Abstract
Background
Understanding resource utilization patterns among high-cost patients may inform cost reduction strategies.
Objective
To identify patterns of high-cost healthcare utilization and associated clinical diagnoses and to quantify the significance of hot-spotters among high-cost users.
Design
Retrospective analysis of high-cost patients in 2012 using data from electronic medical records, internal cost accounting, and the Centers for Medicare and Medicaid Services. K-medoids cluster analysis was performed on utilization measures of the highest-cost decile of patients. Clusters were compared using clinical diagnoses. We defined “hot-spotters” as those in the highest-cost decile with ≥4 hospitalizations or ED visits during the study period.
Participants and Exposure
A total of 14,855 Medicare Fee-for-service beneficiaries identified by the Medicare Quality Resource and Use Report as having received 100 % of inpatient care and ≥90 % of primary care services at Cleveland Clinic Health System (CCHS) in Northeast Ohio. The highest-cost decile was selected from this population.
Main Measures
Healthcare utilization and diagnoses.
Key Results
The highest-cost decile of patients (n = 1486) accounted for 60 % of total costs. We identified five patient clusters: “Ambulatory,” with 0 admissions; “Surgical,” with a median of 2 surgeries; “Critically Ill,” with a median of 4 ICU days; “Frequent Care,” with a median of 2 admissions, 3 ED visits, and 29 outpatient visits; and “Mixed Utilization,” with 1 median admission and 1 ED visit. Cancer diagnoses were prevalent in the Ambulatory group, care complications in the Surgical group, cardiac diseases in the Critically Ill group, and psychiatric disorders in the Frequent Care group. Most hot-spotters (55 %) were in the “frequent care” cluster. Overall, hot-spotters represented 9 % of the high-cost population and accounted for 19 % of their overall costs.
Conclusions
High-cost patients are heterogeneous; most are not so-called “hot-spotters” with frequent admissions. Effective interventions to reduce costs will require a more multi-faceted approach to the high-cost population.
Keywords: High-cost, Hot-spotter
Introduction
Healthcare costs are concentrated among a small fraction of the population,1 – 4 and a reasonable strategy to reduce healthcare costs is to focus efforts on this high-cost group. Most studies of high-cost patients have focused on how they differ from the remaining low-cost population, including their older age, multiple chronic illnesses, and more frequent hospitalizations.5 – 7 Commonly, high-cost patients are thought to be “hot-spotters,” i.e., chronic disease patients with a high utilization of inpatient and emergency services due to inadequate primary care.8 – 10
Based on this understanding of high-cost patients, reducing admissions through outpatient care coordination—including programs to increase patient adherence to medications and self care, facilitate patient-physician communication, and numerous other activities11 – 13—is an appealing method of reducing healthcare costs. However, care coordination programs, which generally emphasize intensive telephone and office-based follow-up, have not yielded definitive savings.14 , 15 One explanation is that high-cost patients are often admitted for non-preventable causes.16 Another observation is that there are at least two types of high-cost inpatient groups: patients with frequent medical admissions and surgical patients with infrequent admissions, whose utilization is unlikely to be affected by intensive outpatient follow-up.17
Thus, not all high-cost patients may benefit from care coordination. The proportion of high-cost patients with frequent hospitalizations and ED visits is unknown, and care coordination may not affect other types of high-cost utilization. Better characterization of the spectrum of high-cost utilization patterns can offer insights to inform cost-reduction strategies.
The purpose of this study was to characterize the utilization patterns of high-cost patients. First, we performed a cluster analysis of high-cost patients’ inpatient and outpatient utilization over 1 year. We then examined characteristic conditions and mortality rates among clusters. Finally, we sought to quantify the extent to which high-cost patients were also hot-spotters of admissions and ED visits and to quantify the contribution of hot-spotters to the total cost of high-cost patients.
Methods
Patients and Setting
We performed a retrospective chart review of high-cost patients in a single health system. As part of the Physician Feedback/Value-Based Payment Modifier Program, the Center for Medicare and Medicaid Services (CMS) provides comparative performance information through the Quality and Resource Use Report (QRUR).18 Individual-level data provided in the report include the percentage of primary care services billed to the provider group and the dates and admitting hospitals for all hospitalizations, excluding those with a primary diagnosis of alcohol and substance abuse. Using the 2012 QRUR, we identified 14,855 Medicare fee-for-service patients who were hospitalized exclusively at Cleveland Clinic Health System (CCHS) hospitals and received at least 90 percent of their primary care services at a CCHS facility in 2012. We included all patients meeting these criteria, including those younger than 65 who received Medicare for other qualifying conditions. CCHS is a nonprofit, multispecialty practice comprising a 1440-bed academic medical center, eight community hospitals, and over 75 regional outpatient clinics in Northeast Ohio.
