Abstract
Background
The influence of moderately reduced kidney function on late survival after surgical aortic valve replacement (AVR) is unknown. We analyzed survival after AVR in patients with moderately reduced kidney function.
Methods and Results
All patients who underwent primary AVR in Sweden 1997–2013 were identified from the Swedish Web system for Enhancement and Development of Evidence‐based care in Heart disease Evaluated According to Recommended Therapies register. Patients were categorized according to estimated glomerular filtration rate (eGFR). Of 13 102 patients, 9836 (75%) had normal kidney function (eGFR >60 mL/min per 1.73 m2) and 3266 (25%) had moderately reduced kidney function (eGFR 30–60 mL/min per 1.73 m2). Mean follow‐up time was 6.2 years. Mortality was higher in patients with moderately reduced kidney function; 5‐, 10‐, and 15‐year survival was 76%, 48%, and 25% versus 89%, 73%, and 55% (adjusted hazard ratio [HR], 1.28; 95% CI, 1.18–1.38; P<0.001). Patients with moderately reduced kidney function had a nonsignificantly higher risk of major bleeding (HR, 1.18; 95% CI, 1.00–1.39; P=0.051) and a lower risk for aortic valve reoperation (HR, 0.54; 95% CI, 0.38–0.79; P=0.001) compared to those with normal kidney function. In patients with moderately reduced kidney function, survival was similar in those who received bioprostheses compared to those who received mechanical valves (HR, 0.85; 95% CI, 0.70–1.03; P=0.094).
Conclusions
Moderately reduced kidney function was strongly associated with increased mortality after AVR. These results have important implications for preoperative risk stratification, and suggest that patients with eGFR 30 to 60 mL/min per 1.73 m2 warrant careful observation after AVR.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unique identifier: NCT02276950.
Keywords: aortic valve replacement, cardiac surgery, chronic kidney disease
Subject Categories: Aortic Valve Replacement/Transcather Aortic Valve Implantation, Cardiovascular Surgery, Valvular Heart Disease, Mortality/Survival
Introduction
Chronic kidney disease (CKD) is a common condition affecting 7% to 13% of the general population and up to 37% of the population above 70 years of age.1, 2 CKD is a strong risk factor for cardiovascular disease,3 which is the most frequent cause of death in these patients.4 CKD is also closely associated with valvular disease, especially aortic stenosis.5
The incidence of aortic stenosis increases with age, and it is present in ≈2% of the population aged over 65 years.6 In patients with end‐stage renal disease (ESRD), prevalence of aortic stenosis is higher than in the general population, and, once developed, the disease progresses more rapidly.7 The standard treatment for aortic stenosis is aortic valve replacement (AVR). Patients with ESRD have a substantially higher risk of mortality and bleeding after AVR.8, 9 Additionally, bioprostheses degenerate faster in patients with ESRD.9 Moderately reduced kidney function is much more common than ESRD, and 23% to 27% of all patients who undergo cardiac surgery suffer from moderately reduced renal function.10, 11 The impact of moderately reduced kidney function after coronary artery bypass grafting (CABG) and transcutaneous aortic valve implantation has been investigated in several studies.12, 13, 14 However, the influence of moderately reduced kidney function on late survival after isolated surgical AVR is not well known.
We analyzed the prognosis after AVR in patients with moderately reduced kidney function in a large, nation‐wide, population‐based cohort study. The primary objective of our study was to analyze all‐cause long‐term mortality in patients with moderately reduced kidney function compared to those with normal kidney function. The secondary outcome measures were early mortality, rate of major bleeding events, and aortic valve reoperation. Additionally, we compared long‐term mortality in patients with moderately reduced kidney function who received a bioprosthesis versus those who received a mechanical valve prosthesis.
Methods
Study Design
This was an observational, nation‐wide, population‐based cohort study. Ethical approval was obtained from the regional Human Research Ethics Committee, Stockholm, Sweden. No informed patient consent was required. The Swedish Web system for Enhancement and Development of Evidence‐based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) register15, 16 was used to identify patients who underwent AVR. This register contains clinical and operative information on all patients who have undergone cardiac surgery in Sweden since 1992. All patients who underwent AVR in Sweden from January 1, 1997 until December 31, 2013 were included. Exclusion and inclusion criteria are shown in Figure 1. We categorized patients according to kidney function. Patients were divided into 2 groups according to a modified National Kidney Foundation/Kidney Disease Improving Global Outcomes classification of CKD.17 Patients with estimated glomerular filtration rate (eGFR) >60 mL/min per 1.73 m2 were classified as the normal kidney function group; patients with eGFR 30 to 60 mL/min per 1.73 m2, corresponding to CKD stage III, were classified as the moderately reduced kidney function group.17 Glomerular filtration rate was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD‐EPI) equation18 and the most recent creatinine value before surgery.
Figure 1.
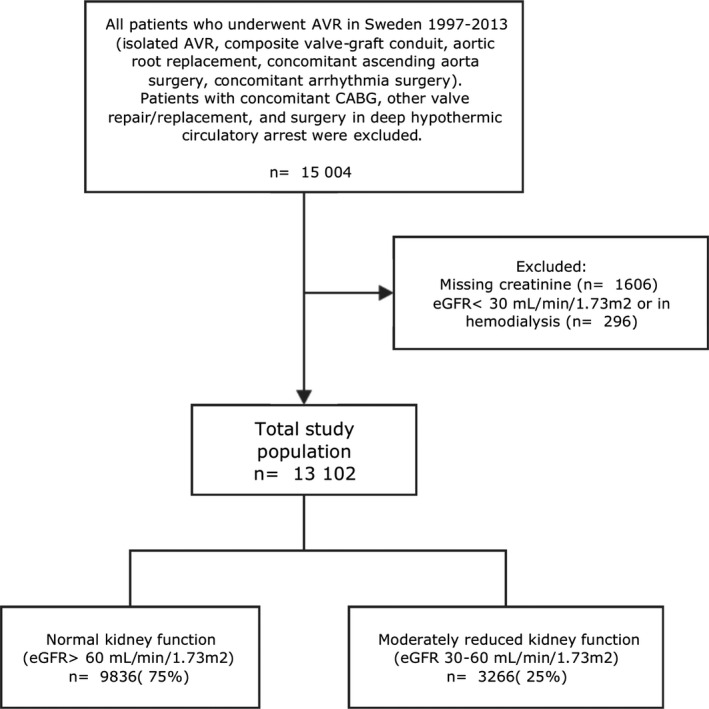
Flow chart of study population. AVR indicates aortic valve replacement; CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate.
