Abstract
Our ability to accurately predict development and outcome of early expression of psychosis is limited. To elucidate the mechanisms underlying psychopathology, a broader, transdiagnostic approach that acknowledges the complexity of mental illness is required. The upcoming network paradigm may be fruitful here. In this study, we applied a transdiagnostic network approach to psychosis. Data pertain to the third wave (second follow-up) of a sample of adolescents originally recruited at age 7–8 years. At baseline, N = 347 children with auditory verbal hallucinations (AVH) and N = 347 control children were included. N = 293 of these N = 694 children participated in the second follow-up (mean age 18.9 years; 59% women). Participants completed the Community Assessment of Psychic Experiences (CAPE) and the Depression, Anxiety and Stress Scale (DASS-21). A specific type of network model, the Ising model, was applied to dichotomized CAPE and DASS items. Interconnections of experiences within the same domain were observed, as well as interconnections between experiences of multiple domains of psychopathology. Quantitative and qualitative differences in network architecture were found in networks of psychopathological experiences in individuals with or without AVH at age 7–8 years. Although adolescents with or without previous AVH did not differ in their current CAPE scores, differences in the interconnectedness of psychopathology items were still found, possibly mirroring a difference in psychosis liability. This study showed that it is possible to map transdiagnostic experiences of psychopathology as a network and that important information can be derived from this approach in comparison to regular approaches.
Key words: psychosis, network analysis, transdiagnostic, CAPE, DASS
Introduction
Evidence is lacking that psychopathology exists as natural kinds, ie, as distinct clinical disorders, separated from mental health and each other by natural boundaries.1–3 Instead, there is evidence that psychopathology may be expressed dimensionally.4,5 Continuous (ie, dimensional) expression of symptoms has been shown, eg, for depression, mania, and psychosis.1,6–11 Symptom expression is not diagnosis specific, which may explain why current diagnostic systems are challenged by high levels of comorbidity, extensive clinical heterogeneity, nonspecific treatment effects, and lack of diagnosis-specific biological and/or cognitive markers.1,3–5,12,13
The hypothesized psychosis continuum is assumed to be continuous in both severity and across time.6 As such, psychotic symptoms can be present in the absence of psychotic disorder.6,14,15 Early psychotic symptoms are often investigated as specific predictors of later psychotic disorder16–18; however, this view may be too narrow, as psychotic disorders are also predicted by other symptoms such as depression.19 Furthermore, psychotic symptoms are often transient,18,20 predict later nonpsychotic disorders18,21–23 and manifest in the context of other disorders, such as depression.24,25 This suggests that the expression of psychopathological symptoms, including psychotic symptoms, is more transdiagnostic than previously assumed and that development from mild to more severe states may cross symptom domains. Given that symptoms do not adhere to diagnostic boundaries and do not always develop within a single diagnostic category,26 a case can be made for a broad, transdiagnostic approach to psychopathology, incorporating multiple symptoms domains.27
The disease model underlying current classification systems assumes that symptoms pertain to a smaller set of underlying disorders that cause these symptoms.1,28 However, this may not be the most accurate representation of psychopathology. There has been a shift in focus from disorders to symptoms, circumventing the need for latent constructs “causing” these symptoms.29–31 However, a focus merely on symptoms may be too reductionist,32 as psychopathology may be better conceptualized as a complex system,32,33 where the whole equals more than the sums of its parts. In other words, not only the presence of symptoms per se but also their global interconnectedness and the role of individual nodes in the network are relevant. The network approach hypothesizes that psychopathology results from interactions between symptoms. Mental disorders are represented by sets of symptoms, connected in networks of causal relationships.3,28,29,34–36 Over time, these symptom networks are dynamic, capturing reciprocal influences between symptoms that may fluctuate over time (eg, feedback loops). Here, symptoms are recognized as causal factors in the development of psychopathology: One symptom (eg, anxiety) causes another (eg, paranoia). The network approach has been successfully applied in other fields,37,38 but is relatively novel in psychiatry, where it has been investigated mainly in common mental disorders,29,30,34,39,40 but less in psychosis.36,41
The aim of the current article was to apply network analysis to psychosis from a transdiagnostic perspective. We examined the network structure of experiences of multiple domains of psychopathology (positive psychotic experiences, negative psychotic experiences, depression, anxiety, and stress) in a group of adolescents with and without previous auditory vocal hallucinations (AVH). First, we examined the general network structure of the total sample, 11 years after AVH assessment. Based on previous work on (a) psychotic experiences/symptoms and their comorbidity with other domains42,43,44 and (b) network analysis of psychopathology,28,45 we expected that (1) multidomain psychopathological experiences could be mapped within a complex network structure (ie, experiences within and across domain boundaries would be interrelated), (2) psychopathological experiences would be more often connected to other experiences within the same domain than to experiences pertaining to other domains (eg, low mood would be more often connected to other depressive experiences than to, eg, experiences of anxiety), and (3) positive psychotic experiences would show less within-domain connections than the other domains. Childhood AVH are often transitory46 but may represent an index of liability for psychosis.17,47,48 Therefore, we were interested in comparing the network structure of adolescents with and without childhood AVH to see if the underlying topography of interrelations of experiences may be different in adolescents with and without this liability. We expected that positive psychotic experiences would play a more prominent role (ie, take a more central position) in the network of experiences in adolescents with previous AVH, as evidenced by both quantitative (ie, stronger) and qualitative (ie, more or different) differences in the interconnections between positive psychotic experiences and other psychopathological experiences.
Methods
Networks
A network (or graph) consists of a collection of nodes (vertices) and links (edges). The nodes represent variables of interest (eg, questionnaire items), and the links represent a measure of dependency/association (eg, partial correlations). The edges can be directed (unidirectional effects) or undirected (bidirectional effects), represented, respectively, as an arrow or line. Edges can be unweighted (indicating presence/absence) or have weights representing the strength of the association. In networks of psychopathology, nodes represent experiences/emotions/symptoms. The main advantage of graphical models over other regular analytic techniques such as linear regression49 is the estimation of complex relationships in a collection of random variables. Another advantage is the availability of concepts and tools from graph theory that allows us to analyze estimated networks in multiple ways. As such, graphical modeling provides information on aspects of individual symptoms as well as on the full graph (the system of all symptoms together). There are many software resources for network analyses and visualization, eg, the R-packages igraph (http://igraph.org/r/) and qgraph.50 Networks can be examined at different levels.