Cost
For each patient, costs were derived from the health system’s cost-accounting system (Enterprise Performance Systems), a commercially available automated system that integrates multiple data sources to calculate costs at a charge code level per patient for services rendered. We summed all direct and indirect costs per patient associated with receiving care at a CCHS facility, including the cost of diagnostic tests, imaging, hospital-administered drugs, Emergency Department services, administrative overhead, and physician salaries. The costs of post-acute services were included only for those patients who were admitted to a CCHS post-acute care facility. We could not estimate the cost of outpatient medication filled at outside pharmacies. We defined high-cost patients as those in the top decile of costs, as others have previously defined high cost.16 , 17 , 19
Utilization Measures, Diagnoses, and Procedures
The electronic medical record (EMR) was used to extract counts of admissions, total hospital days, inpatient surgeries, ICU days, ED visits, primary care (PCP) visits, specialist physician visits, and all other outpatient visits. We used Clinical Conditions Software (CCS) to classify primary and secondary ICD-9 diagnosis and procedures codes into clinically meaningful categories.20 The AHRQ Procedure Classes Software was used to identify ICD-9 procedure codes as major OR procedures.21 We studied the prevalence of a limited number of high-cost diagnoses and procedures in our population. We defined “high-cost” diagnoses based on a literature search; conditions previously identified as “high cost” included COPD, heart failure, COPD, osteoarthritis, and sepsis.16 , 22 – 24 We also used our clinical judgment and added diagnoses with potentially significant influence on cost, such as “abdominal pain.”
Cluster Analysis
Inpatient costs, outpatient costs, inpatient days, hospital admissions, ICU days, ED visits, and major inpatient OR procedures were log-transformed. All variables were then range standardized.25
Cluster analysis is an exploratory method of data analysis whereby groups of individual data points (in this case patients) are formed based on similarity across variables of interest.26 Given the skewed nature of the above variables, the k-medoids method of data clustering was selected because of its robustness to outliers.27 – 29 An important decision in a clustering analysis is to determine the number of clusters (k) to investigate. K-medoids requires that the number of clusters be specified beforehand. To this end, we first employed Ward’s hierarchical minimum variance method to create a clustering dendrogram.30 This diagram, along with PCA plots and the within-cluster error sum of squares, was used to characterize potential clusters and inform our selection of the cluster number. Based on these, we specified five as the number of clusters for the k-medoids analysis. The centroids from the k = 5 Ward’s clustering were also used as the initial seeds for k-medoids. Next, the k-medoids algorithm was run to produce our final clusters.
Cluster validity was assessed via a cross validation technique, in which the data were repeatedly split into random halves and each half was independently clustered for a thousand repetitions. Cluster validity was then expressed as the proportion of repetitions wherein clustering labels matched cross-classification labels, which we termed cluster stability. In addition to a mathematical assessment of cluster validity, clinical information not included in the clustering algorithm can be used to verify cluster validity.26 Therefore, to better understand our clusters we examined the frequency of primary and secondary diagnoses within each cluster. First, we examined the most common primary high-cost diagnoses across the five clusters. Next, we examined the relative incidences of high-cost conditions, both primary and secondary, across all clusters. Odds ratios were calculated based on high-cost condition prevalence in each utilization cluster compared to high-cost condition prevalence in the overall high-cost utilization group. R version 3.0.2 was used for all analyses. The cluster package version 2.0.3 was used for cluster analyses.
Definition of Hot-Spotters
“Frequent ED visits” are commonly defined as four or more in a year.31 , 32 The definition of “frequent hospitalizations” ranges widely, from 2 to 6.17 , 33 – 37 Based on the literature and the distribution of ED visits and admission in our own study population, we defined hot-spotters as those with four or more hospitalizations, ED visits, or both during the study period; these patients were in the 95th percentile for each of those utilization categories.
Results
Our high-cost sample included 1486 patients; 55 % were male, and mean age was 66, which was significantly younger than the rest of the population (Table 1). High-cost patients accounted for 60 % of total costs; the most expensive 5 % of the population accounted for nearly 45 %, and the most expensive 1 % of the population accounted for 19 % of total costs. Only half of the high-cost population’s costs were attributable to hospital admissions; however, the vast majority (87 %) of the total population’s inpatient cost was concentrated in the high-cost decile.
Table 1.
