Abstract
Background
Multiple myeloma (MM) is characterized by a neoplastic proliferation of plasma cells primarily in the bone marrow. Bisphosphonates (BP) are used as supportive therapy in the management of MM. This study aimed to analyze the incidence, risk factors, and clinical outcomes of medication-related necrosis of the jaw (MRONJ) in MM patients.
Methods
One hundred thirty MM patients who had previous dental evaluations were retrospectively reviewed. Based on several findings, we applied the staging and treatment strategies on MRONJ. We analyzed gender, age, type of BP, incidence, and local etiological factors and assessed the relationship between these factors and the clinical findings at the first oral examination.
Results
MRONJ was found in nine male patients (6.9%). The mean patient age was 62.2 years. The median BP administration time was 19 months. Seven patients were treated with a combination of IV zoledronate and pamidronate, and two patients received single-agent therapy. The lesions were predominantly located in the mandible (n = 8), and the most common predisposing dental factor was a history of prior extraction (n = 6). Half of the MRONJ were related to diseases found on the initial dental screen. Patients with MRONJ were treated with infection control and antibiotic therapy. When comparing between the MRONJ stage and each factor (sign, location, etiologic factor, BP type, treatment, and outcome), there were no significant differences between stages, except for between the stage and sign (with or without purulence).
Conclusions
For prevention of MRONJ, we recommend routine dental examinations and treatment prior to starting BP therapy.
Keywords: Multiple myeloma, Bisphosphonate, Medication-related necrosis of the jaw
Background
Multiple myeloma (MM) is characterized by a neoplastic proliferation of plasma cells mostly within the bone marrow [1]. MM comprises 0.5% of all cancers in Korea [2]. Worldwide annual incidence is 1.5 per 100,000 individuals. Anemia, renal dysfunction, infections, and bone lesions are the most common complications of MM. In the majority of patients, slow and steady progressive bone damage, or osteolytic lesions, may lead to fractures of the long bones or compression fractures in the spine. Bone pain is often a symptom of this disease, especially severe back pain. Bisphosphonates (BPs) are used in the management of MM as supportive therapy to inhibit the progression of osteoclast activity, which reduces skeletal-related morbidity and mortality [3].
BPs are non-metabolized pyrophosphate analogues that are capable of localizing in bone and inhibiting osteoclast function [4]. These drugs act at the site of active bone remodeling by binding to hydroxyapatite, inhibiting osteoclast development and migratory activity. Inhibiting osteoclast function leads to cell death, which decreases bone resorption without affecting bone mineralization [5]. These non-metabolized analogues are maintained at high concentrations in bone resorption lacunae for an extended period, allowing long-term inhibition of osteoclastic function. In addition, BPs can inhibit bone resorption and decrease bone turnover at the tissue level, as assessed by biochemical markers [4].
In addition to oral BPs used for osteoporosis and osteogenesis imperfecta, intravenous BPs are effective in the treatment and management of several conditions. Intravenous (IV) BPs treat cancer-related conditions, including hypercalcemia of malignancy, lytic lesions in MM, and the effects of bone metastasis in the context of solid tumors, such as breast cancer, prostate cancer, and lung cancer. In metastatic disease to the bone, BPs prevent skeletal complications, reduce bone pain, and improve the quality of life. Additionally, there is some evidence that BPs also have anti-tumor activity. Bisphosphonate therapy is recommended for all patients with multiple myeloma requiring chemotherapy, whether bone lesions are evident or not [6].
