Abstract
Primary gallbladder lymphoma is rare. Perforated cholecystitis due to primary gallbladder lymphoma and not related to chemotherapy has been unreported. We report the case of an 80-year-old woman presenting with an acute abdomen and clinical peritonitis. Her serum amylase was raised to 878iu/l. Urgent computed tomography revealed generalised free fluid with a normal pancreas and was non-diagnostic as to the underlying pathology. An emergency laparotomy revealed bilious peritonitis with a necrotic patch on a distended gallbladder. A cholecystectomy was carried out and histology of the gallbladder revealed a marginal zone lymphoma.
Keywords: Gallbladder, Lymphoma, Perforation
Primary gallbladder lymphoma (PGL) is rare with approximately 50 cases reported in the literature.1 PGL commonly presents as cholecystitis.2 Extranodal marginal zone lymphoma is the common subtype, and it is more common in old age and women.3 We report the case of an 80-year-old female patient presenting with acute abdominal pain and diagnosed with PGL following an emergency cholecystectomy.
Case history
An 80-year-old woman with a past medical history of peptic ulcer disease and recent non-steroidal anti-inflammatory drug (NSAID) use was admitted to hospital with acute onset generalised abdominal pain. On examination, she manifested systemic inflammatory response syndrome with clinical evidence of generalised peritonitis. An erect chest x-ray was normal and serum amylase was raised to 878iu/l (normal range 27–102iu/l) with normal alkaline phosphatase, normal alanine transaminase and slightly raised bilirubin of 25μmol/l (normal range 0–20μmol/l). Urgent computed tomography (CT) showed a normal pancreas, a moderate amount of free fluid and a thickened duodenum with no definite site of wall perforation and no extraluminal gas but a possible contained perforation in the second part of the duodenum (D2). It also showed a distended but thin walled gallbladder with no evidence of gallstones (Fig 1).
Figure 1.
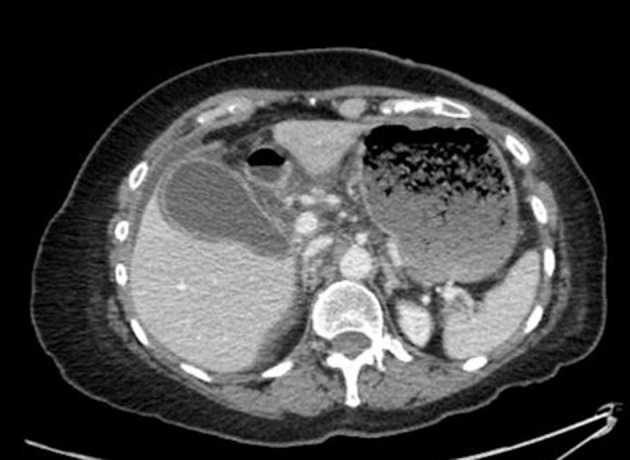
Computed tomography demonstrating a distended gallbladder
Although the serum amylase was raised, given the normal appearance of the pancreas on imaging, the clinical finding of peritonitis and the history of previous peptic ulcer disease together with recent NSAID use, a decision was made to carry out an urgent diagnostic laparoscopy. As the patient became unstable in the anaesthetic room, the surgeon proceeded directly to a laparotomy. Operative findings included generalised biliary peritonitis but no evidence of gastrointestinal perforation or pancreatitis. An on-table intraoperative gastroscopy was normal with no ulcers evident up to D2. The gallbladder was distended with a small necrotic patch at the body suggesting microperforation and accounting for the biliary peritonitis. A cholecystectomy was performed. The patient’s postoperative predicted mortality based on P-POSSUM [Portsmouth Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity] score was 34% but the patient recovered well and was discharged home on postoperative day 14.
Macroscopic pathological examination of the gallbladder revealed two small 5mm black stony fragments. Histology showed a dense transmural infiltrate of small monomorphic appearing lymphocytes. In addition, there was marked acute serositis consistent with perforation (Fig 2). The lymphoid infiltrate did not show an increase in mitotic or apoptotic activity. On immunohistochemistry, the atypical lymphoid cells were positive for CD20 and CD79a, confirming these to be B cells (Fig 3). They also showed lambda light chain restriction. The proliferation fraction as assessed with Ki-67 staining was low. The morphological and immunophenotypic features were those of a low grade B cell lymphoma, in keeping with an extranodal marginal zone lymphoma.
Figure 2.
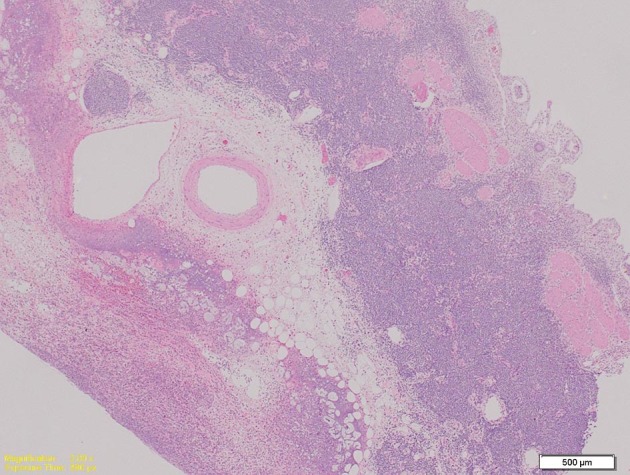
Microphotography showing a dense lymphoid infiltrate and acute serositis (haematoxylin and eosin stain)
Figure 3.
