A study finds that medication histories obtained by the pharmacy technician in a busy emergency department were much more accurate than those obtained by nurses.
Keywords: pharmacy technician, medication history, emergency department
Abstract
Purpose:
To compare the medication history error rate of the emergency department (ED) pharmacy technician with that of nursing staff and to describe the workflow environment.
Methods:
Fifty medication histories performed by an ED nurse followed by the pharmacy technician were evaluated for discrepancies (RN-PT group). A separate 50 medication histories performed by the pharmacy technician and observed with necessary intervention by the ED pharmacist were evaluated for discrepancies (PT-RPh group). Discrepancies were totaled and categorized by type of error and therapeutic category of the medication. The workflow description was obtained by observation and staff interview.
Results:
A total of 474 medications in the RN-PT group and 521 in the PT-RPh group were evaluated. Nurses made at least one error in all 50 medication histories (100%), compared to 18 medication histories for the pharmacy technician (36%). In the RN-PT group, 408 medications had at least one error, corresponding to an accuracy rate of 14% for nurses. In the PT-RPh group, 30 medications had an error, corresponding to an accuracy rate of 94.4% for the pharmacy technician (P < 0.0001). The most common error made by nurses was a missing medication (n = 109), while the most common error for the pharmacy technician was a wrong medication frequency (n = 19). The most common drug class with documented errors for ED nurses was cardiovascular medications (n = 100), while the pharmacy technician made the most errors in gastrointestinal medications (n = 11).
Conclusion:
Medication histories obtained by the pharmacy technician were significantly more accurate than those obtained by nurses in the emergency department.
INTRODUCTION
The Joint Commission defines the process of medication reconciliation as the comparison of the medications a patient is currently taking (and should be taking) with newly ordered medications.1 The process consists of two phases in which a complete and accurate patient medication list must first be obtained, followed by a comparison (or reconciliation) of the obtained history to the list of medications that patients will either continue or discontinue during their stay in the hospital or as they move through the continuum of care.2 It is well established that the process of obtaining an accurate medication history and subsequent medication reconciliation is complex, with numerous opportunities to create discrepancies. These discrepancies may include omissions, duplications, discrepant doses or frequencies, and incorrect drugs or formulations.3,4
Obtaining an accurate medication list is particularly essential during patient transitions of care. The emergency department (ED) stands at a critical crossroads for obtaining an accurate medication list, as many patients who visit the ED may be admitted. At that point, an accurate medication history becomes crucial for maintaining continuity of care. In the demanding and often hectic ED environment, there are numerous barriers to obtaining an accurate medication history that continue to frustrate clinicians. Such barriers include patients who may be obtunded or who present with impaired memory, outdated information from patients or hospital records, patients’ use of multiple pharmacies, restrictive access to patient records, time constraints, and language barriers.5 As a result, a crucial role exists for skilled pharmacy personnel participating in the medication history process.
The American Society of Health-System Pharmacists supports the idea that every hospital pharmacy department should provide its ED with pharmacy services.6 While the role of a clinical pharmacist in the ED cannot be understated, it is the role of the pharmacy technician that has been evolving to encompass patient care activities, such as obtaining the medication history. Pharmacy technicians are in a unique position to fulfill this critical role, as they have a working knowledge of commonly prescribed medications at a significantly decreased personnel cost compared with other health care professionals, such as pharmacists or nurses.
The purpose of this study was to perform a descriptive analysis of the ED workflow for obtaining medication histories after the addition of a pharmacy technician to the staff and to compare the accuracy of the pharmacy technician to that of ED nursing staff and an ED clinical pharmacist. The primary outcome was the evaluation of the number and types of medication history discrepancies resolved by the pharmacy technician. Secondary outcomes included the classes of medications with an intervention and the time it took for various personnel to complete tasks associated with medication reconciliation when a patient presented to the ED.
