Abstract
Objective
Post-mortem examination can provide important information about the cause of death and play a significant role in the bereavement process. Autopsies reveal previous unknown medical problems approximately 20–30% of the time. A non-invasive MRI-based post-mortem examination (PM-MRI) may provide an alternative for families who do not consent to an autopsy.
Study Design
This study was a prospective observational study of recently expired neonates and infants. Subjects underwent a full body MRI scan (brain, chest, abdomen and pelvis) followed by conventional autopsy if the family desired to have one. MRI results were compared to autopsy findings and the ante mortem clinical diagnosis. A follow-up survey was conducted to investigate family perceptions of the PM-MRI process.
Result
Thirty-one infants underwent full PM-MRI. 19/31 (61%) of infants had complete agreement between the clinician’s impression and PM-MRI. Twenty-four infants also had conventional autopsy, with 14/24 (58%) infants having PM-MRI results consistent with autopsy findings. PM-MRI was superior at detection of free intraperitoneal/intrathoracic air and hepatic iron overload. Whole body PM-MRI did not have the resolution to detect focal/microscopic injury, vascular remodeling and some forms of brain injury. Of those families who remembered the PM-MRI findings, the majority felt that the information was useful.
Conclusion
PM-MRI studies may provide an important adjunct to conventional autopsy and a substitute when the latter is not possible for personal or religious reasons. Clinicians should be aware of, and communicate with the family, the resolution limits of the whole body PM-MRI to detect certain types of injury.
Keywords: autopsy, follow-up, pathology, bereavement, MRI
INTRODUCTION
Historically, the post-mortem examination or autopsy has provided vital information to physicians and families of the deceased about abnormalities in anatomy or pathological conditions.1,2 Autopsies allow for the confirmation of the suspected ante-mortem clinical diagnosis, an important component of the bereavement process, allowing the family to have greater confidence in previous end-of-life decisions.3 Furthermore, autopsies may result in unexpected findings in as many as 20–30% of cases,4–7 further justifying the use of this valuable clinical tool.8 The autopsy holds particular value in the case of deceased infants and children, as detailed understanding of the cause of death may enable a more accurate estimation of the risk of recurrence in future children.
Despite the clear potential benefits, rates of autopsy have been declining in the United States and other countries over the past several decades.7,9 The reasons for the decline appear to be multi-factorial, including a decreased perception of utility by physicians and corresponding decline in willingness to request autopsy consent from the family,10,11 concerns from family members regarding "disfigurement," conflict with religious beliefs, and a perceived lack of benefit.12,13
In light of the declining rates of autopsy, the use of radiologic studies to conduct a “virtual autopsy” has been suggested as an adjunct to or substitute for the conventional autopsy3 and has even been accepted as legal forensic evidence in some countries.14 Early work comparing post-mortem MRI (PM-MRI) findings to conventional autopsy in aborted or stillborn fetuses and infants, demonstrated that PM-MRI provided the same or more information than the conventional autopsy in 60–80% of cases.15–18 Subsequent case reports demonstrated that PM-MRI was able to provide a diagnosis where the conventional autopsy was inconclusive19,20 or where conventional autopsy was not performed but the post-mortem MRI (PM-MRI) findings lead to a diagnosis which could not have been obtained otherwise.21 Additionally, several researchers have investigated acceptance of post-mortem MRI from the perspective of the healthcare provider22 and the parents23,24 finding generally high acceptance of the PM-MRI approach. These findings lead Thayyil et al. to conduct the first prospective, large-scale PM-MRI study, comparing PM-MRI alone, PM-MRI with minimally invasive autopsy, and conventional autopsy. They concluded that minimally invasive autopsy in combination with post-mortem MRI may be an acceptable alternative to conventional autopsy.25
Despite mounting evidence of the value of PM-MRI, there have been no studies dedicated to investigating the utility of these scans exclusively in a population of infants admitted to the Neonatal Intensive Care Unit (NICU). The modulating effect of intensive care (e.g. prolonged mechanical ventilation, parenteral nutrition, medications) was not evaluated in previous studies of terminated and stillborn fetuses or neonates who died in the delivery room.
