Abstract
Background
Sarcopenia describes a loss of muscle mass and resultant decrease in strength, mobility and function that can be quantified by CT. We hypothesized that sarcopenia and related frailty characteristics are related to discharge disposition after blunt traumatic injury in the elderly.
Methods
We reviewed charts of 252 elderly blunt trauma patients who underwent abdominal CT prior to hospital admission. Data for thirteen frailty characteristics were abstracted. Sarcopenia was measured by obtaining skeletal muscle cross sectional area (CSA) from each patient’s psoas major muscle using Slice-O-Matic® software. Dispositions were grouped as dependent and independent based on discharge location. Chi-square, Fisher’s exact, and logistic regression were used to determine factors associated with discharge dependence.
Results
Mean age 76 years, 49% male, median ISS 9.0 (IQR=8.0–17.0). Discharge destination was independent in 61.5%, dependent in 29% and 9.5% of patients died. Each 1 cm2 increase in psoas muscle CSA was associated with a 20% decrease in dependent living (p<0.0001). Gender, weakness, hospital complication, and cognitive impairment were also associated with disposition; ISS was not (p=0.4754).
Conclusions
Lower psoas major muscle CSA is related to discharge destination in elderly trauma patients and can be obtained from the admission CT. Lower psoas muscle CSA is related to loss of independence upon discharge in the elderly. The early availability of this variable during the hospitalization of elderly trauma patients may aid in discharge planning and the transition to dependent living.
Keywords: sarcopenia, frailty, trauma
Introduction
The term frailty is used widely throughout geriatric literature to describe the declining elderly condition and identify those at risk for adverse health outcomes. [1] Sarcopenia, a frailty risk factor of particular interest, is the reduction of lean muscle associated with aging. [1] Sarcopenia is often classified as a part of the geriatric syndrome consisting of multiple system impairments and increased vulnerability to stress. [2,3]
Age related changes in muscle include alterations in mass, composition and contractility. [4] With age, the loss of motor units (fast>slow) leads to decreased muscle cross sectional area (CSA). [4] In addition to decreased mass, increased muscle fat infiltration is associated with diminished muscle strength. [5,6] These changes describe sarcopenia.
The gold-standard imaging modality for measuring sarcopenia is CT. [7,8] Abdominal CT images at specific lumbar vertebral levels have been shown to correlate well with total body fat and muscle content. [9] By measuring the CSA of specific muscles at a standardized level, we are able to determine an individual’s relative degree of sarcopenia.
Sarcopenia can be compared to osteopenia. Osteopenia may predict risk of osteoporotic fracture with subsequent disability. Similarly, sarcopenia may predict risk of weakness and disability. [10,11] Osteoporosis can be diagnosed by measuring bone mineral density. Sarcopenia, unlike osteoporosis, should be defined through measurement of muscle mass in addition to other frailty or functional measures. [10] Measurement of frailty risk factors provides additional insight into the elderly syndrome of which sarcopenia is an important factor. [10]
Outcomes in the elderly population are poorer with higher mortality rates when compared to other age groups. [12,13] Age does not independently explain this difference. [14] We set out to determine if sarcopenia and related frailty characteristics, that can be measured early during the care of an injured geriatric patient, are related to discharge disposition after blunt traumatic injury in the elderly.
Materials and Methods
Subjects and Study Design
This is a retrospective chart review aimed at identifying risk factors in elderly blunt trauma victims that can affect discharge disposition. To obtain this data we reviewed the charts of 252 patients admitted to a Level I trauma center, Froedtert Hospital (FH) in Milwaukee, WI, from January 1, 2008 to April 30, 2011. Patients included in this review had been evaluated by and admitted to the trauma service and underwent an abdominal CT scan as part of their initial hospital evaluation. Elderly was defined as 65 years of age and older. We excluded patients who sustained TBI and SCI due to the devastating effects of neurologic injury on recovery and post-injury functioning. While underlying frailty and sarcopenia may influence discharge disposition in these populations, it would be difficult to determine if outcomes were related to frailty or the neurologic injury itself. The effect of frailty on neurologically injured patients should be studied separately.
