ABSTRACT
Vaccine-preventable deaths among adults remain a major public health concern, despite continued efforts to increase vaccination rates in this population. Alternative approaches to immunization delivery may help address under-vaccination among adults. This systematic review assesses the feasibility, acceptability, and effectiveness of community pharmacies as sites for adult vaccination. We searched 5 electronic databases (PubMed, EMBASE, Scopus, Cochrane, LILACS) for studies published prior to June 2016 and identified 47 relevant articles. We found that pharmacy-based immunization services (PBIS) have been facilitated by state regulatory changes and training programs that allow pharmacists to directly provide vaccinations. These services are widely accepted by both patients and pharmacy staff, and are capable of improving access and increasing vaccination rates. However, political and organizational barriers limit the feasibility and effectiveness of vaccine delivery in pharmacies. These studies provide evidence to inform policy and organizational efforts that promote the efficacy and sustainability of PBIS.
Keywords: community pharmacy services; health services delivery; immunization programs, pharmacies; vaccine policy
Background
Among adults in the United States, approximately 50,000 vaccine-preventable deaths occur each year.1 However, despite continued public health efforts, adult vaccination rates in the United States remain below the recommended benchmarks for all routinely recommended vaccinations.2 The actual adult vaccination rates in both 2000 and 2010 were much lower than the Healthy People 2000 and 2010 targets.3,4 Current trends predict vaccination rates will again fall considerably short of the Healthy People 2020 goals.5,6 Significant barriers to achieving these goals include a lack of access to a regular source of care and missed opportunities for healthcare providers' to provide preventative health recommendations.7 One option to address these persistent shortfalls and barriers is to leverage non-traditional sites of vaccination delivery.8,9
With an estimated 56,000 outlets in the United States, community pharmacies have the potential to dramatically increase adult vaccination rates.10,11 Pharmacy-based immunization services (PBIS) are one of a range of primary care services which are increasingly offered by pharmacies.12-14 Pharmacies began offering mass-vaccination clinics run by nurses and other visiting healthcare providers in 1984. Over the following decade, this practice became widespread such that in 1997, 5 million doses of influenza vaccine were administered in 15,000 community pharmacies nationwide.15,16 However, the scope and effectiveness of these mass-vaccination clinics were frequently limited by their temporary operation and narrow range of vaccinations offered.16,17
Pharmacists began regularly providing immunizations directly to adults in 1996. Concurrently, an increasing number of states began changing scope-of-practice policies to explicitly allow pharmacists to vaccinate patients.15,16,18 The updated regulations facilitated the incorporation of immunization services into the year-round, routine care administered at community pharmacies. However, states adopted these policy changes asynchronously over several years, resulting in the differential adoption of PBIS among states.15,16 By 2009 pharmacists in all 50 states, Washington DC, and Puerto Rico were allowed to obtain certification to administer the influenza vaccine, and 46 states allowed pharmacists to administer all adult vaccinations.19 By 2015 an estimated 280,000 pharmacists had been certified to deliver vaccinations.20 The increased involvement of pharmacists in immunization practice was supported by other traditional immunizers including the American College of Physicians-American Society of Internal Medicine, who have pointed out pharmacists' ability to increase vaccination rates among adults and high risk populations.21
PBIS can provide a significant vaccination volume. Pharmacies were the second-most utilized site for influenza vaccination among adults, after physician's offices. Pharmacies delivered 20% of influenza vaccinations in the US in 2011–2012, and up to 25% at the beginning of the 2014–2015 influenza season.22 However, community pharmacies are underutilized as a site of delivery for adult vaccinations such as the pneumococcal; zoster; tetanus, diphtheria, and acellular pertussis (Tdap); and hepatitis A and B vaccines.19,23,24 Further insights into barriers that limit the effectiveness of PBIS may strengthen the role of community pharmacies as part of the community-based “immunization neighborhood.”18,23-26
To date, there has been no comprehensive review of the evidence regarding pharmacies as sites of immunization service delivery for adults or the impact of PBIS on vaccination coverage. This is a critical gap in the understanding of how adults access preventative health services, particularly given the emphasis on accessible and affordable primary health care in the Affordable Care Act.27 To assess the current state of PBIS for adult vaccination and its impact,28 we conducted this systematic review to summarize current literature and identify targets for future research.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to conduct the review and analysis.29 Searches of the indexed literature were conducted from 1992 through 14 July 2013 in the online databases PubMed, EMBASE, Scopus, Cochrane and LILACS with no language limitations. Google Scholar© was also reviewed for gray literature using similar control vocabulary and search criteria. To update the review to reflect developments in the field, a literature search following previously determined criteria was completed for articles published between 15 July 2013 and 20 June 2016. Database searches used relevant terms and control vocabulary that corresponded to our primary research question: immunization; immunization or vaccination services; community or retail pharmacy; community or retail pharmacy services; pharmacist. Population (e.g., pharmacy) and intervention (e.g., immunization services) search terms were constructed according to a population, intervention, control, and outcome (P.I.C.O.) question format.
Study selection
Duplicate studies were removed from the results, and titles and abstracts were screened by the first author using the following inclusion criteria: articles reporting original research on the administration of vaccines routinely recommended for adults, 18 y or older, in community pharmacies in the United States and Territories. Community pharmacies, hereafter referred to simply as pharmacies, were defined as community-based locations that provide pharmaceutical services to the public, and are distinct from hospital or industrial pharmacy settings. Routinely-recommended vaccines refer to vaccines recommended to adults by the Advisory Commission on Immunization Practices (ACIP) that are part of standard immunization needs.30 Studies were excluded if they: 1) were conducted in countries other than the United States; 2) focused on vaccinations delivered at sites other than pharmacies; 3) referred to only child or adolescent vaccinations or 4) referred to only non-standard immunization needs, such as travel vaccinations or pandemic/emergency responses. The co-authors confirmed the preliminary screening of titles and abstracts, with disagreements between reviewers resolved by consensus.
Quality screen and data extraction
Given the variety of study designs, one of 3 quality screens were applied to selected papers. Experimental study designs were assessed using the Effective Public Health Practice Project (EPHPP) tool for quantitative studies.31 Case control and cohort studies were evaluated using the Newcastle-Ottawa rating system.32 Observational cross-sectional studies were assessed using the National Institute of Health's National Heart, Lung and Blood Institute (NHLBI) Quality Assessment Tool for Observational Cohort and Cross-sectional Studies.33 All screened studies met basic quality requirements, so no studies were excluded. Models, case studies and qualitative studies did not undergo quality assessment, and were included in the review.
Data were extracted from included studies using a data extraction template developed by the authors. The first author extracted data from eligible articles, and the co-authors independently reviewed and confirmed extracted data and quality screening results for a subset of papers. Authors resolved outstanding questions and discrepancies through consensus. Data elements extracted included study design, sample, study period, location, main outcome, and key findings. Results were extracted and coded for the 3 principal topics of the review: feasibility, acceptability and effectiveness of PBIS. Studies were further coded to one or more sub-categories created from emergent themes that arose through iterative review of the data.
Results
Database searches yielded 397 results, and Google Scholar© generated an additional 816 results for a total of 1213 publications (Fig. 1). Following review of titles and abstracts, 136 articles underwent screening based on inclusion criteria and study design and an additional 79 studies were excluded. The remaining 57 articles underwent full text review, quality screen, and data abstraction. Of these, 21 studies that did not meet inclusion criteria or met one or more of the exclusion criteria were discarded from the review. Scanning bibliographies of all included studies revealed 4 additional studies that met eligibility criteria. The updated literature search revealed an additional 7 studies, yielding a final total of 47 articles which were included in the review (Table 1). A majority of studies used a cross-sectional study design (n = 25 studies, 53%); the remainder includes 4 cohort studies (8.5%), 4 case studies (8.5%), 4 experimental studies (8.5%), 3 modeling studies (6.5%), and 7 studies of singular design (15%). Results are presented here by outcome theme, including feasibility (n = 30 studies), acceptability (n = 11 studies), and effectiveness (n = 27 studies).
Figure 1.
