Abstract
Summary
One-year mortality following a fracture was greater for men compared to women, varied markedly between regions in England with the lowest rates in the London region, and was higher among black women compared to white women. The excess in mortality did not change during the study period.
Introduction
Fractures are associated with increased mortality. With the shift towards an increasingly elderly demography, and so increasing numbers of fractures, the impact of such events on mortality is of key public health importance. Therefore, we aimed to present up to date mortality rates following fracture in England.
Methods
This was a population-based study within the Clinical Practice Research Datalink, linked to death certificates (1 January 2001 and 31 December 2011). Subjects were followed from their first fracture (hip, wrist, humerus, clinical spine, ribs or pelvis) until death for up to one year. Rate ratios (RRs) were estimated for one-year mortality, stratified by sex, 5-year age categories, ethnicity, and geographical region. Excess mortality was presented as Standardized Mortality Ratios (SMRs).
Results
One-year mortality following fracture increased with age and was higher for men. Black women (RR 1.77; 95% CI: 1.00-3.12) and women with other ethnicities (RR 1.59, 95% CI: 1.16-2.16) were at higher risk of death when compared to white women. Mortality was higher among women in almost all regions when compared to the London region, with the highest risk in the East Midlands (37% higher). The one-year mortality risk was more than 3-fold higher after fracture as compared to the general population (adjusted [adj.] SMR: 3.15, 95% CI: 3.09 – 3.26) and did not change during the study period. Major causes of death were neoplasms, respiratory diseases, and circulatory diseases.
Conclusion
This study provides up to date mortality outcomes following fracture in England, and will aid allocation of healthcare provision to those at greatest need.
Keywords: Osteoporosis, epidemiology, mortality, comobidity
Background
Osteoporosis frequently results in fractures and is a major public health concern. The remaining lifetime risk for sustaining any fracture from the age of 50 years has been estimated to be as high as 53% among women and 21% among men in the United Kingdom [1]. The increased risk of death following hip and spinal fractures is well established, and emerging evidence shows that other fracture types are also associated with increased mortality rates [2–4]. The excess mortality is highest for fractures of the hip, where the risk of death is twice that of the general population of the same age, and is even higher among men (3-4 fold higher risk in the first year compared to the general population) [5, 6]. Fractures may also lead to severe morbidity in terms of pain, loss of mobility and loss of independence. Importantly, this burden will continue to increase, since the total number of fractures has been projected to rise substantially over the coming decades due to the ageing of the population [7].
Because of this projected increase in the total number of fractures, it is important to update the epidemiology of the associated mortality outcome. A previous study of post-fracture mortality in England and Wales sampled 5 million adults from the General Practice Research Database (GPRD, now known as the Clinical Practice Research Datalink [CPRD]) during the period 1988-1998, but was unable to stratify the post-fracture mortality risk by geographical region, ethnicity or cause of death [1]. In addition, secular trends for excess mortality after fractures are scarce and remain unknown for fractures other than the hip over the past decade in the United Kingdom [6]. Therefore, we used records from the Clinical Practice Research Datalink linked to death certificates to update the epidemiology of post-fracture mortality, stratified by age, sex, geographical region, ethnicity, calendar year, and the major causes of death.
Methods
Source population
We undertook a cohort study within the Clinical Practice Research Datalink (CPRD) (www.cprd.com, formerly known as the General Practitioner Research Database). This database contains computerised medical records of 674 primary care practices in the United Kingdom, representing approximately 6.9% of the total population [8]. Data recorded in the CPRD include demographic information, laboratory tests, specialist referrals, hospital admissions, prescription details, and lifestyle variables such as body mass index (BMI), smoking, and alcohol consumption. Previous studies have shown a high validity of fracture registration (>90% of fractures were confirmed) [9], and high degrees of accuracy and completeness of these data have been shown for other diagnoses and for smoking status [10–12]. The source population was restricted to practices from the Clinical Practice Research Datalink that were linked individually and anonymously to death certificate recordings of the Office of National Statistics. The death certificate lists the date and the cause(s) of death. Death certificates were available from January 1998 to January 2012. Linkage was eligible for 65% of practices, and these practices have been shown to be representative of the broader group of practices included in CPRD [13].