PROGRAM DESCRIPTION
Rationale for the Program
Prior to placing a pharmacy technician in the ED, the documentation of patient medication histories was largely driven by ED nurses. The ED clinical pharmacist participated in obtaining some medication histories; however, the primary focus for the pharmacist was clinical evaluation and interventions. An interview of the nursing staff revealed that given the high patient turnover in the ED and the number of patients and tasks to which they are assigned, most nurses are not able to prioritize obtaining an accurate medication history due to time constraints. Moreover, nurses revealed that they had no time to utilize outside resources, such as contacting the patient’s outpatient pharmacy or speaking with primary care physician offices. As a result, many medication histories were inaccurate, incomplete, imported from the patient’s prior admission and therefore outdated, or simply not done. When the medication history was incomplete or inaccurate, the medical resident admitting the patient assumed responsibility for obtaining the medication history and completing the medication reconciliation. Interviews with the medical residents showed that they too were unable to efficiently prioritize obtaining an accurate medication history due to time constraints and other admission responsibilities. Therefore, inaccurate or only partially complete medication histories were frequently being used as the basis for physicians’ medication reconciliation.
Prior to implementing the pharmacy technician program, the ED clinical pharmacist conducted a study in which she performed a thorough medication history on 24 patients in the ED after a nurse had already documented the medication history as complete. Of the 24 documented medication histories, 22 (91.7%) had at least one error. Of a total of 261 medications, there were 116 errors (44.4%), the majority of which were either medication omissions or errors in documenting the medication dose. Therefore, it was evident that the current process of obtaining medication histories was inaccurate and unreliable, indicating a clear need for a process change.
Implementation
The ED pharmacy technician program was implemented in April 2015 as part of a pilot program across a large health system to optimize the medication history and reconciliation process. Prior to starting work in the ED, the pharmacy technician had been employed for approximately two years in the main inpatient pharmacy, where she did not perform medication reconciliation. The pharmacy technician is registered with the state of New Jersey but not nationally certified. Prior to employment at our facility, she worked as a pharmacy liaison for a different hospital for approximately one year, gathering and processing prescriptions from inpatients and delivering them before discharge. The technician received one week of training from the emergency medicine pharmacist before independently collecting and documenting medication histories. Throughout the course of this study, the pharmacy technician’s work hours shifted to coincide with hours of peak volume in the ED. The initial work hours were 8 a.m. to 4:30 p.m. but gradually transitioned to the current 1 p.m. to 9:30 p.m. schedule.
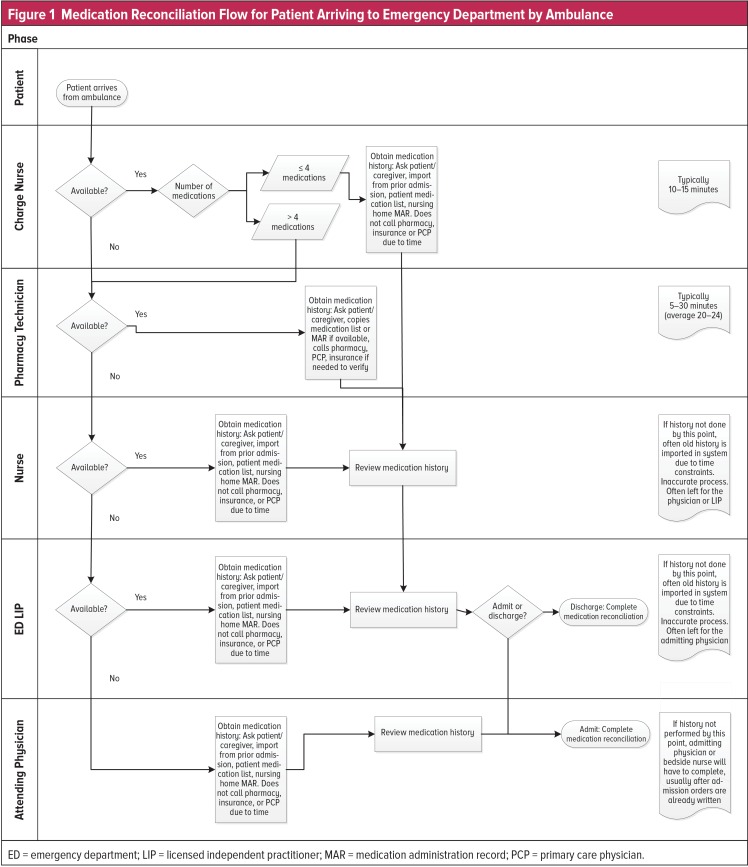
Job Description and Workflow
The workflow for a patient arriving at the ED by ambulance is depicted in Figure 1. After the patient is triaged and assigned a bed in the ED, the pharmacy technician initiates the medication history process, usually after the nurse has imported an outdated medication history from the patient’s past admission. This process consists of asking the patient or caregiver if they know which medications the patient is taking or whether there is a list of medications; utilizing an electronic database of prescriptions filled through insurance; calling the patient’s pharmacy, insurance company, and/or primary care provider; and comparing the newly obtained list to the history documented in the patient’s electronic health record (EHR). The pharmacy technician follows up with the patient to ask whether he or she is taking any over-the-counter medications, such as vitamins or aspirin. The pharmacy technician also updates the patient’s preferred pharmacy in the EHR.
