Abstract
Objective
Comprehensive understanding of the prevalence and quality of work disabilities and unmet needs for health care and rehabilitation to support return to work (RTW) among jobseekers.
Design
Community-level, cross-sectional analysis with multidimensional clinical work ability assessments.
Setting
Paltamo, Finland.
Participants
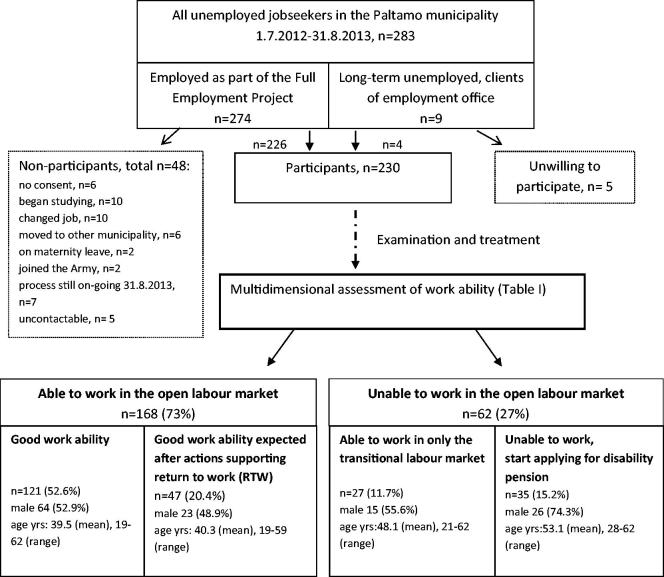
Unemployed citizens either participating in the Full-Employment Project or long-term unemployed (n = 230, 81%).
Main outcome measures
Based on data from theme interviews, patient records, supervisors’ observations of work performance and clinical examinations, a physician concluded the individual’s work ability, categorised into four groups: good work ability, good work ability expected after RTW support, able to transitional work only or unable to work. These groups were cross tabulated with primary diagnoses, types of plans to support RTW, as well as categories of social functioning and motivation, for which sensitivity and specificity scores in detecting work disability were calculated.
Results
Only about half of the jobseekers had good work ability, 27% were found unable to work in the open labour market and 15% even eligible for a disability pension. For 20%, care or rehabilitation was seen necessary to enable RTW. Poor supervisor- and self-rated performance at work or poor social functioning appeared as sensitive measures in detecting work disability.
Conclusions
Work disabilities and unmet needs for health care and rehabilitation are highly prevalent among jobseekers, as depicted using a multidimensional work ability assessment procedure inspired by the International Classification of Functioning (ICF). Further development of work ability assessment practices is clearly needed.
KEY POINTS
Although the association of unemployment with poor health is well known, evidence on the work ability of the unemployed remains scarce.
Work disabilities are common among the unemployed.
Multidimensional work ability assessment among the unemployed reveals unmet needs for care and rehabilitation to support return to work.
Context sensitivity may add to the accuracy of the doctor’s conclusions on work ability.
Keywords: Work ability, work ability assessment, multidimensional, unemployed, health inequality, rehabilitation, work disability, general practice, Finland
Introduction
Unemployment is associated with poor health in many ways.[1–4] Unhealthy workers may drift into unemployment, and unemployment may impair health.[5,6] The unemployed have unmet needs for health care.[7–10] The unemployed are nevertheless expected to be true jobseekers, capable of joining the labour market whenever a job is available. In primary care, physicians play a key role in identifying poor work ability due to poor health. Even in multidisciplinary cooperation, the final decision-making of work ability, rehabilitation or disability compensation is under the responsibility of the physician.
In the traditional ICIDH model (International Classification of Impairments, Disabilities and Handicaps, WHO 1980), a diagnosis of a disease or a disorder is the starting point for assessing functioning and work ability. The disease causes an impairment, leading to dysfunction and disability.[11] Instead, the new conceptual framework, the ICF model (International Classification of Functioning, Disability and Health, WHO 2001) [12] aims to understand and assess an individual’s functioning and work ability in a holistic manner, implying that work (dis)ability cannot simply be measured or readily determined from a diagnosis. However, ICF-based procedures for the routine assessment of the environmental and personal backgrounds of work ability are lacking.[13–17]
Three steps can be distinguished in a work ability assessment procedure: (i) collection of information, (ii) interpretation and (iii) documentation.[18] We have previously introduced a multidimensional procedure (Table 1) for assessing the work ability of individuals with multiple social and medical problems.[19] Our interest is to identify both the need for actions supporting return to work (RTW) and the need for documentation for disability benefits. Covering the three steps of assessment and the ICF, our model has been developed to be used in a primary care or occupational health care (OHC) setting. The basic idea is to first explore the overall functioning by starting the investigation with the individual’s history of social functioning, employment and performance in the contexts of daily life and personal goals, before conducting conventional medical examinations.
