Abstract
Weight suppression predicts the onset and maintenance of bulimic syndromes. Despite this finding, no study has examined psychological mechanisms contributing to these associations using a longitudinal design. Given societal pressures to be thin and an actual history of higher weight, it is possible that greater weight suppression contributes to increased fear of gaining weight and preoccupation with being thin, which increase vulnerability to eating disorders. The present study investigated whether greater drive for thinness mediates associations between weight suppression and bulimic symptoms over long-term follow-up. Participants were women (n = 1190) and men (n = 509) who completed self-report surveys in college and 10- and 20- years later. Higher weight suppression at baseline predicted higher bulimic symptoms at 20-year follow-up (p < .001), while accounting for demographic variables and baseline bulimic symptoms, body mass index, and drive for thinness. Increased drive for thinness at 10-year follow-up mediated this effect. Findings highlight the long-lasting effect of weight suppression on bulimic symptoms and suggest that preoccupation with thinness may help maintain this association. Future studies would benefit from incorporating other hypothesized consequences of weight suppression, including biological factors, into risk models.
Keywords: weight suppression, bulimia, drive for thinness, longitudinal, risk factor
Bulimia nervosa (BN) was originally conceptualized by Russell (1979) as “an ominous variant of anorexia nervosa.” This description was based, in part, on the observation that although not underweight, individuals with BN often present with a history of higher past weight and significant weight loss. The difference between one’s highest previous adult weight and current weight has since been termed “weight suppression” (WS) (Lowe, 1993), and research has yielded accumulating support for the clinical significance of WS in BN.
Several cross-sectional studies have reported significant associations between higher WS and greater frequency of binge eating and purging in individuals with BN (Bodell & Keel, 2015; Butryn, Juarascio, & Lowe, 2011; Lowe, Thomas, Safer, & Buytryn, 2007). Furthermore, longitudinal studies support the role of WS in the maintenance of BN (Butryn, Lowe, Safer, & Agras, 2006; Keel & Heatherton, 2010; Lowe et al., 2011). Butryn and colleagues (2006) found that higher WS at baseline in individuals receiving cognitive-behavioral treatment for BN predicted continued binge eating and purging at treatment discharge. Lowe and colleagues (2011) further identified that higher WS was associated with longer time to remission in an 8-year naturalistic follow-up study of BN (Lowe et al., 2011). Moreover, higher WS predicted the onset and maintenance of bulimic syndromes 10 years later in a college-based community sample (Keel & Heatherton, 2010). Some studies have failed to replicate associations between WS and treatment outcome, potentially due to reduced variability in WS or weight gain over follow-up alleviating risk conferred by WS (Carter, McIntosh, Joyce, & Bulik, 2008; Dawkins, Watson, Egan, & Kane, 2013; Zunker, et al., 2011). However, independent longitudinal studies support the clinical relevance of WS in short- and long-term outcomes in both treatment and non-treatment seeking samples.
Although previous research highlights the importance of WS in bulimic symptomatology, reasons for this finding remain unknown. To our knowledge, only one study has investigated factors contributing to observed associations between WS and bulimic symptoms (Bodell & Keel, 2015). Based on biobehavioral theories, (Bodell & Keel, 2015; Burtyn et al., 2006; Lowe, Davis, Lucks, Annunziato, & Butryn, 2006; Keel & Heatherton, 2010), Bodell and Keel (2015) examined cross-sectional associations between WS, leptin levels, reinforcing value of palatable food, and binge eating in a sample of women with BN and noneating disorder controls. Results provided preliminary evidence that WS may contribute to binge eating through both reduced leptin levels and increased reward value of palatable foods; however, additional factors likely play a role.
