Abstract
Background/Aims
Chronic thromboembolic pulmonary hypertension (CTEPH) is a life-threatening complication after acute pulmonary embolism (APE) and is associated with substantial morbidity and mortality. This study aimed to investigate the incidence of CTEPH after APE in Korea and to determine echocardiographic predictors of CTEPH.
Methods
Among 381 patients with APE confirmed by chest computed tomography (CT) between January 2007 and July 2013, 246 consecutive patients with available echocardiographic data were enrolled in this study. CTEPH was defined as a persistent right ventricular systolic pressure (RVSP) greater than 35 mmHg on echocardiography during follow-up and persistent pulmonary embolism on the follow-up CT.
Results
Fifteen patients (6.1%) had CTEPH. The rate of right ventricular (RV) dilatation (66.7% vs. 28.1%, p = 0.002) and the RVSP (75.5 mmHg vs. 39.0 mmHg, p < 0.001) were significantly higher in the CTEPH group. D-dimers, RV dilatation, RV hypertrophy, RVSP, and intermediate-risk APE were associated with the risk of CTEPH after APE (odds ratio [OR] 0.59, 5.11, 7.82, 1.06, and 4.86, respectively) on univariate analysis. RVSP remained as a significant predictor of CTEPH on multivariate analysis (OR, 1.056; 95% confidence interval, 1.006 to 1.109; p = 0.029).
Conclusions
This study showed that the incidence of CTEPH after APE in Korea was 6.1% and that initial RVSP by echocardiography was a strong prognostic factor for CTEPH.
Keywords: Hypertension, pulmonary; Pulmonary embolism; Echocardiography
INTRODUCTION
The prognosis of patients with chronic thromboembolic pulmonary hypertension (CTEPH) is variable, but the condition may be life threatening in some cases. CTEPH is characterized by chronic organized thrombi that obstruct the pulmonary vascular beds and lead to unfavorable clinical outcomes [1]. Increased pulmonary vascular resistance subsequently leads to progressive pulmonary hypertension (PH) and right heart failure. In the non-occluded areas, pulmonary arteriopathy indistinguishable from that of pulmonary arterial hypertension (PAH) can develop and contribute to disease progression [2]. It is important to determine predictive factors for the early detection of CTEPH that could lead to an improvement in quality of life and reduce the hemodynamic impact of this disease.
It is widely believed that the incidence of CTEPH is approximately 0.1% among patients who survive a pulmonary embolism. However, according to a more recent study, it appears to be more common, with an incidence ranging from 0.5% up to 3.8% [3].
European guidelines recommend that patients with acute pulmonary embolism (APE) who show signs of PH or right ventricular (RV) dysfunction at any time during their hospital stay should undergo follow-up echocardiography after discharge (usually after 3 to 6 months) to determine whether or not the PH has resolved [4]. However, it is difficult to perform this echocardiography in clinical practice for various reasons. This can result in a delayed diagnosis of CTEPH at a time when the disease has already advanced to a stage with severe vascular damage and right-side heart failure.
The purpose of this study was to assess the incidence and characteristics of CTEPH in Korean patients, and to identify risk factors for developing CTEPH after APE.
METHODS
Patient selection and follow-up
This was a single-center, retrospective observational study covering a period from January 2007 to July 2013 in Pusan National University Hospital. Patients with suspected pulmonary embolism underwent a standardized diagnostic work up [4]. Patients who had a diagnosis of APE, confirmed by contrast-enhanced computed tomography (CT), and had undergone an initial transthoracic echocardiographic examination were included in the analysis. All patients with APE were enrolled, regardless of any prior history of venous thromboembolism (VTE). Patients with a combined disease entity (e.g., severe chronic obstructive pulmonary disease, systemic sclerosis, or elevated left ventricular filling pressure) that could have caused non-thromboembolic PAH were excluded from the study.
Patients were treated according to the judgment of the attending physician. The therapeutic regimens used for pulmonary embolism were based on risk stratification and included unfractionated heparin and vitamin K antagonist (VKA), inferior vena cava filter and VKA, new oral anticoagulant, with thrombolysis and thromboembolectomy for hemodynamically unstable cases. Heparin was administered as an intravenous bolus of at least 5,000 IU, and was infused continuously to maintain an activated partial-thromboplastin time that was 1.5 to 2.5 times the control value. Oral anticoagulants were started during the first week and continued for at least 3 months if possible. The target international normalized ratio (INR) was 2.0 to 3.0, depending on the individual risk of recurrent VTE, anticoagulant treatment was continued beyond 3 months.
