In recent years, emphasis on improving the quality of care has increased significantly and continues to gain momentum. This paper examines the process, trends, opportunities, and challenges of quality improvement initiatives to improve outcomes and care quality for patients during and following cancer treatment. Selected improvement program on management of patients presenting with postchemotherapy febrile neutropenia relevant to quality improvement sequence is reviewed.
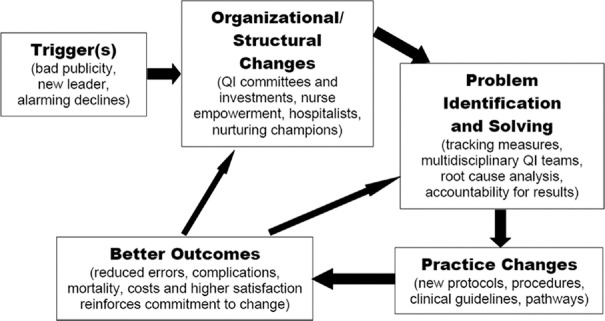
Despite the major differences among the quality improvement initiatives by different hospitals in terms of change nature, size and location of the institution, populations served, and resource status, there is a common temporal and ultimately cyclical sequence of factors resulting in change [Figure 1].[1] This sequence was adopted to facilitate elaborating the process how oncology care and service in Hong Kong to be improved through quality improvement program and what the challenge and opportunity to be experienced.
Figure 1.
Quality improvement sequence
“Trigger” Situations or Events
Chemotherapy services are facing a challenge as therapies become more complex and a growing number of patients become eligible for treatment. There is an exponential increase in the use of chemotherapy for a wide range of cancer. The day chemotherapy attendance in Hospital Authority (HA), Hong Kong has 42% increases from 2011 to 2015.[2] A high proportion of chemotherapy treatment is delivered in the ambulatory setting and even at patients’ home. Chemotherapy has significant and predictable toxicities, the most serious of which are likely to develop while the patient is at home between treatment cycles. Chemotherapy-induced neutropenic sepsis is a notable example of a side effect that is predictable, preventable, and manageable, but which prove fatal if treatment is delayed or is inappropriate. Neutropenic sepsis is a time-dependent medical emergency in which early, goal-directed resuscitation and the urgent administration of broad-spectrum antibiotics have proven benefits on outcome.[3,4]
In 2011, one leukemic male taxi driver had a fever after chemotherapy and subsequently attended in two hospitals, but did not receive antibiotic treatment immediately and died 4 h later due to disseminated intravascular coagulation.
The patient death was avoidable. This is serious shortcomings in the management of neutropenic sepsis in Hong Kong. Coroner's court recommendation came out till 2015.
Organizational and Structural Changes
HA is the predominant provider of secondary and tertiary health-care services in Hong Kong. As cancer treatment cost is very expensive, 90% of people have their cancers treated in HA. In recent years, HA set up and strengthen the role of the specialty-based committee and workgroup such as Coordinating Committee (COC) and Specialty Advisory Group (SAG) which serve as an official platform for clinical leaders from different specialties across different clusters/hospitals to deliberate issues including workforce, training, services, quality, technology, and therapeutics for its respective specialty to achieve more standardized service quality and treatment and to ensure safety. Clinical oncology COC is a committee more medical driven with members mainly oncologists and representatives from partner disciplines including nursing, physicist, and radiation therapist. Oncology SAG is an advisory group seated by nursing clinical leaders of the oncology specialty.
A new post of nurse consultant was first created in HA in 2010 to provide an extension of the clinical nursing career path and foster clinical advancement to ensure clinical service and care quality. Three oncology nurse consultants were already at post in HA.
With support from the oncology SAG, nurses from the six oncology centers who completed the Corporate Overseas Scholarship Training Programs formed a working group to champion the quality improvement efforts at management of neutropenic sepsis that is highlighted as a clinical priority.
Problem Identification and Solving
A cross-cluster survey was firstly conducted in 2012 in six oncology centers of HA to retrospectively analyze the management of patients presenting with FN after chemotherapy in their emergency access by (1) identifying structural problems in the system; (2) determining the time to administration of antibiotics; and (3) assessing the related impact on patient outcomes, so as to facilitate identifying problem and developing solution.
The survey has reviewed the clinical management of 207 patients who were identified being admitted to the oncology wards due to chemotherapy-induced FN between November 2012 and September 2013. The result revealed that the mean time from presentation to administration of first antibiotic dose was 266 min and the longest one was up to 1500 min, which are longer than the international benchmark like the National Chemotherapy Advisory Group in the United Kingdom in 2009 recommending the 1 h Door-to-antibiotic time (DTA) in cases of suspected neutropenic sepsis.[5]
The pathway that individual patients received their first dose of antibiotics after admitted to ward was lengthy especially out of office hours. The prolonged time is multifactorial including patient transportation, administrative procedure on admission, and antibiotic delivery.