Baseline characteristics and clinical outcomes were obtained from the SWEDEHEART register, the National Patient Register (Table 1), the longitudinal integration database for health insurance and labor market studies (maintained by Statistics Sweden), and the Cause of Death Register. Each Swedish citizen has a unique personal identity number,19 which made individual‐level record linkage possible. The formation of the database used in this study was described in detail previously.20
Table 1.
Definition of Diagnoses/Comorbid Conditions
| ICD‐9 Codes | ICD‐10 Codes | |
|---|---|---|
| Myocardial infarction | 410 | I21 to I21.9 |
| Stroke | 430 to 438 | I60 to I69.9 |
| Heart failure | 428 | I50 to I50.9 |
| Atrial fibrillation | 427D | I48 to I48.9 |
| Chronic obstructive pulmonary disease | 490 to 496 | J44 to J44.9 |
| Hypertension | 401 to 405 | I10 to I15.9 |
| Hyperlipidemia | 272 | E78 to E78.9 |
| Peripheral vascular disease | 440 to 446 | I65 to I65.9, I71 to I71.9, I73.8, I73.9 |
| Alcohol abuse | 291, 303, 571 | F10 to F10.9, K70 to K70.9 |
| Liver disease | 570 to 573 | K70 to K77.9 |
| Cancer | 140 to 208 | C00 to C97.9 |
| Endocarditis | 421 | I33.0, I33.9, I38.9 |
| Diabetes mellitus | 250 | E10 to E14.9 |
| Major bleeding event | 285B, 430, 431, 432, 456A, 530H, 531A, 531C, 531E, 531G, 532A, 532C, 532E, 532G, 533A, 533C, 533E, 533G, 534A, 534C, 534E, 534G, 569D, 578 | D629, I60, I61, I62, I850, K226, K250, K252, K254, K256, K260, K262, K264, K266, K270, K272, K274, K276, K280, K282, K284, K286, K290, K625, K920, K921, K922, I312, I230, J942, K661, M250, N421, N501A, N938, N939, N950, R041, R042, R048, R049, R31 |
Primary and secondary diagnoses from the National Patient Register from 1987 and onward. ICD‐9 indicates International Classification of Diseases, Ninth Revision; ICD‐10, International Classification of Diseases, Tenth Revision.
Outcomes
The primary outcome was all‐cause mortality. Secondary outcomes included early mortality (death within 30 days after surgery) and the rate of major bleeding events and aortic valve reoperation. We also investigated all‐cause mortality in patients with moderately reduced kidney function who received a bioprosthesis compared to those who received a mechanical valve prosthesis. Vital status and date of death were obtained from the Cause of Death Register. Information regarding major bleeding events was acquired from the corresponding primary diagnosis code in the National Patient Register (Table 2). Information regarding aortic valve reoperation was acquired from the SWEDEHEART register.
Table 2.
Definition of Major Bleeding Event
| ICD‐10 Codes | |
|---|---|
| Major bleeding event | D629, I60, I61, I62, I850, K226, K250, K252, K254, K256, K260, K262, K264, K266, K270, K272, K274, K276, K280, K282, K284, K286, K290, K625, K920, K921, K922, I312, I230, J942, K661, M250, N421, N501A, N938, N939, N950, R041, R042, R048, R049, R31 |
Primary diagnosis from the National Patient Register. ICD‐10 indicates International Classification of Diseases, Tenth Revision.
Statistical Analysis
Patient characteristics are presented as means and SDs for continuous variables and as frequencies and percentages for categorical variables. For all‐cause mortality, person‐time in days was counted from the date of surgery until the date of death or the end of follow‐up (March 24, 2014). Information regarding major bleeding event and aortic valve reoperation was available until December 31, 2012 and December 31, 2013, respectively; therefore, person‐time in days was counted from the date of surgery until the date of death, date of major bleeding (until December 31, 2012), date of aortic valve reoperation (until December 31, 2013), or end of follow‐up (March 24, 2014), whichever came first. Patients who had undergone surgery during 2013 were excluded from the analyses of major bleeding event. Crude incidence rates and 95% CIs were calculated, and the Kaplan–Meier method was used to calculate cumulative survival. The association between kidney function and mortality, expressed as hazard ratios (HRs), was estimated using the Cox proportional hazards model. In the multivariable analysis, all variables from Table 3 were included, and the model was stratified for hospital and year of surgery. To estimate the risk of major bleeding event and aortic valve reoperation, subdistribution hazard ratios (sHR) and 95% CIs were calculated using competing risk regression based on the Fine‐Gray proportional subhazards model.21 In the analysis of patients with moderately reduced kidney function who received a bioprosthesis versus a mechanical valve prosthesis, logistic regression including all variables in Table 3 (including hospital) was used to calculate a propensity score for each patient. Patients with a bioprosthesis were paired with those with a mechanical valve prosthesis through a 1:1 nearest neighbor matching, with a caliper width of 0.2 of the logit of the SD of the propensity score.22 Age and body mass index were included in the models as restricted cubic splines, and all other parameters were included as categorical variables. Data were missing for left ventricular ejection fraction (24%) and body mass index (7%). Missing data were handled by multiple imputation by chained equations.23 The missing values were assumed to be missing at random and the imputation model included all variables in Table 3, the event indicator, and the Nelson–Aalen estimator of the cumulative baseline hazard.24 The imputation was repeated 25 times, and estimates from the imputed data sets were combined according to Rubin's rules. Data management and statistical analyses were performed using Stata (version 14.1; StataCorp LP, College Station, TX) and R software (version 3.3.0; R Foundation for Statistical Computing, Vienna, Austria).
Table 3.
