From the pressure of an impending deadline to the frustration of sitting in traffic, stress is a normal feature of daily life. In most cases, the stressors are mild and we have both the mental and physical resources with which to cope. However, chronic exposure to high-stress situations is associated with many disease states and psychopathologies, and unfortunately, we don’t have to look far for real-life examples of this. Indeed, posttraumatic stress disorder affects up to 8% of Americans,1 and cardiovascular disease is rife in occupations that are characterized by high workloads with low controllability2. For example, female healthcare professionals who rate their jobs as ‘highly stressful’ are 38% more likely to experience heart problems compared with those with low-stress roles.3 The clear interaction between stress and disease makes furthering our understanding of stress physiology crucial for the future prevention and treatment of disorders with a stress component.
Recently, we identified a novel effect of stress on inwardly-rectifying potassium (KIR) channels located on the smooth muscle of small brain arterioles.4 These ‘parenchymal’ arterioles penetrate deep into the brain tissue, and dilate in response to nearby neuronal activity to deliver a surge of blood to the active region. This increase in blood flow provides the oxygen and glucose needed to offset increased local metabolic demand and importantly, failure of this process can lead to neuronal dysfunction.
To achieve dilation, signaling molecules are released from the specialized projections of a type of glial cell (known as astrocytes, due to their highly branching processes which give them a star-shaped morphology) that contact the vascular smooth muscle. These projections are termed ‘astrocytic endfeet’ and the molecules they release act through various parallel signaling pathways to hyperpolarize the adjacent smooth muscle membrane, which ultimately leads to dilation of the arteriole and increased blood flow. This process is termed ‘neurovascular coupling’. KIR channels appear to have an important part to play in this phenomenon: Potassium (K+) ions are released from the astrocytic endfeet in response to neuronal activity, which causes opening of smooth muscle KIR2 channels. KIR2 channels are activated by a small rise in extracellular K+ and membrane potential hyperpolarization. Activation of smooth muscle KIR channels hyperpolarizes the membrane from about -35 mV to the new K+ equilibrium potential, and this consequently decreases intracellular calcium (Ca2+) through closure of tonically active voltage-gated Ca2+ channels. This fall in intracellular Ca2+ causes smooth muscle relaxation, thereby leading to vasodilation and increased blood flow.5 Intriguingly, after we exposed rats to a one-week chronic stress paradigm—in which rats were exposed to one stressor each day for 7 days and developed an anxiety-like phenotype—we observed a decrease in KIR channel expression and a marked impairment of smooth muscle KIR channel function in parenchymal arterioles from the amygdala, a stress-related brain region.6 This loss of KIR channel function resulted in heavily blunted vasodilations during neurovascular coupling, which would substantially decrease local brain blood flow in vivo. Furthermore, we found that blocking glucocorticoid signaling prior to stress had a protective effect on neurovascular coupling, implying that stress-induced hormonal signaling underlies this phenomenon (Fig. 1).4 Thus, our results indicate that stress has profound effects on the ability of arterioles within the brain to dilate, and put the vascular smooth muscle KIR channel at center-stage as a key control element for arteriolar function during stress.
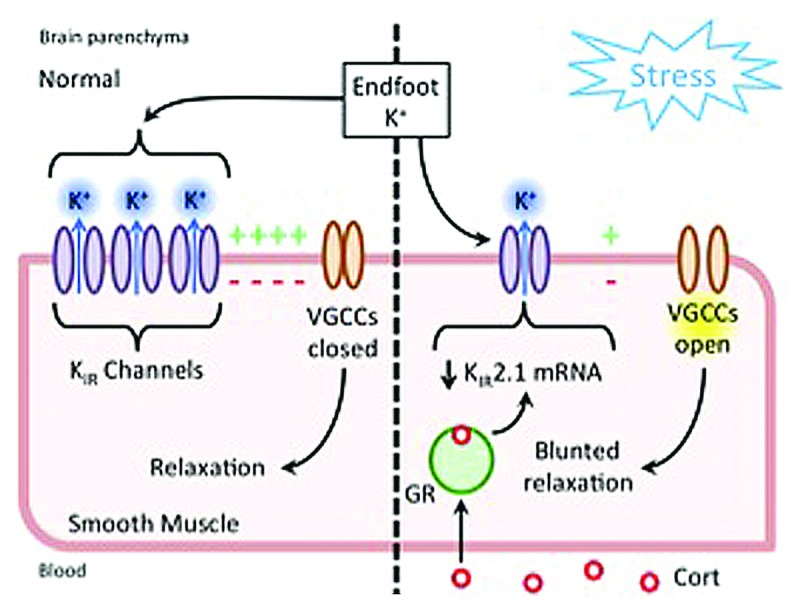
Figure 1. Normally (left), neuronally-evoked K+ release from astrocytic endfeet activates KIR channels on the smooth muscle membrane to cause membrane hyperpolarization, closure of voltage-gated Ca2+ channels (VGCCs), and vasorelaxation. After stress (right), increased circulating corticosterone (cort) causes downregulation of KIR2.1 gene expression via glucocorticoid receptor (GR) signaling, leading to fewer functional channels in the membrane and impaired neuronal-activity evoked vasodilations.
