Abstract
The Peter the Great Museum of Anthropology and Ethnography (Kunstkamera) in Saint Petersburg is the oldest museum in Russia. It keeps the remains of the anatomical collection of the world‐famous 17th century Dutch anatomist Frederik Ruysch. This unique collection was bought and shipped in 1717 by Czar Peter the Great, and presently still comprises more than 900 specimens, a modest number of which concerns specimens with congenital anomalies. We searched for teratological clues in the existing collection and in all his descriptions and correspondence regarding specimens and cases he encountered during his career as doctor anatomiae and chief instructor of the surgeons and midwives in Amsterdam. A total of 63 teratological specimens and case descriptions were identified in this legacy, including some exceedingly rare anomalies. As it turns out, Ruysch was the first to describe several of the conditions we encountered, including intracranial teratoma, enchondromatosis, and Majewski syndrome. Although his comments pose an interesting view on how congenital anomalies were scientifically perceived in early 18th century Europe, Ruysch mostly refrained from explaining the causes of the conditions he encountered. Instead, he dedicated himself to careful descriptions of his specimens. Almost 300 years after his demise, Ruysch's legacy still impresses and inspires both scientists and lay men. © 2016 The Authors. American Journal of Medical Genetics Part A Published by Wiley Periodicals, Inc.
Keywords: 17th century, acardiac twins, anatomical specimen, ciliary chondrodysplasia, cleft lip/palate, conjoined twins, disorganization‐like syndrome, enchondromatosis, Frederik Ruysch, gastric teratoma, Hirschsprung disease, holoprosencephaly, hydatifom mole, hydrocephaly, intracranial teratoma, Kunstkamera, limb reduction defects, Meckel diverticulum, neural tube closure defects, omental teratoma, Peter the Great, teratology, umbilical angiomyxoma, urogenital anomalies, ventral body wall defects
INTRODUCTION
Frederik Ruysch (1638–1731) (Fig. 1) was a Dutch professor in anatomy and botany at the Athenaeum Illustre, the predecessor of the University of Amsterdam, The Netherlands. During his career as a doctor anatomiae, Praelector of the Amsterdam Guild of Surgeons (Fig. 2) and chief instructor of midwives, he built up a collection of over 2,000 anatomical, pathological, zoological, and botanical specimens, which he preserved either dried or embalmed [Kooijmans, 2004]. He exhibited his collection, open to the public, in his three‐story dwelling at the Bloemgracht in downtown Amsterdam. Already in the 17th century, Ruysch became famous for his meticulous technique of post mortal vascular injections. He developed a mercuric sulfide‐based injection mixture originating from cinnabar, a naturally occurring red colored mineral. This injection fluid gave his specimens, especially the many preparations of fetuses and infants, a reddish, almost lively expression (Fig. 3). With this technique the smallest blood vessels could be visualized and dissected, a groundbreaking technique in the 17th century [Luyendijk‐Elshout, 1970].
Figure 1.
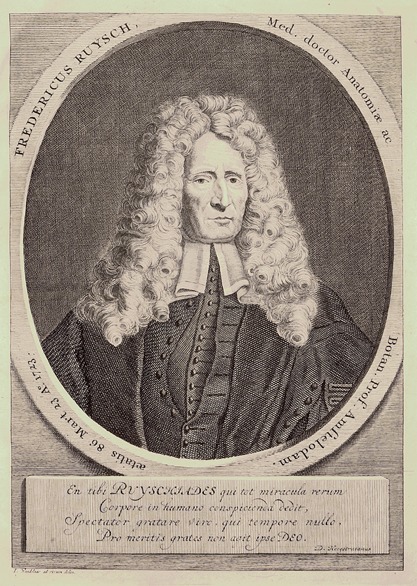
Portrait of Frederik Ruysch at the age of 85, copperplate. Jan Wandelaar, 1723. [Color figure can be viewed at wileyonlinelibrary.com].
Figure 2.

“The anatomical lesson of Frederik Ruysch” (oil painting on canvas). Depicted are the board of the Surgeons Guild, Frederik Ruysch presenting the umbilicus of the “subjectum anatomicum,” and his son Hendrik Ruysch holding a dried neonatal skeleton. Jan van Neck, 1683. Amsterdam Museum. [Color figure can be viewed at wileyonlinelibrary.com].
Figure 3.
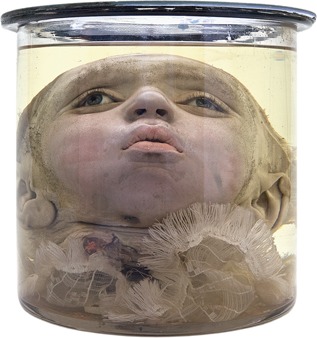
Specimen 4070–174: A child's head with artificial glass eyes and red colored skin resulted from postmortem cinnabar‐containing vascular injections. From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
When Czar Peter the Great (1672–1725) came to power in Russia at the end of the 17th century, he was determined to modernize Russia. Peter the Great had a prestige project: the new city of Saint Petersburg. To achieve this modernization, he let the Dutch republic inspire him; the Golden age in Holland, a perfect model for Russia [Kooijmans, 2004]. Following his visits to Ruysch's anatomical collection in Amsterdam in 1697 and again in 1716, he purchased it for his planned cabinet of curiosities, for an astonishing amount of 30,000 guilders. Upon arrival in 1717, the 2,000 specimens were initially stored in his summer Palace before they were exhibited in the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera). After the grand opening of the Kunstkamera in 1719, in the former mansion of the boyar Alexander Kikin, it started to function as a public museum, the first of its kind in Russia [Radziun and Chistov, 2012]. The new building of the Kunstkamera on the banks of the Neva river in Saint Petersburg (Fig. 4) opened its doors in 1728 and presently houses nearly two million items, including the remnants of the anatomical collection of Frederik Ruysch.
Figure 4.

Peter the Great Museum of Anthropology and Ethnography (Kunstkamera) on the banks of the Neva river in Saint Petersburg (Russia). From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
The collection that was bought by Peter the Great (from here on referred to as Ruysch's first collection) consisted of twelve subsequently composed cabinets (thesauri anatomici), comprising human, animal and plant specimens which, upon completion, were described by Ruysch in Latin and issued as illustrated catalogues. Ten of these cabinets were numbered (Thesaurus Anatomicus I–X), one comprised his earliest specimens (Musaeum Anatomicum Ruyschianum sive Catalogus Rariorum) and one consisted only of animal specimens (Thesaurus Animalium). Together with numerous clinical observations, treatises and correspondences they were collectively re‐issued in 1721 as Opera Omnia Anatomico‐Medico‐Chirurgica (Collected anatomical, medical and surgical works) [Ruysch, 1721], from here on referred to as Opera Omnia or Collected Works (CW). Until 1728, later editions were amended with subsequent contributions, including observations, letters and two additional cabinets, named Curae Posteriores (Subsequent Exercises) and Curae Renovatae (Renewed Exercises) that Ruysch composed after he had sold his first collection. A biography on Ruysch by Johan Friedrich Schreiber was added in 1732. In 1744, 13 years after Ruysch's death, the CW were translated into Dutch by Ysbrand Gysbert Arlebout (Alle de Ontleed‐, Genees‐ en Heelkundige Werken) [Ruysch, 1744]. Only a small part, concerning the 100 clinical observations, was translated into French [Ruysch, 1734] and English [Ruysch, 1751].
Soon after he died in 1731 his second collection, that he had been composing since 1717, was auctioned. The auction catalogue, titled Catalogus Musaei Ruyschianii, listed almost 1,300 indexed specimens in no less than nine cabinets, including the two Curae collections that had appeared in later editions of the CW, albeit in reversed order [Anonymous, 1731]. The present whereabouts of these specimens are unknown.
Although all specimens had made it safely from Amsterdam to Saint Petersburg and the original order of display in their respective cabinets was initially preserved, the matching between specimens and their descriptions got lost in later years during subsequent rearrangements of the exhibition. Over the years, about half of the specimens perished, disappeared or were donated to other institutes [Ternowsky, 1927; Ginzburg, 1953, 1959]. Today, the 916 specimens ascribed to Ruysch that have stood the tooth of time are being restored and investigated by the Ruysch Research Group, an international consortium of Russian and Dutch historians, anatomists and surgeons that focus on the matching of specimens and descriptions. We here report on the proceedings regarding the specimens of human congenital malformations and the diagnoses that we made. Additionally, we discuss the scientific and public opinions of Ruysch and his contemporaries towards congenital malformations and the present day value of his legacy.
MATERIALS AND METHODS
In this survey we included the complete legacy of Frederik Ruysch regarding specimens and descriptions of human cases of congenital anomalies. Animal specimens were left out of this survey. We first investigated the specimens of congenital anomalies, attributed to Ruysch and present at the Kunstkamera in St. Petersburg, and diagnosed the conditions they presented with by means of external inspection. In some cases the specimens were taken out of their jars for restoration purposes, which made it possible to investigate them in more detail. To refer to specimens in the extant collection we used the numbers that they got assigned during the last re‐inventory in 1947 [Ginzburg, 1953]. These numbers consist of two parts, the first of which (4070) refers to the Ruysch collection and the second one (1–935) to the specimen itself. Images and details of the specimens can be found at the website of the Kunstkamera: http://www.kunstkamera.ru/kunst‐catalogue/index.seam?c=RUYSH&page=1.
Secondly, we explored all parts of the CW, as well as the auction catalogue of his second collection (see Table I) for descriptions and pictures of congenital anomalies. Most of these descriptions referred to specimens that were part of the first or second Ruysch collections but several concerned case observations that Ruysch made in his anatomical and obstetric practice without resulting in anatomized preparations. Some specimens and case descriptions were mentioned more than once in the CW. Unlike the Dutch text, the Latin text of the complete set of works (Opera Omnia) was published without a continuous page numbering. To refer to descriptions of specimens and cases we therefore used the page numbering of the separate works, named by codes derived from their (abbreviated) titles (see Table I). These separate works, as well as the two volumes of the CW, have been published as e‐books on Google Books and can be inspected and downloaded for free.
Table I.
Contents of Frederik Ruysch's Written Legacy
| Original title (abbreviated) | Title code a | Year | Contents |
|---|---|---|---|
| Opera Omnia, volume 1 | 1721–1728 | ||
| Historia vitae | 1732 | Biography on Ruysch | |
| Dilucidatio valvularum | Dil Valv | 1665 | Treatise on vascular valves & 26 clinical observations |
| Observationum anatomico‐chirurgicarum | Obs Cent | 1691 | 100 clinical observations |
| Museum anatomicum Ruyschianum | Mus Anat | 1691 | Descriptions of collected specimens |
| Epistola anatomica I | 1695 | Correspondence with Gaubius | |
| Epistola anatomica II | 1695 | Correspondence with Gaubius | |
| Epistola anatomica III | 1695 | Correspondence with Gaubius | |
| Epistola anatomica IV | 1696 | Correspondence with Campdomercus | |
| Epistola anatomica V | 1696 | Correspondence with Frentz | |
| Epistola anatomica VI | 1696 | Correspondence with Graetz | |
| Epistola anatomica VII | 1696 | Correspondence with Graetz | |
| Epistola anatomica VIII | 1696 | Correspondence with Graetz | |
| Epistola anatomica IX | 1697 | Correspondence with Goehlicke | |
| Epistola anatomica X | 1697 | Correspondence with Keerwolff | |
| Epistola anatomica XI | 1698 | Correspondence with Wolf | |
| Epistola anatomica XII | 1699 | Correspondence with Ettmüller | |
| Epistola anatomica XIII | 1700 | Correspondence with Wedel | |
| Epistola anatomica XIV | Ep Anat XIV | 1701 | Correspondence with Van Reverhorst |
| Epistola anatomica XV | 1704 | Correspondence with Graetz | |
| Epistola anatomica XVI | 1713 | Correspondence with Vater | |
| Responsio ad Godefridi Bidloi libellum | 1721 | Answer to Bidloo on his treatise | |
| Adversariorum anatomico‐medico‐chir. decas prima | Adv Dec I | 1717 | 10 clinical remarks |
| Adversariorum anatomico‐medico‐chir. decas secunda | Adv Dec II | 1720 | 10 clinical remarks |
| Adversariorum anatomico‐medico‐chir. decas tertia | Adv Dec III | 1723 | 10 clinical remarks |
| Opera Omnia, volume 2 | 1721–1728 | ||
| Thesaurus animalium primus | 1710 | Descriptions of collected animal Specimens | |
| Thesaurus anatomicus I | Thes Anat I | 1701 | Descriptions of collected specimens |
| Thesaurus anatomicus II | Thes Anat II | 1702 | Descriptions of collected specimens |
| Thesaurus anatomicus III | Thes Anat III | 1703 | Descriptions of collected specimens |
| Thesaurus anatomicus IV | Thes Anat IV | 1704 | Descriptions of collected specimens |
| Thesaurus anatomicus V | 1705 | Descriptions of collected specimens | |
| Thesaurus anatomicus VI | Thes Anat VI | 1705 | Descriptions of collected specimens |
| Thesaurus anatomicus VII | Thes Anat VII | 1707 | Descriptions of collected specimens |
| Thesaurus anatomicus VIII | Thes Anat VIII | 1709 | Descriptions of collected specimens |
| Thesaurus anatomicus IX | Thes Anat IX | 1714 | Descriptions of collected specimens |
| Thesaurus anatomicus X | Thes Anat X | 1716 | Descriptions of collected specimens |
| Curae posteriores | Cur Post | 1724 | Descriptions of collected specimens |
| Curae renovatae | Cur Reno | 1728 | Descriptions of collected specimens |
| Tractatio anatomica de musculo in fundo uteri | Trac Anat | 1723 | Treatise on morphology of uterus and Placenta |
| Epistola problematica Bohlii | 1726 | Correspondence with Bohlius | |
| Epistola problematica Hecqueti | 1726 | Correspondence with Hecquet | |
| Epistola problematica Vateri | 1726 | Correspondence with Vater | |
| Epistola problematica Boerhavi | 1722 | Correspondence with Boerhaave | |
| Other works | |||
| Catalogus Musaei Ruyschiani | Cat Mus | 1731 | Auction catalogue of Ruysch's second collection |
| Observations Anatomiques et Chirurgicales, | 1734 | French translation of the 100 clinical observations | |
| Ruysch's Practical Observations in Surgery and Midwifry | 1751 | English translation of the 100 clinical observations |
Title codes of the relevant sections of the Collected Works are used in the text and in Table II to refer to specimen and case descriptions.