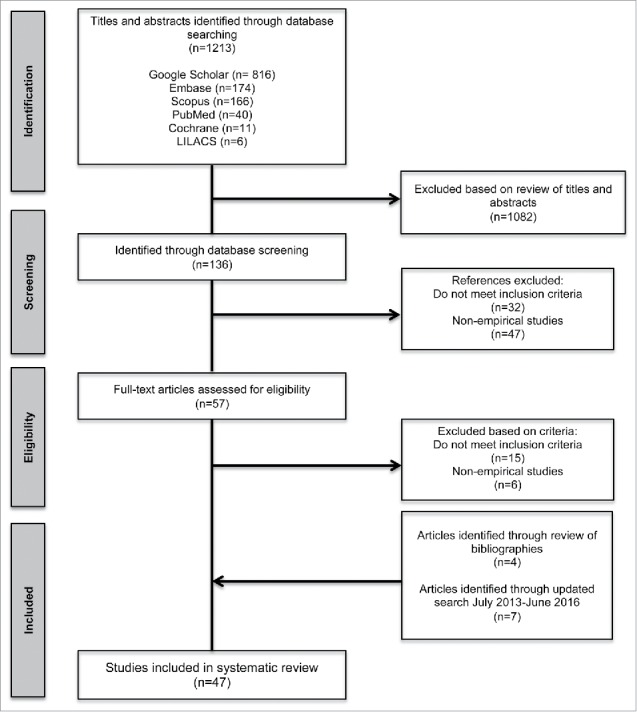
Flow diagram documenting systematic search conducted to identify studies on community pharmacies as sites for adult vaccination.
Table 1.
Summary of characteristics of included studies with results relevant to PBIS, organized in reverse chronological order. Principal category labels: F-Feasibility, A-Acceptability, E-Effectiveness.
| Study | Design | Sample | Study Period | Location | Main Outcome | Category | Summary of Main Findings |
|---|---|---|---|---|---|---|---|
| Westrick et al. (2016)57 | Cluster-randomized experimental design | 96 Community pharmacies | 2013–2015 | US | Number of pneumococcal vaccination administered; program evaluation indicators | F, E | Both self-directed and coaching groups had significant increases in pneumococcal vaccination rates; pharmacies in the coaching group completed a greater number of process indicators. |
| Brackett et al. (2015)73 | Pilot evaluation | 1 Pharmacy; 19 customers received motivational interviewing intervention | September 2013-April 2014 | Atlanta, GA | Number of vaccines delivered at pharmacy chain; pharmacists attitudes | E | Due to a limited sample size, the effect of a motivational interviewing (MI) intervention on vaccination rates was inconclusive; pharmacists considered MI to be an effective communication tool. |
| Singhal and Zhang (2014)23 | Cross-sectional | 2 Health insurance databases, representing 48.7 million patients | 2010 | US | Vaccine administration costs | F | The total direct cost for the influenza, pneumococcal, and zoster vaccinations were cheaper at pharmacies than other sites. Patients paid the least out-of-pocket cost for influenza and pneumococcal at pharmacies. |
| Teeter et al. (2014)45 | Cross-sectional | 688 Pharmacy patients, 65 y or older | Summer 2013 | AL & FL | Vaccination rates; patient characteristics and knowledge | F, E | After a herpes zoster educational intervention led by pharmacy students, 72.5% of unvaccinated patients were interested in speaking with a pharmacist/doctor. Patients who had received a healthcare provider's recommendation were more likely to be vaccinated. |
| Erickson and Workman (2014)76 | Cross-sectional | 503 Community pharmacies | February 2011 | Wayne County, MI | Pharmacy characteristics and service offerings | E | Pharmacies in ZIP codes with higher annual household income and higher percentage of white residents offered more immunization services. |
| Hedden et al. (2014)69 | Cost Analysis Model | 19 Pharmacies from one chain | September 2011- January 2012 | Kansas City, KA | Financial gains and losses for vaccines administered per pharmacy site | E | Two different pharmacoeconomic models both indicated that a herpes zoster vaccine program at a local pharmacy chain yielded a net profit. |
| Goad et. al (2013)24 | Cross-sectional | National pharmacy chain | August 2012-July 2013 | US | Date and time of vaccines administered | E | 30.5% of all adult vaccines delivered at a major national pharmacy chain were administered during off-hours (i.e. nights, weekends, and holidays) |
| Hess (2013)72 | Randomized Control Trial | 16 Pharmacies; 9650 prescription holders received phone message | December 2006- May 2007 | GA & TN | Number of vaccines administered | E | Automated telephone messaging to at-risk patients significantly increased herpes zoster vaccination rates between the 2 cohorts. |
| Bryan et al. (2013)70 | Pre/post with comparison group | 745 Pharmacy customers received personal selling in experimental group, 614 in control group | November 2010 - February 2011 | MO | Patient commitments to vaccinate and attitudes; time spent with pharmacist | E | Personal selling techniques were more effective than passive methods at increasing herpes zoster vaccination commitments and delivered vaccinations. |
| Wang et al. (2013)66 | Prospective Intervention; Pre/post Design | 3 Pharmacy sites; 16,121 during control, 16,062 during intervention | February 2008 - March 2008 | TN | Vaccination rates; patient knowledge | A | Pharmacy-based flyers and letter-based interventions increased herpes zoster vaccination rates and increased acts of vaccination. |
| Wang et al. (2013)77 | Cross-sectional | 71,135,249 Survey responders from the Medicare Expenditure Survey | 2009 | US | Vaccination rates; patient characteristics | E | Significant racial disparities between black and white responders were found for both community pharmacy and non-pharmacy populations. Community pharmacy patients reported higher overall influenza vaccination rates. |
| Doucette et al. (2012)75 | Case Report | 1 Independent community pharmacy | 2008–2010 | Iowa City, IA | Profitability of pharmacy services | E | Influenza and herpes zoster immunizations yielded a net profit, while pneumococcal vaccines showed a net loss during the study period. |
| Murphy et al. (2012)25 | Cross-sectional | 6936 Walgreens pharmacies, over 18,000 pharmacists | September 2009-February 2010 | US | Number of influenza vaccinations provided in medically-underserved areas | A, E | A single national pharmacy chain served 43.2% of medically underserved areas (MUAs), and 37.7% of the chain's total influenza vaccines were delivered in MUAs. |
| Crawford et al. (2011)59 | Cross-sectional | 103 Pharmacy sites, 437 pharmacy staff | January 2008-March 2009 | New York, NY | Individual and neighborhood characteristics of staff; staff support for PBIS | F, A, E | Pharmacists working in pharmacies that provided other public-health services were more supportive of PBIS. Pharmacists working in high-minority communities were significantly less supportive. |
| Taitel et al. (2011)78 | Cross-sectional | 1,343,571 At-risk patients | August 2010 - November 2010. | US | State-level vaccination rates | E | Pharmacies were successful at identifying at-risk patients, and providing additional vaccinations. At-risk patients were vaccinated against pneumococcal at significantly higher rates than adults using traditional care (4.88% vs. 2.90%). |
| Penfold et al. (2011)42 | Qualitative | 65 Flu vaccine stakeholders; 7 pharmacy stakeholders | January 2009 - June 2010 | US | Stakeholder perceptions of barriers and solution to community delivery of influenza vaccines | F | Pharmacies cited barriers in billing and insurance reimbursement, and legal constraints based on scope-of-practice. |
| Pace et al. (2010)40 | Cross-sectional | 122 Pharmacists or pharmacy managers | February - March 2009 | AR | Practice site characteristics and demographics; pharmacist involvement; perceived barriers | F | A majority of pharmacists believed pharmacist-delivered vaccinations advanced the field and increased access to care. Cited barriers varied by pharmacy setting. |
| Pilisuk et al. (2010)39 | Mixed Methods; Cross-sectional | Representatives from 8 chain pharmacies, 2,500 store locations | 2006–2007 | CA | Pharmacy policies and protocols; practice site characteristics and demographics | F | Representatives reported that all chains offered adult immunization services. Maintaining records with patients' medical home was cited as one of the biggest challenges. |
| Westrick (2010)50 | Cohort | 155 Pharmacies responded to both survey stages. | 2003, 2004, 2006–2007 | WA | Pharmacy and immunization service characteristics | F | Type of pharmacy and time since implementation of vaccination programs affected the scale and pharmacist-involvement in PBIS. |
| Westrick (2010)55 | Cross-sectional | 106 Pharmacies included | 2003–2004 | WA | Pharmacist characteristics and attitudes; pharmacy organizational factors | F | Pharmacy attitudes toward pharmacist-delivered and out-sourced vaccination services were correlated with decisions to adopt or discontinue services. |
| Westrick et al. (2009)53 | Cross-sectional | 1704 Pharmacists or pharmacy managers | July 2005- February 2006 | AL, AZ, ID, MD, MS, MT, NM, NY, OK, OR, PA, SD, TN, TX, WA, WI, WV | Pharmacist involvement and characteristics | F | Pharmacies affiliated with pharmacy schools were significantly more likely to participate in public health services. However, affiliation was non-significant when the presence of a certified pharmacist or positive attitudes were considered. |
| Grabenstein (2009)17 | Retrospective Cohort Study | 13 Pharmacies in Oregon and 11 pharmacies in Washington | 1997 and 1998 | OR & WA | Number of vaccines administered per pharmacy site | F, E | Pharmacists offering daily vaccinations administered more vaccinations over an influenza season than nurses operating single-day clinics. |
| Westrick and Breland (2009)56 | Cross-sectional | 206 Key informants of pharmacies | 2006 | WA | Practice site characteristics; pharmacy organizational factors | F | Compatibility between the site and immunization services was found to be key to sustainability. Two paths to compatibility are discussed. |
| Westrick et al. (2009)54 | Cross-sectional | 1704 Pharmacists, 301 offered pharmacist-delivered vaccination services | July 2005- February 2006 | AL, AZ, ID, MD, MS, MT, NM, NY, OK, OR, PA, SD, TN, TX, WA, WI, WV | Number of vaccines purchased, administered, and distributed to other sites | F | About one third of vaccines purchased by pharmacies are administered in pharmacies, while the remaining two-thirds are distributed to other vaccinators. |
