Abstract
Secondhand tobacco smoke exposure in pregnancy increases the risk of neurodevelopmental disorders. We evaluated in rats whether there is a critical period during which tobacco smoke extract (TSE) affects the development of acetylcholine and serotonin systems, prominent targets for adverse effects of nicotine and tobacco smoke. We simulated secondhand smoke exposure by administering TSE so as to produce nicotine concentrations one-tenth those in active smoking, with 3 distinct, 10-day windows: premating, early gestation or late gestation. We conducted longitudinal evaluations in multiple brain regions, starting in early adolescence (postnatal day 30) and continued to full adulthood (day 150). TSE exposure in any of the 3 windows impaired presynaptic cholinergic activity, exacerbated by a decrement in nicotinic cholinergic receptor concentrations. Although the adverse effects were seen for all 3 treatment windows, there was a distinct progression, with lowest sensitivity for premating exposure and higher sensitivity for gestational exposures. Serotonin receptors were also reduced by TSE exposure with the same profile: little effect with premating exposure, intermediate effect with early gestational exposure and large effect with late gestational exposure. As serotonergic circuits can offset the neurobehavioral impact of cholinergic deficits, these receptor changes were maladaptive. Thus, there is no single ‘critical period’ for effects of low-level tobacco smoke but there is differential sensitivity dependent upon the developmental stage at the time of exposure. Our findings reinforce the need to avoid secondhand smoke exposure not only during pregnancy, but also in the period prior to conception, or generally for women of childbearing age.
Keywords: acetylcholine, developmental neurotoxicity, nicotine, serotonin: tobacco smoke.
Active maternal smoking during pregnancy contributes significantly to neurodevelopmental disorders in the offspring, with nicotine causing much of the adverse effects (England et al., 2015; Pauly and Slotkin, 2008). A larger population is exposed to secondhand cigarette smoke, about which much less is known (U.S. Surgeon General, 2006). Prenatal exposure to secondhand smoke is positively associated with neurodevelopmental deficits, including cognitive impairment and emotional disorders (DiFranza et al., 2004; Herrmann et al., 2008; Yolton et al., 2005), but causal proof has remained elusive for 2 reasons: the difficulty of exposure assessment in human studies, and the dearth of animal studies focusing on secondhand smoke (U.S. Surgeon General, 2006). Nearly all preclinical research reports on cigarette smoke have simulated active smoking rather than lower, secondhand levels. In general, the outcomes of these higher exposures resemble those of nicotine (Fuller et al., 2012; Golub et al., 2007; Gospe et al., 2009; Slotkin et al., 2006b, c), albeit that the smoke exposure includes the confound of unavoidable stress resulting from repetitive, involuntary confinement in a smoke-filled chamber.
Recently, we developed a tobacco smoke administration model in pregnant rats that ensures reliable dosing and avoids the stress of inhalation exposure (Hall et al., 2016; Slotkin et al., 2015). We paralleled the standard technique for nicotine delivery in pregnant rats, namely subcutaneously-implanted pumps (Slotkin, 2008) that deliver standardized tobacco smoke extract (TSE). We found that low TSE levels, comparable to secondhand smoke exposure (i.e. producing plasma nicotine levels one-tenth of those in typical smokers), nevertheless engendered synaptic dysfunction in acetylcholine (ACh) and serotonin (5-hydroxytryptamine, 5HT) systems, culminating in impaired cognitive and emotional behaviors (Hall et al., 2016; Slotkin et al., 2015). TSE exposure had greater effects than did comparable treatment with nicotine alone and indeed, TSE was similar to a 10-fold higher nicotine level; that is, TSE simulating secondhand exposure elicited outcomes like nicotine at active smoking levels. Importantly, TSE impaired adaptive changes to the synaptic damage. Nicotine alone produced compensatory upregulation of nicotinic ACh receptors (nAChRs) and 5HT receptors (Slotkin et al., 2015), effects that would serve to offset deficits in presynaptic ACh activity (Aldridge et al., 2005). With TSE, these compensatory effects were not only absent, but actually showed opposite changes, namely, receptor reductions that augment presynaptic deficits. Finally, many of the TSE effects reflected a direct impact on neurodifferentiation, as they were recapitulated with an in vitro TSE exposure model (Slotkin et al., 2014).
Our prior work established the effect of TSE with exposures encompassing the entire period of development from conception through the second postnatal week (Hall et al., 2016; Slotkin et al., 2015), paralleling stages of human fetal brain development in all 3 trimesters (Rodier, 1988). The current study addresses the important issue of whether there is a critical period for the adverse effects of low-level TSE exposure on development of ACh and 5HT systems. This type of information is vital to understanding whether there is a ‘safe’ period in which exposure might not be so injurious, or a particularly sensitive period in which the major damage occurs. We evaluated exposure prior to mating, exposure in early gestation (conception through the neural tube stage), and exposure in late gestation (primary period of neuronal cell replication and differentiation), modeled on our earlier work (Slotkin et al., 2015). We assessed the impact on brain regions comprising the major ACh and 5HT projections and their corresponding cell bodies. For ACh, we assayed choline acetyltransferase (ChAT), presynaptic high-affinity choline transporters (hemicholinium-3 [HC3] binding) and α4β2 nAChRs. ChAT and high-affinity choline transporters are constitutive components of ACh nerve terminals but differ in their functional significance. ChAT synthesizes ACh, but is not regulated by nerve impulse activity, so that it provides an index of the development of ACh projections (Slotkin, 2008). However, HC3 binding to the choline transporter is regulated by neuronal activity (Klemm and Kuhar, 1979), so that the comparative effect on HC3 binding versus ChAT (HC3/ChAT ratio) additionally enables the characterization of presynaptic impulse activity (Slotkin, 2008). The α4β2 nAChR is the most abundant nAChR subtype in the mammalian brain and regulates the ability of ACh systems to release other neurotransmitters involved in reward, cognition and mood (Dani and De Biasi, 2001). For 5HT systems, we focused on 5HT1A and 5HT2 receptors, the subtypes that are known to be major targets for developmental neurotoxicity of nicotine (Slikker et al., 2005; Slotkin et al., 2007), and that play major roles in 5HT-related mental disorders, including depression (Maes and Meltzer, 1995).