Characteristics of the High-Cost Population Compared to Low-Cost
| High-cost population | Low-cost population | |
|---|---|---|
| n | 1486 | 13,369 |
| Male (%) | 55 | 51 |
| Average age (SD) | 66 (14) | 70 (11) |
| % of Total cost | 60 | 40 |
| % of Group cost attributable to inpatient utilization | 48 | 9 |
| Median inpatient days (IQR) | 4 (9) | 0 (0) |
In the cluster analysis, we identified five clusters (Table 2). The “ambulatory” cluster primarily received outpatient care; cancer and chemotherapy were common conditions in this group (Table 3). The “surgical” cluster had a median of two inpatient surgeries, compared to none in the other groups. They had the highest odds of care complications and osteoarthritis. Sixty-one percent of these patients with osteoarthritis underwent arthroplasty. “Critically Ill” patients had a median of 4 days in the ICU, while ICU stays were rare for the other groups. Critically ill patients had higher odds of heart failure and cardiac arrhythmia and arrest and the highest median inpatient costs. The “Frequent Care” cluster had a median of 2 admissions, 3 ED visits, and 29 outpatient visits, placing them at or near the top of these utilization categories. Psychiatric disorders, substance abuse, and COPD/asthma were common. “Mixed Utilization” patients had a median of one admission, one ED visit, and 23 outpatient visits.
Table 2.
Results: Cluster Analysis of Utilization Among High-Cost Clusters, Median (Inter-Quartile Range)
| Ambulatory Care | Surgical | Critically Ill | Frequent Care | Mixed Utilization | |
|---|---|---|---|---|---|
| Patients (n)* | 415 | 297 | 164 | 281 | 329 |
| Age* | 68 (14) | 68 (10) | 69 (23) | 67 (23) | 68 (14) |
| Admissions | 0 (0) | 1 (1) | 2 (2) | 2 (1) | 1 (0) |
| Inpatient days | 0 (0) | 5.8 (6.1) | 19.4 (18.6) | 11.8 (10.0) | 4.8 (3.6) |
| ICU days | 0 (0) | 0 (0.2) | 4.0 (4.3) | 0 (0) | 0 (0) |
| Inpatient surgeries | 0 (0) | 2 (1) | 0 (1) | 0 (0) | 0 (0) |
| ED Visits | 0 (1) | 0 (1) | 2 (3) | 3 (3) | 1 (2) |
| PCP visits | 2 (3) | 2 (4) | 2 (4) | 3 (5) | 3 (4) |
| Specialist visits | 14 (13) | 9 (8) | 10 (12) | 13 (13) | 11 (10) |
| Ancillary visits | 10 (13) | 12 (13) | 9 (17) | 13 (18) | 9 (14) |
| Inpatient costs ($) | 0 | 27,851 | 48,019 | 22,453 | 12,611 |
| Outpatient costs ($) | 30,266 | 10,645 | 12,106 | 16,564 | 15,794 |
*Represents variables that were not incorporated in the cluster analysis
Table 3.
Percent Prevalence of High-Cost Conditions among the Five High-Cost Utilization Clusters