Adverse effects associated with the use of BP include pyrexia, gastrointestinal symptoms, hypocalcemia, and renal dysfunction [3, 7]. In 2003, Marx [8] described bisphosphonate-related osteonecrosis of the jaw (BRONJ) as a new complication associated with nitrogen-containing BP use. The American Association of Oral and Maxillofacial Surgeons (AAOMS) published a position paper providing guidance regarding the prevention, diagnosis, and treatment of BRONJ according to the different stages. BRONJ is diagnosed when BP administration is followed by bone exposure that does not heal within 8 weeks of identification and when patients have no history of local radiation therapy [9, 10]. Recently, the term medication-related osteonecrosis of the jaw (MRONJ) was introduced in the updated AAOMS position paper discussing bisphosphonate-related osteonecrosis of the jaw. This updated paper accommodates the growing number of osteonecrosis cases involving the maxilla and mandible associated with other anti-resorptive (denosumab) and anti-angiogenic therapies.
Presently, few reports addressing the epidemiology of MRONJ in patients with MM have been published. Furthermore, few studies with stage and treatment strategies that are recommended by the AAOMS have been published yet. The aim of this study was to analyze the incidence of MRONJ in multiple myeloma patients and to analyze the systemic and local risk factors, including stage and clinical outcome, with standard treatments recommended by the AAOMS position paper. This report focuses on both medical and dental databases at a single-center.
Methods
This retrospective study included MM patients with a history of intravenous bisphosphonate therapy at the Department of Hematology, St. Mary’s Hospital of the College of Medicine, The Catholic University of Korea, who had been referred to the Department of Dentistry for oral examination or dental care. MRONJ was defined when all of the following characteristics were present: (1) current or previous treatment with BPs, (2) exposed bone in the maxillofacial region persisting for more than 8 weeks, and (3) no history of radiation to the jaw. We recorded patients’ clinical signs and symptoms, including the location of exposed and necrotic bone, evidence of infection, pain, and the extent of osteolysis. Based on these findings, we applied the staging and treatment strategies described by the AAOMS position paper on MRONJ to each patient (Table 1) [10]. We analyzed gender, age, type of BP, incidence, and local etiological factors, including their relationship to the clinical findings at the first oral examination. The institutional review board of St. Mary’s Hospital approved this study.
Table 1.
Staging and treatment strategies described by the American Association of Oral and Maxillofacial Surgeons position paper on MRONJ of the jaw
| MRONJ staging | Description | Treatment strategies |
|---|---|---|
| At risk category | No apparent necrotic bone in patients who have been treated with either oral or IV bisphosphonates | No treatment indicated Patient education |
| Stage 0 | No clinical evidence of necrotic bone but non-specific clinical findings and symptoms | Systemic management, including use of pain medication and antibiotics |
| Stage 1 | Exposed and necrotic bone in patients who are asymptomatic and have no evidence of infection | Antibacterial mouth rinse. Clinical follow-up on a quarterly basis. Patient education and review of indications for continued bisphosphonate therapy. |
| Stage 2 | Exposed and necrotic bone associated with infection as evidenced by pain and erythema in the region of the exposed bone with or without purulent drainage | Symptomatic treatment with oral antibiotics. Oral antibacterial mouth rinse. Pain control. Superficial debridement to relieve soft tissue irritation. |
| Stage 3 | Exposed and necrotic bone in patients with pain, infection, and one or more of the following: exposed and necrotic bone extending beyond the region of alveolar bone (i.e., inferior border and ramus in the mandible, maxillary sinus and zygoma in the maxilla) resulting in pathologic fracture, extra-oral fistula, oral antral/oral nasal communication, or osteolysis extending to the inferior border of the mandible of sinus floor | Antibacterial mouth rinse. Antibiotic therapy and pain control. Surgical debridement/resection for long-term palliation of infection and pain. |
For statistical analysis, SAS software package (Version 9.3, SAS Institute) was used. Categorical variables such as sign, location, etiologic factors, BP type, treatment, and outcome were analyzed by Fisher’s exact tests, and continuous variables such as duration were analyzed by Wilcoxon tests. A p value <0.05 was considered statistically significant.
