with Medicare and Medicaid were more likely to be discharged to a Skilled Nursing Facility (<65 years OR 2.08 [CI 1.96‐2.2]; OR 2.01 [95% CI 1.91‐2.13]; ≥65 years OR 1.1 [95% CI 1.07‐1.13]; OR 1.41 [95% CI 1.35‐1.46]).
Conclusions
Preventative care prior to ischemic stroke, time to presentation for acute treatment, access to rehabilitation, and in‐hospital mortality differ by patient insurance status.
Keywords: health outcomes; health policy; health services research; insurance; stroke, ischemic
Subject Categories: Ischemic Stroke
Introduction
Approximately 795 000 strokes occur every year in the United States, 87% of which are ischemic, and 6.6 million living adults have experienced a stroke.1 It is the fifth leading cause of death, the leading cause of long‐term disability, and costs $33 billion per year in health care expenses and lost productivity.1 Effective healthcare delivery can prevent strokes through risk factor modification,1 and can improve long‐term recovery and outcomes after stroke,2 but insurance status affects access to healthcare.3
In the United States, employer‐sponsored private health insurance covers about half of the population.4 Private insurance covers the majority of healthcare costs, with patients accountable for only a copay or deductible usually amounting to less than 10% of total costs. Medicaid is a public insurance program for persons earning <138% of the federal poverty level and covers all services without any patient obligation. Medicare covers all persons aged 65 and older. The uninsured receive no financial assistance with the costs of care and must pay for doctor visits, medications, procedures, and hospitalizations in full out of pocket.
Being uninsured increases mortality for cancer,5, 6 trauma,7, 8 sepsis,9 heart failure,10 and acute myocardial infarction.11 Medicaid insurance status is also associated with the risk for death in several of these conditions.5, 6, 10 There is evidence that disability and mortality are also higher for Medicaid and uninsured patients after stroke,12, 13 with the largest and most recent study being specific to hemorrhagic strokes.14 Despite the Affordable Care Act, in the United States the uninsured rate remained at 11.9% in the fourth quarter of 2015.15
Therefore, the objective of this study was to determine whether patients without insurance or with government‐sponsored insurance had worse care or outcomes in acute ischemic stroke (IS) than the privately insured, using a large, nationally representative stroke registry. We specifically sought to investigate differences in prevention, presentation, in‐hospital care, acute outcomes, and use of rehabilitation services after discharge.
Methods
We used clinical data from the American Hospital Association's Get With The Guidelines (GWTG)‐Stroke, a continuous stroke registry, details of which have been published previously.16 Quintiles (Cambridge, MA) is the data collection coordination center for the GWTG programs. Duke Clinical Research Institute (DCRI) serves as the data analysis center for GWTG, and the reported analyses of aggregate deidentified data were approved by the Duke University Medical Center Institutional Review Board. Participating hospitals nationwide use trained hospital personnel to enter deidentified patient‐level data into the database for all of their stroke hospitalizations. Data collected include patient demographics, medical history, and comorbidities, in‐hospital treatment, discharge treatment and counseling, mortality, and discharge destination. The registry began in 2003, and this study presents data collected between October 1, 2012 and June 30, 2015 to minimize shifts in IS care and insurance trends that have occurred over time. Patients with stroke types other than ischemic, or with missing insurance or discharge information, were excluded from this study, leaving 589 320 IS patients treated in 1604 US hospitals analyzed here (Figure 1): 197 474 (33.5%) patients from 1534 hospital sites were aged <65 years of age (15.9% uninsured, 53.0% private, 12.0% Medicare, 19.1% Medicaid), and 391 846 (66.5%) patients from 1593 hospital sites were aged 65 years of age and older (1.0% uninsured, 39.4% private, 52.1% Medicare, 7.4% Medicaid).
Figure 1.
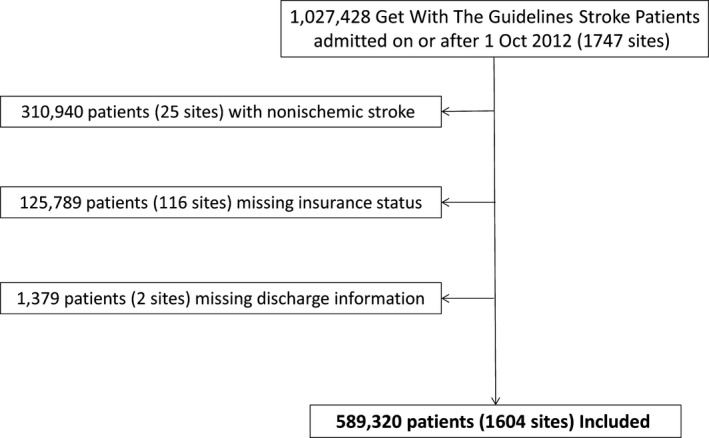
Patient inclusion algorithm.
