Abstract
Introduction
Rates of contralateral risk reducing mastectomy (CRRM) are rising despite a paucity of data to support this practice. Surgeons work as part of the multidisciplinary team (MDT). They may counsel women on these requests without the benefit of established guidelines or agreed protocol. This study assessed the practices and perceptions of breast and plastic surgeons in England on CRRM.
Methods
A postal questionnaire was sent to 455 breast and 364 plastic surgeons practising in England. Basic demographics, trends in CRRM, risk assessment, role of the MDT and knowledge base were assessed.
Results
The response rate among breast surgeons was 48.3% (220/455) and 12.6% (46/364) among plastic surgeons. Nearly half (44%) of the respondents felt there had been an increase in rates of CRRM over the last three years. Seventy-one per cent of those surveyed performed 1–5 CRRMs annually while sixteen per cent did not perform this procedure at all. A third (32%) of respondents correctly quoted their patients an annual risk of 0.5–0.7%. Funding was refused in 4% of cases and 43% of the surgeons felt that in the future they would have to apply to relevant clinical commissioning groups. Over half (58%) of all respondents reported that decisions for CRRM are always discussed in the MDT meeting but 6% stated that these cases are never discussed by the MDT.
BRCA mutation was perceived as the main risk factor for contralateral breast cancer by 81% of respondents. Surgeons felt that women requested CRRM mainly to alleviate anxiety. The next most common reasons were carriage of BRCA mutation and a desire to have reconstructions match.
Conclusions
A wide variation of surgical practices and perceptions exist in assessing women for CRRM. Guidelines to standardise practices are required.
Keywords: Contralateral breast cancer, Risk reducing mastectomy, Multidisciplinary team
Contralateral risk reducing mastectomy (CRRM) is the removal of a healthy, non-affected breast in women with breast cancer. The last decade has seen this practice increase by 150% in the US1,2 although this may not be the same in Europe.3 Rates of CRRM are also increasing among patients at high risk of contralateral breast cancer (CBC) such as BRCA1/2 mutation carriers4
The ‘Angelina Jolie effect’ (a term coined following her decision to undergo bilateral risk reducing mastectomies for her BRCA1 mutation in 2013) has seen a rise in the awareness of risk reducing mastectomy with a 250% increase in referrals to the genetics clinics in the UK and a doubling of BRCA1/2 testing5 Multiple other factors may contribute to this phenomenon of CRRM. Frequent use of MRI,6,7 rapid genetic testing,8 availability of immediate breast reconstruction and unsuccessful attempts at breast conservation9 have all been implicated in this changing trend. These factors contribute to the anxiety among many breast cancer patients, culminating in a request for CRRM.
This rise in CRRM is somewhat surprising. The worldwide incidence of CBC is decreasing10 Quoted annual incidence rates of 0.5% are probably outdated, a likely effect of successful adjuvant therapy. Survival data5 and cost effectiveness analysis11 favour this procedure in high risk patients, with unconvincing benefits in the remainder of patients.1,12 Low risk groups with sporadic breast cancer pose a particular challenge as the increasing number of requests for CRRM are not supported by survival data13
Multidisciplinary teams (MDTs) draw from the expertise of various key members and are invaluable in the decision making process of this complex procedure. There is paucity of data on the actual practices of CRRM at a national level. Little is known about the decision making process (eg whether formal risk assessment is carried out or whether each request is assessed in a multidisciplinary setting). The 2013 National Institute for Health and Care Excellence guidelines made a number of recommendations on preoperative assessment and counselling for risk reducing mastectomy and CRRM in high risk patients14 Although high risk patients may account for a significant proportion of CRRMs, no agreed protocol exists for the majority of breast cancer patients who fall outside this high risk group.
