Abstract
Objective:
Urological cancer and its surgeries have great impact on male sexuality which could have physical or emotional consequences. In India, speaking openly about the sexual matter is a taboo and an aspect considered forbidden. Therefore, the aim of the present study is to develop an information booklet about male sexual dysfunction and assess its impact on knowledge of patients with urological cancers.
Methods:
Information booklet was developed after literature review, and its content validity was established. Reliability of the questionnaire was 0.95. A randomized control trail using pre- and post-test design was used for 30 male urological cancer patients and was assigned to experimental group (15) who received information booklet and control group (15) who received standard treatment. Subjects in the experimental group were provided with opinionnaire during posttest. Data were analyzed using descriptive and inferential statistics.
Results:
In experimental group, 40% of the subjects were ≤ 40 years, whereas 27% in the control group (P = 0.699). The pre- and post-mean difference score was significantly higher in experimental group (mean difference - 5) than control group (mean difference - 0.4). All subjects (100%) opined that the information booklet was useful, adequate, self-explanatory, sequential, and clear.
Conclusions:
Information in the booklet will help subjects to understand the common sexual problems after urological surgeries and help them to cope with the problems, thereby improving their quality of life.
Keywords: Common male sexual dysfunction, sexual measures, urological cancers, urological surgeries

Introduction
The diagnosis of cancer and its treatment can have devastating effect on psychological and emotional well-being of a cancer survivor.[1] Urological cancer and its surgeries have great impact on male sexuality as it interferes with mechanisms of erections in different ways, mainly by damaging nerves, blood vessels, or by causing generalized weakness. The commonly experienced side effects are erectile dysfunction (ED), premature ejaculation, delayed ejaculation, or emotional deviation such as lack of interest in sexual activity which can affect interaction with his partner/spouse and also cause low self-esteem. It has been recently estimated that more than 152 million men worldwide experienced sexual dysfunction and that this number will increase to approximately 322 million by the year 2025.[2]
Studies have shown that ED is prevalent in patient with renal cancer, testicular cancer, and penile cancer.[3,4,5] Organ associated problems, urinary incontinence during sexual activity, penile sensory changes, penile shrinkage, and penile deformity are common side effects experienced by patient who had undergone radical prostatectomy and testicular cancer.[4,6]
In India, speaking openly about sexual matter is a taboo and an aspect considered forbidden in many cultures of India. Patients are selective in talking about sexual problems with health care professionals. Many a times, patients do not clarify their doubts about sexual life posttreatment because they are concerned about how the physician would perceive them and may disregard their sexuality since cancer is a more important health problem or they may accept changes in sexuality as part of the cancer experience and not know that they can be addressed. It is seen that health-care professionals also do not give much importance to sexual component of the patient in posttreatment phase. More specifically measures included mechanical (penile rings, vaccum pump), medical (use of drugs for dysorgasmia, penile enlargement), surgical (penile implants), behavioral (use of Kegel and Squeeze techniques) and general measures (healthy diet, warm bath, aerobics), etc., although available are not discussed with patients.
Therefore, the aim of the study was to develop an information booklet about male sexual dysfunction and its measures to overcome these problems, for patients who have undergone surgery for urological cancer and also to assess the change in knowledge scores of patients after implementation of the information booklet.
Orem's self-care deficit theory
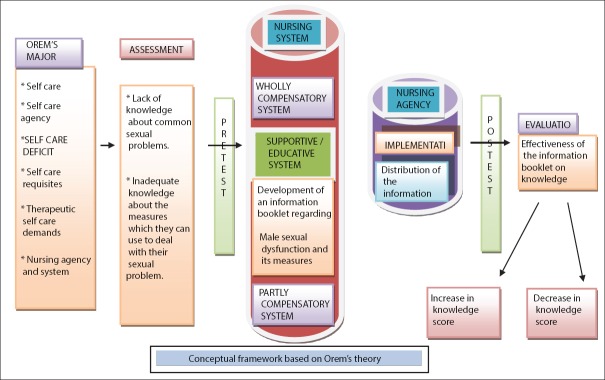
Orem's theory focuses on human beings as self-reliant and being responsible for their own care,[7] successfully meeting universal and development self-care requisites is an important component of primary care prevention. Nurses do play an important role in action/interaction in all patients.[8] Supportive–educative nursing system is one of the classifications of Orem's nursing system where the emphasis is on nurse's role in promoting the patient as a self-care agent[9] [Figure 1].
