Abstract
Background
A patent foramen ovale (PFO) with atrial septal aneurysm (ASA) has been identified as a risk factor for cryptogenic stroke. Patients with migraine with aura (MA) appear to be at risk for silent brain infarction, which might be related to the presence of a PFO. However, the association between MA and PFO with ASA has never been reported. We examined this association in a large observational study.
Methods and Results
Patients (>18 years) who underwent an agitated saline transesophageal echocardiography (cTEE) at our outpatient clinics within a timeframe of 4 years were eligible to be included. Before cTEE they received a validated headache questionnaire. Two neurologists diagnosed migraine with or without aura according to the International Headache Criteria. A total of 889 patients (mean age 56.4±14.3 years, 41.7% women) were included. A PFO was present in 23.2%, an isolated ASA in 2.7%, and a PFO with ASA in 6.9%. The occurrence of migraine was 18.9%; the occurrence of MA was 8.1%. The prevalence of PFO with ASA was significantly higher in patients with MA compared to patients without migraine (18.1% vs 6.1%; OR 3.72, 95% CI 1.86‐7.44, P<0.001). However, a PFO without ASA was not significantly associated with MA (OR 1.50, 95% CI 0.79‐2.82, P=0.21). Interestingly, a PFO with ASA was strongly associated with MA (OR 2.71, 95% CI 1.23‐5.95, P=0.01).
Conclusion
In this large observational study, PFO with ASA was significantly associated with MA only. PFO closure studies should focus on this specific intra‐atrial anomaly.
Keywords: atrial septal aneurysm, cerebrovascular disorders, echocardiography, heart septal defect, migraine, patent foramen ovale
Subject Categories: Cerebrovascular Disease/Stroke, Congenital Heart Disease
Introduction
Migraine is a common neurological disorder and has been acknowledged as 1 of the most important causes of disability burden.1 The prevalence of migraine in the population is 18.5%, and for migraine with aura (MA) 4.4%.2 The peak prevalence for women is reached in the third decade of life and thereafter declines with age, whereas the prevalence for men is virtually flat.3 Migraine seems to be a complex disorder in which both genetic and environmental factors play an important role.4
The patent foramen ovale (PFO) is a slitlike interatrial opening that is present in about 27% of the general population.5 It is 1 of the major causes of a cardiac right‐to‐left shunt (RLS). An atrial septal aneurysm (ASA) is a congenital bulging of the atrial septum involving the fossa ovalis region. An ASA has been found in 1% to 2.5% of the general population in large autopsy studies and population‐based studies using echocardiography.5, 6
The presence of PFO and ASA has been associated with cryptogenic stroke.7, 8 Patients with migraine with aura (MA) appear to be at risk for stroke,9, 10 which might be related to the presence of a PFO. However, the association between MA and PFO with ASA has never been reported.4
We investigated the association of the presence of PFO with ASA with the occurrence of MA in patients who underwent an agitated saline transesophageal echocardiography (cTEE) at our outpatient clinics.
Methods
Study Design and Population
All consecutive patients (>18 years) who underwent a cTEE at the outpatient departments of the University Hospital Gasthuisberg, Leuven, Belgium and the St. Antonius Hospital, Nieuwegein, the Netherlands within a timeframe of 4 years were eligible to be included in the study. All patients received a Dutch headache questionnaire for the diagnosis of migraine. The following patients were excluded: patients who did not undergo an agitated saline examination, patients who did not complete the headache questionnaire, and patients with an atrial septal defect (ASD). The patients' medical history was retrieved from the medical records. Informed consent was obtained from all patients, and the ethical committees of the participating centers approved the study.
Transesophageal Echocardiography
An ultrasonography system with a 5‐MHz transducer was used for transesophageal echocardiography (TEE) examinations. The agitated saline examination was performed by injection of a bolus of agitated saline solution into a peripheral vein with and without a provocative maneuver during TEE. A RLS through a PFO was diagnosed when microbubbles were detected in the left atrium within 4 cycles after right atrial opacification with or without a provocative maneuver. The provocative maneuver was performed by asking the patient to stop breathing, close his or her mouth and nose, and strain. After the right atrium was filled with agitated saline, the patient was asked to release the strain. The shunt size was measured as previously published and graded as none, minimal, moderate, or large, based on the maximal amount of bubbles measured on a still frame.11 An atrial septal aneurysm (ASA) was defined as a bulging of the atrial septum of at least 10 mm beyond the plane of the atrial septum into either the right or left atrium. Experienced independent physicians who were unaware of the presence of migraine performed and reviewed the echocardiographic examinations.
