Abstract
Introduction
Trauma is a significant cause of morbidity and mortality in the UK. Since the inception of the trauma networks, little is known of the temporal pattern of trauma admissions.
Methods
Trauma Audit and Research Network data for 1 April 2011 to 31 March 2013 were collated from two large major trauma centres (MTCs) in the South East of England: Brighton and Sussex University Hospitals NHS Trust (BSUH) and St George's University Hospitals NHS Foundation Trust (SGU). The number of admissions and the injury severity score by time of admission, by weekdays versus weekend and by month/season were analysed.
Results
There were 1,223 admissions at BSUH and 1,241 at SGU. There was significant variation by time of admission; there were more admissions in the afternoons (BSUH p<0.001) and evenings (SGU p<0.001). There were proportionally more admissions at the weekends than on weekdays (BSUH p<0.001, SGU p=0.028). There was significant seasonal variation in admissions at BSUH (p<0.001) with more admissions in summer and autumn. No significant seasonal variation was observed at SGU (p=0.543).
Conclusions
The temporal patterns observed were different for each MTC with important implications for resource planning of trauma care. This study identified differing needs for different MTCs and resource planning should be individualised to the network.
Keywords: Major trauma, Injury, Temporal variation
Trauma is one of the leading causes of death in children and adults under 50 years of age in England and Wales.1 In addition, trauma is a significant cause of moderate or severe disability, causing the loss of over 250 million disability adjusted life years worldwide each year.2 Emergency treatment and hospital care for trauma has an estimated annual cost of £300–£400 million to the National Health Service (NHS) in England and presents an estimated burden of £3.3–£3.7 billion in lost economic output per year.3
Following the establishment of the London trauma network in 2010 and the UK-wide trauma network in 2012, trauma related mortality has improved. Data from the 2013 Trauma Audit and Research Network (TARN) national audit that are yet to be published in the peer reviewed literature have demonstrated a 20% reduction in trauma mortality.4
The current concept of a seven-day, ‘consultant-led’ working week for the NHS has been a focus of political policy and the media5 with some evidence to suggest that patient mortality in the UK is higher at weekends in emergency medicine6 and trauma care.7,8 The first priority of the NHS seven-day plan is the provision of urgent and emergency care.9–12 Under this plan, centres with appropriate patient volume should provide the same standard of emergency care 24 hours a day, 7 days a week. For major trauma, this includes the provision of consultant-led care, adequate staffing, staffed operating theatres and access to imaging as well as the provision of essential support services and allied health professionals.
Resource and workforce planning are important aspects of trauma care organisation and delivery, particularly at major trauma centres (MTCs), where a balance must be struck between limited resources and potential caseload. A lack of appropriately qualified staff or sufficient resources risks substandard patient care while an excess in the ratio of staffing/resources to caseload is neither efficient nor cost effective, especially given the specialist nature of care that MTCs provide.
Major trauma is relatively rare with many hospitals only admitting one major trauma patient (injury severity score [ISS] >15) per week8 and major trauma only forming 0.1% of emergency department admissions.13 Understanding the temporal and regional variation of trauma would enable more appropriate staffing and resource allocation. Furthermore, the evidence base for the temporal pattern and severity of trauma admissions in the UK is lacking. The aims of this study were to analyse the temporal variation in trauma admissions at two large MTCs in South East England and to investigate the temporal pattern of injury severity associated with these admissions.
This study will provide useful data for effective planning of staffing and resource allocation, with implications for patient care and cost of care within the context of two MTCs. It remains unclear whether the resource requirements of a London MTC are similar to those MTCs outside London and whether trauma resource planning can use a ‘one size fits all’ approach for MTCs.
Methods
The Trauma Audit and Research Network (TARN) is a national body that records the frequency, severity and mechanism of injury for major trauma. In order to maintain MTC status, there must be 95% compliance with TARN data. These data are audited annually and monitored by TARN.
TARN data for 1 April 2011 to 30 March 2013 were analysed for two MTCs: Brighton and Sussex University Hospitals NHS Trust (BSUH) and St George’s University Hospitals NHS Foundation Trust (SGU). The BSUH MTC is a three-site, urban/rural MTC based in Sussex. It provides specialist trauma care to a population of approximately 1.5 million.14 SGU is an urban MTC based in Tooting, London. It is part of the South West London and Surrey trauma network and provides specialist trauma care to a population of approximately 2.6 million.15
TARN data are collected on all patients admitted to hospital who have sustained an injury, who are alive at the time of admission and who fulfil one or more of the following criteria:
-
>
Patient's length of stay ≥72 hours.
-
>
The patient was admitted to a high dependency area.
-
>
The patient was transferred to or from another hospital for specialist care or a high dependency bed.
-
>
The patient died in hospital.
A detailed description of the TARN collection criteria (including criteria for exclusion) can be found in the TARN procedures manual.16
The primary outcomes of our study were the hour of admission, day of the week, month/season and ISS.17 Weekdays were defined as Monday to Friday (12.00am – 11:59pm) and the weekend was defined as Saturday and Sunday (12.00am – 11:59pm). Winter was defined as December to February, spring as March to May, summer as June to August and autumn as September to November. ISS was divided into four bands: ISS <9, ISS 9–15, ISS 16–24 and ISS >24.