Figure 1.
Conceptual framework based on Orem's theory
The booklet would help patients to have awareness about the topic and will help them to adopt measures to have a positive sexual experience. Development of booklet was based on analyze, design, develop, implement, and evaluate model.
Methods
The study was conducted on patients visiting urology Outpatient Department (OPD), Tata Memorial Centre for cancers of prostrate, testicular, urinary bladder, kidney, and penis. Literature review was conducted using various search engines such as PubMed, Science Direct, CINHALs, and Cochrane. The investigator reviewed various studies and articles on the topic and it helped to gain clarity about the topic under study. The following tools were developed.
Information booklet
The information booklet covered general concept of sexual dysfunction, common male sexual dysfunction such as low libido, ED, premature ejaculation, dysorgasmia, delayed ejaculation, Peyronie's, and penile shrinkage, measures to improve sexual dysfunction, for example, behavioral measures, sexual measures, psychological measures, general measures, mechanical measures, medical, and surgical measures. Factors considered while preparing the information booklet were simplicity of language and the content to cover all the items in the questionnaire for testing the knowledge. Size of the information booklet was 18 cm × 24 cm with a colorful background and a cover page in white. It is a paper-bound booklet with 8 pages in total.
A semi-structured questionnaire
A questionnaire was developed to assess patient's knowledge on sexual dysfunction and measures to overcome them. The tool had two sections with a total of 28 items. The questionnaire was administered before and after the information booklet was handed over to the patients in the experimental arm. No information regarding sexual dysfunction was given to the control arm, which is a routine practice in our institute.
Section 1 includes eight items related to the demographic variables of the respondents about age, marital status, diagnosis, surgery, prior chemotherapy or radiation therapy and prior any sexual dysfunction.
Section 2 includes 20 multiple choice questions to assess the knowledge before and after administering information booklet on “Male sexual dysfunction and its measures.” Out of 20 questions, 6 questions were based on “General concept of sexual dysfunction,” 4 questions were based on “Common male sexual dysfunction” and 10 questions were based on “Measures of sexual dysfunction.”
All the 20 objective type items had one right answer and three distracters. Only one option had to be encircled for each item. It was mandatory to attempt all questions. Each correct answer was given a score of one and wrong answers a score of 0. The maximum score that could be obtained was “20” and the minimum score was “0.” The score was arbitrarily graded (<5 score – poor, 5–10 – good, 11–16 – very good, >16 score – excellent).
Semi-structured opinionnaire
Opinionnaire was developed to obtain feedback with respect to the quality and rating of the content and their views about the booklet. It consisted of 5 dichotomous (yes or no) questions with scope for respondents comment, 1 rating question (rate this information booklet as (1) excellent, (2) very good, (3) good, (4) average, (5) not up to the mark) and 1 open-ended question requesting them to share their views related to effectiveness of information booklet.
The content validity was established by giving to 11 experts from the field of nursing, clinicians, sex experts, and statisticians. Reliability of the questionnaire was established by test-retest method using Pearson's correlation formula, and it was found to be 0.95. The study was initiated after receiving ethical clearance from the Institutional Ethics Committee of Tata Memorial Hospital (TMH).
Pilot study
Pilot study was undertaken on five subjects using nonprobability convenience sampling at urology OPD to gain an understanding on the feasibility of the study. They were explained about the study and consent was solicited. They responded to the semi-structured questionnaire, and the booklet was distributed in a language they understood. A posttest was administered after a week.
A randomized control study using pre- and post-test design was carried out on 30 adult male patients with urological cancers who had undergone surgery, who were in the posttreatment phase and visiting urology Out Patient Department (OPD) for follow-up in TMH. Eligibility criteria included all adult male patients who had undergone surgery and are on follow-up (for at least a month and maximum up to 1 year), residing in Mumbai, signed the consent form and are able to read, write, and speak Hindi/Marathi/English. A nonprobability convenience sampling using self-reporting technique was used. Informed consent was handed over to subjects in a language they understood. The subjects were assigned to experimental group (15) and control group (15) based on randomization with the help of a statistician. The experimental group received information booklet and standard treatment while control group received only standard treatment.