Aspects of Individual Nodes in the Network
At the level of individual nodes, a relevant question is which nodes are important (ie, have a more central role in the network), known as node centrality. There are various notions of centrality.51 In an unweighted, undirected network, the degree of a node counts the number of edges incident to that node. In a directed network, we differentiate between in-degree and out-degree, counting the number of incoming and outgoing edges, respectively. When the edges have weights, the degree also accounts for the strength of the edges by summing the absolute value of the weights and is also known as strength. Every node in a network has a degree, so we can characterize a network by looking at its degree sequence. Another notion of node centrality is betweenness. Betweenness centrality of a node is the number of shortest paths between any 2 other nodes that pass through that particular node. A node with high betweenness centrality lies on many shortest paths between other nodes in the network, acting as a kind of “hub” (a node with a degree greatly exceeding the average degree).
Aspects of the Full Network
Information can also be deduced on the full network. For example, we can look for subgraphs within the network. In this case, we look for groups of nodes (also known as communities) that have a strong interdependency. In general, communities are seen as groups of nodes where the groups share few edges between them. Several methods for finding communities exist (see supplementary appendix). Different communities can be connected by so-called “bridge-symptoms”: Individual symptoms that are linked through edges to multiple communities and thus act as a “bridge” of communication between 2 clusters.35 Another example of a network characteristic is the probability distribution of the strength of the nodes. Certain types of network (eg, small-world networks52) have specific governing distributions that can be estimated. A common distribution found in many real-life phenomena53 is the power law distribution. This distribution is based on the mathematical formulation f(x) = axk and has the property that scaling the input of the function results in a proportional scaling of the relationship itself. This is used to identify power law relationships; if a number of points follow a power law relationship, then the log-log plot of x and f(x) should roughly show a straight line. If the distribution of connection strengths would follow a power law, this suggests that the network adheres to a so-called “80/20” rule, meaning that relatively few nodes in the network have a lot more connections than others (“80% of the connections are linked to only 20% of the nodes”).
Sample
Data come from the second follow-up of a sample of adolescents who were originally recruited at age 7–8 years.54 The baseline case–control sample consisted of N = 347 children with AVH and N = 347 matched controls (total N = 694). N = 293 adolescents participated in the second follow-up, where a broad spectrum of psychopathological experiences was assessed. For more details, see ref. Bartels-Velthuis et al46. At baseline, AVH were assessed in a 2-stage procedure. First, children were screened with the question: “In the past year, have you heard one or more voices that only you and no one else could hear?” When answered positively, a structured interview to assess AVH was conducted with the Auditory Vocal Hallucination Rating Scale (AVHRS).55 Control children were selected from the same original population by applying a matching algorithm that took sex, age, and degree of urbanization of the school into account.
Instruments
Networks of psychopathological experiences were based on data from 2 questionnaires indexing a broad symptom spectrum. First, the Community Assessment of Psychic Experiences (CAPE) was completed,43 a 42-item self-report questionnaire assessing mild psychotic experiences that covers 3 subscales: positive psychotic experiences (20 items), negative psychotic experiences (14 items), and depressive feelings (8 items). Each item assesses frequency and associated distress on a 4-point scale. Only frequency items were used. Two items of the positive subscale were strongly interdependent, namely, “hearing voices” and “hearing voices talking to each other.” The latter item was deleted because of multicollinearity. Second, the Depression, Anxiety and Stress Scale (DASS-21) was completed,56 covering 3 subscales: depression (7 items), anxiety (7 items), and distress (7 items). Each item is scored on a 4-point scale. The Depression subscale was excluded because of multicollinearity with the CAPE Depression subscale.
Analyses
The network model that was estimated was the Ising model34 (see supplementary appendix for details on this model and model estimation). The Ising model requires dichotomous data (a symptom is either present or absent) and assumes (among others) that activation of a node is dependent on the activation of its neighboring nodes. We chose this model because (a) it uses a regularization approach, alleviating the fact that there are many items relative to the sample size, (b) model interpretation is intuitively easy to grasp, and (c) given that this field of analysis is relatively novel, we wanted to use a network model that has already been investigated in the area of psychopathology to facilitate the comparison and replicability of results and the Ising model has been used before.34,40,45 For model estimation, data were recoded to 0 as “not present” and 1 as “present.” Other recoding schemes (eg, rescoring both 0 and 1 to 0) were less than optimal, leading to very skewed proportion of 0 vs 1 responses. After fitting the Ising model, we analyzed the resulting network using the qgraph package50 that visualizes graphs and calculates centrality indices. We used the “centrality_auto” function to assess node centrality. Also, we calculated the connectedness per domain by calculating the ratio of the number of actual edges compared the number of possible edges separately for positive psychotic experiences, negative psychotic experiences, depression, anxiety, and stress. Analysis of the full network was done by investigating which nodes form communities, using the function “edge.betweenness.community” from the “igraph” package. We also considered the distribution of the strength of all the nodes and investigate its shape using the poweRlaw package57 (see supplementary appendix for R code).
Example
We compared symptom networks of the 2 original subsamples (ie, children with/without AVH at age 7–8 years) to examine the network structure of a broader spectrum of psychopathological experiences for differences between these 2 groups to provide us with more insights into the underlying mechanisms in individuals with lower or higher liability for psychosis.
Results
Sample
This follow-up was completed by N = 293 children. N = 283 completed the both CAPE and DASS, leaving a final dataset consisting of 55 items in N = 283 children. Mean age was 18.9 (SD 0.4) years, and N = 166 (59%) were female. N = 14 (0.4%) currently reported AVH, as opposed to 50% at baseline. Mean CAPE positive sum score was 4.3 (SD 4.4), mean negative sum score was 8.3 (SD 5.6), and mean depressive sum score was 4.7 (SD 3.4). Mean DASS anxiety score was 2.8 (SD 2.8), and mean stress score was 4.7 (SD 3.9). Response patterns are shown in table 1.