MATERIALS AND METHODS
Tobacco smoke extract
TSE was prepared from Kentucky Reference cigarettes (KY3R4F) on a Rotary Smoke Machine under ISO (International Organization for Standardization, Geneva, Switzerland) smoke conditions. The smoke condensate was collected on 92 mm filter pads, which were then extracted by shaking for 20 min with undiluted dimethylsulfoxide (DMSO), to obtain a solution of approximately 20 mg of condensate per ml. Condensate aliquots were stored in amber vials at -80 °C until used. Two cigarettes were smoked to produce each ml of extract and the final product contained 0.8 mg/ml nicotine (determined by the manufacturer).
Animal treatments
All experiments were carried out humanely and with regard for alleviation of suffering, with protocols approved by the Duke University Animal Care and Use Committee and in accordance with all federal and state guidelines. Sprague-Dawley rats were shipped by climate-controlled truck (transportation time < 1 h) and were allowed to acclimate to the housing facility for 2 weeks prior to treatment. Treatments were given via iPrecio® microinfusion pumps, implanted subcutaneously. These pumps are refillable via a percutaneous septum, so that a single surgery and pump implant could be used for delivery of different treatments in sequence. Animals were anesthetized (60 mg/kg ketamine + 0.15–0.50 mg/kg dexmedetomidine given i.p.; followed post-implant by 0.15 mg/kg atipemezole + 5 mg/kg ketoprofen given s.c. and topical bupivicaine). There were 4 treatment groups, each comprising 12–13 dams: (1) controls received DMSO vehicle throughout the entire 30-day treatment period; (2) the TSE premating group received TSE for the first 10 days, followed by DMSO for the remaining 20 days; (3) the TSE early gestation group received DMSO for the first 10 days, then TSE for the next 10 days, followed by DMSO for the last 10 days; and (4) the TSE late gestation group received DMSO for the first 20 days, then TSE for 10 days. To maintain a constant dose level equivalent to 0.2 mg/kg/day of nicotine, the pump flow rate was adjusted upward to compensate for weight gain during pregnancy. At the end of the first 10-day infusion period, mating was initiated by including a male rat in the cage for 4 days, after which the pregnant dams were placed in breeding cages. Because conception could have taken place at any point during the mating period, the actual gestational exposure periods have an uncertainty of a few days; using parturition dates as a benchmark, the values ranged as follows: TSE premating group, begun 10-13 days prior to fertilization and terminating between 0 and 3 days prefertilization; TSE early gestation group, begun between 1 and 4 days prefertilization and terminating between gestational days 6–9; TSE late gestation group, begun between 7 and 9 days of gestation and terminating between days 17 and 19 of gestation. We previously established the bioequivalence of nicotine delivered in TSE as compared to nicotine alone (Slotkin et al., 2015).
The birth date was considered to be postnatal day (PN) 0, at which point litters were culled to 8-10 pups to ensure standard nutrition. Weaning occurred on PN21. On PN30, 60, 100 and 150, animals were decapitated and brain regions were dissected for determination of ACh and 5HT synaptic markers: frontal/parietal cortex, temporal/occipital cortex, hippocampus, striatum, midbrain and brainstem. The 2 cortical regions were sectioned at the midline and the right half used for the current determinations. The left halves of the cortical regions were reserved for future studies, along with the cerebellum, which is sparse in ACh and 5HT projections. Tissues were frozen in liquid nitrogen and stored at −80 °C until assayed. Each treatment group comprised 12 animals at each age point, equally divided into males and females. Animals were selected such that, for any single time point, no more than 1 male and 1 female were chosen from the same litter for each treatment group; over the 4 sequential time points, no more than 3 males and 3 females were utilized from each litter out of a total of 48 animals for a given treatment group (4 time points, 2 sexes, n = 6 at each time point).
Assays
Assays were conducted on each individual tissue, so that each determination represented a value from the corresponding brain region of 1 animal. Tissues were thawed in 79 volumes of ice-cold 10 mM sodium-potassium phosphate buffer (pH 7.4) and homogenized with a Polytron (Brinkmann Instruments, Westbury, New York, USA). Aliquots of the homogenate were assayed for ChAT using established procedures (Qiao et al., 2003). Each tube contained 50 µM [14C]acetyl-coenzyme A as a substrate and activity was determined as the amount of labeled ACh produced relative to tissue protein. For measurements of HC3 binding, the cell membrane fraction was prepared from an aliquot of the same tissue homogenate by sedimentation at 40 000 × g for 15 min. The pellet was resuspended and washed, and the resultant pellet was assayed, using a ligand concentration of 2 nM [3H]HC3 with or without 10 µM unlabeled HC3 to displace specific binding (Qiao et al., 2003). Determinations of nAChR binding were carried out in another aliquot, each assay containing 1 nM [3H]cytisine with or without 10 µM nicotine to displace specific binding (Slotkin et al., 2008). Similarly, we determined binding to 5HT receptors with established techniques (Slotkin et al., 2006a), using 1 nM [3H]8-hydroxy-2-(di-n-propylamino)tetralin for 5HT1A receptors, and 0.4 nM [3H]ketanserin for 5HT2 receptors. For 5HT1A receptors, specific binding was displaced by addition of 100 µM 5HT; for 5HT2 receptors, we used 10 µM methylsergide for displacement. Ligand binding was calculated relative to the membrane protein concentration.
Some of the regions had insufficient amounts of tissue to permit all assays to be performed. Accordingly, we did not obtain values for 5HT receptors in either the striatum or hippocampus, nor did we measure nAChRs in the striatum on PN30.
Data analysis
The initial statistical comparisons were conducted by a global analysis of variance (ANOVA; data log-transformed because of heterogeneous variance among regions, measures and ages) incorporating all the variables and measurements in a single test so as to avoid an increased probability of type 1 errors that might otherwise result from multiple tests of the same data set. The variables in the global test were prenatal treatment (vehicle and the 3 different TSE exposure windows), brain region, age and sex, with multiple dependent measures (hereafter, designated simply as ‘measures’): ChAT, HC3 binding and nAChR binding for the ACh synaptic makers; 5HT1A and 5HT2 receptor binding for the 5HT synaptic markers. For both transmitter systems, the dependent measures were treated as repeated measures, since all the determinations were derived from the same sample. Where we identified interactions of treatment with the other variables, data were then subdivided for lower-order ANOVAs to evaluate treatments that differed from the corresponding control or from each other. As permitted by the interaction terms, individual treatments that differed from control were identified with Fisher’s Protected Least Significant Difference Test. However, where treatment effects were not interactive with other variables, we report only the main treatment effects without performing lower-order analyses of individual values. Significance was assumed at the level of P < .05.