| Overall % (N = 1486) | Ambulatory % (n = 415) | Surgical % (n = 297) | Critically Ill % (n = 164) | Frequent Care % (n = 281) | Mixed Utilization % (n = 329) | |
|---|---|---|---|---|---|---|
| Cancer | 52 | 63 ** | 52 | 34** | 47 | 52 |
| Diabetes | 42 | 34** | 47 | 50* | 45 | 42 |
| Cardiac arrhythmia/arrest | 40 | 22 ** | 41 | 62** | 44 | 38 |
| Ischemic heart disease | 33 | 20 ** | 37 | 48** | 35 | 34 |
| Renal disease | 29 | 15 ** | 23** | 55** | 34** | 32 |
| Trauma | 27 | 20 ** | 22* | 36** | 44 ** | 22 * |
| Osteoarthritis | 26 | 23 | 29 | 20 | 28 | 27 |
| Heart failure | 21 | 7 ** | 16 | 43** | 29 ** | 25 |
| Procedure/device complication | 20 | 9 ** | 22 | 36** | 25** | 17 |
| COPD/asthma | 24 | 15 ** | 21 | 27 | 40 ** | 24 |
| Abdominal pain | 16 | 13 | 8** | 19 | 26 ** | 15 |
| Chemo-radiation | 15 | 29 ** | 6 ** | 6** | 12 | 14 |
| Cerebrovascular disease | 14 | 9 ** | 16 | 22** | 14 | 14 |
| Heart valve disorder | 16 | 9 ** | 17 | 28** | 19 | 16 |
| Psychiatric disorder | 25 | 18 ** | 20* | 30 | 39 ** | 22 |
| Complication of care | 23 | 8 ** | 33** | 43** | 29* | 17* |
| Pneumonia | 7 | 2 ** | 4 | 15** | 13** | 7 |
| Peripheral atherosclerosis | 15 | 7** | 17 | 24** | 20* | 15 |
| Substance-related disorder | 7 | 3** | 4 | 9 | 14** | 6 |
| Respiratory failure | 8 | 1** | 6 | 35** | 10 | 4* |
| Cognitive disorder | 5 | 2** | 3 | 9 * | 8* | 6 |
| Liver disease | 5 | 3* | 5 | 6 | 8* | 3 |
| Sepsis | 4 | 0 | 2 | 17** | 8** | 3 |
*p ≤ 0.05, **p ≤ 0.01, p-values compare prevalence in the specific utilization cluster to prevalence in the overall high-cost population
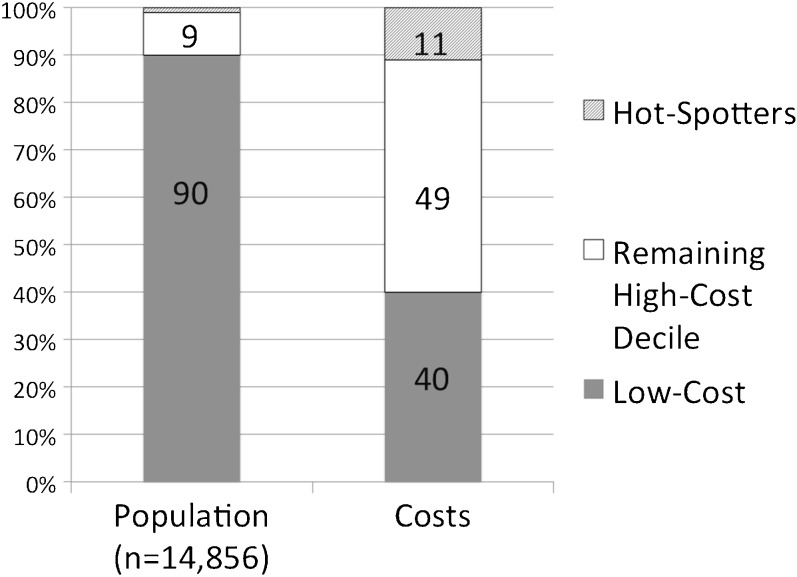
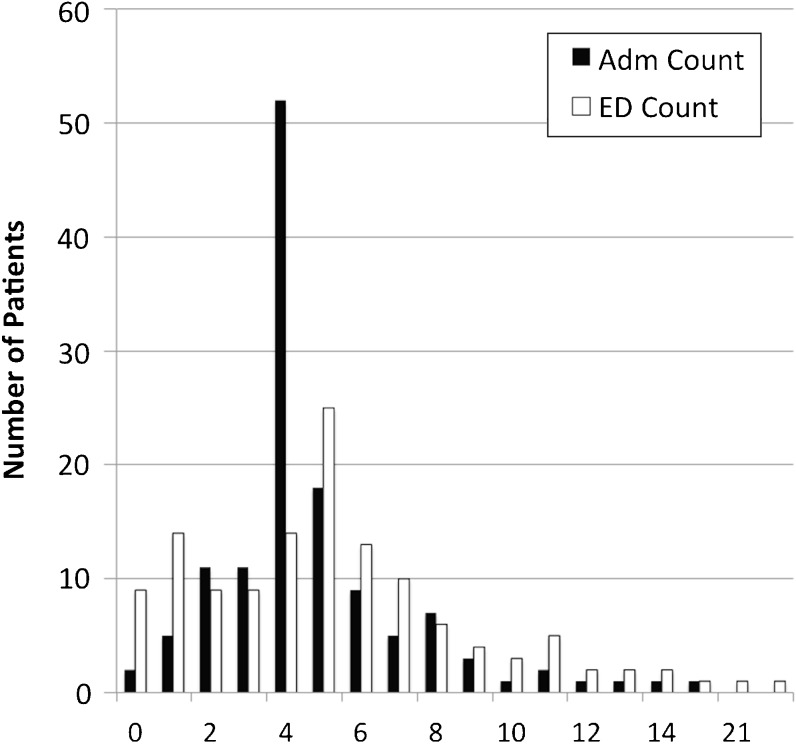
Hot-spotters (n = 130), i.e., those with four or more admissions (n = 55), four or more ED visits (n = 29), or both (n = 46), were 52 % male with a mean age of 62. They accounted for 9 % of high-cost patients and 19 % of that population’s costs (11 % of the total population’s costs; Fig. 1). Fifty-five percent of hot-spotters were in the “Frequent Care” cluster, 37 % in the “Critically Ill” cluster, 5 % in the “Mixed Utilization” cluster, and the remaining 2 % in the other clusters. Hot-spotters had a wide range of admissions and ED visits (Fig. 2). Hot-spotters had a 14 % 1-year mortality rate, higher than 8.6 % observed among all high-cost patients.
Figure 1.
Distribution of hot-spotters among high-cost patients and their attributable costs. Diagonal stripes: hot-spotters. White bar: remaining high-cost patients. Gray bar: low-cost patients.
Figure 2.
Distribution of admissions and ED visits among hot-spotters. Black bar: Admission counts. White bar: ED visits.
