Abstract
Introduction
The National Institute for Health and Care Excellence (NICE) currently recommends the use of total hip replacement (THR) for displaced intracapsular hip fractures in patients who meet certain mobility, cognitive and health criteria.
Methods
A multicentre prospective audit was conducted within a defined geographic region to assess current practice and variation in provision of THR for displaced intracapsular hip fractures.
Results
A total of 879 patients with hip fractures, admitted to 8 acute trauma units, were included in this study. Of 462 patients with displaced intracapsular hip fractures, 169 fulfilled the NICE criteria for THR. THR was performed for only 49 of (29%) the eligible patients.
There was significant variation in THR provision between the eight units (0% to 50% THR usage, p<0.001). There were statistically significant differences in age, ASA (American Society of Anesthesiologists) grade, abbreviated mental test score and walking ability prior to the injury between patients who underwent fixation, THR or hemiarthroplasty (all p≤0.05). There was a significantly increased chance of not undergoing THR if a patient was older than 77 years (median age for the THR eligible cohort; relative risk [RR]: 7.9, 95% confidence interval [CI]: 2.8–22.0, p<0.001). There was also a trend for this with patients who were ASA grade 3 compared with ASA grade 1 or 2 (RR: 2.7, 95% CI: 1.0–7.3, p=0.06). The surgeons gave multifactorial reasons for not performing THR in eligible patients.
Conclusions
There is significant variation in the provision of THR for eligible hip fracture patients, which is influenced by both patient demographics and the unit to which a patient is admitted.
Keywords: Arthroplasty, Replacement, Hip fracture, Physician’s practice patterns
Arthroplasty following displaced intracapsular hip fracture is standard practice in the UK.1 Hemiarthroplasty is the procedure of choice, providing the usually low demand patients with good pain relief and satisfactory functional status as well as preventing the need for reoperation compared with internal fixation.2–4 For active patients, there are reports suggesting that total hip replacement (THR) confers better short-term benefits with improved clinical function, and longer term benefits with lower patient mortality, rates of revision and cost compared with hemiarthroplasty.5–7
Based on this evidence, the National Institute for Health and Care Excellence (NICE) strongly recommends the use of THR for displaced intracapsular hip fractures in cognitively competent patients who were independently mobile with the maximum use of one stick prior to their injury.8 This is similar to the criteria suggested in the British Orthopaedic Association’s ‘blue book’.9 Despite the recommendations, there are still reservations about THR performed for hip fracture, particularly regarding the risks of dislocation and the long-term clinical benefit.7,10–15
This study was performed to assess the practice and variation in the provision of THR for displaced intracapsular hip fractures in a defined geographic region. The reasons for not performing THR when a patient was deemed eligible based on the NICE criteria were also evaluated.
Methods
Eight trauma units (including two major trauma centres) in the North of England took part in this prospective trainee-led audit performed between October 2013 and April 2014. Each unit audited the management of 110 consecutive patients admitted with hip fractures. Audit standards were based on NICE guidelines and the National Hip Fracture Database report where the eligibility criteria for THR are an abbreviated mental test score (AMTS) of ≥8, ASA (American Society of Anesthesiologists) grade 3 or less and ability to walk outdoors with a maximum of one stick.8,16 Demographic details were recorded using a standard proforma. Information collected included age, sex, mobility and walking aid status prior to the injury, AMTS, ASA grade, fracture pattern and details of surgery. The only exclusion criterion applied to the collected data was to remove any patient aged under 18 years. Using this criterion, only one patient was excluded from the analysis.
The primary outcome was the proportion of THRs performed in the group of patients who met the eligibility criteria. When patients who met the criteria for THR did not undergo that procedure, the reason was recorded as free text.
Each hospital retained a local database before the final centralised anonymised analysis. All textual data were coded to allow identification of common themes. Statistical analysis was performed using Minitab® 17 (Minitab, Coventry, UK). A p-value of =0.05 was considered statistically significant.
This regional audit was registered with each individual hospital’s audit department prior to commencement of the project.
Results
A total of 879 patients (607 female, 272 male) were available for analysis, of whom 547 (62%) had sustained an intracapsular hip fracture. Of the cases in the intracapsular fracture group, 462 fractures (84%) were displaced. Among these, 169 patients (37%) met the criteria for THR (Table 1), which equates to 19% of the total hip fracture cohort. In the eight participating centres, the proportion of patients eligible for THR who subsequently underwent THR ranged from 0% to 50% (Table 2).
Table 1.
