Abstract
Objective Left ventricular outflow tract (LVOT) obstruction is a complication in 15-25% of patients with Takotsubo cardiomyopathy and sometimes leads to catastrophic outcomes, such as cardiogenic shock or cardiac rupture. However, the underlying mechanisms have not been clarified.
Methods and Results We experienced 22 cases of Takotsubo cardiomyopathy during 3 years, and 4 of these 22 cases were complicated with LVOT obstruction in the acute phase (mean age 79±5 years, 1 man, 21 women). The LVOT pressure gradient in the acute phase was 100±17 mmHg. Transthoracic echocardiogram (TTE) revealed left ventricular hypertrophy (LVH) in one case and sigmoid-shaped septum without LVH in three cases. The complete resolution of the LVOT obstruction was achieved in a few days with normalization of the left ventricular wall motion following administration of beta-blockers. A dobutamine provocation test after normalization of the left ventricular wall motion reproduced the LVOT obstruction in all cases and revealed the presence of latent LVOT obstruction.
Conclusion The manifestation of latent LVOT obstruction in the acute phase of Takotsubo cardiomyopathy is one potential reason for the complication of LVOT obstruction with Takotsubo cardiomyopathy.
Keywords: latent left ventricular outflow tract obstruction, Takotsubo cardiomyopathy, sigmoid-shaped septum, dobutamine
Introduction
Takotsubo cardiomyopathy is an important disorder in the differential diagnosis of acute myocardial infarction (AMI) (1). This disorder usually occurs in postmenopausal women of an advanced age and is characterized by transient left ventricular apical wall motion abnormalities associated with emotional or physical stress. Typically, left ventricular apical wall motion abnormalities are transient and resolve over a period of days to weeks. However, several acute complications have been reported, such as congestive heart failure, cardiac rupture, hypotension, left ventricular apical thrombosis, Torsade de Pointes, and transient left ventricular outflow tract (LVOT) obstruction. The mechanisms and features of the appearance of LVOT obstruction in the early phase of Takotsubo cardiomyopathy remain unclear. We herein report four cases of LVOT obstruction in the acute phase of Takotsubo cardiomyopathy that recurred with dobutamine (DOB) provocation in the chronic phase. We also considered the mechanisms and features of LVOT obstruction in Takotsubo cardiomyopathy based on these four cases.
Materials and Methods
We encountered 22 patients with Takotsubo cardiomyopathy from January 2010 to December 2012 in Niigata City General Hospital. Takotsubo cardiomyopathy was diagnosed by transthoracic echocardiogram (TTE) and cardiac catheterization in the acute phase. Of these 22 cases, 4 were complicated with LVOT obstruction in the acute phase. We evaluated the features of the TTE findings in these four cases and performed a DOB provocation test after achieving normalization of the left ventricular wall motion. The method for measuring the aorto-septal angle was described previously (2). The features of these four cases are described in Table.
Table.
The Features of Four Takotsubo Cardiomyopathy Cases Complicated with Left Ventricular Outflow Tract Obstruction in the Acute Phase.
| Case | Age (y.o.) |
Sex | LVOT-PG at admission (mmHg) |