Indeed, psychological aspects of WS may contribute to increased vulnerability to bulimic symptoms. It is well established that current Western sociocultural ideals of beauty contribute to body dissatisfaction and general pressures to be thin (Stice, Spangler, & Agras, 2001; Stice, Maxfield, & Wells, 2003). Individuals who lose weight (i.e., are weight suppressed) often are positively reinforced for weight loss. This positive reinforcement may motivate some individuals to maintain their thinness and contribute to a higher drive for thinness (DT). Additionally, longitudinal studies suggest that WS contributes to greater risk for future weight gain (Carter et al., 2008; Herzog et al., 2010; Lowe, et al., 2006). Thus, those who are high in WS may develop increased fears of returning to their higher prior weights and increased preoccupation with being thin (Loth, MacLehose, Bucchianeri, Crow, & Neumark-Sztainer, 2014). These cognitions may then contribute to vulnerability to binge eat, given that high DT and dietary restraint predict onset of binge eating (Stice, Davis, Miller, & Marti, 2008). Thus, continued thinness preoccupation may contribute to illness maintenance among those with greater WS.
Improved understanding of mechanisms driving the relationship between WS and bulimic symptoms may help inform specific treatment targets and ameliorate suffering. The purpose of the current study is to examine whether DT influences associations between WS and bulimic symptoms using a longitudinal design with 20-year follow-up across three waves of data collection. Given associations found in previous samples, we hypothesized that higher WS in college would be associated with greater severity of bulimic symptoms in mid-life, controlling for bulimic symptoms in college, and that this association would be mediated by increased DT.
Methods
Participants and Procedures
Participants were women (n = 1190) and men (n = 509) from two cohorts of students at a northeastern university who completed self-report surveys as part of a study examining eating and health-related behaviors. The first cohort completed baseline surveys in 1982 and then 10- and 20-year follow-up surveys in 1992 and 2002, respectively. The second cohort was established in 1992 and completed 10- and 20-year follow-up surveys in 2002 and 2012, respectively. Approximately 78.7% (n = 1337) of the baseline sample was retained at 10-year follow-up, and 70.3% (n = 1194) was retained at 20-year follow-up. Detailed descriptions of participants and sampling procedures have been documented in prior publications (Keel & Heatherton, 2010; Keel, Heatherton, Dorer, Joiner, & Zalta, 2006; Tzoneva, Forney, & Keel, 2015). At baseline, the mean (SD) age of the sample was 19.9 (1.8) years. Approximately two thirds of the sample was white, non-Hispanic (66.9%), 11.1% was Asian, 5.4% was African-American, and 1.9% identified as “other”. Approximately 5.1% of the sample (n = 86) was Hispanic. Race/ethnicity data were not available on 14.7% of the participants. The 1992 cohort included a greater proportion of individuals who identified as Hispanic (χ2= 3.88, p < .05) compared with the 1982 cohort. There were no additional demographic differences between cohorts.
All study procedures were approved by the relevant institutional review boards at the universities where the research was conducted. All participants provided informed consent prior to the completion of surveys.
Measures
Weight Suppression
WS was calculated as the difference between self-reported current and highest previous adult weight (excluding pregnancy), consistent with its definition in prior studies (e.g., Keel & Heatherton, 2010; Lowe et al., 2006). Importantly, research supports the validity of self-reported weight history in both eating and non-eating disordered samples (Swenne, Belfrage, Thurfjell, & Engstrom, 2005; Tamakoshi et al., 2003).
The Eating Disorders Inventory (Garner, Olmsted, Polivy, 1983; EDI)
The EDI bulimia and DT subscales available when the parent study was initiated in 1982 were used to measure bulimic symptoms and DT. The EDI-bulimia subscale assesses aspects of binge eating such as “I stuff myself with food.” The EDI-DT subscale consists of items related to fear of weight gain and thinness preoccupation such as “I am preoccupied with being thin,” “I’m terrified of gaining weight,” and “If I gain a pound, I worry that I will keep gaining.” These subscales have demonstrated excellent reliability and validity in previous samples (Nevonen, Clinton, & Norring, 2006; Thiel & Paul, 2006) as well as evidence of factor invariance between genders and across the ages included in the current study (Spillane, Boerner, Anderson, & Smith, 2004; Keel, Baxter, Heatherton, & Joiner, 2007). Cronbach’s alpha for the subscales in the current study was greater than .80 across all time points.
