Abstract
Background
Laparoscopic right hemicolectomy for colon cancer is associated with substantial morbidity despite the introduction of enhanced recovery protocols and laparoscopic surgery. Laparoscopic right hemicolectomy with an intracorporeal anastomosis (IA) is less invasive than laparoscopic assisted hemicolectomy, possibly leading to further decrease in post-operative morbidity and faster recovery. The current standard technique includes an extracorporeal anastomosis with mobilization of the colon, mesenteric traction and a extraction wound located in the mid/upper abdomen with relative more post-operative morbidity compared to extraction wounds located in the lower abdomen.
Methods
A systematic review of PubMed and Embase databases was performed on studies comparing the intracorporeal versus the extracorporeal performed anastomosis in laparoscopic right hemicolectomy. Primary outcomes were mortality, short-term morbidity and length of stay. For quality assessment, the MINORS checklist was used. Meta-analysis was performed using a random-effects model, and a subgroup analysis was performed for data regarding short-term morbidity and length of stay in studies published in 2012≥.
Results
A total of 2692 papers were identified, 12 non-randomized comparative studies were included in the analysis with a total number of 1492 patients. No significant change in mortality was found (OR 0.36, 95 % CI 0.09–1.46; I 2 = 0 %). Short-term morbidity decreased significantly in favour of IA (OR 0.68, 95 % CI 0.49–0.93; I 2 = 20 %). Length of stay was decreased, but with serious risk of heterogeneity (MD −0.77 days, 95 % CI −1.46 to −0.07; I 2 = 81 %). Subgroup analysis for papers published in 2012≥ resulted in an even larger decrease in short-term morbidity (OR 0.65, 95 % CI 0.50–0.85; I 2 = 0 %) and a significant decrease in length of stay with low risk of heterogeneity (MD −0.77 days, 95 % CI −1.17 to −0.37; I 2 = 4 %).
Conclusion
Intracorporeal anastomosis in laparoscopic right hemicolectomy is associated with reduced short-term morbidity and decreased length of hospital stay suggesting faster recovery as shown in this meta-analysis.
Keywords: Laparoscopy, Right hemicolectomy, Totally laparoscopic, Laparoscopic assisted, Intracorporeal, Extracorporeal, Anastomosis
Background
Colorectal carcinoma is the second most common form of cancer in the western world, with an estimated incidence of 1.36 million cases in 2012 worldwide [1, 2]. Right sided hemicolectomy for right sided colonic cancer is a common performed procedure [3]. Currently, in most countries, the laparoscopic assisted right hemicolectomy with an extracorporeal anastomotic (EA) technique is the standard technique. However, despite introduction of laparoscopic surgery [4] and enhanced recovery protocols [5] in colorectal surgery, morbidity remains substantial. Large randomized trials and national registry data show that the overall in hospital morbidity is still approximately 30 % [3, 5, 6].
Morbidity associated with laparoscopic right hemicolectomy includes prolonged ileus, pain-associated decreased pulmonary function and wound infection leading to subsequent increased length of stay [3, 5, 6]. The current standard procedure for laparoscopic right hemicolectomy includes formation of an extracorporeal anastomosis requiring mobilization of the colon and mesenteric traction in order to extract the ileum and ascending colon theoretically leading to more surgical trauma [7]. Furthermore, the EA technique requires the extraction wound to be located in the mid/upper abdomen with relative more post-operative morbidity compared to a wound in the lower abdomen, since it is known that an incision in the mid/upper abdomen tend to result in increased post-operative pain and compromise pulmonary function compared to lower extraction wounds such as the Pfannenstiel [5, 8].
Recent developments in minimal invasive techniques have facilitated intracorporeal stapled anastomosis (IA). This technique enables a smaller extraction wound in the lower abdominal wall and enables a resection of the right colon with less mobilization and mesenteric traction. Potentially, the risk of mesenteric twisting is less compared to the EA technique [9]. Disadvantages of the intracorporeal anastomosis technique include a longer learning curve and laparoscopic skills including suturing and a risk of intraabdominal faecal spillage [10]. Despite potential benefits of the intracorporeal technique, previous reviews published in 2013 failed to show clear advantages of the newer technique [11, 12]. Since the more recently published studies [13–19] show benefits in short-term morbidity and shorter length of stay for the IA technique, we have conducted an up-to-date systematic review with the most recent studies to investigate the value of the intracorporeal anastomotic technique for laparoscopic right hemicolectomy. We hypothesized that an intracorporeal performed anastomosis leads to a decrease in short morbidity resulting in a shorter length of stay. Secondary endpoints include anastomotic leakage, ileus, incisional surgical site infection and incisional hernia. This systematic review aims to provide a complete overview of studies comparing both techniques.
Methods
A systematic literature review was performed according to guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist (PRISMA) [20].
Search strategy
A comprehensive search was performed in the bibliographic databases PubMed and Embase from inception to 21 December 2015, in collaboration with a medical librarian. Search terms included controlled terms (Mesh in PubMed, Emtree in Embase), as well as free-text terms. The following terms were used (including synonyms and closely related words) as index terms or free-text words: ‘colectomy’, ‘anastomosis’, ‘intracorporeal’, ‘extracorporeal’ and ‘laparoscopy’. The search was performed without date, language or publication status restriction. All titles were screened, and appropriate abstracts were reviewed. See ‘Appendix’ for the search strategy.
In- and exclusion criteria
Studies eligible for inclusion were: RCT’s, comparative studies on intra- versus extracorporeal anastomosis in laparoscopic right hemicolectomy, and human studies. Exclusion criteria were: non-right hemicolectomy (i.e. transverse or left hemicolectomy, sigmoidectomy, subtotal colectomy), non-comparative (case series, description of technique), single-incision surgery, purely robotic surgery and open hemicolectomy.