TTE after normalization of LV wall motion | LVOT-PG provoked by DOB (mmHg) |
Beta blockers |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| LVDd (mm) |
EF (%) |
AS angle (° ) |
Sigmoid | LVH | ||||||
| 1 | 75 | F | 157 | 47 | 70 | 84 | Y | N | 80 | Metoprolol 60 mg/day |
| 2 | 76 | M | 100 | 38 | 74 | 82 | Y | N | 121 | Atenolol 50 mg/day |
| 3 | 85 | F | 90 | 40 | 65 | 55 | Y | N | 100 | Metoprolol 40 mg/day |
| 4 | 79 | F | 111 | 37 | 81 | 128 | N | Y | 100 | Carvedilol 10 mg/day |
M: male, F: female, LVOT-PG: pressure gradient at left ventricular outflow tract, TTE: transthoracic echocardiogram, LVDd: LV diastolic dimension, EF: ejection fruction, AS angle: aorto-septal angle, Sigmoid: sigmoid-shaped septum, LVH: left ventricular hypertrophy, Y: yes, N: no, DOB: dobutamine
Case Reports
Case 1
A 75-year-old woman with hypertension (HT) was admitted to our hospital for chest pain with cold sweating. Her blood pressure (BP) was 70/40 mmHg, and her heart rate (HR) was 68 beats/min. A grade 3/6 ejection systolic murmur (ESM) was detected at the apex. Electrocardiogram (ECG) revealed sinus rhythm (60 beats/min) and ST elevation in V3-6, I, and aVL. TTE showed anterior-apical hypokinesis and basal hyperkinesis, a sigmoid-shaped septum, systolic anterior movement of the mitral valve (SAM), moderate mitral regurgitation (MR), and a peak Doppler velocity of 6.3 m/sec, corresponding to a peak pressure gradient (PG) of 157 mmHg across the LVOT. Emergent coronary angiography (CAG) revealed normal coronary findings. Left ventriculography (LVG) demonstrated anterior-apical akinesia, posterobasal hypercontractility with an ejection fraction (EF) of 70%, and a moderate level of MR (Fig. 1A). From the findings of TTE and cardiac catheterization, she was diagnosed with Takotsubo cardiomyopathy. The BP increased after intravenous administration of disopyramide 50 mg and propranolol 2 mg during cardiac catheterization (Fig. 1B). She was then treated with metoprolol (60 mg/day), and the LVOT obstruction disappeared thereafter. Five days later, TTE revealed normalization of the LV wall motion, an EF of 70%, and a sigmoid-shaped septum with an aorto-septal angle of 84° (Fig. 1C). No left ventricular hypertrophy (LVH) was noted. After 2 weeks, cardiac catheterization was performed again. LVG revealed normal LV wall motion, and vasospasm was not induced by an ergonovine maleate provocation test. No PG was noted between the left ventricular apex (LVA) and the ascending aorta (AAo). After the intravenous infusion of DOB (15 μg/kg/min), the PG of the LVOT increased to 80 mmHg (Fig. 1D). Thereafter, she continued to take metoprolol for latent LVOT obstruction.
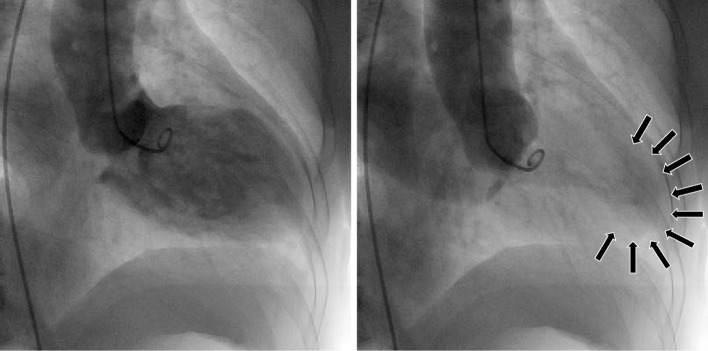
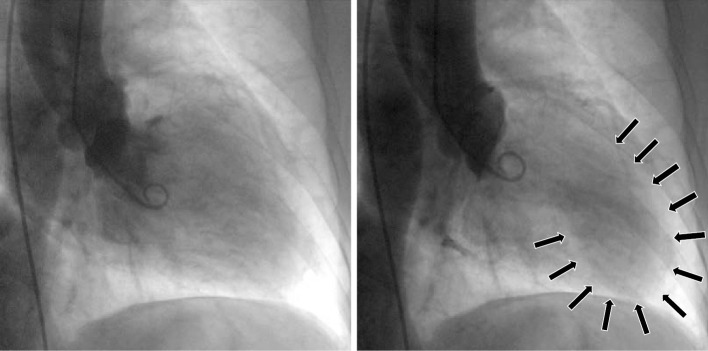
Figure 1A.
The LVG findings of the RAO view in Case 1. The LVG findings, in diastole (left) and systole (right), revealed anterior-apical akinesia (arrows in right), hypercontractility of other regions, and moderate MR.
Figure 1B.
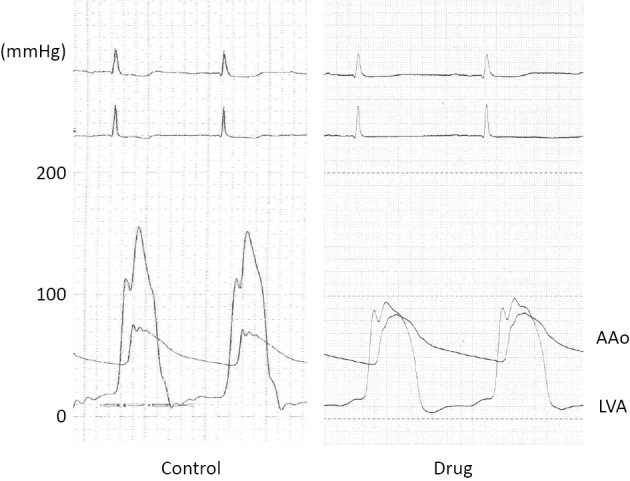
The findings for the LVA and AAo pressure before (left) and after (right) administration of disopyramide 50 mg and propranolol 2 mg during emergent cardiac catheterization in Case 1. Disopyramide and propranolol increased the systolic BP by 15 mmHg and decreased the PG between the LVA and AAo from 80 to 10 mmHg.