Demographics of patients in participating hospitals
| Hospital | Male | Female | Median age | ICNOF | Met THR criteria |
|---|---|---|---|---|---|
| A | 40 | 70 | 78 years | 72 | 14 (13%) |
| B | 34 | 76 | 81 years | 80 | 26 (24%) |
| C | 23 | 87 | 83 years | 67 | 18 (16%) |
| D | 38 | 71 | 81 years | 68 | 17 (16%) |
| E | 36 | 74 | 82 years | 61 | 27 (25%) |
| F | 38 | 72 | 82 years | 67 | 24 (22%) |
| G | 28 | 82 | 84 years | 65 | 16 (15%) |
| H | 35 | 75 | 82 years | 67 | 27 (25%) |
| Total | 272 | 607 | 82 years | 547 | 169 (19%) |
ICNOF = intracapsular neck of femur fracture; THR = total hip replacement
Table 2.
The proportion of total hip replacements (THRs) performed in patients who met the eligibility criteria
| Hospital | Patients | Type of operation | |
|---|---|---|---|
| Not THR | THR | ||
| A | 14 | 9 (64%) | 5 (36%) |
| B | 26 | 13 (50%) | 13 (50%) |
| C | 18 | 12 (67%) | 6 (33%) |
| D | 17 | 9 (53%) | 8 (47%) |
| E | 27 | 23 (85%) | 4 (15%) |
| F | 24 | 15 (63%) | 9 (38%) |
| G | 16 | 16 (100%) | 0 (0%) |
| H | 27 | 23 (85%) | 4 (15%) |
| Total | 169 | 120 (71%) | 49 (29%) |
In those cases in which THR was not performed, patients either underwent internal fixation or hip hemiarthroplasty. Table 3 shows the demographics of patients grouped by the operative intervention employed. This demonstrated there were statistically significant differences in patient age (p<0.001), ASA grade (p<0.001), walking ability (p=0.005) and AMTS between these groups (p=0.05).
Table 3.
Demographics for the 169 patients who fulfilled the criteria for THR by type of operation they eventually received
| Demographic | Type of operation | p-value | ||
|---|---|---|---|---|
| Fixation (n=27) | Hemiarthroplasty (n=93) | THR (n=49) | ||
| Median age in years | 55 (IQR: 49–64, range: 18–77) |
82 (IQR: 77–85, range: 48–94) |
71 (IQR: 64–76, range: 50–86) |
<0.001* |
| Sex Male Female |
12 (44%) 14 (56%) |
28 (30%) 65 (70%) |
17 (35%) 32 (65%) |
0.39** |
| ASA grade 1 2 3 |
12 (44%) 9 (33%) 6 (22%) |
5 (5%) 45 (48%) 43 (46%) |
5 (10%) 35 (71%) 9 (18%) |
<0.001** |
| Walking aids No aids One stick |
26 (96%) 1 (4%) |
68 (73%) 25 (27%) |
43 (88%) 6 (12%) |
0.005** |
| AMTS 8 9 10 |
1 (4%) 5 (19%) 21 (78%) |
14 (15%) 14 (15%) 65 (70%) |
1 (2%) 6 (12%) 42 (86%) |
0.05** |
THR = total hip replacement; IQR = interquartile range; ASA = American Society of Anesthesiologists; AMTS = abbreviated mental test score
Kruskal–Wallis test;
chi-squared test
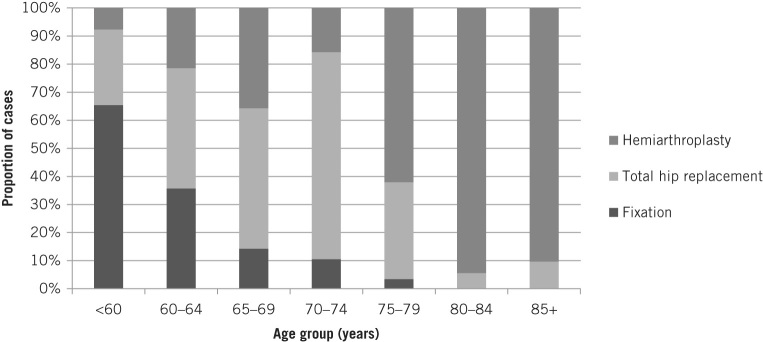
Figure 1 shows the types of surgery performed for patients who fulfilled the criteria for THR. Patients aged 70–74 years were most likely to undergo THR while those aged 80–84 years were least likely to have this procedure.
Figure 1.