Patient characteristics analyzed include demographics, medical comorbidities, and medications prior to admission. Presenting characteristics include information on arrival to the hospital, initial NIH stroke scale score, initial vital signs, and laboratory results on admission such as cholesterol and hemoglobin A1c levels. Hospital characteristics include stroke center designation by the Joint Commission, teaching status, rural location, geographic region, number of beds, and annual volume of IS admissions. Quality achievement measures analyzed include use of IV t‐PA in patients arriving within the treatment window, early antithrombotics, and prophylaxis for venous thromboembolism (VTE) acutely, as well as discharge with antithrombotics, anticoagulants in patients with atrial fibrillation or atrial flutter, statins in patients with LDL>100 mg/dL, and smoking cessation prior to discharge for smokers.17 The quality of care delivered is summarized by the defect‐free care measure, which measures whether or not a patient's hospital treatment met all Get With The Guidelines quality measures.17, 18 Outcomes analyzed include in‐hospital mortality (excluding patients who transferred out or left against medical advice), ambulatory status at discharge, modified Rankin Scale at discharge, and discharge destination. Ambulatory status and discharge destination measures excluded those who died during hospitalization.
Patient and hospital characteristics and quality and outcomes measures were initially compared using chi‐squared tests for categorical variables and Kruskal‐Wallis tests for continuous variables. The associations among quality measures, stroke outcomes, and insurance status were evaluated using unadjusted and adjusted logistic regression models and with generalized estimating equations (GEE) to account for hospital clustering. Covariates in adjusted analyses included patient characteristics (demographics, comorbidities, initial NIH stroke scale score, off‐hour arrival), and hospital characteristics (region, teaching status, size, rurality, annual stroke and t‐PA volumes, and Joint Commission Stroke Center designation). To handle missing data, multiple imputation with 25 independently created imputation data sets and the fully conditional specification approach, also known as multiple imputation by chained equations, were performed in SAS (all variables had <5% missing data with the exception of initial NIHSS with ~18% missing). All analyses were stratified by age less than or ≥65 years because the majority of the population becomes eligible for Medicare at age 65. All hypothesis tests are 2‐sided, with values of P<0.05 considered statistically significant. All analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC).
Results
Patient and hospital characteristics for IS patients under 65 are shown in Table 1 and Table S1. Uninsured and Medicaid patients were more likely to be black or Hispanic than privately insured or Medicare patients. Uninsured IS patients were less likely than privately insured, Medicare, or Medicaid patients to be taking stroke‐preventative medications including antiplatelets, anticoagulants, antihypertensives, cholesterol‐reducers, and diabetes mellitus medications, including those with preexisting conditions that would indicate need for such medications.
Table 1.
Patient and Hospital Characteristics for Acute Ischemic Stroke in Patients Younger Than 65 Years Old, Overall and by Insurance Statusa
| Variable | Overall (N=197 474) | Uninsured (N=31 437) | Private (N=104 623) | Medicare (N=23 759) | Medicaid (N=37 655) |
|---|---|---|---|---|---|
| Patient demographics | |||||
| Age, yb | 56 (50–61) | 54 (48–59) | 56 (50–61) | 58 (53–62) | 55 (49–60) |
| Sex | |||||
| Female | 82 084 (41.57) | 11 471 (36.49) | 42 868 (40.97) | 9961 (41.93) | 17 784 (47.23) |
| Male | 115 390 (58.43) | 19 966 (63.51) | 61 755 (59.03) | 13 798 (58.07) | 19 871 (52.77) |
| Race/Ethnicity | |||||
| White | 116 248 (58.89) | 15 483 (49.27) | 69 111 (66.08) | 14 119 (59.46) | 17 535 (46.58) |
| Black | 51 332 (26) | 9629 (30.64) | 21 358 (20.42) | 7027 (29.59) | 13 318 (35.38) |
| Hispanic (any race) | 16 288 (8.25) | 4185 (13.32) | 6565 (6.28) | 1597 (6.73) | 3941 (10.47) |
| Asian | 5116 (2.59) | 852 (2.71) | 3010 (2.88) | 283 (1.19) | 971 (2.58) |
| Other | 8419 (4.26) | 1276 (4.06) | 4540 (4.34) | 721 (3.04) | 1882 (5) |
| Medications prior to admission in those with a medical history | |||||
| Antihypertensives with prior hypertension | 92 565 (74.51) | 11 747 (60.52) | 47 881 (76.31) | 13 452 (81.38) | 19 485 (76.26) |
| Cholesterol reducers with prior dyslipidemia | 48 014 (65.27) | 4534 (52.96) | 26 336 (65.55) | 7661 (71.6) | 9483 (67.15) |
| Diabetic medications with prior diabetes mellitus | 47 570 (74.67) | 5835 (65.97) | 23 355 (76.36) | 7724 (76.87) | 10 656 (74.89) |
| Arrival information | |||||
| Arrival mode: EMS (excluding transfer‐in) | 68 502 (37.94) | 10 528 (35.71) | 33 569 (34.85) | 9225 (43.87) | 15 180 (44.99) |
| Onset to arrival time, minutesb | 266 (82‐700) | 306 (90‐791) | 247 (77‐655) | 271 (85‐697) | 292 (88‐747.5) |
| Initial NIH Stroke Scale (0‐42)b | 3 (1–7) | 3 (1–7) | 3 (1–6) | 4 (2–9) | 4 (2–9) |
| Ambulate independently on admission | 67 270 (41.73) | 11 203 (42.39) | 38 828 (45.89) | 6381 (33.67) | 10 858 (34.8) |
| Hospital characteristics | |||||
| TJC primary stroke center | 93 669 (47.43) | 14 546 (46.27) | 51 288 (49.02) | 11 144 (46.9) | 16 691 (44.33) |
| Academic/teaching hospital | 121 135 (63.64) | 18 574 (61.67) | 64 042 (63.34) | 14 044 (61.48) | 24 475 (67.49) |
| Rural location | 7975 (4.04) | 1324 (4.21) | 3785 (3.62) | 1423 (5.99) | 1443 (3.83) |
| Annual volume of ischemic stroke admissionsb | 234.49 (155.61–367.92) | 225.67 (155.24–352.83) | 235.56 (157.9–368.86) | 235.07 (154.59–361.7) | 229.86 (152.24–369.4) |
MI indicates myocardial Infarction; NIH, National Institutes of Health; TIA, transient ischemic attack; TJC, The Joint Commission.
