Abstract
Hearing voices that are not present is a prominent symptom of serious mental illness. However, these experiences may be common in the non-help-seeking population, leading some to propose the existence of a continuum of psychosis from health to disease. Thus far, research on this continuum has focused on what is impaired in help-seeking groups. Here we focus on protective factors in non-help-seeking voice-hearers. We introduce a new study population: clairaudient psychics who receive daily auditory messages. We conducted phenomenological interviews with these subjects, as well as with patients diagnosed with a psychotic disorder who hear voices, people with a diagnosis of a psychotic disorder who do not hear voices, and matched control subjects (without voices or a diagnosis). We found the hallucinatory experiences of psychic voice-hearers to be very similar to those of patients who were diagnosed. We employed techniques from forensic psychiatry to conclude that the psychics were not malingering. Critically, we found that this sample of non-help-seeking voice hearers were able to control the onset and offset of their voices, that they were less distressed by their voice-hearing experiences and that, the first time they admitted to voice-hearing, the reception by others was much more likely to be positive. Patients had much more negative voice-hearing experiences, were more likely to receive a negative reaction when sharing their voices with others for the first time, and this was subsequently more disruptive to their social relationships. We predict that this sub-population of healthy voice-hearers may have much to teach us about the neurobiology, cognitive psychology and ultimately the treatment of voices that are distressing.
Key words: hallucinations, schizotypy, continuum, distress, control, phenomenology
Introduction
The positive symptoms of psychosis (hallucinations and delusions, amongst others) may be present in the general, non-help-seeking population.1–7 They may not be pathognomonic of serious mental illness, but rather, there could be a continuum from milder attenuated forms to more severe.8 Such observations suggest a destigmatization of anomalous perceptions and beliefs.1 The impact of these observations on research practice has been extensive.2–7,9–12 However, these observations have not yet changed clinical practice.13 Indeed, some are skeptical whether they even can.13 There is considerable overlap between clinical and nonclinical psychosis-like experiences,13 making it difficult to discern which warrant intervention and which do not.13 People with a diagnosed psychotic illness tend to be significantly more distressed by their atypical experiences than those who do not, despite similar assent, conviction, and preoccupation.11 However, this has yet to be converted into new therapeutic approaches.13 Here we consider what may protect nonclinical voice hearers, inspired by similar studies in addiction,14 oncology,15 and infectious diseases16,17: there are individuals who are resilient despite similar exposure to risk factors as individuals who become ill.
We identify a new population—clairaudient psychics—who report receiving auditory messages from other realms. Psychics have long concerned the American Society for Psychical Research and such luminaries as William James, Pierre Janet, and Wilhelm Wundt,18 whose interests lay in testing the veracity of psychics’ claims. Just as we do not do this with our patients’ claims regarding the provenance of their voices, we are not interested in debunking the psychics. Rather, we study clairaudient psychics much as Garety and Peters studied druids to better understand the distinction between anomalous belief and delusion.11
Clairaudience, in the parlance of spiritualist communities, involves receiving auditory messages from spirits (as opposed to clairvoyance, which entails visions). We compared the phenomenology of voices in self-proclaimed clairaudient psychics to those of patients with a psychotic illness who have auditory hallucinations. Good overlap could be grounds to conclude that these psychics are not malingering with regard to having voice-hearing experiences. Understanding the differences may provide insights into problematic voice-hearing.
Non-help-seeking voice-hearers have relatively intact verbal and executive functioning,19 though the neural circuitry engaged during voice hearing experiences appears to be broadly similar.20 Numerous studies have highlighted important differences in the emotional valence and content of voice experiences, as well as the explanatory schema evoked.21,22 Some individuals in these prior studies would, undoubtedly, describe themselves as clairaudient psychics. However, non-help-seeking voice hearers evoke a range of explanatory frameworks.21 Here, we focus, for the first time, on just 1 sub-group: clairaudient psychics. We aim to understand how and in what way their voices can be positive, life-affirming experiences.
Methods
Four groups of participants were recruited: (1) voice-hearers with a diagnosable psychotic disorder (P+H+; n = 16); (2) voice-hearers without a diagnosable psychotic disorder (clairaudient psychics, P−H+; n = 17); (3) non-voice-hearers with a diagnosable psychotic disorder (P+H−; n = 16); and (4) non-voice-hearers without a diagnosable psychotic disorder (P−H−; n = 18). Subjects were recruited via local advertisement and word of mouth. Some patients were referred to the study through their clinicians at the Connecticut Mental Health Center (CMHC). Clairaudient psychics were self-identified as such on websites and/or at local psychic meetings and were recruited through discussions held at these meetings and referrals from other psychics. All potential subjects were telephone screened. If they met inclusion criteria they were invited for an in-person interview at the CMHC. Exclusion criteria for all participants were as follows: (1) any neurological disorder or head trauma resulting in loss of consciousness or sustained deficits; (2) any recreational drug or alcohol use meeting criteria for at-risk drinking (>2 drinks/d or 14 drinks/wk for males, >1 drink/d or 7 drinks/wk for females) for 1 month prior to enrollment; (3) left-handedness; and (4) self-reported abnormal hearing or vision. Voice-hearing participants had to report auditory hallucinations at least once per day. Non-voice-hearing participants must have had no voice-hearing experiences for at least 6 months prior to enrollment. Of the recruited non-voice-hearing participants with a diagnosable psychotic disorder, 69% (11/16) had no prior voice-hearing experiences. Of those who did, a mean of 8.0 years (±4.9, SD; min: 1 y, max: 15 y) had elapsed since their last voice-hearing experience, most of which (4/5) were reported to have occurred in the time surrounding their first psychotic episode. Non-treatment-seeking voice-hearers were required to be antipsychotic-naive and not in treatment of any psychiatric issue, and upon further screening could not have a diagnosable Axis I disorder; no participants were excluded after interview for this reason. Healthy control participants also had no diagnosable Axis I disorder.
All participants had the opportunity to read and discuss the consent form. All gave written informed consent before participating. All procedures were approved by the Yale University Human Investigations Committee. Participants completed a series of pen-and-paper questionnaires and underwent a semi-structured interview, including standard psychiatric ratings scales. Some participants went on to participate in a functional neuroimaging study (data reported elsewhere). Here we report findings from the following questionnaires and rating scales:
Positive and Negative Syndrome Scale (PANSS)23: to assess for and quantify positive and negative psychotic symptoms in both help-seeking and non-help-seeking populations.
Structured Clinical Interview for DSM-4 (SCID) Axis I Disorders24 and Axis II Disorders25: to detect the presence of a diagnosable psychiatric condition and administered by a trained psychiatrist (ARP).
Launay-Slade Hallucinations Scale-Revised (LSHS-R)10,26: to quantify hallucination severity in clinical and nonclinical groups.
Auditory Hallucinations Rating Scale (AHRS)27: to quantify hallucination severity, with additional key elements (distress, frequency, and preoccupation) not covered by the LSHS.