Frailty Risk Factors
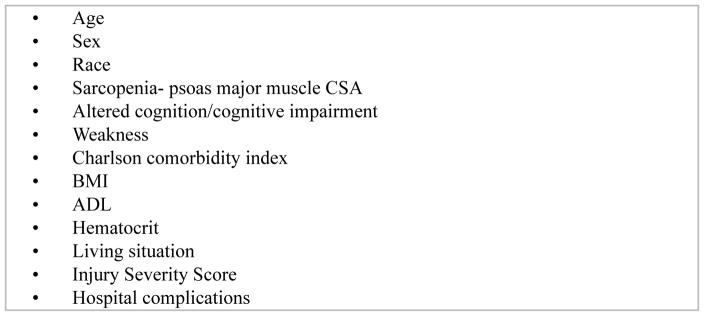
Data for thirteen frailty risk factors were abstracted from medical records and the FH trauma registry (Figure 1). Risk factors were chosen by senior authors, based loosely on the domains of frailty defined by Robison et al, [15] but limited by our retrospective approach and the size of our study population. Robinson et al proposed that frailty characteristics related to the need for post-operative institutionalization include: older age, increased Charlson score, lower hematocrit, functional dependence, prolonged up-and-go test, albumin, low Mini-Cog score and recent fall. [15] Based on these findings we observed age/sex/race, weakness, sarcopenia, altered cognition, Charlson score, BMI, ADL’s, hematocrit and living situation as measures of pre-existing frailty. Albumin was not routinely available in our subject’s records. We added Injury Severity Score (ISS) and hospital complications to broaden the scope of our focus and provide information regarding type of injury and how the hospital course may affect outcomes.
Figure 1.
Frailty risk factors
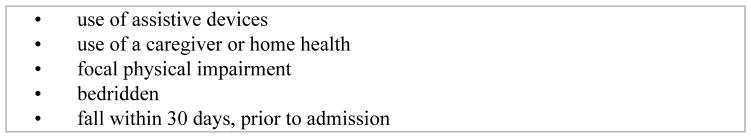
Through chart review we identified patients who had less than full strength by the presence of specific pre-injury features (Figure 2). Patients with one or more indication of weakness were grouped together in the weak group. Patients without indication of pre-existing weakness comprised the non-weak group.
Figure 2.
Indicators of weakness
In a similar fashion, we used chart review to identify patients with pre-existing cognitive impairment or mental illness (Figure 3). Patients with pre-injury altered cognition were grouped together. All patients without documented cognitive impairment or mental illness were grouped separately into the normal cognition group.
Figure 3.
Altered cognition
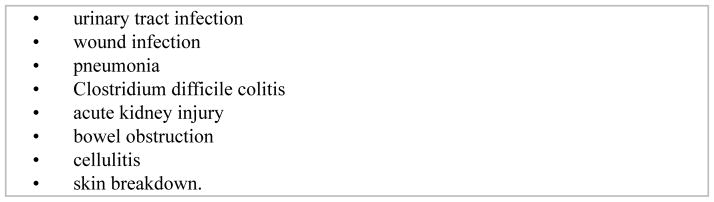
Hospital complications were determined from chart review. Complications that were identified in our database are listed in Figure 4. Patients who suffered complications in addition to their primary injury were grouped together and patients without complications were grouped separately.
Figure 4.
Hospital complications
Activities of Daily Living (ADL’s) were observed as an additional measure of pre-existing disability. Record of ability to perform ADL’s was gathered from patient medical records. Those patients who were independent with ADL’s were grouped into one category and those requiring assistance were grouped separately.
Living Situation provides additional insight into pre-injury functional status and ability to discharge home post-injury. We group patients into two categories. Those living at home, alone or with others were grouped together and those living in a rehabilitation facility, assisted living, nursing home or residential facility pre-injury were grouped separately.