In the UK, appropriately trained oncoplastic breast and plastic surgeons perform both CRRM and reconstruction. This is in contrast to the US and parts of Europe, where breast surgeons would perform the mastectomy followed by reconstruction by plastic surgeons. The majority of plastic surgeons involved with the reconstructive element of CRRM work together with breast surgeons. As such, they would not necessarily be formally involved with risk assessment. An exception may be those women requiring a therapeutic mastectomy for cancer who choose immediate transverse rectus abdominis myocutaneous (TRAM)/deep inferior epigastric perforator (DIEP) flaps as their preferred reconstruction. (These procedures use tissue from the abdomen that can only be used once so a delayed contralateral mastectomy and reconstruction would need to employ tissue from elsewhere or an implant.) In these situations, an appreciation of risk assessment is crucial to balance the oncological issues surrounding CRRM and the desire for symmetrical reconstructions.
The principle objective of this study was to assess the practice and experience of surgeons involved with CRRM in England. We wanted to assess their perceptions on CBC risk and what factors they felt contributed to this risk. In addition, we sought to identify any interspecialty differences that may explain different attitudes to CRRM, to establish the role of the MDT and to investigate whether funding has been an important determining factor or whether it could be in the future.
Methods
We reviewed risk factors for CBC15 and designed a questionnaire to assess some of these factors. In particular, we wanted to gauge how surgeons assess requests for CRRM, what factors they considered important when recommending this procedure and issues on funding. Internal validation was included in the design by collection of questionnaire data from two other breast units. The questionnaire was piloted among local surgeons for ease of response, validity and relevance prior to posting them out (with a stamped addressed envelope). No reminders were sent and responses were considered over a three-month period.
The names of breast surgeons were obtained by contacting all the hospitals in England listed on the nhs.co.uk website while information for plastic surgeons was received from the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS). The BAPRAS members list consisted of 437 surgeons in the UK but questionnaires were sent only to those with an address in England (n=364). Consultants and non-consultant grades (staff and associate specialist doctors) were surveyed. Trainees were excluded from the study. It was accepted that not all BAPRAS members surveyed were reconstructive breast surgeons.
Statistical analysis
Statistical analysis was performed using SPSS® version 20 (IBM, New York, US). The chi-squared test and Kendall’s tau-b statistic were used to evaluate any differences between surgeons.
Results
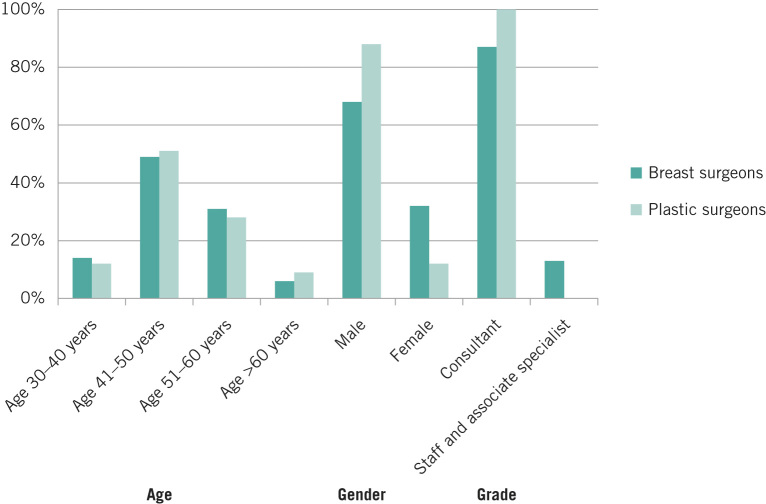
A total of 819 questionnaires were sent out. The response rate for breast surgeons was 48.3% (220/455) compared with 12.6% (46/364) for plastic surgeons. Not all respondents answered all questions. Nearly half of the surgeons sampled were between 41 and 50 years old, with less than 10% aged over 60 years across both specialties. The majority were male and of consultant grade (Fig 1).
Figure 1.
