Abstract
Introduction
Volar locking plates are used to treat unstable and displaced fractures of the distal radius. Potential advantages of stable anatomical reduction (eg early mobilisation) can be limited by penetration of dorsal screws, leading to synovitis and potential rupture of extensor tendons.
Despite intraoperative imaging, penetration of dorsal screws continues to be a problem in volar plating of the distal radius. Ultrasound is a well recognised, readily available, diagnostic tool used to assess soft-tissue impingement by orthopaedic hardware.
In this cadaveric study, we wished to ascertain the sensitivity and specificity of ultrasound for identification of protrusion of dorsal screws after volar plating of the distal radius.
Methods
Four adult, unpaired phenol-embalmed cadaveric distal radii were used. A VariAx™ Distal Radius Volar Locking Plate system (Stryker, Kalamazoo, MI, USA) was employed for instrumented fixation. A portable SIUI CTS 900 ultrasound machine (Providian Medical, Eastlake, OH, USA) was used to image the dorsal cortex to ascertain screw penetration.
Results
Specificity and sensitivity of ultrasound for detection of screw protrusion through the dorsal cortex was 100%.
Conclusions
Ultrasound was found to be a safe and accurate method for assessment of dorsal-screw penetration through the dorsal cortex of the radius after volar plating of the distal radius. It also aids diagnosis of associated tendon disorders (eg tenosynovitis) that might cause pain and limit wrist function.
Keywords: Ultrasound, Radius, Dorsal screws, Volar plates
Percutaneous pinning and plastering are established treatments for dorsally displaced fractures of the distal radius.1–3 Fixation using volar plates is first-line treatment for unstable intra-articular or extra-articular distal fractures of the radius.4–10 Penetration of the dorsal cortex leading to irritation or attrition of extensor tendons is a complication of fixation using volar plates.12–21
Screws can compromise the volume of the dorsal compartments. Chronic conflict between tendons and screws can result in local hyperaemia, tenosynovitis, and persistent impingement, eventually leading to tendon rupture.21–23 Prevalence of tendon-related problems (irritation and tears) is 2–14%.12,13,15 In a meta-analysis, Margaliot et al 22 reported the prevalence of tendon rupture to be 2.6% and that of tenosynovitis to be 5.2%. These values can lead to poor outcomes despite satisfactory reduction and fixation of fractures, as well as a delay to return to work in young, active patients.16
Conflict between orthopaedic hardware and soft tissue is difficult to visualise on standard radiographs owing to: overlying bone;21,24 static nature of images; insufficient contrast for soft tissues; absence of real-time correlation between pain and the structures being observed. Ultrasound eliminates all of these problems and also offers excellent spatial resolution.21
We use ultrasound in the outpatient clinic to identify screw penetration of the dorsal cortex after volar plating of fractures of the distal radius. This simple test can be done with minimal training, and could be used to reduce the need for computed tomography (CT) and, as such, radiation exposure and cost. With the ready availability of sterile ultrasound units in theatres, this test could be done intraoperatively for difficult cases.
In this cadaveric study, we wished to ascertain the sensitivity and specificity of ultrasound for identification of protrusion of dorsal screws after volar plating of the distal radius.
Methods
Four adult, unpaired phenol-embalmed cadaveric distal radii were used. A VariAx™ Distal Radius Volar Locking Plate system (Stryker, Kalamazoo, MI, USA) was employed for instrumented fixation. Plates are contoured anatomically and have four options for variable-angle distal locking screws that allow for 15° of freedom. A portable SIUI CTS 900 ultrasound machine (Providian Medical, Eastlake, OH, USA) was used to image the dorsal cortex for screw penetration.
The volar aspect of four cadaveric distal radii was exposed using a modified version of Henry's approach. The pronator quadratus was exposed through the bed of the flexor carpi radialis tendon. Then, the pronator quadratus was reflected from its radial insertion.
Plates were applied to the volar cortex of the distal radius (just proximal to the watershed line) and fixed with a single cortical non-locked screw in the distal diaphysis. Distal screw holes were numbered from one to four starting from the ulna side (Fig 1).
Figure 1.