Follow-up of patients was performed after APE, in order to monitor the development of CTEPH on transthoracic echocardiography or contrast enhanced CT and to record any cause of death. Follow-up echocardiography was performed for patients who had otherwise unexplained persistent dyspnea, or where the attending physician deemed it clinically necessary. The patients were divided into two groups based on whether CTEPH developed or not. We evaluated the incidence of CTEPH after APE, the clinical and echocardiographic characteristics of the CTEPH group, and potential risk factors for developing CTEPH.
Echocardiography and contrast-enhanced CT
Routine transthoracic echocardiography for the assessment of RV function was performed and interpreted according to the guidelines of the American Society of Echocardiography (ASE) [5] by an experienced physician on the patient’s first hospital visit after APE had been confirmed by CT. RV diastolic diameters were measured at the level of the mitral and tricuspid valve tips during late diastole. Tricuspid annular plane systolic excursion was assessed in the M-mode presentation by placing a sample volume cursor in the tricuspid annulus and measuring the amount of longitudinal motion of the annulus at peak systole [6]. Tricuspid annular velocity (S’) was measured in the apical 4-chamber view by placing a tissue Doppler cursor on the lateral tricuspid annulus and measuring the peak velocity of this reference point during systole [7]. Tricuspid valve regurgitation was qualitatively assessed by color Doppler, and peak gradient was calculated using a simplified Bernoulli’s formula, based on the tricuspid regurgitant flow peak velocity [5].
Standard contrast-enhanced CT thromboembolism protocols were used in most cases for the diagnosis of APE and deep vein thrombosis (image acquisition beginning with a scanning delay of ~15 to 20 seconds after the start of the injection of contrast medium) [8]. The location of the thrombus and the pulmonary artery involved were recorded.
Definitions
CTEPH was defined as a state in which systolic and mean pulmonary artery pressures exceeded 35 and 25 mmHg, respectively, at rest on follow-up transthoracic echocardiography at least 6 months after the initial diagnosis of APE, while there was no evidence of elevated left ventricular filling pressure, chronic obstructive pulmonary disease, or congenital anomaly. Evidence of pouching, webs, or bands with or without post-stenotic dilatation, intimal irregularities, abrupt narrowing, or total occlusion of a pulmonary artery on follow-up contrast enhanced CT might be concomitant findings. Each of these findings is consistent with the presence of CTEPH [9].
RV dysfunction and other echocardiographic parameters used to assess RV morphology and function were defined according to the ASE guidelines [5] on the diagnosis and management of APE.
The severity of APE was stratified into three levels of risk of early mortality, based on the presence of risk markers (e.g., shock or hypotension, RV dysfunction, myocardial injury). Thus, patients with APE were classified into high-risk, intermediate-risk, or low-risk [10].
The following potential risk factors for CTEPH were considered: age, sex, type of initial treatment, severity of the pulmonary embolism at presentation, initial presentation with idiopathic pulmonary embolism or pulmonary embolism due to permanent risk factors, concomitant symptomatic deep-vein thrombosis at presentation, and a history of VTE [11].
Statistical analysis
Data characterized by a normal distribution are expressed as mean ± standard deviation. Parameters without such a distribution are expressed as median with maximum and minimum values. The Student t test or the Mann-Whitney U test was used for comparisons between two groups. The chi-square test was used to compare discrete variables. The impact of clinical and echocardiographic parameters on CTEPH was evaluated using univariate logistic regression, and multivariable analysis was used to identify significant risk factors using the enter method. The investigation of a diagnostic cutoff value was based on receiver operating characteristic (ROC) curves. Results are given as odds ratio (OR; 95% confidence interval [CI]) and data were considered significant at p < 0.05. SPSS version 22 (IBM Co., Armonk, NY, USA) was used for statistical analysis and calculation.
RESULTS
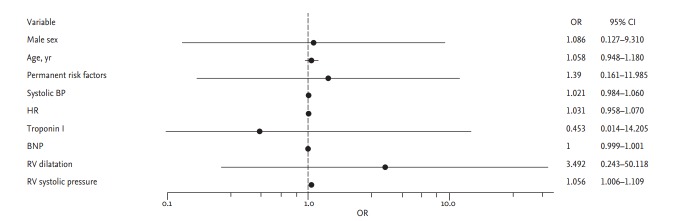
We identified 381 consecutive patients with APE confirmed by contrast-enhanced CT at baseline from January 2007 to July 2013. In total, 135 patients were excluded because they had no initial transthoracic echocardiographic data. Thus, 246 patients were assessed retrospectively (Fig. 1).
