Abstract
Purpose: This evaluation study sought to assess the impact of an evidence-based medicine (EBM) course on students' self-perception of EBM skills, determine their use of EBM skills, and measure their performance in applying EBM skills in a simulated case scenario.
Methods: Pre- and post-surveys and skills tests were developed to measure students' attitudes toward and proficiency in EBM skills. Third-year students completed the voluntary survey and skills test at the beginning and completion of a twelve-week clerkship in internal medicine (IM) co-taught by medical and library faculty. Data were analyzed using the Mann-Whitney U test for a two-tailed test.
Results: A statistically significant increase was found in the students' self-assessment of skills. Students reported using the journal literature significantly more frequently during the clerkship than before, although textbooks remained their number one resource. A majority of students reported frequent use of EBM skills during the clerkship. Statistically significant improvement in student performance was also found on the posttest, although the level of improvement was more modest than that found on the post-surveys.
Conclusion: The introduction of EBM skills to students during a clinical clerkship provides students an opportunity to practice EBM skills and reinforces the use of evidence in making patient-care decisions.
INTRODUCTION
The Medical School Objectives Project of the Association of American Medical Colleges (AAMC) identified attributes, knowledge, and skill sets that medical students should possess at the time of graduation. One of the identified skills was the ability to retrieve, manage, and utilize biomedical information for clinical decision making. Further, the report advocated incorporating evidence-based medicine (EBM) principles throughout undergraduate medical education [1]. In response to this recommendation, teaching of EBM with its associated skills of literature searching and critical appraisal, took hold in the last decade and has become even more widespread in medical education at the graduate and undergraduate levels [2–5].
A critical appraisal course, focusing on finding and evaluating the best evidence, was formally introduced into the undergraduate curriculum at the University of Illinois College of Medicine at Peoria (UICOMP) in the mid-1980s, and, from the beginning, library involvement was integral to the program [6]. A controlled study in 1992 found that Peoria students scored significantly higher on a test of critical appraisal skills compared with students at another regional site of the medical college who had not received such instruction [7]. In the intervening years, the course continued to develop and evolve in response to student and faculty feedback, course evaluations, and knowledge gained about the teaching of EBM [8].
A recent restructuring of the EBM curriculum emphasized an interactive and real-time approach to learning. To test the effectiveness of this approach, faculty developed a two-part evaluation plan that included a pre- and post-clerkship survey to assess students' self-perceived EBM skills and attitudes and a pre- and posttest to measure their application of EBM skills to a clinical case scenario. The objectives of the evaluation were to (1) assess the self-perception of students' EBM skills before and after completion of the EBM seminar series, (2) determine whether students used EBM skills for patient-care decisions during the clerkship, and (3) measure student performance on a standardized case scenario that required application of EBM skills.
LITERATURE REVIEW
Much of what is known about the effectiveness of curricula for evidence-based practice relies on observational data as reported in the literature [9]. A 1998 systematic review of the effectiveness of instruction in critical appraisal identified seventeen studies, only ten of which were found to be methodologically acceptable, according to the author's inclusion criteria of having a control group and a direct measure of performance. Analysis of these studies showed that interventions implemented in undergraduate programs resulted in significant gains in knowledge as assessed by a written test [10].
In contrast, changes in knowledge at the residency level were small. Green's 1999 critical review of graduate medical education curricula in clinical epidemiology, critical appraisal, and EBM included eighteen reports of varying rigor, with only four meeting a minimum methodological standard of a pretest/posttest controlled trial [11]. Green's analysis of the studies concluded that, although the reports provided useful guides for educators, future studies should increase methodological rigor and focus on more meaningful outcomes.