Demographics of respondents
Number of procedures performed
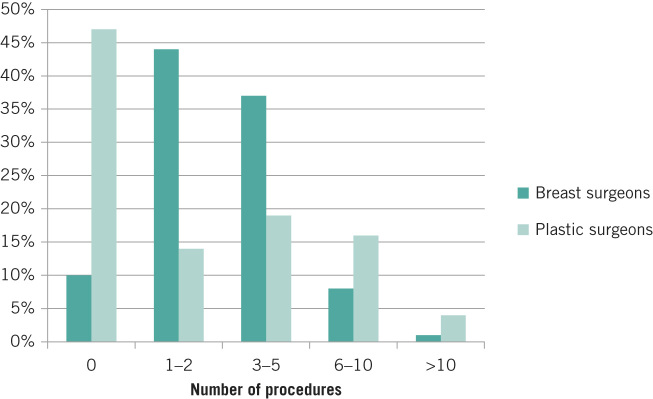
Of the 220 breast surgeons, 174 (79%) had performed 1–5 CRRMs over the past year, with only 2 (1%) having performed more than 10 operations (Fig 2). Twenty-two (10%) had not performed any CRRMs. Among the 46 plastic surgeons, 14 (30%) had performed 1–5 CRRMs over the last year whereas 2 (4%) had performed more than 10. Twenty (43%) had not performed any CRRMs in the last year. Overall, breast surgeons had performed more CRRMs than plastic surgeons (p<0.05).
Figure 2.
Number of contralateral risk reducing mastectomies performed by respondents
Nearly half of the respondents from both specialties (118/266, 44%) felt that requests for CRRM by patients were increasing while a third (101/266, 38%) believed there was no change. Approximately 2% (5/266) thought requests for CRRM were decreasing, with the remaining respondents unsure.
Risk assessment
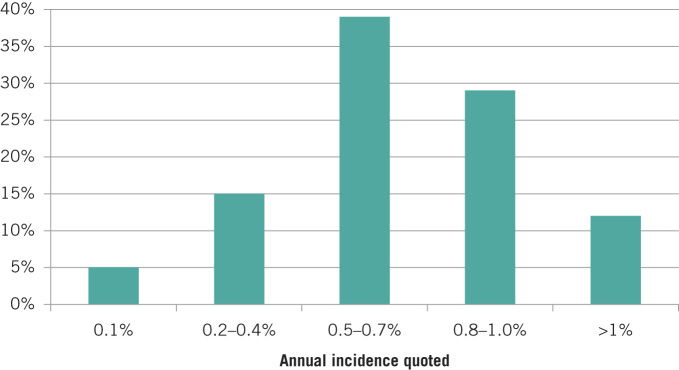
Each surgeon was asked to comment about the perceived incidence of CBC. The majority felt that the incidence in their practice was unchanged. When asked what approximate risk (annual incidence) of developing CBC surgeons quoted their patients (without any additional risk factors), 11 breast surgeons (5%) reported quoting an annual incidence of 0.1%, 29 (13%) quoted 0.2–0.4%, 77 (35%) quoted 0.5–0.7%, 57 (26%) quoted 0.8–1.0% and 18 (8%) quoted >1%. Of the plastic surgeons, 1 (2%) reported quoting 0.1%, 5 (11%) quoted 0.2–0.4%, 8 (17%) quoted 0.5–0.7%, 6 (13%) quoted 0.8–1.0% and 8 (17%) quoted >1%. The combined results are displayed in Figure 3.
Figure 3.
Annual incidence of developing contralateral breast cancer quoted by respondents to their patients
Those respondents who did not choose any of the listed options stated that they do not quote a risk to their patients or that the percentage they quoted depended on the risk of the individual patient. Plastic surgeons were less likely to quote a risk to their patients than breast surgeons (p<0.0001).
The questionnaire asked the surgeons to rank the top five reasons why patients requested CRRM. Options on the list of reasons included fear/anxiety of getting another breast cancer, young age, desire to have reconstruction match/symmetry, concern regarding family history, mistrust of surveillance, BRCA status, recommendation from family/friend and ‘other’. Fear/anxiety of getting another breast cancer was deemed the most important reason for requesting CRRM, followed by BRCA status (Fig 4). The next most common reasons were desire to have reconstruction match/symmetry, concern regarding family history and mistrust of surveillance.