Selection process
After removal of duplicates, two independent reviewers (SvO and AE) selected the studies by screening on title and abstract. If necessary, a third author was consulted in case of disagreement. Two reviewers (SvO and AE) analysed the resulting papers in full text using the online Covidence review manager (Covidence online review manager 2015, www.covidence.org). Further studies were identified by reference checking of the included studies.
Quality assessment and scoring
To asses methodological quality of the included studies, the ‘Methodological index for non-randomized studies’ (MINORS) instrument was used [21]. We considered follow-up for short-term outcomes as a period 30 days. ‘Follow-up period appropriate to the aim of the study’ was considered reported inadequate if outcomes were not defined as 30-day complications or 30-day readmission rate. The interval of long- or medium-term follow-up (FU) had to be reported explicitly. ‘Loss to follow-up’ was scored with 2 points if mentioned explicitly or if it could be derived from the outcomes (i.e. percentage 30-day readmission). If end of the FU-period was not yet achieved in all patients, ‘Loss to follow-up’ was rewarded 1 point. Prospective collection of data was adequately reported if the authors explicitly mentioned the use of a prospectively maintained database.
Outcomes of interest
Our primary outcomes of interest were short-term morbidity, mortality and length of stay. Secondarily, we looked at the intraoperative outcomes and the rates of anastomotic leak rate, ileus, incisional surgical site infection (SSI) and incisional hernia. Because the definitions of short-term morbidity varied among the included studies, we derived short-term morbidity of each study separately. If the Clavien–Dindo classification for post-operative complications was used, class V (death) was separated from the total of complications to assess mortality. SSI was considered to be a superficial or deep incisional wound infection, but not as an intraabdominal abscess or organ space infection. Incisional hernia was specified to the extraction site and did not include trocar site herniation. It was postulated that the learning curve of the surgeons could have an impact on the outcomes of the IA. Therefore, a subgroup analysis was performed for studies published in 2012 and later on short-term morbidity and length of stay to see whether the more recent studies showed a larger effect.
Quantitative analysis
Data analysis was performed with the use of Revman 5.0 (Review Manager 5.0, Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008). Dichotomous outcomes were statistically analysed and summarized by using the odds ratio (OR) with a confidence interval (CI) of 95 %. Mantel–Haenszel method was used to combine the OR of the outcomes using a random-effects model. Continuous outcomes were analysed by computing a mean difference (MD). OR < 1 favours the IA group and was considered statistically significant if p < 0.05 if the 95 % CI did not include 1. Heterogeneity was assessed by performing an I 2 statistic and a Chi-squared test, considering I 2 > 50 % and Chi-squared p value <0.1 as statistically significant heterogeneity [22]. A subgroup analysis was done for data regarding short-term morbidity and length of stay in studies published in 2012≥.
Results
Literature search
The search resulted in a total of 2692 papers after removal of duplicates. After screening on title and abstract, 24 papers were assessed by full text. A total of 12 papers were excluded for various reasons [9, 11, 12, 23–31], see Fig. 1. Finally, 12 studies were incorporated in the qualitative analysis [13–19, 32–36]. For studies with overlap, we included the most recent publications which consisted of more patients [13, 36] and excluded the earlier studies [9, 23]. No additional studies were identified by cross-checking the references of the included papers.
Fig. 1.
Flowchart
Magistro et al. reported the only prospective study that alternatively assigned patients to the two procedures [14]. Eleven studies were of retrospective design [13, 15–19, 32–36]. Milone et al. [16] matched the control group using a propensity score. Trastulli et al. [18] reported a retrospective multicenter case series on right colectomy comparing robotic intracorporeal anastomosis to laparoscopic intracorporeal anastomosis and laparoscopic extracorporeal anastomosis. The included studies resulted in a total number of 1492 participants who underwent a laparoscopic right hemicolectomy further specified to 763 and 729 patients for intra- or extracorporeal anastomosis, respectively. Study design and patient characteristics are described in Table 1. In nine studies, the intracorporeal performed anastomosis was created using a mechanical stapler with [13–15, 17–19, 33, 35, 36] or without [16] additional sutures in the IA technique. A mechanical stapler was most commonly used for the extracorporeal anastomosis as well (with [13, 14, 18, 36] or without [16, 19] additional sutures). One study made a hand-sewn anastomosis [15] or according to the preference of the individual surgeon (mechanical or hand-sewn) [17, 33]. Two studies did not specify the creation of the anastomosis [32, 34].
Table 1.