Figure 1.
Study f low diagram. CT, computed tomography; PTE, pulmonary thromboembolism; CTEPH, chronic thromboembolic pulmonary hypertension.
Fifteen patients (6.1%) developed CTEPH and 231 (93.9%) did not. Follow-up echocardiography and contrast-enhanced CT was used for the diagnosis of CTEPH during a median of 314 days. The baseline characteristics of the groups are shown in Table 1. There were no significant differences in baseline characteristics between groups, except that patients without CTEPH had higher admission levels of D-dimers (4.64 vs. 1.52, p = 0.002). Age and sex as potential risk factors for developing CTEPH did not show any differences between groups. Transient risk factors (e.g., recent operation, use of hormonal therapy, use of oral contraceptives, pregnancy, history of trauma) and permanent risk factors (e.g., prior VTE, malignancy, spinal cord injury, stroke, heart failure, family history of VTE) for APE and developing CTEPH did not differ between groups. The incidence of high-risk PE did not differ between groups (6.7% vs. 9.1%, p = 0.074).
Table 1.
Baseline characteristics
| Characteristic | CTEPH group (n = 15, 6.1%) | Non-CTEPH group (n = 231, 93.9%) | p value |
|---|---|---|---|
| Demographic characteristic | |||
| Mean age, yr | 70.8 ± 8.1 | 66.5 ± 12.7 | 0.190 |
| Male sex | 6 (40.0) | 92 (39.8) | 0.989 |
| Body mass index | 23.41 ± 2.81 | 24.13 ± 3.33 | 0.430 |
| Past history, % | |||
| History of operation | 5 (33.3) | 98 (42.4) | 0.489 |
| Malignancy | 4 (26.7) | 69 (29.9) | 1.000 |
| Bedridden state | 3 (20.0) | 69 (29.9) | 0.563 |
| Stroke | 3 (20.0) | 29 (12.6) | 0.423 |
| Chemotherapy | 2 (13.3) | 40 (17.3) | 1.000 |
| Lung disease | 5 (33.3) | 37 (16.0) | 0.084 |
| Spinal cord injury | 1 (6.7) | 8 (3.5) | 0.438 |
| Hormone therapy | 0 | 4 (1.7) | 1.000 |
| Pregnancy/peripartum | 0 | 2 (0.9) | 1.000 |
| Hematologic disease | 1 (6.7) | 12 (5.2) | 0.568 |
| Autoimmune disease | 1 (6.7) | 1 (0.4) | 0.118 |
| Oral contraceptives | 0 | 1 (0.4) | 1.000 |
| Symptoms at admission, % | |||
| Dyspnea | 12 (80.0) | 143 (61.9) | 0.181 |
| Chest pain | 3 (20.0) | 40 (17.3) | 0.731 |
| Cough | 0 | 13 (5.6) | 1.000 |
| Hemoptysis | 1 (6.7) | 6 (2.6) | 0.360 |
| Wheezing | 1 (6.7) | 4 (1.7) | 0.272 |
| Syncope | 0 | 9 (3.9) | 1.000 |
| Leg pain | 2 (13.3) | 44 (19.0) | 0.744 |
| Mental change | 0 | 12 (5.2) | 1.000 |
| Vital sign | |||
| Systolic blood pressure, mmHg | 112.0 ± 20.1 | 111.1 ± 23.1 | 0.876 |
| Heart rate, bpm | 90.5 ± 16.6 | 88.3 ± 19.3 | 0.668 |
| Respiratory rate, /min | 19.9 ± 3.3 | 20.0 ± 2.9 | 0.922 |
| SaO2, % | 92.9 ± 6.5 | 94.7 ± 5.9 | 0.334 |
| Laboratory test | |||
| Troponin I, ng/mL | 0.02 (0.02–0.13) | 0.03 (0.0–0.16) | 0.600 |
| CK-MB, μg/L | 1.91 (0.74–3.73) | 1.71 (0.92–3.69) | 0.898 |
| D-dimer, μg/mL | 1.52 (0.24–3.36) | 4.64 (2.47–7.58) | 0.002 |
| BNP, pg/mL | 231.0 (47.0–1,421.4) | 158.0 (29.5–605.4) | 0.353 |
| APE-risk stratification, % | |||
| Low risk group | 2 (13.3) | 94 (40.7) | 0.074 |
| Intermediate risk group | 12 (80) | 116 (50.2) | |
| High risk group | 1 (6.7) | 21 (9.1) |
Values are presented as mean ± SD, number (%), or median (interquartile range).