A systematic review of ten studies published in 2000 showed some evidence that teaching critical appraisal skills not only improves knowledge about research methodology and statistics in clinical research, but also improved attitudes toward use of the medical literature. However, the evidence for an improvement in the ability to appraise evidence critically was not convincing, because only one study employed a randomized controlled design. The authors suggested the need for further development of instruments that can accurately measure the components that contribute to effective EBM interventions [12]. Taylor's questionnaire to evaluate the effectiveness of evidence-based practice teaching is an example of work to this end [13]. Burrows et al. described the development of an EBM course for first-year medical students as a component of a longitudinal outcomes-based curriculum. Course outcomes were demonstrated through various measures including multiple-choice tests, questionnaires, clinically based tests, and observation [14]. Davidson et al. also measured students' competencies in EBM skills and in transmitting information to patients in the context of a performance-based examination [15].
Several rating scales for evaluating searching skills have been reported in the literature. Examples include a scale for student MEDLINE searches used as part of an Objective Structured Clinical Examination (OSCE) for third-year medical students by Burrows and Tylman [16], a survey to assess change in reading and literature searching skills by Ghali et al. [17], a MEDLINE performance checklist for medical residents by Vogel et al. [18], a library skills assessment as part of an EBM curriculum evaluation by Barnett et al. [19], a pre- and post-intervention survey and search strategy evaluation by Bradley et al. [20], and an unpublished scale by Nesbit et al. [21]. Another model used a set of four examination stations to measure skills in searching MEDLINE and the Internet, evaluating research articles, and using the information to make recommendations to patients [22]. Bradley and Humphris also used the exam station model to assess the ability of medical students to apply evidence in practice [23]. Hersh et al. examined the ability of medical and nurse practitioner students to use MEDLINE to obtain evidence for answering clinical questions and concluded that, at best, students were only moderately successful at answering clinical questions correctly with the assistance of a literature search [24].
COURSE DESCRIPTION AND EVALUATION
The practice of medicine is based upon and justified by a vast body of scientific observation, experimentation, and reports of this body of scientific evidence in the medical literature. One of the objectives of the third-year internal medicine (IM) clerkship at UICOMP is for every medical student to learn the basic skills needed to use the medical literature to answer questions that arise in the care of patients. Another objective is to foster the habit of lifelong learning. To best accomplish these objectives, an EBM curriculum was introduced into the clerkship in the mid-1980s. During the last several years, this experience has evolved from a lecture-based and teacher-centered format into an interactive case-based and learner-centered series of seminars.
The current EBM seminar series consists of eight one-hour weekly seminars during the twelve-week IM clerkship. The seminars progress through the five steps of practicing EBM. Prior to each seminar, the students are provided reading materials and worksheets that assist with the critical appraisal process. The focus of the first two sessions, taught by library faculty, is to define EBM, formulate clinical questions based on a standardized case scenario, and identify and review EBM search strategies and resources. The next three sessions are designed to develop the critical appraisal skills of the students with emphasis on therapy, diagnosis, and meta-analysis. General internal medicine faculty lead students through an analysis of selected papers and help students identify clinical questions related to the actual care of their patients. The final three seminars are practice sessions in which students present critically appraised topics (CAT) based on typical patient-care problems encountered during the clerkship to consolidate and demonstrate the learned skills. The CAT presentations are evaluated for formulation of the clinical question, search strategy, assessment of the evidence, applicability of the evidence to the case, and presentation skills.
METHODS
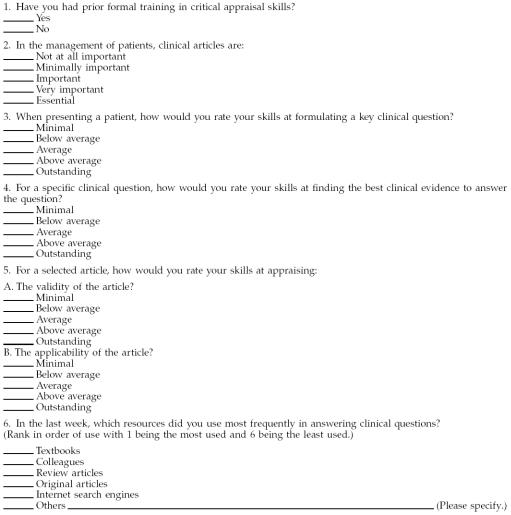
To assess the critical appraisal skills gained by the students and to evaluate course effectiveness, the students were asked to complete a voluntary and anonymous survey at the beginning and end of the clerkship during the 2000/01 academic year (Appendix A). The main objective of the survey was to assess the students' self-perception of change in their EBM skills after completing the EBM seminars. A test was also administered at the beginning and at the end of the EBM seminar series. This instrument was used to assess the skills that the learners had gained during the sessions.