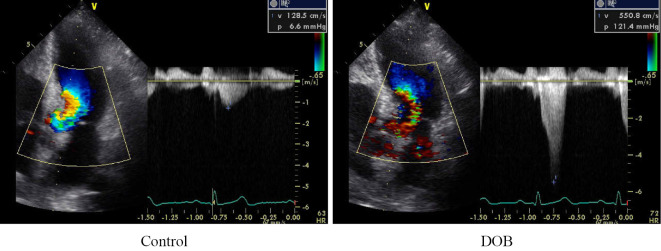
Figure 1C.
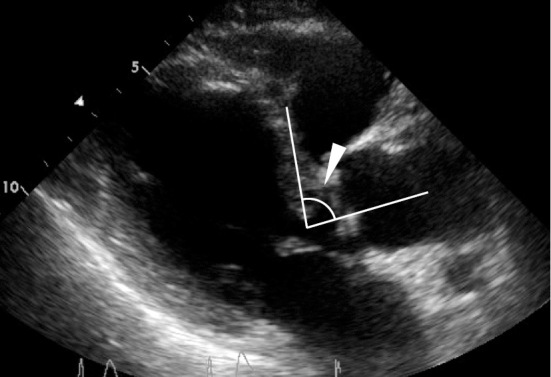
The TTE findings after normalization of the LV wall motion in Case 1. The parasternal long-axis view showed a sigmoid-shaped septum with a diminished AS angle of 84° (white arrowhead). No LVH was noted.
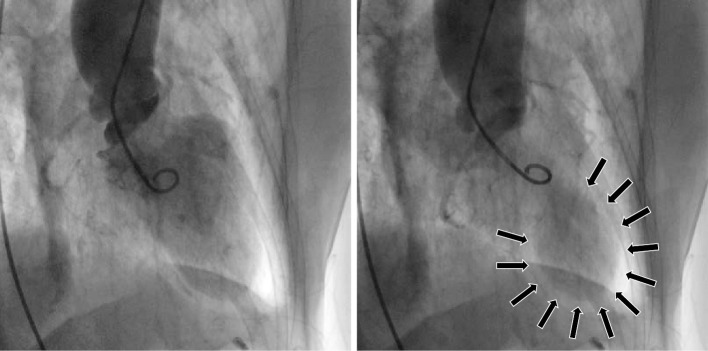
Figure 1D.
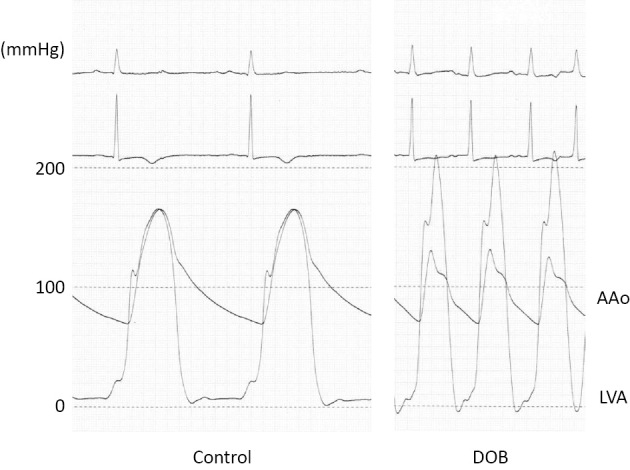
The findings of the LVA and AAo pressure before (left) and after (right) the DOB infusion in Case 1. The DOB infusion provoked a 80 mmHg PG between the LVA and the AAo.