Discussion
Previous reports on high-cost patients have compared differences among high- and low-cost patients, highlighting the fact that high-cost patients are admitted more frequently and have more chronic diseases, but few have characterized differences among high-cost patients. In this study, we identified five distinct phenotypes of high-cost patients with diverse drivers of cost and quantified the significance of hot-spotters among them. The majority of “hot-spotters” were in the cluster of patients who had frequent care, and as expected, they were very expensive. This top 1 % of the total population accounted for 11 % of their entire cost. Notably, they had high mortality rates, consistent with observations that high-cost patients are those near the end of life.38 – 40 Care coordination efforts may be most effective when targeted at the remainder of the frequent care group, which was characterized by comorbid psychiatric illness, substance abuse, and asthma/COPD.
However, hot-spotters and other frequent utilizers represented only a small portion of high-cost patients and their costs. Our observations suggest that limited cost savings can be achieved by targeting frequent hospitalizations alone. For example, the ambulatory cluster of high-cost patients had no inpatient utilization at all. This group had high rates of chemo- and/or radiation therapy and other treatments for cancer. With the projected rise of cancer incidence and treatment cost, their contribution to overall costs will likely accelerate.41 – 43 Few programs are aimed at reducing cancer costs, but tools that allow patients and providers to weigh treatment options based on cost vs. marginal benefit are available.44
Another cluster had costs driven primarily by surgery. Others have observed surgeries to contribute to high costs without frequent admissions.17 Almost half of total hospital costs may be attributable to stays involving OR procedures, the most common of which involve the musculoskeletal system.45 , 46 Joint replacements represent the largest portion of Medicare payments to hospitals by diagnosis-related grouping.47 Some studies suggest that improving efficiency and bundling payments by episodes of care may result in substantial savings.48 , 49 Increasing price transparency and creating marketplace competition for devices could also reduce costs.50 – 52
Critically ill patients represent another high-cost group for whom care coordination is unlikely to be effective. Critical care medicine already poses a significant burden on the US health system, and intensive care units (ICU) continue to expand.53 With increased ICU bed supply, patients who are not critically ill and those who are unlikely to survive regardless of ICU care may nevertheless be admitted to ICUs,54 highlighting the need for policies that incentivize the judicious use of ICU resources. Avoiding delays in transfer from the ICU to regular nursing floors55 , 56 and appropriate initiation of palliative care may also reduce costs.57
Table 4 provides a consolidated overview of suggested first steps that could be taken to decrease healthcare costs based on our description of these five utilization groups. These suggestions are by no means definitive or comprehensive, as there is still much to be learned regarding different high-cost utilization groups. For starters, we do not know whether patients in a given cluster 1 year remain in the same utilization cluster the following year. In addition, high-cost patients in a different payor group may form different clusters of utilization groups.58 There were some conditions that were prevalent in two or more utilization groups, such as renal disease, heart failure, and procedure/device complications. What drives different patterns of utilization even among patients with the same disease? Looking at combinations of comorbidities, as well as disease severity, may help answer this question. For those patients with frequent admissions, it would be interesting to know what their actual inpatient needs are and whether a scaled-down version of inpatient care (whether through observation services or specific outpatient procedure) could decrease their admissions. We also have limited understanding regarding the drivers of cost in the mixed utilization group. Further understanding of length of stay in a single admission, diagnostic tests, and non-OR procedures conducted in this group might further clarify their drivers of cost.
Table 4.
Suggested Steps Toward Reducing Costs in Each Utilization Cluster
| Ambulatory | Surgical | Critically Ill | Frequent Utilization | Mixed Utilization | |
|---|---|---|---|---|---|
| Type of Utilization | Purely outpatient utilization, with high rates of chemo- and/or radiation therapy | Admitted for surgical procedures | Utilization of intensive care services | Frequent ED and hospital visits | Minimal annual utilization of hospital/ED resources |
| Suggested Steps | Implementation of tools that allow patients and providers to weigh treatment options based on cost vs. marginal benefit | Promote price transparency and marketplace competition for devices/surgical parts | Incentives to reduce delays from ICU to hospital floor transfers | Outpatient-based care coordination strategies targeting disease control and psychiatric services | Further research needed |
| Encourage price transparency and market place competition for expensive drugs | Transparent reporting of surgical costs, resource use, and complications | Appropriate initiation of palliative care discussions | |||
| Identify surgical risk and avoid high-risk surgeries | |||||
| Prevent post-op delirium | |||||
| Who Should be Implementing | Providers | Payors, government | Payors | Care coordinators, mental health specialists | Researchers |
| Government, payors | Providers, payors | Providers | |||
| Researchers, providers | |||||
| Providers |
A major strength of this study is that in using the QRUR report we were able to identify patients who received care almost exclusively at our institution. This allowed us to harness EMR and hospital accounting data to identify the entire spectrum of resource utilization among high-cost patients as well as compare clinical diagnoses among clusters. Also, by using cost data from the hospital cost accounting system, we were able to capture costs more accurately than we would have using Medicare reimbursement rates, which do not necessarily cover the cost of care. Our study population included an academic medical center and eight community hospitals, as well as regional outpatient facilities across Northeast Ohio. The fact that our distribution of costs was comparable to reported Medicare costs suggests that our population was nationally representative.5 , 59Finally, because our physicians are employed by the health system, we were able to capture physician as well as hospital costs.