Statistical analysis
Statistical analysis was performed using SPSS® version 21.0 (IBM, New York, US) with the guidance of a medical statistician. Data were analysed by MTC. Chi-squared tests were performed for caseload by year, by time of admission, by weekdays versus weekend and by season. The chi-squared test was also used for comparison of the number and proportion of severely injured patients (ISS >24) by time of admission and season. The binomial test was used for comparison of the proportion of severely injured patients by weekdays versus weekend. The Mann–Whitney U test was used for comparison of ISS by hospital and by weekdays versus weekend. Kruskal–Wallis one-way analysis of variance was used to compare ISS by season and time of admission. A p-value of <0.05 was considered statistically significant.
Results
There were 2,464 cases submitted to TARN for the time period studied. This included 1,223 patients from BSUH and 1,241 patients from SGU. Three cases from BSUH were missing data for hour of admission so these were excluded from analysis by time of admission. There was no significant difference in the total number of admissions between BSUH and SGU (p=0.717). The estimated admission rate per catchment population was 47 trauma patients per 100,000 per year for BSUH and 24 for SGU using known population estimates.14,15 The ISS range observed was 1–75. The median ISS for BSUH was 13 (interquartile range [IQR]: 9–24) while for SGU, it was 14 (IQR: 9–24). This difference was not statistically significant (p=0.068). The number of major trauma admissions (ISS >15) during the study period was 582 and 596 for BSUH and SGU respectively. Major trauma formed 48% of the caseload at both MTCs.
Caseload by year
There was an increase in admissions observed at both MTCs during the study period. For BSUH, trauma admissions increased from 506 (41% of BSUH total during study period) between April 2011 and March 2012 to 717 (59%) between April 2012 and March 2013 (p<0.001). For SGU, trauma admissions increased from 587 (47% of SGU total during study period) to 654 (53%) although this was not statistically significant (p=0.057).
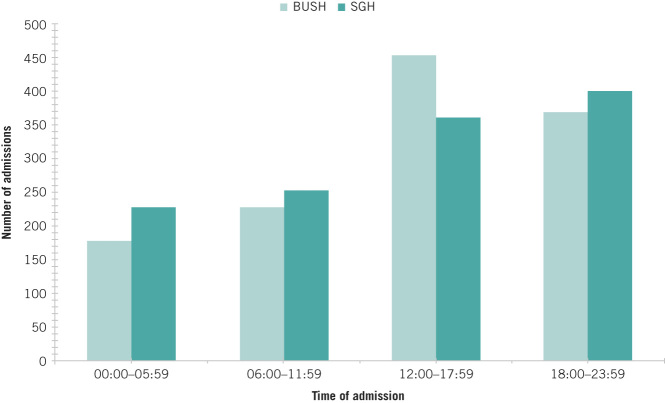
Caseload by time of admission
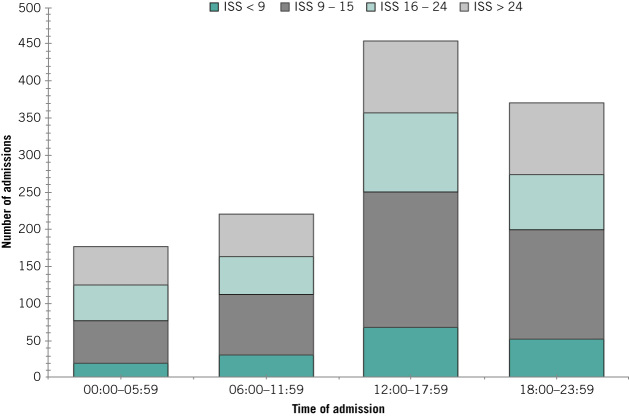
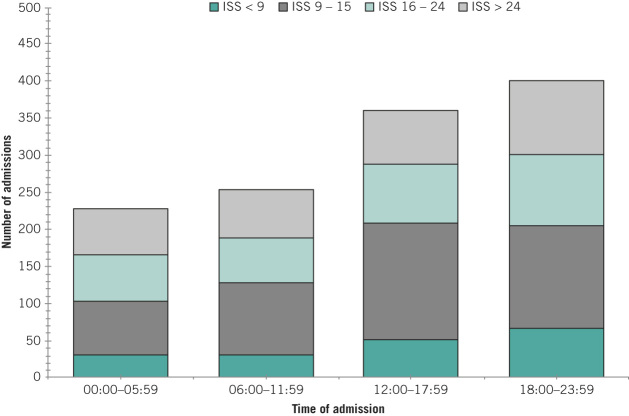
For BSUH, the largest number (37%) of admissions occurred in the afternoon (12.00pm – 5:59pm) while at SGU, the largest number (32%) occurred in the evening (6.00pm – 11:59pm) (Fig 1). The fewest admissions occurred between 12.00am and 5.59am for BSUH (15%) and SGU (18%). There was significant variation in caseload by time of admission (p<0.001 for each MTC).
