Dear Editor, The hallmark of eczema is intense itch that can disturb all aspects of patients' lives. Sweating is one of the most commonly reported exacerbants of itch in eczema.1,2 Thus, patients with eczema may avoid exercise or vigorous physical activity, which are typically accompanied by increased sweating, in order to avoid worsening itch. If patients with eczema have a lower physical activity profile, they could potentially be at higher risk for obesity and cardiovascular disease. It is therefore important to understand the relationship between eczema and physical activity and to develop clinical interventions to improve the overall health of patients with eczema. We conducted a systematic review of the literature and meta-analysis to explore the relationship between eczema and vigorous physical activity.
We searched the following databases up to 11 March 2015: PubMed (1946 to present), Embase (1947 to present), Scopus (1823 to present), Global Resource for Eczema Trials (all years) and the Cochrane Library (1992 to present). The search strategy was based on a previous Cochrane review3 (Table S1). Studies were excluded based on the title and/or abstract if there was no clear indication that they were investigating physical activity in patients with eczema or if they were case series (i.e. there was no patient group without eczema). There were no relevant studies in foreign languages.
Both reviewers, A.K. and J.I.S., independently performed data extraction from these studies, and differences were resolved by discussion. The following data items collected were: first author name; year of publication; location; study design; how eczema was diagnosed; number of patients in study; level of physical activity; age range; and percentage of male subjects in the study. Two studies presented the total odds ratios (ORs) of eczema for the level of activity,4,5 but the frequencies were not presented, thereby precluding inclusion in the meta-analysis. Repeated attempts to obtain the data were made for all of these studies, although unsuccessfully. One study presented total group sizes for eczema classification and the ORs of physical activity.6 The frequencies of eczema within each level of physical activity were reconstructed as previously described.7
The exposure was the level of physical activity and the dependent variable was eczema. The definitions for physical activity varied by study. Eczema was also defined differently throughout studies, where some used the clinical criteria and others used various questions from the International Study of Allergy and Asthma in Children,8 or other definitions. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses was used to assess (i) study quality based on selection criteria, (ii) between-group comparability and (iii) study outcome using a nine-star scoring system.9,10 We included only studies with NOS ≥ 7 in the meta-analysis.
Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, U.S.A.). Studies of eczema and vigorous physical activity or exercise were combined. ORs of eczema in exercise or vigorous physical activity at least once or at least three times a week with 95% confidence intervals (CIs) were estimated. Forest plots were constructed for studies included in the meta-analysis. Pooled ORs were estimated using both fixed-effects models and random-effects models that accounted for variability between studies. Egger regression, Begg rank correlation and funnel plot regression were used to assess potential publication bias. A two-sided P-value of 0.05 was taken as significant.
The literature search yielded 4993 nonduplicate articles. After review of the titles and abstracts, 229 full-text articles were reviewed and seven manuscripts including eight studies were included in the final analysis.4–6,11–14 Of these, five manuscripts had sufficient data for inclusion in a meta-analysis.6,11–14 The PRISMA flow diagram is presented in Figure 1. The studies were all cross-sectional, with either retrospective or prospective data collection; included both male and female subjects; and encompassed subjects of all ages. The studies were published between 2008 and 2014. Quality assessment using the NOS scale revealed that five of the eight studies had scores ≥ 7 (good quality) (Table S2).
Fig 1.
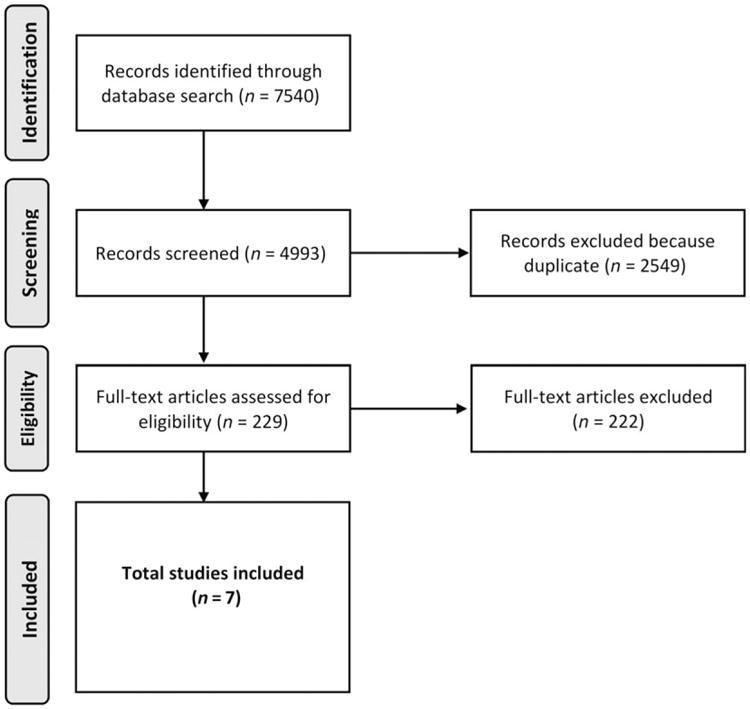
PRISMA flow diagram of the literature search and study selection for meta-analysis of eczema, exercise and vigorous activity.