The goal of this study was to determine the degree of agreement between conventional autopsy and PM-MRI in a highly-targeted population of neonates. We hypothesized that (i) PM-MRI in an exclusive neonatal population would have similar agreement with conventional autopsy as has been reported in other patient populations, (ii) PM-MRI findings would support the ante-mortem clinical diagnosis at the time of death, and that (iii) families of the deceased would, in general, find the PM-MRI results to be useful in understanding their child’s cause of death and aid in the grieving process.
METHODS
Study Design and Population
This was a prospective observational study evaluating PM-MRI scans of the brain, chest, abdomen and pelvis of neonates or infants who expired while admitted to the Neonatal Intensive Care Unit (NICU) at St. Louis Children’s Hospital during the study period of November 2011 to July 2013. Eligible cases included any patient that expired during the study period while admitted to the NICU, and for whom verbal consent was able to be obtained from the parents. There were no exclusion criteria for eligibility to participate in the study. The study protocol, verbal consent document, and survey were evaluated and approved by the Washington University Human Research Protection Office.
After patient expiration, the clinical team caring for the patient approached the family for consent for autopsy, per usual clinical protocol. Once the decision was made whether to pursue autopsy, the clinical team then approached the family for consent for post-mortem MRI. This sequence of events was standardized in order to minimize the risk that the offer of post-mortem MRI would interfere with the decision to pursue a conventional autopsy.
Procedures
All subjects underwent three-dimensional T1 and T2 weighted sequences of the brain, chest, abdomen and pelvis without the administration of contrast agents. The MRI scans were performed on the clinical scanners at St. Louis Children’s Hospital outside routine hours. The scans were performed on either a Siemens 1.5T Avanto or Siemens 3.0T Trio scanner (Siemens Healthcare, Erlangen, Germany) by the radiology technologist on duty at the time the scan occurred. Total MRI sequence length was 30 minutes (Coronal STIR slice thickness 3mm, acquisition matrix: 144×256, TR/TE 4000/91 ms; Axial T1 slice thickness 4mm, acquisition matrix 256×148, TR/TE 464/8 ms; Axial T2 FS slice thickness 4mm, acquisition matrix 256×144, TR/TE 3000/100 ms). The scans were completed as quickly as possible after expiration, with all scans occurring less than 24 hours after death. A portion of the subjects were placed in a refrigerated holding unit prior to scanning, thus the body temperature at the time of scan varied by patient. The body temperature of the patient was not recorded at the time of scan.
MRI images of the chest, abdomen, and pelvis were analyzed by a single pediatric radiologist (GK), who reported on each organ system individually. MRI images of the brain were analyzed by a single pediatric neuroradiologist (JS). The radiologists were masked to autopsy results.
For those patients who underwent either limited or full autopsy, a clinical autopsy was performed in the standardized fashion by the Washington University School of Medicine Department of Pathology, and included involvement of both pathology faculty and their trainees. This procedure includes a review of clinical history, external examination, and open dissection with macroscopic examination followed by removal and histological examination of organs. In cases without autopsy restrictions on the head, the brain was removed and fixed in formalin prior to histological examination. The pathologists were not aware of the PM-MRI results at the time of the autopsy.
Statistical approach
For all patients, PM-MRI findings were compared to the primary and contributing cause(s) of death, as identified on the death certificate. For those patients who also underwent a conventional autopsy, PM-MRI findings were compared to the cause(s) the degree in the final pathologic diagnosis. In addition, agreement between the two modalities was assessed by organ system (respiratory, cardiovascular, gastrointestinal, hepatic, genitourinary, and central nervous system). All comparisons were scored as complete, partial, or no agreement.
Follow-up
Per standard clinical practice, the parents of each patient were contacted 30–90 days after expiration to arrange a meeting so that the results of the autopsy and PM-MRI could be discussed. The meeting occurred by telephone or in-person, according to parental preference.
Two researchers (KL, AM) designed and administered a telephone survey to the parents of the neonates who underwent PM-MRI between 6 and 24 months after expiration. The survey consisted of nine questions which looked to identify whether each family recalled that their child had undergone a PM-MRI and if the family recalled being notified of the results of the PM-MRI. Of those who recalled the results, further questions were asked to determine how useful the results were in understanding their child’s medical condition and whether they felt that PM-MRI was a valuable piece of information as they coped with their child’s death.
The contact information for the parents of all 31 subjects was identified via the electronic medical record. Multiple attempts were made to reach each parent. If unsuccessful, any alternative contact numbers, such as numbers for other family members, were called in an attempt to locate the subject’s parents. Once the parent was contacted, an assent document was read over the telephone in order to verbally secure informed consent.