Case 2
A 76-year-old man was admitted to our hospital for severe chest pain. He was undergoing HT treatment. His BP and HR were 106/58 mmHg and 90 beats/min, respectively. A grade 2/6 ESM was detected by chest auscultation. ECG revealed sinus rhythm (110 beats/min) and ST elevation in V3-6, II, III, and aVF, with T wave inversion in V3-6. TTE revealed apical akinesis with basal hyperkinesis, a sigmoid-shaped septum and a PG of 100 mmHg across the LVOT. LVH was not evident. Emergent CAG revealed normal coronary artery. LVG demonstrated anterior-apical-diaphragmatic akinesia with anterobasal and posterobasal hypercontractility with an EF of 47% and moderate MR (Fig. 2A). From these findings, he was diagnosed with Takotsubo cardiomyopathy. During the cardiac catheterization, the patient entered a shock state. Intravenous administration of disopyramide 50 mg and propranolol 2 mg decreased his LVOT-PG from 100 to 20 mmHg and restored his BP. He was treated with atenolol (50 mg/day), and the LVOT obstruction disappeared within a few days. Seven days later, TTE revealed normalization of the LV wall motion, an EF of 74%, and a sigmoid-shaped septum with an aorto-septal angle of 82° (Fig. 2B). No LVH was noted. After 6 months, DOB stress TTE was performed. The patient had a PG of 7 mmHg at the LVOT without DOB, and intravenous infusion of DOB (15 μg/kg/min) provoked a PG of 121 mmHg (Fig. 2C). He was diagnosed with latent LVOT obstruction and continued to take atenolol.
Figure 2A.
The LVG findings of the RAO view in Case 2. The LVG findings, in diastole (left) and systole (right), revealed anterior-apical-diaphragmatic akinesia (arrows in right) with anterobasal and posterobasal hypercontractility and moderate MR.
Figure 2B.
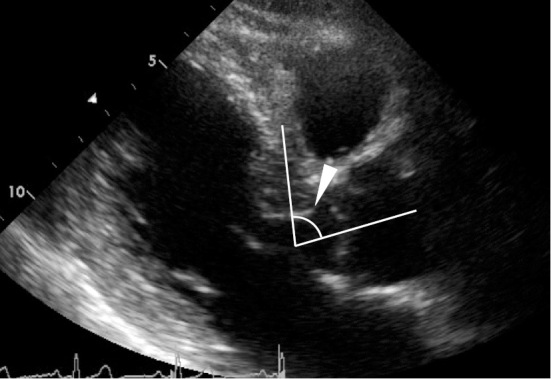
The TTE findings after normalization of the LV wall motion in Case 2. The parasternal long-axis view showed a sigmoid-shaped septum with a diminished AS angle of 82° (white arrowhead). No LVH was noted.
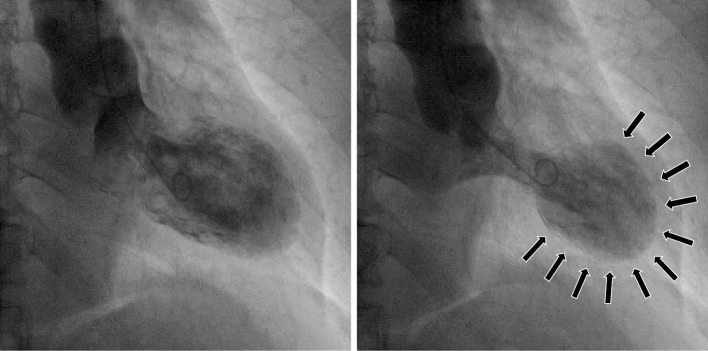
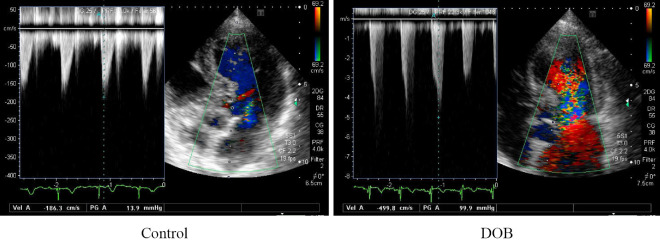
Figure 2C.
The findings of DOB stress TTE in Case 2, control (left) and DOB stress (right). DOB infusion (15 µg/kg/min) provoked a 121 mmHg PG at the LVOT.
Case 3
An 85-year-old woman was admitted to our hospital after experiencing severe epigastralgia while sleeping. Her BP and HR were 104/60 mmHg and 90 beats/min, respectively. Chest examination revealed a grade 3/6 ESM, and the point of maximum intensity was the apex. ECG showed sinus rhythm (90 beats/min), ST elevation in V3-6, II, III, and aVF, and T wave inversion in I and aVL. TTE revealed LV wall motion typical of Takotsubo cardiomyopathy, a sigmoid-shaped septum, SAM, moderate MR, and a PG of 90 mmHg across the LVOT. Emergent CAG revealed only a moderate stenotic lesion of the distal left circumflex artery. LVG demonstrated anterior-apical-diaphragmatic akinesia with anterobasal and posterobasal hypercontractility, an EF of 51%, and a moderate level of MR (Fig. 3A). From the TTE and cardiac catheterization findings, she was diagnosed Takotsubo cardiomyopathy. She was treated with metoprolol (40 mg/day), and the LVOT obstruction disappeared within 4 days. After 1 week, TTE revealed normalization of the LV wall motion, an EF of 65%, and a sigmoid-shaped septum with an aorto-septal angle of 55° (Fig. 3B). No LVH was noted. She was discharged a few days later.