Thirdly, we tried to match the descriptions and pictures with the specimens still present in the Kunstkamera collection. All (references to) specimens and descriptions were reduced to “unique cases,” meaning that if more than one description of, or references to, a case and/or specimen was found, they were counted as one collective case. This also concerns cases consisting of multiple specimens. Regarding the specimens, cases and descriptions, we defined the following categories: 1. Specimens of the first collection with matching descriptions. 2. Specimens of the first collection without matching descriptions. 3. Descriptions referring to either the first or the second collections without matching specimens. 4. Descriptions of case observations that did not result in anatomized specimens. Finally, we searched the literature for references to Ruysch's specimens and case descriptions.
RESULTS
In the existing anatomical collection present at the Kunstkamera, we identified 17 specimens that showed one or more congenital anomalies. In the CW and the auction catalogue, we found descriptions of 32 specimens with one or more congenital anomalies. Five of these descriptions could be matched with certainty to a specimen in the existing collection (category 1). Twelve specimens could not be matched with descriptions, mainly because uniquely identifying structures were lacking (category 2). Furthermore, we found descriptions of 27 cases without matching specimens (category 3), ten of which concerned specimens of the second collection (including the Curae), and 19 case descriptions that did not refer to anatomical specimens (category 4). In total we found 63 unique cases, most of which could be diagnosed with reasonable certainty, in that a single diagnosis or a confined group of related diagnoses was applicable to the presented condition. If two or more divergent diagnoses were equivalently applicable, we considered the condition to be indiscernible. In Table II the cases, numbered 1–63, in each of the defined categories are listed according to the diagnoses we made. The characteristics of these cases are given below. Unless stated otherwise they concerned Ruysch's first collection.
Table II.
Human Congenital Anomalies Found in the Legacy of Frederik Ruysch
| Case | Category a | Diagnosis | Specimen(s) b | Description(s) in CW c | Figures |
|---|---|---|---|---|---|
| 1 | 3 | Acardiac twin | Thes Anat IX, p.17, 41; Adv Dec II, p.42 | 5 | |
| 2 | 3 | Cleft lip and palate | Thes Anat VI, p.34; Adv Dec I, p. 21 | ||
| 3 | 3 | Gastric teratoma | Adv Dec III, p.2‐7; Cur Post, p.23 | 6 | |
| 4 | 1 | Intracranial teratoma | 4070–906, −672, −681 | Thes Anat II, p. 16–18, 43, 44 | 7 |
| 5 | 3 | Omental teratoma | Obs Cent, p.23, 24; Mus Anat, p.36; Thes Anat III, p. 27; Cur Post, p. 11; Cat Mus, p.54 | 8 | |
| 6 | 3 | Ovarial teratoma | Thes Anat I, p.29, 30, 33 | 9 | |
| 7 | 3 | Umbilical haemagiomyxoma | Thes Anat IX, p.10 | ||
| 8 | 1 | Lateral conjoined twins | 4070–913 | Thes Anat VII, p. 3; Adv Dec I, p.20 | 10A |
| 9 | 2 | Lateral conjoined twins | 4070–911 | ||
| 10 | 2 | Lateral conjoined twins | 4070–914 | 10B | |
| 11 | 2 | Lateral conjoined twins | 4070–916 | 10C | |
| 12 | 1 | Ventral conjoined twins | 4070–912 | Adv Dec I, p.21, Adv Dec II, p.42 | 10D |
| 13 | 4 | Membranous rectal atresia | Adv Dec II, p.43 | ||
| 14 | 4 | Rectal agenesis | Adv Dec II, p.43 | ||
| 15 | 4 | Hirschsprung disease | Obs Cent, p.86 | ||
| 16 | 3 | Meckel diverticulum | Mus Anat, p.63; Thes Anat VII, p.3, 7 | 11 | |
| 17 | 3 | Meckel diverticulum | Thes Anat VII, p.7 | ||
| 18 | 3 | Meckel diverticulum | Cur Post, p.22 | ||
| 19 | 3 | Multiple liver cysts | Cat Mus, p.70 | ||
| 20 | 3 | Holoprosencephaly | Cur Reno, p.10; Adv Dec I, p.21 | ||
| 21 | 3 | Hydatidiform mole | Cur Post, p.7 | ||
| 22 | 3 | Hydatidiform mole | Cur Post, p.15 | ||
| 23 | 3 | Hydatidiform mole | Cat Mus, p.62 | ||
| 24 | 4 | Hydatidiform mole | 4070–666 | ||
| 25 | 4 | Hydatidiform mole | 4070–669 | ||
| 26 | 4 | Hydatidiform mole | 4070–670 | ||
| 27 | 4 | Hydatidiform mole | 4070–673 | ||
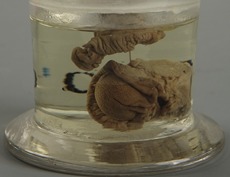
| 28 | 4 | Hydatidiform mole | 4070–674 | 12 | |
| 29 | 4 | Hydatidiform mole | 4070–675 | ||
| 30 | 3 | Hydrocephaly | Mus Anat, p.65; Thes Anat III, p.11 | ||
| 31 | 3 | Hydrocephaly | Thes Anat IX, p.19 | ||
| 32 | 1 | Limb malformation | 4070–907 | Thes Anat VIII, p.16 | 13 |
| 33 | 2 | Limb malformation | 4070–039 | 14A | |
| 34 | 2 | Limb malformation | 4070–908 | 14B | |
| 35 | 1 | Anencephaly | 4070–915 | Adv Dec I, p.20 | 15 |
| 36 | 3 | Anencephaly | Thes Anat VIII, p.3; Adv Dec I, p.20 | 16 | |
| 37 | 3 | Anencephaly | Adv Dec I, p.20 | ||
| 38 | 3 | Anencephaly | Cat Mus, p.85 | ||
| 39 | 3 | Meningo(myelo)cele | Obs Cent, p.33 | ||
| 40 | 4 | Meningo(myelo)cele | Obs Cent, p.33 | 17 | |
| 41 | 4 | Meningo(myelo)cele | Obs Cent, p.33 | ||
| 42 | 4 | Meningo(myelo)cele | Obs Cent, p.35 | ||
| 43 | 4 | Meningo(myelo)cele | Obs Cent, p.35 | ||
| 44 | 3 | Ciliary chondrodysplasia | Mus Anat, p.186; Adv Dec I, p.20 | 18 | |
| 45 | 4 | Enchondromatosis | Ep Anat XIV, p.9‐18 | 19 | |
| 46 | 4 | Disorder of sex development | Thes Anat VIII, p.17; Adv Dec I, p.22 | ||
| 47 | 3 | Fallopian tube duplication | Thes Anat IV, p.20 | ||
| 48 | 2 | Hypospadias | 4070–600 | 20 | |
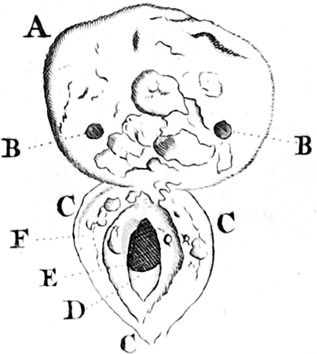
| 49 | 4 | Imperforate hymen | Obs Cent, p.42 | ||
| 50 | 4 | Transverse vaginal septum | Obs Cent, p.27 | 21 | |
| 51 | 4 | Ureteral duplication | Dil Valv, p.18 | ||
| 52 | 4 | Ureteral duplication | Dil Valv, p.25 | ||
| 53 | 4 | Ureteral duplication | Obs Cent, p.100 | 22 | |
| 54 | 3 | Ureteral duplication | Thes Anat VII, p.9 | ||
| 55 | 4 | Bladder exstrophy | Obs Cent, p.22, 23 | 23 | |
| 56 | 4 | Omphalocele | Obs Cent, p.92 | 24 | |
| 57 | 4 | Omphalocele | Obs Cent, p.93 | ||
| 58 | 4 | Omphalocele/gastroschisis | Obs Cent, p.93 | ||
| 59 | 4 | Axial skeletal anomaly | Dil Valv, p.14 | ||
| 60 | 3 | Axial skeletal anomaly | Cat Mus, p.90 | ||
| 61 | 4 | Cranial tumor | Obs Cent, p.50 | 25 | |
| 62 | 3 | Other generalized condition | Thes Anat VI, p.34 | ||
| 63 | 3 | Other generalized condition | Cat Mus, p.60 |
See text for category definitions.
Numbers refer to specimens in the extant collection.
Title codes are explained in Table I.
Acardiac Twin
Case 1
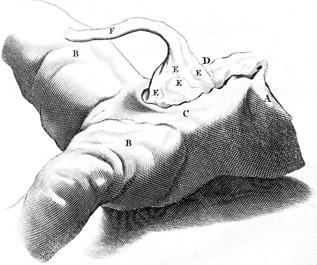
As part of his ninth cabinet (the 24th specimen) and in his second set of ten clinical remarks Ruysch described and depicted a placenta showing a marginally located protruding mass with an appended leg and foot with three toes (Fig. 5), delivered together with a healthy newborn [Ruysch, 1714, 1720]. Ruysch noted that inside the fatty tissue mass a femoral bone was present that was completely hollow. Only a thin cortex was noticeable with complete absence of spongious bone. Additionally, there was absence of any muscle tissue.
Figure 5.

Based on Ruysch's description, this case can either be diagnosed as an acardiac twin or as a placental teratoma. Following Fox and Butler‐Manuel [1964], it is generally assumed that acardiac twins have their own umbilical cord and vessels and a rudimentary axial organization, whereas placental teratomas do not. As it appears, however, none of these criteria is truly pathognomonic [Stephens et al., 1989]. Placental teratomas are often smooth surfaced, round or oval shaped with diameters ranging from 2.0–7.5 cm consisting of mature fat tissue, skin and skin appendices, bone and cartilage. Furthermore, placental teratomas are often marginally located on the placenta. However, each of these characteristics may also be applicable to acardiac twins. What made us incline to diagnose the latter condition is the well recognizable foot, the size of which is seemingly in accordance with the gestational age of the host twin. To the best of our knowledge fetiform structures have never been reported as part of placental teratomas.
Cleft Lip and Palate
Case 2
Ruysch described a miscarriage in which an immature child was seen with a split lip and palate. This description concerns the 52nd of his sixth cabinet and the first set of ten clinical remarks [Ruysch, 1705, 1717]. Ruysch stated that there was no need for grief when this child died, as it would have been born with a malformed lip and mouth, which was possibly a condition with a poor prognosis in the 17th century. Ruysch referred only once to this congenital anomaly, that we diagnosed as cleft lip and palate.
Congenital Tumors
Gastric teratoma
Case 3
In his third set of ten clinical remarks and as part of the second cabinet of his second collection (the 160th and 161st specimens), Ruysch described the case history of a man, presenting with a supra‐umbilical ulcerating lesion, who was admitted to the hospital in Semarang, Indonesia, on August, 15th, 1716 [Ruysch, 1723a, 1724]. The patient lived for an additional 4 months during which he received extensive treatment for his abdominal ulcer, including daily drainages of the opened ulcer. After the patient died, the body was dissected by the chief of surgery, Cornelis Smit. On exploration, the stomach was found to be filled with a white substance, a bundle of hair and two tissue masses, one attached to the cardia, containing skin covered osseous or cartilaginous structures and four well‐recognizable teeth (Fig. 6A). No other abnormalities regarding the autopsy were described, except for the liver, which appeared to be “putrid.” The specimen was donated to Ruysch by his friend and colleague Caspar Commelin (1668–1731), professor of exotic botany at the Athenaeum Illustre, together with a written statement, signed by all eyewitnesses who were present at the autopsy. Ruysch confirmed the description of Smit and additionally mentioned a finger‐like structure that he compared with the foreleg of a small hartebeest (Alcelaphus buselaphus), the nail of which resembled a human nail (Fig. 6B). The skin of the putative paw showed multiple fine little hairs resembling the skin of a human hand. Anticipating on the skepticism of his peers concerning the extraordinarity of this report, he published it together with Smit's statement, thereby defying any allegations of forgery.