Study characteristics
| Study (author, YoP) | Design | Malignant | Benign | Patients (n) | Age | BMI (kg/m2) | ASA classification | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IA | EA | IA | EA | IA | EA | IA | EA | ||||
| Anania, 2012 | Retrospective CCS | + | − | 39 | 33 | 74.5 (53–89)b | 74 (45–96)b | 26.3 (20–37)b | 28.1 (19.9–37)b | NR | NR |
| Chaves, 2011 | Retrospective CCS | + | + | 35 | 25 | 62.6 (13.4)a | 58.9 (12.9)a | 25.9 (3.1)a | 26.7 (3.9)a | 17/18c | 15/10c |
| Fabozzi, 2010 | Retrospective CCS | + | − | 50 | 50 | 62.1 (8.3)a | 59.4 (9.5)a | 21.4 (2.3)a | 22.1 (1.6)a | 2 (1–2)b | 2 (1–2)b |
| Lee, 2013 | Retrospective CCS | + | + | 51 | 35 | 70 (43–90)b | 66 (48–93)b | 25.7 (18–46.5)b | 25.4 (18.3–45.3)b | 3 (2–4)b | 3 (1–3)b |
| Magistro, 2013 | Prospective CCS | + | + | 40 | 40 | 70.9 (13.4)a | 71.2 (10.5)a | 24.8 (2.8)a | 23.9 (4.4)a | 2 (1–3)b | 2 (1–3)b |
| Marchesi, 2013 | Retrospective CCS | + | + | 28 | 27 | 66.2a | 67.7a | 26.1a | 26.2a | 19/9c | 17/10c |
| Milone, 2015 | Retrospective CCS | + | + | 286 | 226 | 67.7 (12.6)a | 65.6 (11.4)a | 25.2 (3.8)a | 25.4 (3.8)a | 2 (1–4)b | 2 (1–4)b |
| Roscio, 2012 | Retrospective CCS | + | − | 42 | 30 | 63.5 (10.3)a | 63.7 (10.3)a | 26.0 (4.0)a | 26.3 (3.8)a | 2 (1–3)b | 2 (1–3)b |
| Scatizzi, 2010 | Retrospective CCS | + | − | 40 | 40 | 70 (47–87)b | 68.5 (41–85)b | 28a | 27b | 2 (1–3)b | 2 (1–3)b |
| Shapiro, 2015 | Retrospective CCS | + | − | 91 | 100 | 72 (45–90)b | 72 (49–90)b | 27.8 (4.6)a | 26.9 (4.3)a | 3 (1–4)b | 3 (1–4)b |
| Trastulli, 2015 | Retrospective CCS | + | + | 40 | 94 | 71.5a | 70.8a | 26.6a | 25.4a | 2 (1–3)b | 2 (1–3)b |
| Vergis, 2015 | Retrospective CCS | + | + | 21 | 29 | 65a | 69a | 27a | 28a | 2.65a | 3.04a |
YoP year of publication, CCS case-controlled series, ASA American Society of Anaesthesiologists, N number
aMean (SD), b median (range), c ASA-score 1 + 2/3 + 4, number of patients
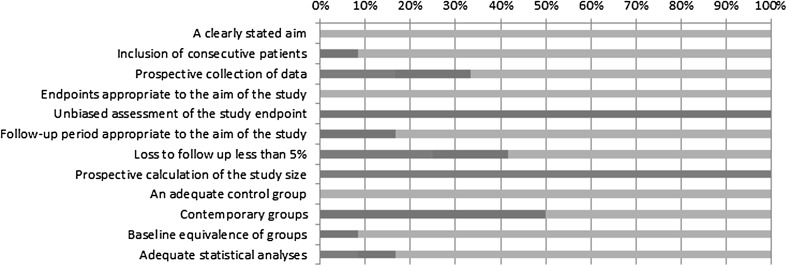
Quality assessment: MINORS instrument
The quality assessment is shown in Table 2 and Fig. 2. The mean score was 18.8 (range 16–21) out of a total of 24 points. In some studies reporting on mid- or long-term outcomes, the foreseen follow-up period was not achieved in all patients and was regarded as reported but defined as ‘not adequately’ [13, 17]. Several studies, aiming to compare short-term outcomes, failed to (adequately) report 30-day outcomes including readmission and/or reported no visits to the outpatient clinic after discharge [14, 16, 32]. Interestingly, Scatizzi et al. [36] defined short-term outcomes as 90 days and reported an outpatient clinic visit 8 days after discharge, but subsequently failed to report on the 3 month FU besides readmission. Half of the studies changed their way of operation halfway during the score inclusion period from EA to IA, using their last EA as ‘historic’ control group [15, 18, 19, 32, 33, 35]. All studies scored low on unbiased assessment of outcomes due to lack of blinding and randomization. None calculated a sample size since 11 studies were retrospective and 1 study was only pseudo-randomized [14].
Table 2.
MINORS quality assessment
| A clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | Endpoints appropriate to the aim of the study | Unbiased assessment of the study endpoint | Follow-up period appropriate to the aim of the study | Loss to follow-up less than 5 % | Prospective calculation of the study size | An adequate control group | Contemporary groups | Baseline equivalence of groups | Adequate statistical analyses | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anania | 2 | 2 | 1 | 2 | 1 | 2 | 0 | 0 | 2 | 1 | 2 | 2 | 17 |
| Chaves | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 20 |
| Fabozzi | 2 | 1 | 0 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 17 |
| Lee | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Magistro | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 19 |
| Marchesi | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 20 |
| Milone | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 20 |
| Scatizzi | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 21 |
| Shapiro | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 20 |
| Roscio | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 1 | 2 | 2 | 19 |
| Trastulli | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 16 |
| Vergis | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 19 |
| Not reported | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 12 | 0 | 0 | 0 | 1 | 17 |
| Reported, inadequate | 0 | 1 | 2 | 0 | 12 | 2 | 3 | 0 | 0 | 6 | 1 | 1 | 28 |
| Reported, adequate | 12 | 11 | 8 | 12 | 0 | 12 | 7 | 0 | 12 | 3 | 11 | 10 | 98 |
Fig. 2.
MINORS quality assessment
Percentage adequately reported (italics). Percentage reported but inadequate: 1 point (bold). Percentage not reported: 0 points (bold italics).
Primary outcomes
Mortality
No significant difference in mortality was observed for both procedures: OR 0.36, 95 % CI 0.09–1.46; I 2 = 0 % (Fig. 3).
Fig. 3.
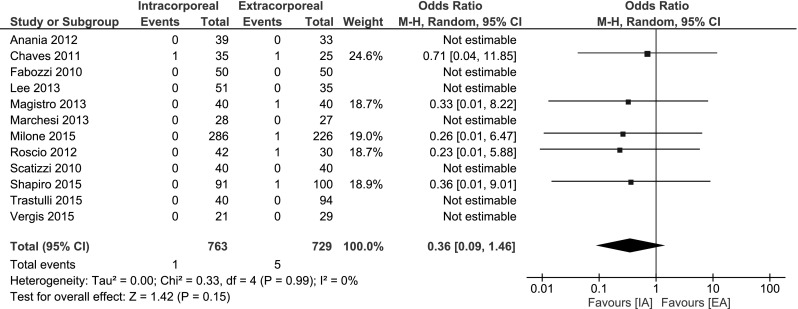
Mortality
Short-term morbidity
A significant decrease in short-term morbidity was observed when performing an IA: OR 0.68, 95 % CI 0.49–0.93; I 2 = 20 %. Subgroup analysis on studies published ≥2012 showed a larger decrease and less risk at heterogeneity: OR 0.65, 95 % CI 0.50–0.85; I 2 = 0 %. Four studies reported morbidity according to Clavien–Dindo [15–17, 35]. Two other studies reported 30-day complication rate [18, 33]. One study described the amount of complications in text [32]. The remaining studies provided a table of complications differentiated to mortality, minor and major morbidity [13, 14, 34, 36] (Fig. 4).
