Abstract
Background
Length of stay after total hip arthroplasty (THA) has decreased over the last two decades. However, published studies that have examined same-day and early discharge protocols after THA have been done in highly selected patient groups operated on by senior surgeons in a nonrandomized fashion without control subjects.
Questions/purposes
The purpose of this study was to evaluate and compare patients undergoing THA who are discharged on the same day as the surgery (“outpatient,” less than 12-hour stay) with those who are discharged after an overnight hospital stay (“inpatient”) with regard to the following outcomes: (1) postoperative pain; (2) perioperative complications and healthcare provider visits (readmission, emergency department or physician office); and (3) relative work effort for the surgeon’s office staff.
Methods
A prospective, randomized study was conducted at two high-volume adult reconstruction centers between July 2014 and September 2015. Patients who were younger than 75 years of age at surgery, who could ambulate without a walker, who were not on chronic opioids, and whose body mass index was less than 40 kg/m2 were invited to participate. All patients had a primary THA performed by the direct anterior approach with spinal anesthesia at a hospital facility. Study data were evaluated using an intention-to-treat analysis. A total of 220 patients participated, of whom 112 were randomized to the outpatient group and 108 were randomized to the inpatient group. Of the 112 patients randomized to outpatient surgery, 85 (76%) were discharged as planned. Of the remaining 27 patients, 26 were discharged after one night in the hospital and one was discharged after two nights. Of the 108 patients randomized to inpatient surgery with an overnight hospital stay, 81 (75%) were discharged as planned. Of the remaining 27 patients, 18 met the discharge criteria on the day of their surgery and elected to leave the same day, whereas nine patients stayed two or more nights.
Results
On the day of surgery, there was no difference in visual analog scale (VAS) pain among patients who were randomized to discharge on the same day and those who were randomized to remain in the hospital overnight (outpatient 2.8 ± 2.5, inpatient 3.3 ± 2.3, mean difference −0.5, 95% confidence interval [CI], −1.1 to 0.1, p = 0.12). On the first day after surgery, outpatients had higher VAS pain (at home) than inpatients (3.7 ± 2.3 versus 2.8 ± 2.1, mean difference 0.9, 95% CI, 0.3–1.5, p = 0.005). With the numbers available, there was no difference in the number of reoperations, hospital readmissions without reoperation, emergency department visits without hospital readmission, or acute office visits. At 4-week followup, there was no difference in the number of phone calls and emails with the surgeon’s office (outpatient: 2.4 ± 1.9, inpatient: 2.4 ± 2.2, mean difference 0, 95% CI, −0.5 to 0.6, p = 0.94).
Conclusions
Outpatient THA can be implemented in a defined patient population without requiring additional work for the surgeon’s office. Because 24% (27 of 112) of patients planning to have outpatient surgery were not able to be discharged the same day, facilities to accommodate an overnight stay should be available.
Level of Evidence
Level I, therapeutic study.
Introduction
Length of stay (LOS) after THA has slowly decreased over the last two decades, mirroring trends for other procedures commonly performed in many surgical specialties. This has been driven by several factors including the development of clinical pathways that have been proven to reduce LOS after elective procedures [7, 9–12, 14, 16, 19, 20], a focus on reduction of healthcare expenditures in the last decade, an increased awareness of complications associated with decreased mobilization, and published studies demonstrating no compromise in outcome with early “full” weightbearing and early mobilization in cementless THA [2, 21, 22].
With the goal of decreasing LOS, modern surgical techniques, advances in regional anesthesia, improved postoperative pain management with multimodal and preemptive analgesia, and rapid rehabilitation protocols have allowed patients undergoing THA to be discharged from the hospital as early as the day of surgery with high patient satisfaction and infrequent complications in appropriately selected patients [1, 5, 6, 8]. However, the published studies that have examined same-day and “early” discharge protocols after THA are in highly selected patient groups operated on by senior surgeons in a nonrandomized fashion without control subjects [5, 8].
The first purpose of this prospective, randomized, multicenter study was to evaluate and compare patients undergoing THA who are planned to be discharged on the same day as their surgery (“outpatient,” less than 12-hour stay) with those who are planned to be discharged after an overnight hospital stay (“inpatient”) with regard to the following outcomes: (1) postoperative pain; (2) perioperative complications and healthcare provider visits (readmission, emergency department or physician office); and (3) relative work effort for the surgeon’s office staff. A secondary purpose of this study was to determine whether there are specific patient or surgical factors that are associated with discharge on the day of THA and whether these factors can be identified preoperatively.