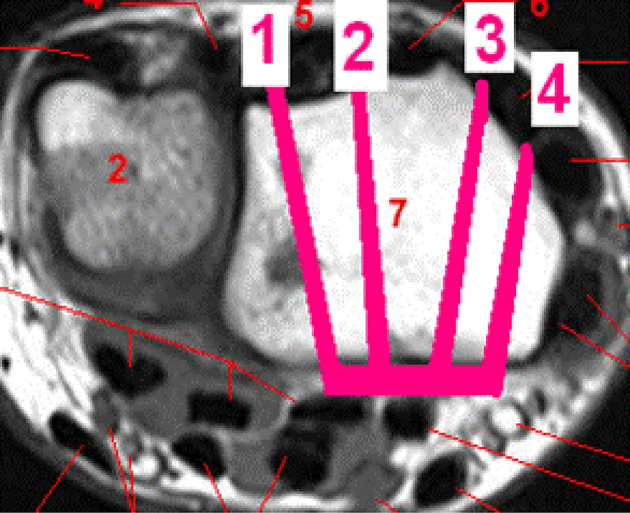
The volar cortex of the distal radius was divided into four zones from medial (ulnar) to lateral
Bi-cortical holes were drilled sequentially through the locking holes in the distal row of the plate without fluoroscopic guidance. The optimum length of each screw was measured using a standard depth gauge from Stryker VariAx instrumentation. Then, locking screws (2.3mm) were inserted at different lengths into all four distal locking holes. Screws were inserted at –2mm to the measured depth in cadaver specimen number (CSN)1, at 0mm in CSN2, at +2mm in CSN3, and at +4mm in CSN4.
Using the SIUI CTS 900 ultrasound machine, the dorsal surface of the wrist was imaged to detect the site (extensor compartment) and length of screw penetration. Figure 2 shows a typical appearance of a screw penetrating the dorsal cortex. Ultrasound findings for each specimen were recorded.
Figure 2.

Ultrasound image showing screw penetration just radial to Lister's tubercle as a hyperechoic structure
Cadaveric specimens were dissected in the dorsal plane to identify and quantify screw penetration. Penetration of the extensor compartment and screw length were recorded.
Results
In CSN1, the depth was measured and screws were inserted 2mm short of the measured depth. No screws were found to be prominent of the dorsal cortex upon ultrasound or dissection. Upon dissection, the most ulnar-directed screw was found to have penetrated the distal radioulnar joint (DRUJ) but this phenomenon was not detected on ultrasound.
In CSN2, the screw lengths selected were the same as the measured depth. Ultrasound detected one screw in the second extensor compartment that was prominent by 1mm, and this phenomenon was confirmed upon dissection. Dissection also revealed that one screw had penetrated the radiocarpal joint (RCJ) (Fig 3): this phenomenon was not detected on ultrasound.
Figure 3.

Axial CT of same patient in Figure 2 demonstrating screw penetration through the dorsal cortex of the distal radius just radial to Lister's tubercle
Figure 4.

Screw protrusion in the radiocarpal joint upon dissection
In CSN3, 2mm-longer screws were inserted. Three of the four screws were prominent upon ultrasound and the fourth screw was at the level of dorsal cortex in extensor compartment four.
In CSN4, screws were inserted 4mm-longer than the measured depth. Three of the four screws were found to be long on ultrasound and dissection (Fig 5). All results are summarised in Table 1.
Figure 5.
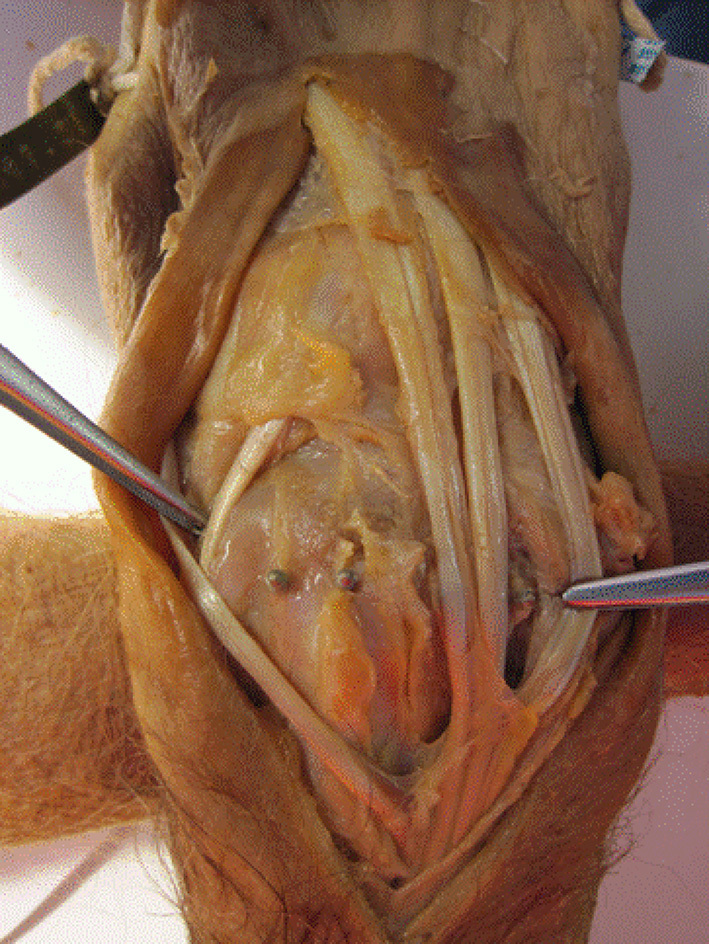
Screw prominence revealed upon dissection
Table 1.