Diagnosis of Migraine
As described previously,12 a structured headache questionnaire was composed in such a way that a neurologist could diagnose MA and migraine without aura (MA−), according to the criteria of the International Headache Society.13 All patients received the Dutch questionnaire before undergoing cTEE. Two independent neurologists who were blinded to the patients' files and cTEE results diagnosed MA and MA−. When there was not a perfect agreement, both neurologists discussed the case to reach consensus.
In addition, in patients with MA, headache characteristics were analyzed by means of the headache questionnaire. First, the duration of headache was recorded. Second, headache severity was measured on a scale ranging from 0 (no pain) to 10 (very severe pain). Third, the frequency of headache attacks was noted.
Statistical Analysis
Descriptive statistics were used to describe patient characteristics. Continuous variables were tested on normality and presented as mean±standard deviation. Median and first and third quartiles (IQ1 and IQ3) were used when normal distribution was absent. Percentages were used to report categorical variables. Univariate and multivariate logistic‐regression analyses were used to estimate the unadjusted and adjusted odds ratios (OR) and the corresponding 95% confidence intervals (CI). In the multivariate analyses, the most significant clinically relevant univariate variables were included. Kruskal‐Wallis tests were performed to analyze any association between headache characteristics and the atrial septal anatomic variables in patients with MA. Interobserver reliability for the diagnosis of migraine was evaluated by calculating the κ coefficient. The Mann‐Whitney test was performed to analyze any association between having a PFO with ASA and the degree of right‐to‐left shunting.
All tests were 2‐sided, and P<0.05 was considered to be statistically significant. All statistical analyses were performed using SPSS software (SPSS Inc, version 22.0 for Windows, IBM Corp, Armonk, NY).
Results
Patient Characteristics
Within the time frame, 2349 patients underwent a TEE at the outpatient departments of the participating centers. Patients who did not fully complete the headache questionnaire or did not understand the Dutch questionnaire (1190), patients who did not undergo an agitated saline examination (213), and patients with an ASD (57) were excluded. In total 889 (38%) patients (mean age 56.4±14.3 years, 41.7% women) were included in the present study. A flowchart of the patient inclusion is depicted in Figure. The patient characteristics are summarized in Table 1.
Figure 1.
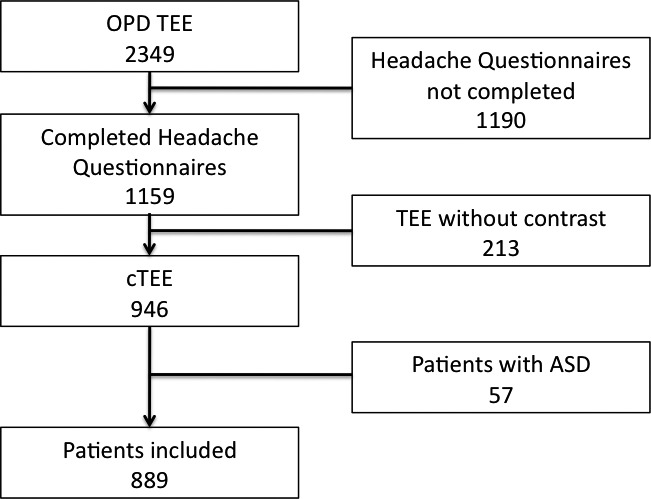
Flowchart of patient inclusion. ASD indicates atrial septal defect; cTEE, transesophageal echocardiography with agitated saline; OPD, outpatient department; TEE, transesophageal echocardiography.
Table 1.