Data were collected from December 22, 2014, to January 31, 2015. Instruction on how to fill the questionnaire and their doubts regarding the procedure were clarified. Subjects were provided privacy to fill the questionnaire. All subjects were called back for posttest in the same OPD setting. Along with posttest questionnaire subjects in the experimental group were also provided with opinionnaire.
Statistical analysis
All categorical data were summarized using frequency and percentage. All pre- and post-test scores were compared using McNemar's test for each group.
The total scores for pre- and post-test were calculated for both groups separately. The difference between the total pre- and post-test scores was also calculated for each group separately. The normality assumptions were checked for the difference in scores for experimental and control group using Shapiro–Wilks test. An unpaired t test or Mann–Whitney U-test will be used depending on normality of the data. All P values are two-sided and P < 0.05 was considered statistically significant. Data were analyzed using SPSS. (BM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.
Results
Demographic data
Experiment group
Maximum subjects (40%) were in the age group of 18–40 years, whereas 26% were in the age group of 61 years and above (P = 0.699). Around 67% of the subjects were married (33%) of the subjects were diagnosed with bladder cancer and testicular cancer and majority (27%) of subjects had undergone orchidectomy surgery.
Control group
Maximum 46% were in the age group of 61 years and above and 27% each in the age group of 18–40 years and 41–60 years, respectively. Around 87% of the subjects were married (27%) were of prostate cancer and testicular cancer and majority (33%) of subjects had undergone orchidectomy surgery [Table 1].
Table 1.
Demographic variables
| Characteristics | Category | Frequency (%) | ||
|---|---|---|---|---|
| E (n=15) | C (n=15) | CB (n=30) | ||
| Age (years) | 18-40 | 6 (40) | 4 (27) | 10 (33) |
| ≥41 | 9 (60) | 11 (73) | 20 (67) | |
| Marital status | Married | 10 (67) | 13 (87) | 23 (77) |
| Unmarried | 4 (27) | 2 (13) | 6 (20) | |
| Widow/divorce | 1 (7) | 0 | 1 (3) | |
| Diagnosis | Cancer of bladder | 5 (34) | 3 (20) | 8 (27) |
| Cancer of kidney | 1 (7) | 1 (7) | 2 (7) | |
| Cancer of prostate | 2 (13) | 4 (27) | 6 (20) | |
| Cancer of testis | 5 (34) | 4 (27) | 9 (30) | |
| Prior sexual dysfunction | Erectile dysfunction | 5 (33) | 5 (34) | 10 (33) |
| Low libido | 0 | 2 (13) | 2 (7) | |
| None | 10 (67) | 8 (53) | 18 (60) | |
E: Experimental group, C: Control group, CB: Combined
In both groups, over 50% of the subjects were in 9–12 months follow-up period, 73.3% of the subjects had not received neoadjuvant treatment and 30% of subjects in the age group of 41 and above had impotency (ED) before surgery (data not shown).
Area wise pretest and posttest knowledge score of experimental and control group
Experimental group
A significant improvement was observed between pre- and post-test knowledge score with regard to “Normal sexual cycle” (pre - 33%, post - 100%; P = 0.002) and “Symptoms of sexual dysfunction” (pre - 33%, post - 93%; P = 0.004). For question on “Measures for sexual dysfunction” there was marked improvement from 0% to 67% (P = 0.006). The finding of the result showed that there was an improvement in pretest knowledge scores from 27% to posttest knowledge score 67% and 87% (P = 0.03 and P = 0.004), respectively, for question on “ED” and “Premature ejaculation.”
None of the subjects in the pretest had knowledge about start-stop technique as a behavioral measure to premature ejaculation which improved to 13% in posttest. Knowledge about milking technique improved from 7% in pretest to 60% (P = 0.008) in posttest. Majority of the subjects had increased knowledge scores regarding nonpenetrative sexual activity from 20% in pretest to 67% in posttest (P = 0.03). Whereas regarding dysorgasmia the knowledge score had been same in both pretest and posttest. Regarding postsurgical measures, there had been decrease in knowledge scores from 100% in pretest to 60% in posttest which may be due to confusion with the remaining options [Table 2].
Table 2.
