Abstract
Background
The incidence of hypertensive emergency in US emergency departments (ED) is not well established.
Methods and Results
This study is a descriptive epidemiological analysis of nationally representative ED visit‐level data from the Nationwide Emergency Department Sample for 2006–2013. Nationwide Emergency Department Sample is a publicly available database maintained by the Healthcare Cost and Utilization Project. An ED visit was considered to be a hypertensive emergency if it met all the following criteria: diagnosis of acute hypertension, at least 1 diagnosis indicating acute target organ damage, and qualifying disposition (admission to the hospital, death, or transfer to another facility). The incidence of adult ED visits for acute hypertension increased monotonically in the period from 2006 through 2013, from 170 340 (1820 per million adult ED visits overall) to 496 894 (4610 per million). Hypertensive emergency was rare overall, accounting for 63 406 visits (677 per million adult ED visits overall) in 2006 to 176 769 visits (1670 per million) in 2013. Among adult ED visits that had any diagnosis of hypertension, hypertensive emergency accounted for 3309 per million in 2006 and 6178 per million in 2013.
Conclusions
The estimated number of visits for hypertensive emergency and the rate per million adult ED visits has more than doubled from 2006 to 2013. However, hypertensive emergencies are rare overall, occurring in about 2 in 1000 adult ED visits overall, and 6 in 1000 adult ED visits carrying any diagnosis of hypertension in 2013. This figure is far lower than what has been sometimes cited in previous literature.
Keywords: cost, high blood pressure, hypertension, hypertensive emergency, hypertensive urgency, utilization
Subject Categories: Cardiovascular Disease, Myocardial Infarction, Heart Failure, Cerebrovascular Disease/Stroke, Epidemiology
Hypertensive emergencies are defined by marked blood pressure (BP) elevations (typically >180 mm Hg systolic or >110 mm Hg diastolic, though this cutoff is arbitrary) that are associated with acute target organ damage.1, 2, 3, 4 Target organs typically involved include those in the cardiovascular, renal, or central nervous systems.5, 6 While not all patients with markedly elevated BP have a hypertensive emergency, initiation of appropriate treatment for those who do is critical as delays are associated with significant morbidity and mortality.7 However, caution is warranted as patients with chronically elevated BP have a rightward shift in cerebral blood flow autoregulation, placing them at risk of stroke and myocardial infarction when BP is lowered too rapidly.
Despite the importance of hypertensive emergency, the burden of this condition is not known, and there are conflicting views of the epidemiology in academic literature. Prior empirical evidence from claims data suggests that the annual hospitalization rate for hypertensive emergencies is 1 or 2 per million.8 Data from the Nationwide Inpatient Sample, a multicenter database developed as part of the Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project to track hospital discharges, analyzed in the wake of the Seventh Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure,9 place this figure higher, reporting an annual frequency of hospitalizations for a hypertensive emergency in US adults of 101 per 100 000 in 2000 and 111 per 100 000 in 2007.10
While important, these data exclude information on the emergency department (ED) phase of patient care and provide little insight into the relative volume of patients who present to EDs with a hypertensive emergency. At present, the only existing comprehensive epidemiological data related to this come from 1 study of a Brazilian population, where hypertensive emergencies were found to be present in 0.3% of all ED visits.11 Despite the limited empirical evidence, there are claims in the literature that hypertensive emergencies make up as much as one fourth of all ED visits,12 orders of magnitude more than existing estimates. Such uncertainty about the incidence of hypertensive emergencies occurs in the context of a significant and growing perspective that hypertension is a public health problem.13, 14 One study found that hypertension‐related hospitalizations increased by more than 27% in the period from 2000 to 2011.15 Hypertension‐related ED visits increased in the period from 2006 to 2012 by an estimated 5.2% per year, from 20.5% to 25.7%.16 From both epidemiological and clinical perspectives, more information on the ED burden of hypertensive emergencies would be of great value.
Goals of This Investigation
The goal of this investigation is to characterize the incidence of hypertensive emergency in EDs nationwide in the period from 2006 through 2013.