Beliefs About Voices Questionnaire-Revised (BAVQ-R)28: to assess for beliefs about voice identities and engagement. BAVQ-R scores are related to voice-induced distress.29
Peters et al Delusions Inventory (PDI)30: to assess endorsement, conviction, preoccupation, and distress for a range of unusual beliefs.
Brief Multidimensional Measurement of Religiosity and Spirituality (BMMRS)31 to quantify religious/spiritual engagement, given psychics’ identification as members of a spiritual community.
We also administered the computerized binary scale of auditory speech hallucinations (cbSASH)32 as a semi-structured, in-person interview with a focus on malingering about voices,33–35 a concern in the psychics. A subset of participants (P−H+ n = 16; P+H+ n = 13) also described their earliest experiences with hearing voices and sharing those experiences with others.
All analyses were conducted in Matlab version 2014b. Group differences in endorsement of categorical variables (table 2, supplementary table 1) were assessed via chi-square tests with Holm-Sidak36 correction for multiple comparisons. Holm-Sidak correction was also used in comparing the results of specific voice-hearing scales between the 2 voice-hearing groups (table 3). When Holm-Sidak correction could not be used because of multiple P values per category, the more conservative Bonferroni method was employed (supplementary table 3). In the case of 4-group comparisons, t tests were employed when initial 2-way ANOVA results indicated a significant interaction effect after Bonferroni correction for multiple comparisons.
Table 2.
Phenomenological Characteristics of Voice-Hearing Experiences
| Voice Characteristic | P+H+ (Proportion Endorsing Characteristic) | P−H+ (Proportion Endorsing Characteristic) | P | P (Corr) | |
|---|---|---|---|---|---|
| Low-level acoustic characteristics | Clear (like external speech) | 0.94 | 0.71 | .0847 | — |
| Deep (like thinking in words) | 0.06 | 0.65 | .0005 | .0310 | |
| Men | 0.94 | 0.94 | .9647 | — | |
| Women | 0.88 | 1.00 | .1326 | — | |
| Has loudness | 0.94 | 1.00 | .2952 | — | |
| Conversational volume | 0.56 | 0.53 | .8487 | — | |
| Louder than conversational volume | 0.31 | 0.41 | .5536 | — | |
| Softer than conversational volume | 0.50 | 0.47 | .8658 | — | |
| Loudness varies with time | 0.81 | 0.76 | .7371 | — | |
| Comes from inside self | 0.56 | 0.47 | .5975 | — | |
| Comes from inside head | 0.56 | 0.41 | .3865 | — | |
| Comes from other body part | 0.06 | 0.06 | .9647 | — | |
| Comes from outside self | 0.63 | 0.88 | .0847 | — | |
| Comes from within usual hearing distance | 0.56 | 0.76 | .2181 | — | |
| Comes from outside usual hearing distance | 0.19 | 0.47 | .0847 | — | |
| Comes through ears | 0.69 | 0.65 | .8055 | — | |
| One voice | 0.13 | 0.06 | .5087 | — | |
| More than one voice | 0.88 | 0.94 | .5087 | — | |
| Associated with perceptual abnormalities in other modalities | 0.38 | 0.71 | .0564 | — | |
| Occurs simultaneously with other perceptual abnormalities | 0.19 | 0.71 | .0028 | .1652 | |
| Content, syntax, and structure | Voices speak amongst themselves | 0.56 | 0.59 | .8812 | — |
| Voices speak directly to hearer | 0.69 | 0.53 | .3530 | — | |
| Use first-person syntax | 0.56 | 0.53 | .8487 | — | |
| Use second-person syntax | 0.88 | 0.88 | .9484 | — | |
| Use third-person syntax | 0.50 | 0.59 | .6109 | — | |
| Hearing words | 0.13 | 0.18 | .6802 | — | |
| Hearing sentences | 0.63 | 0.59 | .8290 | — | |
| Hearing conversations | 0.25 | 0.24 | .9215 | — | |
| Content related to the moment heard | 0.63 | 0.88 | .0847 | — | |
| Repetitive content | 0.75 | 0.53 | .1880 | — | |
| Systematized content | 0.06 | 0.00 | .2952 | — | |
| Content focused on hearer | 0.94 | 0.76 | .1665 | — | |
| Content focused on others | 0.19 | 0.47 | .0847 | — | |
| Replays things heard | 0.56 | 0.53 | .8487 | — | |
| Replays things spoken | 0.56 | 0.12 | .0067 | .3752 | |
| Replays things thought | 0.50 | 0.06 | .0045 | .2610 | |
| Frequency | Occurs constantly | 0.25 | 0.06 | .1258 | — |
| Occurs episodically | 0.75 | 1.00 | .0279 | 1.0000 | |
| External factors increase frequency | 0.81 | 0.76 | .7371 | — | |
| External factors decrease frequency | 0.69 | 0.47 | .2077 | — | |
| Happens more when speaking | 0.00 | 0.06 | .3245 | — | |
| Happens more when listening to speech | 0.00 | 0.06 | .3245 | — | |
| Happens more when listening to non- speech sounds | 0.25 | 0.12 | .3245 | — | |
| Happens more during activities requiring attention | 0.31 | 0.18 | .3621 | — | |
| Control strategies: listening to speech | 0.00 | 0.06 | .3245 | — | |
| Control strategies: speaking | 0.00 | 0.18 | .0780 | — | |
| Control strategies: listening to non- speech sounds | 0.38 | 0.06 | .0264 | 1.0000 | |
| Control strategies: activities requiring attention | 0.38 | 0.12 | .0847 | — | |
| Control strategies: other | 0.44 | 0.41 | .8812 | .8812 | |
| Interaction, interpretation, and affective response | Occur spontaneously (uncontrollably) | 1.00 | 0.88 | .1569 | — |
| Inducible by will | 0.31 | 0.88 | .0008 | .0480 | |
| Other triggers | 0.31 | 0.24 | .6187 | — | |
| Listens to voices | 1.00 | 1.00 | — | — | |
| Talks back to voices | 0.81 | 0.94 | .2577 | — | |
| Converses with voices | 0.38 | 0.76 | .0236 | 1.0000 | |
| Positively affects safety | 0.00 | 0.53 | .0006 | .0366 | |
| Negatively affects safety | 0.13 | 0.06 | .5087 | — | |
| Comforting | 0.50 | 0.88 | .0169 | .9126 | |
| Bothersome | 0.94 | 0.29 | .0002 | .0128 | |
| Source: self | 0.50 | 0.06 | .0045 | .2565 | |
| Source: god or other spiritual being | 0.44 | 1.00 | .0003 | .0189 | |
| Source: deceased person | 0.25 | 0.59 | .0494 | 1.0000 | |
| Related to brain process | 0.63 | 0.18 | .0084 | .4620 | |
| Characteristics stable across time | 0.81 | 0.71 | .4751 | — |
Note: Results are represented as the proportions of each group endorsing individual voice characteristics. Boldface represents significant values after correction for multiple comparisons.
Table 3.