CTEPH, chronic thromboembolic pulmonary hypertension; SaO2, oxygen saturation; CK-MB, creatine kinase MB fraction; BNP, brain natriuretic peptide; APE, acute pulmonary embolism.
The initial echocardiographic and contrast-enhanced CT features of the studied patients are shown in Table 2. The presence of deep vein thrombosis (26.7% vs. 45%, p = 0.19), location (p = 0.309) and the pulmonary arteries affected by PE (p = 0.306) did not show any differences between groups. Most echocardiographic parameters that assess RV morphology and function or dysfunction indicated more significant RV impairment in patients with CTEPH than in patients without: RV dilatation (66.7% vs. 28.1%, p = 0.002), RV dysfunction (46.7% vs. 26.8%, p = 0.098), RV hypertrophy (40% vs. 7.9%, p < 0.001), D-shaped left ventricle (40% vs. 9.5%, p < 0.001), right ventricular systolic pressure (RVSP, 75.5 mmHg vs. 39 mmHg, p < 0.001).
Table 2.
Contrast-enhanced CT and echocardiographic findings
| Characteristic | CTEPH group (n = 15, 6.1%) | Non-CTEPH group (n = 231, 93.9%) | p value |
|---|---|---|---|
| Contrast-enhanced CT | |||
| Deep vein thrombosis | 4 (26.7) | 104 (45.0) | 0.190 |
| Thrombus location | 0.309 | ||
| Bilateral | 6 (40.0) | 120 (51.9) | |
| Unilateral, left | 0 | 20 (8.7) | |
| Unilateral, right | 9 (60.0) | 91 (39.4) | |
| Thrombus site | 0.306 | ||
| Main pulmonary artery | 9 (60.0) | 93 (40.3) | |
| Lobar pulmonary artery | 4 (26.7) | 99 (42.9) | |
| Segmental pulmonary artery | 1 (6.7) | 33 (14.3) | |
| Subsegmental pulmonary artery | 1 (6.7) | 6 (2.6) | |
| Echocardiographic parameter | |||
| RV dilatation, % | 10 (66.7) | 65 (28.1) | 0.002 |
| RV dysfunction, % | 7 (46.7) | 62 (26.8) | 0.098 |
| RV hypertrophy, % | 6 (40.0) | 18 (7.9) | < 0.001 |
| D-shaped LV, % | 6 (40.0) | 22 (9.5) | < 0.001 |
| RV systolic pressure, mmHg | 75.5 (42.0–98.8) | 39.0 (28.0–49.0) | < 0.001 |
| Inferior vena cava size, mm | 23.0 (20.5–23.5) | 21.5 (20.0–24.0) | 0.839 |
| Follow-up echo periods, day | 314.5 (205–367) | 122 (15.5–476.5) | 0.023 |
| Follow-up RV systolic pressure, mmHg | 77 (52.5–89.8) | 35.5 (32–41) | < 0.001 |
Values are presented as number (%) or median (interquartile range).
CT, computed tomography; CTEPH, chronic thromboembolic pulmonary hypertension; RV, right ventricular; LV, left ventricular.
A comparison of therapeutic strategies for APE between groups is shown in Table 3. Thrombolysis and embolectomy were performed in 19 of the 231 patients (8.2%) without CTEPH, whereas no patient with CTEPH received such treatment. More patients in the CTEPH group (n = 14, 93.3%) than in the non-CTEPH group (n = 157, 68%) were given activated partial thromboplastin time-adjusted unfractionated heparin intravenous infusion, and VKA was administered overlapping heparin infusion, with a target INR of 2 to 3. The rate of treatment-related bleeding during follow-up was similar between groups (7.8% vs. 6.7%, p = 1.000). Patients with CTEPH had a longer duration of warfarin treatment (9 months vs. 6 months, p = 0.163) and a longer prothrombin time (PT/INR) (1.98 vs. 1.7, p = 0.111) compared to patients without CTEPH, but the differences were not statistically significant. Additionally, there was no significant difference between the groups in the time in therapeutic range during the first 3 months after initiation of warfarin (38.9% vs. 27%, p = 0.423).
Table 3.