Materials and Methods
Study Design, Setting, and Study Population
This is a descriptive epidemiological analysis of ED visit data from the Nationwide Emergency Department Sample (NEDS) for 2006–2013. NEDS is a publicly available database maintained by the Healthcare Cost and Utilization Project and funded by the Agency for Healthcare Research and Quality. NEDS is designed to provide nationally representative estimates of all ED visits. These databases are compiled from State Emergency Department Databases and State Inpatient Databases as part of the Healthcare Cost and Utilization Project. In 2013, 30 states and 947 hospitals contributed data on ED visits representing ≈20% of all hospital‐based ED visits. Up to 15 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9 CM) codes for the ED visit are included, as well as more than 50 other patient, visit, hospital, and region‐level variables. Observation‐level weighting was used to generate estimates representative of ED visits nationwide, and standard errors are calculated with adjustment for the complex sampling design of the survey. Estimates of ED utilization using NEDS are congruent with results from the National Hospital Ambulatory Medical Care Survey.17, 18, 19 As all NEDS data are fully deidentified, this analysis was approved by the Wayne State University Institutional Review Board under exempt status.
The study population was limited to adult (age ≥18 years) ED visits from January 2006 through December 2013. Patient diagnoses were defined according to ICD‐9 CM codes. An ED visit was considered to be a hypertensive emergency if it met all of the following criteria: diagnosis of acute hypertension (any ICD‐9 CM code of primary malignant hypertension [401.0], secondary malignant hypertension [405.01, 405.09], or malignant hypertensive heart/kidney disease [402.00, 402.01, 403.00, 403.01, 404.00, 404.01, 404.02, 404.03]), at least 1 concurrent diagnosis indicating acute target organ damage (defined below), and qualifying disposition (admission to the hospital, death, or transfer to another facility). There is support in the literature for the view that hypertensive emergency is a clinical condition that requires hospital admission.20 Thus, all visits that culminated in discharge from the ED were excluded as such a disposition is inconsistent with presence of a true hypertensive emergency, regardless of ICD‐9 coding. Acute target organ damage was defined by additional coding for any one of the following: retinal hemorrhage (362.81), papilledema with increased intracranial pressure (377.01), acute or unspecified (not chronic) heart failure (428.0, 428.1, 428.20, 428.21, 428.23, 428.30, 428.31, 428.33, 428.40, 428.41, 428.43, 428.9), acute myocardial infarction/acute coronary occlusion (410.x), ruptured aneurysm or dissection of a major vessel (414.12, 443.21, 443.22, 443.23, 443.24, 443.29, 441.x), subarachnoid hemorrhage (430.x), intracerebral hemorrhage (431.x), nontraumatic extradural hemorrhage (432.x), cerebral thrombosis (434.x), transient cerebral ischemia (435.x), other cerebrovascular disease (436.x), or hypertensive encephalopathy (437.2). An ED visit was defined to be hypertension‐related generally if any 1 of the following diagnosis codes were present: 401.x to 405.x, or 437.2.
Data Analysis
The analyses for this study were performed according to recommendations from the Agency for Healthcare Research and Quality for weighting and stratification. All values reported are weighted to be nationally representative. Yearly incidence rates were calculated for the criteria defining hypertensive emergency, including subgroup analyses for each type of target organ damage (eye, heart, blood vessel, and brain). The proportions of ED visits for hypertensive emergency were calculated separately with denominator of all ED visits, ED visits resulting in admission, and hypertension‐related ED visits (401.x–405.x, 437.2). Patient and hospital‐level characteristics were compiled among ED visits with hypertensive emergency. Variables summarized for those visits qualifying as hypertensive emergencies are the following: ED disposition, hospital disposition (for those patients who were admitted to the same hospital where they presented to the ED), ED charges (by quartile), primary payer (Medicare, Medicaid, private insurance, self‐pay, and no charge), hospital length of stay in days (by quartile), age in years (by quartile, where all ages over 89 are placed into a single category), percent female, and median household income in patient's home zip code (by percent in each income quartile). A logistic regression model was performed to estimate the unadjusted annual change in incidence rates for hypertensive emergency ED visits, taking into account the complex sampling design, including weighting and stratification, of the sample. An additional logistic regression model was also performed, which included adjustment for primary payer, income quartile of the patient's zip code, age, and sex. All analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC).