| Wood et al.(2009)63 | Retrospective Cost Analysis | 1 Independent community pharmacy | February 2007- January 2008 | Iowa City, IA | Financial gains and losses for PBIS | F | A financial analysis of the first 11 months of a herpes zoster immunization program resulted in a net profit. |
| Westrick and Mount (2009)58 | Cohort | 115 Pharmacies participated in both stages II and III. | 2004 and 2006–07 | WA | Immunization service characteristics | F | Perceived benefit, perceived compatibility, and perceived complexity of PBIS independently predicted adoption of pharmacist-delivered immunization services; when considered together, perceived benefit was the only significant predictor. |
| Westrick et al. (2008)47 | Cross-sectional | 1707 Community pharmacists | July 2005- February 2006 | AL, AZ, ID, MD, MS, MT, NM, NY, OK, OR, PA, SD, TN, TX, WA, WI, WV | Pharmacy and immunization service characteristics | F | There are wide state-level variations in pharmacies' stages of involvement in PBIS |
| Kummer and Foushee (2008)38 | Cross-sectional | 1,274 Active pharmacists | January- February 2007 | NC | Characteristics and perceived barriers of PBIS and practice sites | F, E | Only 22% of responding pharmacists were immunization certified, and 52% had immunized in the last year. Barriers were analyzed based on involvement with immunization services. |
| Prosser et al. (2008)74 | Cost Decision Model; Qualitative | Cost breakdowns by population, health status, and age group | n/a | n/a | Health benefits and financial costs | E | The mean cost of vaccinations and the cost to prevent a case of influenza were both lower in pharmacies than physician's offices and mass vaccination clinics. |
| Turner et al. (2007)44 | Cohort; Cross-sectional | 2nd and 3rd year pharmacy students (n=121–125, and n=123) | 2004–2005 | Denver, CO | Number of vaccines administered; pharmacy student and mentor attitudes | F | 2nd and 3rd year pharmacy students delivered an estimated 5,000 and 15,000 vaccines in community pharmacies. Self-confidence to administer increased and was maintained a year later. |
| Goode et al. (2007)49 | Case series | 29 Grocery stores, 23 with pharmacies | 1998–2005 | VA | Number of influenza and pneumococcal vaccines delivered at a pharmacy chain | F, A, E | Documents the expansion of immunization services program at a local pharmacy chain, and increases in the number of vaccines delivered. |
| Doucette et al. (2006)46 | Cross-sectional | 611 Pharmacists, of which 290 community pharmacists | 2004 | US | Type and frequency of pharmacy services | F | Immunization services were the most commonly offered non-dispensary services (15.1% of pharmacies). Three or more pharmacists on duty, and pharmacy innovativeness were positively associated with greater service offerings. |
| Capurso and Powers (2006)2 | Cross-sectional | 43 Pharmacists | February 2005 | OH | Pharmacist-perceived barriers to PBIS | F, A | Surveyed pharmacists cited similar barriers to effective immunization services. |
| Marrero et al. (2006)71 | Controlled Clinical Trial | 50 Pharmacy patients in experimental group with educational activity, and 50 in control group | June-July 2000 | Puerto Rico | Vaccination rates; patient knowledge | E | Following a pharmacist-led educational intervention, patients demonstrated greater influenza vaccination knowledge and higher rates than the control group. |
| Bearden and Holt (2005)37 | Cross-sectional | All pharmacies with immunization programs: 56 in 2001, 88 in 2002, 132 in 2003 | 2001–2003 | OR | Pharmacy-based vaccination rates and characteristics | F, E | In the 3 y following regulatory changes that allowed pharmacist vaccination, the number of adult influenza vaccinations delivered and participating pharmacies increased each year. Over one quarter of vaccines were delivered in rural counties. |
| Steyer et al. (2004)36 | Quasi-experimental Matched Pair | Sixteen states; 8 that passed legislation in 1997 allowing pharmacist-administered vaccination, and 8 that did not pass until after 2000 | 1995 and 1999 | States with legislation (AR, KS, NE, ND, OK, TN, TX, VA) and those without (LA, MO, IA, WY, UT, WV, FL, MD) in 1997 | State vaccinations rates | F, E | States that allowed pharmacist-vaccination had significantly higher influenza vaccination rates for adults 65 y and older, after controlling for policy changes. |
| Neuhauser et al. (2004)48 | Cross-sectional | 90 Immunization-certified pharmacists and 169 pharmacists for control | Not Reported | TX | Practice site characteristics and demographics; pharmacist involvement and satisfaction | F, A | Certified pharmacists were more involved in PBIS than non-certified pharmacists in some capacity. Seventy-four percent of certified pharmacists administered vaccines. |
| Kamal et al. (2003)1 | Cross-sectional | 1266 Immunization-certified Pharmacists | Fall 2001 | US | Characteristics and perceived barriers of PBIS; pharmacist involvement | F, E | From 1998 to the updated survey in 2001, nurse- and pharmacist-administered adult vaccinations increased (16.2% to 30.2% and 2.2% to 6.8%, respectively). |
| Kamal et al. (2003)51 | Cross-sectional | 194 Immunization-certified pharmacists | Prior to August 2001 | US | Pharmacist involvement and satisfaction | F | 92.3% of pharmacists would recommend the certification course. Barriers were assessed for both immunizing and non-immunizing pharmacists. |
| Grabenstein et al. (2002)35 | Retrospective Cohort | 80,462 Pharmacy prescription recipients from 24 Fred Meyer chain pharmacies, 11 in WA and 13 in OR, 4403 pharmacy patients. | 1999 | OR & WA | Customers' vaccination status, choice of immunization provider, and attitudes | F, A | Responders were most likely to return to their previous vaccine provider. Convenience and provider experience were the 2 most influential factors in determining the choice of vaccine provider. |
| Grabenstein et al. (2001)34 | Cohort | 2090 Adult pharmacy patients in either Washington or Oregon, and either age 21–64 with chronic conditions or age ≥65 | Spring 1999 | OR & WA | Customers' vaccination status and choice of immunization provider | F, E | Of the studied cohorts, adults age 21–64 with chronic conditions, and patients who were unvaccinated the year prior had significantly higher vaccination rates in Washington state, which offers PBIS. |
| Ernst et al. (2001)67 | Cross-sectional | 11 Physician offices and 16 community pharmacies, 25 pharmacy customers per site | January 1999 | IA | Patient history and attitudes toward immunizations | A, E | Pharmacists were the second most supported immunizer behind physicians. Patients with prior experience receiving a vaccination at non-traditional sites were more likely to support immunization at pharmacies. |
| Grabenstein et al. (2001)65 | Cross-sectional | 90 Participating pharmacists, 21 pharmacies returned surveys from 17 cities in 10 states. | August 1998-January 1999 | AL, AR, IA, ID, MI, NE, TN, TX, VA, WI | Patient characteristics, history and attitudes toward vaccinations | A, E | Vaccine recipients reported they were treated respectfully, and considered pharmacies to be advantageous because of access, proximity, and/or convenience. |
| Madhavan et al. (2001)43 | Cross-sectional | 1348 Pharmacists | Not Reported | US | Characteristics and perceived barriers of PBIS | F, A, E | Pharmacist involvement in vaccination counseling and promotion were high, while delivery was low. Those who attended educational programs were more involved and perceived barriers to be less problematic. |
| Weitzel and Goode (2000)41 | Cross-sectional | 27 Chain pharmacies | September-December 1998 | VA | Number of influenza and pneumococcal vaccines delivered by pharmacists | F, E | Documents the implementation of pharmacist- and nurse-operated immunization services. The program increased the number of vaccines administered in the years after implementation. |
| Ernst et al. (1997)64 | Implementation Study; Cross-sectional | 1 Independent community pharmacy | Fall 1996 | Rural IA | Accessibility of influenza vaccines | A, E | The steps to establish PBIS at the study pharmacy are reviewed. Almost one third of patients vaccinated at rural PBIS had not been vaccinated the year before, 60% of patients said they would likely not have been vaccinated elsewhere. |
| Grabenstein et al. (1992)68 | Cost Analysis Model | n/a | n/a | n/a | Financial gains and losses for vaccine-advocacy letters; vaccination rates | E | Model indicates that a pharmacist-written letter campaign advocating influenza vaccination could prevent hospitalizations and deaths, and yield a net savings to Medicare. |
Feasibility
Results from studies evaluating the feasibility of pharmacies as a site for adult vaccination clustered around 4 main themes: pharmacist scope of practice (n = 15 studies); certification and training (n = 16 studies); setting and affiliations (n = 15 studies); and reimbursement (n = 9 studies). Sustainability of services, a measure of long-term feasibility, was also observed (n = 5 studies).