Figure 6.
Case 3. Gastric teratoma, copperplate, presenting with (A) teeth and hair and (B) a nail‐bearing finger‐like protrusion. [Ruysch, 1723a, 1724].
We diagnosed this condition as gastric teratoma. At least part of the tumor appeared to have been located endogastrically, whereas the ulceration and subsequent fistulization may have been indicative for a proliferative exogastric component in response to an inflammation or a malignant degeneration. In this respect the “putrid” liver could be interpreted as hepatic metastases. Nails, in addition to hairs and teeth, are common findings in teratomas, and even nail baring finger‐like structures have been described, particularly in non‐ovarian teratomas [Dutz and Sadeghee, 1968], although their fetiform nature is disputed [Damjanov et al., 1983].
Intracranial teratoma
Case 4
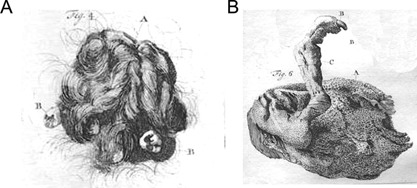
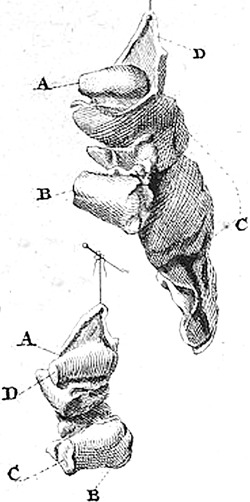
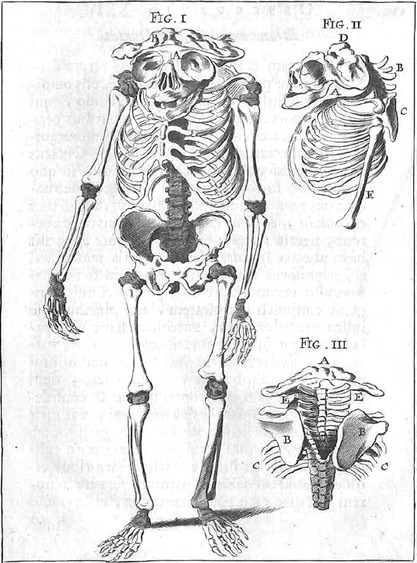
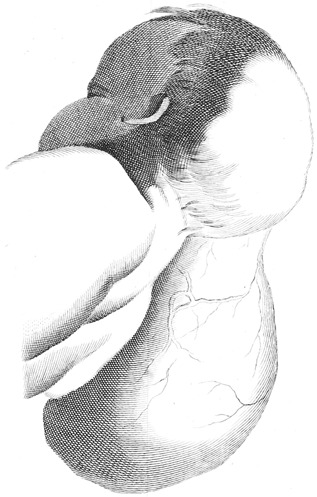
This case concerns the specimen of a male neonate with a grossly enlarged head (Fig. 7A and B), which was part of the second cabinet [Ruysch, 1702]. According to Ruysch, the child whom he considered to suffer from hydrocephalus, was born around 6 months of gestation. His assistance was requested by the midwife who conducted the delivery because expulsion was stagnant. Arriving at the scene, both the child and the placenta had nevertheless already been delivered but the uterine cavity was still occupied, according to the midwife. Subsequently, several shapeless, multi‐structured lumps of tissue were expelled in which Ruysch, much to his surprise, recognized remnants of no less than twenty miniature extremities without any other recognizable body parts. Ruysch separately bottled five of these tissue lumps (Fig. 7C and D), two of which have been identified in the extant collection.
Figure 7.
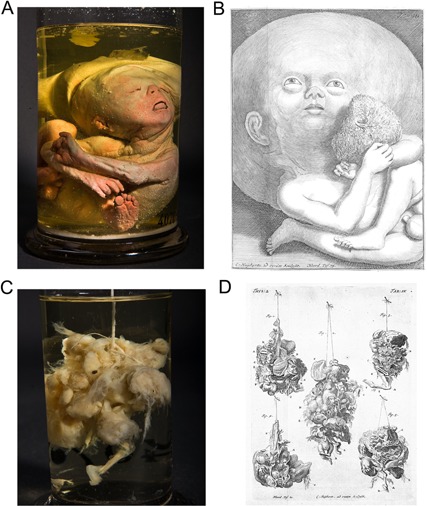
Case 4. Intracranial fetiform teratoma. (A) Specimens 4070–906: neonate with asymmetrical enlarged head. (C) Specimens 4070–672: detail of the teratoma, presenting with limb‐like structures. From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. (B, D) Copperplates. [Ruysch, 1702]. [Color figure can be viewed at wileyonlinelibrary.com].
Inspection of the child's head showed an asymmetrical sac‐like enlargement of the cranial vault, with a 3 cm wide roughly edged opening at the top of the sac. Deviating positions of hands and feet indicated that the child was probably stillborn. Apart from the reddish colouring of the skin, resulting from postmortem cinnabar containing vascular injections, no additional abnormalities were found. Inspection of the tissue lumps confirmed Ruysch's descriptions in detail: several more or less well‐formed arms and legs were recognizable among various ill‐definable tissue types. Some parts of the appendages were de‐fleshed, resulting from careless handling by onlookers during the delivery as Ruysch stated, but thereby showing that they contained skeletal elements resembling tubular bones. The size of these parts would have been in accordance with around 3 months of gestation, again confirming Ruysch's estimation.
The combination of multi‐structured tissue lumps and several limb‐like appendages, the size of which is not in accordance with the actual gestational age, is a strong indication for fetiform teratoma. Considering the consecutive expulsion of the child, the placenta and the tumorous tissue, we think that the latter originated from the sac‐like protrusion of the child's head, which ruptured during birth (hence the roughly edged opening), a mechanism that has been reported several times [e.g., Washburne et al., 1995; Bolat et al., 2008]. Subsequently, its contents were expelled in the uterine cavity. We therefore diagnosed this condition as intracranial fetiform teratoma.
Omental teratoma
Case 5
In the 18th of the 100 clinical observations Ruysch described the postmortem examination of a woman that he performed in 1683 and depicted the specimen that he subsequently obtained [Ruysch, 1691a]. Prior to her death the patient experienced a supra‐umbilical inflammation of the abdominal wall after she had been suffering from ascites for 15 years. Upon surgical relief of the ascitis, large quantities of clear fluid oozed out of the wound, both spontaneously and after repeated drainage. Although initially odourless, the fluid that was evacuated rapidly acquired an unbearable stench, which heralded her death 5 days later. At autopsy, Ruysch found a tumor as big as a fist, located in the major omentum and additionally attached to the peritoneum. The tumor consisted of a soft, non‐smelling, white substance as well as a substantial amount of matted and curled hair (Fig. 8). Ruysch found these hairs to be similar to those growing on a human head, which he concluded by microscopic examination, albeit that no roots were visible.
Figure 8.

Case 5. Omental teratoma, presenting with matted and curled hair, copperplate. [Ruysch, 1691a].
Fragments of the tumor became specimens in four different cabinets including the ninth specimen on the fourth shelf of his earliest cabinet, the 23rd specimen of the third anatomical cabinet, and the 74th and 106th specimens in the second and third cabinets of his second collection [Ruysch, 1691b, 1703, 1724; Anonymous, 1731]. We diagnosed the condition as cystic omental teratoma (dermoid cyst). The reported ascites may have resulted from malignant transformation of an initially benign tumor [Kubosawa et al., 2006], although this seems unlikely considering its longstanding existence. Alternatively, the ascites and the inflammation of the abdominal wall were caused by co‐occurring, unrelated conditions.
Ovarian teratoma
Case 6
A short case description of a 24‐year‐old woman who suffered from fever and complained about pain in the lower abdominal region is mentioned and depicted as the 17th specimen of the first cabinet [Ruysch, 1701b]. When Ruysch and his son (Hendrik Ruysch) opened the women's body after she had died, they both noticed a hardening of the left ovary. Subsequently, they dissected the dysmorphic ovary, finding four teeth‐like structures (Fig. 9). This report can be diagnosed as an ovarian teratoma.
Figure 9.
Case 6. Ovarial teratoma, presenting with four teeth, copperplate. [Ruysch, 1701b].
Umbilical angiomyxoma
Case 7
The third specimen in the ninth cabinet concerned a piece of an umbilical cord with a hardened tumor in it [Ruysch, 1714]. Because of its position quite proximal to the ventral wall of the otherwise healthy child, the midwife that conducted the delivery probably suspected an umbilical hernia, as Ruysch initially did, and she had cut the cord distal to the tumor. On dissection Ruysch found the tumor to contain solid structures and to be partially filled with a curious fluid‐like substance.
What Ruysch described seems to have been a true neoplasm of the umbilical cord, considering the solid and cystic components. The mentioned substance could be interpreted as degenerated Wharton jelly, which is indicative for haemangioma (angiomyxoma). Nevertheless a teratoma, although exceedingly rare, cannot be ruled out in the absence of histology [Iyoob et al., 2006]. One can easily understand Ruysch's initial assumption that the tumor was an umbilical hernia, considering the overall rarity of umbilical tumors and its superficial morphological resemblance to umbilical hernias, especially when located in close proximity to the umbilicus.
Conjoined Twins
Laterally conjoined twins
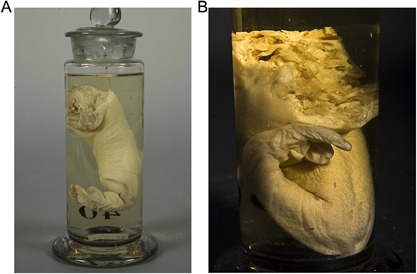
Case 8
This case concerns the embalmed and mummified body of a conjoined twin (Fig. 10A). According to Ruysch, who purchased the specimen from an unknown seller for his seventh cabinet, the applied embalming technique was quite different from his own [Ruysch, 1707, 1717]. This rendered the specimen very hard and stripped from its natural complexity. He described the specimen as a term neonate with two heads, three arms and two legs. External inspection confirmed this description. We diagnosed the condition as a laterally conjoined twin, more specific; dicephalus tribrachius dipus. We made the diagnosis laterally conjoined twins in three other specimens as well (Fig. 10B and C) none of which was described or mentioned in the CW (cases 9–11).
Figure 10.

Conjoined twins. (A) Specimen 4070–913: Dicephalus tribrachius dipus (case 8). (B) Specimen 4070–914: Dicephalus tribrachius dipus (case 10). (C) Specimen 4070–916: Dicephalus tribrachius dipus (case 11). (D) Specimen 4070–912: Thoracoileopagus tetrabrachius tetrapus (case 12). From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
Ventrally conjoined twins
Case 12
This case concerns the embalmed and mummified body of a conjoined twin (Fig. 10D). Ruysch described this specimen briefly in both his first and second sets of ten clinical remarks [Ruysch, 1717, 1720]. However, this specimen is not mentioned as part of any of the cabinets. According to Ruysch the twin were two prematurely born children joined together at the thorax and abdomen. It surprised him that women can actually give birth to conjoined twins vaginally and apparently survive. In this specific case Ruysch made a special arrangement with the parents in that they were allowed at all times to visit their children at his dwelling. External inspection confirmed Ruysch's description. We diagnosed the condition as a ventrally conjoined twin, more specific: thoracoileopagus tetrabrachius tetrapus.
Gastrointestinal Anomalies
Anorectal malformations
Case 13
In the second set of ten clinical remarks Ruysch described a male infant which was seen by him at home, dated August 1718 [Ruysch, 1720]. The affected child was suffering from an anal malformation in which the anus was closed by a very thin, round membrane. Behind this membrane, Ruysch noted the presence of meconium. After 5 days this membrane ruptured spontaneously and meconium oozed out. Unfortunately, the child died after a couple of days. No cause of death was identified. We diagnosed the condition membranous rectal atresia. Ruysch noted that this anomaly could have healed properly after incision of the membrane with a trocart.
Additionally, Ruysch mentioned two children with congenital absence of the rectum and external opening. Ruysch described that in one of them (case 14) surgeon Pieter Adriaanze pierced the skin at the place where the anus should be located. After piercing the skin the length of an entire small finger could be inserted before Adriaanze reached the intestine. Ruysch concluded that the entire rectum was absent. We therefore diagnosed this condition as rectal agenesis, apparently without fistula.