Body Composition Methodology
In order to quantify sarcopenia we used CT to measure cross-sectional area of the bilateral psoas major muscle at the level of the L4–L5 intervertebral disk space. CT is used to determine muscle area via Slice-O-Matic software. [16] Using the Slice-O-Matic software we traced the boundary between skeletal muscle and extra-muscular fat. The Hounsfield units (HU) were set to gate out intramuscular and inter-muscular fat with parameters between 0–140 HU. [16]
HU measurements of skeletal muscle reflect density, with lower HU indicating lower density and greater fat infiltration. [3,16] Patients with greater fat infiltration or lower overall muscle mass have a lower CSA. Patient CT scans, measured using this technique, were compared to determine if pre-existing differences in CSA alter outcomes after traumatic injury. We measured the baseline CSA only, obtained from CT scans completed during initial ED evaluation, soon after traumatic injury. This measure reflects the baseline muscle mass, before muscle composition has been altered by injury or hospitalization.
The youngest subjects in our study were 65 years old. We analyzed groups of elderly patients at various age increments to determine if continued advancement in age affected the degree of sarcopenia, presence of frailty risk factors and overall outcomes.
Outcomes
Discharge destinations were defined as death, skilled-nursing facility (SNF), nursing home (NH), rehabilitation, home and home-health. The latter 3 were grouped as independent outcomes in order to look at variance by rank and obtain binary outcomes. Patients with dependent outcomes require a greater level of assistance or care after hospital discharge. Those patients discharged to home, home health or rehab have independent outcomes. Patients with independent outcomes require less care or assistance. Groups were determined using pre-existing categories in FH database. While patients in SNF and NH require essentially the same amount of care, they are separated because Medicare regulates only SNF’s. Chi-square, Fisher’s exact, and logistic regression were used to determine factors associated with discharge dependence.
Statistics
Statistical analysis was performed using SAS 9.2 (SAS Institute, Cary NC). The association between patient discharge disposition (independent living vs. dependent living) and categorical variables were analyzed using Chi-square and Fisher’s exact tests. The Wilcoxon rank-sum test was used to compare the distribution of the continuous variable (psoas muscle CSA) between the disposition categories. Logistic regression analysis was used to analyze associations between covariates and discharge disposition, controlling for effects of other covariates in the model. The forward stepwise variable selection procedure was used to identify a parsimonious model.
Results
Mean age was 76 years, the population was 49% male, and the median ISS was 9.0 (IQR=8.0–17.0). Patients were discharged to the following destinations: nursing home 5%, SNF 18%, Rehab 24%, home with home health 7%, and home 35%.
The association of discharge destination with covariates (race, age, gender, Charlson score, BMI, ADL, hematocrit, cognitive impairment, weakness, living situation, hospital complications and psoas muscle cross sectional area) was analyzed using the Chi-square and student’s t-test. We grouped patients who died into the dependent outcome category. Groups labeled missing did not have the specified variable accessible from the medical record.
The results of our data collection are listed in Table 1. Several of the measured variables were statistically significant including race, age, Charlson score, BMI, ADL, hematocrit, cognition, weakness, living situation, hospital complications and psoas CSA.
Table 1.
Summary of statistics by discharge destination
| Discharge destination | |||