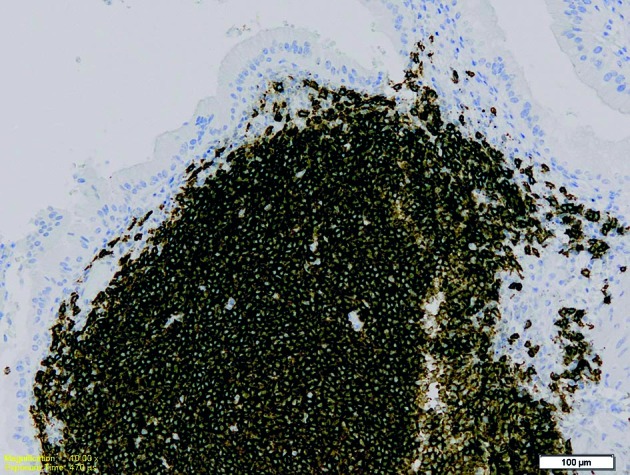
The neoplastic infiltrate showing strong and diffuse positivity with CD20, confirming these to be B cells (CD20 immunohistochemistry)
Staging CT carried out two months after the surgery showed uniform enhancement of the pancreas with no evidence of a mass or duct dilation and no evidence of residual or recurrent lymphoma. At oncology review, no adjuvant therapy was recommended and the cholecystectomy was considered curative. The patient remained symptom free at her six-month follow-up visit and is now due to be seen in one year.
Discussion
Extranodal lymphomas constitute approximately a quarter of all non-Hodgkin’s lymphomas.4 These extranodal, mucosa associated lymphoid tissue lymphomas occur most commonly in the gastrointestinal tract with the gallbladder being an unusual site.4 PGL is a rare entity; over 98% of malignant tumours of the gallbladder are adenocarcinomas and malignant lymphomas constitute only 0.1–0.2%.5 Clinically, PGLs tend to present mostly with features suggestive of acute cholecystitis and less often as a gallbladder mass.3 Radiologically, high grade lymphomas tend to form a mass presenting as irregular wall thickening whereas low grade lymphomas tend to show only slight thickening of the gallbladder wall.5
Serum amylase has a diagnostic sensitivity of 78.6% and a specificity of 99.4% for acute pancreatitis.6 Although highly specific, there are still clinical scenarios where a raised amylase level does not correspond to a diagnosis of acute pancreatitis. These include salivary gland diseases, abdominal pathology associated with inflammation, peptic ulcer disease and gynaecological conditions.6
Our case posed a diagnostic challenge. The clinical presentation of acute abdominal pain and raised serum amylase was highly suggestive of pancreatitis, which is usually managed non-operatively. However, the high suspicion of peritonitis and the absence of pancreatitis on imaging prompted us to proceed to an exploratory laparotomy to search for an alternative pathology. This decision was supported by the high suspicion of viscus perforation based on the clinical presentation, the recent history of NSAID use and the past medical history of peptic ulcer disease. In this case, early surgical intervention led us to an unexpected diagnosis of biliary peritonitis from gallbladder microperforation.
PGL causing perforation of the gallbladder is rare and has only been reported twice previously.7,8 In both those cases, the perforation was considered to be a complication of chemotherapy due to rapid tumour shrinkage.
Conclusions
There are two learning points from this case: 1) PGL is rare and can present as an acute abdomen secondary to perforation of the gallbladder, and 2) a high amylase level is not always associated with pancreatitis and other surgical causes that require surgical intervention may need to be explored.
References
- 1.Psarras K, Symeonidis N, Vlachaki E et al. . Primary gallbladder small lymphocytic lymphoma as a rare postcholecystectomy finding. Case Rep Hematol 2014; 716071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitra S, Mukherjee S, Chakraborty H. Mucosa associated lymphoid tissue lymphoma of gallbladder: a rare presentation. Indian J Pathol Microbiol 2014; : 502–503. [DOI] [PubMed] [Google Scholar]
- 3.Mani H, Climent F, Colomo L et al. . Gall bladder and extrahepatic bile duct lymphomas: clinicopathological observations and biological implications. Am J Surg Pathol 2010; : 1,277–1,286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zucca E, Roggero E, Bertoni F, Cavalli F. . Primary extranodal non-Hodgkin’s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol 1997; : 727–737. [DOI] [PubMed] [Google Scholar]
- 5.Ono A, Tanoue S, Yamada Y et al. . Primary malignant lymphoma of the gallbladder: a case report and literature review. Br J Radiol 2009; : e15–e19. [DOI] [PubMed] [Google Scholar]
- 6.Gomez D, Addison A, De Rosa A et al. . Retrospective study of patients with acute pancreatitis: is serum amylase still required? BMJ Open 2012; : e001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaafsma MR, Peters WG, Tham RT et al. . Gall bladder perforation in response to chemotherapy in a patient with a histiocytic lymphoma. Neth J Med 1988; : 78–82. [PubMed] [Google Scholar]
- 8.Kurtz RC, Geller W, Winawer SJ. Choledochoduodenal fistula and gall bladder perforation complicating Hodgkin’s disease. Am J Dig Dis 1974; : 275–277. [DOI] [PubMed] [Google Scholar]


