Abstract
PURPOSE
We aimed to assess the role of computed tomography (CT) perfusion in differentiation of thymoma from thymic hyperplasia, lymphoma, thymic carcinoma, and lung cancer invading anterior mediastinum.
METHODS
In this study, 25 patients with an anterior mediastinal lesion underwent CT perfusion imaging from January 2015 to February 2016. Diagnoses included thymoma (n=7), thymic hyperplasia (n=8), lymphoma (n=4), thymic carcinoma (n=3), and invasive lung cancer (n=3). Lymphoma, thymic carcinoma, and lung cancer were grouped as malignant tumors for statistical analysis. Values for blood flow, blood volume, and permeability surface were measured in CT perfusion.
RESULTS
Blood flow and blood volume values were higher in thymoma in comparison to thymic hyperplasia; however, the difference was not statistically significant. Blood volume values were significantly higher in thymoma (mean, 11.4 mL/100 mL; range, 5.2–20.2 mL/100 mL) compared with lymphoma (mean, 5.3 mL/100 mL; range, 2.5–7.2 mL/100 mL) (P = 0.023). Blood flow and blood volume values were significantly higher in thymoma compared with non-thymoma malignant tumors (P = 0.025).
CONCLUSION
CT perfusion is helpful in differentiating thymoma from non-thymoma malignancies including lymphoma, thymic carcinoma, and invasive lung cancer involving the anterior mediastinum.
Anterior mediastinal lesions cover a heterogeneous group of cystic and solid masses (1, 2). Thymoma is the most common tumor in the anterior mediastinum with germ cell tumors, lymphoma, thymic cysts, and thymic hyperplasia accounting for the majority of the rest (1, 3). Anterior mediastinal tumors have some typical computed tomography (CT) and magnetic resonance imaging (MRI) findings; however, CT and MRI in some cases may fail to differentiate between anterior mediastinal lesions, posing diagnostic and therapeutic challenges (4, 5). While thymectomy is often performed for thymoma, it is not therapeutic for thymic hyperplasia, thymic cysts, and lymphoma. Nontherapeutic thymectomy rates range from 22% to 68% in the literature (6).
Diffusion-weighted MRI, contrast-enhanced MRI, chemical shift MRI, [18F] Fluoro-2-deoxy-D-glucose–positron emission tomography (FDG-PET), and thallium-201 scintigraphy have been evaluated as alternative modalities for differentiating among thymic cysts, thymoma, and thymic hyperplasia (3, 7–11). CT perfusion offers an alternative approach for a preoperative noninvasive diagnosis. CT perfusion is a functional imaging technique, providing quantitative data on tissue perfusion by acquiring graphs of blood flow (BF), blood volume (BV), and permeability surface (PS). CT perfusion has been found useful in evaluating tumor angiogenesis, malignant infiltration of surrounding tissue, and tumor response to chemoradiotheraphy (12).
In this prospective study, we evaluated the role of CT perfusion in differentiation of thymoma from thymic hyperplasia, lymphoma, thymic carcinoma, and invasive lung cancer involving the anterior mediastinum.
Methods
Patient selection
Patients with an anterior mediastinal mass observed on antecedent CT, MRI, or FDG-PET were enrolled in this study. Exclusion criteria were myasthenia gravis (due to possible exaggeration of symptoms by iodinated contrast agent), renal failure, history of allergy to iodinated contrast agent, pregnancy, untreated hyperthyroidism, chemotherapy, or radiotherapy (due to possible interference with perfusion results in thymic hyperplasia and lymphoma).
Based on these criteria, 25 patients (16 women, 9 men; mean age: 47±17 years, age range: 19–74 years) were enrolled from January 2015 to February 2016. Tumor size ranged from 23 mm to 110 mm (mean diameter, 52±22 mm) on greatest axis length. Pathologic confirmation was based on surgical resection in 14 patients and percutaneous core-needle biopsy in seven patients. The diagnosis of thymic hyperplasia of remaining four patients was verified by chemical shift MRI based on the signal loss opposed-phase images suggestive of microscopic fat after CT perfusion examination.
Surgical and percutaneous biopsy specimens were reviewed and diagnosed at the pathology department of our home institution. The pathologic examination and follow-up imaging revealed diagnoses of thymoma (n=7), thymic hyperplasia (n=8), lymphoma (n=4), thymic carcinoma (n=3), and invasive lung cancer (n=3). This study was approved by the institutional review board and informed consent was obtained.