Figure 1.
Medication Reconciliation Flow for Patient Arriving to Emergency Department by Ambulance
ED = emergency department; LIP = licensed independent practitioner; MAR = medication administration record; PCP = primary care physician.
When the patient is unable to provide a medication history or a medication list or the caregiver is unavailable, the technician will compile a list as accurately as possible using available resources. These resources may include past medication histories if available, electronic databases, calling the patient’s pharmacy, or asking the ED pharmacist to generate a New Jersey prescription-monitoring program report when appropriate. In these cases, the pharmacy technician will indicate in the medication history that she is not able to assess adherence to the documented regimen and will alert the physician.
By mutual agreement given the high patient volume, the nurse will generally independently complete the medication history when the patient has four or fewer medications. If the patient has more than four medications or if the medication history is complex or time consuming (such as patients coming from long-term-care facilities, who tend to have long medication histories), the nurse will reach out to the pharmacy technician by phone or in person or will record the term “MAR” (medication administration record) in the notes field on the electronic ED patient-tracking queue to alert the technician that a medication history needs to be completed. In the meantime, the technician independently looks at new patient records between documentations to proactively identify patients who will need medication histories.
In the daily workflow, multiple patients may simultaneously require a medication history to be completed by the pharmacy technician. In these instances, the pharmacy technician will “triage” patients with physician and nursing assistance, taking into account the disease state that precipitated the ED visit. For example, a stroke patient being assessed for administration of tissue plasminogen activator will take precedence over other patients. The technician will also prioritize medication histories for patients who are being admitted so that the admitting physicians can quickly reconcile and order the medications to ensure smooth continuity of care. Often, the technician will speak to multiple patients who need medication histories in one trip, make copies of medication lists, and bring the documentation back to her workstation to complete the medication histories as efficiently as possible.
During one work shift, the pharmacy technician is able to complete approximately 20 medication histories. The duration of time spent on each medication history varies based on the complexity of the medication list and the available resources. Generally, each history takes about five to 30 minutes to complete, with an average of 20 to 24 minutes. It is important to note that the pharmacy technician’s workspace is located in the high-traffic geriatric ED. As a result, the pharmacy technician frequently interacts with patients and family members, assisting patients who have questions or fielding them to the appropriate nurse. The pharmacy technician also attends codes in the ED in case she might be able to help the medical staff obtain a medication.
METHODS
Study Setting
This study was conducted between July 2015 and March 2016 at a 520-bed community academic hospital that had 48,544 ED visits in 2015. The 47-bed ED consists of three triage beds, six overflow beds, 19 adult beds, six express care beds, a six-bed geriatric emergency medicine unit, and a seven-bed pediatric ED. The average daily volume in the ED is approximately 115 patients.