Hirschsprung disease
Case 15
Ruysch described a 5‐year‐old girl with an excessively dilated colon (“Enormis intestini coli dilatatio”) in the 92nd of his 100 clinical observations [Ruysch, 1691a]. This child complained of abdominal pain and constipation for a long time. All kind of remedies were tried, to no avail. When Ruysch opened the body of the child after its demise, he was astonished by the extent and size of the colon. Most other viscera were hidden under this dilated colon. Unfortunately, this case was not depicted. Although the clinical description is rather incomplete, it is generally assumed that this case report—which has been referred to multiple times in the literature—is the first cited case of aganglionic megacolon (Hirschsprung disease), thus leading to the eponym Ruysch disease (see Discussion).
Meckel diverticulum
Case 16
Ruysch described a dried piece of an ileum with a blind ending dilatation (Fig. 11) as part of his earliest collection and mentioned and depicted it again when describing a similar specimen (case 17) as part of his 7th cabinet [Ruysch, 1691b, 1707]. Ruysch noted that such a diverticulum mostly originated from the ileum although other part of the intestines could be affected as well. If the small intestines were located at the lower abdominal regions, these affected pieces of intestine could herniate into the inguinal region. As part of the second cabinet of his second collection Ruysch mentioned a third similar specimen (case 18) [Ruysch, 1724]. We diagnosed all three cases as Meckel diverticulum.
Figure 11.
Case 16. Meckel's diverticulum, copperplate. [Ruysch, 1691b].
Multiple liver cysts
Case 19
The 29th specimen in the seventh cabinet of the second collection concerned part of the liver of a new born child. According to the brief description, it presented with water‐filled vesicles [Anonymous, 1731]. Despite the paucity of information we are inclined to diagnose the condition as multiple liver cysts.
Holoprosencephaly
Case 20
The 74th specimen in the first cabinet of the second collection concerns a case description of a 3‐month‐old fetus with a snout‐like appendage, instead of a nose, which according to Ruysch resembled a male genital organ [Ruysch, 1728]. Ruysch referred to this case previously in the first set of clinical remarks [Ruysch, 1717]. Despite the paucity of details in this brief description we are inclined to diagnose the condition as holoprosencephaly (cebocephaly or ethmocephaly).
Hydatidiform Moles
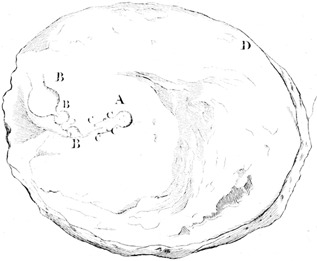
The CW contains at least four references (Mus Anat, p.93; Thes Anat III, p.11; Thes Anat VI, p.47; Thes Anat X, p.27) [Ruysch 1703, 1705, 1716] to specimens that, according to Ruysch, concerned placentas, together with their membranes and umbilical cords, that changed completely into grapelike water‐filled vesicles and sometimes proliferated to astonishing amounts (Fig. 12A). Three additional similar specimens (cases 21–23) were described as part of his second collection [Ruysch, 1724; Anonymous, 1731]. As he stated on several occasions throughout the CW (Obs Cent, p.34 and 43; Adv Dec II, p.32; Trac Anat, p.16) [Ruysch, 1691a, 1720, 1723b], he considered them to be the result of postpartum retained and subsequently degenerated, yet initially normal placentas. He claimed this to be demonstrated in placentas that were only partially vesicularized, of which he described four specimens. The extant collection contains six specimens of typical complete hydatidiform moles (cases 24–29), with or without parts of the uterine wall (Fig. 12B). Quite probably, these specimens overlap with the four CW references above (and perhaps with some of the less specific specimen descriptions as well) but a one‐on‐one matching is impossible since specimen‐specific features are lacking. Moreover, there are several other specimens with less typical characteristics of hydatidiform mole that could be partial moles but are more likely to be hydropic abortions. This also counts for the several partially vesicularized specimens mentioned by Ruysch. Convincing cases of partial moles were not found in the extant specimens collection.
Figure 12.
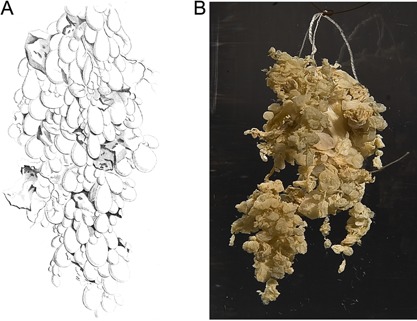
Hydatidiform moles. (A) Copperplate. [Ruysch, 1691b]. (B) Specimen 4070–674 (case 28). From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
Hydrocephaly
Case 30
The ninth and tenth specimen in Ruysch's earliest collection concern preparations of the septum pellucidum and part of the skull of an 8‐year‐old child who suffered from congenital hydrocephaly [Ruysch, 1691b]. Ruysch noted that the caudal end of the septum pellucidum was extended to the inferior parts of the brain and contained multiple perforations permitting flow of fluid between the ventricles. According to Ruysch the increase of fluid caused the amount of brain tissue to diminish and the sutures of the skull to widen at least the width of a finger. Interestingly, the ninth specimen in the third cabinet concerns a piece of brain derived from the same patient [Ruysch, 1703]. A second case of hydrocephaly concerns a 6‐month‐old fetus (case 31), being the 29th specimen in the ninth cabinet [Ruysch, 1714]. Ruysch used this specimen as part of a display of different natural products, such as corals, casts of blood vessels, bones and urinary‐ and bladder‐stones.
Limb Malformations
Case 32
This case concerns the specimen of a neonate with asymmetrical limb malformations, affecting all but one of the extremities (Fig. 13A and B). Ruysch had placed it in the back of the eighth cabinet, out of courtesy for his visitors, who might consider its appearance to be too confrontational [Ruysch, 1709]. He noticed that the right arm was bent markedly, and that the right hand only had three fingers. The right foot contained three toes: a deviating big toe and two normal toes. The left lower limb seemed to be lacking at all, apart from a slight elevation in the hip region. Furthermore, there was a tail‐like appendage attached to the abdominal wall. The left upper limb, as well as the head and body, showed no malformations.
Figure 13.

Case 32. Limb malformation with tail like appendage. Specimen 4070–907, (A) ventral and (B) dorsal views. From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
External inspection confirmed the observations done by Ruysch. In addition to the oligodactyly, the affected extremities were markedly shortened. The facial appearance, which we considered mildly dysmorphic, might have resulted from oligohydramnios but is probably a fixation and storage artifact. The reddish coloring of the skin resulted from postmortem cinnabar‐containing vascular injections. Undoubtedly, the most remarkable symptom is the tail‐like appendage. In combination with the otherwise nonspecific reduction defects, the only condition that comes to mind is disorganization‐like syndrome (MIM 223200). Profound investigation of the specimen, including imaging, would be necessary to confirm this diagnosis, but is unfortunately impossible. Limb malformations (presumably radial aplasia) with oligodactyly were present in two other specimens. These two specimens (cases 33 and 34) were upper extremities of neonates, neither of which was described or mentioned in the CW (Fig. 14A and B).
Figure 14.
Limb malformations. (A) Specimen 4070–039 (case 33). (B) Specimen 4070–908 (case 34). From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
Neural Tube Closure Defects
Case 35
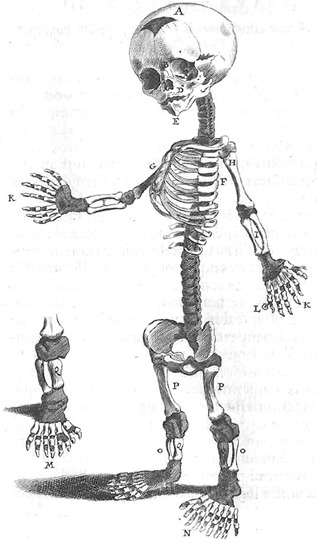
This case concerns the dried skeleton of a neonate (Fig. 15). Ruysch mentioned this specimen quite briefly in his first set of ten clinical remarks in the section on misconceptions but not as part of any of the cabinets [Ruysch, 1717]. It is one of the three specimens in his first collection of prematurely born children lacking a brain and a cranial cavity, according to Ruysch. Of the other two specimens, he skeletonized one (case 36, see further) and kept the other on embalming fluid (case 37). The latter one has apparently gone lost. On external inspection we confirmed Ruysch's description and found all vertebral arches to be intact. We diagnosed the condition as anterior neural tube closure defect (holoacrania).
Figure 15.

Case 35. Anterior neural tube closure defect (holoacrania), specimen 4070–915 From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
The first specimen of Ruysch's eighth cabinet concerned the dried skeleton of a prematurely born infant without a brain and a cranial cavity (case 36) [Ruysch, 1709]. Additionally, he found the cervical and upper thoracic vertebral arches to be cloven. At these levels the spinal cord was absent, whereas it was intact and well formed at lower thoracic and lumbar levels. Ruysch did not depict the specimen himself but instead referred to drawings made by his friend and colleague Theodor Kerckring (1638–1693), a Dutch anatomist and alchemist, who described and depicted this specimen in his Spicilegium anatomicum, a collection of 100 anatomical curiosities [Kerckring, 1670]. Based on the drawings (Fig. 16) and descriptions we made the diagnosis anterior neural tube closure defect (holoacrania with partial rachischisis).
Figure 16.
Case 36. Anterior neural tube closure defect (holoacrania with partial rachischisis), copperplate [Kerckring, 1670].
A fourth case of anterior neural tube closure defect (holoacrania with or without partial rachischisis) is found as the 24th specimen in the ninth cabinet of his second collection [Anonymous, 1731]. According to Ruysch it concerned a fetus that lacked a brain and a neck (case 38). It cannot be excluded that this case is the same as the embalmed specimen Ruysch referred to in the first set of ten clinical remarks, since this part of the CW was written after he had sold his first collection, and there seems to be no specimen in the first collection to which the description applies. On the other hand there are more specimens, including specimen 4070–915 (see above), that were not described as part of any of the cabinets of the first collection.
In the 34th, 35th, and 36th of his 100 clinical observations, Ruysch described five cases (although he mentioned to have seen at least ten) of one or more bifid vertebral arches whereas the vertebral bodies appeared morphologically normal (cases 39–43) [Ruysch, 1691a]. He found these defects to co‐occur with soft tumors of different sizes which were filled with clear fluid, interpreted by Ruysch as spinal cord tissue that changed into a water‐like substance. He compared this with the changing of neural tissue into water occurring inside the head, resulting in hydrocephaly. Most children that Ruysch encountered with this condition had paralyzed legs, could not be treated other than palliatively and died soon after birth, especially when the tumor was perforated. Ruysch therefore recalled the words of one of his anatomical predecessors in Amsterdam, Nicolaas Tulp (1593–1674), who founded the name “spina bifida” for this condition, to carefully handle the tumor and prevent it from being damaged [Tulp, 1641]. However, Ruysch observed two infants, one with a sacral lesion, who survived until her first year. Ruysch concluded that this relative long survival period may have been due to the low insertion of the tumor. Among the described observations of posterior neural tube closure defects, we diagnosed three cases of lumbar meningo(myelo)cele, two of which were depicted (Fig. 17), and one sacral meningo(myelo)cele. Additionally, Ruysch mentioned in the 34th observation a specimen of what seemed to have been a cervical meningo(myelo)cele, that supposedly was part of his earliest cabinet. However, none of the specimens in this or any other cabinet matched with that description.
Figure 17.
Case 40. Posterior neural tube closure defect (cystic spina bifida), copperplate [Ruysch, 1691a].
Skeletal Dysplasias
Ciliary chondrodysplasia
Case 44
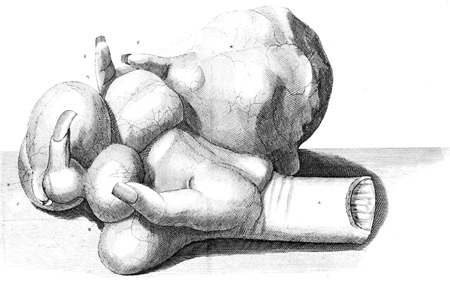
As part of his earliest collection, Ruysch mentioned the dried skeleton of a neonate, whose body was found floating in the IJ‐river in Amsterdam (Fig. 18) [Ruysch, 1691b]. It was brought to him for dissection by the city council. On examination Ruysch noted several peculiarities, including a disproportion between the head and the body, short limbs and supernumerary fingers and toes. The frontal fontanel was twice the expected size, the temporal bones were very small, the orbits were somewhat misshapen and the nasal bones were broad and depressed. There was a small median cleft in the upper jaw, whereas the lower jaw showed a median crest‐like elevation, absence of the mandibular symphysis and bony protrusions of the rami. Some teeth were already erupting. The thorax showed very short ribs, small shoulder blades and a little sternum. The tubular bones of all extremities were very short, their length not exceeding the width of one or two fingers. The right hand had seven complete fingers, the left hand six, with a round appendage on both the thumb and the 5th finger. The right and left feet contained eight and nine toes respectively. He referred to this specimen additionally in his first set of ten clinical remarks [Ruysch, 1717] where he stated that there is a certain size or measure in all things: if nature creates things in abundance like supernumerary fingers and toes, this is often useless and prejudicial. Finally, he noticed several carpal, tarsal and metatarsal ossicles in both hands and feet. Ruysch did not depict the specimen himself but again referred to drawings made by Theodor Kerckring for his Spicilegium Anatomicum [Kerckring, 1670]. Interestingly, although Kerckring gave an equally detailed report of his own examination, these findings differ slightly from those made by Ruysch, especially regarding the lower limbs. He noticed the tibiae to be equally thick to the femora, with cartilage on either site. Unfortunately, neither of the reports includes any soft tissue characteristics.