CT perfusion imaging
The CT examinations were obtained with a 128-row CT scanner (Somatom Definition AS; Siemens Healthcare). Initially, an unenhanced low-dose thorax CT was obtained. Subsequently, a 6.9 cm to 9.6 cm z-axis coverage CT perfusion scan was performed based on the lesion size. We used the following CT perfusion parameters: for patients who weighed less than 70 kg, tube current was 80 mAs and the voltage was 80 kV; for patients who weighed 70 kg or more, tube current was 100 mAs and the voltage was 100 kV. The collimation was 32×1.2 mm. The scanning time of total CT perfusion was 47 s with a gantry rotation time of 0.3 s. Patients were advised to maintain shallow breathing in the course of perfusion scanning.
A total dose of 50 mL of contrast material (Ultravist 370, Bayer Schering Pharma) was administered through an 18 G needle at a flow rate of 5 mL/s followed by a saline flush of 50 mL NaCl at 5 mL/s, after a start delay of 4 s. The contrast material was injected into an antecubital vein using a dual head pump injector (Medrad). The reconstruction of images, which had a slice thickness of 3 mm, was performed using 512×512 pixel and medium smooth B20f kernel.
CT perfusion analysis
All CT perfusion data were transferred to a workstation (Leonardo Volume Perfusion CT Body, Siemens) for image processing. CT perfusion images were evaluated in consensus by two radiologists (C.A. and S.B.) experienced in chest imaging. For CT perfusion data evaluation, noise reduction and motion correction of the datasets were performed automatically. The window width and center for the reference vessel input were 400 HU and 40 HU, respectively.
The software generated three-dimensional color-coded maps for BF, BV, and PS. BF (mL/100 mL/min) is defined as the amount of blood flowing through 100 mL of tumor tissue within 1 min. BV (mL/100 mL) is defined as the amount of blood within 100 mL of tumor tissue. PS (mL/100 mL/min) is an area product, which measures contrast medium extravasation into the extravascular space, in milliliters per 100 mg per minute. Arterial input information was obtained by manually placing a region of interest inside the thoracic aorta (range, 14–28 mm2). A volume of interest was drawn manually around the whole tumor in the mediastinum window. Care was taken to exclude adjacent vascular structures, bones, and lungs. The mean values of the perfusion parameters were recorded for statistical analyses.
Statistical analysis
Descriptive statistics were presented as median, minimum, and maximum. Mann Whitney U-test was used to compare BF, BV, and PS values between thymoma, thymic hyperplasia, lymphoma, and all malignant tumors (including lymphoma, thymic carcinoma, and invasive lung cancer). For statistical significance, the alpha level was set at 0.05. Statistical analyses were performed with SPSS v. 21 (IBM Corp.).
Results
Diagnoses of the 25 patients included thymoma (n=7), thymic hyperplasia (n=8), lymphoma (n=4), thymic carcinoma (n=3), and invasive lung cancer (n=3). Lymphoma, thymic carcinoma, and invasive lung cancers were grouped as malignant tumors for statistical analyses (Table). The BF, BV, and PS values for all anterior mediastinal lesions are given in the Table. Representative cases for thymoma, lymphoma, and invasive lung cancers are presented in Figs. 1–3, respectively.
Table.
Perfusion parameters for subtypes of anterior mediastinum lesions
| Perfusion parameters | Thymoma (n=7) | Thymic hyperplasia (n=8) | Lymphoma (n=4) | All malignant tumors (n=10) | P | ||
|---|---|---|---|---|---|---|---|
| Thymoma vs. | |||||||
|
| |||||||
| Thymic hyperplasia | Lymphoma | All malignant tumors | |||||
| BF | 61.7 (34.9–231) | 57.4 (19.0–72.7) | 35.7 (24.5–59.8) | 42.5 (17.8–78.6) | 0.355 | 0.059 | 0.032* |
|
| |||||||
| BV | 11.4 (5.2–20.2) | 8.5 (3.9–13.1) | 5.3 (2.5–7.2) | 6.2 (2.5–11.8) | 0.165 | 0.023* | 0.025* |
|
| |||||||
| PS | 22.3 (9.3–36.8) | 21.7 (7.1–32.7) | 11.0 (2.2–14.8) | 13.8 (2.2–23.2) | 0.817 | 0.089 | 0.205 |
Data are presented as median (min–max).
BF, blood flow; BV, blood volume; PS, permeability surface.