Results
Main Results
Figure 1 depicts how the study population was derived, and from that sample, how hypertensive emergency was defined. Figure 2 shows the trend in absolute number of ED visits for acute hypertension, acute hypertension with qualifying disposition (admission, death in ED, transfer to another hospital), acute hypertension with target organ damage, and hypertensive emergency (all 3 criteria). As depicted in Figure 2, the incidence of ED visits carrying a diagnosis of acute hypertension increased monotonically from 2006 through 2013, from a low of 170 340 (95% CI 155 291–185 340) to a high of 496 894 (95% CI 448 103–545 586). This tracked the total number of ED visits in the United States fairly closely as depicted in the figure. In 2013, this accounted for 4610 per million ED visits for patients 18 years and older nationwide. There was a similar increase in the number of ED visits for acute hypertension that also carried a diagnosis for acute target organ damage, from 65 925 (95% CI 59 872–71 966) to 188 696 (95% CI 170 284–207 082), and in the number of ED visits for acute hypertension that also carried a qualifying disposition (admission, death in ED, or transfer to another facility), from 63 406 (95% CI 57 297–69 584) to 398 506 (95% CI 356 724–440 243). Among diagnoses for acute target organ damage, heart failure was the most common, present in 117 848 hypertensive emergencies in 2013. The second most common diagnosis was cerebrovascular disease or stroke, with 51 062 visits in 2013. Papilledema and retinal hemorrhage associated with increased intracranial pressure were relatively rare, with only 194 total hypertensive emergencies in 2013 carrying these ICD‐9 CM diagnosis codes.
Figure 1.
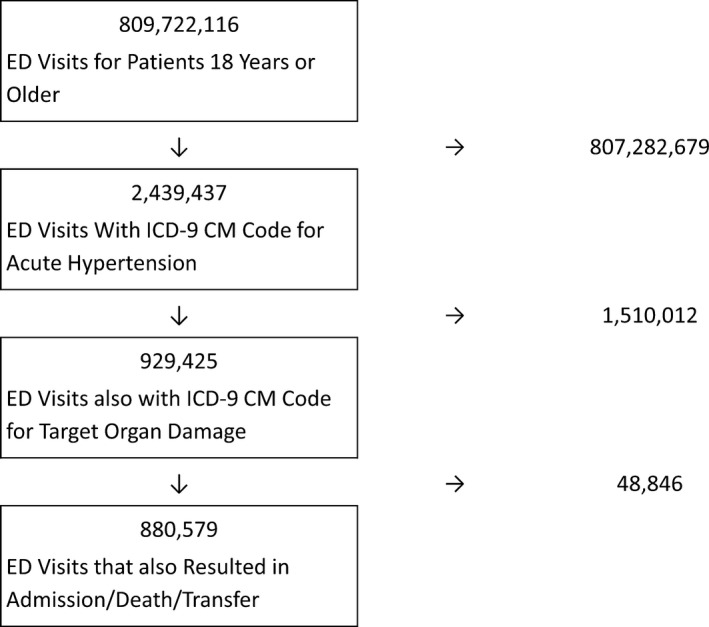
Study design and sample, NEDS 2006–2013. ICD‐9 CM codes: malignant hypertension (401.0) including hypertensive heart/kidney disease (402.00, 402.01, 403.00, 403.01, 404.00, 404.01, 404.02, 404.03), target organ damage including any 1 of the following: retinal hemorrhage (362.81), papilledema with increased intracranial pressure (377.01), acute or unspecified (not chronic) heart failure (428.0, 428.1, 428.20, 428.21, 428.23, 428.30, 428.31, 428.33, 428.40, 428.41, 428.43, 428.9), acute myocardial infarction/acute coronary occlusion (410.x), ruptured aneurysm or dissection of a major vessel (414.12, 443.21, 443.22, 443.23, 443.24, 443.29, 441.x), subarachnoid hemorrhage (430.x), intracerebral hemorrhage (431.x), nontraumatic extradural hemorrhage (432.x), cerebral thrombosis (434.x), transient cerebral ischemia (435.x), other cerebrovascular disease (436.x), or hypertensive encephalopathy (437.2). ED indicates emergency department; ICD‐9 CM, International Classification of Diseases, Ninth Revision, Clinical Modification; NEDS, Nationwide Emergency Department Sample.
Figure 2.
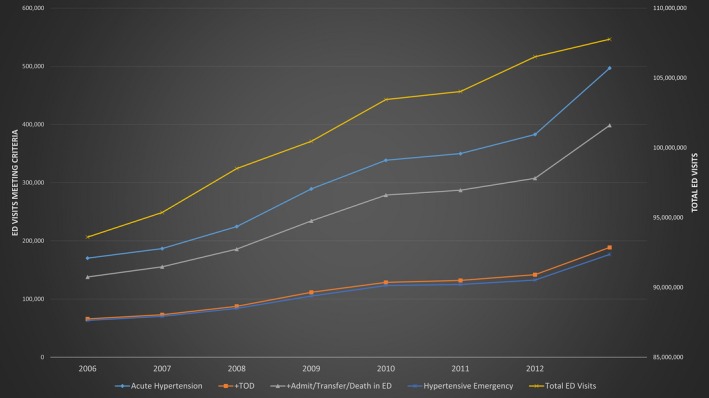
Trends in the incidence of hypertensive emergency in US Emergency Departments, 2006–2013. ED indicates emergency department; TOD, target organ damage; the right‐sided vertical axis is for number of total ED visits; the left‐sided vertical axis is for ED visits meeting each of the criteria given.