Baseline Characteristics in 13 102 Patients Who Underwent AVR Between 1997 and 2013 According to Kidney Function
| All Patients n=13 102 | Normal Kidney Function n=9836 (75%) | Moderately Reduced Kidney Function n=3266 (25%) | |
|---|---|---|---|
| Age, yr, mean (SD) | 66.8 (12.9) | 64.3 (13.1) | 74.4 (8.5) |
| Female sex (%) | 5222 (39.9) | 3441 (35.0) | 1781 (54.5) |
| Civil status (%) | |||
| Not married | 5251 (40.1) | 3956 (40.2) | 1295 (39.7) |
| Education (%) | |||
| <10 years | 5222 (39.9) | 3783 (38.5) | 1439 (44.1) |
| 10 to 12 years | 5467 (41.7) | 4074 (41.4) | 1393 (42.7) |
| >12 years | 2413 (18.4) | 1979 (20.1) | 434 (13.3) |
| Region of birth (%) | |||
| Non‐Nordic countries | 769 (5.9) | 610 (6.2) | 159 (4.9) |
| Body mass index, kg/cm2, mean (SD) | 26.7 (4.5) | 26.7 (4.5) | 26.8 (4.7) |
| Biological valve prosthesis (%) | 8258 (63.0) | 5676 (57.7) | 2582 (79.1) |
| Diabetes mellitus (%) | 1713 (13.1) | 1164 (11.8) | 549 (16.8) |
| Atrial fibrillation (%) | 1850 (14.1) | 1151 (11.7) | 699 (21.4) |
| Hypertension (%) | 3210 (24.5) | 2142 (21.8) | 1068 (32.7) |
| Hyperlipidemia (%) | 1061 (8.1) | 782 (8.0) | 279 (8.5) |
| Stroke (%) | 1131 (8.6) | 769 (7.8) | 362 (11.1) |
| Peripheral vascular disease (%) | 1076 (8.2) | 805 (8.2) | 271 (8.3) |
| Chronic pulmonary disease (%) | 992 (7.6) | 705 (7.2) | 287 (8.8) |
| Past myocardial infarction (%) | 906 (6.9) | 569 (5.8) | 337 (10.3) |
| Past PCI (%) | 515 (3.9) | 350 (3.6) | 165 (5.1) |
| Past major bleeding event (%) | 620 (4.7) | 406 (4.1) | 214 (6.6) |
| Alcohol dependency (%) | 272 (2.1) | 223 (2.3) | 49 (1.5) |
| Liver disease (%) | 115 (0.9) | 83 (0.8) | 32 (1.0) |
| Cancer (%) | 930 (7.1) | 622 (6.3) | 308 (9.4) |
| eGFR, mL/min per 1.73 m2 (%) | |||
| >60 | 9836 (75.1) | 9836 (100.0) | — |
| 45 to 60 | 2377 (18.1) | — | 2377 (72.8) |
| 30 to 45 | 889 (6.8) | — | 889 (27.2) |
| Heart failure (%) | 2176 (16.6) | 1284 (13.1) | 892 (27.3) |
| Left ventricular ejection fraction (%) | |||
| >50 | 7564 (76.3) | 5979 (77.7) | 1585 (71.3) |
| 30 to 49 | 1905 (19.2) | 1425 (18.5) | 480 (21.6) |
| <30 | 449 (4.5) | 290 (3.8) | 159 (7.1) |
| Endocarditis (%) | 720 (5.5) | 565 (5.7) | 155 (4.7) |
| Emergent surgery (%) | 215 (1.6) | 162 (1.6) | 53 (1.6) |
| Isolated AVR (%) | 10 869 (83.0) | 7934 (80.7) | 2935 (89.9) |
| Year of surgery (%) | |||
| 1997 to 2001 | 2538 (19.4) | 1706 (17.3) | 832 (25.5) |
| 2002 to 2006 | 3816 (29.1) | 2717 (27.6) | 1099 (33.6) |
| 2007 to 2013 | 6748 (51.5) | 5413 (55.0) | 1335 (40.9) |
Normal kidney function (eGFR >60 mL/min per 1.73 m2) versus moderately reduced kidney function (eGFR 30–60 mL/min per 1.73 m2). Data are n (%), unless otherwise noted. AVR indicates aortic valve replacement; eGFR, estimated glomerular filtration rate; PCI, percutaneous coronary intervention.
Results
Study Population
Of 15 004 patients who underwent primary AVR in Sweden between 1997 and 2013, we excluded 1606 (11%) with missing creatinine values and 296 (2%) with severe kidney failure or ESRD (those who had eGFR <30 mL/min per 1.73 m2 or were on dialysis). A total of 13 102 patients were included in the study. Of these, 9836 (75%) had normal kidney function and 3266 (25%) had moderately reduced kidney function. Of the patients with moderately reduced kidney function, 2582 (79%) received a bioprosthesis and 684 (21%) received a mechanical valve prosthesis. Baseline characteristics according to kidney function are shown in Table 3. The mean age was 64.3 years in the normal kidney function group and 74.4 years in the moderately reduced kidney function group. Additive EuroSCORE was 5.4 (SD 2.5) in patients with normal kidney function and 7.2 (SD 2.5) in those with moderately reduced kidney function. Patients with moderately reduced kidney function were more likely to receive a bioprosthesis, and were also more likely to be female and have less years of education and more comorbidities.
Survival
During a mean follow‐up of 6.2 years (maximum, 17.2) and a total follow‐up time of 81 871 patient‐years, 1890 (19%) patients in the normal kidney function group died and 1422 (44%) died in the moderately reduced kidney function group. The 5‐, 10‐, and 15‐year survival was 89% versus 76%, 73% versus 48%, and 55% versus 25% in patients with moderately reduced kidney function and normal kidney function, respectively (HR, 2.51; 95% CI, 2.34–2.70; P<0.001). After adjusting for differences in baseline characteristics, the relative risk of death was 28% higher in patients with moderately reduced kidney function compared with those with normal kidney function (HR, 1.28; 95% CI, 1.18–1.38; P<0.001). The early mortality rate was 1.23% (121 of 9837) in the normal kidney function group and 3.52% (115 of 3266) in the moderately reduced kidney function group (adjusted HR, 1.87; 95% CI, 1.39–2.51; P<0.001). Survival curves are shown in Figure 2, and event rates and relative risks are shown in Table 4.
Figure 2.