Three studies found a positive association between eczema and physical activity; 4,11,12 three found an inverse association5,6,14 and one found no association.13 No published studies of the association between exercise or physical activity and eczema severity were found. There were four studies with NOS ≥ 7 included in the meta-analysis encompassing 61 974 patients, including 3065 children and 58 909 adults, of whom 5434 (8.8%) had eczema. Overall, 3298 (8.7%, range 7.5–47.3) of patients with less than once-weekly exercise, 2136 (8.8%, range 6.8–51.0) with at least once-weekly exercise and 147 (23.8%, range 14.9–47.9) with at least thrice-weekly exercise had a history of eczema.
Significant heterogeneity was identified between studies that assessed once-weekly (Cochran Q-test, P < 0.001; I2 = 87.5%), but not thrice-weekly vigorous activity or exercise (P = 0.37; I2 = 4.3%). Vigorous physical activity or exercise at least once weekly (OR 1.04, 95% CI 0.92–1.17) or thrice weekly (OR 1.11, 95% CI 0.88–1.40, P = 0.40) were not associated with eczema in a random-effects model (Fig. 2). Publication bias was not detected, as judged by nonsignificant Egger regression, Begg rank correlation or funnel plot regression for any of the above-mentioned outcomes (P ≥ 0.27).
Fig 2.
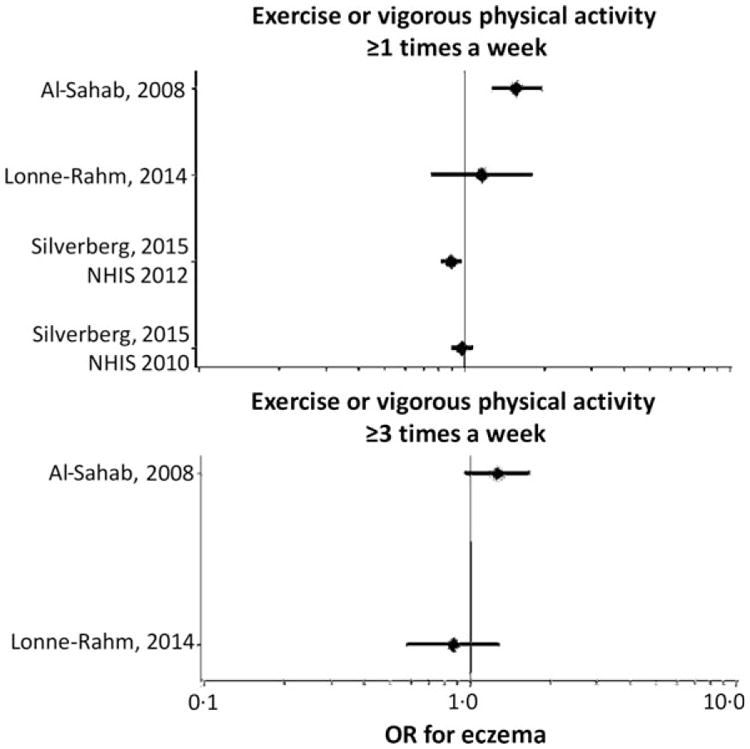
Association between eczema, exercise and vigorous activity. Forest plots are presented for the log odds ratios (ORs) and 95% confidence intervals of eczema in patients with at least once-weekly or thrice-weekly exercise and vigorous activity compared.
It is interesting that some studies found associations between eczema and increased physical activity.4,11 Al-Sahab et al. noted that, in Lebanon, people are mostly physically active outdoors and are thereby exposed to airborne pollutants that could exacerbate eczema.11 Furthermore, the frequency and types of physical activity and exercise performed are likely modified by a number of factors, including access to parks and recreational spaces, adiposity, functional limitation from medical disorders such as asthma or arthritis, sociocultural factors and attitudes towards healthfulness.