Table 1.
Percentages of Community Assessment of Psychic Experiences (CAPE) and Depression, Anxiety and Stress Scale (DASS) Responses by Subscale
| CAPE | DASS | ||||||
|---|---|---|---|---|---|---|---|
| Positive | Negative | Depression | Total | Anxiety | Stress | Total | |
| Original responses | |||||||
| 0 (never) | 81.8 | 54.7 | 53.3 | 67.0 | 69.0 | 48.8 | 58.9 |
| 1 (sometimes) | 14.6 | 33.7 | 36.2 | 25.3 | 23.4 | 37.5 | 30.4 |
| 2 (often) | 3.0 | 9.4 | 8.4 | 6.2 | 6.2 | 11.1 | 8.6 |
| 3 (almost always) | 0.6 | 2.2 | 2.1 | 1.4 | 1.4 | 2.7 | 2.0 |
| After recoding | |||||||
| 0 (never) | 81.8 | 54.7 | 53.3 | 67.0 | 69.0 | 48.8 | 58.9 |
| 1 (ever) | 18.2 | 45.3 | 46.7 | 33.3 | 31.0 | 51.2 | 41.1 |
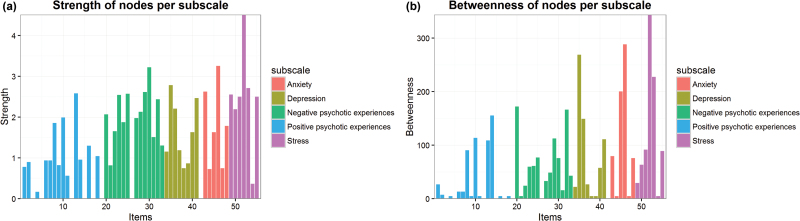
Analysis of Individual Nodes
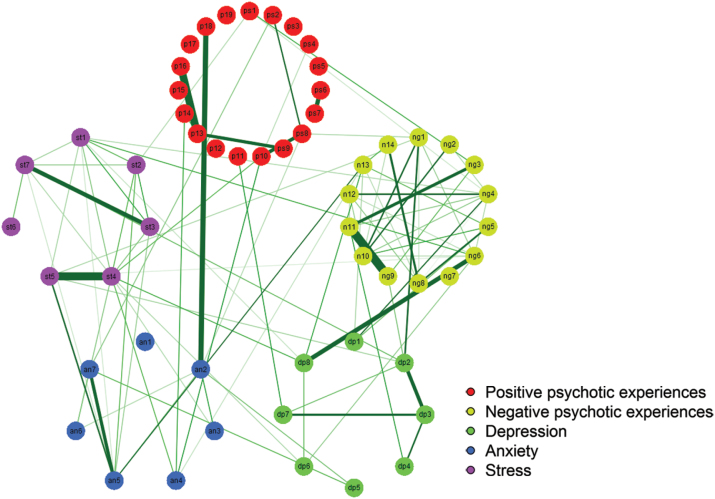
Results of the Ising analysis are shown in figure 1. Labels of the nodes in the network are listed in supplementary table 1. Individual node strength and betweenness are shown in figures 2a and 2b, respectively. Note that because not all nodes lie on a shortest path, some nodes have zero betweenness. Positive psychotic experiences tended to have lower strength compared to the other subscales. Summary statistics of strengths are shown in table 2. Inspecting both figures and the table together, it can be seen that there are many interconnections (a) within each symptom domain and (b) between experiences of different domains. Strong within-domain links that stand out were seen between “feelings lacking intensity” and “feelings are blunted” within negative psychotic experiences and between “using a lot of nervous energy” and “feeling touchy” and between “feeling agitated” and “finding it difficult to relax” when experiencing stress. Within positive psychotic experiences, a strong link was observed between the items “thoughts in your head are not your own” and “feeling under external control.” Especially negative psychotic experiences and stress show a strong within-domain interconnectedness, also expressed in their high values of connection strengths. Also, as indicated by the high betweenness values, these experiences were often on pathways between other experiences. Thus, they play a very central role in the interconnections of the full symptom network. When examining connections between experiences of different domains, strong links are observed between the negative item of “feeling that you are lacking in energy” and the depression item of “feeling tense.” Another strong link was seen between the anxiety item of “experiencing breathing difficulty” and the positive psychotic item of “doppelganger.”
Fig. 1.
Representation of network model of Community Assessment of Psychic Experiences (CAPE) and Depression, Anxiety and Stress Scale (DASS) items.
Fig. 2.
Strength and betweenness of nodes per subscale.
Table 2.
Mean Node Strength of the 5 Subscales
| Strength | Mean | Variance | Median |
|---|---|---|---|
| Positive psychotic experiences | 0.78 | 0.58 | 0.82 |
| Negative psychotic experiences | 1.91 | 0.68 | 2.02 |
| Depressive feelings | 1.63 | 0.59 | 1.41 |
| Anxiety | 1.54 | 1.31 | 1.63 |
| Stress | 2.47 | 1.45 | 2.50 |
When comparing the connectedness within the 5 subdomains, positive psychotic experiences showed the lowest within-domain connectedness (ratio of number of actual edges vs the number of possible edges of 0.047) followed by depressive experiences (ratio 0.179). Experiences of stress had the highest connectedness (ratio 0.619). The connectedness of negative psychotic experiences (ratio 0.247) and of experiences of anxiety (ratio 0.286) was comparable. This means that positive psychotic experiences were less connected to each other than experiences of other psychopathological domains and that experiences of stress were more connected to each other.
In total, 101 edges were identified in the network. Of these, 56 edges were within-domain edges (eg, a depressive item connected to another depressive item) and 45 were between-domain edges (eg, a depressive item connected to an anxiety item). Thus, there were more within-domain connections than between-domain connections.