Figure 18.
Case 44. Ciliary chondrodysplasia (Majewski syndrome), copperplate [Kerckring, 1670].
This case has been referred to several times in the literature (see Discussion), in most instances understandably, but erroneously, assigned to Kerckring. Inspection of Kerckring's images largely confirms the reported findings. The drawing of the skull implies a short cranial base, relative bulging of the forehead, mild hypertelorism, a broad and depressed nasal bridge and a small medial cleft of the maxilla. The polydactyly of most extremities appears to be of both pre‐ and post‐axial nature, with both proximal and distal duplications. The detailed drawing of the right leg suggests that the tibia was significantly shorter than the fibula and somewhat ovoid in shape. The combination of very short ribs and limbs, polydactyly and apparent neonatal death is very suggestive of a lethal skeletal dysplasia, in this case a ciliary chondrodysplasia (short‐rib thoracic dysplasia/short‐rib polydactyly syndrome). Most findings, including the median cleft, the severe shortening of the ribs and the limbs, the mixed polydactylies and the dysplastic tibiae, are in line with Majewski syndrome (SRTD6, SRPS2, MIM 263520) although the cranial dysmorphology (except for the median cleft) is more suggestive of Verma‐Naumoff syndrome (SRTD3, SRPS3, MIM 613091). Neonatal teeth have been reported occasionally in various ciliary chondrodysplasias [Koppang et al., 1983].
Enchondromatosis
Case 45
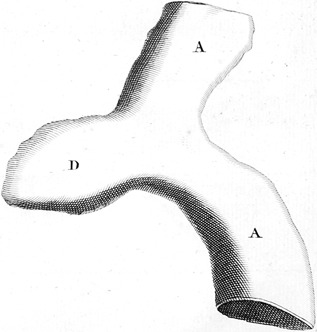
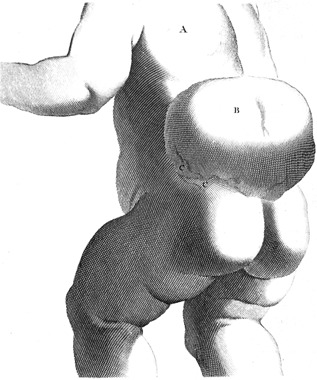
Corresponding with his well‐acquainted colleague Mauritius van Reverhorst (1666–1722), medical doctor and professor of anatomy and surgery at the Leiden University, Ruysch described the amputation of the left forearm in a 16 years old male [Ruysch, 1701a]. The patient was suffering from large tumors in his hands and, to a lesser extent, in his feet. The tumors appeared small at the time of birth but steadily grow over the years to such proportions that especially his left hand became merely a useless, increasingly painful hindrance that he had to support with his other hand because of its weight. Damage to the hand and infection were repeatedly followed by excessive bleeding of one of the tumors. Ruysch considered the shape of the tumors, most of which were solid and very hard, to resemble that of potatoes, tubers of cyclamens or roots of chrysants. Interestingly, the mother of the patient admitted that she found chrysant roots (Chrysanthemum spp.) very tasteful and she had been eating them abundantly during the pregnancy. After the amputation, which was post operatively complicated by infection, progressive inflammation and phantom limb pain, Ruysch examined and depicted the hand (Fig. 19) and opened one of the tumors at the request of Van Reverhorst. It appeared to contain numerous cartilaginous proliferations, some perhaps even osseous, together with mucous‐filled spaces.
Figure 19.
Case 45. Enchondromatosis, copperplate [Ruysch, 1701a].
Although Ruysch stated that he would keep the hand for future examination, it was never admitted to his collection as a specimen. The pictures of the grossly deformed hand suggest that most of the tumors originated from the metacarpals and proximal phalanges. The overall presentation of the condition, the medical history and the cartilaginous nature of the tumors are quite suggestive of enchondromatosis (MIM 166000). If the repetitive and excessive bleeding of one of the tumors is to be interpreted as a haemangioma, Maffucci syndrome (MIM 614569) would be the most probable diagnosis, although metachondromatosis (MIM 156250) cannot be ruled out, if there were truly osseous tumors present as well.
Urogenital Anomalies
Disorder of sex development
Case 46
In the eighth cabinet and the 18th description of the first set of 10 clinical remarks Ruysch reminisced to have seen several cases of “man‐wives,” although he stated never to have encountered true hermaphrodites, having both testicular and ovarian tissue, and he discarded reports of alleged cases as pseudohermaphroditism [Ruysch, 1709, 1717]. The only case Ruysch actually described concerns a 24‐year‐old individual with ambiguous genitalia. Although this person had a male facial appearance and claimed to be a heterosexual male, the phallic organ lacked a urethral orifice, which made Ruysch conclude that she was a female. He considered persons like this one to be incapable of reproduction because the sexual organs of either sex were not completely developed. Additionally, two testicle‐like organs were located in the groin area but Ruysch assumed that they were little more than lumps of fatty tissue, as he had experienced from the dissection of a sheep with a similar condition. We diagnosed this condition as a disorder of sex development. Since the secondary sex characteristics and the internal sex organs were not described it is impossible to be conclusive on the precise diagnosis. Depending on the nature of the gonads both congenital adrenal hyperplasia and partial androgen insensitivity syndrome seem likely.
Fallopian tube duplication
Case 47
In the 83th specimen of the fourth cabinet Ruysch described the presence of three Fallopian tubes [Ruysch, 1704]. He stated that this was the only case of multiple Fallopian tubes he had ever seen, although he mentioned that it was possible that both Fallopian tubes were absent, and that unilateral absence occurred as well. This short case can be clearly interpreted as fallopian tube duplication.
Hypospadias
Case 48
This case concerns a specimen of the distal part of a penis presenting with a slit‐like urethra orifice at the caudal aspect of the glans, which we diagnosed as distal hypospadias (Fig. 20). Although Ruysch stated to have encountered several patients in which the external urethral meatus was not located at the normal place and referred to these patients when describing similar conditions in animal specimens [Ruysch, 1691b, 1709], no descriptions of any human specimens were found. According to Ruysch urethral malposition caused infertility because the expulsion of the sperm was not in line with the cervix of the uterus.
Figure 20.
Case 48. Hypospadias, specimen 4070–600. From the collection of the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences. [Color figure can be viewed at wileyonlinelibrary.com].
Imperforate hymen
Case 49
Ruysch described a case of a 20‐year‐old virgin who complained of agonizing cyclical abdominal pain in the 32nd of his 100 clinical observations [Ruysch, 1691a]. With the help of obstetrician Andries Boekelman, Ruysch concluded that this re‐occurring illness was due to an intra‐vaginal membrane which covered the entire vaginal opening. After incision in this membrane, which turned out to be curative, a vast amount of black non‐clotted blood was expelled, weighting around four pounds. We diagnosed the condition as haematocolpos resulting from an imperforate hymen.
Transverse vaginal septum
Case 50
Ruysch described a case of an obstructed labor in which an intra‐vaginal hymen and a thick concomitant vaginal membrane arrested delivery of the child. He described this case in the 22nd of his 100 clinical observations [Ruysch, 1691a]. During examination of the woman in labor Ruysch noticed an elongated hymen which appeared to be the reason for the stagnant delivery because it was pressing on the child's head. Obstetrician Andries Boekelman and surgeon Pieter Adriaansz assisted Ruysch to surgically remove this hymen. After the surgical procedure another thick membrane was noticeable, again causing a stagnant delivery. Therefore, the second membrane was cut as well, and a healthy newborn was delivered. Ruysch stated that it was possible to become pregnant with a remaining hymen. Interestingly, he thought that the second membrane had arisen after intercourse. This clinical case can be interpreted as a transverse vaginal septum (Fig. 21). Pregnancy in the presence of a seemingly intact hymen can occur due to a micro perforation in the hymen [Goto et al., 2006]. However, concomitant occurrence of a micro perforated hymen and a vaginal septum is very rare.
Figure 21.
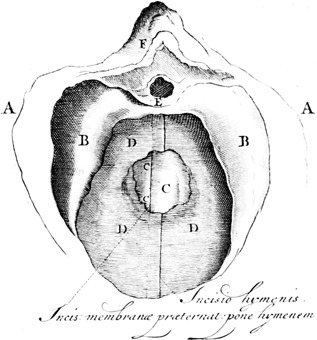
Case 50. Transverse vaginal septum, copperplate [Ruysch, 1691a].
Ureteral duplication
Cases 51–54
The CW contains at least four references to cases and specimens that, according to Ruysch, concerned ureteral anomalies (Fig. 22) [Ruysch, 1665, 1691a, 1707]. Ruysch described both complete duplication of the ureters as well as ureters which unite before entering the bladder. These four cases were diagnosed as (partial) ureteral duplications.
Figure 22.
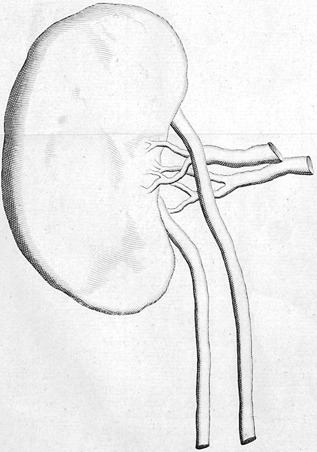
Case 53. Ureteral duplication, copperplate [Ruysch, 1691a].
Ventral Body Wall Defect
Bladder exstrophy
Case 55
In the 23rd of his 100 clinical observations Ruysch described the examination of a 6 days old girl that was born with a malformation of the ventral body wall [Ruysch, 1691a]. The external genitalia seemed to have merged with the umbilicus, thus creating a disorganized mass of tissue with several eminences. In the caudal part of the defect two openings were seen from which urine was continuously oozing, especially when the child cried. No bladder or urethra could be recognized. Additionally, Ruysch asked himself, without giving an answer, whether this anomaly could have been caused by a falling accident that the mother experienced a few weeks before the delivery. The description, as well as a picture of the defect (Fig. 23), fit completely with the diagnosis vesical exstrophy. Ruysch apparently did not recognize the infra‐umbilical tissue mass as being the muscular folds on the inner side of the open and everted bladder wall. The mentioned openings are the ureteral orifices.
Figure 23.
Case 55. Bladder exstrophy, copperplate [Ruysch, 1691a].
Omphalocele/gastroschisis
Cases 56–58
In his 71st, 72nd, and 73rd observations of his 100 clinical observations Ruysch described three cases of ventral body wall defects [Ruysch, 1691a]. In observation 71 Ruysch mentioned the absence of the abdominal skin and muscles around the insertion of the umbilicus (Fig. 24). The intestines, as well as intestinal peristalsis, could be seen through a thin umbilical membrane. Ruysch stated that he encountered this anomaly rather often. However, he never saw recovery and all the affected children died a couple of days after birth. According to Ruysch the term “umbilical hernia” for this condition was chosen incorrectly since there was no true umbilicus noticeable. Instead, there was an outpouching of the peritoneal membranes. We diagnosed this case as an omphalocele. Additionally, in the 73rd observation Ruysch mentioned one other case of omphalocele.
Figure 24.
Case 56. Omphalocele, copperplate [Ruysch, 1691a].
In his 72nd observation Ruysch described a neonate that was born with its stomach, intestines and spleen located outside its body. In this case, the organs, which bulged through the abdominal wall, were not covered with a membrane. The child lived for a couple of hours, and peristaltic movements of the bowel were noticeable during the short life of the newborn. Ruysch described that these abdominal wall defects were caused by the absence of the abdominal skin and muscles, and not by assumed obstetric malpractice. Unfortunately, Ruysch did not mention anything about the absence or presence of the umbilicus or umbilical cord. With the present information we are inclined to diagnose this case as gastroschisis.