There are a number of limitations to our study. Our study population represents a group whose care is more coordinated than usual—all patients had insurance, received primary care services at least once in the year prior, and received care at a single institution with an integrated electronic medical record. We included only Medicare Fee-for-service patients; therefore, conditions related to trauma or obstetric complications are likely underrepresented. Hospitalizations due to alcohol and substance abuse are also underrepresented because the 2012 QRUR excludes these primary diagnoses. Hot-spotters may be more prevalent among this group. Although substance abuse and mental health disorders are common,60 they are rarely reported as the primary cause of hospitalization. Based on available HCUP data, about 0.005 % of admissions are likely attributable to a primary diagnosis of alcohol abuse.61
Another limitation is that we did not include costs for medications, other medical products (e.g., durable medical equipment), and post-acute care and hospice, which are all known drivers of cost.49 , 62 , 63 In our study, 62 patients (4 %) were admitted to a CCHS post-acute care facility. These post-acute care costs were counted as part of their inpatient costs. Finally, 15 percent of our population had some costs covered by a secondary payer. Although we included these costs when they occurred within our system, services paid for by a secondary payer at a non-Cleveland Clinic institution would not have been identified.
Conclusion
Our findings offer a framework for understanding and approaching high-cost users of healthcare. In a representative sample of Medicare Fee for Service patients, high-cost patients had diverse utilization patterns, and most are not admittedly frequently. Outpatient-based care coordination may decrease costs for an important subset of high-cost patients, but a more comprehensive approach that addresses cancer treatment and surgery, and that emphasizes the judicious use of critical care services, may have a more meaningful impact on overall healthcare spending.
Acknowledgments
Contributors
We are sincerely grateful to David Acciarri, Justin Fink, Kathryn Martinez, Parth Parikh, and Aditi Patel for their indispensable help with key components of data collection, gathering, and analysis.
Compliance with Ethical Standards
Funders
This study was conducted without funding.
Prior Presentations
Presented at the 38th Annual Society of General Internal Medicine National Meeting, Toronto, Canada, April 22, 2015.
Conflicts of Interest
There are no conflicts of interest to disclose.
References
- 1.Birnbaum H. A National Profile of Catastrophic Illness (NCHSR Research Summary Series). NCHSR Office of Scientific and Technical Information.
- 2.Congressional Budget Office USC. Catastrophic Medical Expenses: Patterns in the Non-Elderly, Non-Poor Population. December 1982.
- 3.Riley G, Lubitz J, Prihoda R, Stevenson MA. Changes in distribution of Medicare expenditures among aged enrollees, 1969-82. Health Care Financ Rev. 1986;7(3):53–63. [PMC free article] [PubMed] [Google Scholar]
- 4.Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff Proj Hope. 2001;20(2):9–18. doi: 10.1377/hlthaff.20.2.9. [DOI] [PubMed] [Google Scholar]
- 5.Congressional Budget Office. High-Cost Medicare Beneficiaries. May 2005. http://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/63xx/doc6332/05-03-medispending.pdf. Accessed June 2, 2016.
- 6.Conwell L, Cohen J. Statistical Brief #73: Characteristics of Persons with High Medical Expenditures in the US Civilian Noninstitutionalized Population, 2002. March 2005.
- 7.Chronic Care: Making the Case for Ongoing Care. RWJF. http://www.rwjf.org/en/research-publications/find-rwjf-research/2010/01/chronic-care.html. Accessed June 2, 2016.
- 8.Gawande A. The Hot Spotters. New Yorker. January 2011. http://www.newyorker.com/reporting/2011/01/24/110124fa_fact_gawande. Accessed June 2, 2016.
- 9.Hasselman D. Super-Utilizer Summit. October 2013. http://www.rwjf.org/en/library/research/2013/10/super-utilizer-summit.html. Accessed June 2, 2016.
- 10.Emeche U. Is a strategy focused on super-utilizers equal to the task of health care system transformation? Yes. Ann Fam Med. 2015;13(1):6–7. doi: 10.1370/afm.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Care Coordination, Quality Improvement. http://www.ahrq.gov/research/findings/evidence-based-reports/caregaptp.html. Accessed June 2, 2016.
- 12.Schultz EM, Pineda N, Lonhart J, Davies SM, McDonald KM. A systematic review of the care coordination measurement landscape. BMC Health Serv Res. 2013;13(1):119. doi: 10.1186/1472-6963-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonald KM, Sundaram V, Bravata DM, et al. Definitions of Care Coordination and Related Terms. June 2007. http://www.ncbi.nlm.nih.gov/books/NBK44012/. Accessed June 2, 2016.