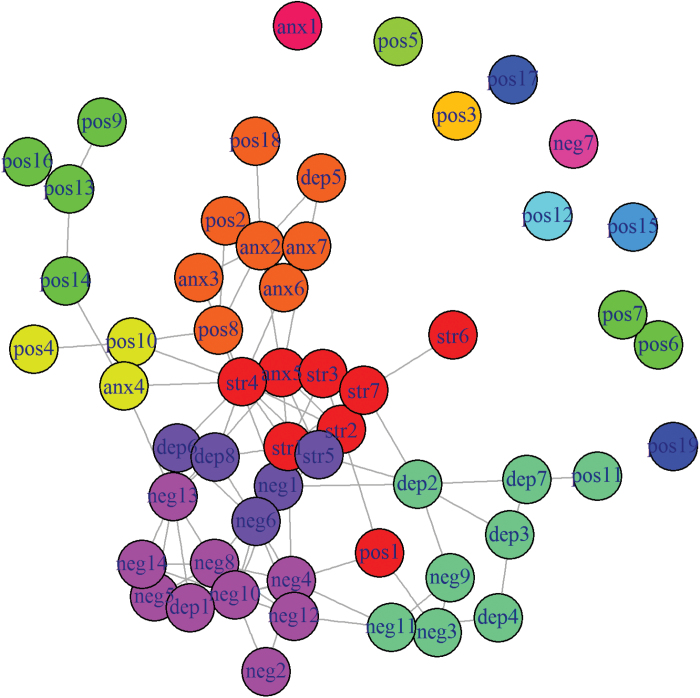
Analysis of the Full Network
We found 6 large communities. Grouping of the items into these communities is listed in table 3 and visualized in figure 3. Two smaller communities were found, with, respectively, 3 or 4 experiences. The other 4 communities contained larger groups of items. Only 1 community (community 5) consisted of items all belonging to the same domain (positive psychotic experiences). The other communities were a mix of experiences of multiple domains, although often experiences pertaining to 1 domain were “dominant” (eg, in community 2, the vast majority of items pertain to negative psychotic experiences). There were various items that were not connected to any community, meaning that they were not detected by this specific community-detection algorithm as belonging particularly to any of the communities. Thus, these items are less likely to co-occur with other items. Items of different communities that share an edge serve as a bridge between 2 communities (referred to in the literature as “bridge-symptoms,” a term we will also use here even though we in general speak about experiences instead of symptoms). One such bridge-symptom is the item “I worried about situations in which I might panic,” connected to 3 other communities outside its own. This item thus refers to a crucial experience in terms of spreading of activity: Whenever this particular symptom is present, the chance that other communities of experiences also are activated (ie, the chance of comorbidity) increases. This chance of coactivation is less when non-bridge-symptoms are activated.
Table 3.
Grouping of Items Into 6 Communities
| Item | Domain | 1 (yellow) | 2 (light purple) | 3 (dark purple) | 4 (red) | 5 (green) | 6 (orange) | 7 (mint green) |
|---|---|---|---|---|---|---|---|---|
| Being persecuted | Positive | x | ||||||
| Believe in occult | Positive | x | ||||||
| Worried about panic | Anxiety | x | ||||||
| Not much of a talker | Negative | x | ||||||
| No interest in people | Negative | x | ||||||
| Lacking motivation | Negative | x | ||||||
| Spending days doing nothing | Negative | x | ||||||
| Lacking spontaneity | Negative | x | ||||||
| Neglecting hygiene | Negative | x | ||||||
| Never get things done | Negative | x | ||||||
| Few hobbies or interests | Negative | x | ||||||
| Feel sad | Depressive | x | ||||||
| Not a very animated person | Negative | x | ||||||
| Lacking in energy | Negative | x | ||||||
| Feel guilty | Depressive | x | ||||||
| Feel tense | Depressive | x | ||||||
| Difficult to relax | Stress | x | ||||||
| Hard to wind down | Stress | x | ||||||
| Over-react to situations | Stress | x | ||||||
| Using a lot of nervous energy | Stress | x | ||||||
| Getting agitated | Stress | x | ||||||
| Intolerant of anything | Stress | x | ||||||
| Rather touchy | Stress | x | ||||||
| Close to panic | Anxiety | x | ||||||
| Double meaning | Positive | x | ||||||
| Electrical devices | Positive | x | ||||||
| Thoughts in your head | Positive | x | ||||||
| Vivid thoughts | Positive | x | ||||||
| Under control of force | Positive | x | ||||||
| Things in magazines or on TV | Positive | x | ||||||
| Communicate telepathically | Positive | x | ||||||
| Doppelganger | Positive | x | ||||||
| Breathing difficulty | Anxiety | x | ||||||
| Experienced trembling | Anxiety | x | ||||||
| Over-react to situations | Anxiety | x | ||||||
| Scared without reason | Anxiety | x | ||||||
| Cry about nothing | Depressive | x | ||||||
| Pessimistic about everything | Depressive | x | ||||||
| No future | Depressive | x | ||||||
| Do not want to live anymore | Depressive | x | ||||||
| Feel like a failure | Depressive | x | ||||||
| No emotions at important events | Negative | x | ||||||
| Feelings lacking intensity | Negative | x | ||||||
| Emotions are blunted | Negative | x | ||||||
| Look oddly appearance | Positive | x |
Note: As not all nodes are grouped into communities (some items are isolated, as shown in figure 3), not all items are in this table.
Fig. 3.
Grouping of Community Assessment of Psychic Experiences (CAPE) and Depression, Anxiety and Stress Scale (DASS) items in communities.