Ultrasound and dissection findings in cadavers using different screw lengths
| Cadaver specimen number | Screw length* (mm) | Ultrasound protrusion (mm) | Dissection prominence | Extensor zone |
|---|---|---|---|---|
| 1 (2mm–shorter screw) | –2 | 0 | 0 | DRUJ |
| –2 | 0 | 0 | ||
| –2 | 0 | 0 | ||
| –2 | 0 | 0 | ||
| 2 (normal–length screw) | 0 | 0 | 0 | RCJ |
| 0 | 0 | 0 | ||
| 0 | 0 | 0 | ||
| 0 | 1 | 1 | ||
| 3 (2mm–longer screw) | +2 | 1 | 1 | 4 |
| +2 | 0 | 0 | ||
| +2 | 3 | 3 | 3 (in EPL groove) | |
| +2 | 0 | 0 | ||
| 4 (4mm–longer screw) | +4 | 4 | 3 | 4 |
| +4 | 0 | 0 | ||
| +4 | 4 | 4 | 2 | |
| +4 | 4 | 5 | 1 |
Screws inserted in order 1–4 as shown in Fig 1.
DRUJ, distal radioulnar joint; EPL, extensor pollicis longus; RCJ, radiocarpal joint
Specificity of ultrasound at detection of prominent screws was 100%. No screws were classified as ‘prominent‘ upon ultrasound and found subsequently not to be prominent upon dissection. Sensitivity of ultrasound was 100% for dorsal penetration of screws. One screw was found in the RCJ and another screw penetrated into the DRUJ, but this was not prominent beyond the dorsal cortex. We expect these to be picked up by fluoroscopy intra operatively. We did not use fluoroscopy for our cadaveric study. We wished only to investigate prominence of dorsal screws on ultrasound and correlate findings by dorsal dissection.
Discussion
The complex geometry of the dorsal cortex of the distal radius makes confirmation of screw length with fluoroscopic or standard radiographic imaging methods quite difficult.24–26 Protrusion of distal locking screws on the dorsum of the distal radius can lead to attrition and rupture of extensor tendons.15,16,27–30 and hence reduced function, pain and disability
The dorsal tangential view31,32 has been adopted in many UK centres (including our unit) to assess screw length intraoperatively, and often results in a change of screw. Nevertheless, whether routine use can reduce the prevalence of penetration of dorsal screws is not known. The ‘gold standard’ for assessment of long screws is CT but is not practical intraoperatively as well as being time-consuming, expensive and exposes the patient to radiation. Ultrasound has two advantages for assessment of penetration of dorsal screws: (i) allows for dynamic examination; (ii) can be used if hardware limits use of magnetic resonance imaging.17,31,32 The screw appears as a hyperechoic structure created by multiple, parallel, oblique echogenic lines that correspond to the screw thread (Figure 2). Figure 3 shows similar pathology on axial CT.
Bianchi et al17 used ultrasound to detect penetration of dorsal screws after fixation of the distal radius using a volar plate. The diagnosis was confirmed surgically in all nine patients who had fixation using a volar plate. They correlated the ultrasound appearance in vitro with appearance of a protruding screw tip as multiple hyperechoic lines in vivo, similar to our findings. They concluded that, apart from detection of dorsal-screw penetration, ultrasound offers the added advantage of the diagnosis of tears to the extensor tendon and tendon disorders such as tenosynovitis.