- 14.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA J Am Med Assoc. 2009;301(6):603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 15.Williams BC. Limited effects of care management for high utilizers on total healthcare costs. Am J Manag Care. 2015;21(4):e244–e246. [PubMed] [Google Scholar]
- 16.Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA J Am Med Assoc. 2013;309(24):2572–2578. doi: 10.1001/jama.2013.7103. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen OK, Tang N, Hillman JM, Gonzales R. What’s cost got to do with it? Association between hospital costs and frequency of admissions among “high users” of hospital care. J Hosp Med Off Publ Soc Hosp Med. 2013;8(12):665–671. doi: 10.1002/jhm.2096. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare Medicaid Services. 2012-QRUR. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/2012-QRUR.html. Accessed June 2, 2016.
- 19.Cohen S. Statistical Brief #392: The Concentration and Persistence in the Level of Health Expenditures over Time: Estimates for the US Population, 2009-2010. November 2012.
- 20.Healthcare Cost and Utilization Project (HCUP). HCUP Tools and Software. May 2014. www.hcup-us.ahrq.gov/tools_software.jsp. Accessed June 2, 2016.
- 21.HCUP Procedure Classes. Healthcare Cost and Utilization Project (HCUP). March 2014. www.hcup-us.ahrq.gov/toolssoftware/procedure/procedure.jsp. Accessed June 2, 2016.
- 22.Olin GL, Rhoades JA. Statistical Brief #80: THe Five Most Costly Medical Conditions, 1997 and 2002: Estimates for the US Civilian Noninstitutionalized Population. May 2005.
- 23.Friedman B, Henk R, Wier L. Statistical Brief #97: Most expensive hospitalizations, 2008. October 2010. [PubMed]
- 24.Torio CM, Andrews RM. Statistical Brief #160: Healthcare Cost and Utilization Project (HCUP). National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. August 2013. [PubMed]
- 25.Milligan GW, Cooper MC. A study of standardization of variables in cluster analysis. J Classif. 1988;5(2):181–204. doi: 10.1007/BF01897163. [DOI] [Google Scholar]
- 26.Clatworthy J, Buick D, Hankins M, Weinman J, Horne R. The use and reporting of cluster analysis in health psychology: A review. Br J Health Psychol. 2005;10(3):329–358. doi: 10.1348/135910705X25697. [DOI] [PubMed] [Google Scholar]
- 27.Kaufman L, Rousseeuw PJ. Finding Groups in Data: An Introduction to Cluster Analysis. 1st ed. Wiley-Interscience; 2005.
- 28.Jain AK. Data clustering: 50 years beyond K-means. Pattern Recognit Lett. 2010;31(8):651–666. doi: 10.1016/j.patrec.2009.09.011. [DOI] [Google Scholar]
- 29.Hennig C, Liao T. Comparing latent class and dissimilarity based clustering for mixed type variables with application to social stratification. Research report no. 308. 2010.
- 30.Ward JHJ. Hierarchical grouping to optimize an objective function. J Am Stat Assoc. 1968;58:236–244. doi: 10.1080/01621459.1963.10500845. [DOI] [Google Scholar]
- 31.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48(1):1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 32.Byrne M, Murphy AW, Plunkett PK, McGee HM, Murray A, Bury G. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med. 2003;41(3):309–318. doi: 10.1067/mem.2003.68. [DOI] [PubMed] [Google Scholar]
- 33.Woo BKP, Golshan S, Allen EC, Daly JW, Jeste DV, Sewell DD. Factors associated with frequent admissions to an acute geriatric psychiatric inpatient unit. J Geriatr Psychiatry Neurol. 2006;19(4):226–230. doi: 10.1177/0891988706292754. [DOI] [PubMed] [Google Scholar]
- 34.Schrag D, Xu F, Hanger M, Elkin E, Bickell NA, Bach PB. Fragmentation of care for frequently hospitalized urban residents. Med Care. 2006;44(6):560–567. doi: 10.1097/01.mlr.0000215811.68308.ae. [DOI] [PubMed] [Google Scholar]
- 35.Longman JM, Rolfe MI, Passey MD, et al. Frequent hospital admission of older people with chronic disease: a cross-sectional survey with telephone follow-up and data linkage. BMC Health Serv Res. 2012;12(1):373. doi: 10.1186/1472-6963-12-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robbins JM, Webb DA. Hospital admission rates for a racially diverse low-income cohort of patients with diabetes: the Urban Diabetes Study. Am J Public Health. 2006;96(7):1260–1264. doi: 10.2105/AJPH.2004.059600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Houston-Yu P, Rana SR, Beyer B, Castro O. Frequent and prolonged hospitalizations: a risk factor for early mortality in sickle cell disease patients. Am J Hematol. 2003;72(3):201–203. doi: 10.1002/ajh.10305. [DOI] [PubMed] [Google Scholar]
- 38.Schroeder SA, Showstack JA, Roberts HE. Frequency and clinical description of high-cost patients in 17 acute-care hospitals. N Engl J Med. 1979;300(23):1306–1309. doi: 10.1056/NEJM197906073002304. [DOI] [PubMed] [Google Scholar]