The utilization of pharmacies for adult vaccination has been facilitated by an expansion of pharmacists' scope of practice as immunizers. State-level policy changes that allowed pharmacists to directly administer vaccinations to patients were associated with significantly increased pharmacy-17,34,35 and state-level36,37 vaccination rates. Additional regulations in some states that required pharmacists to inform the patient's provider prior to38 or following38-41 vaccination delivery were viewed as barriers by pharmacy staff. Other barriers frequently expressed by pharmacists included concerns about the limiting effect of scope-of-practice policies,42 legal liability,1,43 and ability to treat potential adverse effects.2
Involving other pharmacy personnel also supported the implementation of immunization service offerings. Immunization-certified pharmacy students can support PBIS through direct administration of vaccines,44 assistance with program organization,41 and patient education.45 However, in 2009, 2 y after regulatory changes allowed Arkansas pharmacy students to provide supervised immunizations, only half of practicing Arkansas pharmacists reported they were aware of this training opportunity, and only 33% of pharmacists had allowed a pharmacy student to administer immunizations.40 Pharmacies have employed nurses as immunizers for single-day mass vaccination clinics in pharmacies without PBIS, or operated alongside pharmacists as alternative immunizers. 1,41,43 However, limited frequency of mass vaccination clinics yielded fewer average vaccinations delivered per influenza season for nurses (91–233 doses per pharmacy per season) versus pharmacists (528–807 doses per pharmacy per season).17 Trained pharmacy technicians can also support PBIS through managing workflow, such as processing patient information or billing.41 However pharmacies with greater numbers of pharmacy technicians were associated with fewer total service offerings.46
In studies that discussed pharmacist training, the percentage of pharmacists aware that vaccination was within their scope-of-practice 1,2,42,43 or who were interested in offering vaccinations varied.46,47 A number of studies reported less than 40% of pharmacists were immunization certified,2,38,40,48 however there was considerable variation in certification rates across groups of surveyed pharmacists.39,49,50
Not surprisingly, 3 studies found formal training to be an important factor in incorporating immunization services into community pharmacies.2,48,51 Pharmacists who believed that the ability to vaccinate advanced their field were 7 times more likely to be immunization certified.40 Conversely, non-certified pharmacists commonly cited lack of knowledge or training as a major barrier to participating in immunization services when compared to certified pharmacists.38
In-pharmacy training and formal certification programs, such as those offered by the American Pharmacists Association, are used to train and educate pharmacy students44 and practicing pharmacists51 about immunization practice. Furthermore, immunization certification is now a required element of any accredited Doctor of Pharmacy curriculum.52 Studies found that following in-clinic training, pharmacy students were more self-confident in administering adult vaccinations.44 Pharmacists who had received immunization-related educational training were more willing to vaccinate than those who had not, and found common barriers to be less problematic.43,51 Similarly, immunization-certified pharmacists were much more likely to be involved in some aspect of immunization (99%) than non-certified pharmacists (24%).48 The presence of one or more immunization-certified pharmacists was correlated with the pharmacy offering immunization services,53 and with a transition from no or outsourced services to a pharmacist-delivered immunization system.47,54 However, the number of years a pharmacist has been practicing may be associated with immunization participation. A 2010 study found that pharmacists who had practiced for less than a decade were less likely to have administered vaccinations in the previous year when compared to pharmacists who had practiced for more than 10 y.40
Several studies considered the relationship between the type of pharmacy ownership (e.g. chain, independent, etc.) and feasibility of providing immunization services. Community pharmacies that had a greater number of certified pharmacists were more likely to offer immunization services.46 Certified pharmacists were more likely to work in independent community pharmacies and mass merchandising pharmacies.48 Independent pharmacies were more likely than chain and mass merchandiser pharmacies to be associated with increased and sustained public health service offerings, including PBIS,46,50 and more frequent vaccination administration.1 However, in one study, over half of independent pharmacies abandoned outsourcing immunization services to an external workforce (e.g., visiting nurse vaccinators) and did not adopt in-pharmacy services. The same study found that half of chain and mass-merchandising pharmacies, and a majority of supermarket pharmacies, maintained an outsourcing model of immunization services without further adoption of PBIS.55
Studies of pharmacies' organizational structure determined that compatibility between implementing immunization services and pharmacy structure is necessary for PBIS to become part of standard pharmacy practice.56,57 Staff and management support were considered important for the success of a vaccination program, with lack of support cited as a barrier.40,48 Lack of time and inability to fit immunization services into the workflow was another frequently cited barrier to the adoption of PBIS.1,2,38,40,41,43 Pharmacy staff also expressed concerns about privacy during the vaccination process and lack of space needed to offer the services.2,38,43 Factors such as participation in other public health services like HIV testing and needle exchange, and perceived benefit of PBIS were predictors of in-pharmacy immunization service adoption.50,55,56,58,59 These factors were also associated with the decision to either outsource immunization services to other health professionals or implement in-pharmacy services.46,47 A multi-state survey indicated that a high percentage of pharmacies either lacked interest in or information about how to implement pharmacist-delivered immunization services.47
While many pharmacist-administered vaccines are covered under a number of private insurance plans, as well as Medicare Part B and D,60-62 reimbursement and insurance logistics were cited as barriers for both patients and pharmacists.38,46 Pharmacists reported that the level of insurance reimbursement was a barrier in their provision of vaccinations.1,43 Similarly, insurance coverage and out-of-pocket costs were perceived as 2 potential barriers for patients.1,39,43,63 Moreover, patients reported that insurance coverage and their perceived ability to pay were important factors in selecting their vaccination site.35,39 Several strategies, including the implementation of an insurance assessment step prior to vaccination, were reported to simplify the reimbursement and billing processes for patients.42,63
The sustainability of PBIS is a key determinant of the effectiveness and future outcomes of pharmacies as sites of adult vaccination. Compatibility of PBIS with pharmacy services or pharmacist and staff attitudes toward offering immunization services were influential in determining program sustainability.50,55,56,58 Two main pathways to sustain practice-site innovations were identified: 1) a continuous process of assessment, modification and adaptation; or 2) having an “operational champion” with insider knowledge of the organizational structures to ensure PBIS fit within existing structures.56 Discontinuation of in-pharmacy services was commonly reported when challenges or barriers to PBIS outweighed perceived benefit or revenue; state-level discontinuation rates ranged from 3 to 23%.47
Acceptability
The included studies captured 2 main sub-categories of acceptance: pharmacist or pharmacy staff's comfort providing PBIS (n = 5 studies), and patient's acceptance of PBIS (n = 6 studies). Pharmacists48,49 and pharmacy staff59 both generally had positive attitudes about PBIS. However, several studies cited pharmacists' discomfort with carrying out different aspects of immunization services,2 including administering vaccinations, managing any adverse events, billing procedures, and patient counseling.43
Several factors influenced patient acceptance of pharmacies as sites for vaccination, including convenience, accessibility, and expanded hours of operation.25,35,64,65 Most patients felt comfortable with pharmacists delivering vaccinations in pharmacies, with pharmacists ranked the second most highly trusted immunizers65,66 after physicians.67 Overall, patients were more likely to return to the same vaccination sites as previous vaccinations, including patients who used pharmacies or other non-traditional immunizers. 35,67
Effectiveness
Twenty studies reported the effect of PBIS on patient vaccination rates as a primary outcome measure. Other outcome measures including the cost-effectiveness of PBIS (n = 5 studies), and their impact on health disparities and access among medically at-risk or underserved populations (n = 19 studies).