Table 1.
The procedure and content of the multidimensional work ability assessment, in relation to the aspects of International Classification of Functioning, Disabilities and Health (ICF)a.
| Focus | Source/method | Dimensions in ICF | |
|---|---|---|---|
| Information collected by themultidisciplinary team | History of functioning and work ability Performance at school Performance during studentship Performance during military service Labour market trajectory |
Rehabilitation counsellor appointment Theme interview Results and reports from school Definition of labour markettrajectory from documents |
Activities, Participation, Environment, Personal factors |
| Social performance Social network, family, Economic situation, housing conditions |
Rehabilitation counsellorappointment Theme interview Sociogram |
Participation, Environment | |
| Performance at work Basic skills in labour market(5 items) Performance at work and in work community (8 items) Health and physical capacity at work (1 item) Impression of the ability to work in the open labour market(3 items) |
Supervisor and participantcomplete identical forms | Activities, Participation, Environment, Personal factors | |
| Personal concerns about health and work ability Health behaviour History of health, previous examinations and rehabilitation Plans for health promotion Risk factors for common illnesses Risk factors at work |
Occupational health nurse appointment Previous medical records ordered after participant’s consent |
Personal factors Health, disease/disorder Body functions or structures |
|
| Information collected at thephysician’s appointment(s) | Preference, perceived competence and perceived opportunities to work/study Perceived work ability Own desires and plans |
Theme interview at physician appointment | Personal factors |
| Diseases and disorders Psychological health Physical capacity Intelligence Impairments |
Medical records of occupational nurse appointment, clinical measurements Dialogue Observation and clinicalexaminations Specialist consultations if needed |
Health, disease/disorder Body functions or structures Personal factors |
|
| Interpretation and conclusions of the physician | Plans for treatment, rehabilitation or other support that could support return to work (RTW) | Physician’s suggestions based on the aforementioned evidence and findings | Health, disease/disorder |
| Knowledge of the characteristics of work environment local and national labour market health and social services labour, social and health policy |
Reports of workplace visits by occupational health care Experience and know-how of the physician |
Environment | |
| functioning and work ability | Physician’s interpretation of the participant’s overall functioning and work ability after exploring all information, interviews and medical examinations | All | |
| Documentation | Plans for further treatment, rehabilitation, other support or applying for social benefits | Physician’s suggestions based on the aforementioned documents. Medical certifications for applications for rehabilitation and other social security benefits | All |
Modified from Ref. [23] in Finnish.
This is the first community-level study on jobseekers’ work ability that is based on clinical investigations. We investigated the work disabilities and needs for health care and rehabilitation of all unemployed citizens of one Finnish municipality using the multidimensional procedure. We also sought to evaluate the aspects of social functioning as diagnostic tools, and what kinds of health problems may remain undetected without systematic interpretation of functioning-related information from multiple sources.
Materials and methods
Setting and participants
In a unique Full-Employment Project (1 January 2009–31 December 2013), funded by the State of Finland, all jobseekers residing in the Finnish municipality of Paltamo (3998 inhabitants, unemployment rate 17.8% as of 31 December 2008) [20] were offered work irrespective of their age or work ability. The work was performed either within the transitional labour market (sheltered employment): at workshops founded for this purpose, producing handicrafts or woodwork and selling products, or through subcontracting staff to other employers within the open labour market.
Consequently, the newly employed workers became entitled to the statutory OHC services at the expense of the Project. As a part of the OHC action plan, it was agreed upon with the employer and the employees’ representatives that every employee in the Project will be referred for a work ability assessment in the OHC, starting from January 2012. During the following 6 months, the accuracy of the conventional health-focused work ability examinations became questioned; some of those concluded to be fit for work, performed poorly at work. The OHC action plan was then revised by replacing the health-focused work ability assessments with multidimensional work ability assessments for all employees, regardless whether conventional examinations had been conducted. The same opportunity for a multidimensional work ability assessment was offered also to those long-term unemployed jobseekers (n obs) who had preferred to remain listed as unemployed instead of assignment to the Project.
The multidimensional work ability assessments were completed between 1 July 2012 and 31 August 2013 for 230 participants, 81% of those eligible. The detailed flow of the study is presented in Figure 1.
Figure 1.
Study participants and the results of work ability assessment categorised into four groups.