Due to large sample size, all P‐values are statistically significant to <0.0001.
Continuous/ordinal row variables designated by * are presented as Median (IQR). All other values are presented as Patient Count (%).
Patients with IS who were uninsured arrived to the hospital later after symptom onset, and fewer arrived by ambulance than Medicaid or Medicare patients (Table 1). Privately insured patients arrived the earliest after symptom onset. However, uninsured and privately insured patients were more likely to be able to ambulate independently when they arrived than Medicare or Medicaid patients. The private and uninsured IS patients also had lesser stroke severity by NIHSS at presentation than Medicare or Medicaid patients. Characteristics of IS patients aged 65 and older are similar and can be found in Table S2.
Medicaid patients under the age of 65 and uninsured and Medicaid patients aged 65 and older were less likely to be treated in designated primary stroke centers, more likely to be treated in academic hospitals, and more frequently treated in hospitals with slightly lower annual ischemic stroke volumes (Table 1 and Tables S1 and S2). The majority of all IS admissions in the data set occurred in the South, and the South had a larger share of uninsured IS patients than other areas of the country.
Process of care, quality, and outcome measures by insurance status are shown in Table 2 and Tables S3 and S4. Although nearly all of the differences were statistically significant due to the large sample size, there were few absolute differences in achievement or quality measures by insurance status that were large enough to have a clinical impact, including the provision of defect‐free care that met all Get With The Guidelines quality measures and evaluation for rehabilitation. In‐hospital mortality was lower in privately insured patients under 65 and higher in uninsured patients aged 65 and older (Tables S3 and S4), and uninsured patients were more likely to go home and less likely to go to rehab facilities after discharge. During their stroke hospitalization, uninsured patients were more likely to receive a new diagnosis of diabetes mellitus that had not been previously known.
Table 2.
Process of Care Measures and Other Outcomes of Interest in Acute Ischemic Stroke Patients Younger Than 65 Years Old, Overall and by Insurance Statusa
| Variable | Overall (N=197 474) | Uninsured (N=31 437) | Private (N=104 623) | Medicare (N=23 759) | Medicaid (N=37 655) |
|---|---|---|---|---|---|
| Achievement measures | |||||
| Stroke defect‐free care (GWTG) | 174 946 (93.11) | 28 069 (93.37) | 93 405 (93.6) | 20 732 (92.24) | 32 740 (92.08) |
| Quality measures | |||||
| IV t‐PA arrive by 3.5 and treated by 4.5 hours | 16 774 (76.38) | 2642 (78.05) | 9550 (76.17) | 1721 (74.12) | 2861 (77.01) |
| Rehabilitation considered | 172 777 (97.62) | 27 601 (97.71) | 92 149 (97.35) | 20 576 (97.92) | 32 451 (98.12) |
| Reporting measures | |||||
| In‐hospital mortality (excluding transfer‐out, AMA, missing) | 5706 (3.01) | 989 (3.29) | 2634 (2.62) | 839 (3.67) | 1244 (3.46) |
| Discharge destination (excluding death) | |||||
| Home | 123 036 (64.16) | 22 301 (73.24) | 67 970 (66.64) | 12 081 (52.71) | 20 684 (56.81) |
| Hospice | 2199 (1.15) | 285 (0.94) | 1008 (0.99) | 399 (1.74) | 507 (1.39) |
| Inpatient rehab facility | 40 465 (21.1) | 4755 (15.62) | 21 910 (21.48) | 5685 (24.8) | 8115 (22.29) |
| Skilled nursing facility | 15 006 (7.83) | 1459 (4.79) | 5663 (5.55) | 3301 (14.4) | 4583 (12.59) |
| Other outcomes | |||||
| Ambulate independently (excluding death) | 113 976 (59.43) | 19 078 (62.66) | 64 001 (62.75) | 11 367 (49.59) | 19 530 (53.64) |
| Ambulatory status returned to independent during admission, excluding death | 46 706 (24.35) | 7825 (25.70) | 25 173 (24.68) | 4986 (21.75) | 8672 (23.82) |
| Modified Rankin Scale at discharge (total)b | 2 (1–4) | 2 (1–4) | 2 (1–4) | 3 (1–4) | 3 (1–4) |
| New diagnosis of diabetes mellitus | 3461 (3.82) | 982 (6.07) | 1744 (3.47) | 201 (2.41) | 534 (3.36) |
| Stroke rehab services | |||||
| Received rehabilitation services during hospitalization | 146 666 (92.51) | 23 831 (92.97) | 77 217 (91.69) | 17 362 (94.13) | 28 256 (93.45) |
| Transferred to rehabilitation facility | 40 863 (25.78) | 4811 (18.77) | 21 170 (25.14) | 6033 (32.71) | 8849 (29.27) |
| Referred to rehabilitation services following discharge | 30 047 (18.95) | 4925 (19.21) | 15 023 (17.84) | 3614 (19.59) | 6485 (21.45) |
| Ineligible to receive rehabilitation services because symptoms resolved | 13 271 (8.37) | 2266 (8.84) | 8060 (9.57) | 1075 (5.83) | 1870 (6.18) |
| Ineligible to receive rehabilitation services due to impairment (ie, poor prognosis, unable to tolerate rehabilitation therapeutic regimen) | 487 (0.31) | 72 (0.28) | 202 (0.24) | 76 (0.41) | 137 (0.45) |
AMA indicates against medical advice; GWTG, Get With the Guidelines.