Pre- and post-clerkship survey
Third-year medical students completed a survey at the beginning and end of a twelve-week IM clerkship. The questions focused on the learner's self-perceived EBM skills and use of resources. Data were analyzed using the Mann-Whitney U test for a two-tailed test.
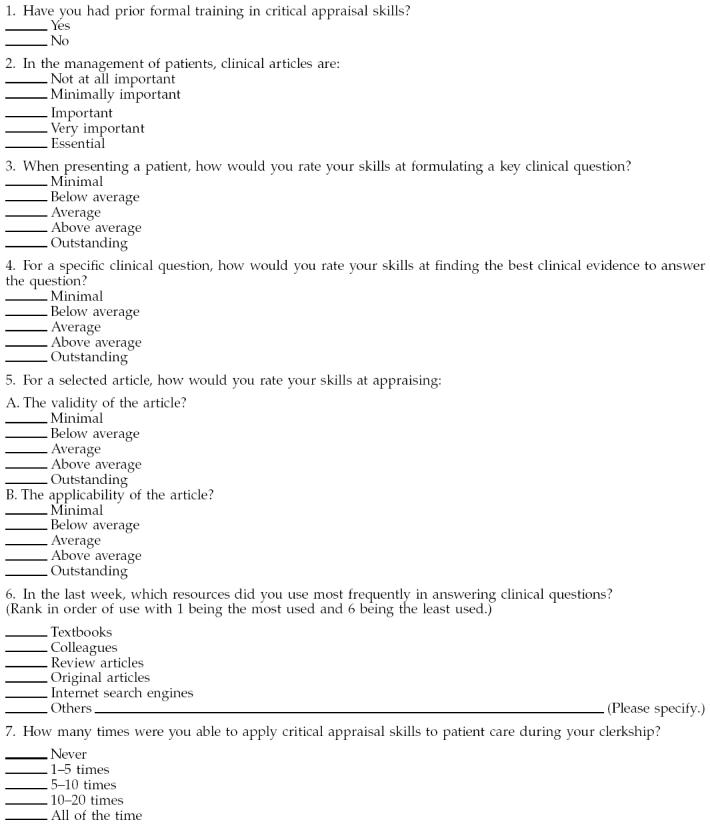
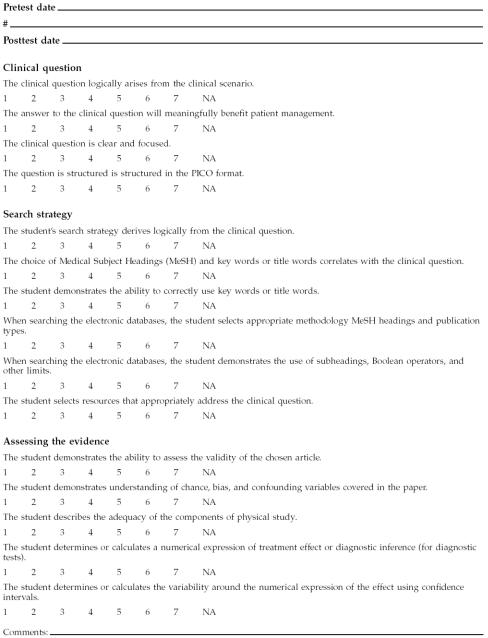
Pre- and posttest skills assessment
The students were given simulated case scenarios both at the beginning and at the end of the clerkship (Appendix B). The posttest was administered the last day of the clerkship and assessed multiple competencies, including formulating a clinical question, using effective strategies to identify the best clinical literature to answer the question, and analyzing the relevance and validity of the retrieved article. The question could be one of therapy, diagnosis, or etiology. A librarian and an internal medicine faculty member evaluated the test answers using a competency-based instrument developed to measure critical appraisal skills (Appendix C).