Patient Characteristics, Interatrial Septal Anatomy and Occurrence of Migraine (MA and MA−)
| Patient Population (n=889) | |
|---|---|
| Patient characteristics | |
| Age (y) ±SD | 56.4±14.3 |
| Women, n (%) | 371 (41.7) |
| Mean BMI (kg/m2) ±SD | 26.2±4.5 |
| History | |
| Stroke or TIA, % | 34.7 |
| CAD, % | 14.2 |
| Diabetes mellitus, % | 7.5 |
| Hypertension, % | 34.0 |
| Hypercholesterolemia, % | 34.3 |
| Smoking, % | 31.4 |
| Atrial fibrillation, % | 32.8 |
| Medication | |
| Aspirin, % | 32.8 |
| Warfarin, % | 31.6 |
| β‐Blocker, % | 42.0 |
| Indication for TEE | |
| Suspicion of endocarditis, % | 3.1 |
| Evaluation of valve abnormalities/prosthesis, % | 18.9 |
| Evaluation of cardioembolic source, % | 45.1 |
| Evaluation of atrial thrombi pre‐PVI/ECV, % | 20.2 |
| PFO on cTTE, % | 8.5 |
| Other, % | 4.2 |
| Interatrial septal anatomy | |
| No PFO, no ASA, n (%) | 659 (74.1) |
| Isolated PFO, n (%) | 145 (16.3) |
| Isolated ASA, n (%) | 24 (2.7) |
| PFO with ASA, n (%) | 61 (6.9) |
| Migraine | |
| Migraine, n (%) | 168 (18.9) |
| Migraine without aura, n (%) | 96 (10.8) |
| Migraine with aura, n (%) | 72 (8.1) |
ASA indicates atrial septal aneurysm; BMI, body mass index; CAD, coronary artery disease; cTTE, agitated saline transthoracic echocardiography; ECV, electrical cardioversion; n, number; PFO, patent foramen ovale; PVI, pulmonary vein isolation; SD, standard deviation; TEE, transesophageal echocardiography; TIA, transient ischemic attack.
A PFO was found in 23.2% of the cases; the prevalence of an isolated ASA was 2.7%. The prevalence of other atrial septal abnormalities and the occurrence of migraine are shown in Table 1. The κ coefficient for interobserver reliability for the diagnosis of migraine was 0.77 (P<0.001).
Migraine With Aura
In univariate analysis the presence of PFO with ASA, compared to the absence of an atrial septal anomaly, was associated with MA (OR 3.72, 95% CI 1.86‐7.44, P<0.001). A PFO without ASA was not significantly associated with MA (OR 1.50, 95% CI 0.79‐2.82, P=0.21), nor was an isolated ASA (OR 1.48, 95% CI 0.33‐6.63, P=0.61) (Table 2).
Table 2.
Factors Associated With MA and MA−, Univariate Analysis
| No Migraine | MA | MA− | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
|---|---|---|---|---|---|---|---|---|---|
| Patient characteristics | MA vs no migraine | MA− vs no migraine | MA vs MA− | ||||||
| Total | 721 | 72 | 96 | — | — | — | — | ||
| Age (y) ±SD | 58.5±13.6 | 44.4±14.1 | 49.6±13.2 | 0.93 (0.92‐0.95) | <0.001 | 0.96 (0.94‐0.97) | <0.001 | 0.97 (0.95‐1.00) | 0.02 |
| Women, n (%) | 269 (37.3) | 48 (66.7) | 54 (56.3) | 3.36 (2.01‐5.61) | <0.001 | 2.16 (1.41‐3.32) | <0.001 | 1.56 (0.83‐2.93) | 0.17 |
| BMI (kg/m2) ±SD | 26.4±4.2 | 26.7±6.7 | 24.7±4.3 | 1.02 (0.94‐1.10) | 0.71 | 0.90 (0.82‐0.97) | 0.01 | 1.07 (0.98‐1.17) | 0.12 |
| History | |||||||||
| Stroke or TIA, % | 33.8 | 40.3 | 37.2 | 1.32 (0.79‐2.21) | 0.87 | 1.16 (0.73‐1.85) | 0.53 | 1.14 (0.59‐2.19) | 0.70 |
| CAD, % | 16.1 | 3.0 | 8.2 | 0.16 (0.04‐0.67) | 0.01 | 0.47 (0.21‐1.04) | 0.06 | 0.34 (0.07‐1.71) | 0.19 |
| Diabetes mellitus, % | 7.7 | 4.5 | 8.1 | 0.56 (0.17‐1.85) | 0.34 | 1.06 (0.47‐2.42) | 0.88 | 0.53 (0.13‐2.13) | 0.37 |
| Hypertension, % | 37.3 | 16.4 | 22.1 | 0.33 (0.17‐0.64) | 0.01 | 0.48 (0.28‐0.81) | 0.006 | 0.69 (0.30‐1.58) | 0.42 |
| Hypercholesterolemia, % | 37.0 | 19.4 | 25.6 | 0.41 (0.22‐0.77) | 0.005 | 0.59 (0.35‐0.98) | 0.04 | 0.70 (0.32‐1.52) | 0.44 |