The implementation and expansion of immunization programs in community pharmacies generally increased the number of vaccinations administered.17,37,41,43,49,57,65 In particular, pharmacy-based vaccination appears to have been effective in increasing influenza vaccination rates among patients who had missed the previous year or who would not have otherwise received an influenza vaccine.34,35,64,65
In addition to administering vaccines, pharmacist participation in vaccination counseling and advocacy increased from 1998 to 2001.1 An early cost analysis model predicted that letters from pharmacists that prompted patients to receive vaccinations could hypothetically decrease influenza healthcare utilization costs through increased vaccination rates among letter recipients.68 Subsequent studies demonstrated that advertising pharmacy immunization programs was correlated with increased profits for pharmacies due to increased vaccine administration and the profitability of vaccination delivery.69 Active or personalized methods (e.g., direct communication with customers, personalized letters, and educational interventions) were shown to be more effective at increasing immunization rates than passive or general methods.45,66,70,71 Other methods of advertising, such as flyers and automated voice messages, were shown to increase vaccination rates to varying degrees. 66,68-70,72,73
Several studies examined the cost-effectiveness of PBIS. A recent study of 2 major health insurance claims databases revealed that, on average, the total cost of influenza and pneumococcal vaccination were lower in pharmacies than in physician offices for both patients and insurers; however, the zoster vaccine had a lower cost in physicians' offices.23 When examining the costs of immunization programs in individual pharmacies, studies show more variability. The maintenance of pharmacy services were largely cost-effective for influenza 74,75 and herpes zoster vaccination programs.63,69,75 One study cited a net loss for pneumococcal vaccinations at a single independent pharmacy.75 Prosser et al. (2008) determined that pharmacies were more cost-effective sites of vaccination than physicians' offices due to decreased time spent waiting and lower operation costs.74
PBIS are uniquely positioned to improve access to vaccines through non-traditional service offerings. Community pharmacies offered more consistent hours and days of operation, and more flexible scheduling than physicians' offices or public health clinics.17,41,64,65 One study of a national pharmacy chain found that 30.5% of the more than 6 million vaccines doses dispensed were administered during nights, weekends and holidays. Additionally, more than one million vaccinations (17.5% of all vaccinations) were administered during lunch hours (11am-1pm). Uninsured patients were more likely to be vaccinated during these off-clinic hours than individuals with insurance. 24
There is mixed evidence about the potential for PBIS to reduce geographic and socioeconomic disparities in vaccine access. A study of pharmacy offerings in Wayne County, Michigan reported that pharmacies located in lower income ZIP codes and areas with a higher percentage of minorities were less likely to offer PBIS.76 A 2012 study of a large national chain pharmacy highlighted that 41% of the chain's locations service medically underserved areas throughout the United States, and 37.7% of influenza vaccines delivered were administered in medically underserved areas.25 Similarly, patients living in smaller towns were more likely to receive vaccinations in non-traditional settings, such as pharmacies.67 Another study examining PBIS in New York City found that pharmacy staff at pharmacies located in predominately racial and ethnic minority neighborhoods were significantly less likely to be supportive of PBIS, while pharmacies located in neighborhoods with greater numbers of immigrants were only marginally supportive of these services.59 Finally, a 2013 study reported that both white and black community pharmacy patients had significantly higher influenza vaccination rates than responders who did not fill prescriptions at community pharmacies, but racial disparities between these groups of patients were significant in both pharmacy and non-pharmacy populations.77
Pharmacies may also effectively reach medically high-risk populations. Pharmacy staff are capable of identifying patients who meet the recommendation criteria for certain vaccinations based on the patient's health status and prescription history.37,64,78 Vaccine promotion practices at pharmacies were able to increase herpes zoster vaccination 45,66,70,72 and influenza vaccination rates36,64 in 2 target populations for this vaccine: patients 65 y or older and patients between the ages of 18–64 with co-morbid chronic conditions.34,49
Discussion
Our review of published literature shows that pharmacies are capable of successfully implementing cost-effective in-house immunization services, which in turn can increase adult vaccination rates. We found that policy changes have expanded pharmacy services, while training programs have engaged pharmacists and pharmacy staff in immunization practices. Pharmacies are uniquely positioned as vaccination sites. For patients, they offer a convenient and accessible alternative for immunization services. Results also indicate that PBIS are an effective method of increasing vaccination rates at both the pharmacy- and state-level, particularly among medically underserved populations. Furthermore, as pharmacies continue to expand primary and preventative care services, PBIS offer cost-effective business opportunities. Yet, despite these benefits, many legal, organizational, and attitudinal barriers hinder the feasibility and effectiveness of pharmacy immunization initiatives. Targeted research interventions and innovative approaches to overcome these barriers can improve the implementation and sustainability of PBIS.
Despite the policy changes that allowed pharmacists to administer vaccinations, state scope-of-practice policies such as the variety of vaccines offered, and Medicare Part B and D reimbursement methods, continue to shape PBIS feasibility and impact.18,60,79 While these regulations help to maintain complete and accurate patient records, they may unintentionally lead to “missed opportunities” to vaccinate. Moreover, the additional demands placed on pharmacists and their staff to complete these requirements may ultimately pose a barrier for pharmacy involvement in immunization services.38,39,41 Several studies have documented the potential effects of past scope-of-practice regulatory expansions that allowed for pharmacists to immunize, yielding higher state-level vaccination rates and increased access.36-39,41,43 Yet, there is scant research on the impact of current policies on vaccination rates or PBIS service offerings. Further research may provide a better understanding of these effects and identify regulations that better facilitate the implementation of PBIS.
While many of the reviewed studies reveal that PBIS are feasible and acceptable, barriers at many levels still persist. Future research and interventions to address these remaining impediments can target 3 potential areas. First, efforts can be made to ensure that pharmacists and other personnel involved in PBIS are able to provide vaccinations effectively. Immunization training is a necessary prerequisite to providing PBIS and can help decrease the burden of certain barriers.43,51 However, this is not sufficient to ensure or maintain pharmacists' participation in PBIS, as evidenced by immunization-certified pharmacists who are not actively involved with PBIS or who have discontinued offering immunizations due to difficulties encountered after certification.38,40,55 In order to maintain immunization services, additional resources beyond certification are needed to efficiently train pharmacists, such as the RxVaccinate program which provides training and tools for PBIS implementation.57 Evidence indicates that the integration of pharmacy technicians and students into immunization delivery can relieve the strain of organizational barriers and led to greater health promotion and administration of vaccinations.41,45 These experiences allow pharmacy students to gain clinical exposure to immunization services while strengthening the connection between pharmacy schools and the surrounding community pharmacies.53 Initiatives to involve nurses and physicians in PBIS may further promote collaborative approaches to improving primary and preventative care services for patients.
The second target area for increasing the effectiveness of PBIS is addressing organizational and logistical concerns to increase perceived compatibility between PBIS and the pharmacy. An existing body of evidence has identified several determinants of successful and sustainable pharmacy innovations50,55,58 that can inform future interventions. Further research is needed on how to tailor pharmacy-based immunization services to match heterogeneous practice sites.43 Planning and implementation should occur at multiple levels by preparing individual personnel, adapting PBIS to the specific pharmacy site, and addressing organizational and attitudinal barriers.57,79
Lastly, interventions to increase effectiveness can leverage the potential financial benefits of PBIS. PBIS represent a financially feasible alternative to traditional immunization sites; however, efforts should be made to address the existing billing and reimbursement barriers to mitigate lost opportunities to provide vaccinations. There has been little research into optimal financing mechanisms and billing procedures;79 our results indicate that streamlining PBIS billing and reimbursement could improve feasibility.
In the era of the Affordable Care Act (ACA), pharmacies are well-positioned to provide affordable, accessible preventative health services, including vaccination.14,79 The ACA instituted measures to increase access and funding for preventative health services including mandated insurance coverage of ACIP-recommended vaccinations when delivered by in-network providers.80,81 However, pharmacies are still largely considered out-of-network providers and the ACA did not change the terms of Medicare Part D coverage, which create additional challenges for both patients and pharmacists pursuing insurance coverage and reimbursement. Higher rates of insured adults and a greater emphasis on providing services through patient-centered medical homes will likely influence the utilization and sustainability of PBIS. Further evaluation of the effect of the ACA on pharmacy-based programs and vaccination delivery is needed to support the long-term effectiveness of PBIS.
Limitations
There are several limitations to consider in this review. Due to the asynchronous expansion of states' scope-of-practice regulation and differential adoption of PBIS in pharmacies, the included studies report pharmacy practices at different stages of implementation and operation. The rapidly changing nature and variability of PBIS creates a temporal aspect that should be considered in the interpretation of results and conclusions. Our conclusions are drawn primarily from observational studies, limiting our ability to infer casual relationships or fully account for confounders or biases. Additionally, community pharmacies were largely analyzed as homogenous practice settings, both in the literature and in this review, despite differences in ownership, management structure, geographic location and time period that may potentially influence practice. Therefore, further studies addressing these confounding factors are needed.