Procedures performed for the 169 patients who fulfilled the criteria for total hip replacement
Where THR was performed (n=49), the cemented technique (n=42, 86%) was most commonly used, with cementless (n=1) and hybrid (n=2) implants used in a small number of cases. For the remaining four cases, the implants used were unknown. The posterior (n=24, 49%) and lateral (n=20, 41%) approaches were both commonly used. For the remaining five cases, the type of approach used was not known.
The Thompson hemiarthroplasty was used in all eight hospitals and was the preferred prosthesis (n=66) for hemiarthroplasty, followed by the Exeter Trauma Stem (Stryker, Newbury, UK; n=16) and Austin Moore (n=1) prostheses. A bipolar hemiarthroplasty prosthesis was used in ten patients. Twenty-seven patients underwent closed reduction and internal fixation of the displaced intracapsular hip fracture using either cannulated screws (n=14) or dynamic hip screws (n=13). These were chosen because of the patients’ young age (n=7, age range: 18–64 years), team decision (n=3, age range: 70–77 years), configuration of fracture (n=2, age range: 57–58 years) and patient’s request (n=1, age: 62 years). In 14 cases, the reasons were not known.
Analysing the textual data, the common themes given by surgeons for performing hemiarthroplasty in patients who fulfilled the criteria for THR were patients with advanced age, coexisting morbidities and surgeon’s preference (Table 4). This is consistent with the patient demographic data for each of the operative interventions shown in Table 3. Factors such as cognition and excessive alcohol intake, which may affect postoperative mobility and compliance, were also reported.
Table 4.
Reasons for performing hemiarthroplasty in patients who met the total hip replacement criteria
| Reasons | n | Notes |
|---|---|---|
| Advanced age | 22 | Age 80–94 years |
| Co-morbidities / combinations of medical issues | 21 | |
| Surgeon’s preference | 10 | Age 76–88 years |
| Falls / balance, epilepsy, alcohol | 7 | |
| Acute medical issues | 3 | |
| No lower limb arthroplasty surgeon | 3 | Weekend / bank holiday |
| Impaired cognition | 2 | AMTS 8 |
| Not documented | 25 | Age 74–90 years |
Subgroup analysis of the patient characteristics between hospitals with the highest (Hospitals B, D and F) and lowest (Hospitals E, G and H) THR provision revealed that the patients eligible for THR in the low THR usage centres were significantly older than the patients in the high usage centres (median age: 80 vs 73 years, p=0.003, Table 5). The demographics of the two groups were otherwise well matched.
Table 5.
Demographics for the patients who fulfilled the criteria for THR in the hospitals with the lowest (Hospitals E, G and H) and highest (Hospitals B, D and F) rates of THR
| Demographic | Low THR rate (n=70) | High THR rate (n=63) | p-value |
|---|---|---|---|
| Median age in years | 80 (IQR: 72–84) | 73 (IQR: 60–81) | 0.003* |
| Sex Male Female |
24 (34%) 46 (66%) |
25 (37%) 42 (63%) |
0.71** |
| ASA grade 1 2 3 |
6 (9%) 38 (54%) 26 (37%) |
11 (16%) 34 (51%) 22 (33%) |
0.37** |
| Walking aids No aids One stick |
57 (81%) 13 (19%) |
52 (78%) 15 (22%) |
0.58** |
| AMTS 8 9 10 |
5 (7%) 9 (13%) 56 (80%) |
8 (12%) 14 (21%) 45 (67%) |
0.23** |
THR = total hip replacement; IQR = interquartile range; ASA = American Society of Anesthesiologists; AMTS = abbreviated mental test score
Kruskal–Wallis test;
chi-squared test
Binary logistic regression models were constructed including all of the demographic details described previously as explanatory variables and using a binary outcome of THR performed or not as the predictor outcome. This showed that if a patient was over 77 years old, it was more likely that a hemiarthroplasty was performed than in a patient aged 77 years or younger (relative risk: [RR]: 7.9, 95% confidence interval [CI]: 2.8–22.0, p<0.001). Similarly, there was a trend for this with patients who were classified as ASA grade 3 rather than ASA grades 1 or 2 (RR: 2.7, 95% CI: 1.0–7.3, p=0.06).
These models demonstrated that after adjustment for differences in patient demographics between the eight trauma units, there was a statistically significant difference in the chance of undergoing THR between the units with the highest (Hospitals B, D and F) and lowest (Hospitals E, G and H) rates of THR use (RR: 5.8, 95% CI: 2.1–15.9, p=0.001).