Figure 4.
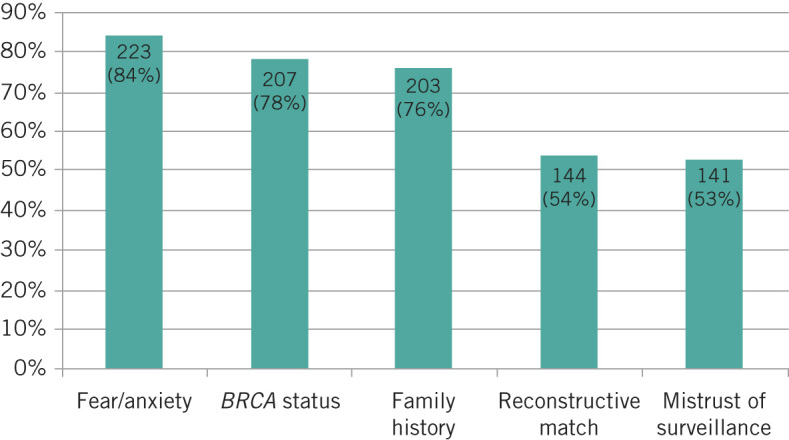
Top five reasons (as ranked by respondents) for patients requesting contralateral risk reducing mastectomy
The surgeons were also asked to rank the top five factors they felt are important in the assessment of a patient’s risk for developing a CBC. Options on the list of factors included young age, histology, family history, BRCA status, lymph node status, grade, stage, oestrogen/progesterone receptor negativity, human epidermal growth factor receptor 2 positivity, multicentric disease, breast density, obesity and premalignant disease. The majority (84%) ranked BRCA status as the most important factor and family history as the second most important factor (72% of surgeons). These results are displayed in Figure 5.
Figure 5.
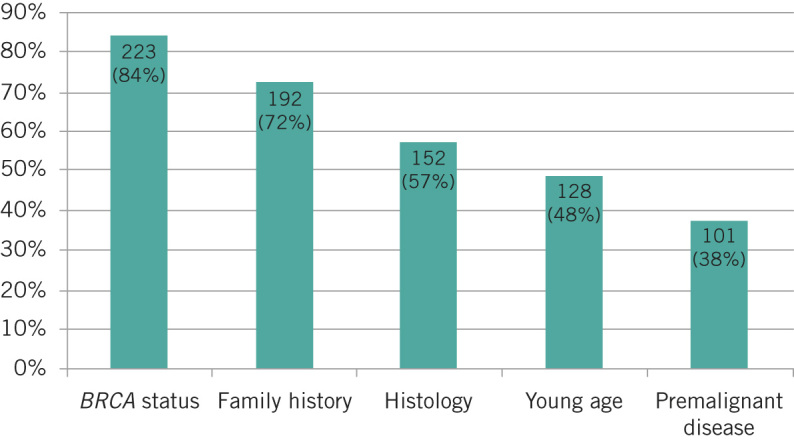
Top five factors that respondents feel are important in the assessment of a patient’s risk for developing contralateral breast cancer
Free text from respondents covered similar themes, namely that ‘the prognosis is determined by the cancer they have got, not the cancer they may never get’ and ‘CRRM should only be offered to high risk patients’. Some stated they ‘dissuade [patients] from’, ‘resist’ or are ‘loath to offer’ CRRM. One surgeon commented that ‘CRRM is a legitimate part of the reconstruction process’ whereas another thought the opposite: ‘CRRM is performed because of increasing availability of oncoplastic procedures rather than a true clinical need.’
Funding
The vast majority of respondents (245/266, 92%) had never been refused funding for CRRM although ten surgeons (4%) had experienced a refusal. Reasons for refusal of funding included lack of genetic testing, a greater than ten-year interval from the original cancer and refusal from private insurance stakeholders. Almost half of all those surveyed (115/266, 43%) felt that within the next three years, special applications for funding to clinical care groups would be mandatory.