Treatment for acute pulmonary embolism
| Characteristic | CTEPH group (n = 15, 6.1%) | Non-CTEPH group (n = 231, 93.9%) | p value |
|---|---|---|---|
| Treatment modality, % | 0.470 | ||
| No therapy | 1 (6.7) | 32 (13.9) | |
| Thrombolysis | 0 | 18 (7.8) | |
| Embolectomy | 0 | 1 (0.4) | |
| Heparin + warfarin | 14 (93.3) | 157 (68.0) | |
| IVC filter ± warfarin | 0 | 16 (6.9) | |
| New oral anticoagulant | 0 | 7 (3.0) | |
| Bleeding complication, % | 1 (6.7) | 18 (7.8) | 1.000 |
| Follow-up mean PT-INR | 1.98 (1.56–2.56) | 1.7 (1.3–2.07) | 0.111 |
| Warfarin use period, mon | 9.0 (4.8–26.8) | 6.0 (2.0–15.0) | 0.163 |
| Mean TTR, % | 38.9 ± 34.2 | 27.2 ± 26.1 | 0.423 |
Values are presented as number (%), median (interquartile range), or mean ± SD.
CTEPH, chronic thromboembolic pulmonary hypertension; IVC, inferior vena cava; PT, prothrombin time; INR, international normalized ratio; TTR, time in therapeutic range.
All-cause death during follow-up eventually occurred in 23 of 246 patients (9.3%). Pulmonary embolism and thrombolysis-related death were observed in three patients, while the 20 deaths not related to pulmonary embolism were due to malignancy (11 cases), sepsis (seven cases), and multiorgan failure (two cases). Only one patient of developing CTEPH group died not related pulmonary embolism.
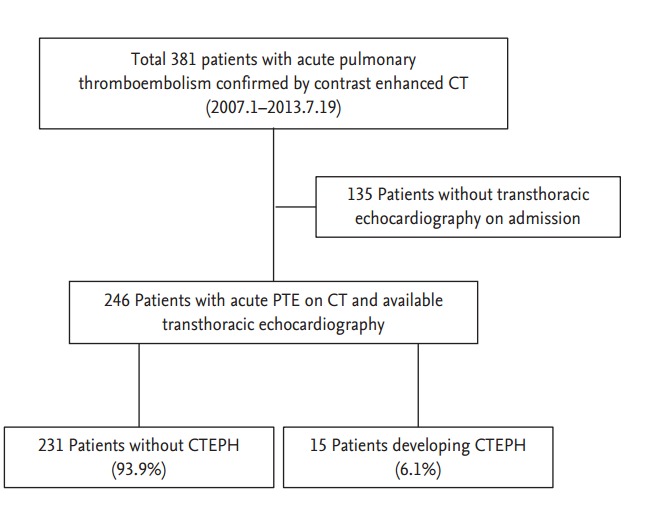
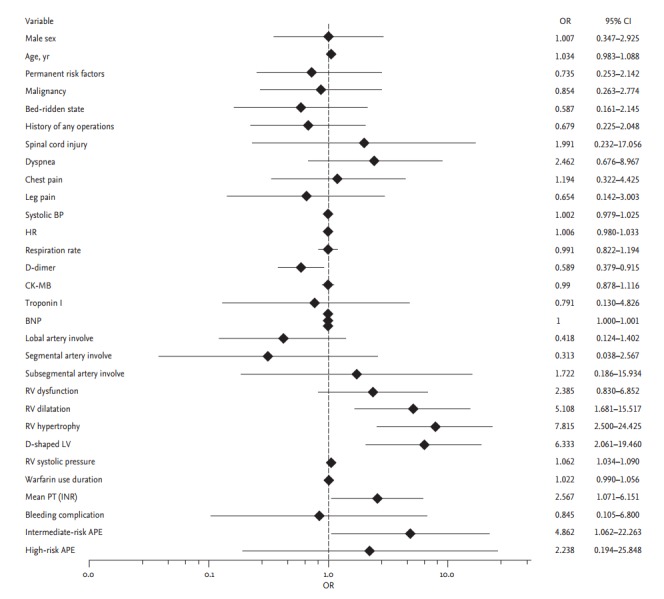
Logistic regression analysis was performed to evaluate the risk factors for developing CTEPH (Figs. 2 and 3). Potential risk factors for CTEPH (e.g., age, sex, initial therapeutic strategy, prior VTE) did not predict the development of CTEPH on univariate analysis. Most echocardiographic RV assessment parameters significantly predicted the development of CTEPH: RV dilatation (OR, 5.10; 95% CI, 1.68 to 15.51), RV hypertrophy (OR, 7.81; 95% CI, 2.50 to 24.42), D-shaped LV (OR, 6.33; 95% CI, 2.06 to 19.4), and elevated RVSP (OR, 1.06; 95% CI, 1.03 to 1.09). An initial low level of D-dimers (OR, 0.58; 95% CI, 0.37 to 0.91) and a prolonged PT (INR) (OR, 2.56; 95% CI, 1.07 to 6.15) were related with developing CTEPH. Intermediate-risk PE was also associated with the development of CTEPH (OR, 4.86; 95% CI, 1.06 to 22.26). On multivariate analysis, elevated RVSP was the only significant predictor for developing CTEPH (OR, 1.05; 95% CI, 1.006 to 1.109).