The delay in an antibiotic administration noted in survey is mainly associated with lack of a fast-track mechanism and policy to be in place for emergency management of postchemotherapy febrile patients between oncology centers and emergency departments, and inadequate staff awareness on the importance of early detection and early treatment of suspected neutropenic sepsis.
The finding also exhibited the delayed antibiotic administration in cancer patients with an episode of FN did increase the length of their hospitalization and have more adverse effects occurred; moreover, the patient had lack of knowledge in responding and managing this complication and consequently sought treatment later increasing risk of overwhelming sepsis and death.
We developed an action plan to tackle the identified problems and to streamline pathway of care for this vulnerable group of patients through various strategies including cross departments collaboration, enhancing patient education and awareness, staff training, and development of a standardized protocol to direct the flow of patients with an episode of FN through the accident and emergency department (AED).
Protocol and Practice Changes
The survey findings were presented in different HA forum and convention as well as in the clinical oncology COC meeting to get others buy in. Not only nursing leadership, but also across the board from the COC down. We engaged stakeholders and every related party through consultation to them including clinical staff in oncology and AED, nurses, physicians, pharmacists and blood laboratories, as well as nonclinical staff, such as transportation. Staff briefing and training were conducted to increase their awareness, knowledge, and engagement. That is important to success.
The oncology centers have implemented improvement strategies in 2015 by phases conforming to their local situations. In Phase 1, specific patient education and alert card were developed for patients who are at risk of FN. A driven triage workflow being created in collaboration with AED was in place to facilitate patients’ access to appropriate treatment. Evidence-based clinical guideline, protocol, and care plan were also established to guide the frontline nurses and doctors in caring the admitted FN patient.
A new clinical pathway was introduced to ensure a clear and timely pathway of care for patients getting help when they suspected neutropenic sepsis during or out of office hour. Identified “high-risk” patients were referred to chemotherapy nurse clinic for proactive chemotherapy education that is structured consultation session including assessment, face to face education with written information about the treatment patient will be receiving, the likely side effects and whom they should contact if problems arise (including out of hours), as well as issued with alert card upon assessment of patient's risk level. When the patient presented with the alert card once they accessed the emergency department or oncology clinic for febrile symptoms after chemotherapy, they would be identified promptly, thus triaged into a fast-track pathway for timely investigation workup and access of appropriate antibiotic treatment.
It is planned to move to Phase 2 in the next to consider introducing the telephone follow-up support and electronic patient alert when the implementation of Phase 1 becomes mature, as well as infrastructure and workforce can support the further proposed change.
Better Outcomes
The new protocols and practices would lead to improved outcomes in the process and health-related measures. The second cross-cluster survey was then initiated in 2016 to review the impact after implementation of a clinical pathway for postchemotherapy FN in malignancy patients. Fifty-three patients identified being admitted to the oncology wards due to FN and receiving chemotherapy within 1 month of the admission between May and July 2016 were recruited to the pathway group. Similar cases recruited in the first survey before implementation of the pathway served as historical referents. Both groups were compared in regard to their baseline characteristics and outcome data.
Implementation of the pathway for the oncology centers and their affiliated hospitals significantly reduces the mean DTA from 266 to 126 min (P < 0.001). Furthermore, patients who could achieve the target DTA of <1 h increase from 11% to 57% (P < 0.001). The improvement program result was satisfactory when compared with similar studies conducted in Europe and North America where reported median DTA ranged from 154 min to 3.9 h.[6,7,8] Audits from the UK report that only 18%–26% of patients receive initial antibiotic within the target DTA of 1 h.[9]
Better outcomes would lead back to a greater intensity of quality improvement work by becoming in effect new “triggers.” That is, success reinforces the logic and commitment to quality improvement efforts.
Challenges and Key for Health-care Process Improvement
During the improvement work, a lot of difficulties were encountered. Although quality improvement is not a new concept to us, there is proliferation of these activities and escalating pressure on staff to participate, many of which are viewed as duplicative, unneeded or insignificant, which lead to staff frustration. Moreover, shortage of nurses and nurses assuming many of added responsibilities are also the challenges that discourage some oncology centers participation in championing this quality improvement initiative at the beginning. It is not that we are going to stop doing quality, but how we address those challenges whereas we are really affecting the outcome. I took a quote from Deming the leading management thinker in the field of quality that “…quality improvement is science of process management…” I added something to this quote to make it more pertinent to our healthcare environment that “quality improvement is a science but also an art of process management.” We have adopted some means that were centered on the notions to make the biggest difference in our quality improvement process.