Patients and Methods
A prospective, randomized study was conducted at two high-volume adult reconstruction centers (Rothman Institute, Philadelphia, PA, USA; and the Anderson Clinic, Alexandria, VA, USA) between July 2014 and September 2015. Institutional review board approval was obtained at both centers before initiation of the study and the study was registered at ClinicalTrials.gov (NCT02230657).
Patients who gave informed consent were randomized in a one-to-one ratio to one of two groups. The key inclusion criteria include that the study was limited to primary unilateral THA in patients younger than 75 years of age at surgery with a body mass index (BMI) less than 40 kg/m2 (Table 1). Also, patients with preoperative ambulatory status requiring use of a walker or wheelchair were excluded along with patients on chronic opioids preoperatively.
Table 1.
Study inclusion/exclusion criteria
| Inclusion criteria |
| Primary THA without acute hip fracture or prior hardware that would need to be removed at the time of surgery |
| Unilateral THA |
| Preoperative body mass index (BMI) < 40 kg/m2 |
| Age < 75 years at the time of surgery |
| Preoperative hemoglobin > 10 g/dL if preoperative hemoglobin data were available |
| No history of cardiopulmonary disease that would necessitate inpatient monitoring after surgery |
| Preoperative ambulatory status did not require the use of a walker or wheelchair |
| No chronic preoperative opioid medication use or opioid addiction |
| Assistance available at home after discharge from the hospital |
| No other condition or circumstance that would preclude rapid discharge from the hospital after surgery |
| Subject consented to participate in this study |
| Exclusion criteria |
| Revision THA |
| Bilateral THA |
| Preoperative BMI ≥ 40 kg/m2 |
| Age ≥ 75 years at the time of surgery |
| Preoperative hemoglobin ≤ 10 g/dL if preoperative hemoglobin data were available |
| History of cardiopulmonary disease requiring acute inpatient monitoring |
| Preoperative ambulatory status requiring the use of a walker or wheelchair |
| Chronic preoperative opioid medication use or opioid addiction |
| Limited or no assistance available at home after discharge from the hospital |
| Any other condition or circumstance that would preclude rapid discharge from the hospital |
| Subject did not consent to participate in this study |
Among the 220 patients who participated in this study, 112 were randomized to the outpatient group and 108 were randomized to the inpatient group (Table 2). Once the study protocol was explained and informed consent was obtained, patients were assigned to outpatient or inpatient surgery by opening a sealed envelope that contained the randomization group.
Table 2.
Demographics
| Demographic | All cases | As randomized (intent-to-treat) | |||
|---|---|---|---|---|---|
| Outpatient | Inpatient | Mean difference with 95% confidence interval | p value | ||
| Number of THAs (%) | 220 | 112 | 108 | N/A | N/A |
| Age at surgery (years) | 60.0 ± 8.7 [59.8] (27–74) | 59.8 ± 8.5 [59.3] (27–74) | 60.2 ± 8.9 [61.0] (34–74) | −0.4 (−2.7 to 2.0) | 0.76 |
| Sex | 103 females (47%) | 53 females (47%) | 50 females (46%) | N/A | 0.89 |
| BMI | 27.9 ± 4.4 [27.6] (18.0–39.9) | 27.6 ± 4.1 [27.1] (18.0–38.4) | 28.3 ± 4.7 [27.7] (18.4–39.9) | −0.8 (−1.9 to 0.4) | 0.19 |
| Preoperative diagnosis | |||||
| Osteoarthritis | 206 (94%) | 104 (93%) | 102 (94%) | N/A | 0.73 |
| Avascular necrosis | 10 (5%) | 5 (4%) | 5 (5%) | ||
| Dysplasia | 3 (1%) | 2 (2%) | 1 (1%) | ||
| Perthes | 1 (0.5%) | 1 (1%) | 0 | ||
| Preoperative comorbidities present | 39 (18%) | 19 (17%) | 20 (19%) | N/A | 0.86 |
Continuous data are specified as mean ± SD [median] (range); BMI = body mass index; N/A = not applicable.