Decision making/multidisciplinary team
When asked about the decision making process in their unit for CRRM, over half (58%) of the respondents said requests for CRRM are always discussed in the MDT meeting. Almost a third (29%) reported that they are sometimes discussed and 6% indicated that these cases are never discussed by the MDT.
The types of healthcare professionals involved in the decision making process for CRRM varied. Overall, a single surgeon and a breast care nurse were always involved in 67% and 75% of cases respectively while a psychologist and an oncologist were always involved in 35% and 34% of cases respectively. Geneticists were always involved in 18% of cases.
Discussion
Our study has highlighted important variations in the management of women seeking CRRM. There is a wide discrepancy in the number of cases performed per surgeon across and within the two specialties surveyed. An explanation could be that it is dependent on the geography and workload of particular breast units, with tertiary centres (which have plastic surgery services and dedicated genetics services) attracting the majority of the work. It is clear from the free text answers that surgeons’ views on CRRM could affect whether a woman seeking surgery can access CRRM, particularly if the decision is taken outside the MDT process.
Surgeons are often at the front line of managing requests for CRRM. Consequently, the wide variation of risk quoted by surgeons is of concern. CBC risk is dependent on several factors including oestrogen receptor status, antiendocrine treatment, age of patient, and (most importantly) family history and genetics15 It may be more accurate to incorporate these factors when carrying out risk assessments so that each patient receives a personal CBC risk score based on known risk factors.
It is clearly best practice to make an assessment of CBC risk in women seeking CRRM14 and it is possible that the calculation of risk of CBC using known objective factors16 may be enough in some instances to encourage a woman towards having/not having CRRM. The counselling process for the majority of breast cancer patients who are not BRCA mutation carriers should emphasise that the risk of relapse arises from the index cancer and as such, CRRM for these women may be of limited survival benefit.
Requests for CRRM are based on a combination of patient and surgical factors. Anxiety about a further breast cancer and mortality, wanting to avoid chemotherapy for a second time or the desire to have matching reconstructions are important considerations. It has been shown that female surgeons are more likely to recommend CRRM7 Surgeon related factors are also affected by country17,18 with the UK among those more likely to recommend CRRM18 Our study found no significant differences in respondents’ age, sex or specialty grade. It had too few female respondents (n=53) to perform any subgroup analysis. However, in a study by Arrington et al, all female surgeons whose patients underwent CRRM were under the age of 50 years7
Cost effectiveness is becoming a major determinant in the medical decision making process. A clear cost benefit over routine surveillance has been shown in BRCA mutation carriers but this is somewhat diminished in non-mutation carriers11 Surgeons feel that the criteria for CRRM funding may become more stringent in a cash stricken UK health economy. Policy makers are likely to scrutinise the survival benefit of this procedure and may restrict access, basing decisions solely on CBC risk without considering the multifactorial reasons that breast cancer patients request CRRM.
A Cochrane analysis from 2010 on CRRM confirmed a reduction in incidence of CBC without a clear survival benefit in non-high risk patients1 Our surgeons ranked gene mutation followed by family history as the most important reasons they would recommend CRRM. This is in keeping with published studies19
To our knowledge, this is the first study to assess the role of the MDT and specific health professionals in the assessment of CRRM. The responses to our questionnaire indicated that most centres in England process requests for CRRM via the MDT although this is not universal. Only a third of patients will access psychologists, which is surprising given that anxiety and psychological wellbeing are major determinants in requests for CRRM17
Access to psychologists may be limited but it is invaluable. It ensures that patients are well informed of alternatives to combat anxiety surrounding CRRM that may include psychological treatment (eg cognitive behaviour therapy or use of appropriate anxiolytic medications). The MDT process should ensure objective CBC risk and psychological assessment have taken place, and that women considering CRRM are well informed of the higher complication rates associated with this procedure20 It is possible that requests for a delayed CRRM may circumvent the MDT process as they are not considered active cancer cases. Our study has shown that surgeons and breast care nurses are the main professionals involved with the decision making process, and we would suggest engaging the core members where possible before making a final recommendation.