Data were compiled as means and standard errors. To enable ready visualization of treatment effects across different regions, ages and measures, the results are given as the percent change from control values, but statistical procedures were always conducted on the original data, with log transforms because of heterogeneous variance as noted above. In addition, the log-transform evaluates the treatment differences as a proportion to control values, rather than as an arithmetic difference. This was important because of technical limitations: on any single day, we could conduct assays for all treatment groups and both sexes, but for only 1 region at 1 age point. Accordingly, representing the data as proportional differences (percent control) enables a full comparison of treatment effects and treatment interactions with all the other variables, even though absolute values for the controls cannot be compared across regions and ages (since assays for each region and age point were run on separate days). Graphs were scaled to encompass the different dynamic ranges of the changes in the various parameters. The absolute values for each set of determinations appear in the Supplementary tables.
Materials
TSE was prepared by Arista Laboratories (Richmond, Virginia, USA). Animals were purchased from Charles River Laboratories (Raleigh, North Carolina, USA) and iPrecio® implantable microinfusion pumps were from Primetech Corp. (Tokyo, Japan). PerkinElmer Life Sciences (Boston, Massachusetts, USA) was the source for [3H]HC3 (specific activity, 125 Ci/mmol), [3H]cytisine (specific activity 35 Ci/mmol), [3H]8-hydroxy-2-(di-n-propylamino)tetralin (specific activity, 135 Ci/mmol), [3H]ketanserin (63 Ci/mmol) and [14C]acetyl-coenzyme A (specific activity 6.7 mCi/mmol). Methylsergide was obtained from Sandoz Pharmaceuticals (East Hanover, New Jersey, USA) and all other chemicals came from Sigma Chemical Co. (St. Louis, Missouri, USA).
RESULTS
Maternal, Litter and Growth Effects
There were no significant effects of any of the treatments on maternal weight gain, the proportion of dams giving birth, litter size, or sex ratio (data not shown). There were small, but statistically significant effects on growth of the offspring (Supplementary Table S1). Two of the TSE groups (premating and early gestational exposure) showed a 3–5% lower overall weight but after subdivision by age, the only significant effect was for the early gestational group on PN30. Brain region weights were not significantly different for any of the treatments (Supplementary Table S1).
ACh Synaptic Markers
Multivariate ANOVA incorporating all 4 treatment groups, sex, age, brain region and the 3 ACh synaptic measures (ChAT activity, HC3 binding, nAChR binding) indicated a main effect of the treatments (P < .0001) that interacted with 3 of the other variables: P < .0001 for treatment × measure, P < .005 for treatment × sex, and P < .02 for treatment × measure × age. In light of the strong interaction of treatment × measure, we subdivided the data into the individual measures and looked for treatment effects and interactions of treatment with the remaining variables.
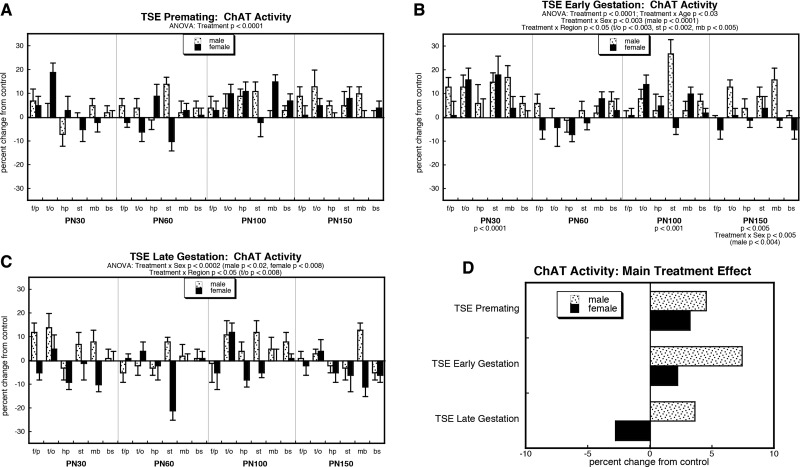
For ChAT activity, ANOVA incorporating all treatment groups indicated a main effect of treatment (P < .0001) that depended on age (treatment × age, P < .02), sex (treatment × sex, P < .0003) and region (treatment × region, P < .04). Accordingly, we evaluated main effects and interactions for each of the treatment paradigms. Premating exposure to TSE produced a consistent, highly significant overall increase in ChAT activity, without distinction by age, sex or region (Fig. 1A). Shifting the exposure period to early gestation likewise produced a significant net elevation (main treatment effect) but with a more selective pattern (Fig. 1B). Values were elevated on PN30 but returned to normal by the closure of adolescence (PN60), only to have the increases reemerge later in adulthood (PN100, PN150). The effects of early gestational exposure were also sex selective, (greater effects in males), and regionally selective (greater effects in temporal/occipital cortex, striatum and midbrain). In contrast, TSE exposure in late gestation elicited a different pattern of effects on ChAT activity (Fig. 1C), with significant elevations in males but decrements in females. To illustrate the differences in the main treatment effects among the 3 groups, we calculated the mean values for effects on ChAT activity, collapsed across region and age (Fig. 1D). This simplified picture dilutes the effects seen for specific regions or ages by averaging them with data points for which there was no effect or an opposite effect, so that the absolute magnitude becomes smaller. Despite these limitations, there was an obvious overall pattern: premating TSE exposure increased ChAT equivalently in males and females, early gestational exposure evoked bigger increases in males than females, and late gestational exposure elicited increases in males but decreases in females. In males, the early gestation period appeared to be the most sensitive, with elevations significantly greater than either the premating group (P < .009) or the late gestational group (P < .0001). In females, the decrease that was unique to late gestational period was statistically distinguishable from the increases seen with the other 2 regimens (P < .0001 for each).
FIG. 1.