| Smoking, % | 29.6 | 29.4 | 42.6 | 0.99 (0.45‐2.18) | 0.98 | 1.76 (0.93‐3.34) | 0.08 | 0.56 (0.22‐1.44) | 0.25 |
| AF, % | 37.2 | 13.4 | 14.0 | 0.26 (0.13‐0.54) | <0.001 | 0.27 (0.15‐0.51) | <0.001 | 0.96 (0.38‐2.43) | 1.00 |
| Medication | |||||||||
| Aspirin, % | 32.9 | 38.1 | 28.6 | 1.26 (0.74‐2.14) | 0.40 | 0.82 (0.50‐1.35) | 0.43 | 1.54 (0.77‐3.08) | 0.29 |
| Warfarin, % | 34.7 | 10.9 | 22.6 | 0.23 (0.10‐0.51) | <0.001 | 0.55 (0.32‐0.94) | 0.03 | 0.42 (0.17‐1.07) | 0.08 |
| β‐Blocker, % | 44.3 | 35.9 | 28.6 | 0.71 (0.41‐1.20) | 0.20 | 0.50 (0.31‐0.83) | 0.007 | 1.40 (0.70‐2.81) | 0.38 |
| Interatrial septal anatomy | |||||||||
| No PFO, no ASA, n (%) | 542 (75.2) | 43 (59.7) | 74 (77.1) | Reference | — | Reference | — | Reference | — |
| Isolated PFO, n (%) | 118 (16.4) | 14 (19.4) | 13 (13.5) | 1.50 (0.79‐2.82) | 0.21 | 0.81 (0.43‐1.50) | 0.50 | 1.85 (0.80‐4.31) | 0.15 |
| Isolated ASA, n (%) | 17 (2.4) | 2 (2.8) | 5 (5.2) | 1.48 (0.33‐6.63) | 0.61 | 2.15 (0.77‐6.01) | 0.14 | 0.69 (0.13‐3.70) | 0.66 |
| PFO with ASA, n (%) | 44 (6.1) | 13 (18.1) | 4 (4.2) | 3.72 (1.86‐7.44) | <0.001 | 0.67 (0.23‐1.91) | 0.45 | 5.59 (1.72‐18.2) | 0.004 |
AF indicates atrial fibrillation; ASA, atrial septal aneurysm; BMI, body mass index; CAD, coronary artery disease; CI, confidence interval; MA, migraine with aura; MA−, migraine without aura; n, number; OR, odds ratio; PFO, patent foramen ovale; SD, standard deviation; TIA, transient ischemic attack.
Additionally, in univariate analysis, female sex and a younger age were found to be associated with MA (Table 2). Although atrial fibrillation and hypercholesterolemia were significant in univariate analysis as well, both are not clinical relevant for migraine with aura and were therefore left out multivariate analysis. In an adjusted multivariable model PFO with ASA appeared to be most strongly associated with MA (OR 2.71, 95% CI 1.23‐5.95, P=0.01). Aside from the combination of PFO and ASA, both female sex (OR 2.44, 95% CI 1.37‐4.34, P=0.002) and age (OR 0.94, 95% CI 0.92‐0.96, P<0.001) were independently associated with MA. There were no missing values in the multivariate analysis.
Migraine Without Aura
Between patients with MA− and patients without migraine, no significant difference was found between the presence of an isolated PFO (13.5% vs 16.4%, P=0.50), isolated ASA (5.2% vs 2.4%, P=0.14) or PFO with ASA (4.2% vs 6.1%, P=0.45) (Table 2).
Additionally, in univariate analysis, female sex, a younger age, and using a β‐blocker were found to be associated with MA−. Importantly, atrial septal anatomy was not associated with MA−. Although atrial fibrillation was significant in univariate analysis as well, it is not clinically relevant for migraine and was therefore left out of the multivariate analysis. In an adjusted multivariable model, female sex (OR 1.83, 95% CI 1.13‐2.97, P=0.01) and age (OR 0.97, 95% CI 0.95‐0.99, P<0.001) were independently associated with MA−. There were 74 missing values in multivariate analysis (9.1%).
Factors Associated With Migraine With and Without Aura by Interatrial Septal Anatomy
Between patients with MA and MA−, having a PFO with ASA was associated with MA (18.1% vs 4.2%, P=0.004). No significant difference was found between MA and MA− and isolated PFO (19.4% vs 13.5%, P=0.15) and isolated ASA (2.8% vs 5.2%, P=0.66).