RESULTS
Survey
The pre-clerkship survey consisted of six questions that assessed the following about the students:
their prior formal EBM training,
their knowledge of the importance of clinical journal articles in the management of patients,
their self-assessment of their skills at formulating clinical questions,
their self-assessment of their skills at finding the best clinical evidence,
their self-assessment of appraising validity and applicability of articles, and
the types of resources they used to answer clinical questions.
The post-clerkship survey asked one additional question that dealt with how many times students applied critical appraisal skills to patient care during the clerkship. Not every student answered every question.
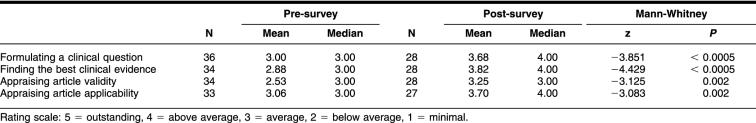
Thirty-six (88%) of forty-one students in the third-year class completed the pre-clerkship survey, and twenty-eight (68%) students returned the post-clerkship survey (Table 1). Only 18.2% (n = 7) stated that they had any formal training in critical appraisal skills prior to the clerkship. On the pre-clerkship survey (using a scale of 1 = not at all important, 3 = important, and 5 = essential), the average rating for the importance of clinical articles in the management of patients was 4.00 (n = 34) or very important. On the post-clerkship survey, the average rating was 3.75 (n = 28). A statistically significant increase was found in the students' perception of their skills in formulating a clinical question, finding the best clinical evidence, and appraising the validity and applicability of an article.
Table 1 Students self-assessment of evidence-based medicine (EBM) skills
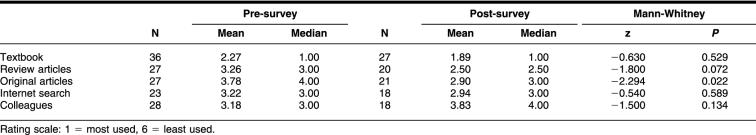
The last question on the post-clerkship survey asked students to rank the resources they used most with 1 being the most used and 6 being the least used (Table 2). The results of the Mann-Whitney U test indicated that students used original articles significantly more frequently after the clerkship than before the clerkship (z = −2.294, two-tailed P = 0.022). There was no statistical significance in the frequency of use in the other resources, and textbooks remained the number one resource used after the clerkship.
Table 2 Resources for answering clinical questions: frequency of use pre- and post-clerkship
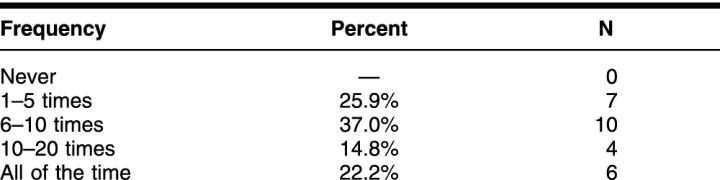
At the end of the twelve-week IM clerkship, students reported the number of times they applied EBM skills. Twenty-six percent of the students reported using EBM skills at least 1 to 5 times, 37% 6 to 10 times, 15% 10 to 20 times, and 22% all of the time (Table 3).