|---|---|---|---|
| Variables | Dead & dependent N=97(%) | Independent N=155(%) | P Value |
| Race | 0.031 C | ||
| Caucasian | 7 (21.9) | 25 (78.1) | |
| Non-Caucasian | 89 (41.8) | 124 (58.2) | |
| Missing | 1 | 6 | |
| Age | <.001 C | ||
| 64–74 | 18 (16.5) | 91 (83.5) | |
| 75–84 | 47 (51.1) | 45 (48.9) | |
| 85 + | 32 (62.7) | 19 (37.3) | |
| Missing | 0 | 0 | |
| Gender | 0.698 C | ||
| Female | 47 (37.3) | 79 (62.7) | |
| Male | 50 (39.7) | 76 (60.3) | |
| Missing | 0 | 0 | |
| Charlson score | 0.006 C | ||
| <3 | 4 (14.3) | 24 (85.7) | |
| >=3 | 87 (40.8) | 126 (59.2) | |
| Missing | 6 | 5 | |
| BMI | 0.0486 C | ||
| <18.5 | 8 (66.7) | 4 (33.3) | |
| 18.5–24.9 | 32 (47.1) | 36 (52.9) | |
| 25–29.9 | 29 (37.7) | 48 (62.3) | |
| >=30 | 23 (30.7) | 52 (69.3) | |
| Missing | 5 | 15 | |
| ADL | <.001 C | ||
| No disability | 26 (20.2) | 103 (79.8) | |
| Disability | 44 (55.7) | 35 (44.3) | |
| MS | 27 (61.4) | 17 (38.6) | |
| Missing | 0 | 0 | |
| Hematocrit | <.001 C | ||
| <35 | 63 (49.2) | 65 (50.8) | |
| >35 | 33 (28.0) | 85 (72.0) | |
| Missing | 1 | 5 | |
| Cognitive impairment | 0.002 C | ||
| Absence | 71 (33.5) | 141 (66.5) | |
| Presence | 21 (61.8) | 13 (38.2) | |
| Discharge destination | |||
|---|---|---|---|
| Variables | Dead & dependent N=97(%) | Independent N=155(%) | P Value |
| Missing | 5 | 1 | |
| Weakness | <.001 C | ||
| 1 | 20 (20.2) | 79 (79.8) | |
| 2–6 | 53 (46.1) | 62 (53.9) | |
| MS | 24 (63.2) | 14 (36.8) | |
| Weakness | <.001 C | ||
| 1 | 20 (20.2) | 79 (79.8) | |
| 2–6 | 53 (46.1) | 62 (53.9) | |
| MS | 24 (63.2) | 14 (36.8) | |
| Missing | 0 | 0 | |
| Living situation | <.001 C | ||
| 0–2 | 57 (29.1) | 139 (70.9) | |
| 3–6 | 12 (80.0) | 3 (20.0) | |
| MS | 28 (68.3) | 13 (31.7) | |
| Missing | 0 | 0 | |
| Hospital complications | <.001 C | ||
| MS | 17 (68.0) | 8 (32.0) | |
| No | 48 (26.5) | 133 (73.5) | |
| Yes | 32 (69.6) | 14 (30.4) | |
| Missing | 0 | 0 | |
| Psoas muscle CSA | <.001 T | ||
| N | 95 | 155 | |
| Mean ± SE | 18.0 ± 0.6 | 22.9 ± 0.6 | |
| Missing | 2 | 0 | |
| ISS | 0.164 W | ||
| Median (q25 – q75) | 9.0 (9.0–17.0) | 9.0 (5.0–17.0) | |
| Missing | 0 | 0 | |
t-test;
Chi-square test;
Wilcoxon rank-sum test
The effect of ISS was not significant (p=0.164). Twenty-nine percent of patients with ISS less than 8, 39.6% of patients with ISS 9–15 and 45.5% of patients with ISS greater than 15 went to dependent living post-injury.
For psoas muscle CSA we compared the means between dependent and independent outcome destinations and the results show that the mean difference in psoas CSA is statistically significant (p <0.001). Mean psoas muscle CSA was 1800 mm2 in the dependent group and 2290 mm2 in the independent group, demonstrating an increased risk for dependence at the time of hospital discharge with lower mean CSA.
After our initial data analysis (Table 1) we performed a multivariate regression (Table 2, 3). Variables listed in Table 2 were significantly associated with disposition in the final parsimonious model. Compared with patients aged 65 to 74, patients 75 years of age or older were more than 3 (3.71–4.19) times more likely to stay in dependent living. Controlling for age and other significant factors in the final model, a 1 cm2 increase in psoas muscle CSA was associated with a 20% decrease in the odds of dependent living (p<0.0001). The other variables significantly associated with the disposition outcome were gender (male vs. female), pre-injury weakness (2–6 vs. 1; missing group vs. 1), hospital complication (yes vs. no; missing group vs. no), and altered cognition (presence vs. absence) (Table 3).
Table 2.
Variables significantly associated with disposition
| Variables | P value |
|---|---|
| Sex | 0.0009 |
| Age | 0.0025 |
| Psoas CSA | <.0001 |
| Weakness | 0.0005 |
| Hospital complication | 0.0001 |
| Cognitive impairment | 0.0325 |
Table 3.