RESULTS
Patient Population
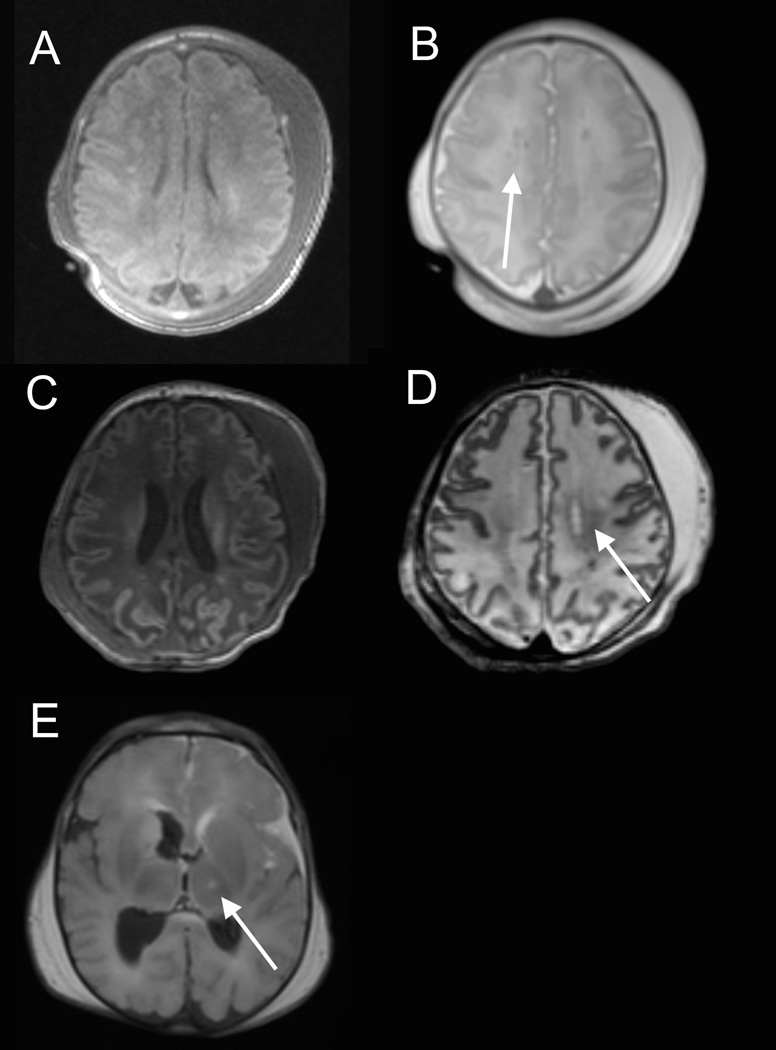
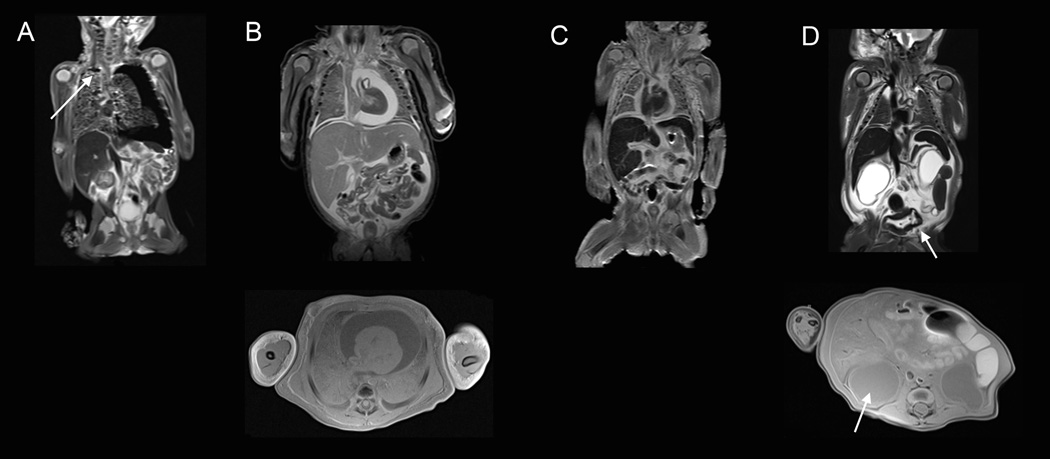
Over the course of the study period, 31 patients were recruited and underwent PM-MRI. Of those, 24/31 (77%) also underwent conventional autopsy. A summary of the patient population is shown in Table 1. An example of PM-MRI neuroimaging is shown in Figure 1 while PM-MRI somatic imaging is shown in Figure 2.