Due to large sample size, all P‐value are significant to <0.001 with the exception of IV t‐PA, arrive by 3.5 hours, and treated by 4.5 hours, P=0.0047.
Continuous/ordinal row variables designated by † are presented as Median (IQR). All other values are presented as Patient Count (%).
After adjustment, quality of care as measured by the provision of defect‐free care was less likely in Medicare and Medicaid patients but slightly more likely in the uninsured than the privately insured (Figure S1). Uninsured patients were more likely to receive a statin when indicated by high LDL, and Medicare and Medicaid patients were less likely to receive antithrombotics, but there were no other differences in quality indicators. In patients aged 65 and older, Medicaid patients were less likely to receive t‐PA when arriving within the window, and uninsured patients remained more likely to receive a statin, but other quality indicators and the provision of defect‐free care were equal among insurance groups (Figure S2). The uninsured had 30% higher odds of dying in hospital than the privately insured, and the odds of death increased to 1.5 for the uninsured aged 65 and older (Figure 2; Figure S2).
Figure 2.
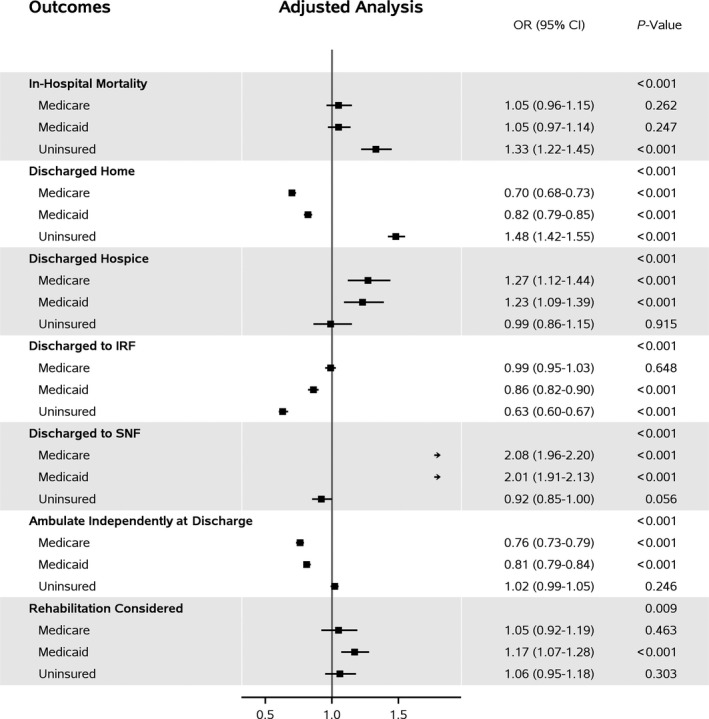
Forest plot for unadjusted and adjusted ORs (95% CI) among patients with age <65 years. Private insurance is the reference group for all ORs. The first P‐value within each outcome tests if OR differs by at least 2 insurance categories; all other P‐values test if OR differs significantly from 1. Covariates in adjusted model include patient age, sex, and race; patient medical history of atrial fibrillation or flutter, stroke/TIA, CAD/MI, carotid stenosis, diabetes mellitus, PVD, hypertension, dyslipidemia, or smoking; arrival off‐hours, NIHSS score; and hospital region, teaching status, number of beds, annual ischemic stroke volume, annual IV t‐PA volume, rurality, primary stroke center.
Compared with the privately insured, patients with Medicaid were more likely to be considered for rehab but had 14% to 24% lower odds of being discharged to an inpatient rehabilitation facility. Instead, patients on Medicare or Medicaid under age 65 had about 25% higher odds of being discharged to hospice and were twice as likely to be discharged to a skilled nursing facility as the privately insured.
Uninsured patients were equally likely to be considered for rehabilitation as the privately insured but had 37% lower odds when under 65 and 44% lower odds when aged 65 and over of being discharged to inpatient rehabilitation, 45% lower odds when aged 65 and older of being discharged to skilled nursing, and more than twice as high odds of being discharged home than the privately insured.