Effects on ChAT activity, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S2. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests for each age were carried out where there was a significant treatment × age interaction (B), as well tests for each region and sex where treatment interacted with those variables (B,C). D, The simple main treatment effects, collapsed across age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; hp, hippocampus; st, striatum; mb, midbrain; bs brainstem.
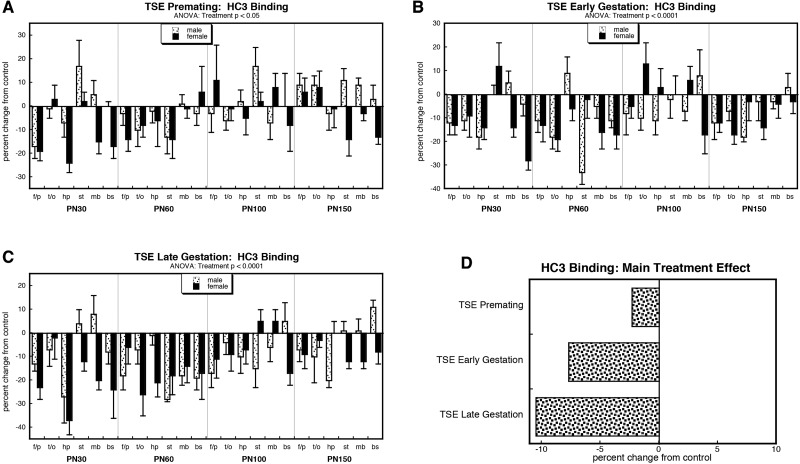
For HC3 binding, the global ANOVA indicated a main treatment effect (P < .0001) but no significant interactions of treatment with the other variables. Accordingly, we examined each exposure group for main treatment effects only (retaining the other factors in the ANOVA design, but ignoring lower-order, ‘significant’ interactions as potentially spurious). TSE administered in the premating period evoked a significant overall decrement (Fig. 2A), as did early (Fig. 2B) or late (Fig. 2C) gestational exposure. Again, we collapsed the treatment effects across the other variables (sex, age, region) to compare the magnitude of the deficits (Fig. 2D), this time also collapsing the sex variable, since there was no treatment × sex interaction. There was a clear progression of sensitivity, with the lowest effect seen for premating exposure, followed by early gestational exposure, and with the greatest effect from late gestational exposure: P < .0003 for premating versus early gestation, P < .0001 for premating versus late gestation, P < .008 for early gestation versus late gestation.
FIG. 2.
Effects on HC3 binding, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S3. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests for each age, sex or region were not carried out because of the absence of interactions of treatment with these variables. D, The simple main treatment effects, collapsed across sex, age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; hp, hippocampus; st, striatum; mb, midbrain; bs brainstem.
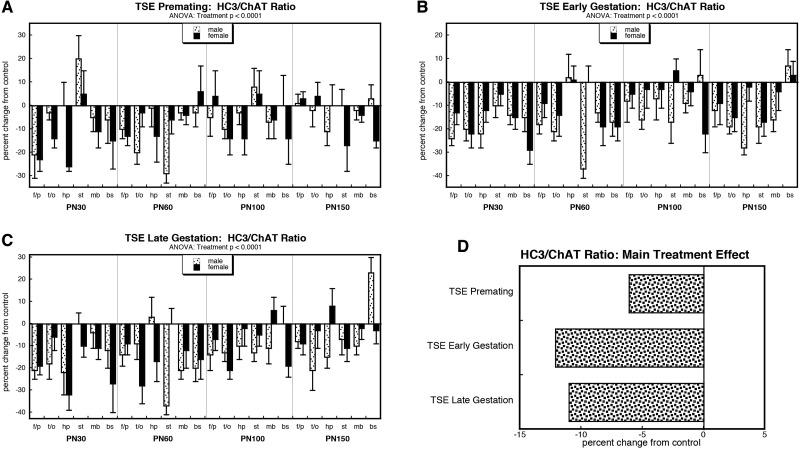
For the HC3/ChAT ratio, there was a significant main treatment effect (P < .0001) that interacted only with sex (treatment × sex, P < .04); however, after subdivision, none of the individual treatments retained sufficient statistical power to give a treatment × sex interaction, so interpretation was again limited to the main treatment effects. TSE given premating produced a significant decrement in the ratio (Fig. 3A), as did exposure during either the early (Fig. 3B) or late (Fig. 3C) gestational period. Collapsing the treatment effects across the other variables again showed that premating exposure had a lesser overall effect than either gestational exposure window (Fig. 3D): P < .0005 for premating versus early gestation, P < .0001 for premating versus late gestation.
FIG. 3.
Effects on the HC3/ChAT ratio, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S4. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests for each age, sex or region were not carried out because of the absence of interactions of treatment with these variables. Panel (D) shows the simple main treatment effects, collapsed across sex, age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; hp, hippocampus; st, striatum; mb, midbrain; bs brainstem.
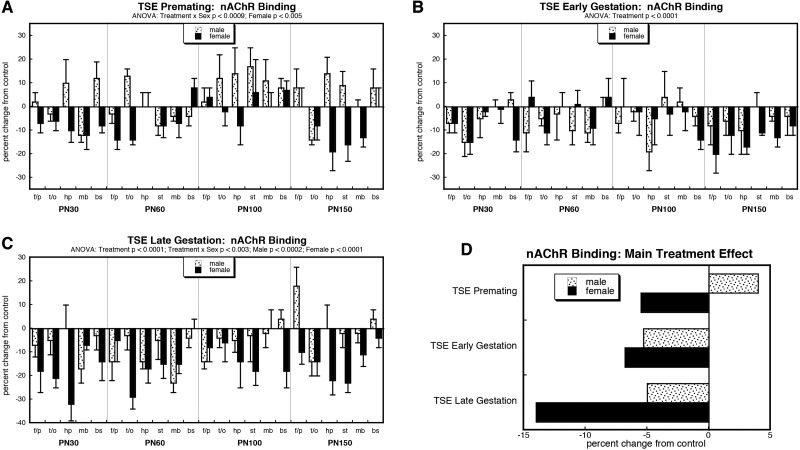
For nAChR binding, the overall ANOVA indicated a significant main treatment effect (P < .0001) and interactions of treatment × age (P < .02) and treatment × sex (P < .002). Again, this justified separation of the individual treatments and examination of main treatment effects and interactions for each. TSE exposure in the premating period elicited a sex-selective effect on nAChR binding, with a significant overall decrement in females but not males (Fig. 4A); in fact, males tended to show an increase instead of a decrease (P < .07). Shifting the exposure window to the early gestational period elicited a consistent decrease in nAChR binding across both sexes (Fig. 4B). With late gestational TSE exposure, there was a robust decrement for both males and females (Fig. 4C), larger than that seen with either of the other exposures (P < .0001 compared to premating TSE, P < .03 compared to early gestation TSE), but again, the decrease in females was much larger. These overall patterns were evident with values collapsed across age and region (Fig. 4D). In males, the decrement caused by exposure in either of the 2 gestational windows was distinguishable from the increase evoked by premating TSE (P < .0001 for each); for females, exposure in the late gestational window had greater effects than for premating or early gestational exposure (P < .0001 for each).