Body Mass Index (BMI)
Self-reported height and weight were used to calculate BMI (kg/m2). Studies have demonstrated high correspondence between self-reported and objectively measured height and weight in college-aged and middle-aged men and women (Imrhan, Imrhan & Hart, 1996; Stunkard & Albaum, 1981). Given potential associations between BMI and DT and bulimic symptoms, BMI was included as a covariate in all analyses.
Statistical Analyses
Analyses were conducted using MPLUS version 7. Little’s MCAR test indicated that follow-up data were not missing completely at random (χ2 = 7.33, p < .03). Sex was a significant predictor of missing data, with men missing significantly more data than women at both 10- and 20-year follow-up (e.g., 35.8% vs. 28.3%; χ2 = 9.29, p = .002). The 1992 cohort also had a greater percentage of missing data at 20-year follow-up compared to the 1982 cohort (33.4% vs. 28%, χ2 = 5.85, p = .02). There were no associations between missing data and eating disorder symptoms or WS, thus, maximum likelihood approach was used to handle missing data (Schafer & Graham, 2002). A linear regression analysis was conducted to examine associations between WS at baseline and bulimic symptoms (EDI-bulimia) at 20-year follow-up. Sex, cohort, baseline bulimic symptoms, baseline body mass index (BMI), and baseline DT (EDI-DT) were included as covariates. Square root transformation was used to correct for non-normality of our bulimic symptoms at 20-year follow-up.1
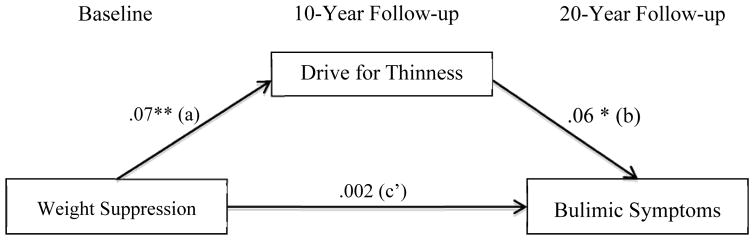
Next, a mediational path analysis using bias corrected bootstrapped 95% confidence intervals (CI) with 10,000 bootstrap samples was used to test the indirect effect of WS at baseline via DT at 10-year follow-up on bulimic symptoms at 20-year follow-up (Preacher & Hayes, 2008) (Figure 1). Bootstrapping is a non-parametric method that generates an estimate of the indirect effect, including a 95% CI. If the CI does not contain zero, then the effect is considered to be statistically significant. Cohort, sex, baseline DT, baseline bulimic symptoms, and baseline BMI were included as covariates in the path from WS to 10-year DT. Baseline WS, cohort, sex, and 10-year DT, 10-year bulimic symptoms, and 10-year BMI were included as predictors or covariates in the prediction of 20-year bulimic symptoms. The ratio of the indirect effect to the total effect (MacKinnon, Warsi, & Dwyer, 1995) was used to estimate the proportion of the effect of WS on 20-year bulimic symptoms that operates indirectly through DT. Furthermore, R2med (Fairchild, MacKinnon, Taborga, & Taylor, 2009) was used to quantify the proportion of variance in 20-year bulimic symptoms attributable to the indirect effect. However, given a number of limitations associated with these effect size measures for mediation, including exclusion of covariates, interpretations of effects sizes should be made with caution (Hayes, 2013).
Figure 1.