Study population
The study population consisted of all patients aged ≥ 50 years with a CPRD Read code for fracture (clinical spine, wrist, hip, humerus, rib, pelvis) between 1 January 2001 and 31 December 2011. The index date was defined as the first record for fracture, and all patients were required to have not sustained such a fracture before the index date. Patients with a code for unspecified fractures or unspecified femur fractures before the index date were excluded, since it was uncertain if the index fracture was actually the first fracture, according to the definition above, for that patient. In sensitivity analyses, the study population was restricted to patients who sustained a fracture according to the FRAX® definition of fractures (first of hip, clinical spine, forearm, humerus). For both fracture definitions, it was not possible to categorise fractures into low or high trauma since the degree of trauma leading to a fracture is not reliably captured in the CPRD. It was also not possibly to reliably ascertain whether a fracture was secondary to specific morbidities. Therefore, some of the included fractures may have been pathological or due to high-trauma.
Outcome
All patients were followed-up from the index date to the patient’s death as recorded on the death certificate or the study end date (365 days following the index date), whichever came first.
Statistical analyses
Rate ratios (RRs) were estimated for the risk of one-year mortality after fracture, stratified by sex, 5-year age categories, ethnicity (white, black, mixed, other [mainly Arab], south Asian, unknown), and geographical region in England. Excess mortality was presented as Standardized Mortality Ratios (SMRs). Age- and sex-specific numbers of observed deaths were extracted from the UK Office of National Statistics using the 21st Century Mortality dataset, England & Wales 2001–12. This was undertaken for males and females, by 5-year age-categories and for each calendar year and included deaths from all causes and from the underlying cause of death. Using the population estimates at mid-year and the number of deaths in the same year, age- and sex-specific mortality rates were calculated for the reference population. The expected number of deaths was calculated by multiplying the number of fracture patients per age- and sex-stratum by the age- and sex-specific mortality rates in the reference population for that same stratum. The observed number of deaths for each stratum in the study population were extracted from the linked CPRD – ONS data. The 95% Confidence Intervals for the SMRs were calculated according to the method of Rothman and Greenland [14]. SMRs were adjusted for age, sex, and calendar year. The Poisson test for trend was used to investigate whether the SMRs changed significantly over the study period. Analyses were performed using SAS V.9.2 (SAS, Cary, North Carolina, USA). A p value of < 0.05 was considered statistically significant.
Results
One-year mortality after fracture by age and sex
There were 22,929 men and 59,446 women with death certificate data available following a fracture of the hip, spine, forearm, humerus, ribs, or pelvis. The mean (SD) ages were 72.5 (12.5) years and 75.5 (12.1) years respectively. Amongst those with known ethnic origin recorded, 98.2% were of white ethnicity. The North West accounted for the largest proportion of individuals (17.4%), with North East (2.5%), Yorkshire and The Humber (4.7%), and East Midlands (3.2%) somewhat lower than for the other areas, which ranged from 10.2% to 13.8% contribution. A total of 11,217 deaths were observed within one year following a fracture of the hip, clinical spine, forearm, humerus, ribs, or pelvis over a total of 66,300 person-years of follow-up. The mortality rate within one year following fracture increased with age for both men (Table 1) and women (Table 2). Among men aged 50 – 54 years, the mortality rate was 2.3 per 100 person-years, which increased to 86.4 per 100 person-years for those aged 90 years or older, such that death was 35.4 times more likely at age 90+ years than at 50 – 54 years (95 % Confidence Interval [CI] for the Rate Ratio [RR]: 25.8 – 48.4). Among women, the mortality rates were lower than in men for all age categories and the corresponding rate ratio for one-year mortality was 23.7 (95% CI: 17.9-31.4). Results were similar for the FRAX definition of major osteoporotic fracture (Supplementary Tables 1 and 2), were there were a total of 10,175 deaths over 59,343 person-years of follow-up.
Table 1.