Given that rates of immediate breast reconstruction have doubled in England,4 there are unanswered questions from this study regarding the different types of reconstructions available and the consequences of choosing them. One respondent felt that CRRM was ‘a legitimate part of the reconstruction process’, raising the concern that not all surgeons involved in CRRM use objective CBC risk in their assessment for this procedure. The desire to have reconstructions match is an important point from the patient’s and surgeon’s view but this needs to be weighed up against the CBC risk and the risk of surgery.
A study from 2013 assessed the patient’s perspective of requesting CRRM in 60 consecutive women under consideration for this procedure21 In almost all cases, requests for CRRM were instigated by the patient and every patient unambiguously wanted CRRM. Patients responded to risk in an ‘all or nothing’ manner and the majority did not quantify this risk objectively. The risk assessment for those who did quantify risk played little role in their decision for surgery. The authors concluded that ‘patients’ subjective sense of vulnerability overwhelmed their appreciation of risk so that, regardless of level of risk of CBC, they found this risk intolerable and felt that only CRRM could reduce it’.
Two important factors raised by the questionnaire were objective assessment of risk of CBC and survival benefit. A third of the surgeons surveyed incorrectly quote an annual CBC risk of 0.8% or more to patients with no additional risk factors. The actual incidence for CBC in such patients is 0.5% per annum10 whereas those with a family history or those who are BRCA mutation carriers have an annual risk of approximately 2–3%22 Overestimation of risk in patients may intensify anxiety levels. Women should have a personalised risk assessment that takes into account the known risk factors of young age (<35 years), oestrogen receptor status, endocrine therapy use (50% reduction), family history, genetic mutation status, oophorectomy at <50 years and age of menopause. Our findings are consistent with those in previous studies,19 namely that surgeons use both objective and subjective factors when recommending CRRM.
Discussions on survival benefit should be tailored to the risk profile of the patient. Two studies on BRCA1/2 patients in 2014 confirmed a survival benefit from CRRM.5,13 Metcalfe et al showed that at 20 years, the survival rate for those who underwent CRRM was 88% compared with 66% for those who did not, with CRRM offering a 48% reduction in death from breast cancer13 In contrast, Portschy et al used a Markov model to compare survival between CRRM and no CRRM in patients without BRCA mutation23 They concluded that the absolute 20-year survival benefit from CRRM was less than 1% among all age, oestrogen receptor status and cancer stage groups.
Studies have demonstrated long-term (up to 20 years) patient satisfaction with CRRM,24,25 with up to 92% of women stating they would choose the procedure again25 Many women will be offered/choose CRRM even without any survival benefit to reduce the anxiety of developing another cancer, and these are important factors to consider during the counselling process.
It is clear that categorising patients who request CRRM according to their CBC risk is critical in the decision making process. The survival benefit in high risk patients5,13 allows a more straightforward counselling process for CRRM. It is evident from our study that the top two reasons surgeons consider CRRM are based on genetic mutation status followed by family history. However, it is the remaining sporadic (‘lower risk’) breast cancer patients, among whom requests for CRRM are increasing, who need careful counselling to establish their CBC risk, psychological status and reconstructive challenges26 Surgeons in our study felt that the main reason patients request CRRM was because of fear and anxiety followed by mutation status and family history. Although there is likely to be an overlap among these reasons, it is in particular the fear and anxiety that needs to be addressed in a multidisciplinary setting.