Table 3 Frequency of use of critical appraisal skills during the internal med icine (IM) clerkship
Pre- and posttest
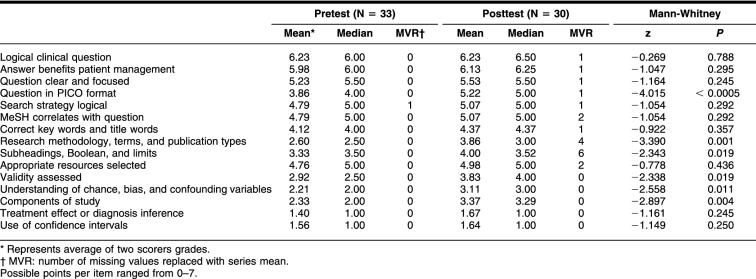
Students were given case scenarios to apply EBM skills to as a pretest and then again as a posttest. The same librarian and internal medicine faculty member graded each student's pretest and posttest. The written case scenarios were graded on 15 different items pertaining to EBM criteria. Each of the 15 items had a possible range of 0 to 7 points. The librarian's and internal medicine faculty member's scores were then averaged for each student's pretest and each student's posttest. The mean and median scores for each of the 15 items for both tests are reported in Table 4. Items where statistically significant improvement occurred were:
structuring the question in the PICO format, which includes (a) the patient or population and the problem, (b) the intervention, (c) the comparison or control, and (d) the outcomes;
when searching the electronic databases, selecting appropriate methodological Medical Subject Headings (MeSH) and publication types;
when searching the electronic databases, demonstrating the use of subheadings, Boolean operators, and other limits;
demonstrating the ability to assess the validity of the chosen article;
demonstrating the understanding of chance, bias, and confounding variables covered in the paper; and
describing the adequacy of the components of the physical study.
Table 4 Comparison of pre- and posttest using case scenarios
On the pretest, students were rated highest (5–7) on the following criteria: (1) the clinical question logically arose from the clinical scenario (mean = 6.23), (2) the answer to the clinical question would meaningfully benefit patient management (mean = 5.98), and (3) the clinical question was clear and focused (mean = 5.23). Students were rated lowest (0–2 points) on: (1) determining or calculating the variability around the numerical expression of the effect using confidence intervals (mean = 1.56) and (2) determining or calculating a numerical expression of treatment effect or diagnosis inference for diagnostic tests (mean = 1.40).
On the posttest, students were rated highest (5–7) on the following criteria: (1) the clinical question logically arose from the clinical scenario (mean = 6.23), (2) the answer to the clinical question would meaningfully benefit patient management (mean = 6.13), (3) the clinical question was clear and focused (mean = 5.53), (4) the question was structured in the PICO format (mean = 5.22), (5) the search strategy derived logically from the clinical question (mean = 5.07), and (6) the choice of MeSH headings and key words or title words correlated with the clinical question (mean = 5.07). Students were rated the lowest (0–2) on: (1) determining or calculating the variability around the numerical expression of the effect using confidence intervals (mean = 1.67) and (2) determining or calculating a numerical expression of treatment effect or diagnosis inference for diagnostic tests (mean = 1.64).
DISCUSSION
Evidence-based medicine is incorporated into the IM clerkship curriculum with the goals of developing critical appraisal skills and establishing lifelong learning habits. Survey results indicate that students' self-perception improved in all the key areas of critical appraisal skills including formulating a clinical question, finding the literature, and evaluating the evidence. Also significant is that students reported using the journal literature more frequently after the clerkship than before. Textbooks remained the number one resource, as would be expected for students at this stage of experience and learning. The pre- and post-questionnaire assessing medical students' attitudes toward and knowledge of the use of the medical literature by Landry et al. showed that knowledge and attitudes did improve, but actual use of literature in patient write-ups did not [25].
The post-survey asked students the additional question of how many times they applied EBM skills to patient care during the clerkship. In this study, the self-report of the number of times students used EBM skills was encouraging, because responses reflected that students were using the skills with regularity.
Although the students' self-perceived skills in EBM improved at the end of the clerkship, some of the results did not match the level of performance on the post-clerkship skills test. This discrepancy could be due to multiple factors. The posttest was administered the last day of the clerkship on a Friday afternoon after the clerkship exam. The posttest assessed multiple competencies, and the results were not counted as part of the clerkship final grade. These factors might have contributed to the impatience with the posttest process that the test administrator observed in many of the students. In the future, changing the timing of the posttest or including the posttest results in the clerkship grade will be considered to see if these would positively affect student performance. Lack of a validated evaluation tool might also have contributed to the uneven results between the survey and the test.