Figure 3A.
The LVG findings of the RAO view in Case 3. LVG findings, in diastole (left) and systole (right), revealed anterior-apical-diaphragmatic akinesia (arrows in right) with anterobasal and posterobasal hypercontractility and moderate MR.
Figure 3B.
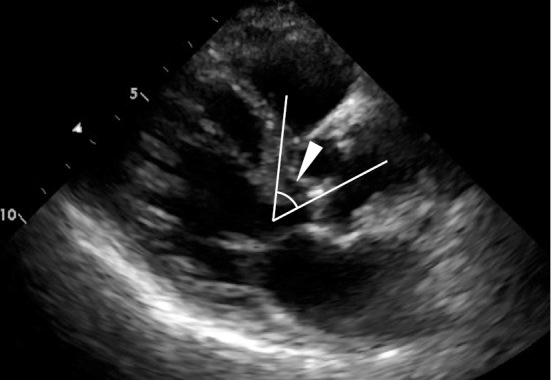
The TTE findings after normalization of the LV wall motion in Case 3. The parasternal long-axis view showed a sigmoid-shaped septum with a diminished AS angle of 55° (white arrowhead). No LVH was noted.
After 6 months, she visited our hospital again for recurrence of Takotsubo cardiomyopathy after falling down, despite the administration of metoprolol. TTE revealed LVOT obstruction with a PG of 56 mmHg. After normalization of the LV wall motion and resolution of the LVOT obstruction, DOB stress TTE was performed. The patient had a PG of 14 mmHg at the LVOT without DOB, and intravenous infusion of DOB (5 μg/kg/min) provoked a PG of 100 mmHg (Fig. 3C). She was diagnosed with latent LVOT obstruction and continued to take metoprolol.
Figure 3C.
The findings of DOB stress TTE in Case 3, control (left) and DOB stress (right). The DOB infusion (5 µg/kg/min) provoked a 100 mmHg PG at the LVOT.
Case 4
A 79-year-old woman visited our hospital for continuous chest discomfort. Her BP and HR were 132/90 mmHg and 95 beats/min, respectively. A grade 3/6 ESM was detected at the apex. ECG revealed sinus rhythm (95 beats/min) and ST elevation in V2-6, I, and aVL. TTE revealed apical akinesis with basal hyperkinesis, concentric LVH, and a PG of 111 mmHg across the LVOT. The findings of emergency CAG were normal, and LVG demonstrated anterior-apical akinesia with anterobasal and posterobasal hyperkinesia, an EF of 41%, and mild MR (Fig. 4A). She was diagnosed with Takotsubo cardiomyopathy based upon the TTE and cardiac catheterization findings. She was treated with carvedilol (10 mg/day), and the LVOT obstruction disappeared after 1 week. TTE revealed normalization of the LV wall motion and concentric LVH (diameters of the intraventricular septum and posterior wall were 14 mm and 13 mm, respectively) (Fig. 4B). Her EF was 81%. No sigmoid-shaped septum was detected (aorto-septal angle of 128°). After 10 days, cardiac catheterization was performed again. LVG revealed normal LV wall motion, and vasospasm was not induced by the ergonovine maleate provocation test. There was no PG between the LVA and AAo. The intravenous infusion of DOB (5 μg/kg/min) increased the PG of the LVOT to 100 mmHg (Fig. 4C). Thereafter, she continued to take carvedilol for the latent LVOT obstruction. After 5 years, the LVOT obstruction worsened, and permenent pacemaker implantation was required to resolve the LVOT obstruction.
Figure 4A.
The LVG findings of the RAO view in Case 4. The LVG findings, in diastole (left) and systole (right), revealed anterior-apical-diaphragmatic akinesia (arrows in right) with anterobasal and posterobasal hypercontractility and mild MR.
Figure 4B.