Study limitations
There are a number of limitations for this study. A postal questionnaire must be concise to ensure that recipients will respond but the results of the survey should also be informative regarding the practices in general around CRRM. It would have been useful to assess respondents’ personal experience of risk assessment (eg use of validated tools such as the Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm, the Tyrer–Cuzick model and the Manchester scoring system). Furthermore, our questionnaire did not ask recipients to include the number of requests received for CRRM or what proportion of these procedures were carried out on high risk patients (positive family history or BRCA mutation carriers). Assessment of differences between immediate and delayed CRRM as well as analysis of characteristics between respondents and non-respondents would be helpful in shaping future practice. Unfortunately, this was outside the scope of this study.
There was a poor response to the questionnaire among plastic surgeons (12.6%). Current estimates are that 30% of BAPRAS members perform oncoplastic breast surgery in the National Health Service and this may explain the low response rate. Although it was recognised that the majority of BAPRAS members would not be reconstructive breast surgeons, the questionnaire was sent to the whole membership list as it was anticipated that only those with a special interest in breast reconstruction would reply. We are unable to determine what proportion of the plastic surgeon non-respondents perform CRRM and there could be an inherent selection bias in respondents compared with non-respondents.
It may be argued that the majority of plastic surgeons are involved solely with the technicalities of breast reconstruction in CRRM and would not become involved in risk counselling. However, it is important for plastic surgeons and, in particular, breast surgeons to have some understanding of risk assessment, especially when discussing an immediate TRAM/DIEP flap for breast cancer. Our study has identified that risk assessment across both specialties can be improved, with almost half of respondents overestimating the risk of CBC.
Conclusions
There is a wide variation of practices and perceptions among surgeons in England dealing with CRRM. It is likely that the number of breast cancer patients requesting this will continue to increase and surgeons need to draw from the expertise of the MDT in assessing these patients. Nationally agreed guidelines would aid surgeons and other medical professionals in counselling this complex group of patients amidst times of increasing pressure on healthcare economics.
Acknowledgements
Funding for the postal questionnaire was received from Genesis Breast Cancer Prevention. The authors would like to thank Gemma Adlington from BAPRAS and Toni Musiello from the University of Western Australia for their help with the design and circulation of the questionnaire.
References
- 1.Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev 2010; : CD002748. [DOI] [PubMed] [Google Scholar]
- 2.Yao K, Stewart AK, Winchester DJ, Winchester DP. Trends in contralateral prophylactic mastectomy for unilateral cancer: a report from the National Cancer Data Base, 1998. –2007. Ann Surg Oncol 2010; 17: 2,554–2,562. [DOI] [PubMed] [Google Scholar]
- 3.Güth U, Myrick ME, Viehl CT et al. Increasing rates of contralateral prophylactic mastectomy – a trend made in USA? Eur J Surg Oncol 2012; : 296–301. [DOI] [PubMed] [Google Scholar]
- 4.Evans DG, Ingham SL, Baildam A et al. Contralateral mastectomy improves survival in women with BRCA1/2-associated breast cancer. Breast Cancer Res Treat 2013; : 135–142. [DOI] [PubMed] [Google Scholar]
- 5.Evans DG, Barwell J, Eccles DM et al. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res 2014; : 442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorbero ME, Dick AW, Beckjord EB, Ahrendt G. Diagnostic breast magnetic resonance imaging and contralateral prophylactic mastectomy. Ann Surg Oncol 2009; : 1,597–1,605. [DOI] [PubMed] [Google Scholar]
- 7.Arrington AK, Jarosek SL, Virnig BA et al. Patient and surgeon characteristics associated with increased use of contralateral prophylactic mastectomy in patients with breast cancer. Ann Surg Oncol 2009; : 2,697–2,704. [DOI] [PubMed] [Google Scholar]