One-year all-cause mortality after fracture for males stratified by age, ethnicity, socioeconomic status, and region (crude rates).
| N deaths | IR (per 100 py) | IR 95% CI | RR (95% CI) | ||
|---|---|---|---|---|---|
| By age categories | |||||
| 50 – 54 | 41 | 2.3 | 1.6 | 3.0 | Reference |
| 55 – 59 | 80 | 3.5 | 2.8 | 4.3 | 1.56 (1.07 - 2.27) |
| 60 – 64 | 130 | 5.8 | 4.8 | 6.9 | 2.62 (1.84 - 3.72) |
| 65 – 69 | 194 | 9.9 | 8.5 | 11.3 | 4.37 (3.12 - 6.11) |
| 70 – 74 | 305 | 15.0 | 13.3 | 16.7 | 6.58 (4.75 - 9.12) |
| 75 – 79 | 550 | 24.3 | 22.3 | 26.3 | 10.5 (7.62 - 14.4) |
| 80 – 84 | 921 | 38.9 | 36.4 | 41.4 | 16.5 (12.1 - 22.6) |
| 85 – 89 | 980 | 54.8 | 51.3 | 58.2 | 23.1 (16.9 - 31.6) |
| 90 + | 877 | 86.4 | 80.7 | 92.1 | 35.4 (25.8 - 48.4) |
| By ethnicity | |||||
| White | 3279 | 21.9 | 21.1 | 22.6 | Reference |
| Black | 10 | 21.1 | 8.1 | 34.5 | 1.30 (0.70 - 2.41) |
| Mixed | 3 | 22.0 | 2.8 | 45.7 | 1.38 (0.44 - 4.27) |
| Other | 17 | 16.2 | 8.5 | 23.9 | 0.98 (0.61 - 1.58) |
| South Asian | 25 | 14.5 | 8.8 | 20.2 | 1.06 (0.71 - 1.57) |
| Unknown | 744 | 32.0 | 29.7 | 34.3 | 1.63 (1.50 - 1.76) |
| By region | |||||
| London | 390 | 22.3 | 20.1 | 24.5 | Reference |
| East Midlands | 137 | 23.9 | 19.9 | 27.9 | 1.04 (0.85 - 1.26) |
| East of England | 501 | 24.5 | 22.3 | 26.6 | 1.02 (0.90 - 1.17) |
| North East | 96 | 19.9 | 15.9 | 23.9 | 0.92 (0.74 - 1.15) |
| North West | 722 | 22.7 | 21.0 | 24.3 | 1.10 (0.97 - 1.24) |
| South Central | 511 | 22.9 | 20.9 | 24.9 | 0.96 (0.84 - 1.10) |
| South East Coast | 495 | 22.9 | 20.9 | 24.9 | 0.97 (0.85 - 1.11) |
| South West | 561 | 23.1 | 21.2 | 25.0 | 0.92 (0.81 - 1.04) |
| West Midlands | 459 | 22.8 | 20.7 | 24.9 | 1.05 (0.91 - 1.20) |
| Yorkshire & The Humber | 206 | 26.2 | 22.6 | 29.8 | 1.20 (1.02 - 1.42) |
IR: incidence rate; RR: rate ratio; py: person-years
Table 2.
One-year all-cause mortality after fracture among women stratified by age, ethnicity, socioeconomic status, and region (crude rates).