Additionally, in univariate analysis, younger age was also associated with MA (Table 2). In an adjusted multivariable model, having a PFO with ASA was the only factor associated with MA (OR 4.34, 95% CI 1.10‐17.1, P=0.04).
Coumadin
A subgroup analysis was performed excluding all patients using coumadin or with a history of atrial fibrillation. A total of 527 patients (59.3%) were included in this subgroup analysis. Only a PFO with ASA was more often found in patients suffering MA compared to MA− (18.2% vs 5.5%, P=0.02). No significant difference was found in the presence of an isolated PFO (20.0% vs 15.1%, P=0.27) or isolated ASA (3.3% vs 5.5%, P=0.77).
PFO Size
Moderate and severe shunt rates were found in 12.0% and 12.0% for MA and 5.7% and 0% for MA−, respectively (P=0.007). The shunt rate differs significantly between MA and patients without migraine (P=0.03). A significantly higher shunt rate was found in patients with a PFO with ASA when compared to patients with an isolated PFO (P=0.015) (Table 3).
Table 3.
PFO Grade in Patients With M−, MA− and MA
| Grade 0, % | Grade 1, % | Grade 2, % | Grade 3, % | |
|---|---|---|---|---|
| M− | 80.6 | 6.8 | 7.0 | 5.6 |
| MA− | 88.6 | 5.7 | 5.7 | 0.0 |
| MA | 60.0 | 16.0 | 12.0 | 12.0 |
| Isolated PFO | — | 44.4 | 35.2 | 20.4 |
| PFO with ASA | — | 20.7 | 37.9 | 41.4 |
PFO grade, maximum number of microbubbles counted in the left ventricle in 1 still frame: grade 0 (no microbubbles), grade 1 (1‐29 microbubbles), grade 2 (30‐100 microbubbles), and grade 3 (>100 microbubbles). ASA indicates atrial septal aneurysm; M−, no migraine; MA, migraine with aura; MA−, migraine without aura; PFO, patent foramen ovale.
Headache Characteristics
The headache characteristics (duration, severity, and frequency of headache attacks) of all patients with MA (n=72) in relation to the interatrial septal anatomy are summarized in Table 4. In this grou, we found no correlation between the MA characteristics and the anatomical variables.
Table 4.
Characteristics of Headache Attacks in Relation to Interatrial Septal Anatomy in Patients With MA (n=72)
| No PFO, No ASA n=43 | Isolated PFO n=14 | Isolated ASA n=2 | PFO With ASA n=13 | P Value | |
|---|---|---|---|---|---|
| Median duration, h (IQ1‐IQ3) | 4 (1‐24) | 1.5 (0.8‐4) | 36 (0.25‐72) | 24 (1.4‐24) | 0.51 |
| Median severity score, scale 0 to 10 (IQ1‐IQ3) | 7 (5‐8) | 7.5 (6‐8) | 6.5 (5‐8) | 7 (6‐8) | 0.62 |
| Frequency of migraine, n of patients | 0.37 | ||||
| ≥Once a month | 21 | 9 | 0 | 7 | |
| ≥Once a week | 22 | 5 | 2 | 6 |
Kruskal‐Wallis tests were performed to compare headache characteristics between groups. ASA indicates atrial septal aneurysm; IQ, interquartile; MA, migraine with aura; n, number; PFO, patent foramen ovale.
Discussion
To our knowledge this is the first observational study reporting a strong association between the presence of a PFO with ASA and the occurrence of MA in a large patient population referred for TEE.