Inclusion and Exclusion Criteria
The study patients were chosen consecutively during the study period by the pharmacy resident based on manual review of paper medication history logs retained by the pharmacy technician, followed by a review of the electronic documentation in the medical chart. To be included in the study, patients had to have a medication history first documented electronically by an ED nurse, followed by the pharmacy technician, so that a comparison could be performed. Due to the nature of the patient population the pharmacy technician targets (see Program Description and Figure 1), patients were included if they were at least 18 years of age, taking at least one medication, and were seen in the ED for a medical condition (and subsequently discharged from the ED, placed on observation status, or admitted to the hospital). We excluded patients younger than 18 years of age, patients seen in the psychiatric emergency screening service, and patients seen in the ED outside of the pharmacy technician’s scheduled work shift.
Study Design
This study was approved by the institutional review board (IRB) and comprised three separate components, including two medication history discrepancy analyses and a workflow description. The first analysis was based on a retrospective chart review by the PGY-1 pharmacy resident of 50 patients visiting the ED at our facility between July and October 2015. To be included in the first analysis, patients had to first have a medication history documented in the electronic medical record by a nurse, and a follow-up medication history electronically documented by the pharmacy technician. The second analysis was a real-time observational study in March 2016, in which the emergency medicine clinical pharmacist accompanied the pharmacy technician in the collection of 50 medication histories, observed the technician’s routine in obtaining the medication history, and intervened as necessary to complete the best possible medication history. Pharmacist interventions were documented as medication discrepancies. The third component of the study consisted of a workflow diagram that was established by the PGY-1 pharmacy resident through interviews of the nursing staff, pharmacy technician, ED pharmacist, resident physicians, and attending physicians.
The IRB waived the need for patient consent in the first analysis because of the retrospective nature of the study design and in the second analysis because the ED pharmacist, by observing the pharmacy technician, was acting within her usual scope of practice in overseeing the pharmacy technician’s work. Additionally, we felt that patients and caregivers might respond differently to standard questions about their medication history and adherence if they knew the process was being monitored for a study.
Data Collection
Baseline characteristics, including the patients’ admission status after being seen in the ED, were collected for both discrepancy analyses. It is important to note that the total number of medications was based on each subject’s final medication list, so medication duplicates or additional medications were not included in this list.
Possible discrepancies recorded included a medication omission (failure to document a medication that the patient is actively taking), medication commission (addition of a medication that the patient is not taking), duplicate medication, incorrect or missing doses, incorrect or missing frequencies, and incorrect or missing formulations (when necessary). It was possible for one medication to have more than one documented discrepancy (for example, an entry of “atenolol” would be documented as a missing dose as well as a missing frequency). The discrepant medications were categorized by therapeutic drug class, which included: pain, gastrointestinal, cardiovascular, neurological or psychiatric, immune, diabetic, asthma or chronic obstructive pulmonary disease, topical, herbal supplements or vitamins, ophthalmic, antibiotic or antiviral, endocrine, or other. Each medication was categorized only once by therapeutic drug class.
Statistical Analysis
Student’s t-tests were used to compare the medications per patient and ages. Fischer’s exact tests were used to compare the number of histories with an error, the number of medications with an error, and the gender of the patients. Results were considered statistically significant if the alpha was less than 0.05. Descriptive statistics were calculated using Microsoft Windows Excel (version 2011) and GraphPad QuickCalcs.
RESULTS
Error Rate Analysis
During the study period, 36,409 patients were seen in the ED; the pharmacy technician saw 2,840 of them. Fifty medication histories were evaluated in each of the two analysis groups. Baseline characteristics (Table 1) between the two groups were similar, with a mean of nine medications per patient in the nurse-pharmacy technician group (RN-PT) and 10 medications in the pharmacy technician-pharmacist group (PT-RPh). However, significantly more patients in the PT-RPh group were admitted to the hospital after being seen in the ED compared with the RN-PT group (70% versus 40%, respectively; P = 0.0046).
Table 1.