Results
A total of 130 MM patients visited the Department of Dentistry. There were 57 females and 74 males. The mean patient age was 57 years (range 36–76 years). At the initial dental examination, we found 50 cases with calculus deposition, 29 cases with dental caries, 25 cases with periodontal diseases, 24 cases with third molar disease, 14 cases with periapical lesions, and 30 cases with other diseases, including hypersensitivity, cervical abrasion, and attrition. Only two cases of MRONJ associated with tooth extraction were present. In addition, we saw 15 MM cases without dental disease (Fig. 1). However, seven of these patients later developed MRONJ. Overall, jaw necrosis occurred after bisphosphonate therapy in nine cases (6.9%). These patients were all male, and the mean patient age was 62.2 years. The median length of BP exposure was 19 months (range 8–69 months). All patients received intravenous BP therapy. Seven of the patients were treated with a combination of zoledronate and pamidronate, one patient received zoledronate alone, and one received pamidronate alone. Four of the patients were also given an oral bisphosphonate (panonin) (Table 2). The observed lesions were predominantly located in the mandible. Only one case had a maxillary lesion. At the initial visit, only two of the patients with MRONJ presented with exposed bone at the extraction socket. In the remaining patients, we found periodontal diseases (n = 5), calculus deposition (n = 2), mucosal irritation (n = 1), third molar problems (n = 1), and periapical lesions (n = 2). Half of the MRONJ cases occurred at sites that were related to the diseases seen at the initial visit. The most common predisposing dental factor was dental extraction (n = 6), followed by prosthesis irritation (n = 2), and periodontal therapy (n = 1) (Fig. 2). However, one patient developed MRONJ spontaneously (Fig. 3).
Fig. 1.
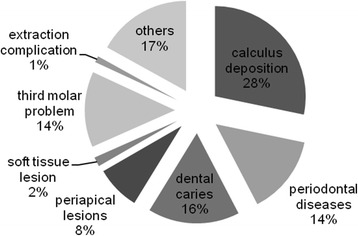
Distribution of the dental problems in multiple myeloma patients at their initial visit
Table 2.
Clinical characteristics of MM patients with MRONJ
| No. | Stage (sign) | locLocation | Etiologic factor | BP types (duration in months) | Treatment | Outcomes (stage) |
|---|---|---|---|---|---|---|
| 1 | II (Bone exposure, pus discharge, pain) | Mandible molar | Denture irritation | Zoledronate, pamidronate (19) | I&D, antibiotics, dressing, biopsy | Bone exposure (stage I) |
| 2 | II (Bone exposure, pus discharge, pain) | Mandible molar | Pontic irritation | Zoledronate, pamidronate (19) | Antibiotics, dressing, biopsy | Bone exposure (stage I) |
| 3 | II (Bone exposure, pus discharge, pain) | Mandible molar | Tooth extraction | Zoledronate (15) | I&D, antibiotics, dressing | Bone exposure (stage I) |
| 4 | II (Bone exposure, pain) | Mandible molar | Tooth extraction | Zoledronate, Pamidronate (69) | Antibiotics, Dressing | Bone exposure (stage I) |
| 5 | II (Bone exposure, pus discharge, pain) | Mandible molar | Tooth extraction | Zoledronate, pamidronate (11) | Saucerization I&D, antibiotics, dressing | No follow-up |
| 6 | I (Bone exposure) | Mandible molar | Spontaneous | Zoledronate, pamidronate (25) | Antibiotics, dressing | Bone exposure (stage I) |
| 7 | II (Bone exposure, pus discharge, pain) | Maxilla molar | Gingival curettage | Zoledronate, pamidronate (40) | Antibiotics, dressing | Bone exposure with pain (stage II) |
| 8 | III (Pain, Osteolytic lesion on Mn. Basal bone) | Mandible molar | Tooth extraction | Pamidronate (8) | Antibiotics, dressing | No f/u |
| 9 | I (Bone exposure) | Mandible molar | Tooth extraction | Zoledronate, pamidronate (17) | Antibiotics, dressing, biopsy | Bone exposure state (died due to systemic disease) |
Fig. 2.