Measures of Voice-Hearing Experiences
| P+H+ Mean ± SEM | P−H+ Mean ± SEM | P | P (Corr) | |
|---|---|---|---|---|
| Total AHRS score | 25±1.09 | 22.78±0.91 | .1277 | — |
| AHRS score frequency item | 4.38±0.81 | 1.65±0.35 | .0036 | .0288 |
| AHRS score reality of voices | 4.44±0.18 | 4.56±0.16 | .6070 | — |
| AHRS score loudness of voices | 2.81±0.25 | 3.12±0.26 | .3966 | — |
| AHRS score number of voices | 4±0.5 | 4.85±0.39 | .1866 | — |
| AHRS score extent of utterance | 3.44±0.29 | 2.82±0.29 | .1419 | — |
| AHRS score influence of voices | 3.31±0.37 | 4.65±0.37 | .0169 | .1180 |
| AHRS score distress due to voices | 2.63±0.41 | 1±0 | .0003 | .0024 |
| BAVQR malevolence score | 5.69±1.29 | 0±0 | .0001 | .0008 |
| BAVQR benevolence score | 4.06±1.36 | 13.53±0.69 | .0000 | .0000 |
| BAVQR omnipotence score | 7.6±1.12 | 4.71±0.68 | .0315 | .1889 |
| BAVQR resistance emotion score | 6.14±1.02 | 0.59±0.41 | .0000 | .0001 |
| BAVQR resistance behavior score | 8.93±1.22 | 0.88±0.4 | .0000 | .0000 |
| BAVQR engagement emotion score | 1.67±0.77 | 8.76±0.54 | .0000 | .0000 |
| BAVQR engagement behavior score | 2.53±0.89 | 8.38±0.69 | .0000 | .0002 |
Note: AHRS, Auditory Hallucinations Rating Scale; BAVQ, Beliefs About Voices Questionnaire. Boldface represents significant values after correction for multiple comparisons
Results
Baseline Demographic and Clinical Characteristics
Baseline characteristics of participants are summarized in table 1. SCID-I diagnoses for the P+H+ and P+H− groups included schizoaffective disorder (n = 9) and schizophrenia (n = 9). All groups included a subset who reported a major depressive episode (MDE) in the past, as well as alcohol and other drug use, currently in remission, but this did not differ significantly across groups (P = .15). Age, sex, race, years of education, and estimated full-scale IQ did not differ significantly. Participants without a diagnosed psychotic disorder were more likely to be employed than those who did not. Antipsychotic burden did not differ between the 2 diagnosed groups.
Table 1.
Demographics
| P+H+ | P−H+ | P+H− | P−H− | P | |
|---|---|---|---|---|---|
| N | 16 | 17 | 16 | 18 | |
| SCID-I Diagnosis (count) | Schizoaffective disorder (9); Schizophrenia (7); past MDE (on sx onset; 3); cannabis use d/o (in remission, 4); alcohol use d/o (in remission, 4); | None (12); Past MDE (4); cannabis use disorder (in remission, 2); alcohol use disorder (in remission, 1); | Schizophrenia (9); schizoaffective disorder (7); cannabis use disorder (in remission, 3); alcohol use disorder (in remission, 3); cocaine use disorder (in remission, 3) | None (15); past MDE (2); alcohol use disorder (in remission, 1) | |
| Age (y) | 42.31±13.76 | 46.8235±12.47 | 37.75±13.78 | 39.67±12.98 | Hall: .075 Psych: .32 Interaction: 0.69 |
| Sex | 43.75% (7) Male; 56.25% (9) Female | 23.5294% (4) Male; 76.4706% (13) Female | 56.25% (9) Male; 43.75% (7) Female | 44.4444% (8) Male; 55.5556% (10) Female | .29 |
| Race | 68.75% (11) White, 18.75% (3) Black, 6.25% (1) Other | 82.3529% (14) White, 11.7647% (2) Black, 5.8824% (1) Other | 56.25% (9) White, 43.75% (7) Black, | 61.1111% (11) White, 33.3333% (6) Black, 5.5556% (1) Other | .21 |
| Years of education | 14.125±1.9958 | 15.1765±2.2146 | 14.6±2.8486 | 14.8333±2.2816 | .63 |
| Currently working | 25% | 82.3529% | 31.25% | 77.7778% | .00036 |
| Full-scale IQ (from WRAT3) | 99.13±4.53 | 98.69±4.36 | 98.67±4.22 | 103.41±3.17 | Hall: .60 Psych: .60 Interaction: .53 |
| Antipsychotic burden (CPZ equiv mgs) | 446.27±110.37 | 401.63±91.91 | .758678 |
Note: SCID-I, Structured Clinical Interview for DSM-4 Axis I Disorders; CPZ equivs, chlorpromazine equivalents (mgs); WRAT3, Wide-Range Achievement Test, 3rd edition; MDE, major depressive episode. Boldface represents significant values after correction for multiple comparisons.
Analysis of Acoustic Characteristics, Content, Frequency, Affective Response, and Interpretation of Voices
We conducted a comprehensive, in-person semi-structured interview in order to compare the 2 hallucinating groups across a variety of voice-hearing experiences (table 2). Voice characteristics, derived from the cbSASH32 and other phenomenological surveys,33–35 were grouped into themes: items assessing low-level voice characteristics, content of utterance, frequency of utterance, and higher-level considerations of the voice-hearer’s interaction with their voices, affective response, and beliefs about the nature of their voices. The 2 voice-hearing groups did not differ on nearly any acoustic characteristics of their voices, including endorsement of voices that sounded clear (“like external speech”), although the P−H+ group did differ in their likelihood of also endorsing voices that were deep (“like thinking in words”). Importantly, several items (end of Low-Level Acoustic Characteristics section of table 2) are extremely rare in voice-hearing patients and may signify atypical or malingered voices.34,35 No participants in either group endorsed these characteristics. Similarly, the content and frequency of voices did not differ between voice-hearing groups.
By contrast, the 2 voice-hearing groups interacted differently with their voices, they inferred different origins for their voices, and had different affective responses to them. The 2 groups similarly endorsed voices that occurred spontaneously (in situations both in and outside of their spiritual practice), but the P−H+ group was more likely report that they could make the voices occur by will and prevent them from occurring (corrected P = .049). The psychics were more likely to identify a divine being as the voice source (corrected P = .018). They were also more likely to say their voices were protective (P = .040), and less likely to describe them as bothersome (P = .010).
More fine-grained examination of voice-hearing experiences was conducted with the use of the AHRS27 and the BAVQ-R28 (table 3). Although groups were specifically selected to have had at least daily hallucinatory experiences, frequency did differ between groups, with P−H+ participants reporting voices occurring between once and 10 times daily, whereas those in the P+H+ group reported voices 3–6 times per hour on average (corrected P = .029). P+H+ participants rated their voices as sometimes producing significant fear or anxiety, whereas all P−H+ participants rated their voice-hearing experiences at the lowest distress rating, “Not distressing, may be enjoyable.” Consistent with this difference, P+H+ participants had higher malevolence scores on the BAVQ (corrected P = .008) and were more likely than P−H+ participants to resist their voices (behavioral resistance score, corrected P < .0001; emotional resistance score, corrected P = .0001). By contrast, P−H+ participants were more likely to characterize their voices as benevolent and were more likely to engage with them emotionally (corrected P < .0001) and behaviorally (corrected P = .0002).