Mediation analysis of weight suppression and bulimic symptoms. This diagram displays the direct effect (c′) of weight suppression on bulimic symptoms and the indirect effect (a*b) through the mediator (i.e., drive for thinness [DT]). Covariates included in path (a): cohort, sex, baseline DT, baseline bulimic symptoms, and baseline body mass index. Covariates included in path (b): cohort, sex, 10-year bulimic symptoms, and 10-year body mass index. **p<.001, *p<.01
Results
Table 1 presents means and unstandardized estimates, standardized errors, and effect sizes from the linear regression analysis predicting bulimic symptoms at 20-year follow-up. At baseline, participants’ BMI ranged from 12.7–42.3 kg/m2, with the average being within a healthy range (21.8 kg/m2). Baseline WS ranged from zero to 76 pounds (mean[SD]=7.0 [7.3]). As hypothesized, the linear regression analysis found that higher WS at baseline predicted greater bulimic symptoms at 20-year follow-up while accounting for sex, cohort, and baseline bulimic symptoms, DT, and BMI. WS explained 1.2% of the variance in bulimic symptoms at 20-year follow-up (Table 1). Higher baseline bulimic symptoms, higher baseline BMI, and being in the 1992 cohort also predicted greater bulimic symptoms at follow-up. Overall, this regression model explained 28.4% of the variance in bulimic symptoms (r2 = .284).
Table 1.
Means and Unstandardized Estimates from a Linear Regression Analysis Predicting Bulimic Symptoms at 20-year follow-up
| Variable | Mean | SD | Estimate | S.E. | p | partial r2 |
|---|---|---|---|---|---|---|
| Sex | -- | -- | −.32 | .24 | .18 | .002 |
| Cohort | -- | -- | .42 | .18 | .02 | .005 |
| EDI Bulimia | 12.45 | 4.94 | .33 | .03 | <.001 | .125 |
| Body Mass Index | 21.82 | 2.79 | .22 | .04 | <.001 | .029 |
| EDI Drive for Thinness | 13.50 | 6.66 | −.01 | .02 | .58 | <.001 |
| Weight Suppression | 7.03 | 7.25 | .05 | .01 | <.001 | .012 |
Note. EDI= Eating Disorder Inventory; SD=standard deviation; SE=standard error; all variables represent those at baseline; Sex coded as 1=females, 2=males.
Regarding mediation results, findings from the path analysis appear in Figure 1. Higher WS at baseline was associated significantly with increased DT at 10-year follow-up controlling for baseline DT, baseline BMI, baseline bulimic symptoms, cohort, and sex (CI: 0.03–0.11). Additionally, greater DT at 10-year follow-up was associated significantly with increased bulimic symptoms at 20-year follow-up controlling for 10-year bulimic symptoms, 10-year BMI, cohort, sex, and baseline WS (CI: 0.02–0.11). Consistent with our mediation hypothesis, the direct effect of WS on bulimic symptoms was non-significant while accounting for 10-year DT (CI: −0.02–0.03), and there was a significant indirect effect of WS on bulimic symptoms through DT (CI: 0.001–0.01). The ratio of the indirect effect to the total effect indicates that approximately 67% of the effect of WS on bulimic symptoms occurs indirectly through DT, and approximately 3% of the variance in 20-year bulimic symptoms is attributable to this indirect effect (R2med = .026).
Given the potential for gender differences in associations among WS, DT, and bulimic symptoms, we also conducted a moderated-mediation path analysis using bias corrected bootstrapped 95% CI to test whether the indirect effect of WS on bulimic symptoms via DT was conditional on sex (Hayes, 2015). We explored the possibility that sex moderates the path from WS to DT and/or the path from DT to bulimic symptoms. The covariates included in this model were identical to the previous mediation model with the exception of sex. Sex did not moderate the effect of WS on DT (CI: −0.02–0.20) or the effect of DT on bulimic symptoms (CI: −0.04–0.16), and there was no evidence of moderated-mediation (CI: −0.001–0.01).