- 8.Francken AB, Schouten PC, Bleiker EM et al. Breast cancer in women at high risk: the role of rapid genetic testing for BRCA1 and -2 mutations and the consequences for treatment strategies. Breast 2013; : 561–568. [DOI] [PubMed] [Google Scholar]
- 9.King TA, Sakr R, Patil S et al. Clinical management factors contribute to the decision for contralateral prophylactic mastectomy. J Clin Oncol 2011; : 2,158–2,164. [DOI] [PubMed] [Google Scholar]
- 10.Lizarraga IM, Sugg SL, Weigel RJ, Scott-Conner CE. Review of risk factors for the development of contralateral breast cancer. Am J Surg 2013; : 704–708. [DOI] [PubMed] [Google Scholar]
- 11.Zendejas B, Moriarty JP, O'Byrne J et al. Cost-effectiveness of contralateral prophylactic mastectomy versus routine surveillance in patients with unilateral breast cancer. J Clin Oncol 2011; : 2,993–3,000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrington LJ, Barlow WE, Yu O et al. Efficacy of prophylactic mastectomy in women with unilateral breast cancer: a cancer research network project. J Clin Oncol 2005; : 4,275–4,286. [DOI] [PubMed] [Google Scholar]
- 13.Metcalfe K, Gershman S, Ghadirian P et al. Contralateral mastectomy and survival after breast cancer in carriers of BRCA1 and BRCA2 mutations: retrospective analysis. BMJ 2014; : g226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute for Health and Care Excellence Familial Breast Cancer: Classification, Care and Managing Breast Cancer and Related Risks in People with a Family History of Breast Cancer. London: NICE; 2013. [PubMed] [Google Scholar]
- 15.Basu NN, Barr L, Ross GL, Evans DG. Contralateral risk-reducing mastectomy: review of risk factors and risk-reducing strategies. Int J Surg Oncol 2015; 901046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basu NN, Ross GL, Evans DG, Barr L. The Manchester guidelines for contralateral risk-reducing mastectomy. World J Surg Oncol 2015; : 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metcalfe KA, Lubinski J, Ghadirian P et al. Predictors of contralateral prophylactic mastectomy in women with a BRCA1 or BRCA2 mutation. J Clin Oncol 2008; : 1,093–1,097. [DOI] [PubMed] [Google Scholar]
- 18.Den Heijer M, van Asperen CJ, Harris H et al. International variation in physicians' attitudes towards prophylactic mastectomy– comparison between France, Germany, the Netherlands and the United Kingdom. Eur J Cancer 2013; : 2,798–2,805. [DOI] [PubMed] [Google Scholar]
- 19.Musiello T, Bornhammar E, Saunders C. Breast surgeons' perceptions and attitudes towards contralateral prophylactic mastectomy. ANZ Surg 2013; : 527–532. [DOI] [PubMed] [Google Scholar]
- 20.Miller ME, Czechura T, Martz B et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol 2013; : 4,113–4,120. [DOI] [PubMed] [Google Scholar]
- 21.Beesley H, Holocombe C, Brown SL, Salmon P. Risk, worry and cosmesis in decision-making for contralateral risk-reducing mastectomy: analysis of 60 consecutive cases in a specialist breast unit. Breast 2013; : 179–184. [DOI] [PubMed] [Google Scholar]
- 22.Basu NN, Ingham S, Hodson J et al. Risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a 30-year semi-prospective analysis. Fam Cancer 2015; : 531–538 [DOI] [PubMed] [Google Scholar]
- 23.Portschy PR, Kuntz KM, Tuttle TM. Survival outcomes after contralateral mastectomy: a decision analysis. J Natl Cancer Inst 2014; : dju160. [DOI] [PubMed] [Google Scholar]
- 24.Frost MH, Hoskin TL, Hartmann LC et al. Contralateral prophylactic mastectomy: long-term consistency of satisfaction and adverse effects and the significance of informed decision-making, quality of life, and personality traits. Ann Surg Oncol 2011; : 3,110–3,116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boughey JC, Hoskin TL, Hartmann LC et al. Impact of reconstruction and reoperation on long-term patient-reported satisfaction after contralateral prophylactic mastectomy. Ann Surg Oncol 2015; : 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy JA, Milner TD, O'Donoghue JM. Contralateral risk-reducing mastectomy in sporadic breast cancer. Lancet Oncol 2013; : e262–e269. [DOI] [PubMed] [Google Scholar]