Baseline Characteristics of Study Groups
| RN-PT | PT-RPh | P Value | |
|---|---|---|---|
| Medications per patient, mean (± SD) | 9 (4.0) | 10 (7.1) | 0.416 |
| Mean age, years (± SD) | 66 (15.9) | 61 (14.6) | 0.154 |
| Male, n (%) | 22 (44) | 20 (40) | 0.840 |
| Admitted to hospital from ED, n (%) | 20 (40) | 35 (70) | 0.0046 |
PT = pharmacy technician; RN = registered nurse; RPh = registered pharmacist; SD = standard deviation.
There were 474 medications evaluated in the RN-PT group and 521 medications in the PT-RPh group (Table 2). Of 50 completed medication histories in each group, nurses documented a medication history with at least one discrepancy for all 50 medication histories (100%), while the pharmacy technician documented a discrepancy that needed to be corrected by the pharmacist in 18 of 50 medication histories (36%). Of the 474 total medications in the RN-PT group, 408 medications had an error, corresponding to an error rate of 86% for nurses. In the PT-RPh group, 30 of 521 medications had an error, corresponding to an error rate of 5.6% (P < 0.0001).
Table 2.
Number of Medications and Errors
| RN-PT | PT-RPh | P value | |
|---|---|---|---|
| Total medications | 474 | 521 | NA |
| Number of histories with error, n (%) | 50 (100) | 18 (36) | < 0.0001 |
| Medications with error, n (%) | 408 (86) | 30 (5.6) | < 0.0001 |
NA = not applicable; PT = pharmacy technician; RN = registered nurse; RPh = registered pharmacist.
Of 502 documented discrepancies across all of the medications (Table 3), the three most common types of medication discrepancies made by nurses included missing a medication (21.7%), including an additional medication the patient was not taking (17.9%), and failing to document the dose of a medication (17.9%). The pharmacy technician had 30 documented discrepancies, the three most common being a wrong frequency (63.3%), a wrong dose (16.7%), and a wrong formulation (13.3%). With regard to the therapeutic drug class of discrepant medications, nurses most commonly made errors with cardiovascular medications, vitamins, and neurological/psychiatric medications, while the pharmacy technician most often made errors with gastrointestinal and neurological/psychiatric medications and vitamins (Table 4).
Table 3.
Classification by Discrepancy Type
| Type | Number of Discrepancies | |
|---|---|---|
| RN-PT, n (%) | PT-RPh, n (%) | |
| Missing medication | 109 (21.7) | 2 (6.7) |
| Additional medication | 90 (17.9) | 0 |
| Missing dose | 90 (17.9) | 0 |
| Missing frequency | 69 (13.7) | 0 |
| Wrong frequency | 54 (10.8) | 19 (63.3) |
| Wrong dose | 42 (8.4) | 5 (16.7) |
| Duplicate medication | 21 (4.2) | 0 |
| Wrong formulation | 15 (3.0) | 4 (13.3) |
| Missing formulation | 12 (2.4) | 0 |
PT = pharmacy technician; RN = registered nurse; RPh = registered pharmacist.
Table 4.
Errors by Therapeutic Drug Class
| Number of Errors | ||
|---|---|---|
| Drug Class | RN-PT, n (%) | PT-RPh, n (%) |
| Cardiovascular | 100 (24.5) | 2 (6.7) |
| Vitamins | 75 (18.4) | 4 (13.3) |
| Neurological/psychiatric | 57 (14.0) | 6 (20.0) |
| Gastrointestinal | 51 (12.5) | 11 (36.7) |
| Diabetes | 21 (5.1) | 1 (3.3) |
| Other | 16 (3.9) | 1 (3.3) |
| Antibiotic/antiviral | 13 (3.2) | 0 |
| Immune | 10 (2.5) | 0 |
| Ophthalmic | 9 (2.2) | 1 (3.3) |
| Asthma/COPD | 6 (1.5) | 0 |
| Endocrine | 6 (1.5) | 0 |
| Topical | 4 (1.0) | 1 (3.3) |
COPD = chronic obstructive pulmonary disease; PT = pharmacy technician; RN = registered nurse; RPh = registered pharmacist.