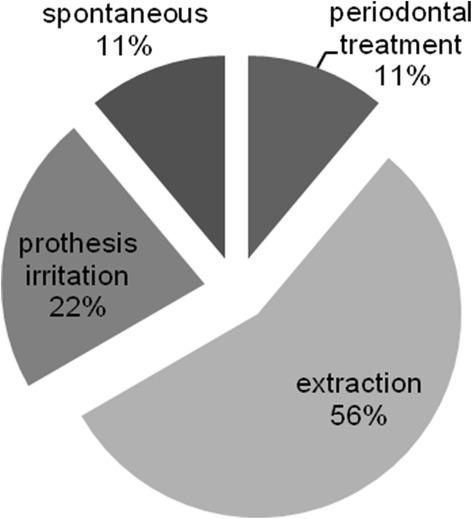
Distribution of cases according to the preceding events
Fig. 3.
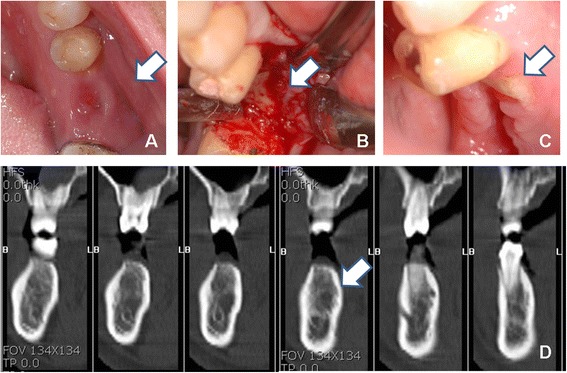
Clinical features and CT of MRONJ patient. a Mucosal fistula on the pontic area. b Intraoperative findings during bone biopsy. c Exposed alveolar bone. d CT findings
According to the AAOMS staging system, five cases were stage II, two cases were stage I, and one case was stage III. One patient progressed from stage 0 to stage II after the biopsy. This patient showed a fistula of unknown origin under the bridge pontic. The Bone scan revealed intense hot uptake in the mandible in this patient, and CT and biopsy exhibited chronic osteomyelitis likely secondary to actinomycosis. However, a few days after the bone biopsy, the bone became exposed despite repair with a primary suture (Fig. 1).
The main treatment methods for patients with MRONJ focus on infection control and antibiotic therapy as recommended by the AAOMS. One patient with stage I MRONJ died after the treatment due to underlying disease, and two patients were lost to follow-up. All six remaining patients presented with non-healing exposed bone during the follow-up. Five of the six patients were stage I, and the remaining patient was stage II. Notably, this stage II patient did not improve with treatment (Table 2).
When comparing between stage and each factor (sign, location, etiologic factor, BP type, treatment, and outcome), there were no significant differences between groups, except for between the stage and sign (with or without pus) (Table 3).
Table 3.