Given that DT may precede weight loss and WS, we also examined an alternative model in which WS at 10-year follow-up mediated associations between DT (baseline) and bulimic symptoms (20-year follow-up). This model was identical to that described previously (Figure 1) except that DT and WS were switched. Although DT at baseline was significantly associated with WS at 10-year follow-up (CI: 0.30–0.54) while controlling for baseline WS, there was no significant indirect effect of DT on bulimic symptoms via WS (CI: −0.002–0.01). These findings suggest that there is a bi-directional relationship between DT and WS; however, the pathways through which they influence bulimic symptoms may differ.
Finally, given the bi-directional relationship between DT and WS, associations found between 10-year DT and 20-year bulimic symptoms could be an artifact of higher levels of WS at 10-year follow-up. However, 10-year DT predicted 20-year bulimic symptoms while controlling for 10-year WS (data available upon request), and 10-year WS did not mediate associations between baseline DT and bulimic symptoms in our alternative model. Thus, cognitive concerns related to being thin appear to be a key link in the WS-bulimic symptoms relationship.
Discussion
The current study further supports the clinical significance of WS in bulimic symptomatology, extending the link between WS and bulimic symptoms from 10- (Keel & Heatherton, 2010) to 20-year follow-up representing mid-life for our cohorts. Reducing body weight may have a lasting effect on eating behavior decades later. As such, assessment of WS and elucidating its link to bulimic behaviors may be an important aspect of prevention and treatment. Our findings indicate that increased DT may help explain this relationship across both women and men and may represent an important treatment target among those who have elevated WS.
It may be beneficial to introduce psychological consequences of WS into the psychoeducational components of prevention programs, given that WS predicts eating disorder risk factors (DT) and the onset of bulimic syndromes (Keel & Heatherton, 2010). This information could be incorporated into existing empirically-supported eating disorder prevention programs, including dissonance-based (Becker, Bull, Schaumberg, Cauble, & Franco, 2008; Brown & Keel, 2015; Stice, Marti, Spoor, Presnell, & Shaw, 2008) and healthy weight (Stice, Shaw, Burton, & Wade, 2006) programs that encourage rejection of the thin-ideal and promote a healthy, individualized body weight. Indeed, eating disorder prevention programs may be effective, in part, due to prevention of radical weight loss and eventual WS that would increase risk for BN.
In addition to informing prevention, findings from the current study provide information that may inform eating disorder treatments. Currently, evidenced-based treatments for BN (e.g., cognitive-behavioral therapy [CBT]) do not consider WS in the assessment or treatment of this disorder. A standard course of treatment emphasizes stabilizing eating patterns before addressing cognitive features. Among patients who are high in WS, targeting fear of weight gain during the first stage of CBT may be particularly crucial given evidence that those high in WS may be most likely to gain weight (Carter et al., 2008; Herzog et al., 2010; Lowe et al., 2006). Although the current CBT manual (Fairburn, 2008) indicates that some individuals may gain weight during treatment, identifying early who is at greatest risk for weight gain improves opportunities for personalized approaches to intervention. The role of DT in mediating the link between WS and bulimic symptoms suggests that weight suppressed patients may not have to gain weight to recover from their bulimic-type eating disorder. Instead, it may be possible for them to maintain their weight while adopting healthier attitudes towards their bodies that would free them from the vicious cycle of extreme dietary restriction and large binge episodes.
Although we found that DT mediated associations between WS and bulimic symptoms, it is likely that other consequences of WS, including biological factors, also play a role. This idea is consistent with psychobiological theories of WS and BN and with our previous study finding correlations between WS and leptin and the reinforcing value of food (Bodell & Keel, 2015). Although speculative, it is possible that leptin may mediate associations between WS and DT found in the current study. Specifically, low leptin and reduced satiation associated with greater WS may contribute to one’s sense of needing to exert cognitive control over their eating, increasing DT, vulnerability to binge, and the continued “psychobiological bind” (Butryn et al., 2006). Future longitudinal studies that incorporate both psychological and biological mechanisms are essential to understanding the nature of this relationship.