| N deaths | IR (per 100 py) | IR 95% CI | RR (95% CI) | ||
|---|---|---|---|---|---|
| By age categories | |||||
| 50 – 54 | 50 | 1.9 | 1.4 | 2.5 | Reference |
| 55 – 59 | 74 | 1.7 | 1.3 | 2.1 | 0.89 (0.62 - 1.27) |
| 60 – 64 | 139 | 2.9 | 2.4 | 3.4 | 1.51 (1.09 - 2.09) |
| 65 – 69 | 197 | 4.0 | 3.4 | 4.5 | 2.03 (1.49 - 2.77) |
| 70 – 74 | 410 | 7.0 | 6.3 | 7.7 | 3.54 (2.64 - 4.74) |
| 75 – 79 | 752 | 10.6 | 9.8 | 11.3 | 5.27 (3.96 - 7.02) |
| 80 – 84 | 1345 | 17.3 | 16.4 | 18.3 | 8.52 (6.43 - 11.3) |
| 85 – 89 | 1836 | 28.0 | 26.7 | 29.3 | 13.7 (10.3 - 18.1) |
| 90 + | 2336 | 50.1 | 48.0 | 52.1 | 23.7 (17.9 - 31.4) |
| By ethnicity | |||||
| White | 5632 | 13.8 | 13.4 | 14.1 | Reference |
| Black | 12 | 14.7 | 6.4 | 22.9 | 1.77 (1.00 - 3.12) |
| Mixed | 5 | 13.1 | 1.6 | 24.7 | 1.97 (0.82 - 4.74) |
| Other | 40 | 15.9 | 11.0 | 20.9 | 1.59 (1.16 - 2.16) |
| South Asian | 24 | 7.5 | 4.5 | 10.4 | 0.94 (0.63 - 1.41) |
| Unknown | 1426 | 20.7 | 19.6 | 21.8 | 1.49 (1.40 - 1.58) |
| By region | |||||
| London | 642 | 13.1 | 12.1 | 14.2 | Reference |
| East Midlands | 257 | 16.8 | 14.8 | 18.9 | 1.37 (1.18 - 1.58) |
| East of England | 861 | 15.5 | 14.5 | 16.5 | 1.19 (1.07 - 1.31) |
| North East | 164 | 13.4 | 11.4 | 15.5 | 1.20 (1.01 - 1.42) |
| North West | 1293 | 15.3 | 14.5 | 16.2 | 1.28 (1.16 - 1.40) |
| South Central | 941 | 15.2 | 14.2 | 16.2 | 1.16 (1.05 - 1.28) |
| South East Coast | 868 | 14.3 | 13.3 | 15.2 | 1.08 (0.98 - 1.20) |
| South West | 982 | 14.6 | 13.7 | 15.5 | 1.06 (0.96 - 1.17) |
| West Midlands | 782 | 14.2 | 13.2 | 15.2 | 1.16 (1.04 - 1.28) |
| Yorkshire & The Humber | 349 | 15.1 | 13.5 | 16.7 | 1.18 (1.04 - 1.35) |
IR: incidence rate; RR: rate ratio; py: person-years
One-year mortality after fracture by ethnicity and geographic location
Patients without a record for ethnicity had significantly higher mortality rates as compared to white patients, which was observed for men (RR 1.63, 95% CI: 1.50 – 1.76) and for women (RR 1.49, 95% CI: 1.40 – 1.58) (Tables 1 and 2). Among women, also blacks (RR 1.77, 95% CI: 1.00 – 3.12) and those with other ethnicities were at higher risk of death (RR 1.59, 95% CI: 1.16 – 2.16). With regard to geographical region, one-year mortality was significantly higher for men in Yorkshire and the Humber (RR 1.20) when compared to the London area (Table 1). Among women, almost all regions were associated with significantly higher mortality as compared to the London region, ranging from a 16% higher risk in the West Midlands and the South-Central region to 37% in the East Midlands (Table 2). Similar results were seen for all subgroups by age, ethnicity and region following a fracture when the FRAX-definition was applied (Supplementary Tables 1 and 2).