FIG. 4.
Effects on nAChR binding, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S5. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests for each age or region were not carried out because of the absence of interactions of treatment with these variables. D, The simple main treatment effects, collapsed across across age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; hp, hippocampus; st, striatum; mb, midbrain; bs brainstem.
5HT receptors
Multivariate ANOVA incorporating all 4 treatment groups, sex, brain region and the 2 5HT receptor measurements (5HT1A and 5HT2 subtypes) indicated a main effect of treatment (P < .0001) that was subtype-selective (treatment × measure, P < .0001) and age-dependent (treatment × age, P < .02). Given the interaction of treatment × measure, we separated the 2 subtypes for lower-order examination of treatment effects and interactions of treatment with the other variables.
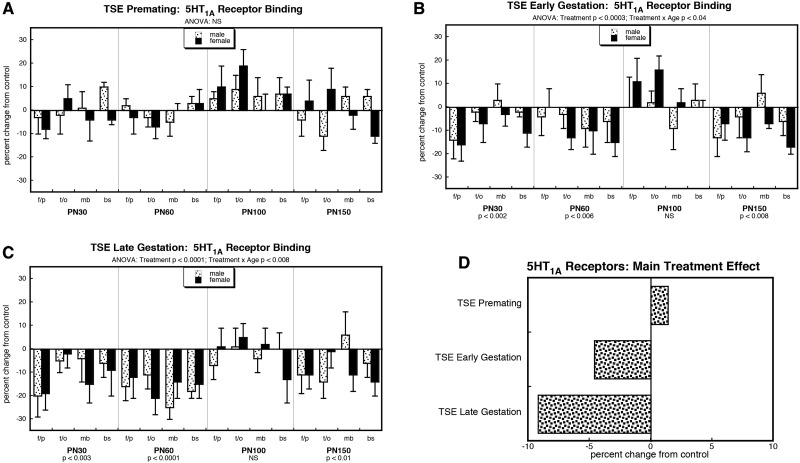
For the 5HT1A subtype, the overall ANOVA indicated a main treatment effect (P < .0001) that interacted with age (treatment × age, P < .05). Premating TSE exposure had no significant effect (Fig. 5A). In contrast, TSE exposure during the early gestational period elicited a significant overall deficit, with a distinct time progression (Fig. 5B): values were initially subnormal, but returned to control values by PN100, only to see reemergence of deficits by PN150. The same pattern was seen for late gestational TSE exposure except that the deficits were larger (P < .01 comparing main treatment effects for the 2 windows; Fig. 5C). The progressive increase in sensitivity to TSE from premating to early gestational to late gestational exposure was readily apparent with values collapsed across sex, age and region (Fig. 5D): P < .0004 comparing premating TSE to early gestational exposure, P < .0001 comparing premating TSE to late gestational exposure, P < .0006 comparing the 2 gestational exposure groups.
FIG. 5.
Effects on 5HT1A receptor binding, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S6. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests for each age were carried out where there was a significant treatment × age interaction (B,C). D, The simple main treatment effects, collapsed across sex, age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; mb, midbrain; bs brainstem; NS, not significant.
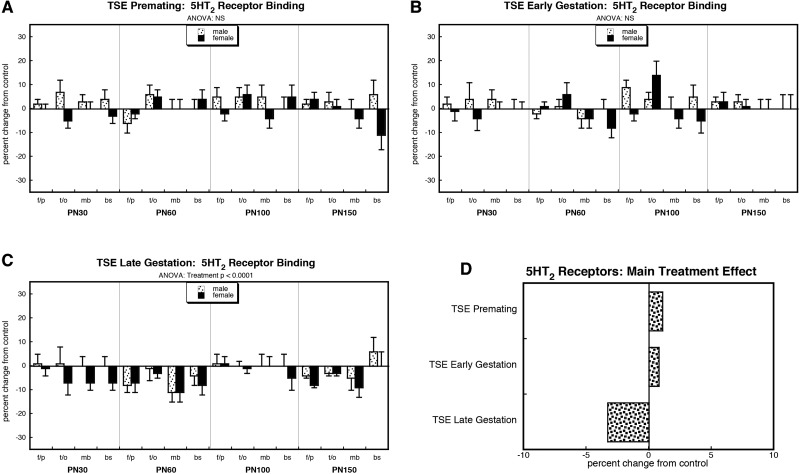
The 5HT2 receptor subtype likewise showed a significant treatment effect (P < .0001) but no interactions with the other factors. Neither premating TSE exposure (Fig. 6A) nor exposure in the early gestational period (Fig. 6B) showed significant differences. However, just as with the 5HT1A subtype, the late gestational exposure group was more sensitive, showing significant deficits compared to control values (Fig. 6C) that were clearly distinguishable from the lack of effect seen in the other 2 windows (P < .0001 comparing main treatment effects). For the late gestational group, the deficit for 5HT2 receptors was notably smaller than that seen for the 5HT1A subtype (P < .0001). Again, these relationships were readily apparent with values collapsed across sex, age and region (Fig. 6D).
FIG. 6.