Ultimately these findings could have implications for human health. The role of stress in a broad range of brain disorders is now widely appreciated. For example, a recent study confirmed an association between stress throughout midlife with the later development of Alzheimer’s disease and other forms of dementia.7 Intriguingly, many brain disorders also have an important vascular component—indeed, it has long been known that cerebral blood flow is disturbed in dementia sufferers.8 Our study may provide a novel link between these two observations: The loss of smooth muscle KIR channel function after stress might impede the delivery of blood to active brain tissue, which could over time precipitate neuronal injury, leading to an eventual disruption of neuronal function. Further work is needed to explore these possibilities.
More broadly, converging evidence from ongoing studies in one of our labs (MTN) has implicated smooth muscle KIR channel dysfunction in several further disorders in which brain blood flow is impaired, which raises the possibility that vascular KIR channel disruption is a common feature in a range of brain diseases. Therefore, therapeutic strategies aimed at preserving or improving vascular KIR channel function to maintain or augment blood flow may be neuroprotective, as they may prevent the negative effects of neuronal energy demand exceeding supply. However, the broad expression profile of the KIR family lends the potential for off-target effects and this has hampered past drug-development efforts. An alternative to pharmacological approaches is to bypass impaired KIR channels entirely, and deliver a readily controllable ion channel or pump to the smooth muscle—for example by utilizing DREADD or optogenetic technology—which could then be stimulated as required to directly hyperpolarize the membrane to produce vasorelaxation and increased blood flow. The major challenge associated with these latter approaches would lie in obtaining tight spatiotemporal control over blood flow that is limited to a desired region.
References
- 1.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. . Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048 - 60; http://dx.doi.org/ 10.1001/archpsyc.1995.03950240066012; PMID: 7492257 [DOI] [PubMed] [Google Scholar]
- 2.Schnall PL, Landsbergis PA, Baker D. . Job strain and cardiovascular disease. Annu Rev Public Health 1994; 15:381 - 411; http://dx.doi.org/ 10.1146/annurev.pu.15.050194.002121; PMID: 8054091 [DOI] [PubMed] [Google Scholar]
- 3.Slopen N, Glynn RJ, Buring JE, Lewis TT, Williams DR, Albert MA. . Job strain, job insecurity, and incident cardiovascular disease in the Women’s Health Study: results from a 10-year prospective study. PLoS One 2012; 7:e40512; http://dx.doi.org/ 10.1371/journal.pone.0040512; PMID: 22815754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longden TA, Dabertrand F, Hill-Eubanks DC, Hammack SE, Nelson MT. . Stress-induced glucocorticoid signaling remodels neurovascular coupling through impairment of cerebrovascular inwardly rectifying K+ channel function. Proc Natl Acad Sci U S A 2014; 111:7462 - 7; http://dx.doi.org/ 10.1073/pnas.1401811111; PMID: 24808139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Filosa JA, Bonev AD, Straub SV, Meredith AL, Wilkerson MK, Aldrich RW, Nelson MT. . Local potassium signaling couples neuronal activity to vasodilation in the brain. Nat Neurosci 2006; 9:1397 - 403; http://dx.doi.org/ 10.1038/nn1779; PMID: 17013381 [DOI] [PubMed] [Google Scholar]
- 6.Roozendaal B, McEwen BS, Chattarji S. . Stress, memory and the amygdala. Nat Rev Neurosci 2009; 10:423 - 33; http://dx.doi.org/ 10.1038/nrn2651; PMID: 19469026 [DOI] [PubMed] [Google Scholar]
- 7.Johansson L, Guo X, Waern M, Ostling S, Gustafson D, Bengtsson C, Skoog I. . Midlife psychological stress and risk of dementia: a 35-year longitudinal population study. Brain 2010; 133:2217 - 24; http://dx.doi.org/ 10.1093/brain/awq116; PMID: 20488887 [DOI] [PubMed] [Google Scholar]
- 8.Hedlund S, Koehler V, Nylin G, Olsson R, Regnstroem O, Rothstroem E, Astroem KE. . Cerebral blood circulation in dementia. Acta Psychiatr Scand 1964; 40:77 - 106; http://dx.doi.org/ 10.1111/j.1600-0447.1964.tb05736.x; PMID: 14217631 [DOI] [PubMed] [Google Scholar]