Causes of mortality and rates of death following fracture
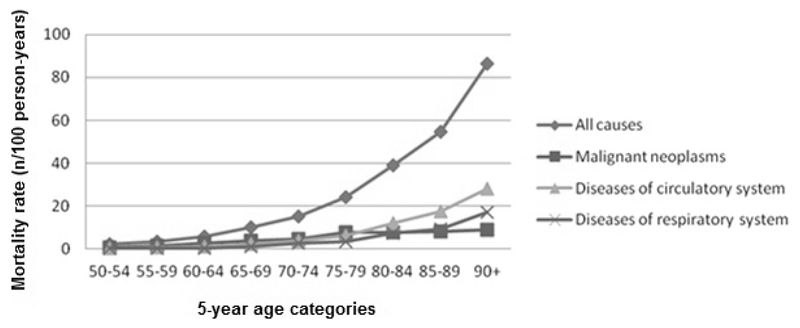
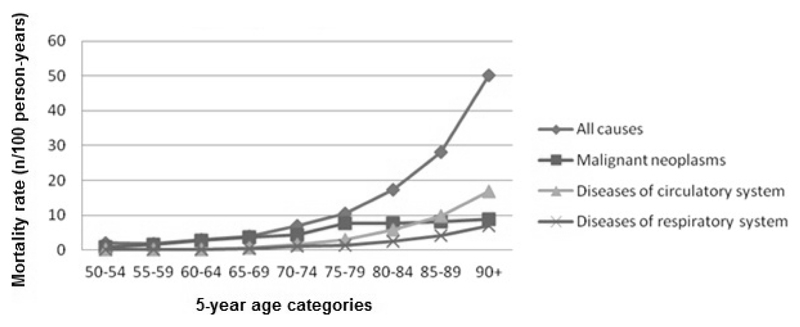
Figure 1 shows the age-specific mortality rates from all-causes and for the three major causes of death in the year following a fracture in men. The major causes of death included malignant neoplasms, diseases of the respiratory system and diseases of the circulatory system. Although the mortality rates were lower in women across all age-categories, the major causes of death were similar as compared to men (Figure 2).
Figure 1.
Age-specific one-year mortality rates after fracture in men, by cause of death
Figure 2.
Age-specific one-year mortality rates after fracture in women, by cause of death
Mortality rates after fracture compared to the general population
The one-year mortality risk was more than 3-fold higher after fracture as compared to the general population (adjusted [adj.] Standardized Mortality Ratio [SMR]: 3.15, 95% CI: 3.09 – 3.26) (Table 3). Excess mortality was especially high among men (adj. SMR 4.32, 95% CI: 4.19 - 4.46). Very similar results were obtained for the FRAX-definition of fracture. In addition, the excess in mortality after fracture did not change during the study period (Poisson test for trend, p value 1.00) and a similar result was found when the FRAX-definition for fracture was used (Poisson test for trend, p value 0.99) (Supplementary Table 3). When stratified by region, the adj. SMR is lowest in the London region, in the South West and the South East Coast (Table 3). Those with unknown ethnicity had higher adj. SMR (4.79, 95% CI: 4.59 - 4.99) as compared to white patients (adj. SMR 2.90, 95% CI: 2.84 - 2.96) (Table 3). Finally, when stratified by the three major causes of death, the adj. SMR ranged between 2.5 (diseases of the circulatory system) to 3.0 (diseases of the respiratory system), and was similar for the FRAX-definition of fracture (Supplementary Table 3).
Table 3.
One-year excess mortality from all causes after fracture, stratified by sex, index year, and major causes of death (adjusted for age).
| N deaths observed | N deaths expected | SMR (95% CI) | |
|---|---|---|---|
| Overall* | 11217 | 3561 | 3.15 (3.09 - 3.21) |
| By sex** | |||
| Male | 4078 | 943 | 4.32 (4.19 - 4.46) |
| Female | 7139 | 2618 | 2.73 (2.66 - 2.79) |
| By index year*** | |||
| 2001 | 855 | 297 | 2.88 (2.68 - 3.07) |
| 2002 | 1007 | 318 | 3.17 (2.98 - 3.37) |
| 2003 | 1153 | 346 | 3.34 (3.14 - 3.53) |
| 2004 | 1148 | 342 | 3.35 (3.16 - 3.55) |
| 2005 | 1061 | 353 | 3.01 (2.82 - 3.19) |
| 2006 | 1075 | 333 | 3.23 (3.04 - 3.42) |
| 2007 | 1133 | 348 | 3.26 (3.07 - 3.45) |
| 2008 | 1122 | 347 | 3.23 (3.04 - 3.42) |
| 2009 | 1006 | 358 | 2.81 (2.64 - 2.98) |
| 2010 | 1022 | 349 | 2.93 (2.75 - 3.11) |
| 2011 | 635 | 171 | 3.72 (3.43 - 4.01) |
| By ethnicity*‡ | |||
| White | 8911 | 3075 | 2.90 (2.84 - 2.96) |
| Unknown | 2170 | 453 | 4.79 (4.59 - 4.99) |
| By region *‡ | |||
| London | 1032 | 377 | 2.87 (2.70 - 3.05) |
| East of England | 1362 | 418 | 3.26 (3.09 - 3.43) |
| North West | 2015 | 582 | 3.46 (3.31 - 3.61) |
| South Central | 1452 | 464 | 3.13 (2.97 - 3.29) |
| South East Coast | 1363 | 458 | 2.97 (2.82 - 3.13) |
| South West | 1543 | 538 | 2.87 (2.73 - 3.01) |
| West Midlands | 1241 | 386 | 3.22 (3.04 - 3.39) |
| By cause of death* | |||
| Neoplasms | 2044 | 737.9 | 2.77 (2.65 - 2.89) |
| Diseases of the respiratory system | 1694 | 565.4 | 3.00 (2.85 - 3.14) |
| Diseases of the circulatory system | 3449 | 1371.5 | 2.51 (2.43 - 2.60) |
SMR; standardized mortality ratio, 95% CI; 95% Confidence Interval
Adjusted for age, sex, index year; ** Adjusted for age, index year; *** Adjusted for age, sex
Not all categories are included due to a too low number of events in the missing categories