Outpatients were expected to be discharged from the hospital within 12 hours of the conclusion of the THA, whereas inpatients were expected to stay one night in the hospital after their surgery.
Regardless of the group they were assigned to, all patients were informed that they would need to meet the same criteria (Table 3) before discharge. These discharge criteria were the same at both institutions and had been in use for all patients undergoing THA before the initiation of this study. Although study patients were told when they were expected to be discharged based on their assigned group, they understood that they could voluntarily elect to be discharged whenever they met the discharge criteria if they wished to go outside the study parameters.
Table 3.
THA discharge criteria
| Domain | Criteria |
|---|---|
| Physical therapy | Walk 80 feet on level ground |
| Walk up and down stairs (if stairs at home) | |
| Demonstrate understanding of home exercises | |
| Perform bathroom transfers | |
| Stand from supine position in bed | |
| Be able to dress self and perform basic activities of daily living | |
| Medical | Void after surgery |
| Tolerate a solid food diet | |
| Pain controlled | |
| Vital signs stable | |
| No significant nausea or vomiting | |
| Patient | Assistance is available at home by family or friends |
| Patient is comfortable with discharge |
All patients had a primary THA performed by the direct anterior approach with spinal anesthesia using 0.5% bupivacaine at a hospital facility. With the exception of seven cases that started in the early afternoon (between noon and 1:15 pm), all procedures in this study began in the morning with the initial incision occurring before noon. The multimodal pain management regimen, perioperative medications, and postoperative management were standardized between the institutions. Preoperative medications were administered orally and included one dose of 975 mg acetaminophen, 75 mg pregabalin, and 400 mg celecoxib immediately before surgery. The postoperative pain medication protocol was comprised of several agents including tramadol, acetaminophen, hydrocodone, ketorolac, pregabalin, and Celebrex (Pfizer, New York, NY, USA) (Table 4). All patients were given 24 hours of antibiotic coverage. Patients discharged the same day as their surgery received an additional IV dosage of antibiotics before discharge or three doses of 500 mg Keflex (Advancis Pharmaceutical Corporation, Germantown, MD, USA) orally every 6 hours after surgery. All drugs and devices used for this study were approved by the US Food and Drug Administration. Physical therapy was typically initiated within 1.5–3 hours of the termination of the surgical procedure depending on the restoration of motor and sensory function of the lower extremities and the patient’s medical status.
Table 4.
Postoperative pain medication protocol
| Medication | Dose | Indications |
|---|---|---|
| Tramadol | 50 mg orally every 6 hours as needed | All patients |
| Ketorolac | 15 mg IV every 6 hours (maximum 6 doses) or 30 mg IV every 6 hours (maximum 6 doses) | 15-mg dosage in patients > 70 years of age or with renal insufficiency 30-mg dosage in patients < 70 years of age without renal insufficiency |
| Pregabalin | 75 mg orally every 12 hours | Patients < 70 years of age |
| Celebrex | 200 mg orally every 12 hours | Contraindicated in patients with sulfa allergy |
| Hydrocodone/acetaminophen | 5 mg/325 mg 1–2 tablets orally every 4–6 hours as needed | All patients |
Patients were assessed for followup after their THA on the day of surgery, on the first day after surgery, and 4 weeks after surgery. All patients completed a visual analog scale (VAS) pain assessment (0 = no pain, 10 = worst pain) preoperatively, on the day of surgery (postoperative day [POD] 0), on the first day after surgery (POD 1), and at their 4-week followup visit. POD 0 assessment was obtained after sensory and motor neurologic recovery of the lower extremities. Patients who were discharged from the hospital on the same day as their procedure were given a POD 1 VAS pain form to complete at home. Study personnel called these patients on the day after their surgery to confirm form completion. Also, between the day of surgery and the 4-week followup visit, all office personnel were instructed to record contact with any study patient, whether it was by phone, fax, email, or other means. If the study patient was using a proxy (family member, friend, or medical professional) to call the office, this was recorded. At their 4-week followup visit, all patients were asked to complete a standardized form inquiring about any problems they had after the THA. A Harris hip score was also assessed preoperatively and at 4-week followup. Study personnel interviewed each patient to assess any complications they had after the procedure, confirming any calls to the surgeon’s office, inquiring about hospital readmissions, visits to emergency departments or urgent care facilities, acute office appointments, and any other adverse events during the 4 weeks after their index THA.