Identify what really make sense in processes of care
Healthcare comprises simply thousands of interlinked processes that result in a very complex system. Do not dare to fix it all at a time. We better focus on the processes of care one at a time, or we can fundamentally change the game and deal with the challenges facing healthcare. Pareto's principle (80-20 rule) tells us there are probably 20% of those processes that will get us 80% of the impact. Hence, the challenge is to identify that 20% and begin the important work of addressing those challenges. That means just identifying what makes sense for our patient population and what initiative addresses an identified need.
If cannot measure it, cannot improve it
Meaningful quality improvement must be data-driven. Hence, data are critical if we are going to have a meaningful impact on healthcare. Benchmarking provides important information to communicate with staff about the hospital's performance and is particularly useful in revealing significant differences both good and bad.
Manage the processes of care, not manage clinicians
Managing care means managing the processes of care. It does not mean managing physicians and nurses. One of the big mistakes made with the “managed care” movement was naively thinking that managing care meant telling clinicians what to do. Clinicians are the frontline workers who understand and own the processes of care. The reality is that we need to engage clinicians in the process because they understand the care delivery process and they are best equipped to figure out how to improve the process of care over time.
Right data in right format at right time in right hands
Clinicians hence definitely need right data to help them manage care. The data have to be delivered into the right hands the clinicians who operate and improve any given process of care. Moreover, the right data are delivered in the right format at the right time and in the right place. The key to effective feedback is not only just the amount of information provided but also how meaningful that information is for staff.
Engage all nurses, not just nursing leadership
Quality improvement initiatives are much more successful in cases where they have developed from the ground up and bedside staff nurses and others have “grabbed hold and made them their own.” Engagement can increase their buy in and support, thus diminish the impression that the related work is more of a burden than an opportunity.
Conclusion
The focus of this paper is demonstrating how the oncology nurses in Hong Kong have committed to lead and implement the quality improvement initiative on FN management. The use of selected tracking measures and root cause analysis to generate data-driven insights about patient-centered outcomes important to the delivery of cancer care is illustrated. The strategies through leadership and collaboration as well as tactics of how to make the biggest difference in healthcare process improvement are highlighted. It is essential that nurses do not work in isolation, but are key team players. Isolated practice would be a great disservice to patients and the nursing profession.
Our tremendous work at quality improvement brought about a step change in the quality and safety of chemotherapy services in Hong Kong. Despite a long way to move forward, our work on the quality improvement will continue to go on. It is clear that there may not achieve initiatives on either service or profession development without a great deal of persuasion, persistence, and teamwork.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was written on the basis of a presentation given at the International Conference on Cancer Nursing 2016 held in Hong Kong, China by the International Society of Nurses in Cancer Care.
References
- 1.Silow-Carroll S, Alteras T, Meyer JA. Hospital Quality Improvement: Strategies and Lessons from U.S. Hospitals. Commonwealth Fund; 2016. Nov, Available from: http://www.cmwf.org . [Google Scholar]
- 2.Coordinating Committee of Clinical Oncology Service. Chemotherapy waiting time survey. Hong Kong: Management Meeting (Clinical Oncology and Cancer Services), Hospital Authority; 2016. Jul, [Google Scholar]
- 3.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 4.Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–53. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 5.National Chemotherapy Advisory Group (NCAG). Chemotherapy Services in England: Ensuring Quality and Safety. London: National Chemotherapy Advisory Group; 2009. [Google Scholar]
- 6.Sammut SJ, Mazhar D. Management of febrile neutropenia in an acute oncology service. QJM. 2012;105:327–36. doi: 10.1093/qjmed/hcr217. [DOI] [PubMed] [Google Scholar]
- 7.Lim C, Bawden J, Wing A, Villa-Roel C, Meurer DP, Bullard MJ, et al. Febrile neutropenia in EDs: The role of an electronic clinical practice guideline. Am J Emerg Med. 2012;30:5–11. doi: 10.1016/j.ajem.2010.08.011. 11.e1-5. [DOI] [PubMed] [Google Scholar]
- 8.Nirenberg A, Mulhearn L, Lin S, Larson E. Emergency department waiting times for patients with cancer with febrile neutropenia: A pilot study. Oncol Nurs Forum. 2004;31:711–5. doi: 10.1188/04.ONF.711-715. [DOI] [PubMed] [Google Scholar]
- 9.Clarke RT, Warnick J, Stretton K, Littlewood TJ. Improving the immediate management of neutropenic sepsis in the UK: Lessons from a national audit. Br J Haematol. 2011;153:773–9. doi: 10.1111/j.1365-2141.2011.08693.x. [DOI] [PubMed] [Google Scholar]