Table 1.
Characteristics of the study population
| Characteristic | |
|---|---|
| Gestational age at birth, M ± SD, weeks | 32 ± 5.5 |
| Male sex, n (%) | 16 (51.6) |
| Race, n (%) | |
| White | 20 (64.5) |
| Black | 9 (29) |
| Hispanic | 2 (6.5) |
| Postnatal age at death, median (range), days | 9 (0.13–180) |
| Elapsed time between death and PM-MRI, M ± SD, hours | 10 ± 6.6 |
| Autopsy, n (%) | |
| Full autopsy | 21 (67.7) |
| Partial autopsy to exclude brain | 3 (9.7) |
| Partial autopsy to include heart only | 1 (3.2) |
| No autopsy | 6 (19.4) |
Figure 1.
Postmortem neuroimaging findings. A- Increased T1 signal intensity in bilateral posterior cortical ribbon consistent with ischemic injury. B- Periventricular white matter injury (arrow). C- Increased T1 signal intensity in bilateral occipital, parietal and frontal lobes consistent with extensive ischemic injury. D- Wallerian degeneration in descending corticospinal tract 28 (arrow). E- Bilateral IVH with T1 hyperintensity in basal ganglia suspicious for ischemic injury.
Figure 2.
Postmortem somatic imaging findings. A- Large left tension pneumothorax, small right pneumothorax (arrow) and extensive pulmonary interstitial emphysema. B- Large pericardial effusion containing predominately water (top- T2 coronal, bottom- T1 axial). C- Moderate pericardial effusion and pulmonary edema. D- Bladder outlet obstruction as evidenced by bladder hypertrophy (top arrow) and marked renal parenchymal loss.
Comparison PM-MRI with ante-mortem clinical diagnosis
19/31 (61%) subjects had complete agreement with PM-MRI findings and the cause of death. An additional 5/31 (16%) had partial agreement of PM-MRI with the cause of death and shared a common finding of pulmonary vascular changes caused by pulmonary hypertension that was missed on PM-MRI. 7/31 (22%) had PM-MRI findings that did not agree with the cause of death as determined by the ante-mortem clinical diagnosis. These included infants with metabolic disturbances such as long-chain fatty acid deficiency, complex cardiac anatomy such as truncus arteriosus, kidney or liver failure or sepsis.
Comparison PM-MRI with autopsy results
Of the infants who also had a conventional autopsy, 14/24 (58%) had a complete agreement between PM-MRI findings and the cause of death as determined by autopsy. An additional 4/24 (17%) had similar findings except for the inability of PM-MRI to detect pulmonary vascular changes of pulmonary hypertension. Six infants (25%) had PM-MRI findings that did not agree with the cause of death.
The extent of agreement across organ systems was quite variable, ranging from 83% complete and partial agreement for findings in the cardiovascular system to 57% complete or partial agreement in the hepatic system. PM-MRI was superior to conventional autopsy in finding free air, both in the thoracic and peritoneal cavities. Five infants were noted to have pneumothorax on PM-MRI but it was only noted in a single case on conventional autopsy. Similarly, five other infants were noted to have pneumoperitoneum with only a single case detected on conventional autopsy. PM-MRI was also superior at detection of hepatic iron overload, detecting 4/4 cases, all of which were missed on conventional autopsy.
Conventional autopsy was superior to PM-MRI in detection of injury in a number of different organ systems including focal bowel necrosis and perforation (PM-MRI missed 3/4 cases), focal pulmonary hemorrhage and consolidation (PM-MRI missed 5/18 cases), medial hypertrophy in the pulmonary vascular bed (PM-MRI missed 5/14 cases), microscopic changes of acute tubular necrosis, focal microscopic white matter injury (PM-MRI missed 5/8 cases), and hypoxic-ischemic injury (PM-MRI missed 2/8 cases).
The agreement between PM-MRI findings and cause of death identified by ante-mortem clinical diagnosis and autopsy are shown in Table 2 and agreement of PM-MRI with autopsy broken down by organ system is shown in Table 3.