Indiscernible Conditions
Axial skeletal anomalies
Case 59
In the first of the 26 clinical reports that were part of his treatise on vascular valves, Ruysch described the bilateral presence of thirteen ribs in a girl who died of cachectic fevers, with two rib pairs being fused [Ruysch, 1665]. Unfortunately, the brief report does not reveal any details about the nature and location of the rib “fusion,” especially regarding the question whether it concerned true fusion (e.g., bridging) or (forked) duplication, nor does it contain any information on the number of (thoracic) vertebrae, or any concomitant anomalies. The differential diagnosis therefore ranges from bifid rib conditions, either isolated or syndromic (e.g., Gorlin–Goltz syndrome), to fused ribs as part of meristic or homeotic segmentation defects of the axial skeleton. If the latter were the case, the cachectic fever that Ruysch mentioned, could be the expression of an end‐stage childhood malignancy, which are known to co‐occur frequently with abnormal rib counts [Schumacher et al., 1992; Merks et al., 2005; Loder et al., 2007]. A comparable description is found in the auction catalogue of the second collection, regarding the 144th specimen in the fourth section of the ninth cabinet [Anonymous, 1731]. It refers to a specimen of two ribs that, according to Ruysch, are congenitally fused (case 60). Since no other information is given a diagnosis cannot be made.
Cranial tumors
Ruysch described several cases of cranial tumors of the occipital and parietal region, often bigger than the head itself, sometimes even bigger than the child. One of these cases (case 61) was described in the 52th of his 100 clinical observations [Ruysch, 1691a]. These tumors were likely to result in problematic labors and peri‐natal deaths. When the tumors were opened they were often filled with fluid, having the same aspect as the fluid present in the ventricles of the brain, but sometimes they appeared to contain more solid, even cartilaginous tissues. The figure that accompanies the observation shows a large parietally located cranial tumor (Fig. 25). Based on the description Ruysch gave of these tumors, the depicted case cannot be diagnosed properly. It is possible though that Ruysch wanted to give an impression of the size of growth of these occipital tumors, without depicting a specific type.
Figure 25.
Case 61. Cranial tumor, copperplate [Ruysch, 1691a].
Other generalized conditions
Case 62
The 53rd specimen of the sixth anatomical cabinet concerns a very short description of a specimen in which Ruysch described a premature stillborn child with curved arms, hands and feet [Ruysch, 1705]. Ruysch imagined that this child would have had a very miserable life if it had been born alive. Considering the bowing of long bones of all extremities campomelic dysplasia or osteogenisis imperfecta could be considered, among other diagnoses. With no further information this case cannot be diagnosed properly and stays indefinite. The 13th specimen of the fifth cabinet of the second collection is described without any additional information as a monstrous fetus of about two inch length (case 63), which makes the condition entirely indeterminable [Anonymous, 1731].
DISCUSSION
It is generally accepted that the Ruysch collection residing in Saint Petersburg is the first of its kind. Although Ruysch's predecessors and contemporaries were familiar with preparation techniques such as embalming, maceration, corrosion and injection, the magnitude, versatility and reputation of his collection was unprecedented. In the subsequent decades Ruysch became a shining example for ambitious anatomists that aspired a specimen collection of their own, not merely for scientific purposes but mainly to amaze and impress their friends and colleagues. Following the heydays of the private anatomical and naturalia collections in the mid‐18th century, a gradual shift took place towards institutionalized collections, that focused on systematic rather than anecdotally collected morphology specimens. Collections like these, primarily meant for the instruction of (bio)medical students and professionals, have been operational up to the present day in many medical schools around the world. What remained, however, is the (partly sensation‐driven) fascination of lay people with human anatomy, which is what Ruysch experienced at the time when making his cabinets publically accessible and what makes exhibitions of plastinated anatomical specimens, such as Günter von Hagens' “Body Worlds” so successful 300 years later.
Until the mid‐20th century it was unknown to Western Europe whether the collection of Frederik Ruysch, or the remains of it, still existed. Publications regarding the collection, including the mid eighteenth century Latin catalogue [Anonymous, 1742] apparently went unnoticed by Western European scholars. According to the German anatomist Josef Hyrtl (1810–1894) both the first and second collections had gone lost in their entirety [Hyrtl, 1860]. He insinuated that the sailors, who shipped the specimens of Ruysch to Saint Petersburg, drank the alcohol‐based embalming fluid from the bottles, leaving the collection in a deplorable state [Hyrtl, 1869]. This entirely fictive assumption subsequently became a tenacious legend that has persisted up to the present day. As it appeared, however, successive Russian curators took well care of the Ruysch collection although they could not prevent a gradual decline in the number of preserved specimens, from around 1,500 specimens in 1808, 1,350 in 1843, 1,086 in 1903, down to 935 in 1947 [Ginzburg, 1953]. Presently, the 916 specimens that survived are constantly being monitored by a team of curators and renovated when necessary.
During the analysis of the extant collection we came across quite a few specimens, both teratological and otherwise, that could not be matched with any of the descriptions, not because they lacked distinctive characteristics (like the hydatidiform moles) but because they had them, without any of the specimen descriptions being applicable to it. An example of this concerns case 35. In the first set of ten clinical remarks Ruysch almost incidentally mentioned a second skeletonized fetus with an anterior neural tube closure defect, yet none of the cabinet inventories (of both the first and the second collections) listed a specimen to which this description could be applied. This proofs that the collection purchased by Peter the Great contained an unknown number of non‐described specimens, which at the time was confirmed by the earliest curators of the collection in Saint Petersburg [Ginzburg, 1953]. In addition to that, Russian anatomists, inspired by Ruysch's preparation techniques, made specimens of their own [Ginzburg, 1953] and it is conceivable that in the course of time they became incorporated in the Ruysch collection, for example, to replace specimens that had gone lost.
Considering the modest size of Ruysch's teratological legacy, it contains a surprisingly high number of exceedingly rare conditions, especially concerning congenital tumors. Intracranial teratomas (like case 4) have a reported incidence of 0.43 in one million [Washburne et al., 1995] with only a fraction of those presenting with fetiform structures. In fact, intracranial teratoma with fetiform remains of multiple individuals, as presented in Ruysch's case, has been reported only twice [Kimmel et al., 1950; Naudin ten Cate et al., 1995]. Gastric teratoma (case 3) accounts for less than 1% of all teratomas in childhood [Cairo et al., 1981] with a 161 reported cases [Ukiyama et al., 2005]. Only five cases concern adult individuals [Gray et al., 1964; Liu et al., 2009]. Omental teratoma (case 5) has been reported in only 31 cases since 1928 [Chen et al., 2008]. Clearly, Ruysch was highly impressed by the shaping powers of nature that could result in tumors containing hairs, teeth, nails and parts of extremities. However, the underrepresentation of more common and explicit congenital conditions, such as cleft lip/palate, limb reduction defects and neural tube closure defects in his collections, may also be a reflection of Ruysch's personal preferences and assumptions. In the description of a neonate with cleft lip and palate (case 2) Ruysch mentioned that he was reluctant to show his visitors frightening specimens like these, unless they insisted. He considered them to be unfit for exposition and should best be buried instead of disharmonizing a fine anatomical exhibition. The purpose of his specimens was to impress his visitors with the beauty of the human body and its tissues and he considered overt “monstrosities” to be in dissonance with this concept, which is why he stored them in the back of his cabinets and is what may have withheld him from proactively collecting this type of specimens. This could account for the fact that, for example, spina bifida, despite being one of the most common malformations and encountered by Ruysch at least ten times, is not represented at all in his collections.
Moreover, Ruysch was aware of the fear among pregnant women to be confronted with congenital anomalies. According to the maternal imagination theory, which was still a well‐grounded conception in the 17th and 18th century, this could be harmful to the unborn child. Ruysch considered this opinion not his to criticize and kept a distance to any verdicts. Although it seems unlikely that Ruysch assumed normally developing fetuses to be susceptible to maternal imaginations, he certainly considered this to be possible with respect to the moment of conception. In the second set of ten clinical remarks Ruysch stressed the importance for parents to explain them the difference between a “monstrosity” and a macerated but otherwise well‐formed fetus, since the latter should be much more comforting to them and would prevent the mother from having falsely induced, yet harmful memories during subsequent procreations [Ruysch, 1720].
Although admired by friend and foe alike for the beauty of his preparations and his skills in vascular injection, his academic contributions to the medical science were disputed already during his lifetime and shortly thereafter. According to Ginzburg [1953] George Cuvier (1769–1832) was his most important proponent and was marveled by all his works, whereas Karl Ernst von Baer (1792–1876), who admired his specimens was not at all impressed by his scientific output. Hyrtl, who erroneously assumed both Ruysch collections had completely gone lost, had no sympathies for Ruysch's legacy whatsoever and considered his injection specimens to be short‐lived artifacts resulting from a destructive technique and worthless for detailed histological investigation [Hyrtl, 1860]. Nevertheless, Ruysch did some important anatomical discoveries including the valves of the lymphatic vessels, the intestinal lymph nodes, the “vasa vasorum” and the bronchial arterial system. Regarding congenital anomalies, Ruysch displayed a certain modesty. Roughly a century after Vesalius, he must have realized that science was not capable yet of giving adequate answers to all the questions that his teratological specimens generated. Perhaps this is why he dedicated himself to careful descriptions rather than to speculative interpretations and bold opinions and to all sceptics he stated that nature can create all sorts of marvelous things, thereby inviting them to come to his dwelling and see it with their own eyes. This does not mean that he refrained from contributing to the current debates on embryological and teratological topics.
One of these topics was superfetation, the process of ovulation and fertilization during an intact pregnancy resulting in two conceptuses of different developmental stages [Roellig et al., 2011]. In the fourteenth of his 100 clinical observations and as 120th specimen of his sixth cabinet Ruysch described a case, dated 1686, of a pregnant women who gave birth to a healthy newborn. Six hours later, she delivered a small fetus of around 3 months gestation (Fig. 26) [Ruysch, 1691a, 1705]. Ruysch initially found the placenta to be unusually large and thick considering the gestational age but as he later admitted this enlargement merely concerned clotted blood. Furthermore, the umbilical cord had changed into a concatenation of fluid‐filled vesicles. According to Ruysch, the finding of a second concomitant and discordant conceptus was evidence for superfetation. The phenomenon of (alleged) superfetation has been abundantly reported in previous times. Gould and Pyle mentioned Ruysch's description and recalled at least thirty other cases, some dating back to classical times [Gould and Pyle, 1896]. Although true superfetation is known to occur in several mammalian species, either frequently or occasionally, it seems extremely rare in humans and its unequivocal existence has yet to be proven [Roellig et al., 2011]. In most cases of alleged superfetation other causes of discordant development between two (or more) fetuses seem much more probable (or at least cannot be ruled out), such as superfecundation (successive fertilizations of two or more oocytes originating from a single ovulation), delayed nidation (timing differences in implantation of two or more zygotes), growth discordance in multiple pregnancies due to placental insufficiency or twin to twin transfusion syndrome, and pre‐ or immature death of a twin sib [Baijal et al., 2007; Roellig et al., 2011]. From Ruysch's description, it seems very likely that the latter was the case. Although not mentioned as such it seems certain that the fetus died long before birth, considering the gestational discrepancy, the hydropic degeneration of the umbilical cord, and the placental hemorrhage, which in first trimester pregnancies has an increased risk of fetal death [Maso et al., 2005].
Figure 26.
Discordant twin fetus, presenting with vesiculated umbilical cord and enlarged placenta, copperplate [Ruysch, 1691a].
Another phenomenon Ruysch, in his profession of chief obstetric instructor, was confronted with is what in the Latin text of the CW is named “mola,” which literally means mass or lump. Confusingly, this did not refer to a hydatidiform mole (“mola hydatidosa”) but to a post‐partum intrauterine residue. In the Dutch text it was dubbed “zuyger,” which would translate to “sucker,” referring to its alleged parasitic lifestyle. Nevertheless, the English translation of this text mentioned the Latin “mola” [Ruysch, 1751]. According to the midwives instructed by Ruysch, these “molae” literally had a life of their own in that they supposedly were able to travel through the room and crawl inside other women via the genitalia to find shelter. Although Ruysch considered these stories to be utter nonsense and exemplary for the general ignorance of the midwives he instructed, he was curious as to what process or phenomenon could underlie these myths. In the 28th and 29th of his 100 clinical descriptions Ruysch suggested that prolonged retained placentas and placental rudiments could be the source of these confabulations [Ruysch, 1691a]. According to Ruysch retained placentas could stay in the uterus for a couple of months without being harmful. By naturally occurring uterine contractions these remnants would be reduced to the size of a chicken egg, reside in the womb during a successive pregnancy and subsequently appear at delivery. As a result of the prolonged compressed state these remnant could take any kind of shape, including that of a frog or another animal. What Ruysch failed to explain however, is the basis for the alleged physical activity of these creatures. Based on his descriptions, we propose that the mythical origin of crawling or flying frog‐like “molae” lies in unexperienced observations of fetuses born with an anterior neural tube closure defect. It is conceivable that the dramatic presentation of an acraniate and neckless fetus with bulging eyes gives the impression of a frog, especially to ignorant lay people. Anencephalic infants, most of which are born alive and die within a day [Pelizzari et al., 2015], have been reported to show bursts of forceful, jerky and sometimes excessive movements—especially those lacking a brain stem—that are quite unlike normal fetal motion patterns [Visser et al., 1985]. Again, in the eyes of ignorants these movements may impress as attempts to crawl or fly.