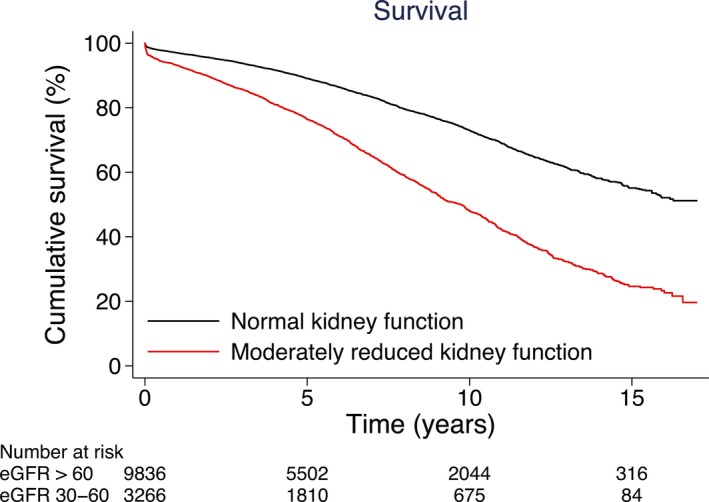
Unadjusted cumulative survival in patients with normal kidney function and moderately reduced kidney function who underwent aortic valve replacement. eGFR indicates estimated glomerular filtration rate.
Table 4.
Event Rates and Relative Risks for All‐Cause Mortality in Patients With Normal Kidney Function (eGFR >60 mL/min per 1.73 m2) and Moderately Reduced Kidney Function (eGFR of 30–60 mL/min per 1.73 m2) Who Underwent AVR in Sweden Between 1997 and 2013
| Normal Kidney Function | Moderately Reduced Kidney Function | |||||
|---|---|---|---|---|---|---|
| Events/PY | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | Events/PY | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | |
| All‐cause mortality | 1890/61 814 | 31 (29–32) | 1422/20 057 | 71 (67–75) | ||
| Unadjusted | 1.00 | 2.51 (2.34–2.70) | ||||
| Adjusted for age | 1.00 | 1.38 (1.28–1.49) | ||||
| Multivariable adjusted modela | 1.00 | 1.28 (1.18–1.38) | ||||
AVR indicates aortic valve replacement; eGFR, estimated glomerular filtration rate; HR, hazard ratio; PY, person‐years.
The multivariable model included all variables in Table 3.
Major Bleeding Events
During a mean follow‐up of 6.4 years (maximum, 16.0) and a total follow‐up of 78 699 patient‐years, a major bleeding event was recorded in 539 (5.9%) patients in the normal kidney function group and 260 (8.4%) in the moderately reduced kidney function group. In the unadjusted analysis, there was a significantly higher risk of major bleeding in patients with moderately reduced kidney function (sHR, 1.20; 95% CI, 1.03–1.39; P=0.018). In the multivariable adjusted analysis, there was a nonsignificant higher risk of major bleeding event in patients with moderately reduced kidney function compared to those with normal kidney function (sHR, 1.18; 95% CI, 1.00–1.39; P=0.051). The cumulative incidence of major bleeding is shown in Figure 3, and event rates and relative risks according to kidney function and prosthesis type are shown in Table 5.
Figure 3.
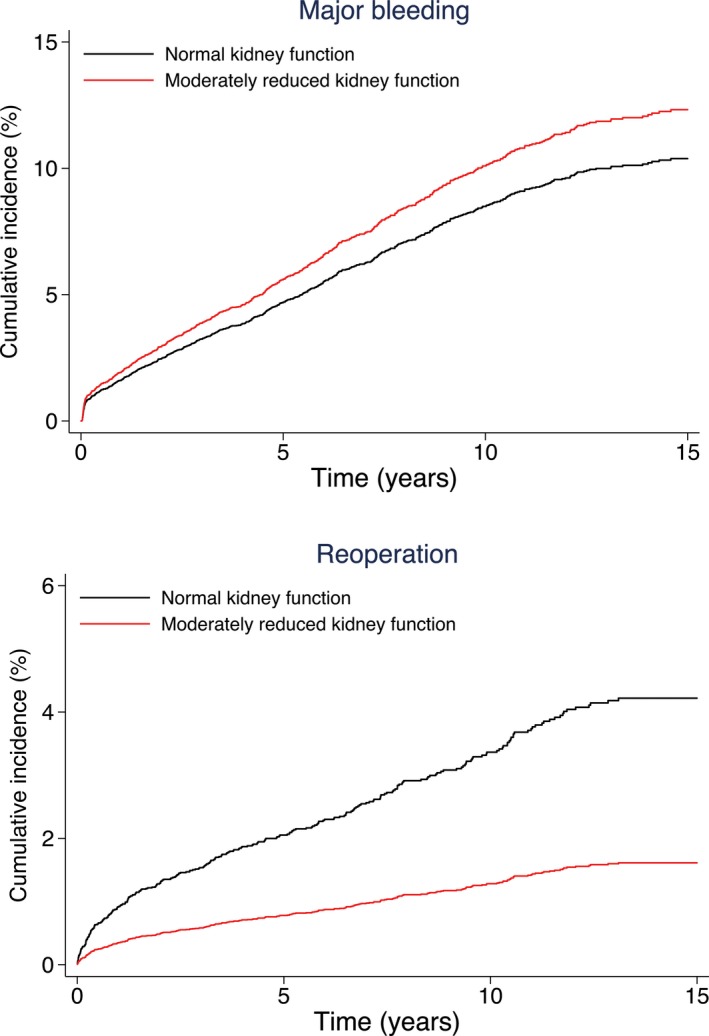
Unadjusted cumulative incidence of major bleeding (upper panel) and aortic valve reoperation (lower panel) in patients with normal kidney function and moderately reduced kidney function who underwent aortic valve replacement.
Table 5.
Event Rates and Relative Risks for Major Bleeding and Aortic Valve Reoperation According to Kidney Function and Prosthesis Type in Patients With Normal Kidney Function (eGFR >60 mL/min per 1.73 m2) and Moderately Reduced Kidney Function (eGFR of 30–60 mL/min per 1.73 m2) Who Underwent AVR in Sweden Between 1997 and 2013
| Normal Kidney Function | Moderately Reduced Kidney Function | |||||
|---|---|---|---|---|---|---|
| Events/No. of Patients | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | Events/No. of Patients | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | |
| Major bleeding | 539/9105 | 10 (9–10) | 260/3100 | 12 (10–13) | ||
| Unadjusted | 1.00 | 1.20 (1.03–1.39) | ||||
| Multivariable adjusted modela | 1.00 | 1.18 (1.00–1.39) | ||||
| Bioprosthesis | 221/5134 | 1.00 | 173/2430 | 1.22 (0.99–1.52) | ||
| Mechanical valve prosthesis | 318/3971 | 1.00 | 87/670 | 1.07 (0.82–1.40) | ||
| Aortic valve reoperation | 265/9836 | 4 (3–4) | 39/3266 | 1 (1–2) | ||
| Unadjusted | 1.00 | 0.38 (0.27–0.53) | ||||
| Multivariable adjusted modela | 1.00 | 0.54 (0.38–0.79) | ||||
| Bioprosthesis | 155/5676 | 1.00 | 23/2582 | 0.40 (0.25–0.63) | ||
| Mechanical valve prosthesis | 110/4160 | 1.00 | 16/684 | 1.03 (0.59–1.79) | ||
AVR indicates aortic valve replacement; eGFR, estimated glomerular filtration rate; HR, hazard ratio; PY, person‐years.