Total hypertensive emergencies by our definition increased by 16.2% per year from 2006 to 2013, while the overall number of ED visits in that same period increased at an average rate of 2.0% year‐over‐year. Despite such a large increase, in terms of the rate per million adult ED visits, hypertensive emergencies remained a rare diagnosis, with an incidence of 677 per million adult ED visits in 2006 and 1640 per million adult ED visits in 2013, yielding an estimated rate increase of 13.9% per year (P<0.0001). This year‐over‐year change in the incidence of hypertensive emergency remained statistically significant (P<0.0001) even after adjustment for payer, income, age, and sex. In these estimates, the denominator is total number of adult ED visits, and this should not be interpreted as the raw number of ED visits for hypertensive emergency, which were given above. Table 1 summarizes these results and the distribution of diagnoses for target organ damage associated with hypertensive emergency, from 2006 through 2013. Table 2 depicts hypertensive emergency rate per million with varying denominator: among all ED visits, among ED visits resulting in admission, and among ED visits with any diagnosis of hypertension.
Table 1.
ED Visits With Diagnoses for Acute Hypertension 2006–2013
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|
| ED visits (total|rate per million) | ||||||||
| Acute hypertension | 170 340 | 186 749 | 224 626 | 289 361 | 338 608 | 349 960 | 382 899 | 496 894 |
| 1820 | 1958 | 2280 | 2880 | 3273 | 3364 | 3595 | 4610 | |
| Acute hypertension+routine discharge from ED | 30 703 | 29 659 | 35 564 | 50 936 | 56 380 | 58 985 | 69 981 | 90 598 |
| 328 | 311 | 361 | 507 | 545 | 567 | 657 | 838 | |
| Acute hypertension+admitted/died in ED/transferred to another hospital | 137 965 | 155 514 | 185 865 | 234 399 | 278 668 | 287 131 | 307 652 | 398 506 |
| 1474 | 1630 | 1897 | 2333 | 2694 | 2760 | 2888 | 3697 | |
| Acute hypertension+target organ damage | 65 925 | 73 021 | 87 546 | 111 640 | 128 710 | 132 002 | 141 885 | 188 696 |
| 704 | 766 | 889 | 1111 | 1244 | 1269 | 1332 | 1751 | |
| Hypertensive emergencya | 63 406 | 70 344 | 83 959 | 105 116 | 123 233 | 125 068 | 132 684 | 176 769 |
| 677 | 738 | 852 | 1046 | 1191 | 1202 | 1246 | 1640 | |
| Papilledema/retinal hemorrhage | 160 | 138 | 180 | 125 | 195 | 217 | 204 | 194 |
| 2 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | |
| Heart failure | 41 962 | 46 712 | 53 641 | 70 038 | 81 549 | 83 287 | 89 242 | 117 848 |
| 448 | 490 | 544 | 697 | 788 | 801 | 838 | 1094 | |
| Myocardial infarction | 6456 | 7042 | 9220 | 12 011 | 13 634 | 14 821 | 16 043 | 22 744 |
| 69 | 74 | 94 | 120 | 132 | 142 | 151 | 211 | |
| Ruptured aneurysm/dissection | 2405 | 2879 | 3556 | 4151 | 4890 | 5135 | 5553 | 6805 |
| 26 | 30 | 36 | 41 | 47 | 49 | 52 | 63 | |
| Intracranial hemorrhage | 5003 | 5667 | 7181 | 7848 | 9743 | 8635 | 9301 | 13 503 |
| 53 | 59 | 73 | 78 | 94 | 83 | 87 | 125 | |
| Other cerebrovascular disease/stroke | 18 317 | 19 715 | 24 353 | 31 405 | 35 284 | 36 359 | 38 063 | 51 062 |
| 196 | 207 | 247 | 313 | 341 | 350 | 357 | 474 | |
ED indicates emergency department.
Note this row includes ED visits that met all 3 criteria: diagnosis of acute hypertension, admission/death/transfer, and additional diagnosis of target organ damage.
Table 2.