Area wise distribution of pre- and post-test knowledge scores
| Items | Experiment (n=15) | P | Control (n=15) | P | |||
|---|---|---|---|---|---|---|---|
| Pretest scores (%) | Posttest scores (%) | Pretest scores (%) | Posttest scores (%) | ||||
| General concepts of sexual dysfunction | Anatomy and physiology | 12 (80) | 15 (100) | 0.250 | 15 (100) | 15 (100) | |
| Normal sexual cycle | 5 (33) | 15 (100) | 0.002 | 13 (87) | 15 (100) | 0.500 | |
| Treatments in urological cancers | 15 (100) | 15 (100) | 15 (100) | 15 (100) | |||
| Symptoms of sexual dysfunction | 5 (33) | 14 (93) | 0.004 | 10 (67) | 11 (73) | 1.000 | |
| Meaning of sexual dysfunction | 0 | 10 (67) | 1.000 | 1 (7) | 7 (47) | 0.727 | |
| Measures of sexual dysfunction | 1 (7) | 11 (74) | 0.006 | 10 (67) | 8 (53) | 0.688 | |
| Common male sexual dysfunction | Inability to achieve or maintain sufficient stiffness of the penis is called as erectile dysfunction | 4 (27) | 10 (67) | 0.031 | 3 (20) | 2 (13) | 1.000 |
| Premature ejaculation means uncontrollable release of sperm | 4 (27) | 13 (87) | 0.004 | 5 (33) | 4 (27) | 1.000 | |
| Low libido means lack of desire for sexual activity | 12 (80) | 11 (7) | 1.000 | 4 (27) | 2 (13) | 0.500 | |
| Delayed ejaculation is a condition in which it takes an extended period to reach sexual orgasm | 15 (100) | 15 (100) | 13 (87) | 9 (60) | 0.125 | ||
| Measures of sexual dysfunction | Behavioral measures | ||||||
| Start – stop technique | 0 | 2 (13) | 0.500 | 1 (7) | 2 (13) | 1.000 | |
| Penis withdrawal technique | 13 (87) | 13 (87) | 1.000 | 10 (67) | 8 (53) | 0.727 | |
| Milking technique | 1 (7) | 9 (60) | 0.008 | 0 | 0 | ||
| Sexual, psychology and general measures | |||||||
| Premature ejaculation | 4 (27) | 2 (13) | 0.625 | 1 (7) | 1 (7) | 1.000 | |
| Nonpenetrative sexual activity | 3 (20) | 10 (67) | 0.065 | 2 (13) | 4 (27) | 0.500 | |
| Couple's behavior | 11 (73) | 15 (100) | 0.125 | 7 (47) | 9 (60) | 0.688 | |
| Dysorgasmia | 9 (60) | 9 (60) | 1.000 | 3 (20) | 1 (7) | 0.500 | |
| Mechanical, medical, and surgical measures | |||||||
| Viagra for erectile dysfunction | 11 (73) | 14 (93) | 0.250 | 14 (93) | 14 (93) | 1.000 | |
| Testosterone for low libido | 0 | 3 (20) | 0.250 | 1 (7) | 2 (13) | 1.000 | |
| Postsurgery, use of nonpenetrative sex, active involvement of both partners | 15 (100) | 9 (60) | 0.031 | 5 (33) | 10 (67) | 0.125 | |
Control group
For the question on “Normal sexual cycle” and “Symptoms of sexual dysfunction” there was only a slight variation of scores from pretest to posttest. Although there was an improvement (7%–47%), in knowledge regarding question on “Meaning of sexual dysfunction” it was not statistically significant (P = 0.72). Overall it has been observed that there was a decline of scores in all area on “Common male sexual dysfunction.”
There had been decrease in knowledge scores regarding penis withdrawal technique from 67% in pretest to 53% in posttest. Knowledge about couple's behavior improved from 47% in pretest to 60% in posttest. There had been an improvement in knowledge scores regarding postsurgical measures from 33% in pretest to 67% in posttest [Table 2].
There had been marked improvement in the overall mean knowledge score from 9.33 to 14.33 in experimental groups, whereas a minimal improvement from 8.87 to 9.27 was seen in the control group. The difference in the pre- and post-test scores for experimental and control group was compared. As shown in Figure 2, there was a significant difference (P < 0.001) in the improvement between experimental (5 point) verses control arm (0.4 point).
Figure 2.