Fig. 4.

Short-term morbidity
Length of stay
In the meta-analysis, Length of stay (LoS) was significantly decreased if favour of IA: MD −0.77 days, 95 % CI −1.46 to −0.07. However, heterogeneity among studies was substantial. Subgroup analysis on studies published ≥2012 was more homogenous and showed a statistically significant decrease in LoS (0.77 days, 95 % CI −1.17 to −0.37) (Fig. 5). Two studies were not included in the meta-analysis. Trastulli et al. [18] provided a median (range) of 5.5 days (3–14) for IA versus 7 (4–21) in the EA group. The mean LoS in the study by Vergis et al. [19] was 5.33 and 5.86 for IA and EA, respectively. Unfortunately, no SD was provided.
Fig. 5.

Length of stay
Secondary outcomes
Intraoperative outcomes
Duration of surgery
Operating time varied widely, with conflicting significant outcomes in either IA or EA. Magistro et al. and Shapiro et al. reported a significant longer duration of surgery (DoS) for IA [14, 17]. In contrast, Fabozzi et al. [34] and Roscio et al. [35] stated the IA technique was faster. However, most studies showed no significant difference. Interestingly, Marchesi et al. reported the time to perform the anastomosis separately and showed an impressive reduction at the end of his IA series indicating a learning curve. The mean DoS of his last 10 IA was 161 min versus his mean EA time of 186.8 min [15]. See ‘Appendix’.
Post-operative outcomes
Anastomotic leak rate
No statistically significant difference between the IA or EA technique was found for anastomotic leakage: OR 0.77, 95 % CI 0.39–1.49; I 2 = 0 % (Fig. 6).
Fig. 6.
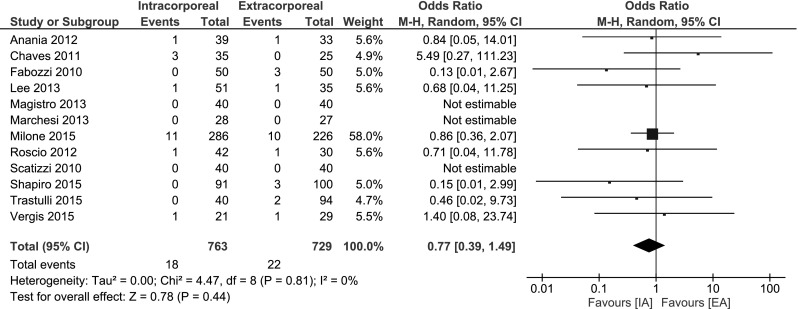
Anastomotic leak
Ileus
The incidence of an ileus was reported in 6 studies [13–18, 33], no significant change was found: OR 0.94, 95 % CI 0.57–1.57; I 2 = 0 % (Fig. 7).
Fig. 7.
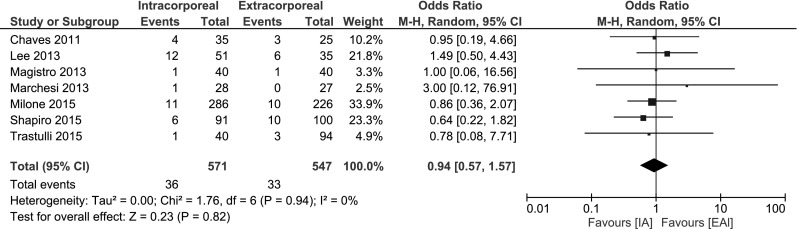
Ileus
Surgical site infection
All but one study [32] mentioned the occurrence of a surgical site infection (please note: superficial and deep incisional surgical site infection, not abscess or organ spaced SSI). A significant decrease in SSI was found (OR 0.56, 95 % CI 0.35–0.88; I 2 = 0 %.) in favour of IA (Fig. 8).
Fig. 8.
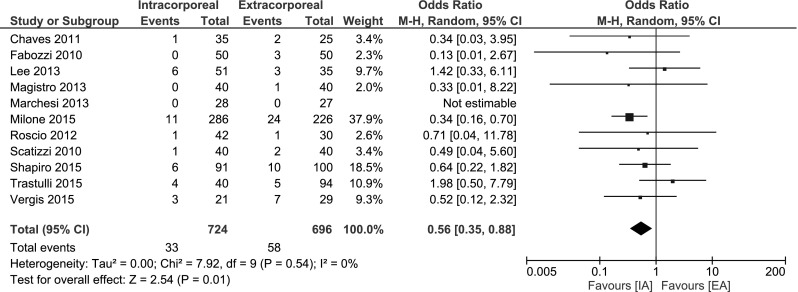
Surgical site infection
Incisional hernia
Five studies reported incisional hernia, see ‘Appendix’. No meta-analysis was performed since follow-up and extraction technique varied. For instance, all the hernia’s in the IA group by Shapiro (n = 2) and Chaves (n = 2) was observed in patients having had an extraction other than the routinely performed Pfannenstiel incision.
Return of bowel function
There was a variety in reporting on return of bowel function among included studies. Four studies [32, 33, 35, 36] showed significant earlier bowel movement in the IA group, and two different papers [14, 16] reported significant earlier first flatus pointing towards an sooner return of bowel function for IA. See ‘Appendix’.