Proportion of ED Visits for Hypertensive Emergency 2006–2013
| ED Visits (Total|Rate Per Million) | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|
| Among ED visits overall | 677 | 738 | 852 | 1046 | 1191 | 1202 | 1246 | 1640 |
| Among ED visits resulting in admission | 3592 | 3899 | 4525 | 5593 | 6495 | 6652 | 7228 | 9529 |
| Among ED visits with diagnosis of hypertension | 3309 | 3429 | 3742 | 4383 | 4791 | 4669 | 4852 | 6178 |
ED indicates emergency department.
Characteristics of ED Visits
Table 3 depicts demographic information about patients with hypertensive emergency from 2006 through 2013. For 2013, 4.5% of ED visits qualifying as hypertensive emergency resulted in patient's death, either in ED or during the following hospital admission. The mortality rate was 4.8% in 2006, for an absolute decrease in total mortality rate of 0.3%, though this change was not monotonic year‐over‐year. Visits for hypertensive emergency tended to occur in older patients (median age was 66 years in 2013) who were slightly more likely to be female (54.5% in 2013). In addition, a sizeable proportion (39.7%) of hypertensive emergency ED visits were from patients who lived in zip codes with average income in the bottom quartile. Overall, 63.0% of ED visits for hypertensive emergency had primary payer as Medicare, 10.7% had Medicaid, and another 7.9% were categorized as self‐pay in 2012. Median total ED charges among visits for hypertensive emergency rose monotonically from $956 in 2006 to $1800 in 2013.
Table 3.
Characteristics of ED Visits Classified as Hypertensive Emergency 2006–2013
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|
| ED disposition, % | ||||||||
| Admitted | 98.4 | 96.6 | 98.4 | 98.4 | 98.7 | 98.8 | 98.4 | 98.7 |
| Died in ED | 1.3 | 1.2 | 1.5 | 1.5 | 1.3 | 1.1 | 1.5 | 1.2 |
| Transferred to another hospital | 0.0 | 0.0 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 |
| Hospital disposition, % | ||||||||
| Routine | 56.5 | 55.2 | 54.5 | 55.0 | 54.0 | 52.2 | 54.2 | 52.1 |
| Transfer to acute care facility | 4.6 | 4.3 | 3.8 | 4.2 | 3.5 | 3.7 | 3.4 | 3.2 |
| SNF/rehabilitation | 21.1 | 22.2 | 22.7 | 22.4 | 22.5 | 23.6 | 22.5 | 23.8 |
| Home health care | 11.6 | 12.1 | 13.2 | 13.4 | 14.7 | 15.8 | 15.4 | 16.2 |
| Against medical advice | 1.4 | 1.6 | 1.4 | 1.3 | 1.3 | 1.5 | 1.5 | 1.5 |
| Died in hospital | 4.7 | 4.5 | 4.4 | 3.7 | 3.9 | 3.2 | 2.9 | 3.2 |
| ED charges (US$) | ||||||||
| Median | $956 | $971 | $1205 | $1298 | $1394 | $1497 | $1671 | $1800 |
| Q1 | $588 | $613 | $785 | $836 | $940 | $1005 | $1080 | $1119 |
| Q3 | $1478 | $1534 | $1835 | $1939 | $2088 | $2288 | $2477 | $2597 |
| Primary payer, % | ||||||||
| Medicare | 60.4 | 59.2 | 59.5 | 60.3 | 60.4 | 62.8 | 62.8 | 63.0 |
| Medicaid | 10.4 | 11.5 | 10.8 | 11.8 | 11.4 | 10.8 | 11.4 | 10.7 |
| Private insurance | 18.1 | 18.9 | 18.7 | 17.8 | 16.4 | 15.4 | 14.5 | 14.8 |
| Self‐pay | 8.2 | 7.7 | 8.2 | 7.6 | 9.0 | 7.6 | 8.2 | 7.9 |
| No charge | 0.7 | 0.6 | 0.5 | 0.6 | 0.4 | 0.7 | 0.5 | 0.8 |
| Length of stay for admitted patients, days | ||||||||
| Median | 4.1 | 4.0 | 4.0 | 3.8 | 3.7 | 3.7 | 3.6 | 3.7 |
| Q1 | 2.3 | 2.2 | 2.2 | 2.1 | 2.0 | 2.0 | 1.9 | 2.0 |
| Q3 | 7.4 | 7.5 | 7.3 | 6.9 | 6.8 | 6.6 | 6.5 | 6.6 |
| Age, y | ||||||||
| Median | 65 | 65 | 65 | 65 | 65 | 66 | 66 | 66 |
| Q1 | 51 | 52 | 53 | 53 | 53 | 54 | 54 | 54 |
| Q3 | 77 | 78 | 78 | 78 | 78 | 79 | 79 | 78 |
| Female, % | 54.8 | 55.0 | 55.1 | 55.4 | 54.8 | 54.7 | 54.3 | 54.5 |
| Median household income, % | ||||||||
| 1st quartile | 39.1 | 37.8 | 37.8 | 37.6 | 38.8 | 36.8 | 37.3 | 39.7 |
| 2nd quartile | 25.5 | 26.6 | 28.1 | 29.3 | 25.9 | 24.8 | 25.7 | 27.0 |
| 3rd quartile | 19.9 | 21.0 | 18.8 | 20.3 | 20.2 | 22.7 | 22.2 | 20.5 |
| 4th quartile | 15.5 | 14.6 | 15.2 | 12.8 | 15.2 | 15.7 | 14.8 | 12.7 |
ED indicates emergency department; SNF, skilled nursing facility.