Final Model: Multivariate Analysis of significant variables
| Odds Ratio Estimates | ||||
|---|---|---|---|---|
| Variables | Point Estimate | 95% Wald Confidence Limits | P value | |
| Sex (M vs F) | 4.516 | 1.853 | 11.003 | 0.0009 |
| Age (75–84 vs 65–74) | 3.714 | 1.631 | 8.459 | 0.0018 |
| Age (85 + vs 65–74) | 4.191 | 1.588 | 11.062 | 0.0038 |
| Psoas muscle CSA | 0.836 | 0.772 | 0.905 | <.0001 |
| Weakness (2–6 vs 1) | 3.184 | 1.426 | 7.107 | 0.0047 |
| Weakness (MS vs 1) | 8.900 | 2.835 | 27.943 | 0.0002 |
| Hospital complication (MS vs no) | 5.566 | 1.604 | 19.322 | 0.0069 |
| Hospital complication (yes vs no) | 5.562 | 2.217 | 13.949 | 0.0003 |
| Cognitive impairment (presence vs absence) | 2.926 | 1.094 | 7.829 | 0.0325 |
Discussion
The primary cause of sarcopenia is inactivity. [17] Physical therapy and nutrition have a positive influence on the frailty syndrome.[18] Resistance training slows the onset of sarcopenia. Recent data emphasizes the importance of protein intake and the possibility that aerobic exercise may play a role in preserving skeletal muscle mass. [19] Muscle is built through protein synthesis, requiring a supply of amino acids from dietary intake. [19, 20] Studies show that complete protein intake is associated with higher skeletal muscle mass. [21,22] Emphasizing dietary protein intake and exercise may alter the number of patients who endure traumatic injury and the outcomes after elderly trauma. If sarcopenia and frailty are not prevented they may alter a patients ability to recover after trauma. Even when frailty is not prevented, value lies in the identification of its presence.
The idea that pre-surgery rehabilitation optimizes outcomes post-operatively has become increasingly acknowledged. Prior to elective surgery, patients can optimize diet and exercise to help facilitate better outcomes after surgery. The presence of frailty pre-operatively is associated with post-operative complications and longer hospital stays. [23] For this reason, frail and sarcopenic patients are poor candidates for surgery. By definition, frail individuals have a decreased physiologic reserve and less ability to cope with the physical stress associated with surgery. [2,3,4] In trauma, due to the emergent nature of surgical intervention, we are unable to encourage pre-surgery rehabilitation. However, value lies in the identification of frailty to aid in the prediction of prognosis and discharge disposition.
Early and appropriate discharge planning has become increasingly important to minimize length of stay, decrease hospital re-admissions and provide patients with the most appropriate care after hospital discharge. Post-discharge site determination is a multi-disciplinary decision, requiring consideration of medical, functional and social aspects of a patient’s illness. [24] The patient, family, physician, social worker, case manager, nurse, therapists, and insurance agency collaborate to optimize the discharge process. [24] Early determination of discharge disposition allows time for planning, facility acceptance, consent and overall increased understanding by the patient and family.
Measures proposed to be helpful in planning long-term care include; Activities of daily living (ADL), Instrumental activities of daily living (IADL), cognition, depression and mobility. [24] We chose to observe presence of pre-existing weakness, altered cognition and sarcopenia in a retrospective manner. Sarcopenia can be measured irrespective of a patient’s condition by implementing measurements from CT scans. We believe that this feature makes CT especially valuable for the early prediction of disposition for the purpose of discharge planning in the trauma population. An alternative measure of sarcopenia is the timed-get-up-and-go test (TGUG), a measure of muscle strength in which the subject completes a series of functionally important tasks scored on a standardized scale. [23] This test is not well suited for the trauma population due to decreased mobility and post-injury associated pain. Since prevention is not possible once injury occurs, benefits lie in early identification of at-risk patients, allowing for more tailored care.
More research is needed in order to validate a major change in practice. Making the proposed measurements requires the use of CT in all patients. Given the safety and cost implications related to CT imaging we do not believe that the routine use of imaging should be performed in trauma patients solely for the purpose of determining the presence of sarcopenia. However, obtaining measurements from CT imaging that is obtained for initial diagnostic purposes incurs little additional cost. Until further research, including collection of prospective data, has been completed, using alternative frailty markers (such as weakness and age) may serve as independent measures of frailty.
