Preparing appropriately for the delivery and immediate care of the preterm infant is essential when time permits and may impact on the eventual outcome for the infant. This article describes the skills and equipment needed for the care and possible resuscitation of these vulnerable babies. The support and advice needed by parents and families at this time is also explored.
Preparation for preterm delivery
When preterm delivery can be anticipated there may be an opportunity for paediatric staff to discuss intrapartum and postnatal care with prospective parents and colleagues from midwifery and obstetrics. Even if detailed discussion is not possible, relevant historical details should be taken to anticipate problems and prepare appropriately for the arrival of the preterm infant.
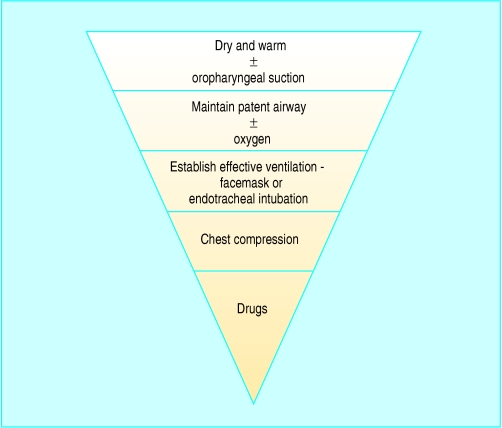
Figure 1.
The “inverted triangle” shows how commonly certain interventions are needed
Broadly, the level of resuscitation that may be needed is inversely related to the gestation of the preterm infant. Usually, the approach taken in resuscitating preterm infants of > 32 completed weeks' gestation is the same as that taken for term infants. Most need only basic measures such as drying and stimulation. Infants of gestation < 32 weeks (or birth weight < 1500 g) require more active support. For infants of < 28 weeks' gestation, this support will probably include endotracheal intubation and assisted ventilation.
Table 1.
Equipment for resuscitation of the preterm infant
| • Clock with second hand |
| • Dry, warmed towels and heat source |
| • Light source |
| • Wide bore suction device |
| • Facemasks in a variety of sizes |
| • Inflatable bag with blow-off valve |
| • Oxygen source with pressure limiting device |
| • Laryngoscope with neonatal blades |
| • Endotracheal tube (sizes 2.5, 3.0, and 3.5) |
| • Needles and syringes |
| • Umbilical catheters |
Ideally, two members of staff who are experienced in the early care of preterm infants should be present at the delivery of each anticipated infant. A senior paediatrician with extensive experience in dealing with preterm babies should be at the delivery of infants of < 28 weeks' gestation. Before delivery, the attending staff should recheck essential equipment for resuscitation.
Table 2.
History relevant to preterm delivery
| • Maternal medical and obstetric history |
| • Estimated gestation |
| • Singleton or multifetal pregnancy? |
| • Assessments of fetal growth and wellbeing |
| • Details of suspected congenital anomalies |
| • Risk of fetal-maternal infection and chorioamnionitis |
| • Course of labour, if labouring |
| • Intrapartum monitoring results |
| • Antenatal interventions, tocolytic drugs, steroids, antibiotics |
| • Use of opiates and anaesthetic drugs |
Assessment and resuscitation
Preterm infants get cold quickly because of their relatively large surface area. Resulting hypothermia reduces surfactant production, may hasten hypoglycaemia and acidaemia, and is associated with increased mortality. Preterm infants should be delivered into warm towels, dried, and transferred to a dedicated neonatal resuscitation platform or trolley with an integral radiant heater. Alternatively, immediate occlusive wrapping in polythene may be at least as effective in reducing evaporative heat loss, especially in extremely preterm infants.
Figure 2.

Preterm infants should be moved to a neonatal resuscitation trolley with radiant heater after delivery as they get cold quickly
As with all acute resuscitation, the aims are to ensure airway patency and support the breathing and circulation. Colour, respiratory effort, tone, and heart rate can be assessed to determine the response of the infant to interventions.
Airway
To obtain a patent airway, the infant's head should be maintained in a neutral position and the chin should be supported while applying gentle forward traction to the mandible (jaw thrust). Careful suction under direct vision may be used to clear secretions that can obstruct the airway.
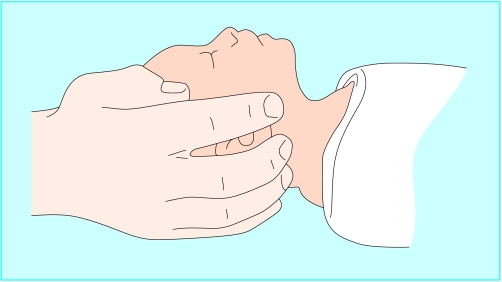
Figure 3.
Correct head position for newborn resuscitation—the neutral position
Breathing
Failure to establish regular breathing in the first minute after birth is an indication for assisted ventilation. The aim is to inflate the newborn's poorly compliant, fluid filled lungs to recruit alveoli for gas exchange. About five initial “inflation” breaths of 2-3 seconds' duration followed by ventilation at a rate of around 40 breaths per minute using pressures of 20-25 cm H2O is appropriate while checking for spontaneous respiration every 30 seconds. Occasionally, higher inflation pressures, up to 30 cm H2O, may be needed. The benefit of using positive end expiratory pressure as part of acute resuscitation has yet to be established. Commonly, 100% oxygen is used, but no evidence exists that this achieves better outcomes than lower concentrations of oxygen.