Figure 1.
Caseload by time of admission at Brighton and Sussex University Hospitals NHS Trust (BSUH) and St George’s University Hospitals NHS Foundation Trust (SGU)
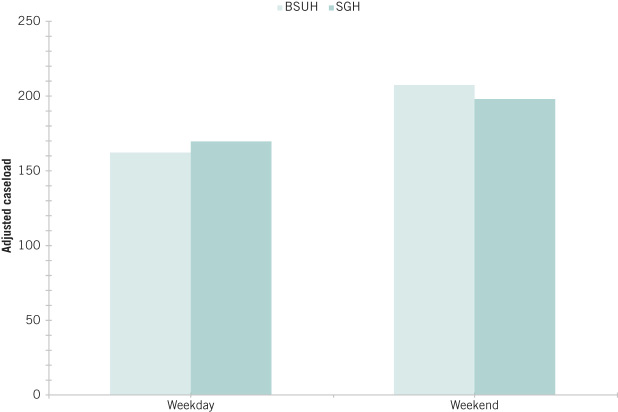
Caseload by weekdays vs weekend
Adjusting caseload for number of days, 34% and 32% of admissions occurred at the weekend for BSUH and SGU respectively. There was a significant difference in the number of admissions on weekdays versus weekends, with a proportionally greater number of admissions on Saturdays and Sundays than on weekdays for both BSUH (12% higher; p<0.001) and SGU (8% higher; p=0.028) (Fig 2).
Figure 2.
Adjusted caseload by weekday versus weekend at Brighton and Sussex University Hospitals NHS Trust (BSUH) and St George’s University Hospitals NHS Foundation Trust (SGU)
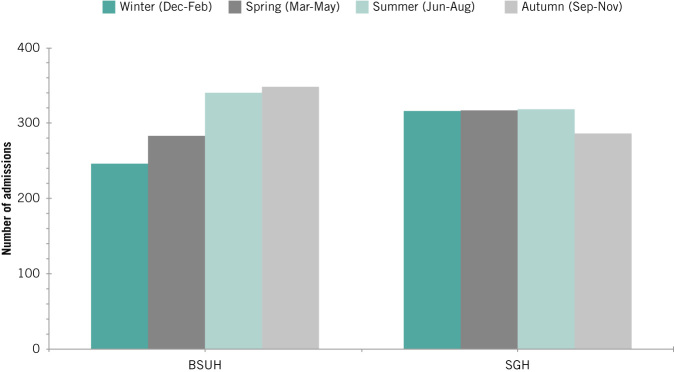
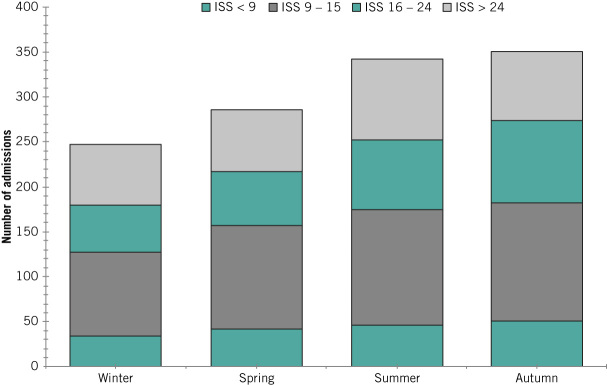
Caseload by season
Significant variation in the number of trauma admissions across the seasons was observed for BSUH (p<0.001). Most admissions there occurred in summer (28%) or autumn (29%) and the fewest occurred in winter (20%). No significant seasonal variation was observed in caseload for SGU (p=0.543). The breakdown for the two MTCs is shown in Figures 3 and 4.
Figure 3.
Caseload by season at Brighton and Sussex University Hospitals NHS Trust (BSUH) and St George’s University Hospitals NHS Foundation Trust (SGU)
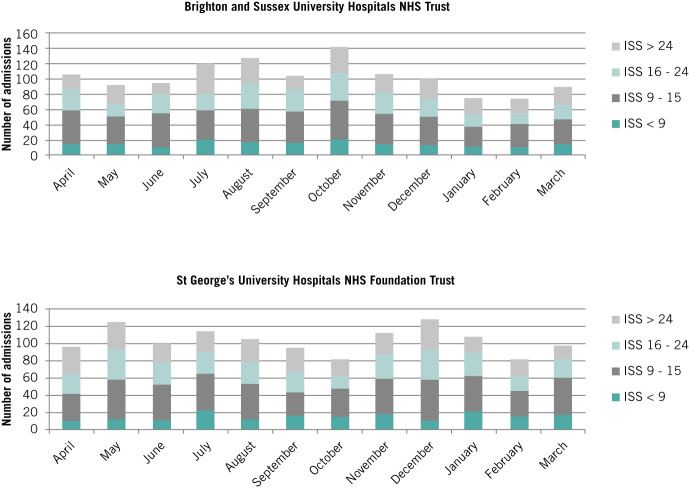
Figure 4.