Since the time this study was completed, a study appeared in the literature in which a questionnaire for measuring improvement in knowledge and skills following a short EBM course in a post-graduate setting was validated [26]. This instrument was shown to reliably assess knowledge and skills in EBM following an intensive three-day course. Although the subjects and course length differ, this, or some other validated tool, may prove useful in future studies of the impact of EBM training in the undergraduate curriculum.
Finally, the complexity of the skills measured by the posttest may require a longer period of time than a short eight-week course that meets once a week. The teaching of the complex cognitive skills required for clinical decision making is important at all levels of the curriculum, and the skills may not be mastered after one intervention. Rather, these skills supply the foundation for making clinical decisions based on the evidence and the practice of lifelong learning.
The areas in which the students scored the lowest on the skills test were the statistical elements. Even though the gains were small in these areas, students might be expected to improve with cumulative clinical exposure and a more integrated, longitudinal EBM curriculum. Srinivasan et al. demonstrated that the introduction of EBM principles as a short course to preclinical medical students even as early as the first year is feasible and practical as an introduction and first step, but they stressed the need for reinforcement through application and integrated repetition [27]. This study did not assess the long-term follow up of students' EBM skills to see if they retained skills at the end of medical school or residency. However, a survey of the graduates of the IM EBM course is currently in progress by the authors to address this question.
CONCLUSIONS
The positive attitude toward EBM shown in the post-survey, the increased use of the literature in answering clinical questions, and the significant improvement in the areas of formulating a question and a literature search strategy are indicators that the educational approach used in these EBM seminar series is effective in promoting awareness and knowledge of EBM. The practice of evidence-based medicine comprises a set of skills and clinical experience that is important for informed clinical decision making. Introducing EBM skills to students during a clinical clerkship provides students an opportunity to practice these skills. It further reinforces the use of current best evidence in making decisions about the care of individual patients, even if all the skills are not immediately mastered. The short-term impact of these sessions on attitudes toward and knowledge of EBM has been positive. However, carefully designed studies are required to evaluate the long-term effects of EBM curricula in changing behaviors, practice patterns, and patient-care outcomes.
APPENDIX A
Internal medicine pre-clerkship survey
Directions: Please select the one best answer for each item. All surveys will be collated for anonymity.
Internal medicine post-clerkship survey
Directions: Please select the one best answer for each item. All surveys will be collated for anonymity.
APPENDIX B
Pre and posttest case scenarios
The goal of the pretest and posttest is to help evaluate the efffectiveness of the ``Critical Appraisal Skills'' seminar. The test results will be used for study purposes only and will not contribute to the final grade. We appreciate your cooperation in this matter. Your feedback will help us develop a better curriculum.
Pretest
A fifty-five-year-old female with significant medical history of hypertension presents to the hospital with complaints of a sudden onset of pleuritic chest pains and shortness of breath. Denies fever, chills, orthopnea, and paroxysmal nocturnal dyspnea (PND). Has noticed increased swelling in her right lower extremity for two days, since she returned from her recent vacation. Her current medications include estrogens and Atenelol. The rest of her past medical history, social history, and family histories are unremarkable.
Her vital signs were remarkable for heart rate (HR) of 112, respiration rate (RR) 24, and pulse oximeter of 88% on room air. Rest of her physical examination was unremarkable. A ventilation-perfusion (V/Q) scan was ordered in the emergency department that was read as high probability for pulmonary embolism. The patient was started on Lovenox based on the test results. Treatment with Coumadin was initiated in the hospital. She was discharged home in stable condition and advised to continue Coumadin for six months.
▪Identify and frame a clinical question based on therapy, diagnosis, or etiology
▪Develop a search strategy to best answer the clinical question
▪Outline the search strategy utilized in finding the answer to your clinical answer
▪Identify an article(s) that answers your clinical question
▪Critically appraise the article for validity
Posttest
Fifty-five-year-old male with history of hypertension and type II diabetes mellitus presents with suddent onset of right-sided weakness and numbness. Denies headache, history of trauma, chest pain, shortness of breath. His current medications include Glucotrol XL, hydrocholorthiazide (HCTZ), lisinopril, and aspirin. On presentation to the Emergency Department (ED), he was in atrial fibrillation with rapid ventricular response. His neurology exam was remarkable for distal weakness in both upper and lower extremities. Plantar was downgoing on the right. The rest of his physical examination was unremarkable.