Crossover Between Groups
Of the 112 patients randomized to outpatient surgery, 85 (76%) were discharged as planned (Fig. 1). Among the remaining 27 patients, 26 were discharged after one night and a single patient was discharged after two nights in the hospital. Among these 27 patients, the reasons for delayed discharge included dizziness/hypotension (nine), pain (six), patient preference (five), nausea (four), ambulatory dysfunction (two), and urinary retention (one). Of the 108 patients randomized to inpatient surgery with an overnight hospital stay, 81 (75%) were discharged as planned. Of the remaining 27 patients, 18 met the discharge criteria on the day of their surgery and elected to leave the same day, whereas nine patients stayed more than one night. The reasons for staying more than one night included dizziness/hypotension (three), pain (two), weightbearing restrictions (two), and urinary retention (two). Compared with the 90 inpatients who remained in the hospital for one or more nights, the 18 patients randomized to inpatient surgery who elected to leave the same day were younger (55 ± 9 versus 61 ± 9, mean difference −6, 95% confidence interval [CI], −2 to −11, p = 0.007) and predominantly male (94% versus 46%, p < 0.001). Compared with the 81 inpatients who were discharged after one night, the nine inpatients who remained in the hospital for more than one night tended to be older (66 ± 7 versus 61 ± 9, mean difference 6, 95% CI, −0.2 to 12, p = 0.06) and were all females (100% versus 49%, p = 0.003).
Fig. 1.
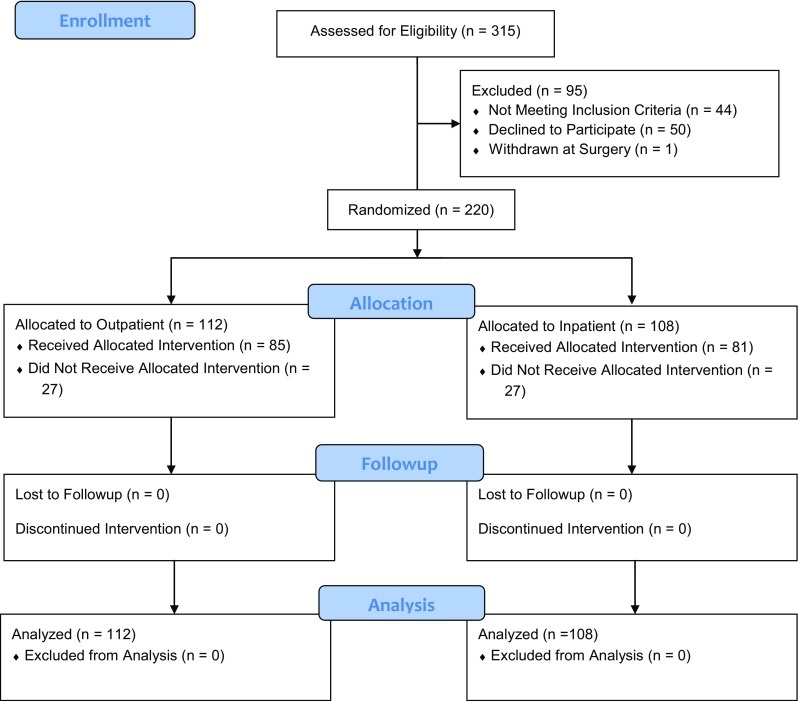
The CONSORT flow diagram for this study illustrates that 220 patients were randomized to outpatient or inpatient THA. The 27 patients randomized to the outpatient group who did not receive the allocated intervention include 26 who remained in the hospital for one night and one patient who remained in the hospital for two nights. The 27 patients randomized to the inpatient group who did not receive the allocated intervention include 18 who elected to be discharged on the day of their surgery and nine who remained in the hospital for two or more nights. All 220 patients had 4-week followup and no patients were excluded from our intent-to-treat analysis.