Association between PFO and MA, the Role of ASA
Current literature remains discordant as to whether a linkage exists between PFO and MA. In many observational studie, an association between PFO and the occurrence of MA has been found.14 However, other studies found no association between migraine with or without aura and the presence of a PFO.15, 16, 17
The discordant findings between the positive and negative studies might be explained in different ways. First, in the observational studies most patients suffered a symptomatic PFO, which means a history of a cryptogenic cerebral ischemic event. In the negative studies patients with these “high‐risk” PFO's were excluded, which could have influenced the findings. Second, 1 of the factors that was most strongly associated with the occurrence of a cryptogenic cerebral event is the presence of a combination of a PFO with an ASA.8 Patients with MA appear to be at risk for stroke, which might be related to the presence of a PFO.9, 10 We therefore hypothesized that the link between the association of PFO and MA might be the ASA. The negative studies did not identify this specific anomaly, which might have influenced their observational results. Indeed, the presence of a PFO and/or ASA can only be clearly demonstrated by TEE and not by transthoracic echocardiography (TTE) or transcranial Doppler (TCD) as used in the negative studies.18
More recently, 2 prospective trials were published. The MIST trial compared percutaneous PFO closure and a sham procedure in 147 patients. No improvement of migraine was found after closure. The PRIMA trial compared percutaneous PFO closure and pharmacological treatment in 107 patients and did show a lower frequency of MA in the percutaneous closure group. The difference in outcome between these trials was probably due to the patient selection and follow‐up time.19, 20
Interestingly, in the current study we found no significant association between PFO without ASA, diagnosed by TEE, and MA. This is comparable with the negative studies. However, PFO with ASA was independently strongly associated with MA (OR 2.7).
Moreover, we found only an association between the presence of PFO with ASA and the occurrence of MA. No association was found with MA−. Second, the shunt size was significantly higher in patients suffering MA.
Pathophysiological Mechanism
The exact pathophysiology for MA is still unknown. A plausible explanation for the association between PFO and MA seems to be the “microthrombi hypothesis.” This hypothesis suggests that, in the presence of PFO, microthrombi or emboli originating in the venous circulation might enter the systemic and cerebral circulation and trigger a migraine attack. By shunting from right to left through the PFO, these microthrombi might bypass the lung filter.21 In situ microthrombus formation secondary to stasis of blood in the PFO tunnel might be another source of migraine‐triggering substances. Another study supporting the microthrombi hypothesis is the study by Mohanty et al describing the positive effect of AF ablation on migraine symptoms. Further, they reported that cases with new migraine had a subtherapeutic INR, which supports the theory that microthrombi could be associated with migraine.22 After exclusion of patients using coumadin or with a history of atrial fibrillation, the presence of a PFO with ASA was still associated with MA in our study.
Bhaskar et al conclude that cortical spreading depression is the physiological substrate of MA and probably also of MA−.23 Because the exact pathophysiology is not clear, the microthrombi hypothesis is still one of the many hypotheses for the cause of MA. Although no studies actually prove the microthrombi hypothesis, several case reports have been published showing benefit of warfarin in patients suffering MA.24, 25 As mentioned before, we did not find a significant association between PFO without ASA and MA in our study. A possible explanation is our finding that PFOs with an ASA have a higher degree of right‐to‐left shunting, which supports our finding that only the presence of PFO with ASA was significantly associated with the occurrence of MA.
In support of this theory and to clarify it, we believe there might be a parallel between the pathophysiology of the association of PFO with ASA and MA on 1 hand and of PFO with ASA and cryptogenic stroke on the other. Paradoxical embolism of thrombus through a PFO may be the most likely pathophysiologic mechanism in young patients with cryptogenic stroke.26 Moreover, a stronger association with cryptogenic stroke has been reported for PFO with ASA as compared to PFO alone.8 Additionally, it has been observed that in cryptogenic stroke patients, the risk of recurrent stroke increased significantly in patients with PFO and ASA when compared to patients with only a PFO or ASA.27 The observation that MA patients have a higher lifetime risk for an ischemic cerebral event compared to the general population supports the parallel even more.9
In support of the microthrombi hypothesis is the finding that treatment with high‐dose aspirin or oral anticoagulants might prevent migraine attacks.24, 28 We also found a protective effect of coumadin on the occurrence of MA in univariate analysis. However, there was no significant difference in coumadin use between the MA and MA− groups (P=0.08), probably based on the small sample size. But both groups were underpowered and different, which makes it difficult to draw any conclusions.
A relatively high prevalence of CAD, hypertension, hypercholestrolemia, and AF was found. The reason is probably that there are more men of higher age in this population. We also found that there is less migraine in patients with higher age as well as a lower frequency of PFO. These findings are in line with earlier studies.3, 29, 30
Limitations
The first limitation of our study is selection bias. All patients were referred to the cardiologic outpatient department to undergo cTEEs for different indications, including referral for ruling out a cardioembolic source. This might have influenced the prevalence of PFO and ASA. However, we found prevalences of PFO and isolated ASA, respectively, of 23% and 2.7%, which are comparable with those in the general population.5, 6 Second, this study was limited because of a relatively high rate of exclusion of patients, partially because they did not undergo an agitated saline examination. When patients experienced too much discomfort during TEE, we decided to abandon the agitated saline examination. However, this is inherent to the semi‐invasive character of TEE. A larger group was excluded because they did not fully complete the survey or master the Dutch language. This could cause a bias also because it is not clear whether only patients with a history of headache agreed to participate. Earlier TTE or TEE data of these patients were not available. Therefore, comparing the patients who did not undergo TEE to those who did was not possible.