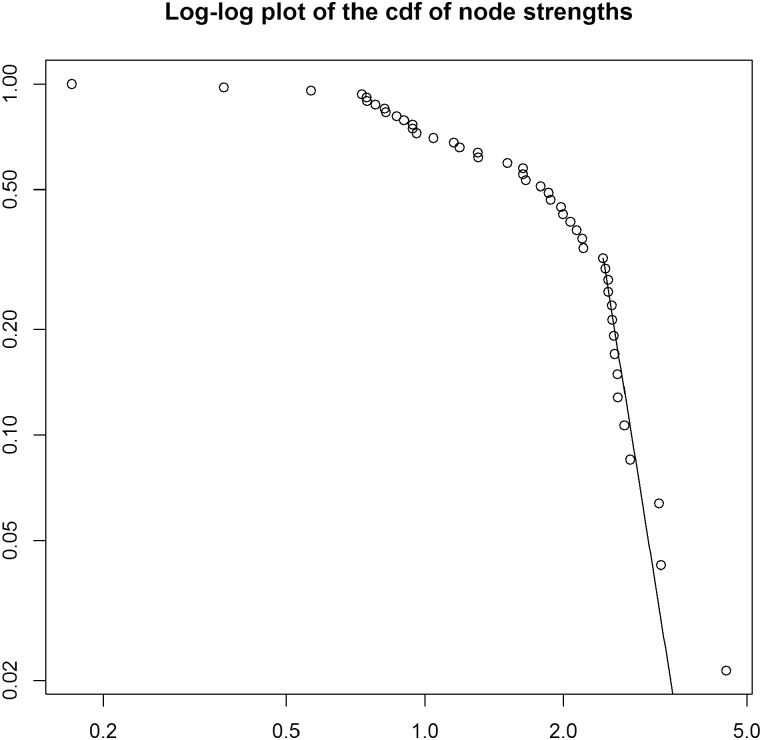
Power Law
The log-log plot of the cumulative distribution function of the data as well as a line representing a power law is presented in figure 4. To assess goodness-of-fit, we followed a bootstrap procedure.58 This resulted in P = .815, indicating that a power law of the node strengths cannot be ruled out. However, because the sample is rather small (48 nodes with nonzero strength), this test is not conclusive.
Fig. 4.
Log-log plot of node strengths.
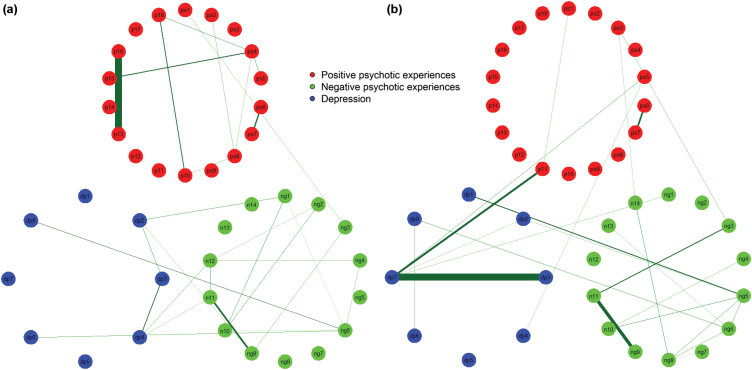
Example
We compared 2 networks of multiple-domain psychopathological experiences in the 2 original subgroups of the sample, namely, individuals with/without AVH at age 7–8 years (figure 5). Although the N = 14 individuals with current AVH scored higher on both CAPE and DASS,46 the original 2 subgroups differed only in DASS anxiety score in the current follow-up (AVH = 3.4, SD 3.2; no AVH = 2.2, SD 2.2; P < .001). As the groups became much smaller, the ratio of number of nodes (experiences) to number of participants became unfavorable for model estimation. To reduce the number of items, we used only the CAPE dimensions, leaving out the DASS. The item on “hearing voices” was excluded for both subgroups, as this is the defining experience that originally differed between subgroups. More connections between positive psychotic experiences and fewer connections between depressive feelings were seen in individuals with AVH. The number of connections between negative psychotic experiences was comparable, but qualitatively different, as different items were connected. Interestingly, the depressive and negative dimensions are closely interconnected in both subgroups but even more strongly in individuals without AVH. Individuals without previous AVH had a strong connection between “feeling like a failure” and “feeling there is no future for me”; individuals with previous AVH had a strong connection between “feeling that thoughts in your head are not your own” and “feeling under external control.”
Fig. 5.
Networks of Community Assessment of Psychic Experiences (CAPE) items for individuals with/without auditory verbal hallucinations at age 7–8 years.
Discussion
We applied a network approach to psychopathology in adolescents, originally recruited as a matched case–control sample of children with/without AVH at age 7–8 years. An important aspect of the study was the transdiagnostic approach, incorporating experiences from multiple domains of psychopathology,3 namely, positive psychotic experiences, negative psychotic experiences, depression, anxiety, and distress. As hypothesized, we found that it was possible to map a complex network of multidomain psychopathological experiences. Also, we found that, although psychopathological experiences showed more connections within each domain than between the different domains, experiences of different domains were closely connected and that positive psychotic experiences were the least connected. Although the adolescents with or without previous AVH did not differ in their scores on the CAPE at the current measurement, differences in the interconnectedness of experiences were still found, possibly reflecting a network characteristic indexing psychosis liability. These differences pertained to the number and nature of the experiences as well as to the strength of the connections.
Our results show that it is possible to map multidimensional experiences as a network and that examination of interconnectedness of experiences provides information that cannot be easily distilled from composite scores, eg, correlations of sum scores.28,39 This was seen within each domain, as not all experiences connected to each other in similar ways. For example, the stress item “using a lot of nervous energy” was connected to many other stress items, and thus formed a more central symptom in the network compared to the item of the same domain “intolerance for distraction” that was only connected to one other stress item. Negative psychotic experiences showed the most interconnections, whereas positive psychotic experiences showed the least. Also, positive psychotic experiences showed the lowest within-domain connectedness (ie, were least often connected to other experiences in the same domain). This suggests that positive psychotic experiences are more “independent” than other psychopathological experiences, in that their presence in itself does not necessarily trigger the activation of other symptom domains. This could be in line with the notion of psychotic experiences as a relative independent “index of severity” that can be copresent in all other psychopathology domains.59 This difference in connectivity may be partly explained by the higher mean scores of the negative domain. However, the difference in mean score does not explain all: Although mean item scores were similar for negative and depressive experiences, negative experiences were more interconnected, reflected in more edges and higher mean edge strength. This is in line with a recent study showing that, in a network of psychopathological experiences, the prevalence of experiences was not associated with the number of connections, although they did find some evidence that floor effects may occur in case of less-frequent experiences.45 Thus, shifting the focus from experiences or symptoms per se to the dynamics between symptoms seems to yield important information, as it allows us to examine roles and/or contributions of individual items. This is important, as different symptoms may play different roles for different patients and this may affect treatment choice and response.