Tenosynovitis can also affect outcomes after volar plating. Ultrasound has the advantage of detection of this disorder14,17 (though this is operator-dependent). Thus, ultrasound can be helpful for the detection of associated tendon disorders, which can limit functional recovery of distal-radius fractures. In their clinical and cadaveric study, De Maeseneer et al33 showed that ultrasound can be used to diagnose tears of the extensor pollicis longus, and similar findings were noted by Santiago et al in their comparative study.34
We found that the sensitivity and specificity of ultrasound was 100% for the detection of penetration of dorsal screws after volar plating in fractures of the distal radius. Importantly, no screws were identified as being ‘long’ when they were in fact not prominent. These findings suggest that, if screws are found to be prominent on ultrasound, then undertaking CT before elective removal of hardware is not necessary.
Intra-articular penetration of screws occurred in our study because screws were placed without fluoroscopic guidance. Ultrasound could not be used to identify these screws as being intra-articular. We did not attempt to identify screws within the joint, but one would expect these screws to be readily identifiable using standard fluoroscopic views intraoperatively. Ultrasound can complement fluoroscopic views obtained intraoperatively, and its use may be helpful in difficult cases.
The method described here is an accurate and cost-effective way of identification of penetration of dorsal screws after volar plating of the distal radius. It could be used as a simple screening method to complement clinical examination in the outpatient setting.
Conclusion
Ultrasound is a quick, inexpensive and a non-traumatic imaging method that allows assessment of tendons and measurement of protruding dorsal screws. This method is simple, safe, can be undertaken with minimal training, and could be used for the early diagnosis of dorsal-screw prominence, thereby reducing the need for CT.
Acknowledgement
We thank Dr Catherine Molyneux, Director of Anatomical Studies, for providing the cadavers and the facilities within the department of Anatomy.
References
- 1.Karantana A, Davis TRC. Extra-articular fractures of the distal radius – a European view point. Hand Clin 2012; : 145–150. [DOI] [PubMed] [Google Scholar]
- 2.Costa ML, Achten J, Parsons NR et al. UK DRAFFT – a randomised controlled trial of percutaneous fixation with kirschner wires versus volar locking-plate fixation in the treatment of adult patients with a dorsally displaced fracture of the distal radius. BMC Musculoskelet Disord 201; : 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am 2009; : 1,837–1,846. [DOI] [PubMed] [Google Scholar]
- 4.Esposito J, Schemitsch EH, Saccone M, Sternheim A. External fixation versus open reduction with plate fixation for distal radius fractures: a meta-analysis of randomised controlled trials. Injury 2013; : 409–416. [DOI] [PubMed] [Google Scholar]
- 5.Jeudy J, Steiger V, Boyer P, Cronier P, Bizot P. Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation “versus” locked volar plating. Injury 2012; : 174–179. [DOI] [PubMed] [Google Scholar]
- 6.Karantana A, Downing ND, Forward DP. Surgical treatment of distal radial fractures with a volar locking plate versus conventional percutaneous methods a randomized controlled trial. J Bone Joint Surg Am 2013; : 1,737–1,744. [DOI] [PubMed] [Google Scholar]
- 7.Gomez–Rice A, Villarrubia E, Bau A. Methodological issues of: should unstable extra-articular distal radial fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomised controlled trial. Injury 2012; : 1,219–1,222. [DOI] [PubMed] [Google Scholar]
- 8.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg 2006; : 2,687–2,694. [DOI] [PubMed] [Google Scholar]
- 9.Twigt B, Bemelman M, Lansink K, Leenen L. Type C distal radial fractures treated with conventional AO plates: an easy and cost-saving solution in a locking plate era. Int Orthop 2013; : 483–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murakami K, Abe Y, Takahashi K. Surgical treatment of unstable distal radius fractures with volar locking plates. J Orthop Sci 2007; : 134–140. [DOI] [PubMed] [Google Scholar]
- 11.Hull P, Baraza N, Gohil M et al. Volar locking plates versus K-wire fixation of dorsally displaced distal radius fractures – a functional outcome study. J Trauma 2011; : E125–E128. [DOI] [PubMed] [Google Scholar]