The multivariable model included all variables in Table 3.
Aortic Valve Reoperation
During a mean follow‐up of 7.4 years (maximum, 17.2) and a total follow‐up of 96 901 patient‐years, aortic valve reoperation was conducted in 265 (2.7%) patients in the normal kidney function group and 39 (1.2%) in the moderately reduced kidney function group. There was a significantly higher risk of reoperation in patients with normal kidney function compared to those with moderately reduced kidney function both in the univariable (sHR, 0.38; 95% CI, 0.27–0.53; P<0.001) and the multivariable adjusted analysis (sHR, 0.54; 95% CI, 0.38–0.79; P=0.001). Cumulative incidence of aortic valve reoperation is shown in Figure 3, and event rates and relative risks according to kidney function and prosthesis type are shown in Table 5.
Bioprostheses Versus Mechanical Valve Prostheses in Patients With Moderately Reduced Kidney Function
In 3266 patients with moderately reduced kidney function, death occurred in 1121 (43%) who received a bioprosthesis and 301 (44%) who received a mechanical valve prosthesis during a mean follow‐up of 6.1 years (maximum, 17.1) and a total follow‐up time of 20 057 patient‐years.
In the unadjusted analysis, patients with moderately reduced kidney function who received a mechanical valve prosthesis had a better survival rate than those who received a bioprosthesis (HR, 1.54; 95% CI, 1.35–1.77; P<0.001). There was a similar risk for all‐cause mortality in patients who received a bioprosthesis compared with a mechanical valve prosthesis in the multivariable adjusted analysis (HR, 0.86; 95% CI, 0.73–1.01; P=0.064) and in the propensity‐score–matched analysis consisting of 480 patient‐pairs (HR, 0.85; 95% CI, 0.70–1.03; P=0.094). All baseline characteristics were well balanced in the propensity‐score–matched cohort (Table 6). Survival curves for the propensity‐score–matched cohort are shown in Figure 4, and the event rates and relative risks are shown in Table 7.
Table 6.
Baseline Characteristics in 960 Propensity‐Score–Matched Patients With Moderately Reduced Kidney Function Who Underwent AVR Between 1997 and 2013
| All Patients (n=960) | Bioprosthesis (n=480) | Mechanical Valve Prosthesis (n=480) | Standardized Difference, % | |
|---|---|---|---|---|
| Age, y, mean (SD) | 69.6 (7.6) | 69.3 (7.3) | 70.0 (7.8) | 8.4 |
| Female sex (%) | 503 (52.4) | 246 (51.2) | 257 (53.5) | 4.6 |
| Civil status (%) | ||||
| Not married | 350 (36.5) | 165 (34.4) | 185 (38.5) | 8.7 |
| Education (%) | ||||
| <10 years | 408 (42.5) | 207 (43.1) | 201 (41.9) | 2.5 |
| 10 to 12 years | 421 (43.9) | 211 (44.0) | 210 (43.8) | 0.4 |
| >12 years | 131 (13.6) | 62 (12.9) | 69 (14.4) | 4.2 |
| Region of birth (%) | ||||
| Non‐Nordic countries | 53 (5.5) | 26 (5.4) | 27 (5.6) | 0.9 |
| Body mass index, kg/cm2, mean (SD) | 26.9 (4.7) | 26.9 (4.9) | 26.9 (4.5) | 0.5 |
| Diabetes mellitus (%) | 147 (15.3) | 78 (16.2) | 69 (14.4) | 5.2 |
| Atrial fibrillation (%) | 266 (27.7) | 142 (29.6) | 124 (25.8) | 8.4 |
| Hypertension (%) | 238 (24.8) | 117 (24.4) | 121 (25.2) | 1.9 |
| Hyperlipidemia (%) | 67 (7.0) | 30 (6.2) | 37 (7.7) | 5.7 |
| Stroke (%) | 103 (10.7) | 56 (11.7) | 47 (9.8) | 6.1 |
| Peripheral vascular disease (%) | 83 (8.6) | 40 (8.3) | 43 (9.0) | 2.2 |
| Chronic pulmonary disease (%) | 96 (10.0) | 52 (10.8) | 44 (9.2) | 5.6 |
| Past myocardial infarction (%) | 74 (7.7) | 33 (6.9) | 41 (8.5) | 6.2 |
| Past PCI (%) | 29 (3.0) | 10 (2.1) | 19 (4.0) | 11.0 |
| Past major bleeding event (%) | 38 (4.0) | 17 (3.5) | 21 (4.4) | 4.3 |
| Alcohol dependency (%) | 16 (1.7) | 7 (1.5) | 9 (1.9) | 3.3 |
| Liver disease (%) | 3 (0.3) | 0 (0.0) | 3 (0.6) | 11.2 |
| Cancer (%) | 70 (7.3) | 38 (7.9) | 32 (6.7) | 4.8 |
| eGFR, mL/min per 1.73 m2 (%) | ||||
| 45 to 60 | 732 (76.2) | 372 (77.5) | 360 (75.0) | 5.9 |
| 30 to 45 | 228 (23.8) | 108 (22.5) | 120 (25.0) | 5.9 |
| Heart failure (%) | 271 (28.2) | 138 (28.7) | 133 (27.7) | 2.3 |
| Left ventricular ejection fraction (%) | ||||
| >50 | 325 (66.7) | 157 (65.4) | 168 (68.0) | 5.5 |
| 30 to 49 | 113 (23.2) | 56 (23.3) | 57 (23.1) | 0.6 |
| <30 | 49 (10.1) | 27 (11.2) | 22 (8.9) | 7.8 |
| Endocarditis (%) | 70 (7.3) | 32 (6.7) | 38 (7.9) | 4.8 |
| Emergent surgery (%) | 22 (2.3) | 11 (2.3) | 11 (2.3) | 0 |
| Isolated AVR (%) | 793 (82.6) | 384 (80.0) | 409 (85.2) | 13.8 |
| Year of surgery (%) | ||||
| 1997 to 2001 | 399 (41.6) | 207 (43.1) | 192 (40.0) | 6.3 |
| 2002 to 2006 | 364 (37.9) | 179 (37.3) | 185 (38.5) | 2.6 |
| 2007 to 2013 | 197 (20.5) | 94 (19.6) | 103 (21.5) | 4.6 |
Divided by prosthesis type. Data are n (%), unless otherwise noted. AVR indicates aortic valve replacement; eGFR, estimated glomerular filtration rate; PCI, percutaneous coronary intervention.