Work ability assessment procedure
A multidimensional procedure (Table 1) was conducted by a multidisciplinary OHC team, including rehabilitation counsellors, nurses and physicians. The medical information was collected and kept in patient records as usual. The non-medical information on the participants’ history and present functioning was collected from records and interviews using structured forms with coded categories as described below. In addition, the supervisors provided written ratings on the participants’ work performance: satisfactory or good, irregular or training needed or poor. In the conclusion phase, all the materials collected from different sources were classified by the physician, as explained below.
First, the physician studied all anamnestic information collected by the multidisciplinary team, and tentatively classified the participant’s labour market trajectory until present. We defined four groups of labour market trajectory: unstable (short and temporary work contracts only, unemployment periods in between); blocked (entry into vocational education or labour market failed or repeatedly interrupted); broken (once established career broken and re-entry to labour market failed) and stable (established career previously, unemployed for less than 1 year before the Project).[21] Educational levels were grouped as follows: basic education (9 years or less), vocational education (12 years or less), high school (12 years) and academic degree. Social functioning was dichotomised to be good or poor; poor if any of the following applied: exceptionally sparse social network, bad housing conditions, reported or observed avoidance of social contact, or inability to take care of financial tasks, for example, debts not under control.
Second, in the interview, the preliminary hypothesis on the labour market trajectory was further tested by the physician, and the participant’s own goals and plans were highlighted. Following action theory,[22] the participant’s motivation to get a job or start studying was measured by a self-rating between 0 and 10 on the following three dimensions: own preference, own competence and perceived opportunities. The self-scalings of work ability were asked as follows: able to work, not able to work, has restrictions on working or cannot say.
Third, after completing the medical history through interviewing and clinically examining the participant (one to three appointments), the physician summarised the collected information and together with the participant, constructed plans for further examinations, care or rehabilitation when necessary. A psychologist, a psychiatrist, the local health centre or the hospital could be consulted. If conflicting information or need for clarification emerged, the multidisciplinary team was gathered for an additional appointment, together with the participant.
Finally, the physician evaluated all diagnoses and plans made, drew a conclusion on the participant’s work ability and communicated it verbally. When drawing conclusions, special attention was paid to dysfunction in any aspect of the ICF or conflicting views with the participant. In such cases, the physician raised a suspicion of a disease or disorder underlying the finding. For instance, when the client expressed no personal concerns but was found to avoid social contact, suspicions of a psychiatric disorder were raised. The examinations otherwise followed normal clinical practice and decision-making, using dialogue to reach mutual understanding with the participant. If workplace arrangements were recommended, a national-level OHC form was given to the employee to be forwarded to the supervisor. Lastly, when needed, documentation for applying for disability benefits was completed.
The work ability of the participants was categorised into four groups. Relying on the ICF, “good work ability” was indicated by not having any diseases, handicaps, limitations or impairments, or only mild forms not affecting bodily structures and functions, activities or participation at work. Those who had more severe but treatable limitations to work were classified as “good work ability expected after actions supporting RTW”. Those considered unable to work in the open labour market, yet not meeting the criteria for disability pension, were categorised as “able to work in the transitional labour market only”. With impairments estimated severe enough to meet the criteria for a disability pension, the participants were concluded to be “unable to work”. In addition, the primary diagnosis, indicating the most disabling aspect for each participant, was determined for the purposes of this study.
The team was trained to perform the multidimensional work ability assessment procedure in a uniform manner. Two physicians, specialising and experienced in OHC and rehabilitation, concluded all of the assessments. They had developed the multidimensional procedure and the form and could consult each other about the cases if necessary.
Statistical analyses
To grasp the prevalence and nature of the jobseekers’ work disabilities at the community level, we calculated the distributions of the work ability categories and the distributions of age, gender and education within these. We then cross tabulated the work ability categories across the categories of the primary diagnoses, the types of plans made to support RTW, the work ability ratings by the Project superiors and the participants themselves, the labour market trajectories, the problems in social functioning and the self-rated dimensions of motivation.
We also evaluated the accuracy of the non-medical variables in detecting work disability (able to work in the transitional labour market only or unable to any work) by counting sensitivity and specificity scores and their 95% confidence intervals for these variables. For the three dimensions of motivation, we applied Youden’s index to identify the optimal cut-off point (0–7 = poor, 8–10 = good).
All statistical analyses were undertaken using SPSS software.
Results
Of the presumably fit jobseekers, more than one-quarter (n = 62, 27%) were found unable to work in the open labour market, and one-sixth (n = 35, 15%) were eligible for a disability pension (Figure 1). The disability pension candidates were mostly men (74.3%), had no vocational education (77.2%) and a mean age of 53.1 years (range: 28–62). Of those concluded able to work (with or without support), 51.8% were men, 40.8% had no vocational education and the mean age was 40.0 yrs (range: 19–62). One in five participants (20.4%) was considered to need planned support as a precondition of RTW. Thus, only half (52.6%) of the jobseekers were considered able to work without any support.