This systematic review revealed few high-quality studies, with varying definitions of exercise and vigorous physical activity, and it appears that none of the self-reported assessments of physical activity was previously validated. Thus, there is insufficient evidence to make solid conclusions. Future studies are needed to address the knowledge gaps about the association of eczema and physical activity. These should include use of objective measures; longitudinal studies to determine the temporal relationship; stratification of results by different sociodemographic groups, including race/ethnicity and sex; and exploration of the mechanisms of association.
Supplementary Material
Table S1. Literature search scheme for Ovid Medline.
Table S2. Study characteristics.
Acknowledgments
Funding sources: This publication was made possible with support from the Agency for Healthcare Research and Quality (AHRQ), grant number K12HS023011, and the Dermatology Foundation.
Footnotes
Supporting Information: Additional Supporting Information may be found in the online version of this article at the publisher's website:
Conflicts of interest: none declared.
References
- 1.Williams JR, Burr ML, Williams HC. Factors influencing atopic dermatitis: a questionnaire survey of schoolchildren's perceptions. Br J Dermatol. 2004;150:1154–61. doi: 10.1111/j.1365-2133.2004.05869.x. [DOI] [PubMed] [Google Scholar]
- 2.Yosipovitch G, Goon AT, Wee J, et al. Itch characteristics in Chinese patients with atopic dermatitis using a new questionnaire for the assessment of pruritus. Int J Dermatol. 2002;41:212–16. doi: 10.1046/j.1365-4362.2002.01460.x. [DOI] [PubMed] [Google Scholar]
- 3.Nankervis H, Pynn EV, Boyle RJ, et al. House dust mite reduction and avoidance measures for treating eczema. Cochrane Database Syst Rev. 2015;1:CD008426. doi: 10.1002/14651858.CD008426.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell EA, Beasley R, Bjorksten B, et al. The association between BMI, vigorous physical activity and television viewing and the risk of symptoms of asthma, rhinoconjunctivitis and eczema in children and adolescents: ISAAC Phase Three. Clin Exp Allergy. 2013;43:73–84. doi: 10.1111/cea.12024. [DOI] [PubMed] [Google Scholar]
- 5.Font-Ribera L, Villanueva CM, Nieuwenhuijsen MJ, et al. Swimming pool attendance, asthma, allergies, and lung function in the Avon Longitudinal Study of Parents and Children cohort. Am J Respir Crit Care Med. 2011;183:582–8. doi: 10.1164/rccm.201005-0761OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brescianini S, Brunetto B, Iacovacci P, et al. Prevalence of self-perceived allergic diseases and risk factors in Italian adolescents. Pediatr Allergy Immunol. 2009;20:578–84. doi: 10.1111/j.1399-3038.2008.00793.x. [DOI] [PubMed] [Google Scholar]
- 7.Di Pietrantonj C. Four-fold table cell frequencies imputation in meta analysis. Stat Med. 2006;25:2299–322. doi: 10.1002/sim.2287. [DOI] [PubMed] [Google Scholar]
- 8.Beasley R. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998;351:1225–32. [PubMed] [Google Scholar]
- 9.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 10.McPheeters ML, Kripalani S, Peterson NB, et al. Closing the quality gap: revisiting the state of the science (vol. 3: quality improvement interventions to address health disparities) Evid Rep Technol Assess (Full Rep) 2012:1–475. [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Sahab B, Atoui M, Musharrafieh U, et al. Epidemiology of eczema among Lebanese adolescents. Int J Public Health. 2008;53:260–7. doi: 10.1007/s00038-008-7085-2. [DOI] [PubMed] [Google Scholar]
- 12.Foliaki S, Annesi-Maesano I, Tuuau-Potoi N, et al. Risk factors for symptoms of childhood asthma, allergic rhinoconjunctivitis and eczema in the Pacific: an ISAAC Phase III study. Int J Tuberc Lung Dis. 2008;12:799–806. [PubMed] [Google Scholar]
- 13.Lonne-Rahm SB, Sundström I, Nordlind K, Engström LM. Adult atopic dermatitis patients and physical exercise: a Swedish questionnaire study. Acta Derm Venereol. 2014;94:185–7. doi: 10.2340/00015555-1556. [DOI] [PubMed] [Google Scholar]
- 14.Silverberg JI, Greenland P. Eczema and cardiovascular risk factors in 2 US adult population studies. J Allergy Clin Immunol. 2015;135:721–8.e6. doi: 10.1016/j.jaci.2014.11.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Literature search scheme for Ovid Medline.
Table S2. Study characteristics.