Discussion
In this population-based study, we have updated the epidemiology of mortality after fracture in England. The mortality risk increased with age, was higher for men, and there were marked differences in mortality according to the geographic location and ethnicity especially among women. Furthermore, the excess in one-year mortality after fracture did not change during the study period, with a 3.2-times higher risk of death as compared to the general population. Major causes of death were neoplasms, respiratory diseases, and circulatory diseases.
Age and sex
The higher mortality risk after fracture with increasing age, and in men as compared to women is consistent with previous literature [3, 15]. The reasons for the sex-difference in post-fracture mortality are not completely understood, and have been most comprehensively evaluated after hip fracture. Male hip fracture patients are on average 4 years younger, but sicker than their female counterparts [6, 16]. However, even after adjustment for age, drug use, and comorbidities, the sex-difference remained in several studies among hip fracture patients but also relative to the general population, which is in line with our results for the composite outcome of fracture. Unmeasured differences in frailty between men and women who sustain a fracture, or differences in complications such as infections and cardiovascular complications may further explain this finding [17]. However, with regard to the latter, we found the causes of death to be similar regardless of sex.
Ethnicity
Data on ethnic differences in mortality after fracture are scarce and have been reported solely after hip fracture. Our finding of a higher mortality rate in black women or women with another ethnicity (Arab) as compared to white women following a fracture is in line with most [18–21], but not all [22], studies that have addressed this issue after hip fracture. The underlying causes for this ethnic difference in survival may be multifactorial. Historical studies, published between 1996-2000, showed that after hip fracture, black patients were less likely to receive high-intensity rehabilitation in hospital [23] or post-discharge physical therapy [24] than white patients. Other potential causes are general, non-fracture related, differences in mortality by ethnicity caused by unmeasured factors such as severity of comorbid conditions, or socioeconomic factors, and warrants further investigation. Furthermore, the sex difference in the association between ethnicity and post-fracture mortality that was observed in this study also requires further investigation.
Geographic region
Stratification by region within England revealed substantial geographic differences in mortality rates among women. The differences in mortality seem to match the variation in deprivation levels across the regions in England, with higher levels of deprivation in the north of England than in the south. Increased mortality rates have been associated with higher levels of deprivation, which likely reflects underlying differences in income, smoking status and other factors that relate to health-related behaviour [25]. In 2014, the SMR in the general population was lowest in London at 9 percentage points below the national level and highest in the North East with mortality rates 14 percentage points above the national level [25]. Indeed, the SMRs in the present study are lowest in the London region and in the southern regions as compared to the northern regions. In the present study, however, no such pattern was observed among males, where only Yorkshire and the Humber showed significant higher mortality rates compared to the London area. The underlying causes for this different pattern compared to women remain to be elucidated.