Discussion
During the study period, the audit found that based on the NICE guidelines without specification for age, only 29% of patients eligible for THR following displaced intracapsular hip fracture subsequently underwent this procedure. This proportion is higher than the reported national average in the two years prior to this study (between 11% and 21%).1,16 Significant variation of THR provision was observed between the trauma units (0–50%) and that remained after adjustment for demographic factors using regression. Other factors affecting the choice of procedure were age, presence of co-morbidities and surgeon’s preference. There is justification for performing femoral head preservation surgery by fixation of a displaced intracapsular hip fracture in young and fit patients but the proportion of THRs performed was only 35% even when this group of patients was excluded.
In our study, the most frequently documented factor for performing hemiarthroplasty in patients who met the NICE THR criteria was advanced age. In this subgroup, the age of the patients ranged from 80 to 94 years old. In fact, there were 66 patients aged 80 years or older but THR was only performed in 5 patients, with the oldest being 86 years. Age is not a criterion outlined in the NICE guidelines. Nevertheless, some surgeons consider it as a relative contraindication given that THR is a more complex procedure requiring a longer operative time.
Furthermore, there is concern regarding a higher risk of THR dislocation in elderly patients and the data currently available have not completely solved this dilemma. Newington et al reported a high rate of dislocation following primary THR in patients over the age of 80 years.10 This trend of dislocation was also observed in patients with dementia when THR was performed following displaced intracapsular hip fracture.11 A meta-analysis of eight randomised trials reported more than twice the RR of dislocation in patients undergoing THR following displaced intracapsular hip fracture.15 However, the meta-analysis found serious limitations in the methodology of all the trials. In contrast, Blomfeldt et al reported no dislocations in patients with a mean age of 81 years (range: 70–90 years) undergoing THR or bipolar hemiarthroplasty following displaced intracapsular fracture of the femoral neck.17
Acetabular erosion following hemiarthroplasty is also a subject of concern, especially in patients who were previously relatively active. In general, symptomatic acetabular erosion following hemiarthroplasty occurs late and is not common.13,18 Younger patients have been found to be at a higher risk for requiring revision surgery for acetabular erosion or loosening of the hemiarthroplasty than patients aged 75 years or older.19 There may be an underestimation of the number of older patients with symptomatic hemiarthroplasties as many will not be suitable for revision owing to frailty and a lack of fitness for anaesthesia or further surgery.
The argument for THR against hemiarthroplasty is that the former demonstrates better functional outcomes, levels of pain and mortality as well as a reduced risk of revision surgery.5–7,13 Although patients may fit the criteria for THR as outlined by NICE, the selection of the right patients for THR remains difficult in clinical practice. For them to be strictly adhered to, guidelines should confer high efficacy but no attributable risk and they should help with difficult decisions, making the process easier.
Stafford et al reported an increased revision rate at three years following THR for hip fractures in patients with a higher ASA grade.20 Our results show that nearly 75% of patients with ASA grade 3 underwent hemiarthroplasty. In principle, a thorough bedside assessment of the patient should be performed and cases for which THR might be indicated should be discussed with a hip specialist. Based on the findings from this study, a credible and relevant superiority, equivalence or non-inferiority randomised trial can be conducted to compare the types of arthroplasty in patients aged over 77 years presenting with displaced intracapsular hip fracture, the effects on clinical outcomes and the economic benefits.
Surgeon’s preference was also listed in our study as a reason for some patients undergoing hemiarthroplasty despite the patients meeting the THR criteria. Warwick et al reported various reasons for certain guidelines not being followed in orthopaedic surgery.21 These included lack of awareness of the guidelines, adverse personal experience with a certain procedure for a specific group of patients, the practicality of implementation and conflicting evidence. The proportions of THR performed in eligible patients have increased since the start of the national hip fracture audit programme,1 demonstrating that perhaps surgeons are becoming more aware of the guidelines and changing their practice.
THR is a more complex procedure, has a longer operative time and, in some patient groups, may not offer any advantage over hemiarthroplasty.19 In our study, in the free text section of the audit proforma, there were comments on patients receiving hemiarthroplasty because of a surgeon’s personal experience of poorer outcomes with THR in displaced intracapsular hip fracture. There were also three records of hemiarthroplasty being performed because of the lack of specialist hip surgeon during weekends or holiday periods in two hospitals.
It is not known how many cases did not achieve the best practice tariff because their surgery was delayed so it could be performed by a hip specialist. (The best practice tariff is an initiative by the Department of Health offering additional payment for hospitals when a case meets agreed standards [eg surgery within 36 hours for hip fractures].) Our study was not set up to assess the correlation between type of procedure and achievement of the best practice tariff. Further studies can assess this in addition to other areas including reasons for individual trauma unit-based factors affecting the choice of surgery.