Overall Symptomatology
In order to determine how the clairaudient psychic group compared to the other 3 groups in terms of overall symptomatology and religious conviction, we compared: the LSHS-R10,26; PANSS23; Brief Psychiatric Rating Scale (BPRS)37; Peters Delusion Inventory (PDI)30; Chapman Anhedonia, Perceptual Aberration, and Magical Ideation subscales38; and the Brief Multidimensional Measurement of Religiosity and Spirituality (BMMRS)31 scores across all 4 groups (supplementary table 1).
Both hallucinating groups had similar scores on the LSHS and did not differ on Auditory Hallucinations (AH), Vivid Daydreams (VDD), Vivid Thoughts (VT), or Intrusive Thoughts (IT) subscales. Interestingly, P−H+ participants exhibited higher scores on the visual hallucinations subset of the LSHS.
There was a significant main effect of hallucination status and psychotic status on total PANSS scores, PANSS positive symptom scores, and PANSS general symptom scores. A main effect of psychotic status but not hallucination status was seen on PANSS negative symptom scores. Analysis of PANSS hallucinations score (P3 ratings) revealed the expected main effect of hallucination status with no main effect of psychotic status or interaction effects. Analysis of delusion scores (P1 ratings) demonstrated main effects of hallucination status and psychotic status as well as interaction effects. Post hoc analysis demonstrated significantly greater P1 ratings in P−H+ and P+H− groups than P−H− groups. A similar pattern was observed in other measures of unusual thought, including BPRS Unusual Thoughts scores, PDI total score, and number of delusional ideas endorsed on PDI.
We also examined spiritual/religious conviction across groups. Few differences in religious experience were found among the groups. Main effects of hallucination status were found in daily experiences and religious coping. Interaction effects were also found in tendency to use religious support for coping, with post hoc tests revealing a higher tendency of P+H+ participants to use religious support to cope with stress than their P−H+ counterparts, who had the lowest tendency to utilize these resources.
Measures of schizotypy were additionally different between hallucinating groups. Significant main effects of hallucination status were seen in total and magical ideation score on the Chapman scales. Interestingly, P−H+ group members had the highest magical ideation (higher than either diagnosed group).
On SCID-II screening (supplementary table 2), P−H+ participants screened positive for Schizotypal Personality Disorder at a rate of 94%, much higher than any other group tested. By contrast, P+H+ were more likely than any other group to screen positive for Borderline Personality Disorder (BPD) (60%).
Early Voice-Hearing Experiences and Social Support
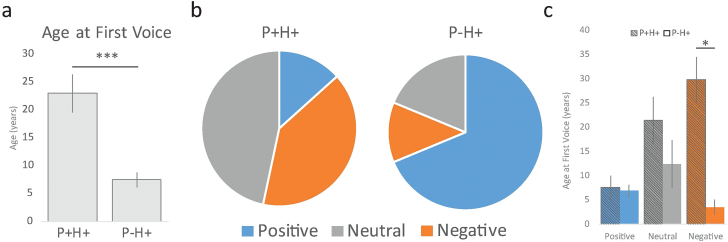
Retrospective estimates of age at first voice were obtained and participants rated how positively these experiences were received within their social networks (figure 1). Age at first voice differed markedly between the 2 groups (figure 1a). P+H+ reported being an average of 22.9 years old when they heard their first voice, compared to 7.5 years of age in the psychic group (P = .0002). Patients reported significantly higher rates of negative and neutral experiences initially telling others about their voice-hearing, and psychics reported more positive experiences (figure 1b; by chi-squared test, P = .0074).
Fig. 1.
Early voice-hearing experiences. (a) Retrospective report of voice-hearing age of onset in individuals interviewed who have hallucinations with a diagnosed psychotic disorder (P+H+) and individuals who self-identify as clairaudient psychics (P−H+). (b) Proportions of each group who rated their first experiences discussing their voice-hearing with another person as positive (blue), negative (orange), and neutral (gray). (c) Age of onset plotted as a factor of the emotional valence of discussing voices for the first time. Error bars represent 1 SEM. *P < .05; ***P < .001.
Two-way ANOVA (figure 1c) with factors psychotic diagnosis and valence of early experiences talking about their voices confirmed a significant main effect of psychotic diagnosis (mean age, P+ = 22.9, P− = 7.4; P = .005) and significant interaction effects (P = .049); the main effect of valence exhibited a trend toward significance (P = .088). Post hoc t tests revealed a significant difference in age between the 2 groups among those who stated they had negative initial experiences revealing that they heard voices (P = .022); no other valence categories demonstrated significant inter-group differences.
Discussion
The voice-hearing experiences of clairaudient psychics exhibit striking similarities and important differences from help-seeking voice-hearers. There were very few differences in the low-level acoustic characteristics, content, or frequency of their experiences. There were key differences in their interpretations of these events, their affective response to them, and their perceived ability to control them. Lastly, investigation into participants’ early voice-hearing experiences revealed a younger age of onset in psychics compared to their treatment-seeking counterparts, with accompanying positive experiences on telling others of their voice-hearing.
To our knowledge, this is the first description of self-identified psychics as a voice-hearing population without the need for psychiatric care. Like their voice-hearing counterparts in the general population, our group of psychics exhibited broadly similar phenomenological features to treatment-seeking voice-hearers.8,22,39 Frequency of voice-hearing was slightly lower than those seeking treatment, again consistent with prior reports.22 Psychics identified their voices as benevolent, also consistent with prior work.40 The decreased distress related to voice-hearing may be crucial to psychics’ avoiding a need for care.3,41 Psychics’ age of onset was lower, again similarly to prior reports in non-treatment-seeking voice-hearers.22,42 Perhaps most notably, like other reports,40 clairaudient psychics reported being able to control voice onset and offset.
Despite these similarities, there are some key differences between the psychics’ experiences and prior descriptions of nonclinical voice-hearing. Most notably, the psychics report ongoing daily voices, whereas other nonclinical voice hearing is often transient and context-dependent.2 Rather than being passive receivers of verbal information, clairaudient psychics seek it out as a part of their daily activities. Indeed, many of those interviewed report an increased perceived ability to control the occurrence of their voices and—crucially—report that they had not always possessed such an ability, instead developing it over time. Rather than reflecting enhanced executive function and cognitive control, as some have suggested,8,43,44 this may instead be the result of intentional practice. This, in turn, may result from the lower distress exhibited by the psychics, leading to an increased willingness to engage with and ultimately control them. This is consistent with a recovery-oriented understanding of voice-hearing.45 Indeed, a similar ability to control voice-hearing was first reported by Romme and Escher in their survey of non-help-seeking voice-hearers.21 Furthermore, anthropological studies of voice-hearing in small face-to-face societies found that shamans, spiritual practitioners who work for the good of the group by channeling metaphysical powers, also maintained a degree of control over their experiences.46 Murphy’s classic analysis of psychosis in culturally different settings observed that the psychotic person’s lack of control over his unusual experience was an important part of what identified him as mad to his social world.47 Taken together with our data, these earlier observations, and the growing Hearing Voices Movement, proffer the exciting possibility that such control could be trained, opening a new therapeutic avenue for voices that are distressing.