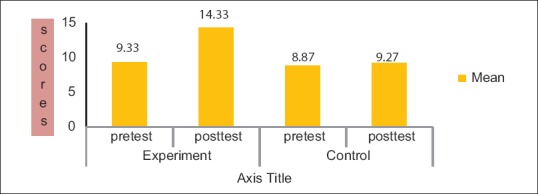
Overall knowledges scores
Grading of the pretest and posttest knowledge score
In experimental group, three subjects got “VERY GOOD” grade in pretest, whereas after intervention majority (13) of the subjects got “VERY GOOD” grade and two of them got “EXCELLENT” grade in posttest, whereas in control group, only four subjects got “VERY GOOD” and one of them got “EXCELLENT” grade in posttest [Table 3].
Table 3.
Grading of the pre- and post-test knowledge scores
| Grade | Experiment (n=15) | Control (n=15) | ||
|---|---|---|---|---|
| Pretest | Posttest | Pretest | Posttest | |
| Poor | 0 | 0 | 0 | 0 |
| Good | 12 | 0 | 13 | 10 |
| Very good | 3 | 13 | 2 | 4 |
| Excellent | 0 | 2 | 0 | 1 |
Poor: <5, Good: 5-10, Very good: 11-15, Excellent: ≥16
Opinion of the subjects regarding information booklet
All the subjects (100%) opined that the information booklet was useful, adequate, self-explanatory, sequential, and clear. They also rated it as very good (80%), good (13%), and excellent (7%). When asked about their views they expressed that the booklet should have little more description on sexual problems (n = 2, 13%) and usage of sex toys (n = 1, 7%) [Figure 3].
Figure 3.
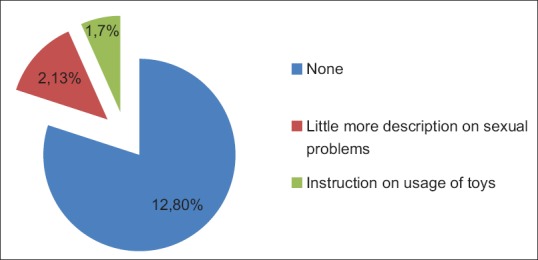
Opinion of subjects on information booklet
Discussion
Urological cancers and its surgeries have a great impact on male sexuality, and efforts must be made to create awareness in the subjects. The information booklet is also an accepted method of disseminating information. Therefore, our study aimed at assessing the knowledge of subjects with regard to sexual dysfunction following urological surgeries and measures to overcome it. Questionnaire addressed general concept of sexual dysfunction, common male sexual dysfunctions, and measures to overcome the problems. In experimental group, 40% of the subjects were in the age group of 18–40 years, whereas in control group, 46% of the subjects were in the age group of 61 years and above. Various research studies have shown that low libido and ED are the most common presenting symptoms in urological cancer patients.[10,11,12] Subjects in the age group of 41 and above had ED (30%) before surgery, probably due to the disease condition. This finding has also been highlighted by Alfredo Nicolosi that age and ED problem go hand in hand.[13]
There is pressing need to address the sexuality issues of these patients as sex is one of the basic need of the human being. Majority (90%) of subjects who had ED (n = 10) were ≥41 years of age.
To the best of our knowledge, this is the first randomized study aiming at the difference in knowledge with respect to sexual dysfunction and measures to overcome it. Areas like general concept of sexual dysfunction had a significant difference while areas like measures to improve sexual dysfunction had least significant difference.
The pre- and post-mean difference score was 0.4 point in control group while it was 5 point for experimental group which shows a significant difference statistically.
Hordon in his study stated that many patients were disappointed by lack of information, support, and practical strategies provided by health professionals to assist them to live with the sexual and intimate changes they had experienced in the face of a life-limiting disease.[14] With regard to “Measures on sexual dysfunction” more than 50% of the subjects were not aware of the common sexual measures which can be used to improve their sexual life and quality of living. which is in conjunction with a study by Hillman in which many middle-aged and older adults were uninformed about the typical physiological changes associated with sexuality and aging and many did not know that ED is typically treatable[15] and there was lack of knowledge regarding available treatments due to reluctance of patients to discuss this issue.[16] Patients with premature ejaculation often view the condition as purely psychological or as a problem that will resolve with time, and many are unaware that medical treatment could be of benefit.[17] In a study by Hartmaan, it was seen that openness and willingness to communicate brought relief in addressing sexual problems of patients.[18] This indicates that more frequent emphasis should be given on this aspect by health-care personnel during routine work-up in the follow-up period.