Statistical Analysis
Study data were evaluated using an intention-to-treat analysis; that is, patients randomized to the outpatient group who stayed overnight were nonetheless analyzed in the outpatient group and vice versa. Patients who were not discharged as planned were also analyzed independently. Study data were characterized using descriptive statistics and differences among groups were evaluated using inferential statistics. Student’s t-test was used to compare continuous data in two groups. A Fisher’s exact test was used for two-by-two categorical variables. Pearson’s chi square was used to compare groups with three or more categories. A p value of 0.05 was used as the threshold for statistical significance. All statistical analyses were performed using the Statistical Package for the Social Sciences software (SPSS, Chicago, IL, USA).
Among the randomized groups, there were no differences in age, gender, BMI, preoperative diagnosis, or the presence of preoperative comorbidities (Table 2). Although not all patients were discharged as planned based on their preoperative randomization, none were lost to followup (Fig. 1).
Results
Pain and Function
On the day of surgery, there was no difference in the VAS pain scores among patients who were randomized to be discharged the same day (outpatients) compared with those who were randomized to remain in the hospital overnight (inpatients) (outpatient: 2.8 ± 2.5, inpatient: 3.3 ± 2.3, mean difference −0.5, 95% CI, −1.1 to 0.1, p = 0.12). On the first day after surgery, the outpatients reported increased pain compared with the inpatients (outpatient: 3.7 ± 2.3, inpatient: 2.8 ± 2.1, mean difference 0.9, 95% CI, 0.3–1.5, p = 0.005). At 4-week followup, there was no difference in VAS pain among the groups (outpatient: 1.7 ± 1.9, inpatient: 1.7 ± 1.9, mean difference −0.1, 95% CI, −0.6 to 0.4, p = 0.77). At baseline, the groups were not different (outpatient: 4.7 ± 2.4, inpatient: 4.4 ± 2.5, mean difference 0.3, 95% CI, −0.3 to 1.0, p = 0.32).
At 4-week followup, there was no difference in Harris hip scores among the groups (outpatient: 75 ± 18, inpatient: 75 ± 14, mean difference −1, 95% CI, −5 to 4, p = 0.77). There was also no difference in preoperative Harris hip scores (outpatient: 53 ± 13, inpatient: 53 ± 14, mean difference 0, 95% CI, −4 to 4, p = 0.98).
Complications and Healthcare Provider Visits
After discharge from the hospital, two patients (one from each study group) underwent reoperations for infection and one additional patient randomized to the outpatient group sustained a periprosthetic fracture in conjunction with a motor vehicle collision that was treated with open reduction and internal fixation. With the numbers available, there was no difference in the reoperations (two outpatients versus one inpatient, p = 1.0). In addition to these reoperations, there were five other hospital readmissions, including one from the outpatient group and four from the inpatient group (p = 0.21). Two inpatients visited an emergency department but were not readmitted (p = 0.24). Two outpatients had acute office visits before their 4-week followup (p = 0.50).
Work Effort for Surgeons’ Office Staff
At 4-week followup, there was no difference among the groups with regard to the mean number of contacts, including calls and emails between the office staff and the patient (outpatient: 2.4 ± 1.9, inpatient: 2.4 ± 2.2, mean difference 0, 95% CI, −0.5 to 0.6, p = 0.94).
Discussion
Outpatient and early-discharge THA is increasing in the United States because perioperative protocols including early mobilization, multimodal pain management, and regional anesthesia have improved the postoperative course considerably. Prior work that has examined outpatient discharge protocols after THA is in highly selected patient groups without control subjects [5, 8]. Also, many studies have used the term “outpatient” loosely and often refer to the “23-hour stay” patient as an “outpatient,” although the patient stayed overnight in the hospital. With this in mind, the purpose of this study was to evaluate and compare (1) postoperative pain; (2) perioperative complications and healthcare provider visits; and (3) work effort for the surgeon’s office staff in a defined population of patients who are discharged on the same day as their surgery (“outpatient”) with those who are discharged after an overnight hospital stay (“inpatient”).