Figure 4.
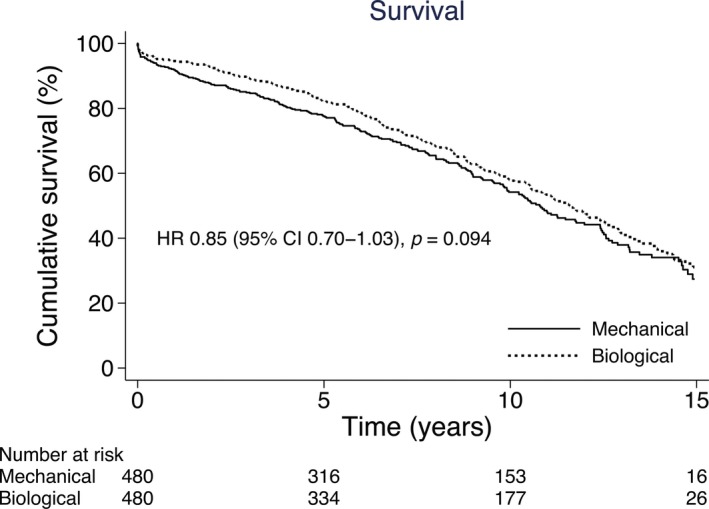
Cumulative survival in propensity‐score–matched patients with moderately reduced kidney function who underwent aortic valve replacement with mechanical valve prostheses versus bioprostheses. HR indicates hazard ratio.
Table 7.
Event Rates and Relative Risks for All‐Cause Mortality in 3266 Patients With Moderately Reduced Kidney Function (eGFR 30–60 mL/min per 1.73 m2) Who Underwent AVR With a Bioprosthesis or a Mechanical Valve
| Mechanical Valve | Bioprosthesis | |||||
|---|---|---|---|---|---|---|
| Events/PY | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | Events/PY | Crude Rate (95% CI) per 1000 PY | HR (95% CI) | |
| Propensity‐score–matched cohort (n=960) | 230/3526 | 6.5 (5.7–7.4) | 1.00 | 220/3809 | 5.8 (5.1–6.6) | 0.85 (0.70–1.03) |
| Overall cohort (n=3266) | 301/5501 | 5.5 (4.9–6.1) | 1121/14 556 | 7.7 (7.3–8.2) | ||
| Unadjusted | 1.00 | 1.54 (1.35–1.77) | ||||
| Adjusted for age | 1.00 | 0.88 (0.75–1.03) | ||||
| Multivariable adjusted modela | 1.00 | 0.86 (0.73–1.01) | ||||
AVR indicates aortic valve replacement; eGFR, estimated glomerular filtration rate; HR, hazard ratio; PY, person‐years.
The multivariable model included all variables in Table 3.
Discussion
In this nation‐wide, population‐based cohort study, the principal finding was that patients with moderately reduced kidney function had a significantly lower long‐term survival rate after AVR than those with normal kidney function. There was a nonsignificantly higher risk for a major bleeding event in patients with moderately reduced kidney function, whereas those with normal kidney function had a significantly higher risk of aortic valve reoperation. In patients with moderately reduced kidney function, there was a similar survival in those who received a bioprosthesis compared to those who received a mechanical valve prosthesis.
Thourani et al10 analyzed the all‐cause mortality and several other factors in 2408 patients after AVR (of which 1502 underwent isolated AVR) with kidney function ranging from normal to ESRD. They found a respective 5‐ and 10‐year survival of 65% and 42% in patients with moderate renal disease (eGFR 30–59 mL/min per 1.73 m2) compared with 79% and 59% in those with mild renal disease (eGFR 60–90 mL/min per 1.73 m2) and 87% and 74% in those with normal renal function (eGFR >90 mL/min per 1.73 m2; HR, 1.55; 95% CI, 1.13–2.12).10 However, they included patients who underwent concomitant CABG.10 This is important because patients with coronary artery disease often have general atherosclerosis. The prognosis after isolated AVR may differ from AVR and concomitant CABG, given that these patients may have a different pathophysiology behind their kidney disease than those with isolated aortic valve disease. Survival in patients with moderate renal disease who underwent isolated AVR (n=369) was not reported in their study.10
Gibson et al25 analyzed all‐cause mortality and 30‐day mortality in 514 patients who underwent AVR and/or mitral valve surgery, with or without CABG, at their institution between 2000 and 2004. Patients were categorized into groups according to eGFR (<45, 45–60, 60–75, and >75 mL/min per 1.73 m2).25 They found that patients with an eGFR <60 mL/min per 1.73 m2 had an increased risk of death at a median of 2 years of follow‐up.25 These results are consistent with our findings. However, inclusion of mitral valve surgery, concomitant CABG, and patients with ESRD makes these results hard to compare, because these are all patient categories that are known to have a worse prognosis.26 Also, their findings are limited by a relatively small sample size and short follow‐up. Other studies in smaller populations and/or based on creatinine as a measure of kidney function have shown similar results.26, 27, 28 In contrast, Ibanez et al29 investigated morbidity and 30‐day mortality in 403 patients after aortic valve surgery with or without CABG with preoperative renal dysfunction (eGFR <60 mL/min per 1.73 m2 excluding hemodialysis) or normal renal function. They found no association between preoperative renal dysfunction and early mortality.29 However, it is difficult to interpret these results because of the small study population, inclusion of patients undergoing concomitant CABG, and lack of long‐term follow‐up.