Besides within-domain interconnections, we also observed many interconnections between multiple domains of psychopathology. In line with previous work,45 more within-domain connections were found than between-domain connections. Studying these interconnections provides more detailed information than a correlation of sum scores: It specifically shows how 2 specific experiences are associated, facilitating development of targeted interventions. The many domain-crossing links, especially between depressive and negative experiences, underline the need to work cross-diagnostically and to examine the relationship of symptom (domains) not only within a single diagnostic construct but also in relation to other symptom (domains). This is especially important when addressing the development of psychopathology, as the level of boundary-crossing may change with phase of illness.60
In addition to information on individual experiences, network analysis also yields important information on the full network, ie, the whole system of experiences together. The (suggested) presence of a power law may indicate that the symptom network acts as a scale-free network, and may have some of its characteristics such as the presence of hubs.35,38 Hubs have central positions in a network and therefore may be ideal for targeted intervention. In the network of the total sample, the item “getting agitated” had the highest strength and thus might qualify as a “hub.” Targeting specifically agitation in treatment may then influence the dynamics of all other symptoms, as the network model assumes direct influence between individual nodes.26
The presence of different communities demonstrates alternative ways of grouping experiences than according to their original domain, providing information on patterns of co-occurrence. Some clusters still capture experiences of 1 domain, eg, cluster 5 only consists of positive psychotic experiences. However, other clusters (eg, clusters 3 and 6) encompass experiences from 3 or 4 domains. One cluster of experiences, eg, shows that some positive psychotic experiences co-occur with specific anxiety experiences. This could alert clinicians on the possible copresence of psychotic experiences when assessing anxiety and may guide intervention strategies in a way that considers dynamic relationships between anxiety and psychosis. These findings also show that not all experiences may have equal roles in clinical presentation. Apparently, certain positive psychotic experiences (eg, “feeling under control of an external force”) are more likely to co-occur with other positive psychotic experiences than others (eg, “feeling persecuted”). These nuances would not have been detected with regular approaches using sum scores.
Identifying communities also helps us to identify bridge-symptoms35 that may play an important role in understanding the spreading of activation through a network. As bridge-symptoms are relatively easy to connect to all other nodes in a network, they have a relatively strong influence on the global structure of the network.35 For example, if a patient reports only non-bridge-symptoms within one cluster, the chances of coactivation of other symptom clusters (communities) is smaller than when a patient does report a bridge-symptom of this symptom community, as the presence of this symptom also increases the chances of activation of the other symptoms in the community that the bridge-symptom is connected to. Similar to identifying hubs, identifying bridge-symptoms could be an important goal for clinicians to guide treatment: Targeting a bridge-symptom could prevent spreading of activation throughout the symptom network and could potentially limit or prevent the presence of comorbidity.
Comparing symptom networks of different populations may reveal interesting information regarding (differences in) the development of psychopathology. Ideally, networks of individuals with/without current AVH would have been compared; however, this was impossible due to the small number of individuals with current AVH. Still, comparing the original subgroups yielded interesting information. Even though adolescents with and without previous AVH scored equally high on positive and negative psychotic experiences, as well as on depression, both qualitative and quantitative differences in network structure between the groups were apparent. These differences in network architecture could thus not be explained by current differences in CAPE sum scores. Analyses showed, eg, that in the group with previous AVH, positive psychotic experiences were more interconnected compared to the group without previous AVH, which could be expected. Interestingly, the group without previous AVH showed more interdomain connections of positive psychotic experiences with both other domains than the group with previous AVH. More detailed examination revealed that the nature of the experiences in the interdomain connections was very different: For example, in the group without previous AVH, the “milder” item of “feeling that people are not what they seem to be” was linked to the (negative) item of “having few interests or hobbies,” whereas in the group with previous AVH, items that were linked with other items were, among others, “feeling under control of an external force,” “seeing things that others do not,” and “hearing your thoughts being echoed back.” These items seem comparatively more “severe.” Again, these nuances at the level of individual items would be lost if plain correlations between the domains would be compared across the 2 groups. Apparently, dynamics between mental experiences have different patterns in individuals who as children had lived experience of psychosis. This may suggest that in individuals with a higher liability for psychosis, interconnectedness between symptoms may be different. Mapping the dynamics between experiences of early psychopathology may help to better understand the ontogenesis of clinical disorders.
Applying the network approach to psychopathology is an exciting new avenue for psychiatric research, as it offers us a new array of tools to examine experiences and symptoms. It allows a focus on the role of individual symptoms and on the dynamics between symptoms. Also, it is very well suited to model psychopathology transdiagnostically. However, some criticisms may be brought to bear on the methodology presented in this article. Although the network approach is conceptually intuitive and attractive in various areas of science, its applicability in psychopathology, as well as its ability to generate replicable results, is still in its infancy. Clearly, more empirical research is needed. Most work to date is cross sectional in nature, often pertaining to (partial) correlations and leaving questions concerning causality, undersampling, and dynamic associations between symptoms over time unanswered. Another complication concerns the choice for a particular network model. A variety of statistical models exist that attempt to uncover network structures between variables, and it is currently not clear which model is appropriate for a given set of research questions. The Ising model makes a number of assumptions, one of the most notable being one that assumes all variables in the network have a “preferred” state. The exact interpretation of this in the context of psychopathology is not clear yet. The inclusion and interpretation of covariates in a network, while mathematically trivial, is also an open matter of research. Moreover, a wide variety of mathematical tools exist, and it is not certain which specific characteristics of a network are relevant to analyze. Most research so far (including the current work) has focused on mapping the network structure of a given set of psychopathological symptoms. However, the true challenge lies in the exploration of the question whether certain network characteristics are able to predict outcome measures of interest, such as developmental course or clinical/functional outcome. Also, it is not known to what degree network models are suitable to describe group tendencies, given the highly individual nature of symptom dynamics that may require a within-person design rather than a between-person design. Also, it is important to keep in mind that network analysis is a tool for understanding psychopathology. As with all theoretical paradigms, the network approach is a(nother) model that we use to attempt to better understand psychopathology, and it cannot provide “the” answer to existing questions. Thorough validation of the model, especially in terms of predictive validity of course and outcome of network parameters, is necessary to better estimate the value of this approach.