Discussion
We investigated whether insurance status affected prevention, presentation, in‐hospital care, acute outcomes, or use of rehabilitation services after discharge among patients with acute IS. Our study identified several important findings. First, uninsured patients have poorer control of several risk factors for stroke when their IS occurs. Second, uninsured patients arrive to the hospital later after symptom onset. Third, Medicaid patients are less likely to receive IV t‐PA when arriving within the window time for IS. Fourth, uninsured patients have higher rates of in‐hospital mortality. Finally, uninsured and Medicaid patients have lower utilization of inpatient rehabilitation services after IS, whereas Medicaid and Medicare patients have higher utilization of skilled nursing facilities and hospice after IS than the privately insured.
Mortality was particularly increased in the uninsured IS patients but also slightly increased in Medicaid patients aged 65 and older and in both Medicare and Medicaid patients under 65. Increased mortality in uninsured IS patients under age 65 has previously been suggested in survey data13 and demonstrated for all uninsured patients with hemorrhagic stroke12, 14 and for all patients with IS with any status other than privately insured19 in national registry data. This study confirms the increased risk of death and adds more information on presenting, prehospital, and in‐hospital factors that can be used for future investigations into the etiology of the mortality disparity.
Differences in prestroke preventative care and initial hospital arrival may partially explain the mortality difference for uninsured patients, particularly because stroke severity and provision of high‐quality processes of care did not differ. Uninsured patients with risk factors for stroke such as diabetes mellitus, high blood pressure, or high cholesterol were less likely to be taking the appropriate medications for primary stroke prevention and had more poorly controlled cholesterol levels than other groups. They were also less likely to be aware of their risk factors for stroke, as evidenced by more frequent first‐time diagnosis of diabetes mellitus during the hospitalization for IS. In addition, the uninsured arrived almost 45 minutes later on average after stroke onset than other IS patients.
These findings correlate with prior evidence that the uninsured delay needed care due to costs,20 have undiagnosed chronic disease,21 do not take appropriate control medications to decrease stroke risk,22, 23 and have poorer control of risk factors for stroke such as blood pressure.24, 25 In the United States the uninsured must pay out of pocket for a physician visit at least once a year at an average cost of $160 to renew prescriptions for preventative medications,26 not including any laboratory tests required to screen for or monitor risk factors such as diabetes mellitus or high cholesterol, and an average of $166 per month for 1 antihypertensive and 1 statin.27 The uninsured are mostly low‐income workers for whom $100 represents a large percentage of their monthly income and are more likely to work at hourly‐wage jobs without sick leave, limiting access to physician offices during weekday working hours.3 The uninsured are more likely to have low health literacy28 and may live in areas with limited access to primary care.29 All of these factors likely contribute to poorer preventative care and worse stroke outcomes in this group. Although this study was unable to evaluate long‐term outcomes such as recurrent stroke or long‐term disability, if these patients remained uninsured after their IS, evidence from this and prior studies30 suggests that they will also be less likely to achieve adequate secondary prevention for recurrent stroke.
Although some differences did exist in quality of care delivered to IS patients by insurance status, they had minimal clinical impact, with less than 10% absolute difference with the exception of IV t‐PA for Medicaid patients over the age of 65. Medicaid patients were less likely to be treated at designated primary stroke centers, which could contribute to this disparity, but it persists after adjustment. Medicaid patients had worse disability and were less likely to walk independently at discharge, but they were also less likely to walk independently at admission, so it is uncertain whether this poorer functional status relates to lack of IV t‐PA or to more severe prestroke disability.
Although IS patients who were uninsured were equally evaluated for rehabilitation, they had more than twice the odds as the privately insured of going home after stroke, and 40% to 50% lower odds of going to inpatient rehabilitation or a skilled nursing facility. Going home is typically viewed as a positive outcome after stroke, but in this group it may be inappropriate. Medicaid patients had lower odds of going home but higher odds of going to hospice (if under 65 years of age) and higher odds of going to skilled nursing rather than inpatient rehabilitation. Similar results have been found in previous national samples of stroke patients, but those have been limited to different subpopulations of stroke patients or to evaluation for rehabilitation without placement data.14, 31, 32 All comparisons were made to privately insured patients, who use inpatient rehabilitation more than the other groups, but ideal utilization levels are unknown, and it is not clear that utilization by privately insured patients represents appropriate utilization rather than overutilization.
However, after suffering IS, patients are at high risk for permanent disability, but evidence shows that rehabilitation improves functional outcomes, particularly when started early.2, 33, 34 Lower utilization of postacute care has also been demonstrated in the uninsured after trauma and sepsis.8, 34 Unfortunately, postacute care is expensive, and acceptance into such programs is highly dependent on ability to pay and insurance authorizations, which likely explains the differences observed in this study. Limited access to rehabilitation after ischemic stroke for the uninsured and Medicaid populations may increase the number of poststroke patients who become disabled, increasing their long‐term costs.
Insurance status is correlated with sociodemographic variables, which may also play a role in the different stroke outcomes found in this study. For example, people on Medicaid qualify due to poverty, and the uninsured are also a low‐income group.3 Persons under the age of 65 on Medicare are typically disabled, whereas almost all US citizens aged 65 and older qualify for Medicare. In the group aged 65 and older, the overall uninsured rate is very low, and those who remain uninsured likely are either not US citizens or have poor social circumstances such as lack of personal identification due to homelessness that prevent them from obtaining Medicare. Persons on Medicaid over the age of 65 are generally dually eligible for Medicare and Medicaid and are impoverished and elderly. However, some low‐income persons may have excellent employer‐sponsored insurance, and some wealthy persons may be uninsured,3 suggesting the importance of insurance status as an independent adjustment factor for stroke population analyses, especially for the under‐65 population.