Table 2.
PM-MRI agreement with cause of death
| Sample sizea | Agreement | Percentage of complete and partial agreement |
|||
|---|---|---|---|---|---|
| Complete | Partial | None | |||
| Ante-mortem clinical diagnosis, n (%) |
31 | 19 (61) | 5 (16) | 7 (22) | 77 |
| Final pathologic diagnosis, n (%) |
24 | 14 (58) | 4 (17) | 6 (25) | 75 |
Footnotes:
31 infants initially recruited for study, 24/31 underwent conventional autopsy.
Table 3.
Agreement of PM-MRI findings with autopsy by organ system
| Organ System | Agreement with autopsy | Percentage of complete and partial agreement |
|||
|---|---|---|---|---|---|
| Complete | Partial | None | Incomplete | ||
| Respiratory n=23 |
14 | 0 | 8 | 1 | 61 |
| Cardiovascular n=24 |
13 | 7 | 4 | 0 | 83 |
| Gastrointestinal n=23 |
18 | 0 | 5 | 1 | 78 |
| Hepatic n=23 |
13 | 0 | 10 | 1 | 57 |
| Genito-urinary n=23 |
14 | 0 | 9 | 1 | 61 |
| Central Nervous n=23 |
10 | 5 | 6 | 1 | 65 |
Family survey
Twenty (65%) families were able to be contacted for the follow-up survey, two (6%) of which declined to participate in the survey. For those lost to follow-up, the universal reason was changed or inactive phone numbers. Median time to follow-up was 479 days (range 258–728 days).
Ten of the eighteen families who completed the survey (56%) remembered that their child had undergone PM-MRI and recalled the results, 5/18 (28%) remembered that their child underwent PM-MRI but could not recall the results, and 3/10 did not remember that their child had undergone PM-MRI.
Of those who recalled the PM-MRI, the responses from the families were positive. 70% of parents found the results helping to relieve, in some way, the burden of responsibility that they felt regarding their child’s death. Another parent stated that the results helped to confirm that the medical team truly treated her child to the best of its ability. 80% of parents felt that the combination of PM-MRI results and the autopsy results provided vital information, and that the combination of the two was preferred over either one alone. Importantly, all 18 (100%) of the respondents stated that obtaining the PM-MRI did not delay their memorial services or interrupt the time spent with their child after he or she died. The survey results are shown in Table 3.
DISCUSSION
Our results demonstrate that PM-MRI studies have a high level of agreement with conventional autopsy, in complete agreement in 60% of cases and partial agreement an additional 20% of the time. In addition, of those parents who recalled the results of the PM-MRI, the majority felt that the information was valuable to their understanding and all agreed that the PM-MRI process did not interfere with memorial arrangements.
The results of this study highlight the logistical feasibility of PM-MRI. We were able to utilize the ancillary staff in the NICU to obtain the PM-MRI quickly, with the only factor delaying the scan being the availability of the clinical MRI scanner and the technologist. The design of this study is one that can be equally replicated by physicians who work in an academic or community hospital setting with utilization of clinical MRI scanners. However, access to interpretative services by pediatric radiology/neuroradiology is important.
PM-MRI is superior to the conventional autopsy in two key scenarios: detection of free air and hepatic iron overload. The enhanced detection of free air may be the results of the proximity of the MR study to the time of death (10 hours, on average) and that much of the gas may diffuse out of the intraperitoneal or intrathoracic spaces by the time the conventional autopsy was performed, making recognition more difficult. Although, hepatic iron overload can be detected on microscopic examination by use of special stains, such as Perl’s iron stain, this is not routinely performed unless there is an a priori suspicion of iron disorders. However, given the physics involved, it requires no special effort for an MRI scan to detect ferrous metal.
Given the lower resolution and nature of the whole body MRI, it is unable to detect focal or microscopic injury (such as bowel necrosis or vascular remodeling), functional changes and some focal forms of brain injury. This is an expected finding as full body MR studies, even on a 3T scanner, will never approach the resolution of microscopic tissue examination at 50 or 100× magnification. Dedicated imaging sequences, focused on a particular region or organ system may provide more detailed information, such as the high-resolution three-dimensional cardiovascular approach suggested by Taylor et al26 or the sub-millimeter sequences suggested by Norman et al.27 These sequences, however, come at a significant time and logistical cost. As the aim of this study was to evaluate a clinically feasible approach to the PM-MRI, these advanced imaging techniques were beyond the scope of this study.