Caseload by injury severity score (ISS) and month
ISS by time of admission
A significant difference in median ISS by time of admission was observed for BSUH (p=0.033) but not for SGU (p=0.084). For BSUH, the median ISS was highest (median 16) in the early hours (12.00am – 5.59am) and decreased through the day to a median of 13 for the period from 12.00pm to 11:59pm. There was also significant variation in the number of severely injured patients (ISS >24) admitted by time of admission. At BSUH, more severely injured patients were admitted in the afternoon and evening (12.00pm – 11:59pm) than in the morning (12.00am – 11.59am) (p<0.001) (Fig 5). At SGU, the majority of severely injured patients were admitted in the evening (6.00pm – 11.59pm) (p=0.011) (Fig 6). However, no significant difference in the proportion of severely injured patients was noted by time of admission for BSUH or SGU (p=0.300 and p=0.306 respectively).
Figure 5.
Caseload by injury severity score (ISS) and time of admission at Brighton and Sussex University Hospitals NHS Trust
Figure 6.
Caseload by injury severity score (ISS) and time of admission at St George’s University Hospitals NHS Foundation Trust
ISS by weekdays vs weekend
There was no significant difference in median ISS by weekdays versus weekend for BSUH (p=0.225) or SGU (p=0.150). There was also no significant difference in the proportion of severely injured patients (ISS >24) admitted at the weekend rather than during the week for BSUH or SGU (p=0.133 and p=0.078 respectively). Figures 7 and 8 illustrate the caseload by ISS band and by weekdays versus weekend for the two MTCs.
Figure 7.
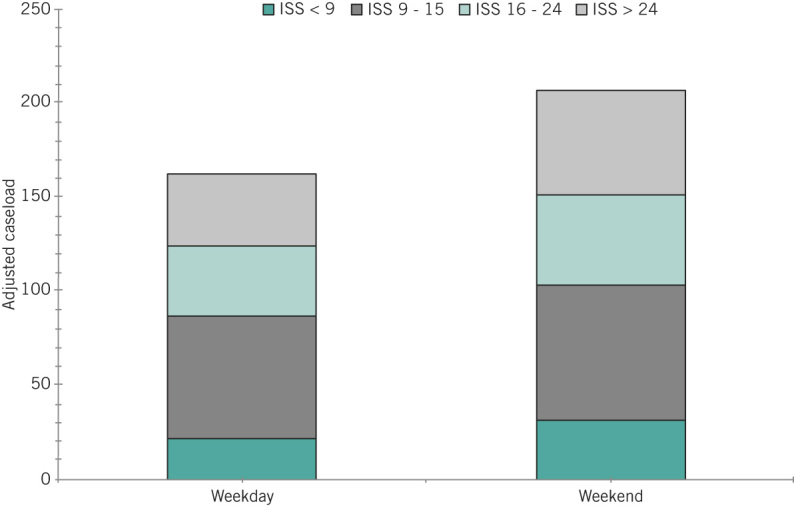
Adjusted caseload by injury severity score (ISS) and weekday versus weekend at Brighton and Sussex University Hospitals NHS Trust
Figure 8.
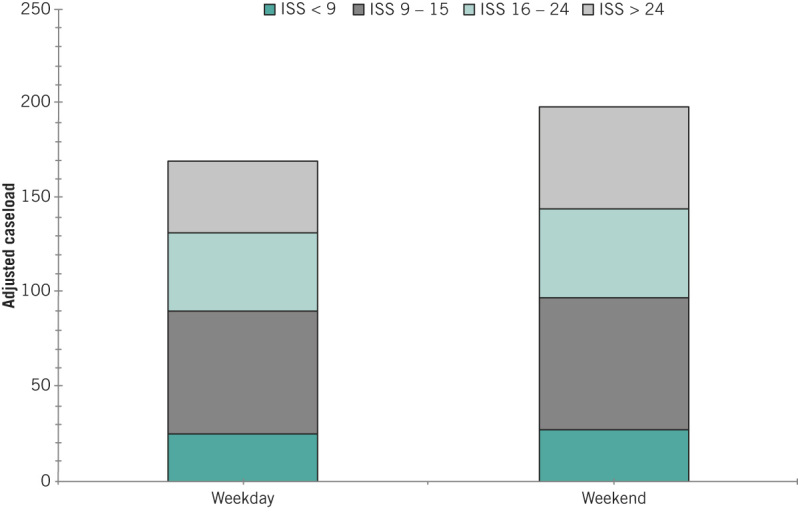
Adjusted caseload by injury severity score (ISS) and weekday versus weekend at St George’s University Hospitals NHS Foundation Trust
ISS by season
There was no significant difference in the median ISS by season for BSUH or SGU (p=0.727 and p=0.860 respectively). Similarly, there was no significant difference in the number or proportion of severely injured patients (ISS >24) admitted by season (BSUH: p=0.245, p=0.519; SGU: p=0.964, p=0.948). The caseload by ISS band and season for the two MTCs is shown in Figures 9 and 10.
Figure 9.
Caseload by injury severity score (ISS) and season at Brighton and Sussex University Hospitals NHS Trust
Figure 10.