The Affordable Care Act has reduced the number of uninsured persons in the United States. However, over 30 million people remain uninsured, and Medicaid enrollment has increased by 12 million.3, 36 Therefore, the findings of this study remain relevant as we consider how to increase insurance coverage and how that coverage equates with access, affordability, and outcomes. Future research should examine how high‐deductible health plans, which are nearly ubiquitous in the marketplace plans that 10 million people have purchased through the ACA and are increasing in prevalence in employer‐sponsored plans, will affect stroke outcomes.36, 37 High deductibles may provide incentives similar to those the uninsured face in barriers to appropriate primary prevention medications prestroke and may or may not affect utilization of rehabilitation poststroke, depending on deductible amounts relative to the cost of stroke hospitalization.
Our study has several important limitations. First, although Get With The Guidelines data represent a large number of stroke admissions across the country, they depend on the accuracy of data collection and entry by staff members at over 1500 different hospitals. As noted, 127 168 patients, or 18% of all acute ischemic strokes, were excluded from this study because they were missing key data, and some of the patients included were still missing other data points that, although predicted using multiple imputation, may introduce bias into the results. Second, all included hospitals are participating in a program to improve stroke quality, and their results may not be generalizable to other hospitals not participating. Third, this was a retrospective observational study, and some factors important to stroke severity or severity of comorbidities may not have been measured, introducing unmeasured or residual confounding. In particular, several socioeconomic factors that may interact with insurance status were not available, such as income level and employment status. Retrospective studies also cannot prove causality of insurance status on stroke outcomes. Finally, although differences were found in acute outcomes and discharge destinations after IS, this registry is limited to hospital‐associated outcomes, and long‐term outcomes such as functional status and disability, recurrent stroke, and survival were not analyzed.
Conclusions
Preventative care prior to IS, time to presentation for acute treatment, access to rehabilitation, and outcomes including mortality differ by patient insurance status. This study suggests that even high‐quality processes of stroke care in hospital cannot overcome the prestroke health status, socioeconomic drivers, and choices of patients in how and when to seek care that vary by insurance status. Because insurance status was independently associated with in‐hospital outcomes, expanded insurance coverage may help reduce death and disability due to IS.
Sources of Funding
The research analysis for this study was funded through a grant from the American Heart Association.
Disclosures
Dr Medford‐Davis receives research funding through the Robert Wood Johnson Foundation Clinical Scholars Program. Dr Fonarow receives research funding from Patient Centers Outcome Research Center, is a member of the GWTG Steering Committee, is employed by UCLA, and holds a patent on an endovascular device. Dr Bhatt discloses the following relationships—Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org), Belvoir Publications (Editor‐in‐Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (Editor‐in‐Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Population Health Research Institute (clinical trial steering committee), Slack Publications (Chief Medical Editor, Cardiology Today's Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR‐ACTION Registry Steering Committee (Vice‐Chair), VA CART Research and Publications Committee (Chair); Research Funding: Amarin, AstraZeneca, Bristol‐Myers Squibb, Eisai, Ethicon, Forest Laboratories, Ischemix, Medtronic, Pfizer, Roche, Sanofi Aventis, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald's Heart Disease); Site Co‐Investigator: Biotronik, Boston Scientific, St. Jude Medical; Trustee: American College of Cardiology; Unfunded Research: FlowCo, PLx Pharma, Takeda. Dr Xu is employed by GWTG. Dr Smith is a member of the GWTG Steering Committee. Dr Suter discloses prior employment by the American Heart Association. Dr Peterson reports serving as principal investigator of the Data Analytic Center for AHA GWTG; receipt of research grants from Johnson & Johnson and Janssen Pharmaceuticals; and serving as a consultant to Bayer, Boehringer Ingelheim, Johnson & Johnson, Medscape, Merck, Novartis, Ortho‐McNeil‐Janssen, Pfizer, Valeant, Westat, the Cardiovascular Research Foundation, WebMD, and United Healthcare. Dr Xian and Dr Matsouaka are employed by GWTG. Dr Schwamm receives research funding from Patient Centered Outcome Research Center and NINDS, is a member of the GWTG Steering Committee, and chair of the GTWTG stroke clinical workgroup.
Supporting information
Table S1. Additional Patient and Hospital Characteristics for Acute Ischemic Stroke in Patients Younger Than 65 Years Old, Overall and by Insurance Status
Table S2. Patient and Hospital Characteristics for Acute Ischemic Stroke Patients Aged 65 Years or Older, Overall and by Insurance Status
Table S3. Additional Stroke Process of Care Measures and Other Outcomes of Interest in Acute Ischemic Stroke Patients Younger Than 65 Years Old, Overall and by Insurance Status
Table S4. Process of Care Measures and Other Outcomes of Interest in Acute Ischemic Stroke Patients Aged 65 Years or Older, Overall and by Insurance Status
Figure S1. Forest plot for unadjusted and adjusted ORs (95% CI) among patients with age <65 years.
Figure S2. Forest plot for unadjusted and adjusted ORs (95% CI) among patients with age ≥65 years.