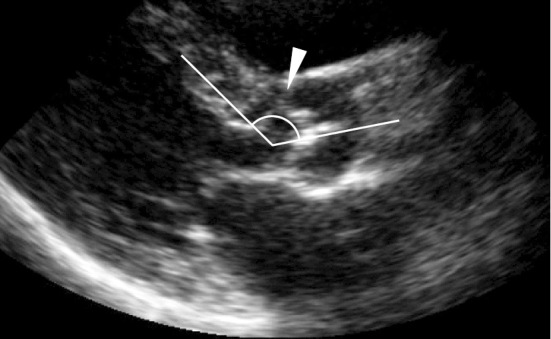
The TTE findings after normalization of the LV wall motion in Case 4. The parasternal long-axis view showed a concentric LVH (diameters of the intraventricular septum and posterior wall were 14 mm and 13 mm, respectively). The AS angle was 128° (white arrowhead), and no sigmoid-shaped septum was evident.
Figure 4C.
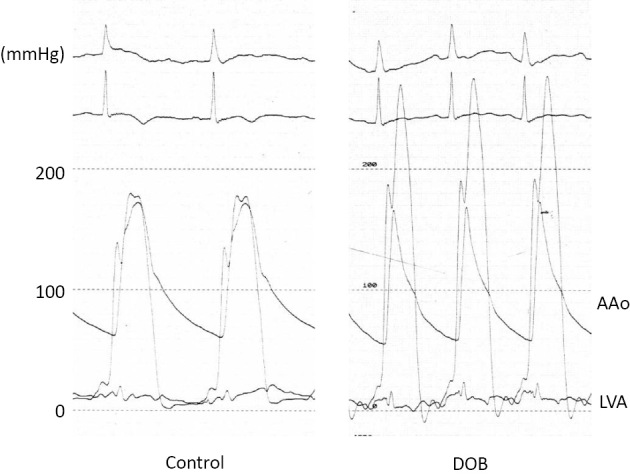
The findings of the LVA and AAo pressure before (left) and after (right) the DOB infusion in Case 4. The DOB infusion provoked a 100 mmHg PG between the LVA and the AAo.
Discussion
We herein report four cases of transient LVOT obstruction in the acute phase of Takotsubo cardiomyopathy. The complication rate of LVOT obstruction in the early phase of Takotsubo cardiomyopathy has been reported to be 15-25% in previous studies (3-5). At our institute, LVOT obstruction occurred in 18% of all Takotsubo cardiomyopathy patients during the acute phase over the past 3 years (Table). Some reports have revealed that the complication of LVOT obstruction with Takotsubo cardiomyopathy sometimes leads to catastrophic outcomes, such as cardiogenic shock (5), as in our Cases 1 and 2, or cardiac rupture (6). ESM was noted with chest auscultation in all four cases in this study, and the complication of LVOT obstruction with Takotsubo cardiomyopathy was diagnosed by TTE. When Takotsubo cardiomyopathy is diagnosed in the emergency room, chest examination is important for clarifying the complication of LVOT obstruction.
The LV wall motion in the acute phase of Takotsubo cardiomyopathy is characterized by akinesis in the apical and mid portions of the LV chamber extending beyond one coronary artery region with hyperkinesis in the basal portion (1). This basal hyperkinesis narrows the systolic LVOT, resulting in the acceleration of blood flow through the LVOT and thereby promoting the Venturi effect and SAM, increasing the LVOT obstruction. This might be one of the most important factors causing LVOT obstruction in Takotsubo cardiomyopathy (7). This mechanism is similar to the cases of LVOT obstruction observed in the acute phase of anteroseptal AMI. Several reports have cited LVOT obstruction with AMI (8-11). One-vessel disease of the left anterior descending artery and maintenance of the major septal branch blood flow are both important factors with respect to the manifestation of latent LVOT obstruction with anteroseptal AMI (11). These factors can induce anteroseptal and apical akinesis with compensatory hyperdynamic contraction of the residual normally-perfused basal segments; this compensatory basal hyperkinesis then narrows the systolic LVOT, resulting in the acceleration of blood flow through the LVOT.
After normalization of the LV wall motion, DOB infusion revealed marked LVOT obstruction in all cases (Table and Fig. 1D, 2C, 3C, 4C). LVOT obstruction is induced by exercise or DOB provocation in patients with latent LVOT obstruction who do not exhibit LVOT obstruction at rest (12). We previously reported two cases of latent LVOT obstruction complicated with anteroseptal AMI, in which DOB provocation led to LVOT obstruction one year after the onset of AMI without LVOT obstruction (11). Similarly, the above-mentioned four cases were thought to exhibit latent LVOT obstruction, and the occurrence of Takotsubo cardiomyopathy manifested as LVOT obstruction in the acute phase.