- 12.Obert L, Rey P-B, Uhring J et al. Fixation of distal radius fractures in adults: a review. Orthop Traumatol Surg Res 2013; : 216–234. [DOI] [PubMed] [Google Scholar]
- 13.Wang J, Yang Y, Ma J et al. Open reduction and internal fixation versus external fixation for unstable distal radial fractures: a meta-analysis. Orthop Traumatol Surg Res 2013; : 321–331. [DOI] [PubMed] [Google Scholar]
- 14.De Maeseneer M, Marcelis S, Osteaux M, Jager T, Machiels F, Van Roy P. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. Am J Roentgenol 2005; : 175–179. [DOI] [PubMed] [Google Scholar]
- 15.Hattori Y, Doi K, Sakamoto S, Yukata K. Delayed rupture of extensor digitorum communis tendon following volar plating of distal radius fracture. Hand Surg 2008; : 183–185. [DOI] [PubMed] [Google Scholar]
- 16.Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (NY) 2007; : 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bianchi S, van Aaken J, Glauser T, Martinoli C, Beaulieu J-Y, Santa DD. Screw impingement on the extensor tendons in distal radius fractures treated by volar plating: sonographic appearance. Am J Roentgenol 2008; : W199–W203. [DOI] [PubMed] [Google Scholar]
- 18.Cho N-Y, Seo C-Y, Kim M-S, Kim H-S, Lee K-B. Extensor pollicis longus rupture after distal radius fracture. J Korean Fracture Soc 2012; : 52–57. [Google Scholar]
- 19.Bianchi S, van Aaken J, Glauser T, Martinoli C, Beaulieu J-Y, Santa Della D. Screw Impingement on the Extensor Tendons in Distal Radius Fractures Treated by Volar Plating: Sonographic Appearance. http://dxdoiorg/102214/AJR081057 American Roentgen Ray Society; 2012. November 23;:W199–W203. [DOI] [PubMed] [Google Scholar]
- 20.Sügün TS, Karabay N, Gürbüz Y, Ozaksar K, Toros T, Kayalar M. Screw prominences related to palmar locking plating of distal radius. J Hand Surg Eur Vol 2011; : 320–324. [DOI] [PubMed] [Google Scholar]
- 21.Guillin R, Bianchi S. Sonographic assessment of orthopedic hardware impingement on soft tissues of the limbs. J Ultrasound 2012; : 50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Margaliot Z, Haase SC, Kotsis SV, Kim HM, Chung KC. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg 2005; : 1,185.e1–1,185.e17. [DOI] [PubMed] [Google Scholar]
- 23.Pichler W, Windisch G, Schaffler G, Rienmüller R, Grechenig W. Computer tomography aided 3D analysis of the distal dorsal radius surface and the effects on volar plate osteosynthesis. J Hand Surg Eur Vol 2009; : 598–602. [DOI] [PubMed] [Google Scholar]
- 24.Thomas AD, Greenberg JA. Use of fluoroscopy in determining screw overshoot in the dorsal distal radius: a cadaveric study. J Hand Surg Am 2009; : 258–261. [DOI] [PubMed] [Google Scholar]
- 25.Sügün TS, Karabay N, Gürbüz Y, Ozaksar K, Toros T, Kayalar M. Screw prominences related to palmar locking plating of distal radius. J Hand Surg Eur Vol. 2011. May;: 320–4. [DOI] [PubMed] [Google Scholar]
- 26.Park DH, Goldie BS. Volar plating for distal radius fractures – do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg 2012; : 169–172. [DOI] [PubMed] [Google Scholar]
- 27.Failla JM, Koniuch MP, Moed BR. Extensor pollicis longus rupture at the tip of a prominent fixation screw: report of three cases. J Hand Surg Am 1993; : 648–651. [DOI] [PubMed] [Google Scholar]
- 28.Benson EC, DeCarvalho A, Mikola EA et al. Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res 2006; : 218–222. [DOI] [PubMed] [Google Scholar]
- 29.Al-Rashid M, Theivendran K, Craigen MA. Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg Br 2006; : 1,610–1,612. [DOI] [PubMed] [Google Scholar]
- 30.Wong-Chung J, Quinlan W. Rupture of extensor pollicis longus following fixation of a distal radius fracture. Injury 1989; : 375–376. [DOI] [PubMed] [Google Scholar]
- 31.Ozer K, Toker S. Dorsal tangential view of the wrist to detect screw penetration to the dorsal cortex of the distal radius after volar fixed-angle plating. Hand (NY) 2011; : 190–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am 2012; : 963–967. [DOI] [PubMed] [Google Scholar]
- 33.De Maeseneer M, Marcelis S, Osteaux M, Jager T, Machiels F, Van Roy P. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. AJR Am J Roentgenol. 2005. January; : 175–9. [DOI] [PubMed] [Google Scholar]
- 34.Santiago FR, Plazas PG, Fernández JM. Sonography findings in tears of the extensor pollicis longus tendon and correlation with CT, MRI and surgical findings. Eur J Radiol 2008; : 112–126. [DOI] [PubMed] [Google Scholar]