Comparing patients with MRONJ between MM stages according to each factor (sign, location, etiologic factor, BP type, treatment, and outcome) of MM
| Stage | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | P value | |
| Number of patients | 2 | 6 | 1 | |
| Location (%) | 1 | |||
| Mandible | 2 (100) | 5 (83.33) | 1 (100) | |
| Maxilla | 0 (0) | 1 (16.67) | 0 (0) | |
| Infection (%) | 0.0476* | |||
| Yes | 0 (0) | 5 (83.33) | 0 (0) | |
| No | 2 (100) | 1 (16.67) | 1 (100) | |
| Etiology (%) | 0.7222 | |||
| Extraction | 1 (50) | 3 (50) | 1 (100) | |
| Prosthesis problem | 0 (0) | 2 (33.33) | 0 (0) | |
| Periodontal problem | 0 (0) | 1 (16.67) | 0 (0) | |
| Spontaneous | 1 (50) | 0 (0) | 0 (0) | |
| Bisphosphonate type (%) | 0.25 | |||
| Combinationa | 2 (100) | 5 (83.33) | 0 (0) | |
| Only zoledronate | 0 (0) | 1 (16.67) | 0 (0) | |
| Only pamidronate | 0 (0) | 0 (0) | 1 (100) | |
| Treatmentb (%) | 0.6429 | |||
| Conservative | 2 (100) | 3 (50) | 1 (100) | |
| Invasive | 0 (0) | 3 (50) | 0 (0) | |
| Outcome (%) | 1 | |||
| 1 | 1 (100) | 4 (80) | 0 (0) | |
| 2 | 0 (0) | 1 (20) | 0 (0) | |
| Duration in months | 21 (17–25) | 19 (11–69) | 9 (9–9) | 0.2992 |
Categorical variables such as sign, location, etiologic factor, BP type, treatment, and outcome were analyzed by Fisher’s exact test. Continuous variables such as duration were analyzed by Wilcoxon test
*Statistically significant (p value <0.05)
aCombination of zoledronate and pamidronate
bConservative: antibiotic therapy and dressing invasive: biopsy or saucerization
Discussion
The exact mechanism of action underlying the pathogenesis of MRONJ is uncertain. MRONJ may be associated with medication-related apoptosis of osteoclasts or to the anti-angiogenic and suppressive effects that BPs have on endothelial cells [11]. The strong association of intravenous nitrogen-containing BPs with MRONJ compared to oral BPs suggests that intravenous BPs are more bioavailable, allowing increased incorporation into the bone matrix. Only 1% of oral BPs are circulated in the serum due to delayed gastrointestinal tract absorption.
The prevalence of MRONJ in patients treated with intravenous BPs ranges from 0.8 to 12% [10]. According to a cohort study, the estimated incidence of MRONJ in MM patients is 8.42%, and the highest incidence is in patients who received a combination of pamidronate and zoledronate (range 5 to 51%). Zoledronate is associated with MRONJ in 3 to 11% of MM cases, while the pamidronate-related frequency of MRONJ ranges from 0 to 18% [3]. The overall incidence of MRONJ in our study was 6.9% (9/130 MM patients). Of these nine patients, 77.7% (n = 7) received a combination of pamidronate and zoledronate.
Studies evaluating the duration of bisphosphonate therapy as a risk factor for MRONJ development in MM patients have yielded inconsistent results [6, 9]. In our patients, the median length of BP exposure was 19 months, which is similar to the results of Berenson et al. (18 months of zoledronate) [12]. However, our results are not consistent with those of Corso et al. [13] (47 months of pamidronate and zoledronate combination therapy), Zervas et al. [14] (24 months of pamidronate), and Dimopoulos et al. (53.4 months of pamidronate and zoledronate combination therapy) [15].
It is thought that the jaw is more predisposed to MRONJ compared to other bones. This may be due to healing of open bone wounds, vulnerability to bacterial infections, and that BPs are preferentially deposited in bone with higher turnover rates, such as the jaw [16, 17]. Wen et al. [18] supported the theory that BPs preferentially deposit into bones with higher rates of remodeling, such as the jaw, relative to non-oral sites. Using athymic rats, they demonstrated a significantly higher release of hydroxyapatite-bound bisphosphonate in oral bones compared to axial and appendicular sites. After injection of fluorescent pamidronate into the mice, more signal was detected and was retained for longer time periods in the mandible than in the femur [19], which demonstrates that the mandible has a high affinity for BPs. Notably, MRONJ is twice as common in the mandible as in the maxilla [10]. Marx et al. [20] reported that 68.1% of the MRONJ cases occur in the mandible and 27.7% occur in the maxilla. Similar results were found in a study by Bardos et al. [5], where 15 of 22 MM patients with MRONJ showed mandibular lesions, five showed both mandibular and maxillary lesions, and two were in the maxilla only. In our study, only one patient presented with MRONJ in the maxilla. One possible explanation for osteonecrosis secondary to BP use, especially in the mandible, may be BP’s anti-angiogenic effects, or the anatomic and physiologic features of the mandible might increase the risk of MRONJ [21, 22]. Unfortunately, the exact mechanism underlying the higher incidence of MRONJ in the mandible remains unknown.