Discussion
This systematic review comparing intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy shows that the intracorporeal technique is associated with significant decreased short-term morbidity and length of stay. No differences were observed for mortality, Ileus and anastomotic leakage. In a subgroup analysis of the more recent studies (2012≥), the observed differences were larger with less heterogeneity in favour of IA.
The observed decreased morbidity of the intracorporeal anastomosis technique seems largely related to the extraction site. By performing an IA, the incision for specimen extraction can be smaller and the incision can be performed in the lower part of the abdomen, which has shown to be associated with less pain, less pulmonary morbidity, a lower infection rate and on the long-term lower herniation rate [37, 38]. The suprapubic (Pfannenstiel) site for specimen extraction is the preferred extraction site since it has been reported to be associated with low site infections and with a low hernia rate of only 0–2 % [39]. Shapiro et al. [17] found such hernia rates in their series (IA 2.2 %, EA 17 %). The 2 hernia’s in the IA were not Pfannenstiel incisions but periumbilical and midline. Chaves et al. [33] report 2 versus 1 hernia in IA and EA, respectively. However, again these two cases in the IA-arm were not extracted by a Pfannenstiel incision, but a midline incision was chosen since both patients had a previous laparotomy. Furthermore, IA requires a smaller incision potentially leading to less post-operative pain [40] with a possible reduction in hospital costs [41], shorter hospital stay [4] and pulmonary dysfunction [8]. The observed decreased morbidity in the IA group might also be related to less mobilization of the transverse colon and less traction on the mesentery and pancreatico-duodenal block, theoretically resulting in surgical trauma and earlier restoration of bowel function [19, 35]. Especially, in obese patients, the mesentery is subject to substantial traction to externalize the bowel in EA [12, 25, 33, 42, 43].
Total mortality did not statistically differ. Short-term morbidity was significantly decreased in favour of IA. This advantage was even larger for the more recent studies as shown after subgroup analysis. The length of stay seems shorter; however, this was not significant. In addition, serious risk at heterogeneity was observed in the meta-analysis, so no conclusions can be made. However, subgroup analysis of the recent studies did reveal an significant decrease in LoS in favour of IA as is expected since the morbidity is less. See Fig. 5.
Incisional SSI was significantly decreased when an IA was performed. Some authors discussed that externalizing the bowel in EA requires more traction and tension of the wound resulting in more tissue trauma [26]. No significant differences in anastomotic leak and ileus rate were found. In contrast, using IA technique, the necessity for intraperitoneal tomies into the contaminated transversum and ileum could lead to a theoretical increase of intraabdominal infections. Chang et al. [44] described the use of atraumatic intracorporeal bulldogs to minimize faecal spillage when performing an IA. Since the included studies heterogeneously reported on intraabdominal abscesses and/or interventions, we cannot conclude that the IA has a significant influence on deep abdominal abscesses compared to standard EA.
Potential new techniques for extraction include transvaginal colectomy, a form of natural orifice specimen extraction (NOSE). This might even further decrease surgical trauma, although large cohort data and randomized evidence is lacking [45]. Nevertheless, small cohort series show promising results for partial colectomy with minor short-term morbidity and a shorter length of stay [45, 46]. For male, transgastric or transrectal extraction creates potential more surgical trauma, and a small Pfannenstiel is still considered as the best option. Currently, the available data are insufficient to make any statements regarding safety and efficacy of natural orifice transluminal endoscopic surgery (NOTES) for laparoscopic right hemicolectomy.
This systematic review and meta-analysis has several limitations. The included studies are merely observational, and the majority (n = 11 out of 12) was of retrospective design. Complications according to Clavien–Dindo classification were reported only in 25 % of the included studies. Studies focused merely on short-term outcomes and reported corresponding follow-up. As we foresee, a considerable reduction in the incidence of incisional hernia following IA technique, and longer follow-up (i.e. 2 years) would provide more insight [37].
Conclusion
This meta-analysis of non-randomized, comparative studies shows that intracorporeal anastomosis in laparoscopic right hemicolectomy is associated with reduced short-term morbidity and decreased length of hospital stay suggesting faster recovery. A randomized controlled trial is warranted to confirm these findings.
Appendix
See Tables 3, 4, 5, 6, 7 and 8.
Table 3.
PubMed search 21 December 2015
| PubMed search 21 December 2015 | N | |
|---|---|---|
| #1 | ‘Colectomy’[Mesh:NoExp] OR colectom*[tiab] OR hemicolectom*[tiab] OR colon resection*[tiab] OR colorectal resection*[tiab] OR large bowel resection*[tiab] | 21,875 |
| #2 | ‘Anastomosis, Surgical’[Mesh:NoExp] OR anastom*[tiab] | 80,578 |
| #3 | intracorpo*[tiab] OR intra-corpo*[tiab] OR intra-abdom*[tiab] OR intraabdom*[tiab] OR ICA[tiab] OR extracorpo*[tiab] OR extra-corpo*[tiab] OR extra-abdom*[tiab] OR extraabdom*[tiab] OR ECA[tiab] | 71,900 |
| #4 | ((‘Laparoscopy’[Mesh:NoExp] OR laparoscop*[tiab]) AND (total*[tiab] OR assisted[tiab])) | 24,110 |
| #5 | #2 AND #3 | 2756 |
| #6 | #4 or #5 | 26,407 |
| #7 | #1 AND #6 | 1990 |
Table 4.