Significant difference.
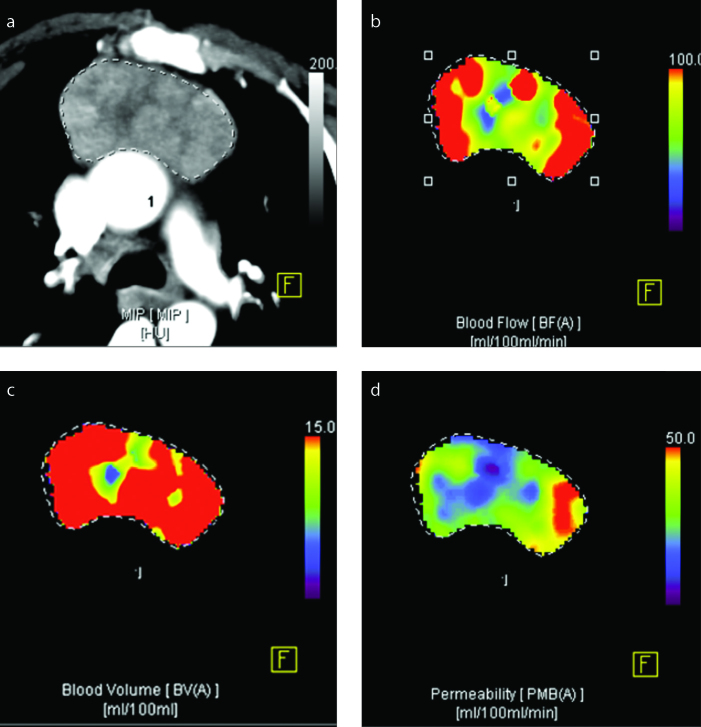
Figure 1.
a–d. A 56-year-old patient with a pathologic diagnosis of thymoma. The maximum intensity projection (MIP) image (a) shows a contrast-enhanced mass at the anterior mediastinum. Corresponding blood flow map (b) shows heterogeneously increased blood flow in the lesion. Blood volume map (c) also shows high values with a relatively homogeneous distribution. Corresponding permeability surface map (d) features areas with decreased permeability within the lesion.
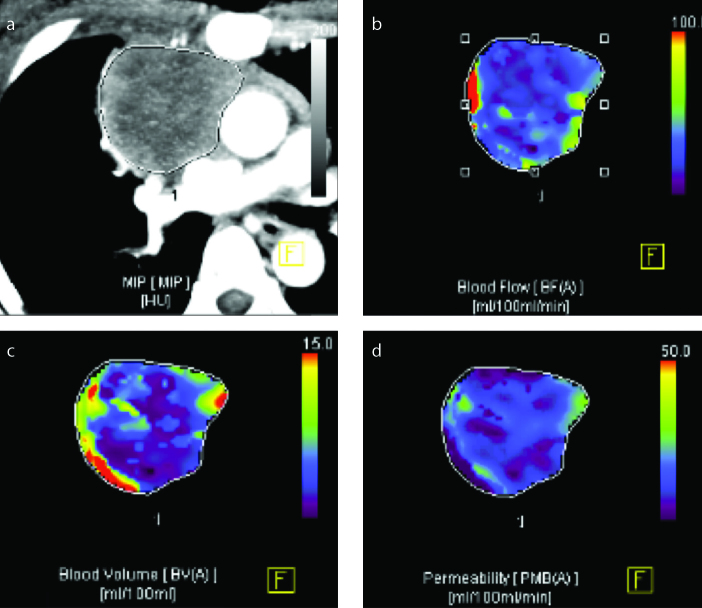
Figure 2.
a–d. A 44-year-old patient with a pathologic diagnosis of lymphoma. The MIP image (a) shows a heterogeneous off-midline mass at the anterior mediastinum. Corresponding blood flow map (b) shows heterogeneously decreased blood flow in the lesion. Blood volume map (c) also shows low values with an inhomogeneous distribution. Corresponding permeability surface map (d) shows areas with homogeneously decreased permeability within the lesion.