Psychics were more likely to engage with their voices and less likely to rely on religiously-based coping strategies than those in the treatment-seeking group, likely denoting a decreased need for coping in general. Here we emphasize the distinction between religiosity (a belief in God or gods, to be worshiped often by engaging in rituals) vs spirituality (a worldview that focuses on transcending what is physically explicable). One can be more religious and less spiritual (to a point) and vice versa.48 While the psychics were more spiritual and less religious, the help-seeking group were significantly more religious. We suggest that one source of support for help-seekers is the church, a physical location and social group who can be depended upon for support and a set of practices that provide meaning.49 In contrast, the psychics had a metaphysical account of their voices, less constrained by doctrine and therefore, perhaps more accommodating of their specific circumstances and experiences. This group may have relied less on communal organization because of their differences in belief, although it should be noted that some psychics did have spiritual organizations to which they belonged in which they often found comfort (see individual quotations in table 4 for instances of this). This will be an important point for future investigation, especially given that religiosity and spirituality can, for some people, signify a barrier to medication adherence and may be a source of both help and difficulty.50
Table 4.
Representative Quotations Regarding Phenomenology of Psychic Voice-Hearing
| Similar To P+H+ | Dissimilar to P+H+ |
|---|---|
| [Researcher: Where in space do they sound like they’re coming from?...] More often, it’s either from within my body or right to the right side of my head [Researcher: Within your head? Or within other parts of your body?] Within my head. | [Researcher: Anything make [the voices] less frequent?] If I’m really worried about something, really preoccupied with something in my own life, not sleeping, caffeine, that kind of thing, I’m more likely to block them out. |
| [Researcher: Is it mostly words, sentences or whole conversations?] It’s mostly words and sentences. Very rarely whole conversations. | [Researcher: Do they affect your safety?] I have gotten voices that calm me down…When I was in a car accident once and they said everything was going to be okay. |
| [Researcher: Do you do anything to control them besides shutting yourself off?] Yes, sometimes I will sing. I will play a song in my head so that I hear a song and not them. | |
| [Researcher: Any environmental things that make them more likely...?] I would say white noise or anytime I’m not really focused on anything so maybe when I’m driving and not really focusing or zoning out | |
| I try not to listen to the T.V. or radio for [personal communications]… I’m very religious… my husband was the president of his church… I try not to… but if I really focus on it I can. | [Researcher: When do [the voices] happen?] If I allow it, it can happen all the time.Sometimes I can put a wall up, but if its meant to be heard or seen, it will be.The voices don’t cause anxiety because I’ve trained myself. |
| [Researcher: Have you ever heard the devil?] Yes. I’ve heard the devil and the Angel of Death. [Researcher: In the past [have you] heard the voice of God speaking?] Yes, all the time! | |
| [Researcher: is that typical of the length [of the voices]?] yes, now I can get sentences. When I was younger, I only really got words but now sentences. | I’ve done a lot of meditation techniques to just make sure that the voices are clear so that I can understand the message. |
| [Researcher: As far as the acoustic qualities...?] As clear as your voice or as clear as my voice | You said to me, “You’re amazing” and then I heard a small voice say, “Yes, you truly are.”...As clear as day. For me, it was a validation. |
| My Husband’s voice is always with me... And it would be something like “Don’t forget to take your pills” [Researcher: And that was from outside of you] Yes, he would tell me like routine things. the routine kind of continued even though my husband wasn’t there. | [Researcher: Can you make it happen?] Yeah, when you’re open it will come. But it takes work. |
| [Researcher: In terms of how real [the voices] sound...] Very real...I think depending on the messages and how in tune you are. Sometimes they can just be jibberish and in the background and sometimes they can be really intense. [Researcher: You hear jibberish sometimes?] Yes, but it’s rare. They’re usually pretty intense. | |
| [Researcher: Do [the voices] ever come when you don’t want it to come?] It always comes when you don’t want it to come; you don’t expect it. [Researcher: Can you stop it?] You can’t stop it. [Researcher: Can you call it?]I can not want to deal with it and it will come later on. [Researcher: Like, postpone it?] Yeah, I can postpone it but I can’t stop it. | |
| It was later on in life... I was like 5 when my mom told me that what I was doing was wrong and I was making things up and I didn’t need to talk about things because people would think I was crazy and stuff. | [Researcher: [Have you] ever been troubled by hearing voices in your head?] No, it doesn’t really faze me. |
| I can turn it off, but it more often sounds like a cocktail party when I shut myself off to them. | These voices are my spirit guides. They come from heaven. They’re departed loved ones. |
| [Researcher: Sounds like they happen in episodes...] I would never quantify that by saying it’s an “episode” at all. There are times when I don’t want to communicate or I’m dealing with something in my earthly life that I just don’t... I tune it out. I am not in constant communication 24/7 | |
| I can’t make them communicate with me but I can make myself open to hearing... | |
| I used to hear so big that I couldn’t function...I would pray and ask for help but it was so big that there was no help and I couldn’t function just from all the overwhelming noise. | I learned to ask God to hear everything out-loud and eventually I learned to ask one spokesperson to step forward and talk to me one at a time. |
| I have a very special relationship with Archangel Michael. He was my imaginary friend when I was a kid, but he wasn’t imaginary. I just didn’t know his name was Michael until he told me way later… after reading the Bible or someone saying something or something. | |
| [Researcher: Do you hear conversations?] Oh yeah [they talk to each other.] It’s just like walking through a cafeteria | |
| When I’m “on” [the number of voices] can be relentless. [Researcher: And for days off?] When I’m off, I can run into some situation and it’s there, like it’s so strong that I have to do whatever it says. | I can turn things on and turn things off. When I’m working, i open myself and when I’m not, i turn it off, like a switch. |
| It can happen two, three times a day [when I’m “off”] spontaneously. | |
| [Researcher: Do you ever get any personal communications from the radio or television?] Every now and then... Like if there’s an energy that wants to communicate but I have the walls up because I don’t want to deal with this... [Researcher: what happens then?] Lets say the screen will get fuzzy and there’s no reason and then you’ll hear through the fuzz... when you shut [the voices] off and they’re like “No, I want to talk to you.” | I’m not scared to hear [a voice] but certain voices are troubling. |
| My phone is weird because I’ll shut everything off and my phone will be like “Nope, you’re not going to shut down on me.” There’s no reason for it. Anything battery or electric they can manipulate. | That noise [from the voices] becomes padded but it’s there...but you’re shutting it away. You’re like, “I don’t want to hear that” so you’re padding it. [Researcher: Because you’re attending to other things?] Exactly. [Researcher: But it’s still there? So there’s chatter now?] It’s off. [So is it still there or are you just not paying attention to it?] I close the wall. It’s almost like there’s a wall and I put the wall up. I taught myself to do this when I was five...because my mother just shut me down [when I tried to talk about my experiences]. |
| When you sleep, you’re out of your body and a lot of times they try to talk to you when you’re sleeping. | You train yourself. You just shut it off...But I can’t make them disappear. They’re like muffled. |