In the ED, he had a computer-assisted tomography (CAT) scan of his head, which had no evidence of an acute bleed or new infarct. His counter immune electrophoreses (CIEs) were negative, thyroid-stimulating hormone (TSH) was normal, and an echo revealed an edema factor (EF) of 34%, dilated left atrium and mild to moderate mitral regurgitation. His complete blood count (CBC) and basic metabolic panel (BMP) were within normal limits.
He was started on IV Cardizem and AZA. He was admitted to the neurology service. During the hospital stay, his symptoms and signs resolved within twenty-four hours. He was started on Coumadin and discharged in stable condition.
▪Identify and frame a clinical question
▪Develop a search strategy to best answer the clinical question
▪Outline the search strategy utilized in finding the answer to your clinical question
▪Attach a copy of the article identified
▪Critically appraise the article for validity
APPENDIX C
Evaluation instrument
Contributor Information
Josephine L. Dorsch, Email: jod@uic.edu.
Meenakshy K. Aiyer, Email: aiyer@uic.edu.
Lynne E. Meyer, Email: lmeyer@uic.edu.
REFERENCES
- Learning objectives for medical student education: guidelines for medical schools: report I of the medical school objectives project. Acad Med. 1999 Jan; 74(1):13–8. [DOI] [PubMed] [Google Scholar]
- Aiyer M, Hemmer P, Meyer L, Albritton TA, Levine S, and Reddy S. Evidence-based medicine in internal medicine clerkships: a national survey. South Med J. 2002 Dec; 95(12):1389–95. [PubMed] [Google Scholar]
- Alguire PC. A review of journal clubs in postgraduate medical education. J Gen Intern Med. 1998 May; 13(5):347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green ML. Evidence-based medicine training in internal medicine residency programs: a national survey. J Gen Intern Med. 2000 Feb; 15(2):129–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green ML. Graduate medical education training in clinical epidemiology, critical literature appraisal, and evidence based medicine: a critical review of curricula. Acad Med. 1999 Jun; 74(6):686–94. [DOI] [PubMed] [Google Scholar]
- Dorsch JL, Frasca M, Wilson M, and Tomsic M. A multidisciplinary approach to information and critical appraisal instruction. Bull Med Libr Assoc. 1990 Jan; 78(1):38–44. [PMC free article] [PubMed] [Google Scholar]
- Frasca M, Dorsch JL, Aldag J, and Christiansen R. A multidisciplinary approach to information and critical appraisal instruction: a controlled study. Bull Med Libr Assoc. 1992 Jan; 80(1):23–8. [PMC free article] [PubMed] [Google Scholar]
- Dl Sackett, Strauss SE, Richardson WS, Rosenberg W, and Haynes RB. Evidence-based medicine: how to practice & teach EBM. 2nd ed. Edinburgh and New York, NY: Churchill-Livingstone, 2000. [Google Scholar]
- Hatala R, Guyatt G. Evaluating the teaching of evidence-based medicine. JAMA. 2002 Sep 4; 288(9):1110–2. [DOI] [PubMed] [Google Scholar]
- Norman GR, Shannon SI. Effectiveness of instruction in critical appraisal (evidence-based medicine) skills: a critical appraisal. Can Med Assoc J. 1998 Jan 27; 158(2):177–81. [PMC free article] [PubMed] [Google Scholar]
- Green ML. Graduate medical education training in clinical epidemiology, critical literature appraisal, and evidence based medicine: a critical review of curricula. Acad Med. 1999 Jun; 74(6):686–94. [DOI] [PubMed] [Google Scholar]
- Taylor R, Reeves B, Mears R, Keast J, Binns S, Ewings P, and ad Khan K. A systematic review of the effectiveness of critical appraisal skills training for clinicians. Med Educ. 2000 Feb; 34(2):120–5. [DOI] [PubMed] [Google Scholar]