Discussion
Our primary finding is that ED visits for hypertensive emergency, that is, ED visits for patients who have markedly elevated BP with acute target organ damage and an acuity level high enough to necessitate hospital admission, are quite rare, accounting for less than 2 in 1000 adult ED visits and 6 in 1000 visits carrying any diagnosis of hypertension in 2013. Thus, while markedly elevated BP at presentation to the ED is quite common,21, 22 occurring in nearly 20% of patients,23 the likelihood that it represents a true hypertensive emergency may be lower than previously thought.12
By definition, true hypertensive emergencies are an indication for rapid BP lowering. The management of hypertensive emergency is to limit and reverse target organ damage, but not to achieve a “normal” BP.24 Treatment of a true hypertensive emergency invariably includes intravenous antihypertensive therapy, but in the wrong patient, their use can precipitate adverse events, including acute kidney injury, myocardial infarct, or stroke. A careful balance is therefore required in the management of patients with markedly elevated BP. By recalibrating the expected proportion of patients with elevated BP who have acute target organ damage, our data could help avoid unnecessary and potentially harmful treatment. Unfortunately, the NEDS cannot clarify whether ED visits qualifying as hypertensive emergencies according to our definition resulted in management that included rapid lowering of BP. As this is a hallmark of treatment for true hypertensive emergencies, addition of such data would be highly informative. In the context of our relatively expansive definition with respect to ICD‐9 codes, and given that adding treatment criteria would narrow the definition's scope, results of this analysis are more likely to be an upper bound. This supports our overall assertion that hypertensive emergencies are, on the whole, relatively rare in the ED setting. In addition, use of treatment status to define hypertensive emergency for the purpose of estimating incidence would require the assumption that every patient with true hypertensive emergency is indeed treated.
An additional potential limitation of this investigation is the definition we used to establish presence of hypertensive emergency. For the purpose of providing a nationwide epidemiological analysis, we defined hypertensive emergency using a combination of ED visit ICD‐9 CM codes and patient disposition from the ED. However, the NEDS database is built out of claims data, rather than prospectively collected data designed to address specific research or clinical questions. Thus, the NEDS database does not contain clinical information such as BPs or laboratory values, and some important demographic data including race and ethnicity. That said, in clinical practice it is uncommon to assign a primary or secondary diagnosis of hypertension, malignant or other, absent elevated BP. This makes it more likely that the visits we captured did indeed reflect clinically relevant BP elevations. There may also have been patients for whom acute target organ damage was secondary to or associated with elevated BP but hypertension itself was not a coded diagnosis for the visit. Unfortunately, these patients cannot be identified using NEDS data. However, given the link between reimbursement and illness severity in the United States, it is likely that, whenever possible, risk‐enhancing variables such as hypertension would be included during the coding process.
In general, hypertensive emergency is an imprecise clinical diagnosis, and this study is fundamentally limited for that reason. Well‐defined clinical criteria in a large prospective study would be necessary to make a more precise statement about incidence, though even then there would be important limitations. As an example, diagnosis of papilledema may vary substantially for the same patient between different physicians. There may also be changing coding patterns over time, so that apparent disease prevalence rises despite no fundamental change in patients’ clinical status. This may be attributable to, for example, increasing awareness of the diagnosis and incentives to alter coding practices. However, this study was predicated on the assumption that changes in diagnosis codes listed for ED visits truly represent the clinical state of patients, and the Healthcare Cost and Utilization Project data cannot by itself reveal whether or not hypertensive emergencies appear more common because of true changes in disease incidence or because of alterations in coding practice. A prospective study that gathered clinical data for the explicit purpose of defining hypertensive emergency, together with coding data for those same visits, might be able to elucidate how coding practices are evolving over time.