There are several limitations of this study, primarily related to the retrospective nature of the ascertainment of the covariates used in the analysis. For data points obtained directly from the patient medical records accuracy of our results is based largely on the accuracy of previous patient charting. In a prospective analysis, we would separate mental illness from cognitive impairment but due to our limited sample size, we chose to group these together as altered cognition. Finally, we included “missing” groups in order to maintain the integrity of out data analysis. Missing groups included patients for which all measured data points were not available. If one of the data point was unavailable for a given subject we analyzed that patient based on the data points we could access. Ideally, we would compare only patients who had data from all categories available but were unable to do so given limitations in the size of our database.
In conclusion, lower psoas major muscle CSA is related to discharge destination in elderly trauma patients and can be obtained from the admission CT. Lower CSA is related to loss of independence upon discharge in the elderly. The early availability of this variable during the hospitalization of elderly trauma patients may aid in discharge planning and the transition to dependent living. We recommend early identification of significant risk factors for frailty such as weakness, altered cognition, increasing age and male gender. Diligence should be taken to avoid hospital complications in all settings. Finally, we hope that with further research, objective measures of frailty (sarcopenia), from available imaging, will be used in the clinical setting to improve discharge planning and ultimately improve the care of elderly trauma patients.
Acknowledgments
Grant support: Funding for this project was supported in part by Centers for Disease Control and Prevention Grant R49/CE001175 and in part by the National Institute on Aging Training Grant T35 AG029793-05. Imaging Software was funded through the MCW Research Affairs Committee Grant.
Footnotes
There are no real or potential conflicts of interest to disclose.
Contributor Information
Berry Fairchild, Medical College of Wisconsin Dept. of Surgery, Division of Trauma and Critical Care 9200 W. Wisconsin Ave, Suite 3510, Milwaukee WI, 53226.
Travis P. Webb, Medical College of Wisconsin Dept. of Surgery, Division of Trauma and Critical Care 9200 W. Wisconsin Ave, Suite 3510, Milwaukee WI, 53226.
Qun Xiang, Medical College of Wisconsin, 9200 W. Wisconsin Ave, Milwaukee WI, 53226.
Sergey Tarima, Medical College of Wisconsin, 9200 W. Wisconsin Ave, Milwaukee WI, 53226.
Karen J. Brasel, Medical College of Wisconsin Dept. of Surgery, Division of Trauma and Critical Care 9200 W. Wisconsin Ave, Suite 3510, Milwaukee WI, 53226.
References
- 1.Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: An undiagnosed condition in older adults, current consensus definition, prevalence, etiology, and consequences. J Am Med Dir Assoc. 2011;12(4):249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cruz-Jentoft A, Landib F, Topinkova E, et al. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010;13:1–7. doi: 10.1097/MCO.0b013e328333c1c1. [DOI] [PubMed] [Google Scholar]
- 3.Goodpaster B, Carlson C, Visser M, et al. Attenuation of skeletal muscle and strength in the elderly: The Health ABC Study. J Appl Physiol. 2001;90(6):2157–2165. doi: 10.1152/jappl.2001.90.6.2157. [DOI] [PubMed] [Google Scholar]
- 4.Lang T, Streeper T, Cawthon P, et al. Sarcopenia: etiology, clinical consequences, intervention, and assessment. Osteoporosis Int. 2010;210(4):543–559. doi: 10.1007/s00198-009-1059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taaffe DR, Henwood TR, Nalls MA, et al. Alterations in muscle attenuation following detraining and retraining in resistance-trained older adults. Gerontology. 2009;55(2):217–223. doi: 10.1159/000182084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Visser M, Goodpaster B, Kritchevsky S, et al. Muscle Mass, Muscle Strength, and Muscle Fat Infiltration as Predictors of Incident Mobility Limitations in Well-Functioning Older Persons. J Gerontol. 2005;60(3):324–333. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 7.Prado C, Birdsell L, Baracos V. The emerging role of computerized tomography in assessing cancer cachexia. Current Opinion in Supportive and Palliative Care. 2009;3:269–275. doi: 10.1097/SPC.0b013e328331124a. [DOI] [PubMed] [Google Scholar]