- Taylor R, Reeves B, Ewings P, Binns S, Keast J, and Mears R. Development and validation of a questionnaire to evaluate the effectiveness of evidence-based practice teaching. Med Educ. 2000 Jun; 35(6):544–7. [DOI] [PubMed] [Google Scholar]
- Burrows S, Moore K, Arriaga J, Paulaitis G, and Lemkau HL. Developing an “Evidence-Based Medicine and Use of the Biomedical Literature” component as a longitudinal theme of an outcomes-based medical school curriculum: year 1. J Med Libr Assoc. 2003 Jan; 91(1):34–41. [PMC free article] [PubMed] [Google Scholar]
- Davidson RA, Duerson M, Romrell L, Pauly R, and Watson RT. Evaluating evidence-based medicine skills during a performance-based examination. Acad Med. 2004 Mar; 79(3):272–5. [DOI] [PubMed] [Google Scholar]
- Burrows SC, Tylman V. Evaluating medical student searches of MEDLINE for evidence-based information. Bull Med Libr Assoc. 1999 Oct; 87(4):471–6. [PMC free article] [PubMed] [Google Scholar]
- Ghali WA, Saitz R, Eskew AH, Gupta M, Quan H, and Hershman WY. Successful teaching in evidence-based medicine. Med Educ. 2000 Jan; 34(1):18–22. [DOI] [PubMed] [Google Scholar]
- Vogel EW, Block KR, and Wallingford KT. Finding the evidence: teaching medical residents to search MEDLINE. J Med Libr Assoc. 2002 Jul; 90(3):327–30. [PMC free article] [PubMed] [Google Scholar]
- Barnett SH, Kaiser S, Morgan LK, Sullivant J, Siu A, Rose D, Rico M, Smith L, Schechter C, Miller M, and Stagnaro-Green A. An integrated program for evidence-based medicine in medical school. Mt Sinai J Med. 2000 Mar; 67(2):163–8. [PubMed] [Google Scholar]
- Bradley DR, Rana GK, Martin PW, and Schumacher RE. Real-time, evidence-based medicine instruction: a randomized controlled trial in a neonatal intensive care unit. J Med Libr Assoc. 2002 Apr; 90(2):194–201. [PMC free article] [PubMed] [Google Scholar]
- Nesbit KW, Glover J, Shipley M, and Holloway RG. What's the score? evaluating student's MEDLINE searches. Presented at: MLA '02, the 102nd Annual Meeting of the Medical Library Association; Dallas, TX: May 17–23, 2002. [Google Scholar]
- Berner ES, McGowan JJ, Hardin M, Spooner A, Raszka W, and Beckow RL. A model for assessing information retrieval skills of medical students. Acad Med. 2002 Jun; 77(6):547–51. [DOI] [PubMed] [Google Scholar]
- Bradley P, Humphris G. Assessing the ability of medical students to apply evidence in practice: the potential of the OSCE. Med Educ. 1999 Nov; 33(11):815–7. [DOI] [PubMed] [Google Scholar]
- Hersh WR, Crabtree K, Hickman DH, Sacherek L, Friedman CP, Tidmarsh P, Mosbaek C, and Kraemer D. Factors associated with success in searching MEDLINE and applying evidence to answer clinical questions. J Am Med Infor Assoc. 2002 Jun; 9(3):283–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry FJ, Pangaro L, Kroenke K, Lucey C, and Herbers J. A controlled trial of a seminar to improve medical student attitudes toward, knowledge about, and use of the medical literature. J Gen Intern Med. 1994 Aug; 9(8):436–9. [DOI] [PubMed] [Google Scholar]
- Fritsche L, Greenhalgh T, Falck-Ytter Y, Neumayer H, and Kunz R. Do short courses in evidence-based medicine improve knowledge and skills? validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002 Dec 7; 325(7376):1338–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan M, Weiner M, Breitfeld PP, Brahmi F, Dickerson KL, and Weiner G. Early introduction of an evidence-based medicine course to preclinical medical students. J Gen Intern Med. 2002 Jan; 17(1):58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]