Weaknesses of this study are that we had two different institutions with distinct differences. Although both sites are high-volume adult reconstruction centers performing more than 2000 joint arthroplasties per year, one is an academic center and the other a more community-based practice in a smaller community hospital. Other aspects that can be considered weaknesses include the fact that we did not “force” patients to remain in the group to which they were randomized. If they decided to go outside their randomized group, we respected their choice as their right. It was explained during the consent process that we requested patients to remain in their randomization group for the purposes of this study, but they could go outside their assigned group if required for their medical safety or personal preference. Additionally, the study is not powered appropriately to assess a true difference in complications and did not evaluate complications that may have occurred after 4-week followup. To assess a true difference in the frequency of complications and depending on what is considered a complication, it may have required up to 1000 patients, which was not feasible for two centers in the context of a prospective, randomized study design at the current time. Although the inclusion and exclusion criteria are defined (Table 1), other limitations of the study include the fact that our enrollment criteria excluded patients aged 75 years or older with a BMI of 40 kg/m2 or greater who were walker/wheelchair-dependent or chronic opioid users. Depending on practice patterns, this may or may not be a large portion of a surgeon’s practice.
As would be expected in a randomized study, preoperative VAS pain scores were not different between the two groups. On the day of surgery, there was no difference in the VAS pain scores between outpatients and inpatients. However, on the day after surgery, the outpatients had higher VAS pain scores than those patients who stayed in the hospital overnight. The difference may not be clinically important, but it may point to a need for improved counseling on pain management at home (when to take medications, which medications to take). Additionally, the difference may reflect an increased amount of pain when patients go home and have potentially increased activity as compared with an overnight stay in a hospital bed. Several investigators [1–5, 8] have written about pathways for the success of early-discharge THA and TKA and more recently [5, 8] have published on prospective evaluations of patients undergoing outpatient THA. Adult reconstructive surgeons nationally have adopted clinical pathways similar to those published by this group for inpatient THA as an evolution of the management of these patients undergoing elective surgery. Overall, pain was not a substantial problem with regard to discharge on the day of surgery or after an overnight stay and this may be related to the pain protocols used at both institutions including preemptive analgesia, spinal anesthesia, and postoperative multimodal pain management. This is in line with contemporary studies demonstrating well-controlled pain with these protocols in place [13, 15, 17, 18].
One of the most important concerns with outpatient surgery has been the potential for increased complications, including readmissions to the hospital and visits to physician providers and emergency departments. Although this study was not powered to assess a difference in complication rates, there was no evidence suggesting differences in readmissions, visits to emergency departments, or acute office appointments during the 4 weeks after surgery. When considered in more depth, this is not surprising, because we did not compare outpatient surgery with a prolonged hospital stay. At both institutions, an outpatient discharge or an overnight stay in the hospital was the normal protocol before the study. Thus, when comparing a same-day discharge with a discharge after an overnight stay, there is in actuality not a large difference in the number of hours of hospitalization, and so it may not be surprising that there was no discernible difference in complications. Three prior studies [2, 5, 8] have affirmed the safety of outpatient THA; however, all of these studies were among nonrandomized, highly selected patient populations with no control group.
Furthermore, there was no difference in “work” for the surgeon’s office with regard to patient followup and phone calls. Based on the results of this study, outpatient THA can be done with little impact to the surgeon’s practice if it is implemented systematically and in partnership with the facility where the surgery is performed. This may be in contrast to anecdotal reports that outpatient joint replacement results in a deluge of phone calls from patients. However, we believe this was not the case in our study because the only difference between the two groups was an overnight stay. Our institutional education and protocols have accommodated a large percentage of patients leaving the hospital after one night for years and more recently leaving on the same day. For this reason, the preoperative patient education and counseling may have accounted for the lack of difference in “work” between the two groups for our clinical offices.