Owing to the large study population and long and complete follow‐up in the present study, our results clearly strengthen the results of previous studies investigating the prognosis after AVR in patients with moderately reduced kidney function. We believe that our data can serve well as a contemporary reference material for clinicians, public health professionals, and researchers designing trials. Our results suggest that patients with moderately reduced kidney function warrant careful observation after AVR in order to optimize medical therapy and monitor kidney function. Our study also adds knowledge concerning major bleeding, aortic valve reoperation, and survival associated with prosthetic valve type in patients with moderately reduced kidney function.
ESRD is associated with anemia as well as abnormalities in platelet function and platelet‐vessel aggregation, which causes a susceptibility to bleeding.30 It is also known that patients treated with dialysis have a higher risk of a bleeding event after AVR than those without dialysis treatment.9 To our knowledge, the risk of a major bleeding event during follow‐up after AVR in patients with moderately reduced kidney function has not been investigated. We found a nonsignificant higher risk of bleeding in patients with moderately reduced kidney function compared to those with normal kidney function; this increased risk was present in patients who received a bioprosthesis, but not in those who received a mechanical valve prosthesis. The majority of patients with moderately reduced kidney function in our study had an eGFR of 45 to 60 mL/min per 1.73 m2. It is possible that abnormalities in coagulation function become more prominent with more advanced kidney dysfunction. It is also possible that the abnormality in coagulation function that comes with mechanical valves and warfarin treatment is so strong that the increased risk of bleeding in patients with moderately reduced kidney function becomes irrelevant in those treated with warfarin, but relevant in patients with bioprostheses.
Even though it is known that patients with ESRD have a higher prevalence of structural valve deterioration,9 which is the most common indication for aortic valve reoperation, we found that reoperation was more common in patients with normal kidney function than in those with moderately reduced kidney function. A possible explanation for this finding is that patients with moderately reduced kidney function were too frail to undergo a second surgery even when it was indicated. Similarly to previous studies examining which valve type is preferable for patients with ESRD,31, 32 we found no significant association between valve type and survival in patients with moderately reduced kidney function.
Study Limitations
Excluding patients with missing eGFR values might have influenced the generalizability of our study. However, generalizability was increased by our study being a large, nation‐wide, population‐based cohort study. The observational study design comes with some inevitable limitations. We used regression models to adjust for measured and known confounding factors. However, there might have been other factors that were unknown or unmeasured that we were not able to account for (residual confounding). For example, we did not have information regarding implanted valve size, cardiopulmonary bypass time, and cause of CKD. Furthermore, creatinine values may differ in the same individual if taken at different occasions; because we based eGFR on a single value of creatinine sampled preoperatively, we might not have gotten a representative value. Also, information about albuminuria, which is considered a sign of CKD, was not available in our study. Furthermore, some adverse events might have happened outside of Sweden, which might have led to underestimation of the rate of major bleeding and aortic valve reoperation. However, all deaths are listed in the Cause of Death Register, regardless of whether death occurred abroad; therefore, follow‐up for the primary outcome was complete. The long and complete follow‐up and the large number of patients are particular strengths of our study, which was made possible by crosslinking of high‐quality Swedish registers.
Conclusions
Moderately reduced kidney function was significantly associated with increased mortality after AVR. There was a nonsignificant higher risk for major bleeding events and a significantly lower risk for aortic valve reoperation in patients with moderately reduced kidney function compared to those with normal kidney function. In patients with moderately reduced kidney function, there was a similar survival in those who received a bioprosthesis and those who received a mechanical valve prosthesis. These results have important implications for preoperative risk stratification, and suggest that patients with eGFR 30 to 60 mL/min per 1.73 m2 warrant careful observation after AVR. Further investigation is needed to determine which prosthesis type (bioprosthetic or mechanical) should be recommended to patients with moderately reduced kidney function.
Sources of Funding
This study was supported by Karolinska Institutet Foundations and Funds (Grant No. 40842 to Sartipy), the Mats Kleberg Foundation (Grant No. 2015‐00097 to Sartipy), the Swedish Heart‐Lung Foundation (Grant No. 20150528 to Sartipy and Grant No. 20150603 to Holzmann), and a donation from Mr Fredrik Lundberg (to Franco‐Cereceda).
Disclosures
None.
Acknowledgments
We thank the SWEDEHEART steering committee for providing data for this study.
(J Am Heart Assoc. 2016;5:e004287 doi: 10.1161/JAHA.116.004287)
Abstract presented and published during the 8th Joint Scandinavian Conference in Cardiothoracic Surgery, August 17 to 19, 2016, in Reykjavik, Iceland.