Overall, the current study advances knowledge on the association between WS and bulimic symptoms through identifying a mediator of this relationship. Additional strengths include the use of a large community-based sample (n = 1699) with a long duration of follow-up (20-years), which allowed us to examine the longer-term consequences of WS using a naturalistic design. Importantly, the retention rate was high, with approximately 70% of the sample at baseline completing surveys at 20-year follow-up. Three waves of data collection allowed us to complete the first test of a mediator for the association between WS and bulimic symptoms in the literature.
Despite noted strengths, there are limitations that warrant attention. Although associations between WS and bulimic symptoms were statistically significant, the effect size was small. This indicates that WS only accounted for a limited proportion of the variance in the maintenance of bulimic symptoms, and examination of effect sizes across durations of follow-up suggests that the strength of the relationship between WS and bulimic symptoms likely decreases over time. Notably, identification of variables that continue to predict bulimic symptoms twenty years later while accounting for a variety of covariates remains remarkable. Additionally, given our interest in WS as a predictor of bulimic symptoms and the nature of this variable (calculated as the difference between highest lifetime weight and current weight – and thus a variable that is always yoked to the time of assessment), we did not examine factors (other than DT) that predate and predict WS that also may contribute to bulimic symptoms. For example, individuals who have high levels of WS have a higher prior weight, which may reflect a drive to excessive food intake that underlies the association between WS and bulimic symptoms. Thus, future studies examining the origin of etiological processes are needed to develop the most effective interventions. Findings from the current study may not generalize to individuals across different weight spectrums, thus, future studies may benefit from examining these associations in samples characterized by a history of obesity in whom maintenance of a lower weight (i.e., high WS) may be necessary to reduce negative health consequences associated with obesity. Similarly, results may not generalize to clinical samples as there may be important differences between predictors of increased levels of self-reported bulimic symptoms and the emergence or worsening of clinically diagnosed BN. Finally, other potentially relevant covariates, such as negative affect, could not be included in analyses, because they were not measured at baseline with the 1982 cohort.
In sum, the current study adds to the growing literature on WS and bulimic symptomatology through use of a 20-year longitudinal design, including three waves of assessment, and examination of a psychological mechanism underlying this association. With over 30% of the United States adult population currently obese (Ogden, Carroll, Curtin, McDowell, Tabak & Flegal, 2006) and an even higher proportion of individuals desiring lasting weight loss (Keel et al., 2006), understanding the link between WS and bulimic symptoms provides important insights into how to free individuals who are weight suppressed from the risk of bulimic symptoms.
Supplementary Material
General Scientific Summary.
Weight suppression is the difference between an individual’s highest past and current weight and is a risk factor for the maintenance of bulimic syndromes. The current study supports that weight suppression contributes to increased preoccupation with being thin, which serves as a key link between weight suppression and bulimic symptoms.
Acknowledgments
This work was supported by a fellowship from the Radcliffe Institute, the Global Foundation for Eating Disorders and grants from the Milton Fund and National Institute of Mental Health (R01MH63758; T32MH93311; T32MH082761). The content of this paper is the sole responsibility of the authors and does not represent the official views of the funding agencies. The authors have no financial conflicts to disclose.
We thank the Radcliffe Institute’s Henry Murray Center for providing access to data from Dr. Colby’s Prevalence of Bulimia among College Students and Dr. Heatherton’s Follow-up and Replication of Prevalence among College Students and the Alumni Office of Harvard University.
Footnotes
Results were identical using transformed or non-transformed variables; thus, results using non-transformed variables are reported.
Portions of this paper were presented at the 2015 International Conference on Eating Disorders in Boston, Massachusetts.