Conclusion
Only a PFO with ASA is significantly associated with MA in this large observational study. Further PFO studies should focus on this specific intra‐atrial anomaly.
Disclosures
None.
(J Am Heart Assoc. 2016;5:e003771 doi: 10.1161/JAHA.116.003771)
References
- 1. Silberstein SD. Migraine. Lancet. 2004;363:381–391. [DOI] [PubMed] [Google Scholar]
- 2. Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53:230–246. [DOI] [PubMed] [Google Scholar]
- 3. Pressman A, Jacobson A, Eguilos R, Gelfand A, Huynh C, Hamilton L, Avins A, Bakshi N, Merikangas K. Prevalence of migraine in a diverse community—electronic methods for migraine ascertainment in a large integrated health plan. Cephalalgia. 2016;36:325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lip PZ, Lip GY. Patent foramen ovale and migraine attacks: a systematic review. Am J Med. 2014;127:411–420. [DOI] [PubMed] [Google Scholar]
- 5. Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20. [DOI] [PubMed] [Google Scholar]
- 6. Di Tullio MR, Sacco RL, Sciacca RR, Jin Z, Homma S. Patent foramen ovale and the risk of ischemic stroke in a multiethnic population. J Am Coll Cardiol. 2007;49:797–802. [DOI] [PubMed] [Google Scholar]
- 7. Handke M, Harloff A, Olschewski M, Hetzel A, Geibel A. Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med. 2007;357:2262–2268. [DOI] [PubMed] [Google Scholar]
- 8. Overell JR, Bone I, Lees KR. Interatrial septal abnormalities and stroke: a meta‐analysis of case‐control studies. Neurology. 2000;55:1172–1179. [DOI] [PubMed] [Google Scholar]
- 9. Etminan M, Takkouche B, Isorna FC, Samil A. Risk of ischaemic stroke in people with migraine: systematic review and meta‐analysis of observational studies. BMJ. 2005;330:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kruit MC, van Buchem MA, Hofman PA, Bakkers JT, Terwindt GM, Ferrari MD, Launer LJ. Migraine as a risk factor for subclinical brain lesions. JAMA. 2004;291:427–434. [DOI] [PubMed] [Google Scholar]
- 11. Velthuis S, Buscarini E, Gossage JR, Snijder RJ, Mager JJ, Post MC. Clinical implications of pulmonary shunting on saline contrast echocardiography. J Am Soc Echocardiogr. 2015;28:255–263. [DOI] [PubMed] [Google Scholar]
- 12. Mortelmans K, Post M, Thijs V, Herroelen L, Budts W. The influence of percutaneous atrial septal defect closure on the occurrence of migraine. Eur Heart J. 2005;26:1533–1537. [DOI] [PubMed] [Google Scholar]
- 13. Headache Classification Committee of the International Headache Society (IHS) . The International Classification of Headache Disorders: 3rd edition. Cephalalgia. 2013;33:629–808. [DOI] [PubMed] [Google Scholar]
- 14. Post MC, Luermans JG, Plokker HW, Budts W. Patent foramen ovale and migraine. Catheter Cardiovasc Interv. 2007;69:9–14. [DOI] [PubMed] [Google Scholar]
- 15. Rundek T, Elkind MS, Di Tullio MR, Carrera E, Jin Z, Sacco RL, Homma S. Patent foramen ovale and migraine: a cross‐sectional study from the Northern Manhattan Study (NOMAS). Circulation. 2008;118:1419–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garg P, Servoss SJ, Wu JC, Bajwa ZH, Selim MH, Dineen A, Kuntz RE, Cook EF, Mauri L. Lack of association between migraine headache and patent foramen ovale: results of a case‐control study. Circulation. 2010;121:1406–1412. [DOI] [PubMed] [Google Scholar]
- 17. Chambers J, Seed PT, Ridsdale L. Association of migraine aura with patent foramen ovale and atrial aneurysms. Int J Cardiol. 2013;168:3949–3953. [DOI] [PubMed] [Google Scholar]