Figure 2.
Risk factors for developing chronic thromboembolic pulmonary hypertension on univariate analysis. OR, odds ratio; CI, confidence interval; BP, blood pressure; HR, heart rate; CK-MB, creatine kinase MB fraction; BNP, brain natriuretic peptide; RV, right ventricular; LV, left ventricular; PT, prothrombin time; INR, international normalized ratio; APE, acute pulmonary embolism.
Figure 3.
Risk factors for developing chronic thromboembolic pulmonary hypertension on multivariate analysis. OR, odds ratio; CI, confidence interval; BP, blood pressure; HR, heart rate; BNP, brain natriuretic peptide; RV, right ventricular.
According to ROC curve analysis, the best cutoff value of RVSP for CTEPH was 75 mmHg (area under curve [AUC], 0.805; p < 0.001), with a sensitivity and specificity of 57.1% and 60%, respectively (Fig. 4).
Figure 4.
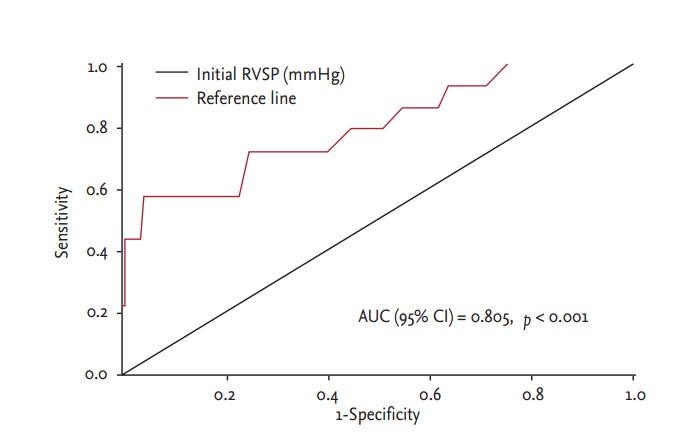
Receiver operating characteristic curve for right ventricular systolic pressure (RVSP) showed that a cutoff value of 74.5 mmHg had 57% sensitivity and 60% specificity for the prediction of developing chronic thromboembolic pulmonary hypertension: area under curve (AUC), 0.805; p < 0.001.
DISCUSSION
In this study, CTEPH appeared to be surprisingly common, with a higher incidence than in any other previous studies: 6.1% of patients who had an episode of APE. In addition, initial echocardiography revealed significant RV impairment in patients with CTEPH. Initial echocardiographic parameters that assessed RV function and morphology were associated with an increased risk of developing CTEPH after the proper management of APE. After adjusting for covariates, RVSP remained a significant risk factor for developing CTEPH, with a best cutoff value of 75 mmHg.
Eventually, 6.1% of patients with APE developed CTEPH. These results challenge the common belief that CTEPH is rare after an episode of APE and occurs long after the acute episode [12]. Previous studies that reported a lower incidence of CTEPH, ranging from 0.8% to 3.8%, included selected patient cohorts—for example, excluding asymptomatic patients and those with a prior episode of pulmonary embolism [13]. In our study, all patients diagnosed with APE were included, regardless of prior VTE or symptom. All patients with CTEPH were symptomatic and six of the 15 patients (40%) had prior VTE. This could be one of the reasons for the higher incidence of CTEPH in our study. The incidence of CTEPH remained higher even after prior VTE was excluded: nine of 178 patients (5%). In some cases, follow-up echocardiography was performed 6 months or more after the initial episode of APE, even if the patient had no symptoms. Taking these considerations into account, we believe that our results reasonably represent the incidence of CTEPH. Patients with APE might need a more aggressive follow-up because of this unexpected higher incidence of CTEPH.
The risk factors for subsequently developing CTEPH have been identified by several studies. The risk of developing CTEPH following an APE was higher in patients who had persistent PAH during follow-up [14]. These results were consistent with our study, where an initial high pulmonary artery pressure was associated with developing CTEPH. Other risk factors for developing CTEPH included traditional risk factors, such as a large perfusion defect on perfusion scan, and idiopathic presentation [3]. However, it seemed unlikely that these traditional risk factors would be related with the development of CTEPH in this study. Hemostatic risk factors, such as an elevated level of factor VIII and abnormalities in fibrinogen structure and function, are also associated with developing CTEPH [15,16]. Prior splenectomy, presence of a ventriculoatrial shunt or infected pacemaker, osteomyelitis, inflammatory bowel disease, and hypothyroidism were found to be risk factors for developing CTEPH in a small-sized study [17]. However, these medical conditions related to developing CTEPH could not be discussed properly, because of the shortage of pertinent data. In addition, these studies excluded patients with APE.