The current article is, to our knowledge, one of the first to examine the interconnectedness of psychotic experiences with other domains of psychopathology. Although half of the sample reported AVH at baseline, the current wave included only a minority of individuals with AVH. Still, the nature of this sample and the fact that the current analyses were secondary to the original research question should be kept in mind when interpreting the results, and replication is necessary. In particular, the division of the subgroups of adolescents with/without previous AVH should be kept in mind and future studies may want to assess subgroups that are based on different criteria. We discussed network aspects that were of interest for the current data; however, our choices inevitably represent a selection of all possibilities. The current article used cross sectional data, and thus, no conclusions can be drawn regarding causality of associations. This article analyzed network structures at the group level. For individualized networks of symptoms that may eventually contribute to personalized medicine and treatment,61 investigating dynamic,62 intraindividual networks over time is necessary. As the network approach in psychiatry is relatively new, current work (including this article) is often more hypothesis-generating in nature. In future research, specific hypotheses should be tested; eg, parameters derived from network analysis could be used to predict important variables, such as course or outcome of early psychopathology. This, eventually, may help to tailor treatment that is better matched to individual needs.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
Stichting tot Steun VCVGZ (Foundation for Support, Christian Union for Care of Mentally Ill); Bensdorp Fund; Maastricht University Medical Centre; Rob Giel Research Center; European Community’s Seventh Framework Program (HEALTH-F2-2009-241909 [Project EU-GEI]); Netherlands Organization for Scientific Research (NWO)-Veni Grant (016.156.019 to J.T.W.W.); NWO-ASPASIA grant (to M.W.); NWO-VICI grant (91812607 to S.d.V. and received by Peter de Jonge).
Supplementary Material
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160:4–12. [DOI] [PubMed] [Google Scholar]
- 2. Frances AJ, Widiger T. Psychiatric diagnosis: lessons from the DSM-IV past and cautions for the DSM-5 future. Annu Rev Clin Psychol. 2012;8:109–130. [DOI] [PubMed] [Google Scholar]
- 3. Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychol Med. 2011;41:1143–1150. [DOI] [PubMed] [Google Scholar]
- 4. Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the diagnostic and statistical manual of mental disorders. J Abn Psychol. 2005;114:494. [DOI] [PubMed] [Google Scholar]
- 5. Widiger TA. A dimensional model of psychopathology. Psychopathology. 2005;38:211–214. [DOI] [PubMed] [Google Scholar]
- 6. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. [DOI] [PubMed] [Google Scholar]
- 7. Haslam N, Holland E, Kuppens P. Categories versus dimensions in personality and psychopathology: a quantitative review of taxometric research. Psychol Med. 2011;1:1–18. [DOI] [PubMed] [Google Scholar]
- 8. Kendler KS, Gardner CO., Jr Boundaries of major depression: an evaluation of DSM-IV criteria. Am J Psychiatry. 1998;155:172–177. [DOI] [PubMed] [Google Scholar]
- 9. Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rössler W. Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J Affect Disord. 2003;73:133–146. [DOI] [PubMed] [Google Scholar]
- 10. Carter RM, Wittchen HU, Pfister H, Kessler RC. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety. 2001;13:78–88. [DOI] [PubMed] [Google Scholar]
- 11. Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behav Res Ther. 2002;40:485–499. [DOI] [PubMed] [Google Scholar]
- 12. Hyman SE. The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol. 2010;6:155–179. [DOI] [PubMed] [Google Scholar]
- 13. Kupfer DJ, First MB, Regier DA. A Research Agenda for DSM V. Washington, DC: American Psychiatric Association; 2008. [Google Scholar]
- 14. McGorry PD, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40:616–622. [DOI] [PubMed] [Google Scholar]
- 15. Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull. 1996;22:283–303. [DOI] [PubMed] [Google Scholar]
- 16. Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC. Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol. 1994;103:171–183. [DOI] [PubMed] [Google Scholar]
- 17. Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. [DOI] [PubMed] [Google Scholar]
- 18. Kaymaz N, Drukker M, Lieb R, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. 2012;42:2239–2253. [DOI] [PubMed] [Google Scholar]
- 19. Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67:131–142. [DOI] [PubMed] [Google Scholar]
- 20. Fusar-Poli P, Yung A, McGorry P, van Os J. Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med. 2013:1–8. [DOI] [PubMed] [Google Scholar]
- 21. Fusar-Poli P, Bonoldi I, Yung AR, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–229. [DOI] [PubMed] [Google Scholar]
- 22. Werbeloff N, Drukker M, Dohrenwend BP, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. 2012;69:467–475. [DOI] [PubMed] [Google Scholar]
- 23. Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR. Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry. 2015;172:249–258. [DOI] [PubMed] [Google Scholar]
- 24. Perlis RH, Uher R, Ostacher M, et al. Association between bipolar spectrum features and treatment outcomes in outpatients with major depressive disorder. Arch Gen Psychiatry. 2011;68:351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wigman J, van Os J, Abidi L, et al. Subclinical psychotic experiences and bipolar spectrum features in major depressive disorder: association with outcome of psychotherapy. Psychol Med. 2014;44:325–336. [DOI] [PubMed] [Google Scholar]
- 26. Cramer AO, Waldorp LJ, van der Maas HL, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33:137–150; discussion 150. [DOI] [PubMed] [Google Scholar]
- 27. Borsboom D, Epskamp S, Kievit RA, Cramer AO, Schmittmann VD. Transdiagnostic networks: commentary on Nolen-Hoeksema and Watkins (2011). Perspect Psychol Sci. 2011;6:610–614. [DOI] [PubMed] [Google Scholar]
- 28. Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. [DOI] [PubMed] [Google Scholar]