Among the strongest epidemiological studies of hypertensive emergency are 2 recent retrospective analyses using the Nationwide Inpatient Sample,9, 15 a database similar to the NEDS that includes only hospitalized patients. These studies also use ICD‐9 codes but do not include explicit requirement for coding that indicated acute target organ damage or other evidence of acuity. In the more recent analysis, Polgreen et al explored the epidemiology of hypertensive emergencies using the following specific ICD‐9 codes: malignant hypertension (401.0), hypertensive encephalopathy (437.2), and essential hypertension (401.9). In particular, they found that malignant hypertension and hypertensive encephalopathy made up an increasing proportion of hospitalizations associated with any 1 of these 3 diagnoses but that overall mortality actually decreased slightly. Unlike this work, our study required ICD‐9 CM codes to indicate target organ damage. Given existing confusion about the diagnosis, where clinical evidence of acute target organ damage should be the decision point for initiating rapid BP lowering, we feel our approach is more likely to yield a clinically meaningful estimate of the true incidence of hypertensive emergency in the ED.
In addition to implications for the ED, these data also have potential bearing on how patients with markedly elevated BP should be approached in non‐ED settings, suggesting that referral to the ED for fear of a hypertensive emergency may not be necessary in the vast majority of cases. Indeed, 1 retrospective study found that patients with hypertensive urgency treated in an office setting are not any more or less likely to have a major cardiovascular event compared to patients referred to the ED or hospital.25 Even among those actually admitted to the hospital, like those patients we defined as hypertensive emergency in the present analysis, charges for ED visits we characterized as hypertensive emergency have risen in the period from 2006 to 2013. Clarifying the epidemiology of hypertensive emergencies in the ED thus has tangible clinical relevance, especially in the context of significant morbidity and mortality in the United States from hypertension‐sensitive conditions such as heart disease and stroke.26
The present study in combination with previous work described above places the balance of evidence in favor of the view that, in absolute terms, hypertensive emergency is rare among ED visits. Even among ED visits with any diagnosis of hypertension (rather than just acute), hypertensive emergency is uncommon. Despite this, hypertension itself remains a major public health problem, contributing substantially to avoidable morbidity and mortality.13, 14 That we also found patients in the lowest quartile of income to represent the greatest proportion of hypertensive emergency visits is important, mirroring what is known to occur with chronic hypertension. While NEDS does not collect data on chronic hypertension management, these data suggest that long‐term challenges with BP control are an important contributor to acute complications. Indeed, in a series of 100 hypertensive emergency cases, 93% were attributed to stopping prescribed medications or patients’ inability to access sources of health care.27 Inadequate outpatient management has been found to be an independent risk factor for markedly elevated BP in a case–control study of Detroit EDs,28 and this provides 1 potential mechanism that would account for the increased occurrence of hypertensive emergency found among patients with low socioeconomic status. Unfortunately, while these data also show related hospitalizations to be more frequent among blacks,9 the NEDS database used in this study does not contain race or ethnicity data, so we could not evaluate such subgroups in our study sample.
Conclusions
Based on data from a valid, nationwide, representative sample, the estimated number of visits for hypertensive emergency and the rate per million adult ED visits has more than doubled from 2006 to 2013. However, hypertensive emergencies are rare, occurring in about 2 of every 1000 adult ED visits in the United States, and 6 in 1000 adult ED visits carrying any diagnosis of hypertension. This figure is far lower than what has been sometimes cited in previous literature.
Disclosures
None.
Author Contributions
Janke, McNaughton, Brody, and Levy conceived the study. Data analysis was performed by Janke and Welch. Janke and Levy drafted the manuscript, and all authors contributed substantially to its revision. Janke takes responsibility for the paper as a whole.
(J Am Heart Assoc. 2016;5:e004511 doi: 10.1161/JAHA.116.004511)
This work was presented at the American College of Emergency Physicians Scientific Assembly Research Forum, October 26–27, 2015, in Boston, MA.