Conclusions
The certification of pharmacist immunizers and integration of immunization programs into the daily routine of pharmacy services greatly facilitates pharmacies as sites of adult vaccination. The studies we analyzed support PBIS as cost-effective innovations that have made considerable contributions to adult vaccination rates. This effect is particularly notable in pharmacies' ability to engage under-vaccinated populations that have been difficult to reach through traditional methods. The sustainability of pharmacy-based immunization programs depends on individual pharmacy characteristics and attitudes of pharmacists and pharmacy management. Remaining barriers to immunization services are multifactorial, and will require strategic interventions and approaches that address the individual-, pharmacy-, and state-level factors. This review provides a critical perspective on the feasibility, acceptability, and effectiveness of PBIS, as well as recommendations for future research and practice of immunization delivery in community pharmacies.
Disclosure of potential conflicts of interest
No conflicts of interest were reported by the authors of this paper.
Funding
This research was funded by a training grant in comparative effectiveness research from the National Cancer Institute (KM1CA156715) and by the Leonard Davis Institute for Health Economics of the University of Pennsylvania.
Author contributions
R. Burson conducted the systematic review and study selection (including title review, abstract review, and full-text review), carried out quality assessment, data extraction and analysis, drafted the article, and prepared figures and tables. K. Feemster and A. Buttenheim originated and guided the study, reviewed data extraction and quality assessment. All authors contributed to the article through critical revision. All authors approved the final article. The authors of this study reported no financial disclosures.
References
- [1].Kamal KM, Madhavan SS, Maine LL. Pharmacy and immunization services: pharmacists' participation and impact. J Am Pharm Assoc 2003; 43(4):470-82; http://dx.doi.org/ 10.1331/154434503322226211; http://173.193.11.207/data/Journals/JAPhA/20401/10.1331_154434503322226211.pdf (accessed July3, 2013) [DOI] [PubMed] [Google Scholar]
- [2].Capurso KA, Powers MF. Barriers to implementing a phamacist-run immunization service, as perceived by pharmacists, in a community pharmacy chain. J Pharm Technol 2006; 22(2):91-4; http://dx.doi.org/ 10.1177/875512250602200204 [DOI] [Google Scholar]
- [3].National Center for Health Statistics. Healthy People 2010 Final Review US Department of Health and Human Services. 2012. http://www.cdc.gov/nchs/healthy_people/hp2010/hp2010_final_review.htm (accessed June26, 2016) [Google Scholar]
- [4].National Center for Health Statistics. Healthy People 2000 Final Review US Department of Health and Human Services. 2001. http://www.cdc.gov/nchs/healthy_people/hp2010/hp2010_final_review.htm (accessed June26, 2016) [Google Scholar]
- [5].Williams WW, Lu P-J, O'Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al.. Surveillance of vaccination coverage among adult populations — United States, 2014. MMWR Surveill Summ 2016; 65(1):1-36; PMID:26844596; http://dx.doi.org/ 10.15585/mmwr.ss6501a1 [DOI] [PubMed] [Google Scholar]
- [6].Office of Disease Prevention and Health Promotion Healthy People 2020, Objctives IID 1.1–33. US Department of Health and Human Services; https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives (accessed June 26, 2016) [Google Scholar]
- [7].Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med 2008; 121(7 Suppl 2):S28-S35; PMID:18589065; http://dx.doi.org/ 10.1016/j.amjmed.2008.05.005 [DOI] [PubMed] [Google Scholar]
- [8].Bodenheimer T. Primary Care — Will It Survive? N Engl J Med 2006; 355(9):861-4; PMID:16943396; http://dx.doi.org/ 10.1056/NEJMp068155 [DOI] [PubMed] [Google Scholar]
- [9].Centers for Disease Control and Prevention Adult immunization programs in nontraditional settings: quality standards and guidance for program evaluation. Morb Mortal Wkly Rep 2000; 49:243-8. [PubMed] [Google Scholar]
- [10].Skelton JB. American Pharmacists Association, Academy of Managed Care Pharmacy. Pharmacist-provided immunization compensation and recognition: white paper summarizing APhA/AMCP stakeholder meeting. J Am Pharm Assoc JAPhA 2011; 51(6):704-12; http://dx.doi.org/ 10.1331/JAPhA.2011.11544 [DOI] [PubMed] [Google Scholar]
- [11].National Association of Chain Drug Stores RxIMPACT 2014: community pharmacy fills gaps in access and affordability for patients, payers. 2013. http://www.drugstorenews.com/sites/drugstorenews.com/files/RxImpact_2014.pdf (accessed January9, 2015) [Google Scholar]
- [12].Mehrotra A, Lave JR. Visits to retail clinics grew fourfold from 2007 to 2009, although their share of overall outpatient visits remains low. Health Aff (Millwood) 2012; 31(9):2123-9; PMID:22895454; http://dx.doi.org/ 10.1377/hlthaff.2011.1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mehrotra A, Liu H, Adams JL, Wang MC, Lave JR, Thygeson NM, Solberg LI, McGlynn EA. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med 2009; 151(5):321-8; PMID:19721020; http://dx.doi.org/ 10.7326/0003-4819-151-5-200909010-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Maine LL, Knapp KK, Scheckelhoff DJ. Analysis & commentary: Pharmacists and technicians can enhance patient care even more once national policies, practices, and priorities are aligned. Health Aff (Millwood) 2013; 32(11):1956-62; PMID:24191086; http://dx.doi.org/ 10.1377/hlthaff.2013.0529 [DOI] [PubMed] [Google Scholar]
- [15].Hogue MD, Grabenstein JD, Foster SL, Rothholz MC. Pharmacist involvement with immunizations: a decade of professional advancement. J Am Pharm Assoc JAPhA 2006; 46(2):168-79; quiz 179-182; http://dx.doi.org/ 10.1331/154434506776180621 [DOI] [PubMed] [Google Scholar]
- [16].Grabenstein JD. Pharmacists and immunization: increasing involvement over a century. Pharm Hist 1999; 41(4):137-52; PMID:11624486 [PubMed] [Google Scholar]
- [17].Grabenstein JD. Daily versus single-day offering of influenza vaccine in community pharmacies. J Am Pharm Assoc 2009; 49(5):628-31; http://dx.doi.org/ 10.1331/JAPhA.2009.08118 [DOI] [PubMed] [Google Scholar]
- [18].Rothholz MC. Role of community pharmacies/pharmacists in vaccine delivery in the United States. 2013. http://www.pharmacist.com/role-community-pharmaciespharmacists-vaccine-delivery-united-states-0 (accessed February 2, 2016) [Google Scholar]
- [19].American Pharmacists Association Pharmacist authority to immunize. 2016. http://www.pharmacist.com/sites/default/files/files/Slides%20on%20Pharmacist%20IZ%20Authority_2_1_16.pptx?dfptag=imz (accessed June17, 2016) [Google Scholar]
- [20].American Pharmacists Association 2015 Annual Report: Expanding Opportunities through Patient Care. 2015. http://www.pharmacist.com/hero/2015-annual-report (accessedJune17, 2016)
- [21].Keely JL, Herald MT, Harris JP, American College of Physicians-American Society of Internal Medicine . Pharmacist scope of practice. Ann Intern Med 2002; 136(1):79-85. [DOI] [PubMed] [Google Scholar]
- [22].Kennedy ED, Santibanez TA, Bridges CB, Singleton JA. Flu vaccination coverage, national flu survey, March 2012. Centers for Disease Control and Prevention; 2012. http://www.cdc.gov/flu/fluvaxview/nfs-survey-march2012.htm#place (accessed September 1, 2015) [Google Scholar]