Contributor Information
Lindsay P. Bodell, University of Chicago
Tiffany A. Brown, University of California, San Diego
Pamela K. Keel, Florida State University
References
- Becker CB, Bull S, Schaumberg K, Cauble A, Franco A. Effectiveness of peerled eating disorders prevention: a replication trial. Journal of Consulting and Clinical Psychology. 2008;76(2):347. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Bodell LP, Keel PK. Weight suppression in bulimia nervosa: associations with biology and behavior. Journal of Abnormal Psychology. 2015;124(4):994–1002. doi: 10.1037/abn0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Keel PK. A randomized controlled trial of a peer co-led dissonance-based eating disorder prevention program for gay men. Behaviour Research and Therapy. 2015;74:1–10. doi: 10.1016/j.brat.2015.08.008. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Juarascio A, Lowe MR. The relation of weight suppression and BMI to bulimic symptoms. International Journal of Eating Disorders. 2011;44(7):612–617. doi: 10.1002/eat.20881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Lowe MR, Safer DL, Agras WS. Weight suppression is a robust predictor of outcome in the cognitive-behavioral treatment of bulimia nervosa. Journal of Abnormal Psychology. 2006;115(1):62–67. doi: 10.1037/0021-843x.115.1.62. [DOI] [PubMed] [Google Scholar]
- Carter FA, McIntosh VVW, Joyce PR, Bulik CM. Weight Suppression Predicts Weight Gain Over Treatment but Not Treatment Completion or Outcome in Bulimia Nervosa. Journal of Abnormal Psychology. 2008;117(4):936–940. doi: 10.1037/A0013942. [DOI] [PubMed] [Google Scholar]
- Dawkins H, Watson HJ, Egan SJ, Kane RT. Weight suppression in bulimia nervosa: Relationship with cognitive behavioral therapy outcome. International Journal of Eating Disorders. 2013;46(6):586–93. doi: 10.1002/eat.22137. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. New York, New York: Guilford Press; 2008. [Google Scholar]
- Fairchild AJ, MacKinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behavior Resarch Methods. 2009;41(2):486–498. doi: 10.3758/BRM.41.2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmsted MP, Polivy J. The Eating Disorder Inventory: a measure of cognitive-beahvioral dimensions of anorexia nervosa and bulimia. Anorexia Nervosa: Recent Developments in Research. 1983;3:173–184. [Google Scholar]
- Hayes AF. An index and test of linear moderated mediation. Multivariate Behavioral Research. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- Herzog DB, Thomas JG, Kass AE, Eddy KT, Franko DL, Lowe MR. Weight suppression predicts weight change over 5 years in bulimia nervosa. Psychiatry Research. 2010;177(3):330–334. doi: 10.1016/j.psychres.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imrhan SN, Imrhan V, Hart C. Can self-estimates of body weight and height be used in place of measurements for college students? Ergonomics. 1996;39:1445–1453. [Google Scholar]
- Keel PK, Baxter MG, Heatherton TF, Joiner TE. A 20-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of Abnormal Psychology. 2007;116:422–432. doi: 10.1037/0021-843X.116.2.422. [DOI] [PubMed] [Google Scholar]
- Keel PK, Heatherton TF. Weight Suppression Predicts Maintenance and Onset of Bulimic Syndromes at 10-Year Follow-Up. Journal of Abnormal Psychology. 2010;119(2):268–275. doi: 10.1037/A0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Heatherton TF, Dorer DJ, Joiner TE, Zalta AK. Point prevalence of bulimia nervosa in 1982, 1992, and 2002. Psychological Medicine. 2006;36:119–127. doi: 10.1017/S0033291705006148. [DOI] [PubMed] [Google Scholar]
- Loth KA, MacLehose R, Bucchianeri M, Crow S, Neumark-Sztainer D. Predictors of dieting and disordered eating behaviors from adolescence to young adulthood. Journal of Adolescent Health. 2014;55(5):705–712. doi: 10.1016/j.jadohealth.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychological Bulletin. 1993;114(1):100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Berner LA, Swanson SA, Clark VL, Eddy KT, Franko DL, Shaw JA, … Herzog DB. Weight suppression predicts time to remission from bulimia nervosa. Journal of Consulting and Clinical Psychology. 2011;79(6):772–776. doi: 10.1037/a0025714. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Davis W, Lucks D, Annunziato R, Butryn M. Weight suppression predicts weight gain during inpatient treatment of bulimia nervosa. Physiology and Behavior. 2006;87(3):487–492. doi: 10.1016/j.physbeh.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Thomas JG, Safer DL, Butryn ML. The relationship of weight suppression and dietary restraint to binge eating in bulimia nervosa. International Journal of Eating Disorders. 2007;40:640–644. doi: 10.1002/eat20405. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behavioral Research. 1995;30:41–62. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Jeffery RW, French SA. Self-reported dieting: how should we ask? What does it mean? Associations between dieting and reported energy intake. International Journal of Eating Disorders. 1997;22:437–449. doi: 10.1002/(SICI)1098-108X(199712)22:4<437::AID-EAT9>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Nevonen L, Clinton D, Norring C. Validating the EDI-2 in three Swedish samples: eating disorder patients, psychiatric patients, and normal controls. Nordic Journal of Psychiatry. 2006;60(1):44–55. doi: 10.1080/08039480500504537. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychological Medicine. 1979;9(3):429–48. doi: 10.1017/S0033291700031974. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7(2):147–177. doi: 10.1037//1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Spillane NS, Boerner LM, Anderson KG, Smith GT. Comparability of the Eating Disorder Inventory-2 between women and men. Assessment. 2004;11(1):85–93. doi: 10.1177/1073191103260623. [DOI] [PubMed] [Google Scholar]
- Stice E, Davis K, Miller NP, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: a 5-year prospective study. Journal of Abnormal Psychology. 2008;117(4):941–946. doi: 10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Fisher M, Lowe MR. Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment. 2004;16(1):51–59. doi: 10.1037/1040-3590.16.1.51. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76(2):329. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Maxfield J, Wells T. Adverse effects of social pressure to be thin on young women: an experimental investigation of the effects of “fat talk. International Journal of Eating Disorders. 2003;43(1):108–117. doi: 10.1002/eat.10171. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: a randomized efficacy trial. Journal of consulting and clinical psychology. 2006;74(2):263. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Spangler D, Agras WS. Exposure to media-portrayed thin-ideal images adversely affects vulnerable girls: a longitudinal experiment. Journal of Social and Clinical Psychology. 2001;20(3):270–289. [Google Scholar]
- Stunkard AJ, Albaum JM. The accuracy of self-reported weights. American Journal of Clinical Nutrition. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- Swenne I, Belfrage E, Thurfjell B, Engstrom I. Accuracy of reported weight and menstrual status in teenage girls with eating disorders. International Journal of Eating Disorders. 2005;38:375–379. doi: 10.1002/eat.20199. [DOI] [PubMed] [Google Scholar]
- Tamakoshi K, Yatsuya H, Kondo T, Hirano T, Hori Y, Yoshida T, Toyoshima H. The accuracy of long-term recall of past body weight in Japanese adult men. International Journal of Obesity and Related Metabolic Disorders. 2003;27(2):247–252. doi: 10.1038/sj.ijo.802195802195. [DOI] [PubMed] [Google Scholar]
- Thiel A, Paul T. Test-retest reliability of the Eating Disorder Inventory 2. Joural of Pscyhosomatic Research. 2006;61(4):567–569. doi: 10.1016/j.jpsychores.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Tzoneva M, Forney KJ, Keel PK. The influence of gender and age on the association between “Fat-Talk” and disordered eating: An examination in men and women from their 20’s to their 50’s. Eating Disorders: Journal of Treatment & Prevention. 2015;23:439–454. doi: 10.1080/10640266.2015.1013396. [DOI] [PubMed] [Google Scholar]
- Zunker C, Crosby RD, Mitchell JE, Wonderlich SA, Peterson CB, Crow SJ. Weight Suppression As a Predictor Variable in Treatment Trials of Bulimia Nervosa and Binge Eating Disorder. International Journal of Eating Disorders. 2011;44(8):727–730. doi: 10.1002/Eat.20859. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.