Effects on 5HT2 receptor binding, of TSE exposure during premating (A), early gestational (B) or late gestational (C) windows. Data represent means and standard errors, presented as the percent change from control values; complete original data are shown in Supplementary Table S6. Multivariate ANOVA for each treatment appears at the top of the panels. Lower-order tests were not evaluated because of the absence of significant interactions of treatment with sex, age or region. D, The simple main treatment effects, collapsed across sex, age and region. Abbreviations: f/p, frontal/parietal cortex; t/o, temporal/occipital cortex; mb, midbrain; bs brainstem; NS, not significant.
DISCUSSION
There are 2 major findings. First, there is a progressive sensitivity of the developing brain to TSE disruption of ACh circuits, with smallest effects from premating exposure, followed by early gestation, and then greatest effects from late gestation. The second finding is that there is no ‘critical period.’ All exposure paradigms produced defects, even premating treatment, where TSE terminated prior to conception. These outcomes are even more notable, given that we modeled low levels paralleling secondhand smoke, rather than active maternal smoking, and that TSE underestimates the impact because it does not include gaseous components that are likely to be injurious, such as HCN and CO.
For each window, our findings resembled those seen earlier for continuous, perinatal TSE exposure (Slotkin et al., 2015), namely a deficit in presynaptic ACh activity augmented by loss of postsynaptic nAChRs and a parallel shortfall of 5HT receptors. With exposure to nicotine alone, there are compensatory responses that partially offset deficient presynaptic ACh activity, including upregulation of both receptor classes (Slotkin et al., 2015); in the face of ACh presynaptic damage, augmented 5HT function can restore behavioral performance (Aldridge et al., 2005). However, TSE exposure instead produces a loss of nAChRs and 5HT receptors, augmenting the presynaptic deficit (Slotkin et al., 2015). Here, this pattern was seen with each treatment paradigm, in whole or in part, with the gestational windows most closely paralleling the effects of more prolonged TSE exposure (Slotkin et al., 2015). Thus the HC3/ChAT ratio, which assesses presynaptic ACh activity, was decreased equivalently with either early gestational or late gestational exposure, but the receptor deficiencies were more profound with the latter. Exposure in the premating period produced a smaller decrement in presynaptic activity, a loss of nAChRs that was limited to females (whereas it involved both sexes for gestational treatments), and maintenance of normal 5HT receptors. Nevertheless, despite the similar directions of overall effects, the different developmental windows exhibited targeting of distinct events in neurodifferentiation. For early gestational exposure, deficient ACh presynaptic activity reflected a greater impact on ChAT activity and a lesser effect on HC3 binding, as compared to late gestation, where the reverse was true. Likewise, the effects on nAChR binding were sex-selective for premating and late gestational exposures, but not for early gestational exposure; again, the sex preference (female effect > male) was the same as that seen earlier with continuous perinatal exposure (Slotkin et al., 2015). Given that the TSE exposures of both sexes were identical, the male-female differences undoubtedly arise from post-injury adaptations that are themselves sex-dependent. Thus, the overall pattern is for increasing fetal sensitivity to TSE as development progresses, but superimposed on this overall pattern, there are maturational events that are distinct to each window and that are differentially vulnerable.
The 2 key questions are: (1) why does sensitivity to TSE increase as gestation proceeds, and (2) why is the premating period vulnerable, when there is no brain formation going on during exposure? Greater sensitivity during late gestation is readily explainable. With early toxicant exposure, lost neurons can be replaced because of the plasticity engendered by high rates of neuronal cell replication, whereas differentiated neurons cannot divide and thus are incapable of making up for deficits (Rodier, 1988). Thus, massive initial disruption of brain structure by nicotine up to the neural tube stage nevertheless is repaired and ultimately results in near-normal morphology (Slotkin, 2008). In contrast, the late gestational exposure window encompasses phases of terminal neurodifferentiation and assembly of higher-order brain structures, events that, if subjected to damage, are not readily reversible. By the same token, it might be expected that postnatal TSE exposure (paralleling third trimester human development) could have even greater effects. Our earlier study of prolonged TSE exposure spanned all of gestation and the first 2 postnatal weeks (Slotkin et al., 2015), but was also limited by the fact that exposure via maternal milk delivers a lower dose than does direct fetal perfusion during gestation; thus, even that study still underestimates the potential impact of tobacco smoke exposure. Cigarette smoke exposure in the postnatal period mimicking active smoking, is known to cause neurobehavioral damage (Torres et al., 2015) and this is also seen with nicotine-containing e-cigarette vapor (Smith et al., 2015). It would thus be worthwhile to devise a secondhand smoke exposure animal model for third trimester human exposure.
Our most intriguing finding is that TSE exposure is injurious even when limited to the premating period. There are 4 possible explanations. First, despite the cessation of TSE administration prior to conception, certain TSE components could persist into the early gestational period and thus affect brain formation. The half-life of nicotine in the rat is only about 1 h (Kyerematen et al., 1988), so it is highly unlikely that the effects of premating TSE exposure reflect this chemical component. However, the same is not true for nicotine metabolites that are also potentially bioactive, and which have half-lives of several days (Kyerematen et al., 1988), or for potentially long-lived lipophilic organic chemicals in TSE; for example, the terminal half-life of benzo[a]pyrene is about 17 hr (Foth et al., 1988). A second possibility is that TSE could produce lasting changes in maternal physiology, hormonal status and/or placental formation or function. Smoking in pregnancy produces persistent changes in plasma thiocyanate levels that compromise oxygen delivery (Jensen and Foss, 1981), in maternal metabolism (Pirani and MacGillivray, 1978), and in the risk of placental disorders (Naeye, 1979), all of which are likely to persist beyond the presence of TSE components. A third reason for premating TSE effects could be epigenetic changes in the ovum. Maternal smoking during pregnancy clearly produces epigenetic changes in the offspring (Knopik et al., 2012; Murphy et al., 2012; Suter et al., 2013) but there are no data available as to whether these can be induced prior to fertilization; clearly, this is an important area for future study. Yet a fourth possibility for sensitivity to premating TSE exposure, is that adverse effects could be contributed by nicotine withdrawal. The current study design involves withdrawal at different points in gestation, whereas our prior study with continuous TSE did not (Slotkin et al., 2015). We regard this explanation as unlikely. First, the exposure model simulates nicotine levels associated with secondhand smoke exposure, not active smoking. Second, the effects of the treatment windows here were equivalent to, or less than, those seen with continuous exposure, whereas if withdrawal were responsible for the effects, they should have been greater. The first 3 possibilities are thus the most likely explanations for premating TSE effects but we have no current information to select among those hypotheses. Regardless, though, the main point is that TSE is injurious to brain development even when discontinued prior to conception.