In MRONJ, dental extraction is the biggest local risk factor [6]. The surgical damage to the jaw that occurs after extraction, especially the damage to the alveolar bone with open bone wounds, seems to be the most potent trigger for MRONJ. In extractions, jaw bone remodeling is depressed, leading to the spontaneous breakdown of the wound after the tooth is removed. Notably, the site of the pre-existing bone might not be of prime importance. Woven bone is not altered by BPs, but remodeling of woven bone into lamellar bone might be impaired, leading to MRONJ [23]. Patients receiving intravenous BPs and undergoing dentoalveolar treatment are at least seven times more likely to develop MRONJ than those who are not [5, 10]. Tooth extraction is associated with 77% of MRONJ cases in the patients with intravenously administrated BPs [6]. In our study, the most common risk factor for MRONJ was dental extraction (n = 6), followed by prosthesis irritation (n = 2), periodontal therapy (n = 1), and unknown causes (n = 1). Half of the MRONJ locations coincided with the site of the dental problem seen at the first visit.
This retrospective study has some limitations. Firstly, we did not evaluate the patients’ oral health prior to initiating bisphosphonate therapy. However, we found that periodontal disease, including calculus deposition, was the most frequent dental disease in the MM patients at the initial dental examination such as in them with MRONJ. Aside from the two patients who initially presented with MRONJ, the majority of MM patients had periodontal problems, such as calculus deposition (n = 50), periodontal lesions (n = 25), and dental caries (n = 29). These results are similar to those of MM patients with MRONJ. In MM with MRONJ, the most common dental disease was periodontal disease (n = 5), followed by calculus deposition (n = 2), periapical lesions (n = 2), mucosal irritation (n = 1), and third molar problems (n = 1). Thus, clinical examinations, including panoramic radiography, may help detect dental problems and improve oral health before and during bisphosphonate therapy.
Based on our data, prevention of MRONJ is optimal because its management is quite challenging. While some case reports have demonstrated surgical treatment with good outcomes, generally, aggressive surgery has been counterproductive, often exacerbating the bone exposure [24]. Hence, most publicized studies suggest that initial treatment (stage I, II) should be conservative, focusing on systematic antibiotic therapy, irrigation to optimize oral hygiene, and careful removal of sequesters [10, 17, 25]. However, only 23–53% of all patients achieve resolution of mucosal discontinuities [26, 27]. Bamias et al. [7] demonstrated that antibiotic therapy resulted in temporary improvement, but only one patient showed sustained improvement of their osteonecrosis after multiple courses of antibiotics. The remaining 11 MM patients with MRONJ had persistent disability, mainly experiencing recurrence with purulent discharge and pain after discontinuing their antibiotics. These results coincide well with ours. In this present study, after conservative treatment as recommended by the AAOMS, the majority of stage II patients has been improved and was reclassified as stage I, but all patients remained with unhealed exposed bone at the follow-up appointment.
Conclusions
Osteonecrosis of the jaw has been recognized as a serious complication of intravenous BP treatment, especially in patients with MM. We found that the majority of MM patients with MRONJ received a combination of pamidronate and zoledronate. The mandible, particularly at molar extraction sites, was the most frequent area affected. In some patients, the location of MRONJ and the type of dental problem coincided with the oral condition seen at the initial visit. Management regimens that lead to complete resolution of MRONJ remain elusive. While conservative therapy improved some conditions, all patients were left with some remaining exposed bone. Therefore, the prevention of MRONJ is crucial. Routine dental examinations and treatment of dental diseases should be performed prior to initiating bisphosphonate therapy.
Acknowledgements
This study was funded by a research grant from the Institute of Clinical Medicine Research at the Catholic University of Korea, Yeouido St. Mary’s Hospital.