- [23].Singhal PK, Zhang D. Costs of adult vaccination in medical settings and pharmacies: an observational study. J Manag Care Pharm JMCP 2014; 20(9):930-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Goad JA, Taitel MS, Fensterheim LE, Cannon AE. Vaccinations administered during off-clinic hours at a national community pharmacy: implications for increasing patient access and convenience. Ann Fam Med 2013; 11(5):429-36; PMID:24019274; http://dx.doi.org/ 10.1370/afm.1542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Murphy PA, Frazee SG, Cantlin JP, Cohen E, Rosan JR, Harshburger DE. Pharmacy provision of influenza vaccinations in medically underserved communities. J Am Pharm Assoc 2012; 52(1):67-70; http://dx.doi.org/ 10.1331/JAPhA.2012.10070 [DOI] [PubMed] [Google Scholar]
- [26].Srivastav A, Santibanez TA, Kahn KE, Zhai Y, Greby SM, Bridges C, Lu P-J, Williams WW, Singleton JA, Stinger MC, et al.. National early season flu vaccination coverage, United States, November 2014. Centers for Disease Control and Prevention. 2014. http://www.cdc.gov/flu/fluvaxview/nifs-estimates-nov2014.htm (accessed January31, 2015) [Google Scholar]
- [27].Maine LL, Rothholz MC. Pharmacy-based immunizations–an idea whose time has come. J Am Pharm Assoc WashingtonDC 1996 2001; 41(1):13-4. [DOI] [PubMed] [Google Scholar]
- [28].Tabuchi H. How CVS quit smoking and grew into a health care giant. The New York Times. 2015. http://www.nytimes.com/2015/07/12/business/how-cvs-quit-smoking-and-grew-into-a-health-care-giant.html (accessed July24, 2015) [Google Scholar]
- [29].Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4):264-9; PMID:19622511; http://dx.doi.org/ 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- [30].Kim DK, Bridges CB, Harriman KH, Advisory Committee on Immunization Practices (ACIP), ACIP Adult Immunization Work Group . Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older — United States, 2016. MMWR Morb Mortal Wkly Rep 2016; 65(4):88-90; PMID:26845417; http://dx.doi.org/ 10.15585/mmwr.mm6504a5 [DOI] [PubMed] [Google Scholar]
- [31].Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2012; 18(1):12-8; http://dx.doi.org/ 10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed] [Google Scholar]
- [32].Wells GA, Shea B, O'connell D, Robertson J, Peterson J, Welch V, Losos M, Tugwell P. The newcastle-ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. http://www.medicine.mcgill.ca/rtamblyn/Readings/The%20Newcastle%20-%20Scale%20for%20assessing%20the%20quality%20of%20nonrandomised%20studies%20in%20meta-analyses.pdf (accessed January7, 2015) [Google Scholar]
- [33].National Institutes of Health. National Heart, Lung, and Blood Institute Quality assessment tool for observational cohort and cross-sectional studies. 2014. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort (accessed January6, 2015) [Google Scholar]
- [34].Grabenstein JD, Guess HA, Hartzema AG, Koch GG, Konrad TR. Effect of vaccination by community pharmacists among adult prescription recipients. Med Care 2001; 39(4):340-8; PMID:11329521; http://dx.doi.org/ 10.1097/00005650-200104000-00005 [DOI] [PubMed] [Google Scholar]
- [35].Grabenstein JD, Guess HA, Hartzema AG, Koch GG, Konrad TR. Attitudinal factors among adult prescription recipients associated with choice of where to be vaccinated. J Clin Epidemiol 2002; 55(3):279-84; PMID:11864799; http://dx.doi.org/ 10.1016/S0895-4356(01)00452-8 [DOI] [PubMed] [Google Scholar]
- [36].Steyer TE, Ragucci KR, Pearson WS, Mainous AG III. The role of pharmacists in the delivery of influenza vaccinations. Vaccine 2004; 22(8):1001-6; PMID:15161077; http://dx.doi.org/ 10.1016/j.vaccine.2003.08.045 [DOI] [PubMed] [Google Scholar]
- [37].Bearden DT, Holt T. Statewide impact of pharmacist-delivered adult influenza vaccinations. Am J Prev Med 2005; 29(5):450-2; PMID:16376709; http://dx.doi.org/ 10.1016/j.amepre.2005.08.003 [DOI] [PubMed] [Google Scholar]
- [38].Kummer GL, Foushee LL. Description of the characteristics of pharmacist-based immunization services in North Carolina: results of a pharmacist survey. J Am Pharm Assoc 2008; 48(6):744-51; http://dx.doi.org/ 10.1331/JAPhA.2008.07080 [DOI] [PubMed] [Google Scholar]
- [39].Pilisuk T, Goad J, Backer H. Vaccination delivery by chain pharmacies in California: results of a 2007 survey. J Am Pharm Assoc 2010; 50(2):134-9; http://dx.doi.org/ 10.1331/JAPhA.2010.09168 [DOI] [PubMed] [Google Scholar]
- [40].Pace AC, Flowers SK, Hastings JK. Arkansas community pharmacists' opinions on providing immunizations. J Pharm Pract 2010; 23(5):496-501; PMID:21507853; http://dx.doi.org/ 10.1177/0897190010362105 [DOI] [PubMed] [Google Scholar]
- [41].Weitzel KW, Goode JV. Implementation of a pharmacy-based immunization program in a supermarket chain. J Am Pharm Assoc 2000; 40(2):252-6; http://dx.doi.org/ 10.1016/S1086-5802(16)31066-X [DOI] [PubMed] [Google Scholar]
- [42].Penfold RB, Rusinak D, Lieu TA, Shefer A, Messonnier M, Lee GM. Financing and systems barriers to seasonal influenza vaccine delivery in community settings. Vaccine 2011; 29(52):9632-9; PMID:22036886; http://dx.doi.org/ 10.1016/j.vaccine.2011.10.041 [DOI] [PubMed] [Google Scholar]
- [43].Madhavan SS, Rosenbluth SA, Amonkar M, Borker RD, Richards T. Pharmacists and immunizations: a national survey. J Am Pharm Assoc 2001; 41(1):32-45; http://dx.doi.org/ 10.1016/S1086-5802(16)31203-7 [DOI] [PubMed] [Google Scholar]
- [44].Turner CJ, Ellis S, Giles J, Altiere R, Sintek C, Ulrich H, Valdez C, Zadvorny E. An introductory pharmacy practice experience emphasizing student-administered vaccinations. Am J Pharm Educ 2007; 71(1): 3; PMID:17429503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Teeter BS, Garza KB, Stevenson TL, Williamson MA, Zeek ML, Westrick SC. Factors associated with herpes zoster vaccination status and acceptance of vaccine recommendation in community pharmacies. Vaccine 2014; 32(43):5749-54; PMID:25171848; http://dx.doi.org/ 10.1016/j.vaccine.2014.08.040 [DOI] [PubMed] [Google Scholar]
- [46].Doucette WR, Kreling DH, Schommer JC, Gaither CA, Mott DA, Pedersen CA. Evaluation of community pharmacy service mix: Evidence from the 2004 National Pharmacist Workforce Study. J Am Pharm Assoc 2006; 46(3):348-55; http://dx.doi.org/ 10.1331/154434506777069471 [DOI] [PubMed] [Google Scholar]
- [47].Westrick SC, Mount JK, Watcharadamrongkun S, Breland ML. Pharmacy stages of involvement in pharmacy-based immunization services: results from a 17-state survey. J Am Pharm Assoc 2008; 48(6):764-73; http://dx.doi.org/ 10.1331/JAPhA.2008.07118 [DOI] [PubMed] [Google Scholar]
- [48].Neuhauser MM, Wiley D, Simpson L, Garey KW. Involvement of immunization-certified pharmacists with immunization activities. Ann Pharmacother 2004; 38(2):226-31; PMID:14742755; http://dx.doi.org/ 10.1345/aph.1D257 [DOI] [PubMed] [Google Scholar]
- [49].Goode J-VR, Mott DA, Stanley DD. Assessment of an immunization program in a supermarket chain pharmacy. J Am Pharm Assoc 2007; 47(4):495-8; http://dx.doi.org/ 10.1331/JAPhA.2007.06100 [DOI] [PubMed] [Google Scholar]
- [50].Westrick SC. Pharmacy characteristics, vaccination service characteristics, and service expansion: an analysis of sustainers and new adopters. J Am Pharm Assoc 2010; 50(1):52-61; http://dx.doi.org/ 10.1331/JAPhA.2010.09036 [DOI] [PubMed] [Google Scholar]
- [51].Kamal KM, Madhavan SS, Maine LL. Impact of the American pharmacists association's (APhA) immunization training certification program. Am J Pharm Educ 2003; 67(4); http://dx.doi.org/ 10.5688/aj6704124 [DOI] [PubMed] [Google Scholar]
- [52].Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree: Standards 2016 Chicago, IL: Accreditation Coucil for Pharmacy Education; 2015. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed June19, 2016) [Google Scholar]