| When I was six, I remember sitting outside by myself and having conversations with something...I thought it was the wind [that I was conversing with], and just hearing the voices, which I was comfortable with... Then there were other times when I would be sent to my room and it was dark and I was being punished and there would be occasional voices that would freak me out. | [Researcher: Are they episodic or do they happen constantly?] They’re not constant. I can shut them off. |
| There would be moments where I would be in kind of a quiet contemplative state, so like I would be cooking a meal and making a recipe and then I would just hear... Sometimes it was like... A lot of chatter, so like a cocktail party and you’re just hearing the overtones of everybody. But there would be a feeling of like I don’t like... if I could make out what they were saying, I would have a feeling that I don’t like that because it’s not pleasant to me. | [Researcher: What do you do to shut them down?] I tell them to shut up. [That’s all you do? Just internal, you just tell them to shut up?] No, I say it out loud...”I’m off duty now. Go away.” |
| There would be moments when the voices would egg me on... Egg my anger on and it would be like “go break something” or “go hit your brother” or go do something like that… a lot of it was more of a self-loathing thing, so I would hear “you’re stupid” or things like that. | |
| When I was a kid we used to joke that there were voices in the fan. | |
| I don’t think I was troubled by it...it was like “Okay, what’s the deal?” and I wanted to understand it. But I always had a sense of reassurance...I never felt like I had to worry for hearing voices in my head. | |
| [What was your first experience hearing a voice?] I don’t remember a time, but I do remember as I got older--closer to my teen years--where I would be upset and it would be like this other person talking to me. I would be like “I’m going freaking crazy”. | Other times I miss it. I’m like, “where are my friends?” [Researcher: Can you turn it back on then?] Yeah, if there’s something I want to know personally I can. |
| “I was troubled until I learned what it was.” | [Researcher: You were getting verbal messages [during your early experiences]?] It would be verbal messages, but it would be more bodily sensations...it turned out to be this mediumship thing. [Researcher: So you started finding meaning in these somatic sensations?] Exactly...it wouldn’t scare me anymore and now I work enough of the energies that I can be like “Bro, back up.” |
| I was [younger] and would be like “I am going to be nothing when I grow up,” and they would be like, “No, you’re going to be a writer and you’re going to help people.”...[Researcher: So your first experience with voices was reassuring?] They were talking to me positively... trying to keep me from being like, “I suck.” | |
| [The voices] never bothered me where I’ve been scared or frightened....I ‘ve always been very comforted and felt not alone in a positive way | |
| [Researcher: [Have you] ever been troubled by hearing voices in your head?] Never been troubled...That’s not true. I’ll say a 2 [on a scale of five] because I was, but I’m not now. | [One of my voices] was a female French scientist...and that was the powerful female, smart female presence that I needed. Having a female scientist who came to me was...very empowering. |
| At that point, I was going absolutely crazy trying to figure out what is wrong with me: why am I hearing all of these things? I really feel nuts. How do I fix this? | I... fumbled through life for a while with this whole hearing [voices] and “knowing” [clairsentience] and “seeing” [clairvoyance] and then a friend of mine...was like, “You have to go to this center because there are people like you! You have a gift and you need to go!” And since then, it has been wonderful. Understanding how to dissect it...being able to understand and dissect what was happening to me. |
| So you’ll think I’m crazy, in the session this morning, I was travelling through this woman’s time and space and we got to a point where it felt like it was her but it wasn’t a person, it was an alien. The alien was speaking to me but I couldn’t understand and my guide had to translate to me. | [Spirits talking to me is] part of being “on” all the time, which I do like, but there are boundaries and I have to set them. [Researcher: So you’re ignoring them.] No, I’m not ignoring them…I’m just like, “No, not right now.” |
| [Researcher: In terms of where they sound like they’re coming from ...] Sometimes it will be from far away. Most of the time it’s like they’re right here...90% of the time they’re right here. | |
| [Researcher: Can you make them happen by will?] By my passions, I’m making them more inclined to happen, but they happen when they happen. | [Researcher: [Have you] ever been troubled by hearing voices in your head?] No, I’ve never been troubled by it. |
| My first big master was the Roman Emperor Julian the apostate. | [Researcher: [Have you] ever been troubled by hearing voices in your head?] I’ve never been troubled... Because I can control it. |
| [Researcher: When you first heard a voice, what was that? How old were you?] 14. [Do you remember what it was like?] Uplifting. Astral projecting. Loving. Protective. | |
| I used to hear voices a lot. What happened was I started to develop a psychic sense. I would hear a cacophony of voices. I would try to go to sleep and I could hear conversations and I would hear the doorbell ring and then five minutes later it would ring and I could hear people knocking....it bothered me because I couldn’t sort it out. I was too open, if that makes sense. | [How old were you when you first heard a voice?] I was around 5 or 7. [Was it a pleasant or unpleasant experience?] It was nurturing. It was effeminate in nature. You might equate it to some kind of benevolent guide. |
Note: Each row comprises quotations from individual subjects.
The psychics exhibited higher schizotypy than the other groups, while treatment-seeking voice-hearers exhibited more traits of BPD. These traits do not necessarily indicate the presence of BPD (as they may be explained by the presence of an Axis I disorder). They are primarily markers of social impairment. Hoffman emphasized that psychotic symptoms develop in social isolation,51 and that voices are perceived as social agents communicating with the experient.52 Perhaps our observation of Borderline symptomatology in the P+H+ group attests to the social difficulties that hearing distressing voices can portend.
While the group differences described above survive correction for multiple comparisons, several others did not. Given the descriptive nature of our study, these items are nonetheless worth noting. Help-seeking voice-hearers appear to have multisensory hallucinations at a rate similar to that previously described,53 while psychics reported a higher rate. However, it is difficult to say whether the hallucinations were truly fused, a rarer phenomenon than simple multisensory hallucinations.54 The increased likelihood that help-seeking voice-hearers’ voices would replay things they have spoken or thought may reflect the unpleasant nature of their experiences, and although no participants met criteria for Posttraumatic Stress Disorder (PTSD), could speak to the possibility of past trauma in the help-seeking group.55 We note that the help-seeking voice-hearers were more likely to screen positive for BPD than psychics or non-voice-hearing help-seekers. BPD involves social dysfunction and is associated with developmental trauma and neglect, in which voices and dissociative experiences are common,56 and wherein voices are similar to those experienced by patients with schizophrenia.57
Other items that did not survive correction may reflect aspects of the illness narrative: treatment-seeking voice-hearers were more likely to ascribe voices to themselves, more likely to say they were the result of brain processes, and less likely to call them comforting. In order to more fully illustrate the similarities and differences between the psychic group and their treatment-seeking counterparts, we include representative quotations regarding voice-hearing experiences (table 4).