Although the present study describes 4 cases of LVOT obstruction among 22 cases of Takotsubo cardiomyopathy during 3 years, it is notable that all 4 of these cases had latent LVOT obstruction. In Case 4, TTE revealed concentric LVH (Fig. 4B), which was considered to be the cause of the latent LVOT obstruction. Although no significant LVH was observed in Cases 1, 2, or 3 (Fig. 1C, 2B, 3B), a sigmoid-shaped septum they all had a low aorto-septal angle (Table). The average aorto-septal angle was smaller in the patients with a sigmoid-shaped septum than in normal controls, 93°±14° vs. 145°±7°, respectively (2). DOB induced dynamic LVOT obstruction in the sigmoid-shaped septum patients with latent LVOT obstruction (13) and provoked LVOT PG, which correlated inversely with the aorto-septal angle in the patients with latent LVOT obstruction (14). A sigmoid-shaped septum is generally considered to be a normal part of the aging process and does not necessarily have any clinical importance (15,16). However, several reports have demonstrated the clinical importance of a sigmoid-shaped septum as a potential cause of LVOT obstruction (13,17-21). The sigmoid-shaped septum in Cases 1, 2, and 3 may be closely associated with the cause of latent LVOT obstruction. Patients with Takotsubo cardiomyopathy complicated by LVOT obstruction have been generally described as older and presenting with a septal bulge, both of which are features of a sigmoid-shaped septum (5).
After the diagnosis of Takotsubo cardiomyopathy complicated by LVOT obstruction, each of these four cases underwent treatment with beta-blockers, which improved the LVOT obstruction within a few days. In Cases 1 and 2, we chose to administer beta-blockers despite the patient being in a shock state in the acute phase, which led to their recovery from the shock state. Beta-blockers have been shown to exhibit hemodynamic effectiveness in Takotsubo cardiomyopathy with dynamic LVOT obstruction (4,22,23). Furthermore, the effectiveness of beta-blockers to relieve LVOT obstruction with HCM is well known, and their effectiveness in reducing LVOT PG due to a sigmoid-shaped septum has been reported (19,21). Catecholamine administration and intra-aortic balloon pumping should be avoided in patients in a shock state with LVOT obstruction, due to the risk of worsening the LVOT obstruction and inducing hypotension (8). Therefore, beta-blocker administration is the first-line medication for patients with Takotsubo cardiomyopathy complicated by LVOT obstruction.
These four cases demonstrate that the occurrence of Takotsubo cardiomyopathy may manifest latent LVOT obstruction, one potential mechanism explaining the complication of LVOT obstruction with Takotsubo cardiomyopathy. This study includes 4 cases of complicated LVOT obstruction in 22 cases of Takotsubo cardiomyopathy during 3 years. Of particular note: all four of these cases had latent LVOT obstruction.
Limitations
One limitation associated with the present study is the small sample size. This study was conducted in a relatively small number of affected individuals. More studies with larger sample sizes are needed to clarify the mechanism of LVOT obstruction with Takotsubo cardiomyopathy.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Kurisu S, Kihara Y. Tako-tsubo cardiomyopathy: clinical presentation and underlying mechanism. J Cardiol 60: 429-437, 2012. [DOI] [PubMed] [Google Scholar]
- 2. Nishida K, Saito T, Kamijima G, et al. . Echocardiographic findings of the “sigmoid septum” and its clinical implication. J Cardiogr 10: 873-879, 1980. [Google Scholar]
- 3. Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart 89: 1027-1031, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tsuchihashi K, Ueshima K, Uchida T, et al. ; , Angina Pectoris-Myocardial Infarction Investigations in Japan. . Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 38: 11-18, 2001. [DOI] [PubMed] [Google Scholar]
- 5. El Mahmoud R, Mansencal N, Pilliére R, et al. . Prevalence and characteristics of left ventricular outflow tract obstruction in Tako-Tsubo syndrome. Am Heart J 156: 543-548, 2008. [DOI] [PubMed] [Google Scholar]