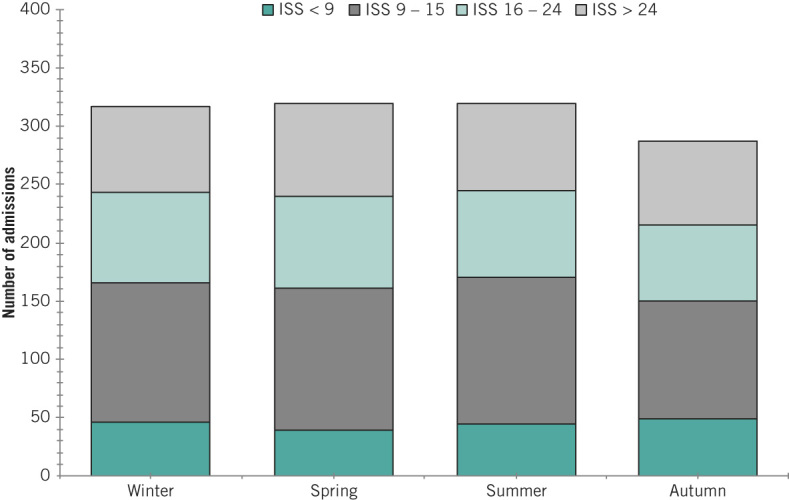
Caseload by injury severity score (ISS) and season at St George’s University Hospitals NHS Foundation Trust
Discussion
This study identified the temporal variation and severity of injury for admissions for two MTCs in the UK, with a combined catchment population of approximately 3.9 million. Trauma admissions at both centres increased during the study period. At BSUH in particular, there was a significant increase in trauma admissions in the second year of the study. This is likely to be a result of BSUH becoming a formally designated MTC at the beginning of the second year of the study period, with triage protocols directing more trauma patients to BSUH who otherwise would have gone elsewhere. During the first year, however, the local ambulance services were diverting major trauma admissions to BSUH using triage tools.
The calculations of the rate of trauma admissions suggest that BSUH has 70% more trauma admissions for a given catchment population than SGU. There are a number of possible reasons for this finding. It may be an indication of greater rates of serious injury in the BSUH catchment area than that of SGU or simply of tourism with more visitors to the South Coast and therefore the BSUH catchment area.
The BSUH catchment area is considerably more rural than that of SGU and this could be a contributory factor. There is literature from North America demonstrating higher injury rates in rural versus urban environments, with higher speed of travel and therefore higher energy road traffic collisions (RTCs) in the rural setting thought to contribute to this.18 Clark and Cushing have also demonstrated the variation in rural and urban traffic fatalities in the US while controlling for vehicle miles travelled.19 They found that population density showed a relatively strong correlation with mortality rates for RTCs.
Whilst UK data comparing urban and rural trauma are currently lacking, there are data from the Department for Transport to suggest that a significantly higher proportion of RTC casualties occurs on rural roads.20 Further analysis of the demographic details of admissions, including postcode or place of residence, with accurate catchment populations will allow more firm conclusions to be generated from the difference in incidence rate of trauma admissions at BSUH and SGU.
Neither of the MTCs in our study reached the minimum of 400 major trauma patients per year to maintain the experience and clinical competency in trauma care suggested by the Intercollegiate Group on Trauma Standards (published prior to the creation of trauma systems in UK).21 This recommendation was based on US volume–outcome trauma data from Nathens and Jurkovich,22 which has since been cast into doubt by a more recent US study23 and a TARN audit,24 both showing no relationship between trauma volume and outcome. The TARN audit of patient volume and outcomes has not been repeated since the implementation of the UK trauma networks, and a reaudit may be required.24
Our findings largely concur with the current literature. The safety of hospital care and acute trauma care out of hours have both been of recent media and political interest.9–12 Consequently, the majority of research on time of trauma admission has examined caseload by ‘working hours’ versus ‘out of hours’ rather than by hour of admission. This makes direct comparison with our study challenging.
An analysis of three years of national TARN data (almost 40,000 patients) by Guly et al revealed that the majority of major trauma admissions occurred ‘out of hours’ (defined as outside 9am – 5pm, Monday to Friday).7 The 2007 National Confidential Enquiry into Patient Outcome and Death review of major trauma also found that more admissions occurred at night (6pm – 8am) than during the day.8 The majority of the international literature, mainly from North America, supports our SGU findings. Ovadia et al25 and Carmody et al26 found that more trauma admissions occurred in the evening and overnight than during the day while Laupland et al found that over 70% of major trauma admissions in Canada occurred between 6pm and 8am.27
Some of the literature is in agreement with our BSUH findings. Robertson and Giannoudis studied five years of Leeds trauma admission data, and observed that over 50% of major trauma admissions occurred between 8am and 6pm.28 A large study of over 600,000 US trauma admissions from the National Trauma Data Bank® (NTDB) found that more admissions occur during the day (6am – 6pm) than in the evening or overnight,29 which is in agreement with the BSUH results. Data entry for the NTDB is voluntary and may therefore not accurately represent the true temporal pattern of trauma admissions. Furthermore, owing to different geographical and population characteristics, it is difficult to compare regional or international findings with those in the present study.