During the process of re‐diagnosing the conditions that Ruysch described and depicted, we assumed that the pictures in the CW were accurate representations of the anatomized preparations and case reports, which he described in such great detail that we could make (differential) diagnoses on most teratological descriptions without any significant discrepancy between reality and the depicted figures. Corresponding with Bartholomaeus Keerwolf, Ruysch expressed his dismay for the lack of detail his peers showed for the characteristic morphology of the left cardiac auricle and admitted that a heart which he wanted to be depicted was drawn differently from what the anatomical specimen actually looked like [Ruysch, 1697]. According to Ruysch, this was mainly due to the multitude of steps which were initiated to create anatomical drawings. However, he did not mention any mistakes in the drawings of the teratological samples.
Several of Ruysch's specimens and case descriptions subsequently re‐appeared in the medical literature, most of them referring to conditions not previously attested. Most contemporary authors consider Lebert to be the first one to have described omental teratoma in 1734. However, the German pathologist Hermann Lebert (1813–1878), who lived almost a century later, actually referred in his paper on dermoid cysts to the French translation of the case described by Ruysch (case 5) [Lebert, 1852; Lannelongue and Achard, 1886; Mumey, 1928]. James Ewing also referred to Ruysch's omental teratoma in his text book on tumors [Ewing, 1919]. The earliest report of gastric teratoma is generally ascribed to Eustermann and Sentry [1922] although already Lebert in 1852, Lannelonge and Achard in 1886 and Gould and Pyle in 1896 referred to Ruysch's description of case 3 [Lebert, 1852; Lannelongue and Achard, 1886; Gould and Pyle, 1896] and Geyl in 1897, with inclusion of the case report and Ruysch's considerations [Geyl, 1897; Bandler, 1901]. Ruysch's description of enchondromatosis (case 45) was referred to by Johannes Müller in 1838 [Müller, 1838; Johnson and Johnsen, 1840], whereas Ollier's description of the disease dates from 1890 [Ollier, 1890]. Ruysch's case descriptions of Meckel diverticulum (cases 16–18), which date from a century before that of Johann Friedrich Meckel the Younger, are also often referred to. Meckel himself, who was the first to realize the developmental nature of the condition, referred to many preceding case reports, including Ruysch's, to whom he ascribed the preponderant ileal location [Meckel, 1809].
Interestingly, Ruysch's well documented and depicted case report of an intracranial teratoma (case 4), although often referred to, has never been diagnosed as such prior to our investigations but instead has always been considered a case of hydrocephalus. The first published description of an intracranial teratoma originates from one and a half century later [Breslau, 1864]. Ruysch's brief and incomplete description of aganglionic megacolon (case 15) [Ruysch, 1691] let to the eponym “Ruysch disease” since it is generally accepted that this case report is the first attested case in pre‐modern medicine [Jayle, 1909; Leenders and Sieber, 1970], almost two centuries prior to that of Hirschsprung [1888]. Strangely enough, therefore, one of his most sparsely documented case report is the one he became famous for. Possibly, this resulted from the relative inaccessibility of Ruysch's works, which were almost exclusively published in Latin and Dutch. The only exceptions to that are the French and English translations of his 100 clinical observations, which include this very case.
One of the other descriptions in the Ruysch legacy that has been frequently referred to concerns the specimen of a neonate with a polydactylous chondrodysplasia, described by both Ruysch and Kerckring (case 44). The earliest known reference is that of Jonathan Hutchinson, who reproduced the drawing of Kerckring in his Archives of Surgery [Hutchinson, 1893; Gould and Pyle, 1896; McKusick et al., 1964]. He recalled Kerckring's description and showed himself particularly struck by the fact that the dwarfing condition in this case was associated with polydactyly. This convinced him that the nature of this condition was entirely different from that of rickets, which at the time was the default diagnosis for any acquired or congenital shortness or bowing of limbs. In 1940, Nicholls wrote a biography on Theodor Kerckring and referred to the case without mentioning Ruysch's involvement, even though he stated Kerckring to be well acquainted with Ruysch [Nicholls, 1940]. In the same year, Ellis and Van Creveld described three cases of a polydactylous chondrodysplasia that would subsequently bear their names. They stressed the resemblance between Kerckring's description (again without mentioning Ruysch) and the phenotype of their own cases and since one of these originated from Amsterdam, they even speculated “whether it was entirely coincidence that this child should have been described in the same city as that in which case 2 of the present series was observed many generations later” [Ellis and Van Creveld, 1940]. Finally, in 1971, Majewski and co‐workers recalled several historical descriptions, including the one by Kerckring, that resembled their own cases [Majewski et al., 1971], which was confirmed by Spranger and co‐workers, in their paper on short‐rib polydactyly syndromes [Spranger et al., 1974]. Although Majewski syndrome still seems the best fitting diagnosis, our analysis of Ruysch's and Kerckring's descriptions illustrates the considerable phenotypic overlap that is contemporarily encountered among the various ciliary chondrodysplasias, that is, the short‐rib polydactyly syndromes [Elçioglu and Hall, 2002; Huber and Cormier‐Daire, 2012; Schmidts, 2014].
Soon after Ruysch sold his first collection to Peter the Great, he started collecting anew, despite being already in his seventies. As stated previously, the auction catalogue that was published after his death in 1731 listed almost 1,300 indexed specimens [Anonymous, 1731]. In addition to the teratological specimens that were part of the first two cabinets of the second collection—described in the CW as the Curae—the subsequent cabinets added to this collection contain only five specimens that unequivocally represent a congenital anomaly and only two of those could be adequately diagnosed. In several other cases however, a congenital condition was suspected but could not be diagnosed with sufficient certainty. For instance, Ruysch described three specimens of newborn children that were “beraved from their brains” without clarifying if this was the reason for dissection or the result of it. The general assumption is that when this second collection was auctioned, it was acquired by the Polish king, Friederich August I, who bought it for 20,000 guilders [Haller, 1774]. His son, Friederich August II supposedly donated the collection to the University of Wittenberg, where it came in the custody of the anatomist Abraham Vater [Schwarz, 1999; Kooijmans, 2004].
Although selling the whole collection, or most of it, to the Polish king may have been Ruysch's intention, it probably never happened. Ginzburg, head of the anthropology department of the Kunstkamera in the middle of the 20th century, casted doubt when he realized that only 5 years after Ruysch had died no more than 59 of the original 1,300 specimens turned up in the museum inventory of the University of Wittenberg [Vater, 1736] and he considered it unlikely that they were bought for 20,000 guilders [Ginzburg, 1953]. Since Vater was a colleague and friend of Ruysch, with whom he corresponded on various anatomical issues, it seems reasonable to assume that he bought the specimens himself or on behalf of his university, without any royal intervention. What remained over time of this sub‐collection must have been transported to the University of Halle upon its fusion with the University of Wittenberg in 1817 but a recent inventory did not surface any remaining Ruysch specimens [Schwarz, 1999]. Specimens of Ruysch's second collection also turned up in the auctioned legacies of other colleagues, including Seba, Gaubius, Deknatel and Houttuyn [Anonymous, 1751, 1765, 1783, and 1787] but the present status and whereabouts of these specimens is unknown. Searching for the remains of these cabinets and their specimens could be the next step in this historical quest of unraveling and revealing the entire Ruysch legacy.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the help of Prof. Yuri Chistov (Director), Dr. Natalia Kopaneva, and Mrs. Olga Panarina for their cooperation and providing all the possibilities to investigate the extant collection in the Peter the Great Museum of Anthropology and Ethnography (Kunstkamera) in Saint Petersburg, Russia. Furthermore, we thank the members of the Ruysch Research Group, Prof. Otto P. Bleker, Dr. Jozien J. Driessen‐van het Reve, Dr. Francisca M.M. Griffioen, Dr. Frank IJpma, Dr. Laurens de Rooij, and Mr. Willem J. Mulder, for their valuable contributions and helpful discussions. We thank Prof. Dirk Ruiter and Dr. Annelieke Schepens‐Franke for their critical review of this article, and Mr. Tim Rijnhout and Mrs. Ksenia M. Vozdigan, for reproduction of the images. We thank the Wilhelmina E. Jansen Fonds for their support of the International Ruysch Research Group.
Boer L, Radziun AB, Oostra R‐J. 2017. Frederik Ruysch (1638–1731): Historical perspective and contemporary analysis of his teratological legacy. Am J Med Genet Part A 173A:16–41.
Conflict of interest: None.
REFERENCES
- Anonymous. 1731. Catalogus Musaei Ruyschiani, sive permagnae, elegantissimae, nitidissimae, incomparabilis et vere regiae collectionis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Anonymous. 1742. Musei Imperialis Petropolitani. Vol.I. Pars prima qua continentur res naturales ex regno animali. St. Petersburg: Academiae scientiarum. [Google Scholar]
- Anonymous. 1751. Catalogus van de uitmuntende cabinetten […] van den professor Ruysch […] met veel moeite en kosten in een reeks van jaaren vergadert en nagelaten door den heere Albertus Seba. Amsterdam: Sluyter, Schut & Blinkvliet. [Google Scholar]
- Anonymous. 1765. Catalogus van de alöm beroemde kabinetten, bestaande in sierlyke anatomische praeparata, onder welke van den prof. F. Ruysch […] Alles by één vergadert en aldus nagelaten door den heer Adrianus Deknatel. Amsterdam: Blinkvliet & Posthumus. [Google Scholar]
- Anonymous. 1783. Musei Gaubiani pars sive catalogus partis supellectis qua usus est vir celeberrimus H.D. Gaubius […]. Amsterdam: Luchtmans. [Google Scholar]
- Anonymous. 1787. Animalium musaei Houttuyniani index. Amsterdam: Posthumus & Blinkvliet. [Google Scholar]
- Baijal N, Sahni M, Neeraj V, Kumar A, Parkhe N, Puliyel M. 2007. Discordant twins with the smaller baby appropriate for gestational age‐ unusual manifestation of superfoetation: A case report. BMC Pediatr 7:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandler SW. 1901. Dermoid and other cysts of the ovaries. Their origin from the Wolffian body. New York: William Wood & Company; p 42. [Google Scholar]
- Bolat F, Kayaselcuk F, Tarim E, Kilicdag E, Bal N. 2008. Congenital intracranial teratoma with massive macrocephaly and skull rupture. Fetal Diagn Ther 23:1–4. [DOI] [PubMed] [Google Scholar]
- Breslau RE. 1864. Geburtsgeschichte und Untersuchung eines Falles von foetus in foeto. Zurich 30:406–417. [Google Scholar]
- Cairo MS, Grosfeld JL, Weetman RM. 1981. Gastric teratoma: Unusual cause for bleeding of the upper gastrointestinal tract in the newborn. Pediatrics 67:721–724. [PubMed] [Google Scholar]
- Chen SS, Chen CP, Chien SC, Hsu CY. 2008. Spontaneous rupture of omental teratoma mimicking a ruptured ovarian teratoma. Taiwan J Obstet Gynecol 47:229–232. [DOI] [PubMed] [Google Scholar]
- Damjanov I, Knowles BB, Solter D. 1983. The human teratomas. Experimental and clinical biology. Clifton NJ: Humana Press. [Google Scholar]
- Dutz W, Sadeghee S. 1968. A teratoid finger in the sigmoid colon. J Pathol Bacteriol 95:289–291. [DOI] [PubMed] [Google Scholar]
- Ellis RWB, Van Creveld S. 1940. A syndrome characterized by ectodermal dysplasia, polydactyly, chondro‐dysplasia and congenital morbus cordis: Report of three cases. Arch Dis Child 15:65–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eustermann GB, Sentry EG. 1922. Benign tumours of the stomach: Report of 27 cases. Surg Gynecol Obstet 34:372–378. [Google Scholar]
- Ewing J. 1919. Neoplastic diseases. A text book on tumors. London & Philadelphia: W.B. Saunders Company; p 953. [Google Scholar]
- Fox H, Butler‐Manuel R. 1964. A teratoma of the placenta. J Pathol Bacteriol 88:137–140. [PubMed] [Google Scholar]
- Geyl. 1897. Betrachtungen über die Genese der sogenannten Ovarialdermoide mit Bezug auf ein Vaginalteratom. Sammlung klinischer Vorträge von Volkmann. Neue Folge No. 190.