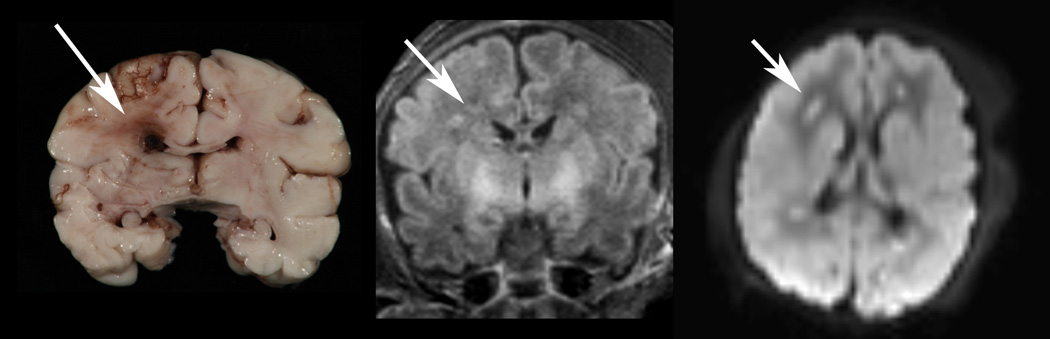
There are also important caveats to the use of PM-MRI to detect brain injury. Although, PM-MRI correctly identified pathology associated with structural or anatomic changes (IVH with ventricular dilation, agenesis of the corpus callosum) it failed to detect hypoxic-ischemic injury. Two of the eight patients with hypoxic injury known ante mortem and identified on pathologic examination of the brain, had no corresponding findings noted on PM-MRI. Given that T1 and T2 changes relating to hypoxic injury may develop over the first week or so after injury, the PM-MRI may have been obtained during this window when MR imaging may appear normal despite evolving injury.
These results suggest the potential role for PM-MRI in the NICU. If offered to the family, the potential shortcomings of the approach should be clearly outlined to the family in advance, and it should not be offered as a replacement for the conventional autopsy. However, in certain circumstances where pediatric autopsy services are unavailable or conventional autopsy is not desired by the family for personal or religious reasons, the PM-MRI has the potential to provide a reasonable surrogate.
While autopsies are typically provided free of charge to the family by most academic pathology departments, whole body MRI scans are not inexpensive, and although these are limited exams compared to a regular MRI study, they can cost between one and several thousand dollars with some of the cost possibly being passed on to the families as a “co-payment.” For the purpose of this study, the cost of the MRI was waived for the families. Given the value of the information to many families, individual institutions may consider a mechanism by which this service is provided at “no-cost” to the families.
The family survey results highlight many of the common struggles of post-discharge communication with families. Although our institutional goal is to provide long-term follow-up for all families, the contact information in the medical record is often incorrect or quickly becomes invalid as phone numbers change or families move to new addresses. The social support provided while the infant is alive, facilitating transportation and/or communication, quickly evaporates after the infant dies, making it difficult or even impossible to ever find a family again in some cases. Furthermore, even when the family could be contacted, the survey demonstrated a significant shortcoming in communicating diagnostic information to families in ways that are memorable; nearly half of respondents could not remember the key findings of the post-mortem MRI. Although the majority of those who remembered the results found the PM-MRI to be helpful, there remains an enormous gap in the post-mortality care of the family.
Future directions
One potential future line of inquiry may be the investigation of a “hybrid autopsy” where a PM-MRI is used as a screening tool to guide the pathologists. The approach could allow an autopsy to be performed in “minimally invasive” fashion, where only organs with MRI abnormalities are examined or could enhance the yield of a conventional autopsy, allowing informed decision making about which regions of the tissue to sample for microscopic examination.
In conclusion, the results of this study suggest that the PM-MRI can be implemented in any institution with pediatric radiology services without the need for substantial changes in infrastructure or logistical support and that it does not interfere with memorial services. It may serve as a viable alternative to conventional autopsy, as long as the diagnostic limitations are understood by the clinicians and family members.
Figure 3.
Matching images of ischemic white matter injury in the periventricular white matter as seen on gross examination (left image), T1 (middle) and diffusion imaging (right image).
Table 4.