There are a number of possible contributing factors to the higher trauma admissions in the evening observed at SGU. The increased incidence and severity of RTCs at lower light levels is likely to have contributed to this.30 While little evidence directly links increased incidence of alcohol related injury in the evening and increased trauma admissions, given that alcohol is estimated to be involved in a considerable proportion of injuries and its use is more common in the evening, this seems a reasonable hypothesis.31–33 The cause of higher admissions in the afternoon for BSUH is not immediately clear. Analysis of the demographics and mechanisms of injury associated with these admissions may provide an explanation.
Median ISS was highest in the early morning (12.00am – 5.59am) and dropped through the rest of the day at BSUH but there was no significant variation in median ISS by time of admission observed at SGU. Very little has been published in the literature on ISS by time of day. The only data are from the study by Vaziri et al using the US NTDB, which observed an increase in the ISS of trauma admissions in the early hours.34 The increased injury severity seen in the early hours may be due to an increased severity of RTCs during this time, with driving speed, alcohol use and fatigue all thought to contribute.30,35 Further analysis of the mechanism of injury associated with the BSUH admissions would be required for any conclusions to be drawn.
Regarding weekend admissions, our study is in agreement with most of the current literature on trauma admissions in the UK and abroad.8,26,27,36,37 BSUH and SGU both had proportionally more trauma admissions at the weekend than on weekdays.
Our study found no significant difference in median ISS or in the proportion of severely injured patients (ISS >24) between weekday and weekend admissions. There is currently no research from the UK that has specifically analysed ISS by weekdays versus weekend. The literature from the US is based on single centre studies and does not reach a consensus; some research has suggested that trauma patients admitted at the weekend have a higher ISS than weekday admissions while other research has found no significant differences in ISS.26,36
It has been hypothesised that more outdoors activity occurs at the weekend and this may increase the incidence of trauma.37 As mentioned above, not much has been published on alcohol associated trauma admissions in the UK. However, considering the role of alcohol in a considerable number of injuries and an increase in alcohol intake at the weekend, it seems reasonable that alcohol associated injury contributes to an increase in weekend trauma admissions.31–33 National data show that more RTC casualties occur on weekdays than at the weekend,20 negating this as a possible cause. There is likely to be regional variation and further analysis of the injury mechanism of our admissions would provide better insight.
Seasonal variation
Weather is thought to play a significant role in the seasonal variation in trauma admissions. Hours of sunshine,37 increased maximum temperature,37–41 decreased minimum temperature,37 precipitation37,39,42 and snowfall37 have all been correlated positively with trauma admissions in the literature.
Our study observed that BSUH trauma admission volume exhibited significant seasonal variation. The highest volume of trauma admissions occurred in summer and autumn, with a trough during the winter months. No significant seasonal variation was noted for the trauma caseload at SGU. The median ISS did not vary significantly by season for either MTC.
Seasonal variation in trauma admissions is well documented in the literature, both in the UK and abroad, with the highest volumes of trauma admissions seen during the summer months.37,38,40,43 For this reason, care providers in the West Country have strategies in place to cope with these influxes resulting from their seasonal population fluctuations.
A large UK study by Parsons et al analysing national TARN data alongside weather variables noted increased admissions in the winter months, possibly due to ice and snowfall.37 They hypothesised that the increase in admissions observed in their data was because adults in the UK are less likely to alter their normal activities in relation to cold weather. US data show lower trauma volumes in the winter months, which is assumed to be the result of a ‘siege mentality’ and reduced outdoors activity during poor weather.38,42,44 There is currently no literature with which to compare our findings on patterns of injury severity by season.
The cause of the seasonal variation in trauma admissions at BSUH is not immediately clear. An increased number of daylight hours and an increased temperature during the summer, with the resulting increase in outdoors activity, are likely to contribute. An alternative hypothesis is linked with tourism. Brighton is well known as a domestic and foreign tourist destination, with over 8 million visitors per year.45 The population of Brighton is thought to nearly double during the summer months and this may contribute to the increased trauma admissions seen during this time. The reduced number of BSUH trauma admissions during the winter months in the present study is in contrast to the results of the abovementioned study by Parsons et al37 but may be due to the reduced outdoors activity described in the US trauma literature.38,42,44
The cause of the peak in BSUH trauma admissions observed during autumn (October in particular) is not clear and our data do not fit with the general patterns described in the literature. The lack of variation observed in SGU trauma volume may be due to the local population being less affected by tourism or by changes in weather conditions. Alternatively, it may be that while total trauma volume does not change by season, the case mix in terms of mechanism of injury does. Further analysis of injury mechanism, meteorological and demographic information including place of residence is required to support these hypotheses.
Implications
This study has important implications for trauma associated resources for prehospital care (including the regional air ambulance services), MTC care (capacity of resuscitation facilities, access to imaging, critical care, polytrauma operating theatres) and rehabilitation (including repatriation to the patient's local trauma unit). Sufficient surge capacity of resources and staffing is required at each step of the patient pathway to cater for the volume and severity of trauma admissions, to ensure patient safety and to provide the best standard of care.