- Ginzburg VV. 1953. Anatomicheskaia kollektsia F. Riuischa v sobraniiakh Petrovskoi Kunstkameri. Sbornik Museia Antropologii I Etnografii 14:263–305. [Google Scholar]
- Ginzburg VV. 1959. Muzej kafedry normal'noi anatomii voenno‐meditsinskoi ordena Lenina Akademii im. S.M. Kirova. Archiv Anatomii. Gistologii I Embryologii Leningrad 11:114–124. [PubMed] [Google Scholar]
- Goto K, Yoshinari H, Tajima K, Kotsuji F. 2006. Microperforate hymen in a primigravida in active labor: A case report. J Reprod Med 51:584–586. [PubMed] [Google Scholar]
- Gould GM, Pyle WL. 1896. Anomalies and Curiosities of Medicine. Philadelphia: W.B. Saunders. [Google Scholar]
- Gray SW, Johnson HC, Jr. , Skandalakis JE. 1964. Gastric teratoma in an adult: With a review of the literature. South Med J 57:1346–1351. [DOI] [PubMed] [Google Scholar]
- Haller A. von . 1774. Bibliotheca Anatomica qua scripta ad anatomen et physiologiam facienta a rerum initiis recensentur. Zurich: Orell, Gessner & Fuessli; p 536. [Google Scholar]
- Hirschsprung H. 1888. Stuhlträgheit Neugeborener in Folge von Dilatation und Hypertrophie des Colons. Jahrb Kinderheilk Phys Erzieh 27:1–7. [Google Scholar]
- Hutchinson J. 1893. A short‐limbed polydactylous dwarf In: Huchinson J, editor. Archives of Surgery. Vol. IV. London: J. & E. Churchill. [Google Scholar]
- Hyrtl J. 1860. Handbuch der praktischen Zergliederungskunst: als Anleitung zu den Sectionsübungen und zur Ausarbeitung anatomischer Präparate. Wien: Wilhelm Braumüller. [Google Scholar]
- Hyrtl J. 1869. Vergangenheit und Gegenwart des Museums für menschlicheAnatomie an der Wiener Universität. Wien: Wilhelm Braumüller. [Google Scholar]
- Iyoob SD, Tsai A, Ruchelli ED, Coleman BG, Wilson RD. 2006. Large umbilical cord hemangioma: Sonographic features with surgical pathologic correlation. J Ultrasound Med 25:1495–1498. [DOI] [PubMed] [Google Scholar]
- Jayle F. 1909. La dilatation congenitale idiopatique du colon observée au XVIIe siècle. Presse Med 17:803–804. [Google Scholar]
- Johnson J, Johnsen HJ. 1840. The medico‐surgical review and the Journal of physical medicine. London: S. Highley; p 370. [Google Scholar]
- Kerckring TT. 1670. Spicilegium Anatomicum, Continens Observationum Anatomicarum Rariorum Centuriam Unam, Nec Non Osteogeniam Foetuum. Amsterdam: Andreas Frisii. [Google Scholar]
- Kimmel DL, Moyer EK, Peale AR, Winborne LW, Gotwals JE. 1950. A cerebral tumor containing five human fetuses: A case of fetus in fetu. Anat Rec 106:141–165. [DOI] [PubMed] [Google Scholar]
- Kooijmans L. 2004. De doodskunstenaar, de anatomische lessen van Frederik Ruysch. Amsterdam: Bert Bakker. [Google Scholar]
- Koppang HS, Boman H, Hoel PS. 1983. Oral abnormalities in the Saldino‐Noonan syndrome. Virchows Arch 398:247–262. [DOI] [PubMed] [Google Scholar]
- Kubosawa H, Iwasaki H, Kuzuta N, Suzuki H, Iura H. 2006. Adenocarcinoma with peritoneal dissemination secondary to multiple mature teratomas of the omentum. Gynecol Oncol 101:534–536. [DOI] [PubMed] [Google Scholar]
- Lannelongue OM, Achard C. 1886. Traité des kystes congénitaux. Paris: Asselin & Houzeau. [Google Scholar]
- Lebert H. 1852. Des kystes dermoides et de l'héterotopie plastique en général, communiqué de la société de biologie en aoÛt I852. Gazette médicale de Paris, 3me série 7:720–722, 793–796, 808–811.
- Leenders E, Sieber WK. 1970. Congenital megacolon, observation by Frederici Ruysch 1691. J Pediatr Surg 5:1–3. [DOI] [PubMed] [Google Scholar]
- Liu L, Zhuang W, Chen Z, Zhou Y, Huang X‐R. 2009. Primary gastric teratoma on the cardiac orifice in an adult. World J Gastroenterol 15:1782–1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loder RT, Huffman G, Toney E, Wurtz LD, Fallon R. 2007. Abnormal rib number in childhood malignancy: Implications for the scoliosis surgeon. Spine (PhilaPa 1976) 32:904–910. [DOI] [PubMed] [Google Scholar]
- Luyendijk‐Elshout AM. 1970. Death enlightened: A study of Frederik Ruysch. JAMA 212:121–126. [DOI] [PubMed] [Google Scholar]
- Majewski F, Pfeiffer RA, Lenz W, Müller R, Feil G, Seiler R. 1971. Polydaktylie, verkürzte Gliedmassen und Genitalfehlbildungen: Kennzeichen eines selbständigen Syndroms? Z Kinderheilkd 111:118–138. [PubMed] [Google Scholar]
- Maso G, D'Ottavio G, De Seta F, Sartore A, Piccoli M, Mandruzzato G. 2005. First‐trimester intrauterine hematoma and outcome of pregnancy. Obstet Gynecol 105:339–344. [DOI] [PubMed] [Google Scholar]
- McKusick VA, Egeland JA, Eldridge R, Krusen DE. 1964. Dwarfism in the Amish. I. The Ellis‐ Van Creveld syndrome. Bull Johns Hopkins Hosp 115:306–336. [PubMed] [Google Scholar]
- Meckel JF. 1809. Über die Divertikel am Darmkanal. Archiv für die Physiologie Halle 9:421–453. [Google Scholar]
- Merks JH, Smets AM, Van Rijn RR, Kobes J, Caron HN, Maas M, Hennekam RC. 2005. Prevalence of rib anomalies in normal Caucasian children and childhood cancer patients. Eur J Med Genet 48:113–129. [DOI] [PubMed] [Google Scholar]
- Müller J. 1838. Über die feineren Bau und die Formen der Krankhaften Geschwülste. Berlin: G. Reimer. [Google Scholar]
- Mumey N. 1928. Dermoid cysts of the greater omentum. Am J Surg 5:56–60. [Google Scholar]
- Naudin ten Cate L, Vermeij‐Keers C, Smit DA, Cohen‐Overbeek TE, Gerssen‐Schoorl KB, Dijkhuizen T. 1995. Intracranial teratoma with multiple fetuses: Pre‐ and post‐natal appearance. Hum Pathol 26:804–807. [DOI] [PubMed] [Google Scholar]
- Nicholls AG. 1940. Theodore Kerckring and his “Spicilegium Anatomicum”. Can Med Assoc J 42:480–483. [Google Scholar]
- LXEL Ollier. 1890. Exostoses multiples. Mémoires et comptes rendus de la Société des sciences médicales de Lyon 29: 12. [Google Scholar]
- Pelizzari E, Valdez CM, Picetti Jdos S, Cunha AC, Dietrich C, Fell PR, Targa LV, Zen PR, Rosa RF. 2015. Characteristics of fetuses evaluated due to suspected anencephaly: A population‐based cohort study in southern Brazil. Sao Paulo Med J 133:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radziun A, Chistov Y. 2012. The first scientific collections of Kunstkamera: Exhibition guide. St. Petersburg: MAE RAS; p 78. [Google Scholar]
- Roellig K, Menzies BR, Hildebrandt TB, Goeritz F. 2011. The concept of superfetation: A critical review on a ‘myth’ in mammalian reproduction. Biol Rev 86:77–95. [DOI] [PubMed] [Google Scholar]
- Ruysch F. 1665. Dilucidatio valvularum in vasis lymphaticis et lacteis cum figuris aeneis, accesserunt quaedam observations anatomicae rariores. The Hague: Herman Gael. [Google Scholar]
- Ruysch F. 1691a. Observationum anatomico‐chirurgicarum centuria, accredit catalogus rariorum quae in museo Ruyschiano asservantur. Amsterdam: Hendrik & Theodoor Boom. [Google Scholar]
- Ruysch F. 1691b. Musaeum anatomicum Ruyschianum, sive Catalogus rariorum, quae in authoris aedibus asservantur. Amsterdam: Hendrik & Theodoor Boom. [Google Scholar]
- Ruysch F. 1697. Epistola anatomica, problematica decima. Auctore Bartholomaeo Keerwolff, med. doct. Ad virum clarissimum Fredericum Ruyschium de auricularum cordis, earumque fibrarum motricum structura. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1701a. Epistola anatomica quarta & decima. Auctore Mauritio á Reverhorst, med. doct et anat. professore. Ad virum clarissimum Fredericum Ruyschium de nova artuum decurtandorum method. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1701b. Thesaurus anatomicus primus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1702. Thesaurus anatomicus secundus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1703. Thesaurus anatomicus tertius, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1704. Thesaurus anatomicus quartus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1705. Thesaurus anatomicus sextus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1707. Thesaurus anatomicus septimus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1709. Thesaurus anatomicus octavus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1714. Thesaurus anatomicus nonus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1716. Thesaurus magnus et regius qui est decimus thesaurum anatomicorum in quo praecipuaecorporis humani partes, ceu in statu vivo, nitidissime praeparatae, reservatur, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1717. Adversariorum anatomico‐medico‐chirurgicorum decas prima, in qua varia notatu digna recensentur, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1720. Adversariorum anatomico‐medico‐chirurgicorum decas secunda, in qua varia notatu digna recensentur, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1721. Opera Omnia Anatomico‐Medico‐Chirurgica. Huc usque edita. quorum elenchus sequenti exhibetur, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1723a. Adversariorum anatomico‐medico‐chirurgicorum decas tertia, in qua varia notatu digna recensentur, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1723b. Tractatio anatomica de musculo in fundo uteri observato, ante hac a nemine detecto cui, accedit depulsionis secundinarum, parturientium foeminarum, instruction. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1724. Curae posteriores seu thesaurus anatomicus omnium praecedentium maximus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1728. Curae renovatae seu thesaurus anatomicus, post curas posteriores, novus, cum figuris aeneis. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1734. Observations Anatomiques et Chirurgicales, au nombre de Cent par Mr. Frédéric Ruysch, très‐célèbre anatomiste. Avec des Figures en Taille‐douce qui représentent les parties dans leur grandeur naturelle. Paris: Guillaume Cavelier. [Google Scholar]
- Ruysch F. 1744. Alle de Ontleed‐, Genees‐ en Heelkundige Werken. Amsterdam: Janssoons‐van Waesberge. [Google Scholar]
- Ruysch F. 1751. The Celebrated Dr. F. Ruysch's Practical Observations in Surgery and Midwifry. now first translated from the Latin Into English, by a Physician. Illustrated with Copper‐plates. London: T. Osborne. [Google Scholar]
- Schmidts M. 2014. Clinical genetics and pathobiology of ciliary chondrodysplasias. J Pediatr Genet 3:46–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher R, Mai A, Gutjahr P. 1992. Association of rib anomalies and malignancy in childhood. Eur J Pediatr 151:432–434. [DOI] [PubMed] [Google Scholar]
- Schwarz S. 1999. Die anatomische Privatsammlung der Anatomenfamilie Meckel unter besonderer Berücksichtigung ihres präparationstechnischen Profils. Thesis. Halle, Martin‐Lüther‐Universität Halle‐Wittenberg.
- Spranger J, Grimm B, Weller M, Weissenbacher G, Herrmann J, Gilbert E, Krepler R. 1974. Short rib‐polydactyly (SRP) syndromes, types Majewski and Saldino‐Noonan. Z Kinderheilkd 116:73–94. [DOI] [PubMed] [Google Scholar]
- Stephens TD, Spall R, Urfer AG, Martin R. 1989. Fetus amorphus or placental teratoma? Teratology 40:1–10. [DOI] [PubMed] [Google Scholar]
- Ternowsky WN. 1927. “Fredericus Ruysch” aus dem Anatomischen Institut der Universität in Kasan. Bulletin du VI. Congres de la Société Internationale d'Histoire de la Médicine: 334–338.
- Tulp N. 1641. Observationes medicae. Amsterdam: Lodewijk Elsevier. [Google Scholar]
- Ukiyama E, Endo M, Yoshida F, Tezuka T, Kudo K, Sato S, Akatsuka S, Hata J. 2005. Recurrent yolk sac tumor following resection of a neonatal immature gastric teratoma. Pediatr Surg Int 21:585–588. [DOI] [PubMed] [Google Scholar]
- Vater A. 1736. Regii in Academia ad Albim musei anatomici Augustei Catalogus universalis. Wittenberg: Henning. [Google Scholar]
- Visser GH, Laurini RN, de Vries JI, Bekedam DJ, Prechtl HF. 1985. Abnormal motor behaviour in anencephalic fetuses. Early Hum Dev 12:173–182. [DOI] [PubMed] [Google Scholar]
- Washburne JF, Magann EF, Clauhan SP, Fratkin JD, Morrison JC. 1995. Massive congenital intracranial teratoma with skull rupture at delivery. Am J Obstet Gynecol 173:126–128. [DOI] [PubMed] [Google Scholar]