As figure 1 shows, those who had positive experiences telling another person about their voices, regardless of treatment-seeking status, tended to have had an earlier age of onset than those who had negative experiences. Indeed, although the overall differences in age of onset may indicate that psychics represent a biologically distinct subset of voice-hearers that does not follow the typical trajectory of psychotic illness, the interaction between these factors may indicate that social factors (such as the age at which one describes voice-hearing to friends and relatives, which may be inversely related to their acceptance of these claims) may represent an important mediating prognostic factor. This is speculative, of course, and we note that we do not know whether the patients’ trajectories would have been any different had they been more accepted by those around them. Differences in family culture may also prove to be an important factor. It will be important to establish whether voice-hearers’ spiritual beliefs predate their voice-hearing experiences in subsequent studies.
Our study carries some limitations. First, the sample is very small compared to studies that used population-based approaches to nonclinical voice-hearing,58,59 although we replicated many of the findings typical of voice-hearing in those studies. Nevertheless, other differences may arise in a larger sample and interesting sub-groups may be identified. Second, our results may have been influenced by our choice of assessments. Other scales may have elicited other aspects of individuals’ experiences. Similarly, demand characteristics specifically related to participants’ professional identities as psychics could be addressed in future. Lastly, concerns about the stability of so-called “healthy” voice-hearing groups has been raised recently.60 For this reason, efforts should be made to follow this unique cohort over time to determine the stability of their experiences and functioning.
We neither confirm nor deny the veracity of psychics’ beliefs regarding their experiences; instead, we study their voice-hearing as a crucial counterpart to clinical voice-hearing—one free, eg, from the stigma of diagnosis and the complications of treatment. We cannot conclude that all clairaudient psychics have similar voice-hearing experiences to treatment-seeking voice-hearers or that all psychics’ claims of voice-hearing are veridical. Indeed, we acknowledge that we likely created a selection bias—those who have veridical voice-hearing may be more likely to participate. However, this homogeneous group of voice-hearers (who share a similar explanatory framework) may facilitate the identification of protective factors undetected in more heterogeneous, population-based samples. These factors could guide the development of treatment strategies for voices that are distressing.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
This work was supported by the Connecticut Mental Health Center (CMHC) and Connecticut State Department of Mental Health and Addiction Services (DMHAS). P.R.C. was funded by R01MH067073, the NCPTSD, an IMHRO/ Janssen Rising Star Translational Research Award and CTSA Grant Number UL1 TR000142 from the National Center for Research Resources (NCRR) and the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official view of NIH or the CMHC/DMHAS. A.R.P. was supported by the Integrated Mentored Patient-Oriented Research Training (IMPORT) in Psychiatry grant (5R25MH071584-07) as well as the Clinical Neuroscience Research Training in Psychiatry grant (5T32MH19961-14) from the NIMH. Additional support was provided by the Yale Detre Fellowship for Translational Neuroscience as well as the Brain and Behavior Research Foundation in the form of a NARSAD Young Investigator Award for Dr. Powers.
Supplementary Material
Acknowledgments
The authors would like to thank all participants who took part in this and related studies. Thanks especially to the participating psychic community, whose willingness to help advance our understanding of voice-hearing may have entailed some personal and professional risk. Thanks also to Robert Stimson, PhD, and clinicians at CMHC who aided with recruitment. The authors declare no conflicts of interest.
References
- 1. Strauss JS. Hallucinations and delusions as points on continua function. Rating scale evidence. Arch Gen Psychiatry. 1969;21:581–586. [DOI] [PubMed] [Google Scholar]
- 2. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. [DOI] [PubMed] [Google Scholar]
- 3. Krabbendam L, Myin-Germeys I, Bak M, van Os J. Explaining transitions over the hypothesized psychosis continuum. Aust N Z J Psychiatry. 2005;39:180–186. [DOI] [PubMed] [Google Scholar]
- 4. van Os J. Is there a continuum of psychotic experiences in the general population? Epidemiologia e psichiatria sociale. 2003;12:242–252. [DOI] [PubMed] [Google Scholar]
- 5. Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res. 2002;54:59–65. [DOI] [PubMed] [Google Scholar]
- 6. van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. [DOI] [PubMed] [Google Scholar]
- 7. van Os J, Verdoux H, Maurice-Tison S, et al. Self-reported psychosis-like symptoms and the continuum of psychosis. Soc Psychiatry Psychiatr Epidemiol. 1999;34:459–463. [DOI] [PubMed] [Google Scholar]
- 8. Johns LC, Kompus K, Connell M, et al. Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull. 2014;40(suppl 4):S255–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schmack K, Gomez-Carrillo de Castro A, Rothkirch M, et al. Delusions and the role of beliefs in perceptual inference. J Neurosci. 2013;33:13701–13712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bentall RP, Slade PD. Reality testing and auditory hallucinations: a signal detection analysis. British J Clin Psychol. 1985;24(Pt 3):159–169. [DOI] [PubMed] [Google Scholar]
- 11. Peters E, Day S, McKenna J, Orbach G. Delusional ideation in religious and psychotic populations. British J Clin Psychol. 1999;38 (Pt 1):83–96. [DOI] [PubMed] [Google Scholar]
- 12. Corlett PR, Fletcher PC. The neurobiology of schizotypy: fronto-striatal prediction error signal correlates with delusion-like beliefs in healthy people. Neuropsychologia. 2012;50:3612–3620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lawrie SM, Hall J, McIntosh AM, Owens DG, Johnstone EC. The ‘continuum of psychosis’: scientifically unproven and clinically impractical. British J Psychiatry. 2010;197:423–425. [DOI] [PubMed] [Google Scholar]
- 14. Cantin L, Lenoir M, Augier E, et al. Cocaine is low on the value ladder of rats: possible evidence for resilience to addiction. PloS One. 2010;5:e11592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Klein G. Toward a genetics of cancer resistance. Proc Natl Acad Sci U S A. 2009;106:859–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pancino G, Saez-Cirion A, Scott-Algara D, Paul P. Natural resistance to HIV infection: lessons learned from HIV-exposed uninfected individuals. J Infect Dis. 2010;202(suppl 3):S345–350. [DOI] [PubMed] [Google Scholar]
- 17. Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36, Table of Contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alvarado CS. G. Stanley Hall on “Mystic or Borderline Phenomena”. J Scient Explor. 2014;28:75–93. [Google Scholar]
- 19. Daalman K, van Zandvoort M, Bootsman F, Boks M, Kahn R, Sommer I. Auditory verbal hallucinations and cognitive functioning in healthy individuals. Schizophr Res. 2011;132:203–207. [DOI] [PubMed] [Google Scholar]
- 20. Diederen KM, Daalman K, de Weijer AD, et al. Auditory hallucinations elicit similar brain activation in psychotic and nonpsychotic individuals. Schizophr Bull. 2012;38:1074–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Romme MA, Escher AD. Hearing voices. Schizophr Bull. 1989;15:209–216. [DOI] [PubMed] [Google Scholar]