It is likely that the best standards of care would be provided with experienced staff involved in trauma care available at all times, particularly during the evenings and at weekends. This will add to the challenge of trauma care planning, procurement and commissioning. There is considerable difficulty in ensuring the provision of appropriately qualified staff during the day and out of hours within the constraints of the European Working Time Regulations and funding. Given the integral role of MTCs in training and teaching, training posts must also be considered.
Our study has demonstrated that ‘one size does not fit all’ when planning resources for MTCs and the MTC catchment population may not provide an accurate estimate of the trauma volume. Instead, planning should cater to the regional patterns of admission. It would be premature to recommend changing staffing or resource patterns by time of day, by weekdays versus weekend or by season based solely on this study. However, these temporal factors should be considered with further analysis of demographics, mechanism of injury, resource use and outcomes to identify any shortcomings in the provision of care so that valuable information can be provided for future trauma care planning. We highly recommend that all MTCs review local data to ensure they are aware of their own temporal variation in major trauma admissions, and can plan their workforce and resources accordingly.
Study limitations
As has been noted in previous work on single centre or regional trauma data, the findings of this study may be only partially translatable to other regions or nations. In the future, the pattern of admissions may alter as additional medical resources become centralised.
TARN does not collect data on victims of trauma who die from their injuries before arriving at hospital. Although these cases are unlikely to significantly impact on our findings or to cause significant use of hospital resources, it should be noted that they are likely to require prehospital services. The volume of trauma admissions in the present study may therefore not correctly represent the workload for trauma associated prehospital services.
Limited demographic information has been provided in this paper for the sake of brevity but the data have been collected and will be analysed in the future. This will assist with developing local injury prevention campaigns and services.
TARN data only include patients who have been admitted for 72 hours. There will therefore be a proportion of patients who are admitted and discharged with successfully treated significant injuries before this time.
Conclusions
This study observed significant variation in trauma caseload and ISS by time of admission, by weekdays versus weekend and by season in the context of two large MTCs. Although there were some similarities, both MTCs had individual temporal patterns of admissions. The results of this study have important implications for resource planning, procurement and training. This study also demonstrates the requirement for further analysis of TARN data on a regional and national level.
Acknowledgement
The authors would like to thank Stephanie Goubet for providing statistical advice.
References
- 1.Leading Causes of Death. Office for National Statistics http://www.ons.gov.uk/ons/rel/vsob1/mortality-statistics--deaths-registered-in-england-and-wales--series-dr-/2012/info-causes-of-death.html (cited November2015).
- 2.Murray CJ, Vos T, Lozano R et al. . Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; : 2,197–2,223. [DOI] [PubMed] [Google Scholar]
- 3.National Audit Office Major Trauma Care in England. London: NAO; 2010. [Google Scholar]
- 4.Independent Review of Major Trauma Networks Reveals Increase in Patient Survival Rates NHS England. http://www.england.nhs.uk/2013/06/25/incr-pati-survi-rts/ (cited November2015).
- 5.NHS Improving Quality NHS Services – Open Seven Days a Week: Every Day Counts. London: NHS IQ; 2013. [Google Scholar]
- 6.Aylin P, Yunus A, Bottle A et al. . Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 2010; : 213–217. [DOI] [PubMed] [Google Scholar]
- 7.Guly HR, Leighton G, Woodford M et al. . The effect of working hours on outcome from major trauma. Emerg Med J 2006; : 276–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Confidential Enquiry into Patient Outcome and Death Trauma: Who Cares? London: NCEPOD; 2007. [Google Scholar]
- 9.National Confidential Enquiry into Patient Outcome and Death Emergency Admissions: A Journey in the Right Direction? London: NCEPOD; 2007. [Google Scholar]
- 10.Royal College of Physicians Acute Medical Care. London: RCP; 2007. [Google Scholar]
- 11.Royal College of Surgeons of England Emergency Surgery. London: RCS; 2011. [Google Scholar]
- 12.Royal College of Physicians Delivering a 12-hour, 7-day Consultant Presence on the Acute Medical Unit. London: RCP; 2012. [Google Scholar]
- 13.D15. Major Trauma NHS England; http://www.england.nhs.uk/commissioning/spec-services/npc-crg/group-d/d15/ (cited November2015). [Google Scholar]
- 14.Trauma and Orthopaedics Brighton and Sussex University Hospitals NHS Trust. http://www.bsuh.nhs.uk/departments/trauma-and-orthopaedics/ (cited November2015).
- 15.Major Trauma Centre. St George's University Hospitals NHS Foundation Trust http://www.stgeorges.nhs.uk/service/emergency/major-trauma-centre/ (cited November2015).