Authors’ contributions
WSC and JIL participated in the data analysis and helped to draft the manuscript. HJY participated in the design of study and revision. CKM participated in the design of study and contributed in the acquisition of data. SHL conceived of the study, participated in the design and coordination of the study and the statistical analysis and helped to draft the manuscript. WSC and JIL equally participated in drafting of the manuscript as first authors. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have ncompeting interests.
References
- 1.Tricot G. Multiple myeloma and other plasma cell disorders. Hematology: basic principles and practice. 3. Philadelphia: Churchill Livingstone; 2000. pp. 1398–416. [Google Scholar]
- 2.Won YJ, Sung J, Jung KW, Kong HJ, Park S, Shin HR, Park EC, Ahn YO, Hwang IK, Lee DH. Nationwide cancer incidence in Korea, 2003-2005. Cancer Res Treat. 2009;41:122–31. doi: 10.4143/crt.2009.41.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mhaskar R, Redzepovic J, Wheatley K, Clark OA, Miladinovic B, Glasmacher A, Kumar A, Djulbegovic B (2012) Bisphosphonates in multiple myeloma: a network meta-analysis. Cochrane Database Rev 16:CD003188. [DOI] [PubMed]
- 4.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–34. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Badros A, Weikel D, Salama A, Goloubeva O, Schneider A, Rapoport A, Fenton R, Gahres N, Sausville E, Ord R, Meiller T. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol. 2006;24:945–52. doi: 10.1200/JCO.2005.04.2465. [DOI] [PubMed] [Google Scholar]
- 6.Boonyapakorn T, Schirmer I, Reichart PA, Sturm I, Massenkeil G. Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol. 2008;44:857–69. doi: 10.1016/j.oraloncology.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Bamias A, Kastritis E, Bamia C, Moulopoulos LA, Melakopoulos I, Bozas G, Koutsoukou V, Gika D, Anagnostopoulos A, Papadimitriou C, Terpos E, Dimopoulos MA. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005;23:8580–7. doi: 10.1200/JCO.2005.02.8670. [DOI] [PubMed] [Google Scholar]
- 8.Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–7. doi: 10.1016/S0278-2391(03)00720-1. [DOI] [PubMed] [Google Scholar]
- 9.Kos M, Kuebler JF, Luczak K, Engelke W. Bisphosphonate-related osteonecrosis of the jaws: a review of 34 cases and evaluation of risk. J Craniomaxillofac Surg. 2010;38:255–9. doi: 10.1016/j.jcms.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J Oral Maxillofac Surg Suppl. 2009;67:2–12. doi: 10.1016/S0278-2391(09)01877-1. [DOI] [PubMed] [Google Scholar]
- 11.Bagan J, Scully C, Sabater V, Jimenez Y. Osteonecrosis of the jaws in patients treated with intravenous bisphosphonates (BRONJ): a concise update. Oral Oncol. 2009;45:551–4. doi: 10.1016/j.oraloncology.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Berenson JR, Yellin O, Crowley J, Makary A, Gravenor DS, Yang HH, Upadhyaya GH, Flinn IW, Staszewski H, Tiffany NM, Sanani S, Farber CM, Morganstein N, Bolejack V, Nassir Y, Hilger JD, Sefaradi A, Shamouelian A, Swift RA. Prognostic factors and jaw and renal complications among multiple myeloma patients treated with zoledronic acid. Am J Hematol. 2011;86:25–30. doi: 10.1002/ajh.21912. [DOI] [PubMed] [Google Scholar]
- 13.Corso A, Varettoni M, Zappasodi P, Klersy C, Mangiacavalli S, Pica G, Lazzarino M. A different schedule of zoledronic acid can reduce the risk of the osteonecrosis of the jaw in patients with multiple myeloma. Leukemia. 2007;21:1545–8. doi: 10.1038/sj.leu.2404682. [DOI] [PubMed] [Google Scholar]