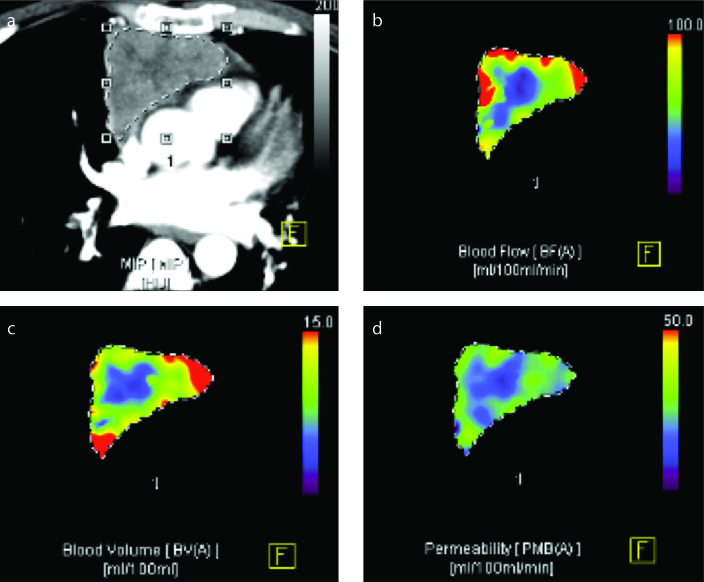
Figure 3.
a–d. A 36-year-old patient with a pathologic diagnosis of non-small cell lung cancer. The MIP image (a) shows a mildly heterogeneous midline mass at the anterior mediastinum. Corresponding blood flow map (b) shows homogeneously decreased blood flow in the center of the lesion. Blood volume map (c) also shows low values. Corresponding permeability surface map (d) shows areas with decreased permeability within the lesion.
Though BF and BV values were higher in thymoma in comparison to thymic hyperplasia, the difference was not statistically significant (Table). BF, BV, and PS values were higher in thymoma compared with lymphoma; however, only the difference between BV values reached statistical significance (Table).
Comparison of perfusion values of thymomas with those of malignant tumors (lymphoma, thymic carcinoma, and invasive lung cancer) revealed significantly higher BF and BV values in thymoma (Table).
Discussion
In the recent literature, there is no study concerning the differences in perfusion characteristics of anterior mediastinum lesions. Our study revealed that CT perfusion values (BF and BV) of thymomas were significantly different from malignant tumors of anterior mediastinum including lymphoma, thymic carcinoma, and invasive lung cancer. In contrast, we did not find any significant difference between CT perfusion values of thymoma and thymic hyperplasia.
The numerous different pathologic lesions in the anterior mediastinum may mimic thymic pathologies leading to diagnostic challenges and invasive therapeutic procedures including thymectomy (5, 13). Thus, differential diagnosis of benign thymic epithelial tumors from other malignant anterior mediastinal tumors has a clinical impact in patient management. In a study comprising 127 patients with anterior mediastinal lesions, the correct diagnosis was achieved in only 61% of patients by CT and in %56 by MRI (14).
CT perfusion is an alternative functional imaging modality that is gaining wider usage, particularly in oncology. CT perfusion allows rapid and quantitative assessment of tissue hemodynamics, thereby providing valuable information in tumor staging and response to therapy evaluation (12). CT perfusion reflects tissue vascularization and angiogenesis and can theoretically discriminate neoplastic tissue from non-neoplastic tissue. The results of the current study show that CT perfusion can help to differentiate between thymoma and malignant lesions of the anterior mediastinum including lymphoma, thymic carcinoma, and invasive lung cancer.
Thymoma is the most common anterior mediastinal mass in adults. On CT, thymomas are homogenous soft-tissue masses with sharp borders and a lobulated, round, or oval shape (13). Although, bipyramidal shape and presence of intercalated fat were pathognomonic for thymic hyperplasia, not all of them exhibit these features on CT. Ackman et al. (4) showed that intercalated fat was not observed on CT in half of the thymic hyperplasia cases. Therefore, chemical shift MRI may provide diagnostic clues to differentiate between thymic hyperplasia and thymoma, based on the signal loss on opposed-phase images in thymic hyperplasia suggestive of microscopic fat (13). Epithelial thymic neoplasms do not demonstrate microscopic fat by histopathology and do not demonstrate a decrease in signal on opposed-phase images (13). In our study, BF, BV, and PS values were lower in thymic hyperplasia compared with thymoma; however, the difference failed to reach a statistically significant level.