Family Survey Results
| Question | Answered yes | Answered no | Not sure/did not recall |
|---|---|---|---|
| Do you remember that your child had a PM-MRI? n (%) |
15 (83) | 3 (17) | 0 (0) |
| Do you recall the results of the PM-MRI? n (%) |
10 (56) | 8 (44) | 0 (0) |
| Did you understand PM- MRI results well enough to describe to someone else? n (%) |
9 (50) | 1 (6) | 8 (44) |
| Was the PM-MRI helpful in understanding your child’s medical condition? n (%) |
8 (44) | 2 (11) | 8 (44) |
| Did the PM-MRI aid in your grief process? n (%) |
7 (38) | 3 (17) | 8 (44) |
| Would you recommend a PM-MRI for the child of a friend? n (%) |
10 (56) | 0 (0) | 8 (44) |
| Did the PM-MRI interrupt the time spent with your child after death? n (%) |
0 (0) | 18 (100) | 0 (0) |
| Did the PM-MRI interfere with funeral/memorial plans? n (%) |
0 (0) | 18 (100) | 0 (0) |
Acknowledgments
Funding source(s):
Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450)
No sponsor had a role in the design, data collection and analysis, the writing of this manuscript or the decision to submit it for publication. Dr. Leadbetter wrote the first draft of this manuscript and did not receive an honorarium or payment of any kind for her effort.
Footnotes
Conflict of interest statement:
There are no potential, perceived or real conflicts of interest to report.
REFERENCES
- 1.Sailer DN. The Clinical Utility of the Perinatal Autopsy. JAMA J Am Med Assoc. 1995;273:663. doi: 10.1001/jama.273.8.663. [DOI] [PubMed] [Google Scholar]
- 2.Craft H. Autopsy: High Yield in Neonatal Population. Am J Dis Child. 1986;140:1260. doi: 10.1001/archpedi.1986.02140260062027. [DOI] [PubMed] [Google Scholar]
- 3.Griffiths PD, Paley MNJ, Whitby EH. Post-mortem MRI as an adjunct to fetal or neonatal autopsy. Lancet Lond Engl. 2005;365:1271–1273. doi: 10.1016/S0140-6736(05)74816-9. [DOI] [PubMed] [Google Scholar]
- 4.Combes A, Mokhtari M, Couvelard A, Trouillet J-L, Baudot J, Hénin D, et al. Clinical and autopsy diagnoses in the intensive care unit: a prospective study. Arch Intern Med. 2004;164:389–392. doi: 10.1001/archinte.164.4.389. [DOI] [PubMed] [Google Scholar]
- 5.Cardoso MP, Bourguignon DC, Gomes MM, Saldiva PHN, Pereira CR, Troster EJ. Comparison between clinical diagnoses and autopsy findings in a pediatric intensive care unit in São Paulo, Brazil. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2006;7:423–427. doi: 10.1097/01.PCC.0000235257.86519.16. [DOI] [PubMed] [Google Scholar]
- 6.Kabra NS, Udani RH. Correlation between clinical diagnoses at the time of death and autopsy findings in critically sick neonates at a regional neonatal intensive care unit in India. J Trop Pediatr. 2001;47:295–300. doi: 10.1093/tropej/47.5.295. [DOI] [PubMed] [Google Scholar]
- 7.Brodlie M. Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ. 2002;324:761–763. doi: 10.1136/bmj.324.7340.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA. 2003;289:2849–2856. doi: 10.1001/jama.289.21.2849. [DOI] [PubMed] [Google Scholar]
- 9.Tsitsikas DA, Brothwell M, Chin Aleong J-A, Lister AT. The attitudes of relatives to autopsy: a misconception. J Clin Pathol. 2011;64:412–414. doi: 10.1136/jcp.2010.086645. [DOI] [PubMed] [Google Scholar]
- 10.O’Grady G. Death of the teaching autopsy. BMJ. 2003;327:802–803. doi: 10.1136/bmj.327.7418.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherwood SJ, Start RD. Asking relatives for permission for a post mortem examination. Postgrad Med J. 1995;71:269–272. doi: 10.1136/pgmj.71.835.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burton JL, Underwood J. Clinical, educational, and epidemiological value of autopsy. Lancet Lond Engl. 2007;369:1471–1480. doi: 10.1016/S0140-6736(07)60376-6. [DOI] [PubMed] [Google Scholar]