References
- 1. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. [DOI] [PubMed] [Google Scholar]
- 2. De Nicola L, Donfrancesco C, Minutolo R, Lo Noce C, Palmieri L, De Curtis A, Iacoviello L, Zoccali C, Gesualdo L, Conte G, Vanuzzo D, Giampaoli S; Group A‐SR . Prevalence and cardiovascular risk profile of chronic kidney disease in Italy: results of the 2008–12 National Health Examination Survey. Nephrol Dial Transplant. 2015;30:806–814. [DOI] [PubMed] [Google Scholar]
- 3. Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW; American Heart Association Councils on Kidney in Cardiovascular Disease HBPRCC, Epidemiology and Prevention . Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension. 2003;42:1050–1065. [DOI] [PubMed] [Google Scholar]
- 4. London GM, Pannier B, Marchais SJ, Guerin AP. Calcification of the aortic valve in the dialyzed patient. J Am Soc Nephrol. 2000;11:778–783. [DOI] [PubMed] [Google Scholar]
- 5. Baglin A, Hanslik T, Vaillant JN, Boulard JC, Moulonguet‐Doleris L, Prinseau J. Severe valvular heart disease in patients on chronic dialysis. A five‐year multicenter French survey. Ann Med Interne (Paris). 1997;148:521–526. [PubMed] [Google Scholar]
- 6. Stewart BF, Siscovick D, Lind BK, Gardin JM, Gottdiener JS, Smith VE, Kitzman DW, Otto CM. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–634. [DOI] [PubMed] [Google Scholar]
- 7. Zentner D, Hunt D, Chan W, Barzi F, Grigg L, Perkovic V. Prospective evaluation of aortic stenosis in end‐stage kidney disease: a more fulminant process? Nephrol Dial Transplant. 2011;26:1651–1655. [DOI] [PubMed] [Google Scholar]
- 8. Thourani VH, Sarin EL, Kilgo PD, Lattouf OM, Puskas JD, Chen EP, Guyton RA. Short‐ and long‐term outcomes in patients undergoing valve surgery with end‐stage renal failure receiving chronic hemodialysis. J Thorac Cardiovasc Surg. 2012;144:117–123. [DOI] [PubMed] [Google Scholar]
- 9. Okada N, Tajima K, Takami Y, Kato W, Fujii K, Hibino M, Munakata H, Sakai Y, Hirakawa A, Usui A. Valve selection for the aortic position in dialysis patients. Ann Thorac Surg. 2015;99:1524–1531. [DOI] [PubMed] [Google Scholar]
- 10. Thourani VH, Keeling WB, Sarin EL, Guyton RA, Kilgo PD, Dara AB, Puskas JD, Chen EP, Cooper WA, Vega JD, Morris CD, Halkos ME, Lattouf OM. Impact of preoperative renal dysfunction on long‐term survival for patients undergoing aortic valve replacement. Ann Thorac Surg. 2011;91:1798–1806. [DOI] [PubMed] [Google Scholar]
- 11. Dalen M, Ivert T, Holzmann MJ, Sartipy U. Household disposable income and long‐term survival after cardiac surgery: a Swedish Nationwide Cohort Study in 100,534 patients. J Am Coll Cardiol. 2015;66:1888–1897. [DOI] [PubMed] [Google Scholar]
- 12. Yamamoto M, Hayashida K, Mouillet G, Hovasse T, Chevalier B, Oguri A, Watanabe Y, Dubois‐Rande JL, Morice MC, Lefevre T, Teiger E. Prognostic value of chronic kidney disease after transcatheter aortic valve implantation. J Am Coll Cardiol. 2013;62:869–877. [DOI] [PubMed] [Google Scholar]
- 13. Cooper WA, O'Brien SM, Thourani VH, Guyton RA, Bridges CR, Szczech LA, Petersen R, Peterson ED. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the Society of Thoracic Surgeons National Adult Cardiac Database. Circulation. 2006;113:1063–1070. [DOI] [PubMed] [Google Scholar]
- 14. Hillis GS, Croal BL, Buchan KG, El‐Shafei H, Gibson G, Jeffrey RR, Millar CG, Prescott GJ, Cuthbertson BH. Renal function and outcome from coronary artery bypass grafting: impact on mortality after a 2.3‐year follow‐up. Circulation. 2006;113:1056–1062. [DOI] [PubMed] [Google Scholar]
- 15. Emilsson L, Lindahl B, Koster M, Lambe M, Ludvigsson JF. Review of 103 Swedish healthcare quality registries. J Intern Med. 2015;277:94–136. [DOI] [PubMed] [Google Scholar]
- 16. Jernberg T, Attebring MF, Hambraeus K, Ivert T, James S, Jeppsson A, Lagerqvist B, Lindahl B, Stenestrand U, Wallentin L. The Swedish web‐system for enhancement and development of evidence‐based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart. 2010;96:1617–1621. [DOI] [PubMed] [Google Scholar]
- 17. National Kidney F . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 18. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD EPI . A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ludvigsson JF, Otterblad‐Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Glaser N, Jackson V, Holzmann MJ, Franco‐Cereceda A, Sartipy U. Aortic valve replacement with mechanical vs. biological prostheses in patients aged 50–69 years. Eur Heart J. 2016;37:2658–2667. [DOI] [PubMed] [Google Scholar]
- 21. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 22. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. [DOI] [PubMed] [Google Scholar]
- 24. White IR, Royston P. Imputing missing covariate values for the Cox model. Stat Med. 2009;28:1982–1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gibson PH, Croal BL, Cuthbertson BH, Chiwara M, Scott AE, Buchan KG, El‐Shafei H, Gibson G, Jeffrey RR, Hillis GS. The relationship between renal function and outcome from heart valve surgery. Am Heart J. 2008;156:893–899. [DOI] [PubMed] [Google Scholar]
- 26. Edwards FH, Peterson ED, Coombs LP, DeLong ER, Jamieson WR, Shroyer ALW, Grover FL. Prediction of operative mortality after valve replacement surgery. J Am Coll Cardiol. 2001;37:885–892. [DOI] [PubMed] [Google Scholar]
- 27. Anderson RJ, O'Brien M, MaWhinney S, VillaNueva CB, Moritz TE, Sethi GK, Henderson WG, Hammermeister KE, Grover FL, Shroyer AL. Mild renal failure is associated with adverse outcome after cardiac valve surgery. Am J Kidney Dis. 2000;35:1127–1134. [DOI] [PubMed] [Google Scholar]
- 28. Nowicki ER, Birkmeyer NJ, Weintraub RW, Leavitt BJ, Sanders JH, Dacey LJ, Clough RA, Quinn RD, Charlesworth DC, Sisto DA, Uhlig PN, Olmstead EM, O'Connor GT; Northern New England Cardiovascular Disease Study G and the Center for Evaluative Clinical Sciences DMS . Multivariable prediction of in‐hospital mortality associated with aortic and mitral valve surgery in Northern New England. Ann Thorac Surg. 2004;77:1966–1977. [DOI] [PubMed] [Google Scholar]
- 29. Ibanez J, Riera M, Saez de Ibarra JI, Carrillo A, Fernandez R, Herrero J, Fiol M, Bonnin O. Effect of preoperative mild renal dysfunction on mortality and morbidity following valve cardiac surgery. Interact Cardiovasc Thorac Surg. 2007;6:748–752. [DOI] [PubMed] [Google Scholar]
- 30. Kaw D, Malhotra D. Platelet dysfunction and end‐stage renal disease. Semin Dial. 2006;19:317–322. [DOI] [PubMed] [Google Scholar]
- 31. Boeken U, Schurr P, Feindt P, Litmathe J, Kurt M, Gams E. Cardiac valve replacement in patients with end‐stage renal failure: impact of prosthesis type on the early postoperative course. Thorac Cardiovasc Surg. 2010;58:23–27. [DOI] [PubMed] [Google Scholar]
- 32. Herzog CA, Ma JZ, Collins AJ. Long‐term survival of dialysis patients in the United States with prosthetic heart valves: should ACC/AHA practice guidelines on valve selection be modified? Circulation. 2002;105:1336–1341. [DOI] [PubMed] [Google Scholar]