Embase search 21 December 2015
| Embase search 21 December 2015 | N | |
|---|---|---|
| #1 | ‘colon resection’/de OR ’hemicolectomy’/exp OR colectom*:ab,ti OR hemicolectom*:ab,ti OR (colon NEAR/3 resection*):ab,ti OR (colorectal NEAR/3 resection*):ab,ti OR (‘large bowel’ NEAR/3 resection*):ab,ti | 42,437 |
| #2 | ‘anastomosis’/exp OR anastom*:ab,ti | 191,035 |
| #3 | intracorpo*:ab,ti OR (intra NEAR/3 corpo*):ab,ti OR (intra NEAR/3 abdom*):ab,ti OR intraabdom*:ab,ti OR ica:ab,ti OR extracorpo*:ab,ti OR (extra NEAR/3 corpo*):ab,ti OR (extra NEAR/3 abdom*):ab,ti OR extraabdom*:ab,ti OR eca:ab,ti | 93,326 |
| #4 | laparoscopy’/exp OR laparoscop*:ab,ti AND (total*:ab,ti OR assisted:ab,ti) | 39,455 |
| #5 | #2 AND #3 | 5822 |
| #6 | #4 OR #5 | 44,350 |
| #7 | #1 AND #6 | 3676 |
| #8 | #7 AND (‘article’/it OR ’article in press’/it OR ’conference paper’/it OR ’review’/it) | 2262 |
Table 5.
Duration of surgery
| Study (author, YoP) | Duration of surgery (min) | ||
|---|---|---|---|
| IA | EA | p | |
| Anania, 2012 | 186.8 (105–280)c | 184.1 (115–285)c | 0.6549 |
| Chaves, 2011 | 227 (44.5)a | 203 (36.4)a | NR |
| Fabozzi, 2010 | 78 (25)a | 92 (22)a | <0.05 |
| Lee, 2013 | 205 (132)a | 196 (56)a | NR |
| Magistro, 2013 | 230 (45)a | 203 (48)a | 0.011 |
| Marchesi, 2013 | 205.79 (45.77)a | 196.78 (22.95)a | 0.3952 |
| Milone, 2015 | 166.9 (10.7)a | 157.5 (67.2)a | 0.06 |
| Roscio, 2012 | 176.5 (40.0)a | 186.3 (40.1)a | 0.039 |
| Scatizzi, 2010 | 150 (115–180)b | 150 (105–245)b | 0.167 |
| Shapiro, 2015 | 155 (37)a | 142 (35)a | 0.006 |
| Trastulli, 2015 | 204.3 (51.9)a | 208 (61)a | NR |
| Vergis, 2015 | 170 (121–237)b | 181 (98–205)b | 0.78 |
Bold values are statistically significant (p < 0.05)
YoP year of publication, Min minutes, N number, NR not reported
aMean (SD), b median (range), c mean (range)
Table 6.
Incisional hernia
| Study (author, YoP) | Hernia n (%) |
||
|---|---|---|---|
| IA | EA | p | |
| Anania, 2012 | NR | NR | – |
| Chaves, 2011 | 2 (5.7) | 1 (4) | – |
| Fabozzi, 2010 | NR | NR | – |
| Lee, 2013 | 1 (1.9) | 3 (8.6) | – |
| Magistro, 2013 | NR | NR | – |
| Marchesi, 2013 | NR | NR | – |
| Milone, 2015 | NR | NR | – |
| Roscio, 2012 | 0 | 1 (3.3) | – |
| Scatizzi, 2010 | NR | NR | – |
| Shapiro, 2015 | 2 (2.2) | 17 (17.0) | 0.001 |
| Trastulli, 2015 | NR | NR | – |
| Vergis, 2015 | 0 | 6 (20.7) | 0.026 |
Bold values are statistically significant (p < 0.05)
YoP year of publication, N number, NR not reported
Table 7.
Return of bowel function
| Study (author, YoP) | Bowel movement (days) | First flatus (days) | ||||
|---|---|---|---|---|---|---|
| IA | EA | p | IA | EA | p | |
| Anania, 2012 | 3.8 (1.4)a | 4.9 (1.5)a | <0.0001 | NR | NR | – |
| Chaves, 2011 | 3 (2–8)b | 4 (2–8)b | 0.004 | NR | NR | – |
| Fabozzi, 2010 | 3.1 (1.2)a | 4.4 (1.6)a | NS | NR | NR | – |
| Lee, 2013 | NR | NR | – | NR | NR | – |
| Magistro, 2013 | 3.5 (1.1)a | 3.8 (1.1)a | 0.234 | 2.2 (0.6)a | 2.6 (0.8)a | 0.043 |
| Marchesi, 2013 | NR | NR | – | NR | NR | – |
| Milone, 2015 | NR | NR | – | 1.7 (1)a | 2.3 (0.8)a | <0.001 |
| Roscio, 2012 | 2.9 (0.9)a | 3.4 (0.9)a | 0.023 | NR | NR | – |
| Scatizzi, 2010 | 0 (0–1)b | 1 (0–1)b | 0.043 | NR | NR | – |
| Shapiro, 2015 | NR | NR | – | NR | NR | – |
| Trastulli, 2015 | NR | NR | – | 4 (1–7)b | 3 (1–6)b | – |
| Vergis, 2015 | NR | NR | – | NR | NR | – |
Bold values are statistically significant (p < 0.05)
YoP year of publication, Min minutes, N number, NR not reported
aMean (SD), b median (range)
Table 8.