References
- 1. Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000;118:214–227. [DOI] [PubMed] [Google Scholar]
- 2. Decker WW, Godwin SA, Hess EP, Lenamond CC, Jagoda AS. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006;47:237–249. [DOI] [PubMed] [Google Scholar]
- 3. Shayne PH, Pitts SR. Severely increased blood pressure in the emergency department. Ann Emerg Med. 2003;41:513–529. [DOI] [PubMed] [Google Scholar]
- 4. Elliott WJ. Clinical features and management of selected hypertensive emergencies. J Clin Hypertens (Greenwich). 2004;6:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ault MJ, Ellrodt AG. Pathophysiological events leading to the end‐organ effects of acute hypertension. Am J Emerg Med. 1985;3:10–15. [DOI] [PubMed] [Google Scholar]
- 6. Phillips RA, Greenblatt J, Krakoff LR. Hypertensive emergencies. Prog Cardiovasc Dis. 2002;45:33–48. [DOI] [PubMed] [Google Scholar]
- 7. Katz JN, Gore JM, Amin A. Practice patterns, outcomes, and end‐organ dysfunction for patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) Registry. Am Heart J. 2009;158:599–606. [DOI] [PubMed] [Google Scholar]
- 8. Felmeden DC, Beevers DG, Yip GYH. Tackling malignant hypertension: not so desperate now [letter]. Am Heart J. 2002;144:E4. [DOI] [PubMed] [Google Scholar]
- 9. Chobanian A, Bakris G, Black H, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ; National High Blood Pressure Education Program Coordinating Committee . The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 10. Deshmukh A, Kumar G, Kumar N, Nanchal R, Gobal F, Sakhuja A, Mehta JL. Effect of Joint National Committee VII report on hospitalizations for hypertensive emergencies in the United States. Am J Cardiol. 2011;108:1277–1282. [DOI] [PubMed] [Google Scholar]
- 11. Martin JF, Higashiama E, Garcia E, Luizon RL, Cipullo JP. Hypertensive crisis profile: prevalence and clinical presentation. Arq Bras Cardiol. 2004;83:131–136. [DOI] [PubMed] [Google Scholar]
- 12. Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am. 2015;33:539–551. [DOI] [PubMed] [Google Scholar]
- 13. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NT, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Executive summary: Heart Disease and Stroke Statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399. [DOI] [PubMed] [Google Scholar]
- 14. CDC . Vital signs: prevalence, treatment, and control of hypertension‐United States, 1992–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:103–108. [PubMed] [Google Scholar]
- 15. Polgreen LA, Suneja M, Tang F, Carter BL, Polgreen PM. Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension. 2015;65:1002–1007. [DOI] [PubMed] [Google Scholar]
- 16. McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy PD. Incidence of hypertension‐related emergency department visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116:1717–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Agency for Healthcare Quality and Research . Overview of the National Emergency Department Sample (NEDS). Available at: http://www.hcup-us.ahrq.gov/nedsoverview.jsp. Accessed July 6, 2015.
- 18. Hirshon JM, Warner M, Irvin CB, Niska RW, Andersen DA, Smith GS, McCaig LF. Research using emergency department‐related data sets: current status and future directions. Acad Emerg Med. 2009;16:1103–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007;386:1–32. [PubMed] [Google Scholar]
- 20. Heath I . Hypertensive urgency—is this a useful diagnosis? JAMA Intern Med. 2016;176:988–989. [DOI] [PubMed] [Google Scholar]
- 21. Niska RW. Blood pressure measurements at emergency department visits by adults: United States, 2007–2008. NCHS Data Brief. 2011;72:1–8. [PubMed] [Google Scholar]
- 22. Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report. 2010;26:1–31. [PubMed] [Google Scholar]
- 23. Adhikari S, Mathiasen R. Epidemiology of elevated blood pressure in the ED. Am J Emerg Med. 2014;32:1370–1372. [DOI] [PubMed] [Google Scholar]
- 24. Vidt DG. Emergency room management of hypertensive urgencies and emergencies. J Clin Hypertens (Greenwich). 2001;3:158–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Patel KK, Young L, Howell EH, Hu B, Rutecki G, Thomas G, Rothberg MB. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016;176:981–988. [DOI] [PubMed] [Google Scholar]
- 26. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Executive summary: Heart Disease and Stroke Statistics—2016 update, a report from the American Heart Association. Circulation. 2016;133:447–454. [DOI] [PubMed] [Google Scholar]
- 27. Bennett SM, Shea S. Hypertensive emergency: case criteria, sociodemographic profile, and previous care of 100 cases. Am J Public Health. 1988;78:636–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brown AD, Goldacre MJ, Hicks N, Rourke JT, McMurry RY, Brown JD, Anderson GM. Hospitalization for ambulatory care‐sensitive conditions: a method for comparative access and quality studies using routinely collected statistics. Can J Public Health. 2001;92:155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]