Lymphoma in anterior mediastinum is often seen in the setting of disseminated disease, most commonly in Hodgkin’s disease (13). In lymphoma, CT may show irregular contours, surface lobulation without vascular invasion with associated mediastinal lymphadenopathy and pleural effusion (2, 13). In general, differentiation of lymphoma from other thymic lesions, particularly thymoma, is difficult on the basis of imaging findings alone, and diagnosis may require invasive procedures (15). In our study, BV was significantly lower in lymphoma compared with thymoma, enabling diagnosis by CT perfusion. Also, BF and BV values were significantly higher in thymoma compared with malignant lesions including lymphoma, thymic carcinoma, and invasive lung cancer. We suggested that the low CT perfusion values of non-thymoma tumors in the present study might be related to presence of necrosis in non-thymoma tumors. It has been shown that predominance of a necrotic or cystic component and heterogeneous enhancement were much more common in thymic cancer compared with thymoma (16). In support of this, in a study by Sakai et al. (9) using dynamic MRI for anterior mediastinal lesions, the mean peak of the time intensity curve was significantly shorter for thymoma than for non-thymoma malignant tumors. In a study comparing thymoma with non-thymoma malignant tumors, Sakai et al. (9) found early contrast peak on dynamic MRI; similarly, higher CT perfusion values (BF and BV) were observed in our study. Both studies indicate that dynamic MRI and CT perfusion may be useful in the differentiation of thymoma from non-thymoma malignant tumors.
There were several major limitations to our study. First, the sample size was small, and it was determined without a power analysis due to the relatively rare incidences. In particular, we were not able to evaluate the CT perfusion values among different grade thymomas. CT perfusion values for the thymoma group had a relatively high standard deviation that might be related to grouping different stages of thymoma under a single group. In future, studies with larger sample sizes should be performed to clarify the efficacy of CT perfusion for diagnosing anterior mediastinal tumors. In addition, malignant lesions did not include germ cell tumor and thyroid lesions. Second, since we excluded patients with myasthenia gravis, our thymoma group is representative of a subgroup of patients with thymoma. Third, we did not obtain pathologic proof of the diagnosis in four thymic hyperplasia patients but performed follow-up chemical shift MRI for confirmation. Although chemical shift MRI is helpful in differential diagnosis, in some cases thymic hyperplasia may not be suppressed (17). In addition, potential pitfalls of CT perfusion should be kept in mind, such as the use of ionizing radiation, examination of a restricted slab of tissue, and interference in measurements from nearby vascular and bony structures.
In conclusion, CT perfusion imaging offers valuable information in differentiating thymoma from lymphoma, thymic carcinoma, and invasive lung cancer in the anterior mediastinum. Further studies with larger patient sample sizes are needed to evaluate the role of CT perfusion in differentiating among anterior mediastinal lesions.
Main points.
Perfusion computed tomography (CT) is a promising technique for diagnosis of anterior mediastinal solid tumors.
Perfusion CT values were significantly higher in thymomas compared with lymphoma and other malignant tumors of anterior mediastinum.
Blood flow and blood volume values were higher in thymomas compared with thymic hyperplasia; however, the difference was not statistically significant.
Perfusion CT can differentiate between thymomas and non-thymoma malignant tumors, reducing the rates of non-therapeutic thymectomies.
Acknowledgements
We would like to thank our radiographers Rahmi Eroğlu and Deniz Kırkan for excellent assistance.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Shin KE, Yi CA, Kim TS, et al. Diffusion-weighted MRI for distinguishing non-neoplastic cysts from solid masses in the mediastinum: problem-solving in mediastinal masses of indeterminate internal characteristics on CT. Eur Radiol. 2014;24:677–684. doi: 10.1007/s00330-013-3054-0. https://doi.org/10.1007/s00330-013-3054-0. [DOI] [PubMed] [Google Scholar]