Secular trends
While several studies have investigated secular changes in mortality post-hip fracture over recent years, very few have investigated whether there were changes in the difference in mortality between fracture patients and the general population [26–29]. Our finding of unchanged excess mortality post-fracture is in line with a prior study that was conducted among hip fracture patients in the CPRD, with linked information from death certificates [6]. We are not aware of any study that has evaluated a secular trend in relative mortality after the composite of fracture. The unchanged mortality outcome relative to the general population implies that the fracture-related mortality has not declined. Future investigations should focus on the cost benefit of targeted interventions including the role of multidisciplinary care, comorbidity management, nutrition, and pharmacological treatment where there is limited but conflicting evidence for reduced mortality with use of bisphosphonates (zoledronic acid) following hip fracture [16]. These interventions may be implemented through a Fracture Liaison Service [30], but it has been shown that there is great heterogeneity in quality of FLS services, which needs to be improved [31].
Strengths and limitations
This study presented mortality outcomes for a large representative sample of community-dwelling patients with fractures in England. Through linkage to death certificates we were able to reliably estimate mortality risk and the associated underlying cause of death. There are, however, several limitations that should be considered. First, it was not possible to categorise fractures as secondary to specific morbidities, or into low or high trauma since the degree of trauma leading to a fracture is not reliably captured in the CPRD. However, the patterns of mortality by age and gender are well in line with those previously reported. Second, a substantial number of individuals had missing data on ethnicity, which may have influenced ethnicity results. Improving database capture of ethnicity will aid in population studies. Furthermore, we were not able to adjust the stratification for geographical region by socioeconomic status. Although we have adjusted the standardized mortality ratio after fracture for age and sex, residual confounding may still have been present. Propensity score adjustment or matching by a comorbidity score may further reduce this confounding issue but we were not able to apply this method in this study. And finally, representativeness of the CPRD when stratified by geographical region and ethnicity has not been documented.
Conclusions
In conclusion, we have documented up-to-date age- and sex-specific mortality rates following fracture for England. We have shown marked differences in mortality according to the geographic region and ethnicity among women, but less so among men. Major causes of death were neoplasms, respiratory diseases, and circulatory diseases for both genders. And finally, the excess in one-year mortality after fracture did not change during the study period with a 3.2-fold higher risk of death as compared to the general population. Future investigations should focus on the cost benefit of targeted interventions for reducing the associated mortality outcome following fracture.
Supplementary Materials
Acknowledgements
The work was supported by a grant from the National Osteoporosis Society. This work was further supported by grants from the Medical Research Council, British Heart Foundation, Arthritis Research UK, National Institute for Health Research (NIHR) Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, and NIHR Musculoskeletal Biomedical Research Unit, University of Oxford.
Footnotes
Conflicts of Interest
Corinne Klop, Tjeerd P. van Staa, Cyrus Cooper, Nicholas C. Harvey and Frank de Vries report no conflicts of interest.
References
- [1].Van Staa TP, Dennison EM, Leufkens HGM, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29:517–522. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- [2].Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- [3].Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int. 2011;22:2439–48. doi: 10.1007/s00198-010-1480-2. [DOI] [PubMed] [Google Scholar]
- [4].Huntjens KMB, Kosar S, van Geel TACM, Geusens PP, Willems P, Kessels A, et al. Risk of subsequent fracture and mortality within 5 years after a non-vertebral fracture. Osteoporos Int. 2010;21:2075–82. doi: 10.1007/s00198-010-1178-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Haentjens P, Magaziner J, Colón-Emeric CS, van der Schueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–90. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Klop C, Welsing PMJ, Cooper C, Harvey NC, Elders PJM, Bijlsma JWJ, et al. Mortality in British hip fracture patients, 2000-2010: a population-based retrospective cohort study. Bone. 2014;66:171–7. doi: 10.1016/j.bone.2014.06.011. [DOI] [PubMed] [Google Scholar]