- 6. Komuro K, Itoh T, Fusazaki T, et al. . A case of cardiac oozing rupture in patient with Takotsubo cardiomyopathy with left ventricular outflow tract stenosis. J Cardiol Jpn Ed 4: 78-82, 2009. (in Japanese). [Google Scholar]
- 7. Chockalingam A, Dorairajan S, Bhalla M, Dellsperger KC. Unexplained hypotension: the spectrum of dynamic left ventricular outflow tract obstruction in critical care settings. Crit Care Med 37: 729-734, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Chockalingam A, Tejwani L, Aggarwal K, Dellsperger KC. Dynamic left ventricular outflow tract obstruction in acute myocardial infarction with shock: cause, effect, and coincidence. Circulation 116: e110-e113, 2007. [DOI] [PubMed] [Google Scholar]
- 9. Ozaki K, Maeda C, Takayama T, et al. . Dynamic intraventricular obstruction in acute myocardial infarction with administration of cilostazol. Circ J 71: 608-612, 2007. [DOI] [PubMed] [Google Scholar]
- 10. Möller M, Völz J, Paliege R, et al. . Cardiogenic shock due to dynamic left ventricular outflow tract obstruction in acute myocardial infarction. Clin Res Cardiol 100: 621-625, 2011. [DOI] [PubMed] [Google Scholar]
- 11. Ozaki K, Okubo T, Yano T, et al. . Manifestation of latent left ventricular outflow tract obstruction caused by acute myocardial infarction: an important complication of acute myocardial infarction. J Cardiol 65: 514-518, 2015. [DOI] [PubMed] [Google Scholar]
- 12. Vaglio JC Jr, Ommen SR, Nishimura RA, Tajik AJ, Gersh BJ. Clinical characteristics and outcomes of patients with hypertrophic cardiomyopathy with latent obstruction. Am Heart J 156: 342-347, 2008. [DOI] [PubMed] [Google Scholar]
- 13. Tano A, Kasamaki Y, Okumura Y, et al. . Major determinants and possible mechanism of dobutamine-induced left ventricular outflow tract obstruction in patients with a sigmoid ventricular septum. J Cardiol 61: 428-435, 2013. [DOI] [PubMed] [Google Scholar]
- 14. Bolca O, Ozer N, Eren M, et al. . Dobutamine induced dynamic left ventricular outflow tract obstruction in patients with hypertrophic nonobstructive cardiomyopathy. Tohoku J Exp Med 198: 79-87, 2002. [DOI] [PubMed] [Google Scholar]
- 15. Goor D, Lillehei CW, Edwards JE. The ‘sigmoid septum’: variation in the contour of the left ventricular outlet. Am J Roentgenol 107: 366-376, 1969. [PubMed] [Google Scholar]
- 16. Toth AB, Engel JA, McManus AM, McManus BM. Sigmoidity of the ventricular septum revisited: progression in early adulthood, predominance in men, and independence from cardiac mass. Am J Cardiovasc Pathol 2: 211-223, 1988. [PubMed] [Google Scholar]
- 17. Iida K, Sugishita Y, Ajisaka R, et al. . Sigmoid septum causing left ventricular outflow tract obstruction: a case report. J Cardiogr 16: 237-247, 1986. [PubMed] [Google Scholar]
- 18. Konishi C, Shiraishi J, Muraguchi N, et al. . Benefical effect of cibenzoline on left ventricular pressure gradient with sigmoid septum. Circ J 68: 968-971, 2004. [DOI] [PubMed] [Google Scholar]
- 19. Fukuda N, Asai M, Tominaga T, et al. . Noninvasive studies of dynamic left ventricular outflow obstruction in patients with sigmoid septum. J Cardiogr 14: 445-457, 1984. [PubMed] [Google Scholar]
- 20. Sonoda M, Takenaka K, Watanabe F, et al. . Dobutamine stress causes left ventricular outflow tract obstruction. J Cardiol 27 Suppl 2: 45-48, 1996. [PubMed] [Google Scholar]
- 21. Ozaki K, Sakuma I, Mitsuma K, et al. . Effect of cibenzoline and atenolol administration od dynamic left ventricular obstruction due to sigmoid-shaped septum. Circ J 72: 2087-2091, 2008. [DOI] [PubMed] [Google Scholar]
- 22. Kyuma M, Tsuchihashi K, Shinshi Y, et al. . Effect of intravenous propranolol on left ventricular apical ballooning without coronary artery stenosis (ampulla cardiomyopathy): three cases. Circ J 66: 1181-1184, 2002. [DOI] [PubMed] [Google Scholar]
- 23. Yoshioka T, Hashimoto A, Tsuchihashi K, et al. . Clinical implications of midventricular obstruction and intravenous propranolol use in transient left ventricular apical ballooning (Tako-tsubo cardiomyopathy). Am Heart J 155: 526.e1-526.e17, 2008. [DOI] [PubMed] [Google Scholar]