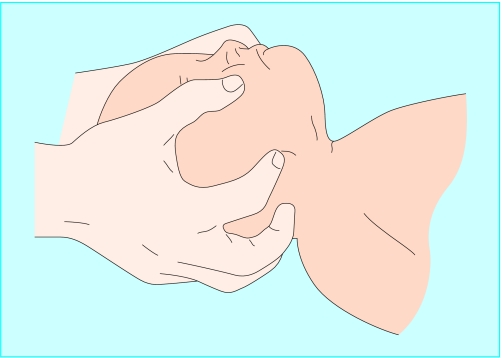
Figure 4.
Jaw thrust for maintaining a patent airway in newborn infant
Inflation breaths, and subsequent ventilation if spontaneous respiration is not established, can be delivered via a facemask attached to a Y piece system with a blow-off valve or via a bag valve mask. A range of masks should be available to fit over the infant's mouth and nose (but not the orbital margin). Staff caring for newborn infants in all centres, including community maternity units, should be trained to deliver facemask ventilation effectively.
Infants of >32 weeks' gestation
For infants of gestation > 32 weeks, failure to respond to appropriately delivered facemask ventilation in the first 2-3 minutes is rare, and may be an indication for endotracheal intubation.
Infants of 28-32 weeks' gestation
Infants born at < 32 weeks' gestation have an increased risk of surfactant deficiency and of developing respiratory distress syndrome. In addition, they have less developed respiratory muscles than term infants and are less able to cope with the increased work of breathing associated with poorly compliant lungs.
Figure 5.
Bag valve mask can be used to deliver inflation breaths and subsequent ventilation if necessary
For infants of gestation 28-32 weeks who do not establish adequate spontaneous respiration in 30-60 seconds, other options to sustain respiration exist. These options include supporting ventilation with continuous positive airway pressure via nasal prongs or facemask, intubating and providing intermittent positive pressure ventilation, and administering prophylactic surfactant.
Infants of < 28 weeks' gestation
Not all infants of < 28 weeks' gestation need intubation at birth. Unless the infant is pink and active, however, immediate endotracheal intubation at birth should be considered. In these infants there is evidence that early prophylactic replacement of natural surfactant is more effective than delayed “rescue” treatment in reducing the incidence of acute lung injury and mortality. For infants born outside the labour ward, resuscitative efforts should concentrate on keeping the infant warm, maintaining a clear airway, administering oxygen, and applying facemask ventilation.
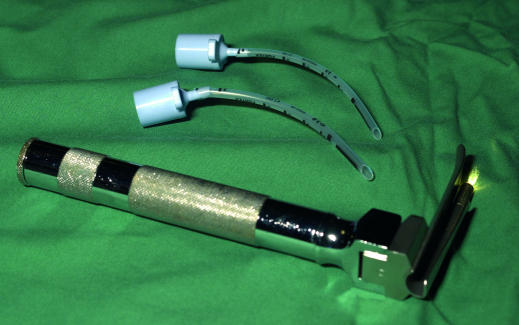
Figure 6.
Laryngoscope and endotracheal tubes for intubating preterm infants
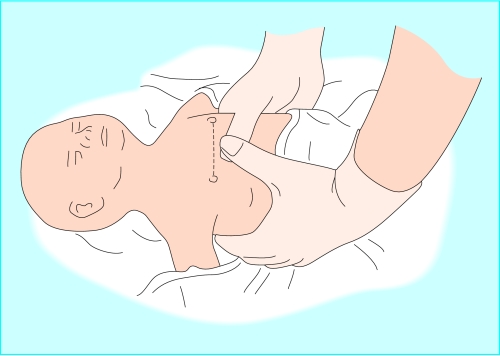
Circulation
Chest compression is indicated if, despite adequate artificial ventilation, the infant's heart rate remains < 60 beats per minute and is not improving. Apply around 90 compressions per minute with lung reinflation after every three chest compressions.
Figure 7.
Chest compressions may be needed to resuscitate newborns if their heart rates are <60 beats per minute and there is no improvement in response to respiratory support
Drugs
If there is no improvement in clinical condition after adequate ventilation and chest compression, then certain drugs may be useful in the acute resuscitation of preterm infants. Persistent bradycardia may respond to adrenaline (epinephrine) and sometimes intravenous sodium bicarbonate can be used to correct acidosis. Dextrose may also be useful during prolonged resuscitation to correct hypoglycaemia. The use of intravenous fluids (normal saline, plasma, and blood) for volume expansion in preterm infants should be limited to those infants known to have volume depletion—for example, after antepartum haemorrhage.
Table 3.