The results demonstrated that 24% (27 of 112) of patients crossed over from the outpatient group to the inpatient group, and 17% (18 of 108) of patients crossed over from the inpatient group to the outpatient group. This illustrates that in a defined group of patients scheduled for outpatient THA at adult reconstruction centers, greater than 75% of patients may actually leave on the day of surgery, passing all of the standardized discharge criteria (Table 3). When evaluating the reasons for delayed discharge among the patients randomized to the outpatient group, some of the more common causes were nausea and dizziness-associated hypotension. This may point to a need for even more aggressive control of anesthesia-related side effects and more aggressive fluid resuscitation. Because all patients received neuraxial (spinal) anesthesia, there also may be a need for shorter acting agents that produce a less prolonged hypotensive effect. No patient or surgical factors were found to be associated with crossover from outpatient to inpatient. There were approximately 8% of patients (nine of 108) who were randomized to the inpatient overnight stay but stayed multiple nights. Compared with the patients randomized to inpatient surgery who were discharged after one night, these patients were all women (100% versus 49%) and tended to be older (66 versus 61 years). Whether women are more susceptible to nausea/hypotension in conjunction with blood loss and anesthesia-related side effects or if this is a motivation or apprehension phenomenon cannot be determined from our study. Previous studies evaluating early discharge after THA [5, 8] have not specifically noted any difficulty with early discharge in older women. Those investigators who have published on outpatient THA have reported substantially contrasting success rates with regard to same-day discharge, from 36% to 100% [5, 8]. In one study [8] only 36% of eligible patients actually wanted to leave on the day of surgery, and only 77% of those patients were able to. They do report that of the 23% who wanted to be discharged home but were unable, nausea/hypotension was the predominant factor limiting discharge. In another report, Berger and colleagues [5] stated that of 150 patients enrolled for same-day discharge, all 150 patients were able to leave on the day of surgery. In their study, 38 (25%) patients required additional treatment secondary to nausea and/or hypotension, which had some effect on delaying discharge until later in the day. However, both of these studies are in line with our results in which approximately one-fourth of patients demonstrated some difficulty with early discharge, predominantly as a result of nausea/hypotension.
Using a multicenter, prospective, randomized design, the current study demonstrates that outpatient THA can be successful in a defined patient population but patient expectations must be appropriately established. Using criteria similar to those established in this study (age < 75 years, BMI < 40 kg/m2, opioid-naïve, and not requiring a walker or wheelchair) may facilitate outpatient discharge. However, postoperative pain management counseling and appropriate medication are critical to address outpatient pain control while at home on the first day after surgery. For arthroplasty programs where LOS has decreased to an overnight stay and preoperative education and counseling is available for patients, implementation of an outpatient arthroplasty program will not result in a substantial increase in patient-generated phone calls or visits for the office or surgeon. However, we recommend that facilities to accommodate an overnight stay should be available because 24% of patients planning to have outpatient surgery were not able to be discharged the same day. For institutions with the resources and expertise, we feel that outpatient THA is the next step in a national movement toward more streamlined inpatient services for elective joint arthroplasty.
Acknowledgments
We thank Supatra Sritulanondha and Ann C. Williams of the Anderson Orthopaedic Research Institute who administered the questionnaires and collected the data for this study.
Footnotes
One of the authors (AFC) has received research support funding from 3M (Maplewood, MN, USA) and Myoscience (Fremont, CA, USA). One of the authors (WGH) has received research support funding from DePuy (DePuySynthes, New Brunswick, NJ, USA), Biomet (Warsaw, IN, USA), and Nimbic Systems (Stafford, TX, USA). The institution of one or more of the authors (NG, SEP, RHH, WGH) has received, during the study period, funding from the Inova Health System (Falls Church, VA, USA). One of the authors (NG), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Cayenne Medical (Scottsdale, AZ, USA) and Stryker Orthopedics (Mahwah, NJ, USA). One of the authors (AFC), or a member of her immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from ACI Clinical (Bala Cynwyd, PA, USA). One of the authors (WGH), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from DePuy, Biomet, and Nimbic Systems. One of the authors (WJH), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount of USD 100,001 to USD 1,000,000 from Stryker. One of the authors (NG) lists the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: Data Trace Publishing Company (Towson, MD, USA) in the amount of USD 10,000 to USD 100,000. One of the authors (AFC) lists the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: SLACK Incorporated (Thorofare, NJ, USA) in the amount of less than USD 10,000.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Rothman Institute & Thomas Jefferson University Hospital, Philadelphia, PA, USA, and the Anderson Orthopaedic Research Institute & Inova Center for Joint Replacement at Mount Vernon Hospital, Alexandria, VA, USA.
A comment to this article is available at http://dx.doi.org/10.1007/s11999-016-4985-y.