All the subjects (100%) opined that the information booklet was useful, adequate, self-explanatory, sequential, and clear and expressed need for more description regarding sexual problems and measures. During the data collection period, many subjects personally expressed that they wanted to be active in sexual life, but were unable to discuss these issues with health-care personnel's and the booklet will help them to deal with their problems. Mohammad Al Qadire in his study suggested that health-care settings must provide cancer patients with booklets about the disease, its treatment, side effects, symptoms management, and other available supportive services.[19] The patient, who is the focus of all interaction, should be involved in decision-making and updated with information relevant to them, which in turn will help to create a sense of well-being and satisfaction.[20]
Conclusion
Sexuality is a multi-dimensional concept that can be profoundly altered by the diagnosis and treatment of cancer.[21] Although there is a change in sexual desire post surgery, patients still want to have an active sexual life, poor communication between the health professionals and patients or patients own inhibitive perception prevents them from openly discussing these issues, and they choose abstinence as a solution to these problems. The information booklet had a positive impact on knowledge of subjects and can be used as an effective methodology for providing information to cancer patients. The information booklet on male sexual dysfunction and its measures had served the purpose/filled the deficit gap and thus attempted to help patients with urological cancers. The findings highlight the importance of providing information related to sexual problems and measures to overcome them who had undergoing surgery for urological cancers. The information booklet can be further developed to make it more concise.
Nursing implication
Several implications can be drawn from the present study for nursing practice. The study showed that information needs of patients can be enhanced by providing information through a booklet which they can read and understand at leisure. Sexual health is one of the important components if we look for providing holistic care in clinical practice. The information booklet should be available in all nursing units and provided to all patients undergoing surgeries for urological cancers. Continuing education programs for nursing staff on cancer and sexuality should be held to sensitize the nurse and also help them address issue in cancer surgery patients by providing the information booklet and thus help subjects to deal with the identified conditions. Oncology nursing curriculum must also include sexual rehabilitation in cancer as a component of nursing care.
Strength and weakness
An important topic which is difficult for health care personnel and subjects to discuss were subtly addressed. The investigator attempted to cover common sexual issues and measures to overcome them in a comprehensive manner using a booklet. Such study is not undertaken by any other investigator in India. The investigator was not able collect information using face-to-face interview which would have yielded many more concerns the subjects face in relation to sexuality after being diagnosed with cancer. This study was a part of the Master of Nursing curriculum and therefore, there was a restriction of time period and investigator had to confine sample size to 30, thus a generalization of result findings is questionable. The randomization was not stratified according to demographic variables due to small sample size, and hence, the balance between the groups could not be achieved.
Limitations
Subjects (men with cancers of urological tract) were available only during OPD days (Tuesday and Thursday of the week) when they would come for their follow-up. Self-report techniques were used to collect data. The study measured only change in knowledge but did not assess the impact of knowledge gained on practice or their quality of life. A self-report technique was used to collect data. In-depth information would have been solicited if an open-ended question using interview technique was used. Since the sample size was small (n = 30), findings of the study can be generalized only to the sample under the study. Study did not include sexual problems and measures separately for penile cancer, prostate cancer, testicular cancer, kidney cancer, and bladder cancer due to time restriction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Katz A. The sounds of silence: Sexuality information for cancer patients. J Clin Oncol. 2005;23:238–41. doi: 10.1200/JCO.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 2.Kandeel FR, Koussa VK, Swerdloff RS. Male sexual function and its disorders: Physiology, pathophysiology, clinical investigation, and treatment. Endocr Rev. 2001;22:342–88. doi: 10.1210/edrv.22.3.0430. [DOI] [PubMed] [Google Scholar]