Drugs used in acute resuscitation of the preterm infant
| • Adrenaline (epinephrine) (1:10 000): 0.1 ml/kg (10 μg/kg) |
| • Sodium bicarbonate (4.2%): 2-4 ml/kg (1-2 mmol/kg) |
| • Dextrose (10%): 2.5 ml/kg (250 μg/kg) |
| • Intravenous volume replacement: saline (0.9%), plasma, blood: 10-20 ml/kg |
| All given via an umbilical venous catheter; adrenaline may also be given via endotracheal tube. |
All drugs are best delivered via an umbilical venous catheter. Adrenaline (epinephrine) may be given via the endotracheal route although its efficacy is unknown when given this way. Sadly, infants who do not respond to appropriate “basic” resuscitation and merit drug intervention will probably have a poor prognosis.
Stopping intensive resuscitation efforts
If the heart rate does not improve despite 15-20 minutes of appropriate efforts, then it may be appropriate to stop resuscitation and to provide palliative care. A decision to stop active intervention should be made by senior staff in consultation with the parents. If an experienced member of staff is not available resuscitation should be continued until a senior colleague is contacted.
Infants born at the threshold of viability
Although interventions (such as prophylactic antenatal steroids and exogenous surfactants) have improved certain outcomes for extremely preterm infants, recent data indicate that the overall prognosis for infants born at < 26 weeks' gestation remains poor. When delivery at < 26 weeks' gestation is anticipated, the most experienced paediatrician available must counsel the parents and inform them of the potential outcomes for mother and infant.
Table 4.
Perinatal management at the threshold of viability
| • Antenatal counselling should be provided by senior neonatologists, obstetricians, and midwives |
| • Management decisions should depend on what the parents and their medical advisers think is in the child's best interests |
| • Parents should have accurate information on likely outcomes for their infant—including their chances of survival and the risk of longer term disability |
| • Information on outcomes provided to parents should cite data from large cohort studies that reported the outcome of all pregnancies for each week of gestation (not just for infants admitted to intensive care units) |
| • Perinatal management plans should consider the mode of delivery, use of intrapartum monitoring, and immediate care of the newborn |
| • Decisions not to provide active resuscitation or intensive care should not be binding, particularly if the newborn seems more mature than anticipated |
| • It may be appropriate to provide full resuscitation and intensive care to infants at birth until the clinical progress becomes clearer and further discussions with the family have been possible |
| • Parents should be supported throughout and encouraged to seek advice and further support from others, such as family members and religious advisers |
| • Infants who are not actively resuscitated or in whom active resuscitation is withdrawn should receive palliative care |
If possible, the parents should then be allowed to reflect on the implications of this information before it is decided how to care for the newborn infant. Some parents and carers may feel that aggressive perinatal interventions are not in the best interests of the infant and family. Such discussions and any decisions reached should be documented and conveyed to all staff who are caring for the mother or infant. The parents should be assured that any decision to withhold or start resuscitation can be revised at any time depending on clinical circumstances.
Table 5.
Factors needed in the palliative care of extremely preterm infants
| • Warmth |
| • Dignity |
| • Human contact |
| • Pain relief |
Palliative care of the newborn infant
If resuscitation is unsuccessful, or if active resuscitation is felt to be inappropriate, then palliative care should be provided for the infant and family. The parents can spend time with their baby, and should be aware that their baby may show signs of life, such as occasional gasps, after birth. Privacy and sensitive support for parents and family with subsequent follow up are essential. The potential importance of postmortem examination should be discussed at an appropriate time.
Audit and review
All deliveries of extremely preterm infants should be reviewed by the neonatal service as part of training and good practice. Particular attention should be given to aspects of care that have been shown to affect outcome. Regular perinatal meetings are an ideal opportunity to examine these episodes of care and should be mandatory for any neonatal service.
The ABC of preterm birth is edited by William McGuire, senior lecturer in neonatal medicine, Tayside Institute of Child Health, Ninewells Hospital and Medical School, University of Dundee; and Peter W Fowlie, consultant paediatrician, Perth Royal Infirmary and Ninewells Hospital and Medical School, Dundee. The series will be published as a book in spring 2005.
Competing interests: For WMcG's competing interests see first article in the series.
The line drawings of head position, jaw thrust and chest compressions in newborns are adapted from Resuscitation at birth: newborn life support provider course manual. London: Resuscitation Council (UK), 2001. The box on perinatal management at the threshold of viability is adapted from the British Association of Perinatal Medicine practice framework (www.bapm.org/documents/publications/)
Further reading and resources
- • Joint Working Party of Royal College of Paediatrics and Child Health and Royal College of Obstetricians and Gynaecologists. Resuscitation of babies at birth. London: BMJ Publishing Group, 1997
- • Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med 2000;343: 378-84 [DOI] [PubMed] [Google Scholar]
- • Gee H, Dunn P. Fetuses and newborn infants at the threshold of viability: a framework for practice. Perinat Neonat Med 2000;5: 209-11 [Google Scholar]
- • Resuscitation Council (UK). Resuscitation at birth: newborn life support provider course manual. London: Resuscitation Council (UK), 2002
- • Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2003;(3): CD000510. [DOI] [PubMed]