Echocardiography is a noninvasive and cost-effective modality that can be used to determine the severity of APE at presentation, and to search systematically for CTEPH in patients diagnosed with APE [18]. In most patients with CTEPH, the disease is observed within 24 months after APE [3], whereas current European guidelines recommend shorter-term follow-up echocardiography only in patients with high-risk APE [4]. A symptom-based approach after APE might not be the most appropriate management, because the diagnosis of CTEPH could be missed in asymptomatic patients, with potentially serious consequences. Therefore, an extension of the follow-up period for echocardiography or exercise echocardiography in patients who have a high risk of developing CTEPH could be helpful. Apart from the significance of echocardiography in the diagnosis of CTEPH, the findings of this study suggest that echocardiographic parameters that assess RV function and morphology could be used as clinical markers for developing CTEPH. Various echocardiographic parameters were found to be significant risk factors for developing CTEPH on univariate analysis. Even after multivariate analysis, RVSP continued to remain a significant risk factor. ROC analysis of RVSP for developing CTEPH showed a high AUC, and patients with an initial RVSP above 74.5 mmHg had a higher chance of developing CTEPH. Another study reported that elevated pulmonary artery pressure in an APE is correlated with the development of persistent PH in the late period [14]. Persistent PH is related with RV dysfunction, and patients with CTEPH and RV dysfunction have a poorer clinical outcome than any other subgroup [19]. Therefore, we suggest that RVSP might be viewed as an important and valuable risk factor among the various echocardiographic parameters at presentation.
High-risk APE may lead patients and physicians to be more cautious in the management of the condition. However, patients with intermediate-risk APE and initial RVSP above 74.5 mmHg should be managed with proper anticoagulation therapy and closely monitored, even after discharge from hospital. Regular follow-up echocardiography and a symptom-related diagnostic modality might be helpful in arriving at the diagnosis of CTEPH earlier in these patients.
The present findings are derived from retrospective observational analysis, which is subject to well-known limitations. The first is the potential for confounding by measured or unmeasured variables, which cannot be ruled out even after multivariate adjustment. Second, the diagnosis of CTEPH was based only on echocardiography and contrast-enhanced CT. In spite of advances in CT and magnetic resonance imaging, a radionuclide ventilation/perfusion scan to screen for CTEPH remains the preferred test and is recommended as the initial step in the diagnosis of CTEPH [4]. Moreover, definite PH was confirmed using pulmonary artery catheterization rather than echocardiography only. However, echocardiography, which could be used to identify risk factors for developing CTEPH, might be useful to arrive at a diagnosis faster and less invasively; thereby, allowing the prediction of disease progression with a view to improving clinical outcomes. Finally, this was a small, single-center study. In particular, the patients with high-risk APE were few in number, which limited the study’s statistical power for predicting the development of CTEPH and the clinical outcomes related to therapeutic strategy.
In conclusion, a high incidence of CTEPH after APE was identified in our single-center, retrospective observational study. Initial echocardiography was a useful tool for evaluating RV impairment and identifying risk factors for the development of CTEPH. We suggest that regular and long-term echocardiographic follow-up might be helpful for the faster diagnosis and management of CTEPH in patients with intermediate-risk APE or elevated RVSP at presentation.
KEY MESSAGE
1. The 6.1% of patients who had an episode of acute pulmonary embolism developed chronic thromboembolic pulmonary hypertension (CTEPH) eventually.
2. Initial echocardiographic parameters that assess right ventricular function and morphology could be used as clinical markers for developing CTEPH.