- 3.Derweesh I, Ryan P, Jonathan L, Caroline J, Wassim M, Christopher J, et al. Researchers identify link between kidney removal and erectile dysfunction. Br J Urol Int. 2013;12:55–65. [Google Scholar]
- 4.Nazareth I, Lewin J, King M. Sexual dysfunction after treatment for testicular cancer: A systematic review. J Psychosom Res. 2001;51:735–43. doi: 10.1016/s0022-3999(01)00282-3. [DOI] [PubMed] [Google Scholar]
- 5.Kieffer JM, Djajadiningrat RS, van Muilekom EA, Graafland NM, Horenblas S, Aaronson NK. Quality of life for patients treated for penile cancer. J Urol. 2014;192:1105–10. doi: 10.1016/j.juro.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Frey A, Sønksen J, Jakobsen H, Fode M. Prevalence and predicting factors for commonly neglected sexual side effects to radical prostatectomies: Results from a cross-sectional questionnaire-based study. J Sex Med. 2014;11:2318–26. doi: 10.1111/jsm.12624. [DOI] [PubMed] [Google Scholar]
- 7.George JB. Nursing Theories the Base for Professional Nursing Practice. 6th ed. India: Pearson Publication; 2011. [Google Scholar]
- 8.Orem DE. Nursing Concepts of Practice. Chicago: Mosby Publications; 1995. [Google Scholar]
- 9.Pearson Alan, Vaughan Barbara, Fitzgerald Mary. Nursing models for practice. 3rd edition. Oxford: Elsevier publication, Health Sciences Division, Butterworth-Heinemann publishers; 2005. [Google Scholar]
- 10.Dahl AA, Bremnes R, Dahl O, Klepp O, Wist E, Fosså SD. Is the sexual function compromised in long-term testicular cancer survivors? Eur Urol. 2007;52:1438–47. doi: 10.1016/j.eururo.2007.02.046. [DOI] [PubMed] [Google Scholar]
- 11.Guo P, Xie Z, Wang Y, Wang J. Prevalence of erectile dysfunction in living donors before and after nephrectomy in China. Urology. 2010;76:370–2. doi: 10.1016/j.urology.2010.03.079. [DOI] [PubMed] [Google Scholar]
- 12.Miranda-Sousa AJ, Davila HH, Lockhart JL, Ordorica RC, Carrion RE. Sexual function after surgery for prostate or bladder cancer. Cancer Control. 2006;13:179–87. doi: 10.1177/107327480601300304. [DOI] [PubMed] [Google Scholar]
- 13.Nicolosi A, Moreira ED, Jr, Shirai M, Bin Mohd Tambi MI, Glasser DB. Epidemiology of erectile dysfunction in four countries: Cross-national study of the prevalence and correlates of erectile dysfunction. Urology. 2003;61:201–6. doi: 10.1016/s0090-4295(02)02102-7. [DOI] [PubMed] [Google Scholar]
- 14.Hordern A, Street A. Issues of intimacy and sexuality in the face of cancer: The patient perspective. Cancer Nurs. 2007;30:E11–8. doi: 10.1097/01.NCC.0000300162.13639.f5. [DOI] [PubMed] [Google Scholar]
- 15.Hillman J. Knowledge of Sexuality and Aging. Sexuality and Aging: Clinical Perspectives. 1st edition. Springer publication: Verlag New York; 2012. pp. 29–58. [Google Scholar]
- 16.Althof SE. Prevalence, characteristics and implications of premature ejaculation/rapid ejaculation. J Urol. 2006;175(3 Pt 1):842–8. doi: 10.1016/S0022-5347(05)00341-1. [DOI] [PubMed] [Google Scholar]
- 17.Sotomayor M. The burden of premature ejaculation: The patient's perspective. J Sex Med. 2005;2(Suppl 2):110–4. doi: 10.1111/j.1743-6109.2005.20371.x. [DOI] [PubMed] [Google Scholar]
- 18.Hartmann U, Burkart M. Erectile dysfunctions in patient-physician communication: Optimized strategies for addressing sexual issues and the benefit of using a patient questionnaire. J Sex Med. 2007;4:38–46. doi: 10.1111/j.1743-6109.2006.00385.x. [DOI] [PubMed] [Google Scholar]
- 19.Al Qadire M. Jordanian cancer patients’ information needs and information-seeking behaviour: A descriptive study. Eur J Oncol Nurs. 2014;18:46–51. doi: 10.1016/j.ejon.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Achrekar MS, Murthy V, Kannan S, Shetty R, Nair M, Khattry N. Introduction of situation, background, assessment, recommendation into nursing practice: A prospective study. Asia Pac J Oncol Nurs. 2016;3:45–50. doi: 10.4103/2347-5625.178171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wade, Derick T. Oxford University Press; 2009. “Holistic Health Care.” What is it, and how can we achieve it; pp. 1–35. [Google Scholar]