- 18. Soliman OI, Geleijnse ML, Meijboom FJ, Nemes A, Kamp O, Nihoyannopoulos P, Masani N, Feinstein SB, Ten Cate FJ. The use of contrast echocardiography for the detection of cardiac shunts. Eur J Echocardiogr. 2007;8:S2–S12. [DOI] [PubMed] [Google Scholar]
- 19. Dowson A, Mullen MJ, Peatfield R, Muir K, Khan AA, Wells C, Lipscombe SL, Rees T, De Giovanni JV, Morrison WL, Hildick‐Smith D, Elrington G, Hillis WS, Malik IS, Rickards A. Migraine Intervention with STARFlex Technology (MIST) trial: a prospective, multicenter, double‐blind, sham‐controlled trial to evaluate the effectiveness of patent foramen ovale closure with STARFlex septal repair implant to resolve refractory migraine headache. Circulation. 2008;117:1397–1404. [DOI] [PubMed] [Google Scholar]
- 20. Hildick‐Smith D. Percutaneous closure of patent foramen ovale in migraine with aura (PRIMA). Presented at Transcatheter Cardiovascular Therapeutics September 16, 2014, Washington, DC; 2014. [Google Scholar]
- 21. Wilmshurst P, Nightingale S. Relationship between migraine and cardiac and pulmonary right‐to‐left shunts. Clin Sci (Lond). 2001;100:215–220. [PubMed] [Google Scholar]
- 22. Mohanty S, Mohanty P, Rutledge JN, Di Biase L, Xue Yan R, Trivedi C, Santangeli P, Bai R, Cardinal D, Burkhardt JD, Gallinghouse JG, Horton R, Sanchez JE, Bailey S, Hranitzky PM, Zagrodzky J, Al‐Ahmad A, Natale A. Effect of catheter ablation and periprocedural anticoagulation regimen on the clinical course of migraine in atrial fibrillation patients with or without pre‐existent migraine. Results from a prospective study. Circ Arrhythm Electrophysiol. 2015;8:279–287. [DOI] [PubMed] [Google Scholar]
- 23. Bhaskar S, Saeidi K, Borhani P, Amin H. Recent progress in migraine pathophysiology: role of cortical spreading depression and magnetic resonance imaging. Eur J Neurosci. 2013;38:3540–3551. [DOI] [PubMed] [Google Scholar]
- 24. Maggioni F, Bruno M, Mainardi F, Lisotto C, Zanchin G. Migraine responsive to warfarin: an update on anticoagulant possible role in migraine prophylaxis. Neurol Sci. 2012;33:1447–1449. [DOI] [PubMed] [Google Scholar]
- 25. Russo A, Santi S, Gueraldi D, De Paola M, Zani F, Pini LA. An unusual case report on the possible role of warfarin in migraine prophylaxis. Springerplus. 2013;2:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Caes FL, Van Belleghem YV, Missault LH, Coenye KE, Van Nooten GJ. Surgical treatment of impending paradoxical embolism through patent foramen ovale. Ann Thorac Surg. 1995;59:1559–1561. [DOI] [PubMed] [Google Scholar]
- 27. Mas J, Arquizan C, Lamy C, Zuber M. Recurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm, or both. N Engl J Med. 2001;345:1740–1746. [DOI] [PubMed] [Google Scholar]
- 28. Lipton RB, Goldstein J, Baggish JS, Yataco AR, Quiring JN. Aspirin is efficacious for the treatment of acute migraine. Headache. 2005;45:283–292. [DOI] [PubMed] [Google Scholar]
- 29. Seiler C. Patent foramen ovale: is there life before death in the presence of PFO. Eur J Clin Invest. 2015;45:875–882. [DOI] [PubMed] [Google Scholar]
- 30. Consoli D, Paciaroni M, Galati F, Aguggia M, Melis M, Malferrari G, Consoli A, Vidale S, Bosco D, Cerrato P, Sacco S, Gandolfo C, Bovi P, Serrati C, Del Sette M, Cavallini A, Diomedi M, Postorino P, Reboldi P, Ricci S; behalf of SISIFO group . Prevalence of patent foramen ovale in ischaemic stroke in Italy: results of SISIFO study. Cerebrovasc Dis. 2015;39:162–169. [DOI] [PubMed] [Google Scholar]