- 22. Daalman K, Boks MP, Diederen KM, et al. The same or different? A phenomenological comparison of auditory verbal hallucinations in healthy and psychotic individuals. J Clin Psychiatry. 2011;72:320–325. [DOI] [PubMed] [Google Scholar]
- 23. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 24. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0). New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995:722. [Google Scholar]
- 25. First MB. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders: SCID-II. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 26. Launay G, Slade P. The measurement of hallucinatory predisposition in male and female prisoners. Pers Indiv Differ. 1981;2:221–234. [Google Scholar]
- 27. Oulis PG, Mavreas VG, Mamounas JM, Stefanis CN. Clinical characteristics of auditory hallucinations. Acta Psychiatr Scand. 1995;92:97–102. [DOI] [PubMed] [Google Scholar]
- 28. Chandwick P, Lees S, Birchwood M. The revised Beliefs About Voices Questionnaire (BAVQ-R). British J Psychiatry. 2000;177:229–232. [DOI] [PubMed] [Google Scholar]
- 29. Peters ER, Williams SL, Cooke MA, Kuipers E. It’s not what you hear, it’s the way you think about it: appraisals as determinants of affect and behaviour in voice hearers. Psychol Med. 2012;42:1507–1514. [DOI] [PubMed] [Google Scholar]
- 30. Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: introducing the PDI (Peters et al. Delusions Inventory). Schizophr Bull. 1999;25:553–576. [DOI] [PubMed] [Google Scholar]
- 31. Idler EL, Musick MA, Ellison CG, et al. Measuring multiple dimensions of religion and spirituality or health research - Conceptual background and findings from the 1998 General Social Survey. Res Aging. 2003;25:327–365. [Google Scholar]
- 32. Stephane M, Pellizzer G, Roberts S, McClannahan K. Computerized binary scale of auditory speech hallucinations (cbSASH). Schizophr Res. 2006;88:73–81. [DOI] [PubMed] [Google Scholar]
- 33. McCarthy-Jones S, Trauer T, Mackinnon A, Sims E, Thomas N, Copolov DL. A new phenomenological survey of auditory hallucinations: evidence for subtypes and implications for theory and practice. Schizophr Bull. 2012;40:231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McCarthy-Jones S, Resnick PJ. Listening to voices: the use of phenomenology to differentiate malingered from genuine auditory verbal hallucinations. Int J Law Psychiatry. 2014;37:183–189. [DOI] [PubMed] [Google Scholar]
- 35. Mason AM, Cardell R, Armstrong M. Malingering psychosis: guidelines for assessment and management. Perspect Psychiatr Care. 2014;50:51–57. [DOI] [PubMed] [Google Scholar]
- 36. Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 37. Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 38. Chapman JP, Chapman LJ, Kwapil TR. Scales for the measurement of schizotypy. In: Raine A, Lencz T, Mednick SA, eds Schizotypal Personality. New York, NY: Cambridge University Press; 1995:79–106. [Google Scholar]
- 39. Hill K, Varese F, Jackson M, Linden DE. The relationship between metacognitive beliefs, auditory hallucinations, and hallucination-related distress in clinical and non-clinical voice-hearers. British J Clin Psychol. 2012;51:434–447. [DOI] [PubMed] [Google Scholar]
- 40. Andrew EM, Gray NS, Snowden RJ. The relationship between trauma and beliefs about hearing voices: a study of psychiatric and non-psychiatric voice hearers. Psychol Med. 2008;38:1409–1417. [DOI] [PubMed] [Google Scholar]
- 41. Beavan V, Read J. Hearing voices and listening to what they say the importance of voice content in understanding and working with distressing voices. J Nerv Ment Dis. 2010;198:201–205. [DOI] [PubMed] [Google Scholar]
- 42. Peters E, Ward T, Jackson M, et al. Clinical, socio-demographic and psychological characteristics in individuals with persistent psychotic experiences with and without a “need for care”. World Psychiatry. 2016;15:41–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Badcock JC, Hugdahl K. Cognitive mechanisms of auditory verbal hallucinations in psychotic and non-psychotic groups. Neurosci Biobehav Rev. 2012;36:431–438. [DOI] [PubMed] [Google Scholar]
- 44. Waters F, Allen P, Aleman A, et al. Auditory hallucinations in schizophrenia and nonschizophrenia populations: a review and integrated model of cognitive mechanisms. Schizophr Bull. 2012;38:683–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Slade M, Longden E. Empirical evidence about recovery and mental health. BMC Psychiatry. 2015;15:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Laroi F, Luhrmann TM, Bell V, et al. Culture and hallucinations: overview and future directions. Schizophr Bull. 2014;40(suppl 4):S213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Murphy JM. Psychiatric labeling in cross-cultural perspective. Science. 1976;191:1019–1028. [DOI] [PubMed] [Google Scholar]
- 48. McEvoy M, Burton W, Milan F. Spiritual versus religious identity: a necessary distinction in understanding clinicians’ behavior and attitudes toward clinical practice and medical student teaching in this realm. J Relig Health. 2014;53:1249–1256. [DOI] [PubMed] [Google Scholar]
- 49. Huguelet P, Mohr SM, Olie E, et al. Spiritual meaning in life and values in patients with severe mental disorders. J Nerv Ment Dis. 2016;204:409–414. [DOI] [PubMed] [Google Scholar]
- 50. Borras L, Mohr S, Brandt PY, Gillieron C, Eytan A, Huguelet P. Religious beliefs in schizophrenia: their relevance for adherence to treatment. Schizophr Bull. 2007;33:1238–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hoffman RE. A social deafferentation hypothesis for induction of active schizophrenia. Schizophr Bull. 2007;33:1066–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bell V. A community of one: social cognition and auditory verbal hallucinations. PLoS Biol. 2013;11:e1001723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lim A, Hoek HW, Deen ML, Blom JD, Investigators G. Prevalence and classification of hallucinations in multiple sensory modalities in schizophrenia spectrum disorders [published online ahead of print June 24, 2016]. Schizophr Res. [DOI] [PubMed] [Google Scholar]
- 54. Waters F, Collerton D, Ffytche DH, et al. Visual hallucinations in the psychosis spectrum and comparative information from neurodegenerative disorders and eye disease. Schizophr Bull. 2014;40(suppl 4):S233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Steel C. Hallucinations as a trauma-based memory: implications for psychological interventions. Front Psychol. 2015;6:1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pearse LJ, Dibben C, Ziauddeen H, Denman C, McKenna PJ. A study of psychotic symptoms in borderline personality disorder. J Nerv Ment Dis. 2014;202:368–371. [DOI] [PubMed] [Google Scholar]
- 57. Tschoeke S, Steinert T, Flammer E, Uhlmann C. Similarities and differences in borderline personality disorder and schizophrenia with voice hearing. J Nerv Ment Dis. 2014;202:544–549. [DOI] [PubMed] [Google Scholar]
- 58. Johns LC, Kompus K, Connell M, et al. Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull. 2014;40:S255–S264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sommer IEC, Daalman K, Rietkerk T, et al. Healthy individuals with auditory verbal hallucinations; Who are they? Psychiatric assessments of a selected sample of 103 subjects. Schizophr Bull. 2010;36:633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Daalman K, Diederen KM, Hoekema L, van Lutterveld R, Sommer IE. Five year follow-up of non-psychotic adults with frequent auditory verbal hallucinations: are they still healthy? Psychol Med. 2016;46: 1897–1907. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.