Acknowledgments
Xu conducted the data analysis at the Duke Clinical Research Institute. She had full access to all of the study data and takes responsibility for the integrity of the data and the accuracy of the data analysis. The American Heart Association collects and maintains the data used for this study.
(J Am Heart Assoc. 2016;5:e004282 doi: 10.1161/JAHA.116.004282)
This work was presented at the AcademyHealth Research Meeting, June 26 to 28, 2016, in Boston, MA.
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2015;133:447–454. [DOI] [PubMed] [Google Scholar]
- 2. Duncan PW, Horner RD, Reker DM, Samsa GP, Hoenig H, Hamilton B, LaClair BJ, Dudley TK. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke. 2002;33:167–177. [DOI] [PubMed] [Google Scholar]
- 3. Henry J Kaiser Family Foundation . Key facts about the uninsured. 2014. Available at: http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/. Accessed January 30, 2014.
- 4. Henry J Kaiser Family Foundation . Health Insurance Coverage of the Total Population. 2015. Available at: http://kff.org/state-category/health-coverage-uninsured/health-insurance-status/Accessed September 30, 2016.
- 5. Shi R, Diaz R, Shi Z, Duvall E, Mills G. The effect of payer status on survival of patients with stage I/II non‐small cell lung cancer: NCDB 1998–2011. Anticancer Res. 2016;36:319–326. [PubMed] [Google Scholar]
- 6. Shi R, Taylor H, McLarty J, Liu L, Mills G, Burton G. Effects of payer status on breast cancer survival: a retrospective study. BMC Cancer. 2015;15:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Downing SR, Oyetunji TA, Greene WR, Jenifer J, Rogers SO Jr, Haider AH, Cornwell EE 3rd, Chang DC. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? J Trauma. 2011;70:130–134; discussion 134‐135. [DOI] [PubMed] [Google Scholar]
- 8. Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE 3rd. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. [DOI] [PubMed] [Google Scholar]
- 9. Kumar G, Taneja A, Majumdar T, Jacobs ER, Whittle J, Nanchal R; Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators . The association of lacking insurance with outcomes of severe sepsis: retrospective analysis of an administrative database. Crit Care Med. 2014;42:583–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kapoor JR, Kapoor R, Hellkamp AS, Hernandez AF, Heidenreich PA, Fonarow GC. Payment source, quality of care, and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol. 2011;58:1465–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vidovich MI, Vasaiwala S, Cannon CP, Peterson ED, Dai D, Hernandez AF, Fonarow GC; Get With Guidelines Steering Committee and Investigators . Association of insurance status with inpatient treatment for coronary artery disease: findings from the Get With the Guidelines program. Am Heart J. 2010;159:1026–1036. [DOI] [PubMed] [Google Scholar]
- 12. Shen JJ, Washington EL. Disparities in outcomes among patients with stroke associated with insurance status. Stroke. 2007;38:1010–1016. [DOI] [PubMed] [Google Scholar]
- 13. McManus M, Ovbiagele B, Markovic D, Towfighi A. Association of insurance status with stroke‐related mortality and long‐term survival after stroke. J Stroke Cerebrovasc Dis. 2015;24:1924–1930. [DOI] [PubMed] [Google Scholar]
- 14. James ML, Grau‐Sepulveda MV, Olson DM, Smith EE, Hernandez AF, Peterson ED, Schwamm LH, Bhatt DL, Fonarow GC. Insurance status and outcome after intracerebral hemorrhage: findings from Get With the Guidelines‐Stroke. J Stroke Cerebrovasc Dis. 2014;23:283–292. [DOI] [PubMed] [Google Scholar]
- 15. Marken S. U.S. uninsured rate 11.9% in fourth quarter of 2015. Gallup 2016.