- 13.Sanner MA. In perspective of the declining autopsy rate. Attitudes of the public. Arch Pathol Lab Med. 1994;118:878–883. [PubMed] [Google Scholar]
- 14.Bolliger SA, Thali MJ. Imaging and virtual autopsy: looking back and forward. Philos Trans R Soc B Biol Sci. 2015;370 doi: 10.1098/rstb.2014.0253. 20140253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brookes JA, Hall-Craggs MA, Sams VR, Lees WR. Non-invasive perinatal necropsy by magnetic resonance imaging. The Lancet. 1996;348:1139–1141. doi: 10.1016/S0140-6736(96)02287-8. [DOI] [PubMed] [Google Scholar]
- 16.Woodward PJ, Sohaey R, Harris DP, Jackson GM, Klatt EC, Alexander AL, et al. Postmortem fetal MR imaging: comparison with findings at autopsy. Am J Roentgenol. 1997;168:41–46. doi: 10.2214/ajr.168.1.8976917. [DOI] [PubMed] [Google Scholar]
- 17.Alderliesten ME, Peringa J, Hulst VPM, Blaauwgeers HLG, Lith JMM. Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG Int J Obstet Gynaecol. 2003;110:378–382. [PubMed] [Google Scholar]
- 18.Arthurs OJ, Thayyil S, Owens CM, Olsen OE, Wade A, Addison S, et al. Diagnostic accuracy of post mortem MRI for abdominal abnormalities in foetuses and children. Eur J Radiol. 2015;84:474–481. doi: 10.1016/j.ejrad.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 19.Vaneckova M, Seidl Z, Goldova B, Vitkova I, Baxova A, Petrovicky P, et al. Post-mortem magnetic resonance imaging and its irreplaceable role in determining CNS malformation (hydranencephaly)--case report. Brain Dev. 2010;32:417–420. doi: 10.1016/j.braindev.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Vaneckova M, Seidl Z, Goldova B, Vitkova I, Calda P. Benefits of examination by post mortem performed magnetic resonance imaging of foetus: haemorrhage in germinal matrix. Neuro Endocrinol Lett. 2010;31:40–42. [PubMed] [Google Scholar]
- 21.Bouchireb K, Teychene A-M, Rigal O, de Lonlay P, Valayannopoulos V, Gaudelus J, et al. Post-mortem MRI reveals CPT2 deficiency after sudden infant death. Eur J Pediatr. 2010;169:1561–1563. doi: 10.1007/s00431-010-1261-0. [DOI] [PubMed] [Google Scholar]
- 22.Ben-Sasi K, Chitty LS, Franck LS, Thayyil S, Judge-Kronis L, Taylor AM, et al. Acceptability of a minimally invasive perinatal/paediatric autopsy: healthcare professionals’ views and implications for practice. Prenat Diagn. 2013;33:307–312. doi: 10.1002/pd.4077. [DOI] [PubMed] [Google Scholar]
- 23.Kang X, Cos T, Guizani M, Cannie MM, Segers V, Jani JC. Parental acceptance of minimally invasive fetal and neonatal autopsy compared with conventional autopsy. Prenat Diagn. 2014;34:1106–1110. doi: 10.1002/pd.4435. [DOI] [PubMed] [Google Scholar]
- 24.Cannie M, Votino C, Moerman P, Vanheste R, Segers V, Van Berkel K, et al. Acceptance, reliability and confidence of diagnosis of fetal and neonatal virtuopsy compared with conventional autopsy: a prospective study. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2012;39:659–665. doi: 10.1002/uog.10079. [DOI] [PubMed] [Google Scholar]
- 25.Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O, et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet Lond Engl. 2013;382:223–233. doi: 10.1016/S0140-6736(13)60134-8. [DOI] [PubMed] [Google Scholar]
- 26.Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RJ, Wade A, et al. Postmortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation. 2014;129:1937–1944. doi: 10.1161/CIRCULATIONAHA.113.005641. [DOI] [PubMed] [Google Scholar]
- 27.Norman W, Jawad N, Jones R, Taylor AM, Arthurs OJ. Perinatal and paediatric post-mortem magnetic resonance imaging (PMMR): sequences and technique. Br J Radiol. 2016;89 doi: 10.1259/bjr.20151028. 20151028. [DOI] [PMC free article] [PubMed] [Google Scholar]