- 29. Borsboom D, Cramer AO, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS One. 2011;6:e27407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bringmann LF, Vissers N, Wichers M, et al. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One. 2013;8:e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wigman JTW, van Os J, Borsboom D, et al. Exploring the underlying structure of mental disorder: cross-diagnostic differences and similarities from a network perspective using both a top-down and a bottom-up approach. 2015;45:2375–2387. [DOI] [PubMed] [Google Scholar]
- 32. Barabási A. The network takeover. Nat Phys. 2011;8:14. [Google Scholar]
- 33. Buckholtz JW, Meyer-Lindenberg A. Psychopathology and the human connectome: toward a transdiagnostic model of risk for mental illness. Neuron. 2012;74:990–1004. [DOI] [PubMed] [Google Scholar]
- 34. van Borkulo CD, Borsboom D, Epskamp S, et al. A new method for constructing networks from binary data. Sci Rep. 2014;4:5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Goekoop R, Goekoop JG. A network view on psychiatric disorders: network clusters of symptoms as elementary syndromes of psychopathology. PLoS One. 2014;9:e112734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vinogradov S, King RJ, Huberman BA. An associationist model of the paranoid process: application of phase transitions in spreading activation networks. Psychiatry. 1992;55:79–94. [DOI] [PubMed] [Google Scholar]
- 37. Newman M. Networks: An Introduction. Oxford, UK: Oxford University Press; 2010. [Google Scholar]
- 38. Barabási A, Frangos J. Linked: The New Science of Networks Science of Networks. New York, NY: Basic Books; 2002. [Google Scholar]
- 39. Fried EI, Nesse RM. Depression sum-scores don’t add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One. 2015;10:e0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Isvoranu A, Borsboom D, van Os J, Guloksuz S. A network approach to environmental impact in psychotic disorder: brief theoretical framework [published online ahead of print May 13, 2016]. Schizophr Bull. doi:10.1093/schbul/sbw049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35:383–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stefanis NC, Hanssen M, Smirnis NK, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002;32:347–358. [DOI] [PubMed] [Google Scholar]
- 44. Shevlin M, Murphy J, Dorahy MJ, Adamson G. The distribution of positive psychosis-like symptoms in the population: a latent class analysis of the National Comorbidity Survey. Schizophr Res. 2007;89:101–109. [DOI] [PubMed] [Google Scholar]
- 45. Boschloo L, Schoevers RA, van Borkulo CD, Borsboom D, Oldehinkel AJ. The network structure of psychopathology in a community sample of preadolescents. J Abnorm Psychol. 2016;125:599–606. [DOI] [PubMed] [Google Scholar]
- 46. Bartels-Velthuis A, Wigman J, Jenner J, Bruggeman R, van Os J. Course of auditory vocal hallucinations in childhood: 11-year follow-up study. Acta Psychiatr Scand. 2016;134:6–15. [DOI] [PubMed] [Google Scholar]
- 47. Welham J, Scott J, Williams G, et al. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychol Med. 2009;39:625–634. [DOI] [PubMed] [Google Scholar]
- 48. Polanczyk G, Moffitt TE, Arseneault L, et al. Etiological and clinical features of childhood psychotic symptoms: results from a birth cohort. Arch Gen Psychiatry. 2010;67:328–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Koller D, Friedman N, Getoor L, Taskar B. Graphical models in a nutshell. Statistical Relational Learning. Getoor L, Taskar B, eds. Cambridge, MA: The MIT Press; Chapter 2; 2007. [Google Scholar]
- 50. Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: Network Representations of Relationships in Data. R package version 0.4. 2011:10. [Google Scholar]
- 51. Costantini G, Epskamp S, Borsboom D, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Personality. 2015;54:13–29. [Google Scholar]
- 52. Watts DJ, Strogatz SH. Collective dynamics of ‘small-world’ networks. Nature. 1998;393:440–442. [DOI] [PubMed] [Google Scholar]
- 53. Newman ME. Power laws, Pareto distributions and Zipf’s law. Contemp Phys. 2005;46:323–351. [Google Scholar]
- 54. Bartels-Velthuis AA, Jenner JA, van de Willige G, van Os J, Wiersma D. Prevalence and correlates of auditory vocal hallucinations in middle childhood. Br J Psychiatry. 2010;196:41–46. [DOI] [PubMed] [Google Scholar]
- 55. Jenner JA, van de Willige G. The Auditory Vocal Hallucination Rating Scale (AVHRS). Groningen, The Netherlands: University Medical Center Groningen, University Center for Psychiatry, University of Groningen; 2002. [Google Scholar]
- 56. Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239. [DOI] [PubMed] [Google Scholar]
- 57. Gillespie CS. Fitting Heavy-tailed Distributions: The poweRlaw Package. R package version 0.20.5; 2014. [Google Scholar]
- 58. Clauset A, Shalizi CR, Newman ME. Power-law distributions in empirical data. SIAM Rev. 2009;51:661–703. [Google Scholar]
- 59. Kelleher I, Keeley H, Corcoran P, et al. Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry. 2012;201:26–32. [DOI] [PubMed] [Google Scholar]
- 60. McGorry P, van Os J. Redeeming diagnosis in psychiatry: timing versus specificity. Lancet. 2013;381:343–345. [DOI] [PubMed] [Google Scholar]
- 61. van Os J, Delespaul P, Wigman J, Myin-Germeys I, Wichers M. Beyond DSM and ICD: introducing “precision diagnosis” for psychiatry using momentary assessment technology. World Psychiatry. 2013;12:113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Odgers CL, Mulvey EP, Skeem JL, Gardner W, Lidz CW, Schubert C. Capturing the ebb and flow of psychiatric symptoms with dynamical systems models. Am J Psychiatry. 2009;166:575–582. [DOI] [PubMed] [Google Scholar]
- 63. Kindermann R, Snell JL. Markov Random Fields and Their Applications. Vol 1 Providence, RI: American Mathematical Society; 1980. [Google Scholar]
- 64. Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc B (Methodol). 1996:58:267–288. [Google Scholar]
- 65. Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. Adv Neural Inform Proc Syst. 2010;23:604–612. [Google Scholar]
- 66. Girvan M, Newman ME. Community structure in social and biological networks. Proc Natl Acad Sci USA. 2002;99:7821–7826. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.