DISCUSSION
This study demonstrated improved accuracy when the pharmacy technician obtained and documented a medication list compared with ED nurses. The findings of this study are congruent with other studies examining the impact of pharmacy technicians on the medication history and reconciliation process.5,7,8 For example, a prospective study by Johnston et al. showed that well-trained pharmacy technicians are able to obtain a medication history with as much accuracy and completeness as pharmacists, without a requirement for additional time.7 A retrospective 720-chart review by Smith et al. revealed that accuracy of the medication history was 45.8% versus 95% using a multidisciplinary process versus a pharmacy-based process, respectively.8 Additional studies have documented the utility of pharmacy technicians in obtaining the best possible medication histories in surgical patients, hemodialysis patients, hospitalized patients infected with human immunodeficiency virus, psychiatric patients, and pediatric cardiology patients.9–14
In our study, we found the pharmacy technician had an accuracy rate of 94.4%, compared with an accuracy rate of 14% for ED nurses. While we did not formally analyze the pharmacy technician’s areas of error, it appeared that many frequency errors pertained to scheduled versus unscheduled dosing (i.e., whether a medication was to be taken on a scheduled basis or only as needed, such as bowel regimens). This overall error rate correlates with the findings of several other studies evaluating the efficacy of pharmacy technicians performing medication histories. For example, Hart et al. found that medication histories obtained by pharmacy technicians in the ED were accurate without any identifiable errors 88% of the time, compared with 57% of medication histories obtained by nursing staff.5 Leung et al. found that pharmacy technicians and pharmacists had an agreement rate of 98.9% on medication histories performed for 99 hemodialysis outpatients.11 Cooper et al. established a pharmacy technician medication history program in a five-hospital community health system, with the finding that pharmacy technicians are capable of completing medication histories accurately and completely at a rate of consistently more than 90%.15
A compelling finding of our study was that the pharmacy technician’s practice of obtaining accurate medication histories often includes the time-consuming tasks of calling pharmacies, insurance companies, and physicians’ offices. In the study of the ED workflow, we were unable to compare the time that the ED nurses spent performing these tasks with that of the pharmacy technician because nurses do not have time to engage in these activities. Simply speaking, when the pharmacy technician is not there, nurses will use readily available information (such as a verbal history or a medication list provided by the patient) or they will import an already documented medication list if available, regardless of whether the list is outdated or not. At this point, it is up to the physicians whether to trust that the existing medication history is current or whether to start obtaining the medication history themselves if the patient is admitted to the hospital.
In addition, it is interesting to note that in the error rate analyses, we found that the pharmacy technician performed medication histories for significantly more patients who were subsequently admitted to the hospital in the PT-RPh group than in the RN-PT group (70% versus 40%, respectively, P = 0.0046). We hypothesize that this may reflect the growing ability of the pharmacy technician to identify and target patients who are more likely to be admitted to the hospital (for example, elderly or acutely ill patients, or those with complex medication regimens), as approximately six months passed between these two data sets.
There are a few limitations to our study. One is a lack of generalizability, given that this study evaluated the process of one technician in one facility. The ED pharmacy technician is part of a new program, and there is no formal process for targeting patients or documenting interventions. In addition, the different design between the two study groups in the error rate analysis may lend itself to potentially skewed results, particularly when accounting for the Hawthorne effect in the group in which the clinical pharmacist observed the pharmacy technician.
At this time, the pharmacy technician is able to see about 20 patients per shift, which accounts for only about 17% of patients seen daily in the ED. While we did not formally measure staff satisfaction before and after the study, it is noteworthy that the ED staff appears quite receptive to the utility of the pharmacy technician and often independently seeks out her service during her shift. This study did not include a financial analysis, but available hourly pay averages for the health care system indicate that pharmacy technicians are compensated at approximately 45% and 29% of the average salary of a staff nurse and a staff pharmacist, respectively. From a monetary perspective, hiring a pharmacy technician to perform medication histories is more cost-effective than hiring an additional nurse or ED pharmacist. It would be interesting for future studies to explore the cost savings in terms of medication errors or adverse events prevented, or even high-risk hospital readmissions prevented. We hope to expand this service with the use of electronic databases to collect outside pharmacy prescription information, which will allow a more streamlined and efficient process. Ultimately, we hope that the sustained success of this program will justify its expansion.