References
- 1.Berger RA. A comprehensive approach to outpatient total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007;36(Suppl):4–5. [PubMed] [Google Scholar]
- 2.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA, Sanders S, D’Ambrogio E, Buchheit K, Deirmengian C, Paprosky W, Della Valle CJ, Rosenberg AG. Minimally invasive quadriceps-sparing TKA: results of a comprehensive pathway for outpatient TKA. J Knee Surg. 2006;19:145–148. doi: 10.1055/s-0030-1248097. [DOI] [PubMed] [Google Scholar]
- 4.Berger RA, Sanders S, Gerlinger T, Della Valle C, Jacobs JJ, Rosenberg AG. Outpatient total knee arthroplasty with a minimally invasive technique. J Arthroplasty. 2005;20(Suppl 3):33–38. doi: 10.1016/j.arth.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Sanders SA, Thill ES, Sporer SM, Della Valle C. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res. 2009;467:1424–1430. doi: 10.1007/s11999-009-0741-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen D, Berger RA. Outpatient minimally invasive total hip arthroplasty via a modified Watson-Jones approach: technique and results. Instr Course Lect. 2013;62:229–236. [PubMed] [Google Scholar]
- 7.Delaney CP, Senagore AJ, Gerkin TM, Beard TL, Zingaro WM, Tomaszewski KJ, Walton LK, Poston SA. Association of surgical care practices with length of stay and use of clinical protocols after elective bowel resection: results of a national survey. Am J Surg. 2010;199:299–304. doi: 10.1016/j.amjsurg.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 8.Dorr LD, Thomas DJ, Zhu J, Dastane M, Chao L, Long WT. Outpatient total hip arthroplasty. J Arthroplasty. 2010;25:501–506. doi: 10.1016/j.arth.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Healy WL, Ayers ME, Iorio R, Patch DA, Appleby D, Pfeifer BA. Impact of a clinical pathway and implant standardization on total hip arthroplasty: a clinical and economic study of short-term patient outcome. J Arthroplasty. 1998;13:266–276. doi: 10.1016/S0883-5403(98)90171-1. [DOI] [PubMed] [Google Scholar]
- 10.Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am. 2002;84:348–353. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Losina E, Solomon DH, Wright J, Katz JN. Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty. 2003;18:69–74. doi: 10.1054/arth.2003.50030. [DOI] [PubMed] [Google Scholar]
- 12.Lawrence JK, Keller DS, Samia H, Ermlich B, Brady KM, Nobel T, Stein SL, Delaney CP. Discharge within 24 to 72 hours of colorectal surgery is associated with low readmission rates when using Enhanced Recovery Pathways. J Am Coll Surg. 2013;216:390–394. doi: 10.1016/j.jamcollsurg.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 13.Lee KJ, Min BW, Bae KC, Cho CH, Kwon DH. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg. 2009;1:155–160. doi: 10.4055/cios.2009.1.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mabrey JD, Toohey JS, Armstrong DA, Lavery L, Wammack LA. Clinical pathway management of total knee arthroplasty. Clin Orthop Relat Res. 1997;345:125–133. doi: 10.1097/00003086-199712000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467:1418–1423. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty. 1998;13:896–900. doi: 10.1016/S0883-5403(98)90196-6. [DOI] [PubMed] [Google Scholar]
- 17.Parvizi J, Bloomfield MR. Multimodal pain management in orthopedics: implications for joint arthroplasty surgery. Orthopedics. 2013;36(Suppl):7–14. doi: 10.3928/01477447-20130122-51. [DOI] [PubMed] [Google Scholar]
- 18.Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2011;93:1075–1084. doi: 10.2106/JBJS.J.01095. [DOI] [PubMed] [Google Scholar]
- 19.Pearson SD, Goulart-Fisher D, Lee TH. Critical pathways as a strategy for improving care: problems and potential. Ann Intern Med. 1995;123:941–948. doi: 10.7326/0003-4819-123-12-199512150-00008. [DOI] [PubMed] [Google Scholar]
- 20.Stephen AE, Berger DL. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery. 2003;133:277–282. doi: 10.1067/msy.2003.19. [DOI] [PubMed] [Google Scholar]
- 21.Taunt CJ, Jr, Finn H, Baumann P. Immediate weight bearing after cementless total hip arthroplasty. Orthopedics. 2008;31:223. doi: 10.3928/01477447-20080301-40. [DOI] [PubMed] [Google Scholar]
- 22.Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H. The effects of different weight-bearing regimes on press-fit cup stability: a randomised study with five years of follow-up using radiostereometry. Int Orthop. 2012;36:735–740. doi: 10.1007/s00264-011-1413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