Study limitations
This study has several limitations. It only included 110 patients from each hospital and is therefore not an accurate representation of hip fracture population in the area. On the other hand, the study period ran for at least three months in each hospital, including over a busy winter period. Our study included both trauma and fragility fractures. This may explain the high number of younger patients as well as those undergoing closed reduction and internal fixation of displaced intracapsular hip fracture. However, high provision rates of THR were found in the two major trauma centres (Hospitals D and F).
There were cases when operations other than THR were performed without a documented reason given by the surgical team. More robust methods of data collection for this information (such as interviewing the treating consultant) may have shed more light on this element of the study. Some trauma units in this study use hip fracture outcome scores routinely in the admission pathway22 but this factor was not accounted for in our analysis. Nevertheless, none of the cases where hemiarthroplasty or internal fixation was performed had the outcome scores as a reason for not performing THR.
Conclusions
The existing NICE guidelines are only adhered to loosely in clinical practice. This may be influenced by the lack of evidence of modern THR in patients of selected age and with medical co-morbidities. Our study found significant variation in the provision of THR for eligible hip fracture patients in a defined geographic region. This was influenced by patient factors such as age, coexisting morbidities, surgeon factors and also the trauma unit to which the patient was admitted.
References
- 1.Johansen A, Wakeman R, Boulton C et al. . National Hip Fracture Database: National Report 2013. London: NHFD; 2013. [Google Scholar]
- 2.Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 2007; : 1,251–1,254x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: a long-term follow-up of a randomised trial. Injury 2010; : 370–373. [DOI] [PubMed] [Google Scholar]
- 4.Parker M, Cawley S, Palial V. Internal fixation of intracapsular fractures of the hip using a dynamic locking plate: two-year follow-up of 320 patients. Bone Joint J 2013; : 1,402–1,405. [DOI] [PubMed] [Google Scholar]
- 5.Keating JF, Grant A, Masson M et al. . Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess 2005; . [DOI] [PubMed] [Google Scholar]
- 6.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am 2006; : 2,583–2,589. [DOI] [PubMed] [Google Scholar]
- 7.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ 2010; : c2332. [DOI] [PubMed] [Google Scholar]
- 8.National Institute for Health and Clinical Excellence Hip Fracture: Management. London: NICE; 2011. [Google Scholar]
- 9.British Orthopaedic Association The Care of Patients with Fragility Fracture. London: BOA; 2007. [Google Scholar]
- 10.Newington DP, Bannister GC, Fordyce M. Primary total hip replacement in patients over 80 years of age. J Bone Joint Surg Br 1990; : 450–452. [DOI] [PubMed] [Google Scholar]
- 11.Johansson T, Jacobsson SA, Ivarsson I et al. . Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 2000; : 597–602. [DOI] [PubMed] [Google Scholar]
- 12.Enocson A, Hedbeck CJ, Tidermark J et al. . Dislocation of total hip replacement in patients with fractures of the femoral neck. Acta Orthop 2009; : 184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avery PP, Baker RP, Walton MJ et al. . Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br 2011; : 1,045–1,048. [DOI] [PubMed] [Google Scholar]
- 14.Yu L, Wang Y, Chen J. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res 2012; : 2,235–2,243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burgers PT, Van Geene AR, Van den Bekerom MP et al. . Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop 2012; : 1,549–1,560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Currie C, Partridge M, Plant F et al. National Hip Fracture Database: National Report 2012. London: NHFD; 2012. [Google Scholar]
- 17.Blomfeldt R, Törnkvist H, Eriksson K et al. . A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br 2007; : 160–165. [DOI] [PubMed] [Google Scholar]
- 18.Khan SK, Jameson SS, Sims A et al. . Cemented Thompson’s hemiarthroplasty in patients with intracapsular neck of femur fractures: survival analysis of 1,670 procedures. Eur J Orthop Surg Traumatol 2015; : 655–660. [DOI] [PubMed] [Google Scholar]
- 19.van den Bekerom MP, Sierevelt IN, Bonke H, Raaymakers EL. The natural history of the hemiarthroplasty for displaced intracapsular femoral neck fractures. Acta Orthop 2013; : 555–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stafford GH, Charman SC, Borroff MJ et al. . Total hip replacement for the treatment of acute femoral neck fractures: results from the National Joint Registry of England and Wales at 3–5 years after surgery. Ann R Coll Surg Engl 2012; : 193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warwick D, Dahl OE, Fisher WD. Orthopaedic thromboprophylaxis. J Bone Joint Surg Br 2008; : 127–132. [DOI] [PubMed] [Google Scholar]
- 22.Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth 2008; : 511–517. [DOI] [PubMed] [Google Scholar]