- 16. Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang L, Peterson E, Labresh KA. Get With the Guidelines‐Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–115. [DOI] [PubMed] [Google Scholar]
- 17. Parmar P, Goolsby CA, Udompanyanan K, Matesick LD, Burgamy KP, Mower WR. Value of mandatory screening studies in emergency department patients cleared for psychiatric admission. West J Emerg Med. 2012;13:388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fonarow GC, Reeves MJ, Smith EE, Saver JL, Zhao X, Olson DW, Hernandez AF, Peterson ED, Schwamm LH; GWTG‐Stroke Steering Committee and Investigators . Characteristics, performance measures, and in‐hospital outcomes of the first one million stroke and transient ischemic attack admissions in Get With the Guidelines‐Stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. [DOI] [PubMed] [Google Scholar]
- 19. Fargen KM, Neal D, Blackburn SL, Hoh BL, Rahman M. Health disparities and stroke: the influence of insurance status on the prevalence of patient safety indicators and hospital‐acquired conditions. J Neurosurg. 2015;122:870–875. [DOI] [PubMed] [Google Scholar]
- 20. Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. [DOI] [PubMed] [Google Scholar]
- 21. Ayanian JZ, Zaslavsky AM, Weissman JS, Schneider EC, Ginsburg JA. Undiagnosed hypertension and hypercholesterolemia among uninsured and insured adults in the Third National Health and Nutrition Examination Survey. Am J Public Health. 2003;93:2051–2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rice T, Lavarreda SA, Ponce NA, Brown ER. The impact of private and public health insurance on medication use for adults with chronic diseases. Med Care Res Rev. 2005;62:231–249. [DOI] [PubMed] [Google Scholar]
- 23. Brown TM, Parmar G, Durant RW, Halanych JH, Hovater M, Muntner P, Prineas RJ, Roth DL, Samdarshi TE, Safford MM. Health professional shortage areas, insurance status, and cardiovascular disease prevention in the reasons for geographic and racial differences in stroke (REGARDS) study. J Health Care Poor Underserved. 2011;22:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Durant RW, Parmar G, Shuaib F, Le A, Brown TM, Roth DL, Hovater M, Halanych JH, Shikany JM, Prineas RJ, Samdarshi TJ, Safford MM. Awareness and management of chronic disease, insurance status, and health professional shortage areas in the REasons for Geographic And Racial Differences in Stroke (REGARDS): a cross‐sectional study. BMC Health Serv Res. 2012;12:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gandelman G, Aronow WS, Varma R. Prevalence of adequate blood pressure control in self‐pay or Medicare patients versus Medicaid or private insurance patients with systemic hypertension followed in a university cardiology or general medicine clinic. Am J Cardiol. 2004;94:815–816. [DOI] [PubMed] [Google Scholar]
- 26. Saloner B, Polsky D, Kenney GM, Hempstead K, Rhodes KV. Most uninsured adults could schedule primary care appointments before the ACA, but average price was $160. Health Aff (Millwood). 2015;34:773–780. [DOI] [PubMed] [Google Scholar]
- 27. Brown P;US PIRG Education Fund . Paying the price: the high cost of prescription drugs for the uninsured. 2006.
- 28. Sentell T. Implications for reform: survey of California adults suggests low health literacy predicts likelihood of being uninsured. Health Aff (Millwood). 2012;31:1039–1048. [DOI] [PubMed] [Google Scholar]
- 29. Brown EJ, Grande DT, Barbu CM, Polsky DE, Seymour JW;US PIRG Education Fund . Location matters: differences in primary care supply by neighborhood in Philadlephia. 2015.
- 30. Bushnell CD, Zimmer LO, Pan W, Olson DM, Zhao X, Meteleva T, Schwamm L, Ovbiagele B, Williams L, Labresh KA, Peterson ED; Adherence Evaluation After Ischemic Stroke‐Longitudinal Investigators . Persistence with stroke prevention medications 3 months after hospitalization. Arch Neurol. 2010;67:1456–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Skolarus LE, Meurer WJ, Burke JF, Prvu Bettger J, Lisabeth LD. Effect of insurance status on postacute care among working age stroke survivors. Neurology. 2012;78:1590–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Prvu Bettger JA, Kaltenbach L, Reeves MJ, Smith EE, Fonarow GC, Schwamm LH, Peterson ED. Assessing stroke patients for rehabilitation during the acute hospitalization: findings from the Get With the Guidelines‐Stroke program. Arch Phys Med Rehabil. 2013;94:38–45. [DOI] [PubMed] [Google Scholar]
- 33. Wang H, Camicia M, DiVita M, Mix J, Niewczyk P. Early inpatient rehabilitation admission and stroke patient outcomes. Am J Phys Med Rehabil. 2015;94:85–96; quiz 97‐100. [DOI] [PubMed] [Google Scholar]
- 34. Wang H, Camicia M, Terdiman J, Hung YY, Sandel ME. Time to inpatient rehabilitation hospital admission and functional outcomes of stroke patients. PM R. 2011;3:296–304; quiz 304. [DOI] [PubMed] [Google Scholar]
- 35. Sacks GD, Hill C, Rogers SO Jr. Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. J Trauma. 2011;71:1011–1015. [DOI] [PubMed] [Google Scholar]
- 36. US Department of Health and Human Services, Assistant Secretary for Public Affairs . The Affordable Care Act Is Working. 2015. Available at: http://www.hhs.gov/healthcare/facts-and-features/fact-sheets/aca-is-working/index.html. Accessed June 28, 2016.
- 37. Gabel J, Whitmore H, Green M, Stromberg S, Oran R. Commonwealth Fund. Realizing Health Reform's Potential. Consumer Cost‐Sharing in Marketplace vs. Employer Health Insurance Plans, 2015. 2015. Available at: http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/dec/1854_gabel_cost_sharing_marketplace_vs_employer_plans_rb.pdf. Accessed June 28, 2016. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Additional Patient and Hospital Characteristics for Acute Ischemic Stroke in Patients Younger Than 65 Years Old, Overall and by Insurance Status
Table S2. Patient and Hospital Characteristics for Acute Ischemic Stroke Patients Aged 65 Years or Older, Overall and by Insurance Status
Table S3. Additional Stroke Process of Care Measures and Other Outcomes of Interest in Acute Ischemic Stroke Patients Younger Than 65 Years Old, Overall and by Insurance Status
Table S4. Process of Care Measures and Other Outcomes of Interest in Acute Ischemic Stroke Patients Aged 65 Years or Older, Overall and by Insurance Status
Figure S1. Forest plot for unadjusted and adjusted ORs (95% CI) among patients with age <65 years.
Figure S2. Forest plot for unadjusted and adjusted ORs (95% CI) among patients with age ≥65 years.