- [7].Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos. 2013;8:137. doi: 10.1007/s11657-013-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, Smeeth L. Data resource profile: clinical practice research datalink (CPRD) Int J Epidemiol. 2015 doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Van Staa TP, Abenhaim L, Cooper C, Zhang B, Leufkens HG. The use of a large pharmacoepidemiological database to study exposure to oral glucocorticoids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf. 2000;9:359–366. doi: 10.1002/1099-1557(200009/10)9:5<359::AID-PDS507>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- [10].Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69:4–14. doi: 10.1111/j.1365-2125.2009.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:e128–36. doi: 10.3399/bjgp10X483562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lewis JD, Brensinger C. Agreement between GPRD smoking data: a survey of general practitioners and a population-based survey. Pharmacoepidemiol Drug Saf. 2004;13:437–41. doi: 10.1002/pds.902. [DOI] [PubMed] [Google Scholar]
- [13].Gallagher AM, Puri S, van Staa TP. Linkage of the General Practice Research Database (GPRD) with other data sources. Pharmacoepidemiol Drug Saf. 2011;20:S230. [Google Scholar]
- [14].Rothman KJ, Greenland S, editors. Modern epidemiology. 2nd ed. Philadelphia: Lippincott-Raven; 1998. [Google Scholar]
- [15].Bliuc D, Nguyen TV, Eisman JA, Center JR. The impact of nonhip nonvertebral fractures in elderly women and men. J Clin Endocrinol Metab. 2014;99:415–423. doi: 10.1210/jc.2013-3461. [DOI] [PubMed] [Google Scholar]
- [16].Sattui SE, Saag KG. Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol. 2014;10:592–602. doi: 10.1038/nrendo.2014.125. [DOI] [PubMed] [Google Scholar]
- [17].Roche JJW, Wenn RT, Sahota O, Mora CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. doi: 10.1136/bmj.38643.663843.55. published 18 November 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–8. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63:867–72. doi: 10.1093/gerona/63.8.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–1150. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lu-Yao GL, Baron JA, Barrett JA, Fisher ES. Treatment and survival among elderly Americans with hip fractures: a population-based study. Am J Public Health. 1994;84:1287–1291. doi: 10.2105/ajph.84.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000-2011. J Orthop Surg Res. 2016;11:4. doi: 10.1186/s13018-015-0332-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hoenig H, Rubenstein L, Kahn K. Rehabilitation after hip fracture–equal opportunity for all? Arch Phys Med Rehabil. 1996;77:58–63. doi: 10.1016/s0003-9993(96)90221-x. [DOI] [PubMed] [Google Scholar]
- [24].Harada ND, Chun A, Chiu V, Pakalniskis A. Patterns of rehabilitation utilization after hip fracture in acute hospitals and skilled nursing facilities. Med Care. 2000;38:1119–1130. doi: 10.1097/00005650-200011000-00006. [DOI] [PubMed] [Google Scholar]
- [25].Office of National Statistics. Statistical bulletin: deaths registered in England and Wales. 2014 [Google Scholar]
- [26].Wu TY, Jen MH, Bottle A, Liaw CK, Aylin P, Majeed A. Admission rates and in-hospital mortality for hip fractures in England 1998 to 2009: time trends study. J Public Health (Oxf) 2010;33:284–91. doi: 10.1093/pubmed/fdq074. [DOI] [PubMed] [Google Scholar]
- [27].Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001-2009. Age Ageing. 2013;42:229–33. doi: 10.1093/ageing/afs177. [DOI] [PubMed] [Google Scholar]
- [28].Gordon J, Pham CT, Karnon J, Crotty M. Monitoring progress in the management of hip frcture in South Australia, Australia. Arch Osteoporos. 2012;7:267–73. doi: 10.1007/s11657-012-0107-y. [DOI] [PubMed] [Google Scholar]
- [29].Brauer CA, Coca-Perraillon M, Cutlet DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–79. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Huntjens KMB, van Geel TACM, van den Bergh JPW, van Helden S, Willems P, et al. Fracture Liaison Service: Impact on Subsequent Nonvertebral Fracture Incidence and Mortality. J Bone Joint Surg Am. 2014;96:e29. doi: 10.2106/JBJS.L.00223. (1-8) [DOI] [PubMed] [Google Scholar]
- [31].Javaid MK, Kyer C, Mitchell PJ, Chana J, Moss C, Edwards MH, et al. Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture Best Practice Framework tool. Osteoporos Int. 2015;26:2573–8. doi: 10.1007/s00198-015-3192-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.