- 16.Trauma Audit and Research Network Procedures Manual. Manchester: TARN; 2014. [Google Scholar]
- 17.Baker SP, O'Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; : 187–196. [PubMed] [Google Scholar]
- 18.Myers SR, Branas CC, French BC et al. . Safety in numbers: are major cities the safest places in the United States? Ann Emerg Med 2013; : 408–418.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark DE, Cushing BM. Rural and urban traffic fatalities, vehicle miles, and population density. Accid Anal Prev 2004; : 967–972. [DOI] [PubMed] [Google Scholar]
- 20.Department for Transport Reported Road Casualties Great Britain: 2012. London: Department for Transport; 2013. [Google Scholar]
- 21.Intercollegiate Group on Trauma Standards Regional Trauma Systems. London: RCS; 2009. [Google Scholar]
- 22.Nathens AB, Jurkovich GJ, Maier RV et al. . Relationship between trauma center volume and outcomes. JAMA 2001; : 1,164–1,171. [DOI] [PubMed] [Google Scholar]
- 23.Glance LG, Osler TM, Dick A, Mukamel D. The relation between trauma center outcome and volume in the National Trauma Databank. J Trauma 2004; : 682–690. [DOI] [PubMed] [Google Scholar]
- 24.Wang W, Dillon B, Bouamra O. An analysis of hospital trauma care performance evaluation. J Trauma 2007; : 1,215–1,222. [DOI] [PubMed] [Google Scholar]
- 25.Ovadia P, Szewczyk D, Walker K et al. . Admission patterns of an urban level I trauma center. Am J Med Qual 2000; : 9–15. [DOI] [PubMed] [Google Scholar]
- 26.Carmody IC, Romero J, Velmahos GC. Day for night: should we staff a trauma center like a nightclub? Am Surg 2002; : 1,048–1,051. [PubMed] [Google Scholar]
- 27.Laupland KB, Ball CG, Kirkpatrick AW. Hospital mortality among major trauma victims admitted on weekends and evenings: a cohort study. J Trauma Manag Outcomes 2009; : 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robertson A, Giannoudis PV. Excessive volume of trauma workload out of hours: is it really true? Injury 2004; : 864–868. [DOI] [PubMed] [Google Scholar]
- 29.Egol KA, Tolisano AM, Spratt KF, Koval KJ. Mortality rates following trauma: the difference is night and day. J Emerg Trauma Shock 2011; : 178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plainis S, Murray IJ, Pallikaris IG. Road traffic casualties: understanding the night-time death toll. Inj Prev 2006; : 125–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor B, Irving HM, Kanteres F et al. . The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend 2010; : 108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacLeod JB, Hungerford DW. Alcohol-related injury visits: do we know the true prevalence in US trauma centres? Injury 2011; : 922–926. [DOI] [PubMed] [Google Scholar]
- 33.Health and Social Care Information Centre Statistics on Alcohol: England, 2013. Leeds: HSCIC; 2013. [Google Scholar]
- 34.Vaziri K, Roland JC, Robinson L, Fakhry SM. Optimizing physician staffing and resource allocation: sine-wave variation in hourly trauma admission volume. J Trauma 2007; : 610–614. [DOI] [PubMed] [Google Scholar]
- 35.Taylor MC, Lynam DA, Baruya A. The Effects of Drivers' Speed on the Frequency of Road Accidents. Crowthorne: Transport Research Laboratory; 2000. [Google Scholar]
- 36.Carr BG, Jenkins P, Branas CC et al. . Does the trauma system protect against the weekend effect? J Trauma 2010; : 1,042–1,047. [DOI] [PubMed] [Google Scholar]
- 37.Parsons N, Odumenya M, Edwards A et al. . Modelling the effects of the weather on admissions to UK trauma units: a cross-sectional study. Emerg Med J 2011; : 851–855. [DOI] [PubMed] [Google Scholar]
- 38.Bhattacharyya T, Millham FH. Relationship between weather and seasonal factors and trauma admission volume at a Level I trauma center. J Trauma 2001; : 118–122. [DOI] [PubMed] [Google Scholar]
- 39.Abe T, Tokuda Y, Ohde S et al. . The influence of meteorological factors on the occurrence of trauma and motor vehicle collisions in Tokyo. Emerg Med J 2008; : 769–772. [DOI] [PubMed] [Google Scholar]
- 40.Friede KA, Osborne MC, Erickson DJ et al. . Predicting trauma admissions: the effect of weather, weekday, and other variables. Minn Med 2009; : 47–49. [PubMed] [Google Scholar]
- 41.Stomp W, Fidler V, ten Duis HJ, Nijsten MW. Relation of the weather and the lunar cycle with the incidence of trauma in the Groningen region over a 36-year period. J Trauma 2009; : 1,103–1,108. [DOI] [PubMed] [Google Scholar]
- 42.Rising WR, O'Daniel JA, Roberts CS. Correlating weather and trauma admissions at a level I trauma center. J Trauma 2006; : 1,096–1,100. [DOI] [PubMed] [Google Scholar]
- 43.Atherton WG, Harper WM, Abrams KR. A year's trauma admissions and the effect of the weather. Injury 2005; : 40–46. [DOI] [PubMed] [Google Scholar]
- 44.Fantus RJ, Fildes J. Trauma season. Bull Am Coll Surg 2006; : 58–59. [PubMed] [Google Scholar]
- 45.Brighton and Hove City Council The City's Approach to Tourism. Brighton: Brighton and Hove City Council; 2010. p27. [Google Scholar]