- 8.Stevens-Simon C, Thureen P, Stamm E, et al. A comparison of four techniques for measuring central adiposity in postpartum adolescents. J Matern Fetal Med. 2001;10(3):209–213. doi: 10.1080/714052734. [DOI] [PubMed] [Google Scholar]
- 9.Mourtzakis M, Prado C, Lieffers J, et al. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006. doi: 10.1139/H08-075. [DOI] [PubMed] [Google Scholar]
- 10.Cooper C, Dere W, Evans W, et al. Frailty and Sarcopenia: definitions and outcome parameters. Osteoporosis Int. 2012;23:1839–1848. doi: 10.1007/s00198-012-1913-1. [DOI] [PubMed] [Google Scholar]
- 11.Studenski S. Evidence-Based Criteria for Sarcopenia with Clinically Important Weakness. Semin Arthritis Rheum. 2013;42:447–449. doi: 10.1016/j.semarthrit.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Broos P, D’Hoorel A, Vanderschot P, et al. Multiple trauma in elderly patients. Factors influencing outcome: importance of aggressive care. Injury. 1993;24:365–368. doi: 10.1016/0020-1383(93)90096-o. [DOI] [PubMed] [Google Scholar]
- 13.Hsia R, Wang E, Saynina O, et al. Factors Associated With Trauma Center Use for Elderly Patients With Trauma. Arch Surg. 2011;146:585–592. doi: 10.1001/archsurg.2010.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perdue P, Watts D, Kaufmann C, et al. Differences in Mortality between Elderly and Younger Adult Trauma Patients: Geriatric Status Increases Risk of Delayed Death. J Trauma. 1998;45:805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 15.Robinson T, Wallace J, Wu D, et al. Accumulated Frailty Characteristics Predict Postoperative Discharge Institutionalization in the Geriatric Patient. J Am Coll Surg. 2011;213:37–42. doi: 10.1016/j.jamcollsurg.2011.01.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lang T, Cauley J, Tylavsky F, et al. Computed Tomographic Measurements of Thigh Muscle Cross-Sectional Area and Attenuation Coefficient Predict Hip Fracture: The Health, Aging, and Body Composition Study. J Bone Miner Res. 2010;25:513–519. doi: 10.1359/jbmr.090807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morely J, et al. Sarcopenia in the Elderly. Family Practice. 2012;29:144–148. doi: 10.1093/fampra/cmr063. [DOI] [PubMed] [Google Scholar]
- 18.Ruiz M, Cefalu C, Reske T. Frailty syndrome in geriatric medicine. Am J Med Sci. 2012;5:395–398. doi: 10.1097/MAJ.0b013e318256c6aa. [DOI] [PubMed] [Google Scholar]
- 19.Koopman R. Dietary protein and exercise training in ageing. Proc Nutr Soc. 2011;70:104–113. doi: 10.1017/S0029665110003927. [DOI] [PubMed] [Google Scholar]
- 20.Nair KS. Muscle protein turnover: methodological issues and the effect of aging. J Gerontol A Biol Sci Med Sci. 1995;50:107–112. doi: 10.1093/gerona/50a.special_issue.107. [DOI] [PubMed] [Google Scholar]
- 21.Houston DK, Nicklas BJ, Ding J, et al. Dietary protein intake is associated with lean mass change in older, community- dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87:150–155. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- 22.Morris MS, Jacques PF. Total protein, animal protein and physical activity in relation to muscle mass in middle-aged and older Americans. British Journal of Nutrition. 2013;109:1294–1303. doi: 10.1017/S0007114512003133. [DOI] [PubMed] [Google Scholar]
- 23.Robinson T, Wu D, Pointer L, et al. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(4):544–550. doi: 10.1016/j.amjsurg.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kane RL. Finding the right level of post-hospital care: “We didn’t realize there was any other option for him”. JAMA. 2011;305(3):284–93. doi: 10.1001/jama.2010.2015. [DOI] [PubMed] [Google Scholar]