- 2.Tomiyama N, Honda O, Tsubamoto M, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol. 2009;69:280–288. doi: 10.1016/j.ejrad.2007.10.002. https://doi.org/10.1016/j.ejrad.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Seki S, Koyama H, Ohno Y, et al. Diffusion-weighted MR imaging vs. multi-detector row CT: Direct comparison of capability for assessment of management needs for anterior mediastinal solitary tumors. Eur J Radiol. 2014;83:835–842. doi: 10.1016/j.ejrad.2014.01.005. https://doi.org/10.1016/j.ejrad.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Ackman JB, Verzosa S, Kovach AE, et al. High rate of unnecessary thymectomy and its cause. Can computed tomography distinguish thymoma, lymphoma, thymic hyperplasia, and thymic cysts? Eur J Radiol. 2015;84:524–533. doi: 10.1016/j.ejrad.2014.11.042. https://doi.org/10.1016/j.ejrad.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 5.Nasseri F, Eftekhari F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiographics. 2010;30:413–428. doi: 10.1148/rg.302095131. https://doi.org/10.1148/rg.302095131. [DOI] [PubMed] [Google Scholar]
- 6.Kent MS, Wang T, Gangadharan SP, Whyte RI. What is the prevalence of a “nontherapeutic” thymectomy? Ann Thorac Surg. 2014;97:276–282. doi: 10.1016/j.athoracsur.2013.07.121. https://doi.org/10.1016/j.athoracsur.2013.07.121. [DOI] [PubMed] [Google Scholar]
- 7.Ferdinand B, Gupta P, Kramer EL. Spectrum of thymic uptake at 18F-FDG PET. Radiographics. 2004;24:1611–1616. doi: 10.1148/rg.246045701. https://doi.org/10.1148/rg.246045701. [DOI] [PubMed] [Google Scholar]
- 8.Higuchi T, Taki J, Kinuya S, et al. Thymic lesions in patients with myasthenia gravis: characterization with thallium 201 scintigraphy. Radiology. 2001;221:201–206. doi: 10.1148/radiol.2211001047. https://doi.org/10.1148/radiol.2211001047. [DOI] [PubMed] [Google Scholar]
- 9.Sakai S, Murayama S, Soeda H, Matsuo Y, Ono M, Masuda K. Differential diagnosis between thymoma and non-thymoma by dynamic MR imaging. Acta Radiol. 2002;43:262–268. doi: 10.1080/j.1600-0455.2002.430306.x. https://doi.org/10.1034/j.1600-0455.2002.430306.x. [DOI] [PubMed] [Google Scholar]
- 10.Takahashi K, Inaoka T, Murakami N, et al. Characterization of the normal and hyperplastic thymus on chemical-shift MR imaging. AJR Am J Roentgenol. 2003;180:1265–1269. doi: 10.2214/ajr.180.5.1801265. https://doi.org/10.2214/ajr.180.5.1801265. [DOI] [PubMed] [Google Scholar]
- 11.Yabuuchi H, Matsuo Y, Abe K, et al. Anterior mediastinal solid tumours in adults: characterisation using dynamic contrast-enhanced MRI, diffusion-weighted MRI, and FDG-PET/CT. Clin Radiol. 2015;70:1289–1298. doi: 10.1016/j.crad.2015.07.004. https://doi.org/10.1016/j.crad.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Trojanowska A, Trojanowski P, Bisdas S, et al. Squamous cell cancer of hypopharynx and larynx - evaluation of metastatic nodal disease based on computed tomography perfusion studies. Eur J Radiol. 2012;81:1034–1039. doi: 10.1016/j.ejrad.2011.01.084. https://doi.org/10.1016/j.ejrad.2011.01.084. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein AJ, Oliva I, Honarpisheh H, Rubinowitz A. A tour of the thymus: a review of thymic lesions with radiologic and pathologic correlation. Can Assoc Radiol J. 2015;66:5–15. doi: 10.1016/j.carj.2013.09.003. https://doi.org/10.1016/j.carj.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Marom EM. Advances in thymoma imaging. J Thorac Imaging. 2013;28:69–80. doi: 10.1097/RTI.0b013e31828609a0. https://doi.org/10.1097/RTI.0b013e31828609a0. [DOI] [PubMed] [Google Scholar]
- 15.Nishino M, Ashiku SK, Kocher ON, Thurer RL, Boiselle PM, Hatabu H. The thymus: a comprehensive review. Radiographics. 2006;26:335–348. doi: 10.1148/rg.262045213. https://doi.org/10.1148/rg.262045213. [DOI] [PubMed] [Google Scholar]
- 16.Sadohara J, Fujimoto K, Muller NL, et al. Thymic epithelial tumors: comparison of CT and MR imaging findings of low- risk thymomas, high-risk thymomas, and thymic carcinomas. Eur J Radiol. 2006;60:70–79. doi: 10.1016/j.ejrad.2006.05.003. https://doi.org/10.1016/j.ejrad.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Ackman JB, Mino-Kenudson M, Morse CR. Nonsuppressing normal thymus on chemical shift magnetic resonance imaging in a young woman. J Thorac Imaging. 2012;27:196–198. doi: 10.1097/RTI.0b013e318249936a. https://doi.org/10.1097/RTI.0b013e318249936a. [DOI] [PubMed] [Google Scholar]