We also considered whether pharmacokinetic factors at the various developmental stages could contribute to differential sensitivity to TSE. Specifically, the premating and early gestational windows involve a span in which there is no direct connection between the maternal circulation and the ovum or embryo; in the rat, fetal implantation in the uterine wall occurs in the latter half of the first week postconception. However, if a direct circulatory connection were required, we would expect no effect whatsoever for the premating window, which was not the case. Indeed, because we used a continuous infusion model, all water spaces within the dam achieve and maintain a steady-state equilibrium for lipophilic substances even without a direct circulatory connection (Goldstein et al., 1974), and these spaces include the ovum, embryo, placenta and amniotic fluid; nicotine and TSE organics are all highly lipophilic and thus will equilibrate. Accordingly, it is likely that the developing organism is exposed to effective concentrations of TSE components in all of the exposure windows. Actually, since the placenta serves as a diffusion barrier and metabolizes many foreign substances, exposure might even be lower in the period after the embryo implants in the uterine wall.
Finally, a number of parameters showed recovery in late adolescence to early adulthood, but a subsequent return to abnormal values: 5HT1A receptors with either gestational window, 5HT2 receptors for late gestational exposure, and ChAT activity for early gestational exposure. The temporary restorative effects may represent compensations for deficient ACh function that eventually fail to keep up with the underlying damage, or, more intriguingly, that may reemerge as a presage of aging. Future work should address whether premating and/or gestational exposure to secondhand smoke could result in earlier onset of the impairments associated with senescence. Indeed, we have already shown this to be the case for organophosphate pesticides, that like TSE, cause damage to ACh and 5HT circuits (Levin et al., 2010).
In conclusion, our results provide some of the first mechanistic connections between secondhand tobacco smoke exposure and adverse neurodevelopmental outcomes, specifically identifying the late gestational stage as the most vulnerable. At the same time, however, we found that susceptibility is present to varying extents at all stages. The fact that damage is produced even when exposure is limited to the premating period has important implications for public health, as it reinforces the need to avoid secondhand smoke exposure not only during pregnancy, but also in the period prior to conception, or generally for women of childbearing age.
SUPPLEMENTARY DATA
Supplementary data are available online at http://toxsci.oxfordjournals.org/.
ACKNOWLEDGMENTS
TAS has received consultant income in the past 3 years from the following firms: Acorda Therapeutics (Ardsley NY), Pardieck Law (Seymour, IN), and Walgreen Co. (Deerfield, IL).
FUNDING
This work was supported by the National Institutes of Health [grant number ES022831] and by the U.S. Environmental Protection Agency [grant number 83543701]. EPA support does not signify that the contents reflect the views of the Agency, nor does mention of trade names or commercial products constitute endorsement or recommendation for use.
REFERENCES
- Aldridge J. E., Levin E. D., Seidler F. J., Slotkin T. A. (2005). Developmental exposure of rats to chlorpyrifos leads to behavioral alterations in adulthood, involving serotonergic mechanisms and resembling animal models of depression. Environ. Health Perspect. 113, 527–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dani J. A., De Biasi M. (2001). Cellular mechanisms of nicotine addiction. Pharmacol. Biochem. Behav. 70, 439–446. [DOI] [PubMed] [Google Scholar]
- DiFranza J. R., Aligne C. A., Weitzman M. (2004). Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics 113, 1007–1015. [PubMed] [Google Scholar]
- England L., Bunnell R. E., Pechacek T. F., Tong V. T., McAfee T. A. (2015). Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am. J. Prevent. Med. 49, 286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foth H., Kahl R., Kahl G. F. (1988). Pharmacokinetics of low doses of benzo[a]pyrene in the rat. Food Chem. Toxicol. 26, 45–51. [DOI] [PubMed] [Google Scholar]
- Fuller B. F., Cortes D. F., Landis M. K., Yohannes H., Griffin H. E., Stafflinger J. E., Bowers M. S., Lewis M. H., Fox M. A., Ottens A. K. (2012). Exposure of rats to environmental tobacco smoke during cerebellar development alters behavior and perturbs mitochondrial energetics. Environ. Health Perspect. 120, 1684–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A., Aronow L., Kalman S. M. (1974). Principles of Drug Action: The Basis of Pharmacology, 2nd ed John Wiley & Sons, New York. [Google Scholar]
- Golub M. S., Slotkin T. A., Pinkerton K. E. (2007). Visual recognition memory and auditory brainstem response in infant rhesus monkeys exposed perinatally to environmental tobacco smoke. Brain Res. 1151, 102–106. [DOI] [PubMed] [Google Scholar]
- Gospe S. M., Jr., Joyce J. A., Siebert J. R., Jack R. M., Pinkerton K. E. (2009). Exposure to environmental tobacco smoke during pregnancy in rats yields less effect on indices of brain cell number and size than does postnatal exposure. Reprod. Toxicol. 27, 22–27. [DOI] [PubMed] [Google Scholar]
- Hall B. J., Cauley M., Burke D., Kiany A., Slotkin T. A., Levin E. D. (2016). Cognitive and behavioral impairments evoked by low level exposure to tobacco smoke components: comparison with nicotine alone. Toxicol. Sci. 151, 236–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann M., King K., Weitzman M. (2008). Prenatal tobacco smoke and postnatal secondhand smoke exposure and child neurodevelopment. Curr. Opin. Pediatr. 20, 184–190. [DOI] [PubMed] [Google Scholar]
- Jensen O. H., Foss O. P. (1981). Smoking in pregnancy. Effects on the birth weight and on thiocyanate concentration in mother and baby. Acta Obstet. Gynecol. Scand. 60, 177–181. [PubMed] [Google Scholar]
- Klemm N., Kuhar M. J. (1979). Post-mortem changes in high affinity choline uptake. J. Neurochem. 32, 1487–1494. [DOI] [PubMed] [Google Scholar]