Incision length and tolerance to solid diet
| Study (author, YoP) | Incision length | Tolerance to solid diet (days) | ||||
|---|---|---|---|---|---|---|
| IA | EA | p | IA | EA | p | |
| Anania, 2012 | NR | NR | – | 4.6 (2.1)a | 5.7 (1.7)a | <0.0001 |
| Chaves, 2011 | NR | NR | – | 1 (1–9)b | 2 (1–10)b | 0.002 |
| Fabozzi, 2010 | 6.0 (1)a | 12.0 (2)a | <0.05 | NR | NR | – |
| Lee, 2013 | NR | NR | – | NR | NR | – |
| Magistro, 2013 | 5.5 (1.1)a | 7.2 (1.3)a | 0.01 | NR | NR | – |
| Marchesi, 2013 | 4.8 (0.9)a | 7.2 (1.1)a | 0.02 | NR | NR | – |
| Milone, 2015 | NR | NR | – | NR | NR | – |
| Roscio, 2012 | NR | NR | – | NR | NR | – |
| Scatizzi, 2010 | 4.0 (3.0–7.0)b | 5.0 (3.0–7.0)b | 0.019 | 1 (1–8)b | 2 (1–12)b | 0.025 |
| Shapiro, 2015 | NR | NR | – | NR | NR | – |
| Trastulli, 2015 | NR | NR | – | NR | NR | – |
| Vergis, 2015 | NR | NR | – | 2.34a | 3.21a | 0.023 |
Bold values are statistically significant (p < 0.05)
YoP year of publication, Min minutes, N number, NR not reported
aMean (SD), b median (range)
Compliance with ethical standards
Disclosures
Stefan van Oostendorp, Arthur Elfrink, Wernard Borstlap, Linda Schoonmade, Colin Sietses, Jeroen Meijerink and Jurriaan Tuynman declare that they have no conflict of interest.
References
- 1.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. EurJCancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.Van Leersum NJ, Snijders HS, Henneman D, Kolfschoten NE, Gooiker GA, ten Berge MG, Eddes EH, Wouters MW, Tollenaar RA, Bemelman WA, Van Dam RM, Elferink MA, Karsten TM, Van Krieken JH, Lemmens VE, Rutten HJ, Manusama ER, van de Velde CJ, Meijerink WJ, Wiggers T, Van Der Harst E, Dekker JW, Boerma D. The Dutch surgical colorectal audit. Eur J Surg Oncol. 2013;39:1063–1070. doi: 10.1016/j.ejso.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Schwenk W, Haase O, Neudecker J, Muller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;20:CD00314. doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AAW, Sprangers MAG, Cuesta MA, Bemelman WA. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study) Ann Surg. 2011;254:868–875. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP, Dutton SJ. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32:1804–1811. doi: 10.1200/JCO.2013.54.3694. [DOI] [PubMed] [Google Scholar]
- 7.Bergamaschi R, Schochet E, Haughn C, Burke M, Reed JF, Arnaud JP. Standardized laparoscopic intracorporeal right colectomy for cancer: short-term outcome in 111 unselected patients. Dis Colon Rectum. 2008;51:1350–1355. doi: 10.1007/s10350-008-9341-1. [DOI] [PubMed] [Google Scholar]
- 8.Barnett RB, Clement GS, Drizin GS, Josselson AS, Prince DS. Pulmonary changes after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1992;2:125–127. doi: 10.1097/00129689-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS. 2009;13:312–317. [PMC free article] [PubMed] [Google Scholar]
- 10.Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008;143:762–767. doi: 10.1001/archsurg.143.8.762. [DOI] [PubMed] [Google Scholar]
- 11.Cirocchi R, Trastulli S, Farinella E, Guarino S, Desiderio J, Boselli C, Parisi A, Noya G, Slim K. Intracorporeal versus extracorporeal anastomosis during laparoscopic right hemicolectomy—systematic review and meta-analysis. Surg Oncol. 2013;22:1–13. doi: 10.1016/j.suronc.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Carnuccio P, Jimeno J, Pares D. Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol. 2014;18:5–12. doi: 10.1007/s10151-013-1029-4. [DOI] [PubMed] [Google Scholar]
- 13.Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A. Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc. 2013;27:1986–1990. doi: 10.1007/s00464-012-2698-1. [DOI] [PubMed] [Google Scholar]
- 14.Magistro C, Lernia SD, Ferrari G, Zullino A, Mazzola M, De Martini P, De Carli S, Forgione A, Bertoglio CL, Pugliese R. Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term outcomes? A prospective comparative assessment in our center. Surg Endosc. 2013;27:2613–2618. doi: 10.1007/s00464-013-2799-5. [DOI] [PubMed] [Google Scholar]
- 15.Marchesi F, Pinna F, Percalli L, Cecchini S, Ricco M, Costi R, Pattonieri V, Roncoroni L. Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech A. 2013;23:418–424. doi: 10.1089/lap.2012.0420. [DOI] [PubMed] [Google Scholar]
- 16.Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP, Napolitano C, Angiolini MR, Bracale U, Clemente M, D’Ambra M, Luglio G, Musella M, Pace U, Rosati R, Milone F. Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc. 2015;29:2314–2320. doi: 10.1007/s00464-014-3950-7. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D (2015) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc. doi:10.1007/s00464-015-4684-x [DOI] [PubMed]
- 18.Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, Di Marino M, Ricci F, Desiderio J, Cirocchi R, Parisi A. Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc. 2015;29:1512–1521. doi: 10.1007/s00464-014-3835-9. [DOI] [PubMed] [Google Scholar]
- 19.Vergis AS, Steigerwald SN, Bhojani FD, Sullivan PA, Hardy KM. Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastamosis: a comparison of short-term outcomes. Can J Surg. 2015;58:63–68. doi: 10.1503/cjs.001914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 21.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZJSurg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 22.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 23.Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi M. Intracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2013;28:1177–1186. doi: 10.1007/s00384-013-1651-7. [DOI] [PubMed] [Google Scholar]