3. Patients with an initial right ventricular systolic pressure above 74.5 mmHg had a higher chance of developing CTEPH.
Acknowledgments
This work was supported by a 2-year Research Grant of Pusan National University.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Lewczuk J, Piszko P, Jagas J, et al. Prognostic factors in medically treated patients with chronic pulmonary embolism. Chest. 2001;119:818–823. doi: 10.1378/chest.119.3.818. [DOI] [PubMed] [Google Scholar]
- 2.Hoeper MM, Mayer E, Simonneau G, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Circulation. 2006;113:2011–2020. doi: 10.1161/CIRCULATIONAHA.105.602565. [DOI] [PubMed] [Google Scholar]
- 3.Pengo V, Lensing AW, Prins MH, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350:2257–2264. doi: 10.1056/NEJMoa032274. [DOI] [PubMed] [Google Scholar]
- 4.Galie N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT) Eur Heart J. 2009;30:2493–2537. doi: 10.1093/eurheartj/ehp297. [DOI] [PubMed] [Google Scholar]
- 5.Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 6.McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78:469–473. doi: 10.1016/s0002-9149(96)00339-6. [DOI] [PubMed] [Google Scholar]
- 7.Kukulski T, Voigt JU, Wilkenshoff UM, et al. A comparison of regional myocardial velocity information derived by pulsed and color Doppler techniques: an in vitro and in vivo study. Echocardiography. 2000;17:639–651. doi: 10.1046/j.1540-8175.2000.00639.x. [DOI] [PubMed] [Google Scholar]
- 8.Yasui T, Tanabe N, Terada J, et al. Multidetector-row computed tomography management of acute pulmonary embolism. Circ J. 2007;71:1948–1954. doi: 10.1253/circj.71.1948. [DOI] [PubMed] [Google Scholar]
- 9.Auger WR, Fedullo PF, Moser KM, Buchbinder M, Peterson KL. Chronic major-vessel thromboembolic pulmonary artery obstruction: appearance at angiography. Radiology. 1992;182:393–398. doi: 10.1148/radiology.182.2.1732955. [DOI] [PubMed] [Google Scholar]
- 10.Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) Eur Heart J. 2008;29:2276–2315. doi: 10.1093/eurheartj/ehn310. [DOI] [PubMed] [Google Scholar]
- 11.Shigeta A, Tanabe N, Shimizu H, et al. Gender differences in chronic thromboembolic pulmonary hypertension in Japan. Circ J. 2008;72:2069–2074. doi: 10.1253/circj.cj-08-0377. [DOI] [PubMed] [Google Scholar]
- 12.Egermayer P, Peacock AJ. Is pulmonary embolism a common cause of chronic pulmonary hypertension? Limitations of the embolic hypothesis. Eur Respir J. 2000;15:440–448. doi: 10.1034/j.1399-3003.2000.15.03.x. [DOI] [PubMed] [Google Scholar]
- 13.Becattini C, Agnelli G, Pesavento R, et al. Incidence of chronic thromboembolic pulmonary hypertension after a first episode of pulmonary embolism. Chest. 2006;130:172–175. doi: 10.1378/chest.130.1.172. [DOI] [PubMed] [Google Scholar]
- 14.Ribeiro A, Lindmarker P, Johnsson H, Juhlin-Dannfelt A, Jorfeldt L. Pulmonary embolism: one-year follow-up with echocardiography doppler and five-year survival analysis. Circulation. 1999;99:1325–1330. doi: 10.1161/01.cir.99.10.1325. [DOI] [PubMed] [Google Scholar]
- 15.Lang I, Kerr K. Risk factors for chronic thromboembolic pulmonary hypertension. Proc Am Thorac Soc. 2006;3:568–570. doi: 10.1513/pats.200605-108LR. [DOI] [PubMed] [Google Scholar]
- 16.Suntharalingam J, Goldsmith K, van Marion V, et al. Fibrinogen Aalpha Thr312Ala polymorphism is associated with chronic thromboembolic pulmonary hypertension. Eur Respir J. 2008;31:736–741. doi: 10.1183/09031936.00055107. [DOI] [PubMed] [Google Scholar]
- 17.Lang IM, Pesavento R, Bonderman D, Yuan JX. Risk factors and basic mechanisms of chronic thromboembolic pulmonary hypertension: a current understanding. Eur Respir J. 2013;41:462–468. doi: 10.1183/09031936.00049312. [DOI] [PubMed] [Google Scholar]
- 18.Galie N, Rubin Lj, Hoeper M, et al. Treatment of patients with mildly symptomatic pulmonary arterial hypertension with bosentan (EARLY study): a double-blind, randomised controlled trial. Lancet. 2008;371:2093–2100. doi: 10.1016/S0140-6736(08)60919-8. [DOI] [PubMed] [Google Scholar]
- 19.Riedel M, Stanek V, Widimsky J, Prerovsky I. Longterm follow-up of patients with pulmonary thromboembolism: late prognosis and evolution of hemodynamic and respiratory data. Chest. 1982;81:151–158. doi: 10.1378/chest.81.2.151. [DOI] [PubMed] [Google Scholar]