- 14.Zervas K, Verrou E, Teleioudis Z, Vahtsevanos K, Banti A, Mihou D, Krikelis D, Terpos E. Incidence, risk factors and management of osteonecrosis of the jaw in patients with multiple myeloma: a single-centre experience in 303 patients. Br J Haematol. 2006;134:620–3. doi: 10.1111/j.1365-2141.2006.06230.x. [DOI] [PubMed] [Google Scholar]
- 15.Dimopoulos MA, Kastritis E, Anagnostopoulos A, Melakopoulos I, Gika D, Moulopoulos LA, Bamia C, Terpos E, Tsionos K, Bamias A. Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica. 2006;91:968–71. [PubMed] [Google Scholar]
- 16.Ruggiero SL, Drew SJ. Osteonecrosis of the jaws and bisphosphonate therapy. J Dent Res. 2007;86:1013–21. doi: 10.1177/154405910708601101. [DOI] [PubMed] [Google Scholar]
- 17.Ikebe T. Pathophysiology of BRONJ: drug-related osteoclastic disease of the jaw. Oral Sci Int. 2013;10:1–8. doi: 10.1016/S1348-8643(12)00045-6. [DOI] [Google Scholar]
- 18.Wen D, Qing L, Harrison G, Golub E, Akintoye SO. Anatomic site variability in rat skeletal uptake and desorption of fluorescently labeled bisphosphonate. Oral Dis. 2011;17:427–32. doi: 10.1111/j.1601-0825.2010.01772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozloff KM, Volakis LI, Marini JC, Caird MS. Near-infrared fluorescent probe traces bisphosphonate delivery and retention in vivo. J Bone Miner Res. 2010;25:1748–58. doi: 10.1002/jbmr.66. [DOI] [PubMed] [Google Scholar]
- 20.Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567–75. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg. 1983;41:283–8. doi: 10.1016/0278-2391(83)90294-X. [DOI] [PubMed] [Google Scholar]
- 22.Wood J, Bonjean K, Ruetz S, Bellahcene A, Devy L, Foidart JM, Castronovo V, Green JR. Novel antiangiogenic effects of the bisphosphonate compound zoledronic acid. J Pharmacol Exp Ther. 2002;302:1055–61. doi: 10.1124/jpet.102.035295. [DOI] [PubMed] [Google Scholar]
- 23.Wutzl A, Pohl S, Sulzbacher I, Seemann R, Lauer G, Ewers R, Drach J, Klug C. Factors influencing surgical treatment of bisphosphonate-related osteonecrosis of the jaws. Head Neck. 2012;34:194–200. doi: 10.1002/hed.21708. [DOI] [PubMed] [Google Scholar]
- 24.Ruggiero S, Gralow J, Marx RE, Hoff AO, Schubert MM, Huryn JM, Toth B, Damato K, Valero V. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract. 2006;2:7–14. doi: 10.1200/JOP.2.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, Gagel RF, Gilsanz V, Guise T, Koka S, McCauley LK, McGowan J, McKee MD, Mohla S, Pendrys DG, Raisz LG, Ruggiero SL, Shafer DM, Shum L, Silverman SL, Van Poznak CH, Watts N, Woo SB, Shane E. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2007;22:1479–91. doi: 10.1359/jbmr.0707onj. [DOI] [PubMed] [Google Scholar]
- 26.Hoff AO, Toth BB, Altundag K, Johnson MM, Warneke CL, Hu M, Nooka A, Sayegh G, Guarneri V, Desrouleaux K, Cui J, Adamus A, Gagel RF, Hortobagyi GN. Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res. 2008;23:826–36. doi: 10.1359/jbmr.080205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van den Wyngaert T, Claeys T, Huizing MT, Vermorken JB, Fossion E. Initial experience with conservative treatment in cancer patients with osteonecrosis of the jaw (ONJ) and predictors of outcome. Ann Oncol. 2009;20:331–6. doi: 10.1093/annonc/mdn630. [DOI] [PubMed] [Google Scholar]