- 24.Tarta C, Bishawi M, Bergamaschi R. Intracorporeal ileocolic anastomosis: a review. Tech Coloproctol. 2013;17:479–485. doi: 10.1007/s10151-013-0998-7. [DOI] [PubMed] [Google Scholar]
- 25.Stein SA, Bergamaschi R. Extracorporeal versus intracorporeal ileocolic anastomosis. Tech Coloproctol. 2013;17(Suppl 1):S35–S39. doi: 10.1007/s10151-012-0937-z. [DOI] [PubMed] [Google Scholar]
- 26.Grams J, Tong W, Greenstein AJ, Salky B. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc. 2010;24:1886–1891. doi: 10.1007/s00464-009-0865-9. [DOI] [PubMed] [Google Scholar]
- 27.Abrisqueta J, Ibanez N, Lujan J, Hernandez Q, Parrilla P. Intracorporeal ileocolic anastomosis in patients with laparoscopic right hemicolectomy. Surg Endosc. 2016;30(1):65–72. doi: 10.1007/s00464-015-4162-5. [DOI] [PubMed] [Google Scholar]
- 28.Iorio T, Blumberg D. A case-control study examining the benefits of laparoscopic colectomy using a totally intracorporeal technique for left-sided colon tumors. Surg Laparosc Endosc Percutan Tech. 2014;24:381–384. doi: 10.1097/SLE.0b013e318290155b. [DOI] [PubMed] [Google Scholar]
- 29.Franklin ME, Jr, Gonzalez JJJ, Miter DB, Mansur JH, Trevino JM, Glass JL, Mancilla G, Abrego-Medina D. Laparoscopic right hemicolectomy for cancer: 11-year experience. Rev Gastroenterol Mex. 2004;69(Suppl 1):65–72. [PubMed] [Google Scholar]
- 30.Feroci F, Lenzi E, Kroning KC, Moraldi L, Cantafio S, Borrelli A, Giaconi G, Scatizzi M. Feasibility and effectiveness of laparoscopic right colectomy with extracorporeal anastomosis. Minerva Chir. 2011;66:41–48. [PubMed] [Google Scholar]
- 31.Moghadamyeghaneh Z, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ. Hand-assisted laparoscopic approach in colon surgery. J Gastrointest Surg. 2015;19:2045–2053. doi: 10.1007/s11605-015-2924-y. [DOI] [PubMed] [Google Scholar]
- 32.Anania G, Santini M, Scagliarini L, Marzetti A, Vedana L, Marino S, Gregorio C, Resta G, Cavallesco G. A totally mini-invasive approach for colorectal laparoscopic surgery. World J Gastroenterol. 2012;18:3869–3874. doi: 10.3748/wjg.v18.i29.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaves JA, Idoate CP, Fons JB, Oliver MB, Rodriguez NP, Delgado AB, Lizoain JLH. A case–control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy. Cir Esp. 2011;89:24–30. doi: 10.1016/j.ciresp.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Fabozzi M, Allieta R, Brachet Contul R, Grivon M, Millo P, Lale-Murix E, Nardi M., Jr Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24:2085–2091. doi: 10.1007/s00464-010-0902-8. [DOI] [PubMed] [Google Scholar]
- 35.Roscio F, Bertoglio C, De Luca A, Frattini P, Scandroglio I. Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int J Surg. 2012;10:290–295. doi: 10.1016/j.ijsu.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 36.Scatizzi M, Kroning KC, Borrelli A, Andan G, Lenzi E, Feroci F. Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg. 2010;34:2902–2908. doi: 10.1007/s00268-010-0743-6. [DOI] [PubMed] [Google Scholar]
- 37.Singh R, Omiccioli A, Hegge S, McKinley C. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc. 2008;22:2596–2600. doi: 10.1007/s00464-008-9845-8. [DOI] [PubMed] [Google Scholar]
- 38.Winslow ER, Fleshman JW, Birnbaum EH, Brunt LM. Wound complications of laparoscopic vs open colectomy. Surg Endosc. 2002;16:1420–1425. doi: 10.1007/s00464-002-8837-3. [DOI] [PubMed] [Google Scholar]
- 39.Kisielinski K, Conze J, Murken AH, Lenzen NN, Klinge U, Schumpelick V. The Pfannenstiel or so called “bikini cut”: still effective more than 100 years after first description. Hernia. 2004;8:177–181. doi: 10.1007/s10029-004-0210-0. [DOI] [PubMed] [Google Scholar]
- 40.Leung AL, Cheung HY, Fok BK, Chung CC, Li MK, Tang CN. Prospective randomized trial of hybrid NOTES colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors. World J Surg. 2013;37:2678–2682. doi: 10.1007/s00268-013-2163-x. [DOI] [PubMed] [Google Scholar]
- 41.Jenks PJ, Laurent M, McQuarry S, Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. J Hosp Infect. 2014;86:24–33. doi: 10.1016/j.jhin.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 42.Blumberg D. Laparoscopic colectomy performed using a completely intracorporeal technique is associated with similar outcome in obese and thin patients. Surg Laparosc Endosc Percutan Tech. 2009;19:57–61. doi: 10.1097/SLE.0b013e318193c780. [DOI] [PubMed] [Google Scholar]
- 43.Lechaux D. Intra-corporeal anastomosis in laparoscopic right hemicolectomy. J Chir (Paris) 2005;142:102–104. doi: 10.1016/S0021-7697(05)80859-2. [DOI] [PubMed] [Google Scholar]
- 44.Chang K, Fakhoury M, Barnajian M, Tarta C, Bergamaschi R. Laparoscopic right colon resection with intracorporeal anastomosis. Surg Endosc. 2013;27:1730–1736. doi: 10.1007/s00464-012-2665-x. [DOI] [PubMed] [Google Scholar]
- 45.Kayaalp C, Yagci MA. Laparoscopic right colon resection with transvaginal extraction: a systematic review of 90 cases. Surg Laparosc Endosc Percutan Tech. 2015;25:384–391. doi: 10.1097/SLE.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 46.Wolthuis AM, de Buck van Overstraeten A, D’Hoore A. Laparoscopic natural orifice specimen extraction-colectomy: a systematic review. World J Gastroenterol. 2014;20:12981–12992. doi: 10.3748/wjg.v20.i36.12981. [DOI] [PMC free article] [PubMed] [Google Scholar]