CONCLUSION
In this study, medication histories obtained by the pharmacy technician were significantly more complete and accurate than those obtained by emergency department nurses.
Acknowledgments
The authors would like to thank their pharmacy technician, Ashley O’Keefe, for her contributions to this work.
REFERENCES
- 1.The Joint Commission Hospital: 2016 national patient safety goals. Available at: www.jointcommission.org/standards_information/npsgs.aspx. Accessed February 14, 2016.
- 2.Porcelli PJ, Waitman LR, Brown SH. A review of medication reconciliation issues and experiences with clinical staff and information systems. Appl Clin Inform. 2010;1(4):442–461. doi: 10.4338/ACI-2010-02-R-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 4.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23(9):1414–1422. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hart C, Price C, Graziose G, Grey J. A program using pharmacy technicians to collect medication histories in the emergency department. P T. 2015;40(1):56–61. [PMC free article] [PubMed] [Google Scholar]
- 6.American Society of Health-System Pharmacists ASHP statement on pharmacy services to the emergency department. Am J Health-Syst Pharm. 2008;65:2380–2383. Available at: www.ashp.org/DocLibrary/BestPractices/SpecificStEmergDept.aspx. Accessed January 18, 2016. [Google Scholar]
- 7.Johnston R, Saulnier L, Gould O. Best possible medication history in the emergency department: comparing pharmacy technicians and pharmacists. Can J Hosp Pharm. 2010;63(5):359–365. doi: 10.4212/cjhp.v63i5.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith SB, Mango MD. Pharmacy-based medication reconciliation program utilizing pharmacists and technicians: a process improvement initiative. Hosp Pharm. 2013;48(2):112–119. doi: 10.1310/hpj4802-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michels RD, Meisel SB. Program using pharmacy technicians to obtain medication histories. Am J Health-Syst Pharm. 2003;60(19):1982–1986. doi: 10.1093/ajhp/60.19.1982. [DOI] [PubMed] [Google Scholar]
- 10.van den Bemt PM, van den Broek S, van Nunen AK, et al. Medication reconciliation performed by pharmacy technicians at the time of preoperative screening. Ann Pharmacother. 2009;43(5):868–874. doi: 10.1345/aph.1L579. [DOI] [PubMed] [Google Scholar]
- 11.Leung M, Jung J, Lau W, et al. Best possible medication history for hemodialysis patients obtained by a pharmacy technician. Can J Hosp Pharm. 2009;62(5):386–391. doi: 10.4212/cjhp.v62i5.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siemianowski LA, Sen S, George JM. Impact of a pharmacy technician-centered medication reconciliation on optimization of antiretroviral therapy and opportunistic infection prophylaxis in hospitalized patients with HIV/AIDS. J Pharm Pract. 2013;26(4):428–433. doi: 10.1177/0897190012468451. [DOI] [PubMed] [Google Scholar]
- 13.Brownlie K, Schneider C, Culliford R, et al. Medication reconciliation by a pharmacy technician in a mental health assessment unit. Int J Clin Pharm. 2014;36(2):303–309. doi: 10.1007/s11096-013-9875-8. [DOI] [PubMed] [Google Scholar]
- 14.Chan C, Woo R, Seto W, et al. Medication reconciliation in pediatric cardiology performed by a pharmacy technician: a prospective cohort comparison study. Can J Hosp Pharm. 2015;68(1):8–15. doi: 10.4212/cjhp.v68i1.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cooper JB, Lilliston M, Brooks D, Swords B. Experience with a pharmacy technician medication history program. Am J Health-Syst Pharm. 2014;71(18):1567–1574. doi: 10.2146/ajhp130590. [DOI] [PubMed] [Google Scholar]