- Knopik V. S., Maccani M. A., Francazio S., McGeary J. E. (2012). The epigenetics of maternal cigarette smoking during pregnancy and effects on child development. Dev. Psychopathol. 24, 1377–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyerematen G. A., Taylor L. H., deBethizy J. D., Vessell E. S. (1988). Pharmacokinetics of nicotine and 12 metabolites in the rat. Application of a new radiometric high performance liquid chromatography assay. Drug. Metab. Dispos. 16, 125–129. [PubMed] [Google Scholar]
- Levin E. D., Timofeeva O. A., Yang L., Ryde I. T., Wrench N., Seidler F. J., Slotkin T. A. (2010). Early postnatal parathion exposure in rats causes sex-selective cognitive impairment and neurotransmitter defects which emerge in aging. Behav. Brain Res. 208, 319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M., Meltzer H. (1995). The serotonin hypothesis of major depression In Psychopharmacology: The Fourth Generation of Progress (Bloom F. E., Kupfer D. J., Bunney B. S., Ciaranello R. D., Davis K. L., Koob G. F., Meltzer H. Y., Schuster C. R., Shader R. I., Watson S. J., Eds.), pp. 933–944. Raven Press, New York. [Google Scholar]
- Murphy S. K., Adigun A. i., Huang Z. G., Overcash F., Wang F., Jirtle R. L., Schildkraut J. M., Murtha A. P., Iversen E. S., Hoyo C. (2012). Gender-specific methylation differences in relation to prenatal exposure to cigarette smoke. Gene 494, 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naeye R. L. (1979). The duration of maternal cigarette smoking, fetal and placental disorders. Early Hum. Dev. 3, 229–237. [DOI] [PubMed] [Google Scholar]
- Pauly J. R., Slotkin T. A. (2008). Maternal tobacco smoking, nicotine replacement and neurobehavioural development. Acta Pædiatr. 97, 1331–1337. [DOI] [PubMed] [Google Scholar]
- Pirani B. B., MacGillivray I. (1978). Smoking during pregnancy. Its effects on maternal metabolism and fetoplacental function. Obstet. Gynecol. 52, 257–263. [PubMed] [Google Scholar]
- Qiao D., Seidler F. J., Tate C. A., Cousins M. M., Slotkin T. A. (2003). Fetal chlorpyrifos exposure: adverse effects on brain cell development and cholinergic biomarkers emerge postnatally and continue into adolescence and adulthood. Environ. Health Perspect. 111, 536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodier P. M. (1988). Structural-functional relationships in experimentally induced brain damage. Prog. Brain Res. 73, 335–348. [DOI] [PubMed] [Google Scholar]
- Slikker W., Xu Z. A., Levin E. D., Slotkin T. A. (2005). Mode of action: disruption of brain cell replication, second messenger, and neurotransmitter systems during development leading to cognitive dysfunction — developmental neurotoxicity of nicotine. Crit. Rev. Toxicol. 35, 703–711. [DOI] [PubMed] [Google Scholar]
- Slotkin T. A. (2008). If nicotine is a developmental neurotoxicant in animal studies, dare we recommend nicotine replacement therapy in pregnant women and adolescents? Neurotoxicol. Teratol. 30, 1–19. [DOI] [PubMed] [Google Scholar]
- Slotkin T. A., Bodwell B. E., Levin E. D., Seidler F. J. (2008). Neonatal exposure to low doses of diazinon: long-term effects on neural cell development and acetylcholine systems. Environ. Health Perspect. 116, 340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotkin T. A., Card J., Stadler A., Levin E. D., Seidler F. J. (2014). Effects of tobacco smoke on PC12 cell neurodifferentiation are distinct from those of nicotine or benzo[a]pyrene. Neurotoxicol. Teratol. 43, 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotkin T. A., Levin E. D., Seidler F. J. (2006a). Comparative developmental neurotoxicity of organophosphate insecticides: effects on brain development are separable from systemic toxicity. Environ. Health Perspect. 114, 746–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotkin T. A., Pinkerton K. E., Seidler F. J. (2006b). Perinatal environmental tobacco smoke exposure in Rhesus monkeys: critical periods and regional selectivity for effects on brain cell development and lipid peroxidation. Environ. Health Perspect. 114, 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotkin T. A., Pinkerton K. E., Tate C. A., Seidler F. J. (2006c). Alterations of serotonin synaptic proteins in brain regions of neonatal Rhesus monkeys exposed to perinatal environmental tobacco smoke. Brain Res. 1111, 30–35. [DOI] [PubMed] [Google Scholar]
- Slotkin T. A., Ryde I. T., Tate C. A., Seidler F. J. (2007). Lasting effects of nicotine treatment and withdrawal on serotonergic systems and cell signaling in rat brain regions: separate or sequential exposure during fetal development and adulthood. Brain Res. Bull. 73, 259–272. [DOI] [PubMed] [Google Scholar]
- Slotkin T. A., Skavicus S., Card J., Stadler A., Levin E. D., Seidler F. J. (2015). Developmental neurotoxicity of tobacco smoke directed toward cholinergic and serotonergic systems: more than just nicotine. Toxicol. Sci. 147, 178–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D., Aherrera A., Lopez A., Neptune E., Winickoff J. P., Klein J. D., Chen G., Lazarus P., Collaco J. M., McGrath-Morrow S. A. (2015). Adult behavior in male mice exposed to e-cigarette nicotine vapors during late prenatal and early postnatal life. PLoS ONE 10, e0137953.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter M. A., Anders A. M., Aagaard K. M. (2013). Maternal smoking as a model for environmental epigenetic changes affecting birthweight and fetal programming. Mol. Hum. Reprod. 19, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres L. H., Garcia R. C. T., Blois A. M. M., Dati L. M. M., Durao A. C., Alves A. S., Pacheco-Neto M., Mauad T., Britto L. R. G., Xavier G. F., et al. (2015). Exposure of neonatal mice to tobacco smoke disturbs synaptic proteins and spatial learning and memory from late infancy to early adulthood. PLoS ONE 10, e0136399.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Surgeon General (2006). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. U.S. Department of Health and Human Services, Rockville. [Google Scholar]
- Yolton K., Dietrich K., Auinger P., Lanphear B. P., Hornung R. (2005). Exposure to environmental tobacco smoke and cognitive abilities among U.S. children and adolescents. Environ. Health Perspect. 113, 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.