- 39.Cullen DJ, Ferrara LC, Briggs BA, Walker PF, Gilbert J. Survival, hospitalization charges and follow-up results in critically ill patients. N Engl J Med. 1976;294(18):982–987. doi: 10.1056/NEJM197604292941805. [DOI] [PubMed] [Google Scholar]
- 40.Lubitz J, Prihoda R. The use and costs of Medicare services in the last 2 years of life. Health Care Financ Rev. 1984;5(3):117–131. [PMC free article] [PubMed] [Google Scholar]
- 41.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27(17):2758–2765. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 42.Oncology BAS of C. The State of Cancer Care in America, 2014: A Report by the American Society of Clinical Oncology. J Oncol Pract. 2014; JOP.2014.001386. [DOI] [PubMed]
- 43.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology Statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23):2563–2577. doi: 10.1200/JCO.2015.61.6706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weiss AJ, Elixhauser A, Andrews RM. Characteristics of Operating Room Procedures in US Hospitals, 2011: Statistical Brief #170. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Health Care Policy and Research (US); 2006. [PubMed]
- 46.Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most Frequent Operating Room Procedures Performed in US Hospitals, 2003–2012: Statistical Brief #186. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Health Care Policy and Research (US); 2006. [PubMed]
- 47.Integrated Healthcare Association. Orthopedics data compendium: use, cost, and market structure for total joint replacement. August 2006.
- 48.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff (Millwood) 2011;30(11):2107–2115. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366(12):1075–1077. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Government Accountability Office. Medicare: lack of price transparency may hamper hospitals’ ability to be prudent purchasers of implantable medical devices. January 2012.
- 51.Rosenthal E. In Need of a New Hip, but Priced Out of the US. The New York Times. http://www.nytimes.com/2013/08/04/health/for-medical-tourists-simple-math.html. Published August 3, 2013.
- 52.Bosco JA, Alvarado CM, Slover JD, Iorio R, Hutzler LH. Decreasing total joint implant costs and physician specific cost variation through negotiation. J Arthroplasty. 2014;29(4):678–680. doi: 10.1016/j.arth.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 53.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38(1):65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 54.Gooch RA, Kahn JM. Icu bed supply, utilization, and health care spending: An example of demand elasticity. JAMA. 2014;311(6):567–568. doi: 10.1001/jama.2013.283800. [DOI] [PubMed] [Google Scholar]
- 55.Johnson DW, Schmidt UH, Bittner EA, Christensen B, Levi R, Pino RM. Delay of transfer from the intensive care unit: a prospective observational study of incidence, causes, and financial impact. Crit Care. 2013;17(4):R128. doi: 10.1186/cc12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garland A, Connors AF. Optimal timing of transfer out of the intensive care unit. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2013;22(5):390–397. doi: 10.4037/ajcc2013973. [DOI] [PubMed] [Google Scholar]
- 57.Smith S, Brick A, O’Hara S, Normand C. Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat Med. 2014;28(2):130–150. doi: 10.1177/0269216313493466. [DOI] [PubMed] [Google Scholar]
- 58.Powers BW, Chaguturu SK. ACOs and high-cost patients. N Engl J Med. 2016;374(3):203–205. doi: 10.1056/NEJMp1511131. [DOI] [PubMed] [Google Scholar]
- 59.Kaiser Family Foundation. Kaiser Family Foundation analysis of the CMS Medicare Current Beneficiary Survey Cost and Use File, 2009. Distrib Tradit Medicare Benef Medicare Spend 2009. 2013; http://kff.org/health-costs/slide/distribution-of-traditional-medicare-beneficiaries-and-medicare-spending-2009/. Accessed June 2, 2016.
- 60.Heslin K, Elixhauser A, Steiner C. Hospitalizations Involving Mental and Substance Use Disorders Among Adults, 2012. HCUP Statistical Brief #191. June 2015. [PubMed]
- 61.Russo CA, Elixhauser, A. Hospitalizations for Alcohol Abuse Disorders, 2003. HCUP Statistical Brief #4. May 2006. [PubMed]
- 62.Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group. National healthcare expenditures data. 2012. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/tables.pdf. Accessed June 2, 2016.
- 63.Riley GF, Lubitz JD. Long-term trends in medicare payments in the last year of life. Health Serv Res. 2010;45(2):565–576. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]