- [53].Westrick SC, Mount J, Watcharadamrongkun S. College/school of pharmacy affiliation and community pharmacies' involvement in public health activities. Am J Pharm Educ 2009; 73(7):123; PMID:19960082; http://dx.doi.org/ 10.5688/aj7307123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Westrick SC, Watcharadamrongkun S, Mount JK, Breland ML. Community pharmacy involvement in vaccine distribution and administration. Vaccine 2009; 27(21):2858-63; PMID:19428895; http://dx.doi.org/ 10.1016/j.vaccine.2009.02.086 [DOI] [PubMed] [Google Scholar]
- [55].Westrick SC. Forward and backward transitions in pharmacy-based immunization services. Res Soc Adm Pharm 2010; 6(1):18-31; http://dx.doi.org/ 10.1016/j.sapharm.2009.02.001 [DOI] [PubMed] [Google Scholar]
- [56].Westrick SC, Breland ML. Sustainability of pharmacy-based innovations: the case of in-house immunization services. J Am Pharm Assoc 2009; 49(4):500-8; http://dx.doi.org/ 10.1331/JAPhA.2009.08055 [DOI] [PubMed] [Google Scholar]
- [57].Westrick SC, Owen J, Hagel H, Owensby JK, Lertpichitkul T. Impact of the RxVaccinate program for pharmacy-based pneumococcal immunization: A cluster-randomized controlled trial. J Am Pharm Assoc JAPhA 2016; 56(1):29-36.e1; http://dx.doi.org/ 10.1016/j.japh.2015.11.010 [DOI] [PubMed] [Google Scholar]
- [58].Westrick SC, Mount JK. Impact of perceived innovation characteristics on adoption of pharmacy-based in-house immunization services. Int J Pharm Pract 2009; 17(1):39-46; PMID:20218028; http://dx.doi.org/ 10.1211/ijpp.17.1.0006 [DOI] [PubMed] [Google Scholar]
- [59].Crawford ND, Blaney S, Amesty S, Rivera AV, Turner AK, Ompad DC, Fuller CM. Individual- and neighborhood-level characteristics associated with support of in-pharmacy vaccination among ESAP-registered pharmacies: pharmacists' role in reducing racial/ethnic disparities in influenza vaccinations in New York City. J Urban Health Bull N Y Acad Med 2011; 88(1):176-85; http://dx.doi.org/ 10.1007/s11524-010-9541-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Centers for Medicare & Medicaid Services Vaccine and vaccine administration payments under Medicare Part D. MLN Matters. 2015. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Vaccines-Part-D-Factsheet-ICN908764.pdf (accessed February 2, 2016) [Google Scholar]
- [61].Cigna Cigna medical vaccine program directory. 2015. https://my.cigna.com/teamsitepublic/js/partner/bni/833008_CIGNA_Pharmacy_Vaccine_Program_Directory.pdf (accessed February 2, 2016) [Google Scholar]
- [62].UnitedHealthCare Adult vaccinations. June 2015. http://consultant.uhc.com/assets/FINAL%20100-13060-external-adult-vaccination-flier-2015.pdf (accessed January31, 2015) [Google Scholar]
- [63].Wood HM, McDonough RP, Doucette WR. Retrospective financial analysis of a herpes zoster vaccination program from an independent community pharmacy perspective. J Am Pharm Assoc 2009; 49(1):12-7; http://dx.doi.org/ 10.1331/JAPhA.2009.08030 [DOI] [PubMed] [Google Scholar]
- [64].Ernst ME, Chalstrom CV, Currie JD, Sorofman B. Implementation of a community pharmacy-based influenza vaccination program. J Am Pharm Assoc 1997; 37(5):570-80; http://dx.doi.org/ 10.1016/S1086-5802(16)30253-4 [DOI] [PubMed] [Google Scholar]
- [65].Grabenstein JD, Guess HA, Hartzema AG. People vaccinated by pharmacists: descriptive epidemiology. J Am Pharm Assoc 2001; 41(1):46-52; http://dx.doi.org/ 10.1016/S1086-5802(16)31204-9 [DOI] [PubMed] [Google Scholar]
- [66].Wang J, Ford LJ, Wingate L, Uroza SF, Jaber N, Smith CT, Randolph R, Lane S, Foster SL. Effect of pharmacist intervention on herpes zoster vaccination in community pharmacies. J Am Pharm Assoc 2013; 53(1):46-53; http://dx.doi.org/ 10.1331/JAPhA.2013.12019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Ernst ME, Bergus GR, Sorofman BA. Patients' acceptance of traditional and nontraditional immunization providers. J Am Pharm Assoc 2001; 41(1):53-59; http://dx.doi.org/ 10.1016/S1086-5802(16)31205-0 [DOI] [PubMed] [Google Scholar]
- [68].Grabenstein JD, Hartzema AG, Guess HA, Johnston WP, Rittenhouse BE. Community pharmacists as immunization advocates. Cost-effectiveness of a cue to influenza vaccination. Med Care 1992; 30(6):503-13; PMID:1593916; http://dx.doi.org/ 10.1097/00005650-199206000-00004 [DOI] [PubMed] [Google Scholar]
- [69].Hedden MA, Kuehl PG, Liu Y. Economic analysis of a herpes zoster vaccination program in 19 affiliated supermarket pharmacies. J Am Pharm Assoc 2014; 5 4(4):390-6; http://dx.doi.org/ 10.1331/JAPhA.2014.13140 [DOI] [PubMed] [Google Scholar]
- [70].Bryan AR, Liu Y, Kuehl PG. Advocating zoster vaccination in a community pharmacy through use of personal selling. J Am Pharm Assoc 2013; 53(1):70-7; http://dx.doi.org/ 10.1331/JAPhA.2013.11097 [DOI] [PubMed] [Google Scholar]
- [71].Marrero W, Hernández L, García R, Gutiérrez LM. Programa de inmunización contra la influenza para adultos de 65 años o más en una farmacia de comunidad en Puerto Rico. P R Health Sci J 2006; 25(1):35-42; PMID:16883677 [PubMed] [Google Scholar]
- [72].Hess R. Impact of automated telephone messaging on zoster vaccination rates in community pharmacies. J Am Pharm Assoc 2013; 53(2):182-7; http://dx.doi.org/ 10.1331/JAPhA.2013.12222 [DOI] [PubMed] [Google Scholar]
- [73].Brackett A, Butler M, Chapman L. Using motivational interviewing in the community pharmacy to increase adult immunization readiness: A pilot evaluation. J Am Pharm Assoc JAPhA 2015; 55(2):182-6; http://dx.doi.org/ 10.1331/JAPhA.2015.14120 [DOI] [PubMed] [Google Scholar]
- [74].Prosser LA, O'Brien MA, Molinari N-AM, Hohman KH, Nichol KL, Messonnier ML, Lieu TA. Non-traditional settings for influenza vaccination of adults: costs and cost effectiveness. PharmacoEconomics 2008; 26(2):163-78; PMID:18198935; http://dx.doi.org/ 10.2165/00019053-200826020-00006 [DOI] [PubMed] [Google Scholar]
- [75].Doucette WR, McDonough RP, Mormann MM, Vaschevici R, Urmie JM, Patterson BJ. Three-year financial analysis of pharmacy services at an independent community pharmacy. J Am Pharm Assoc 2012; 52(2):181-7; http://dx.doi.org/ 10.1331/JAPhA.2012.11207 [DOI] [PubMed] [Google Scholar]
- [76].Erickson SR, Workman P. Services provided by community pharmacies in Wayne County, Michigan: a comparison by ZIP code characteristics. J Am Pharm Assoc JAPhA 2014; 54(6):618-24; http://dx.doi.org/ 10.1331/JAPhA.2014.14105 [DOI] [PubMed] [Google Scholar]
- [77].Wang J, Munshi KD, Hong SH. Racial and ethnic disparities in influenza vaccinations among community pharmacy patients and non-community pharmacy respondents. Res Soc Adm Pharm 2013; 10(1):126-40; http://dx.doi.org/ 10.1016/j.sapharm.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Taitel M, Cohen E, Duncan I, Pegus C. Pharmacists as providers: targeting pneumococcal vaccinations to high risk populations. Vaccine 2011; 29(45):8073-6; PMID:21864625; http://dx.doi.org/ 10.1016/j.vaccine.2011.08.051 [DOI] [PubMed] [Google Scholar]
- [79].Ko KJ, Wade RL, Yu HT, Miller RM, Sherman B, Goad J. Implementation of a pharmacy-based adult vaccine benefit: Recommendations for a commercial health plan benefit. J Manag Care Pharm 2014; 20(3):273-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Shaw FE, Asomugha CN, Conway PH, Rein AS. The Patient Protection and Affordable Care Act: opportunities for prevention and public health. The Lancet 2014; 384(9937):75-82; http://dx.doi.org/ 10.1016/S0140-6736(14)60259-2 [DOI] [PubMed] [Google Scholar]
- [81].Koh HK, Sebelius KG. Promoting prevention through the affordable care act. N Engl J Med 2010; 363(14):1296-9; PMID:20879876; http://dx.doi.org/ 10.1056/NEJMp1008560 [DOI] [PubMed] [Google Scholar]