Table 2 presents the single most disabling (i.e. primary) diagnosis for each participant, and the types of plans to support RTW. Among those unable to work, this diagnosis was most frequently psychiatric (n syc3, 37.1%). Addiction disorders appeared rarely. Among all participants, a somatic diagnosis was primary for 64.3% (n 4.348) and a psychiatric one for 20.9% (n 0.c8). Intellectual deficiency was diagnosed for 3.5% of the participants (n art). Needs for vocational advice and rehabilitation were common, found among 30% of even those with good work ability and targeted in 65% of the plans made for the group requiring support for RTW. Unmet needs for health care and treatment were detected in 16.5% of all participants (n art8), not all of which were essential to work ability (n bil0). Unmet needs for health care and rehabilitation were found in all 5-year age categories, most often among those aged 41–55 years (data not shown).
Table 2.
Descriptive characteristics across the resulting groups of work ability: type of the most disabling diagnosis (according to ICD10, one for each participant) and the types and numbers of plans made to support return to work (RTW).
| Work ability after multidimensional assessment |
||||
|---|---|---|---|---|
| Good work ability | Good work ability expected after RTW support | Able to work in thetransitional labour market only | Unable to work | |
| n(%) | n(%) | n(%) | n(%) | |
| Category (by ICD10) of the single most disabling diagnosis for each participant | ||||
| Musculoskeletal or trauma (M, S) | 34 (28.1) | 19 (40.4) | 8 (29.6) | 10 (28.6) |
| Psychiatric (F) | 12 (9.9) | 15 (31.9) | 8 (29.6) | 13 (37.1) |
| Endocrinological or respiratory (I, J) | 14 (11.6) | 6 (12.8) | 2 (7.4) | 6 (17.1) |
| Other | 27 (22.3) | 7 (14.9) | 9 (33.3) | 6 (17.1) |
| No diagnosis | 34 (28.1) | 0 (0) | 0 (0) | 0 (0) |
| Total | 121 (100) | 47 (100) | 27 (100) | 35 (100) |
| Plansa made to support return to work (RTW) | ||||
| Medical treatment | 12 (10.1) | 10 (17.5) | 4 (12.5) | 12 (34.3) |
| Physical rehabilitation | 4 (3.4) | 5 (8.8) | 3 (9.4) | 2 (5.7) |
| Psychotherapy | 1 (0.8) | 3 (5.3) | 1 (3.1) | 4 (11.4) |
| Treatment for drug abuse | 1 (0.8) | 0 (0) | 3 (9.4) | 1 (2.9) |
| Vocational instruction or rehabilitation | 36 (30.3) | 37 (64.9) | 14 (43.8) | 0 (0) |
| Studies in Finnish language | 4 (3.4) | 2 (3.5) | 2 (6.3) | 0 (0) |
| No plans needed | 66 (51.3) | 0 (0) | 5 (15.6) | 16 (45.7) |
| Total | 124 (100) | 57 (100) | 32 (100) | 35 (100) |
0–3 plans made (mean 0.7) per participant.
Table 3 shows the physician’s conclusions on work ability cross tabulated across the Project superiors’ ratings on performance at work, the participants’ self-ratings of work ability, the labour market trajectories, problems in social functioning and the self-ratings of motivational dimensions, further evaluated as sensitivity and specificity scores in Table 4.
Table 3.
Categorised non-medical covariates across the groups of work ability.
| Work ability after multidimensional assessment |
||||
|---|---|---|---|---|
| Good work ability | Good work ability expected after RTW support | Able to work in thetransitional labour market only | Unable to work | |
| n = 121 | n = 47 | n = 27 | n = 35 | |
| n (%) | n (%) | n (%) | n (%) | |
| Superior’s view of work performance | ||||
| Satisfactory or good | 108 (89.3) | 32 (68.1) | 12 (44.4) | 6 (17.1) |
| Irregular or training needed | 12 (9.9) | 10 (21.3) | 8 (29.6) | 8 (22.9) |
| Poor investigations or support of work ability are of extreme importance | 0 (0.0) | 4 (8.5) | 7 (25.9) | 20 (57.1) |
| Missing information | 1 (0.8) | 1 (2.1) | 0 (0.0) | 1 (2.9) |
| Participant’s self-scaling of work ability | ||||
| Able to work | 110 (90.9) | 10 (21.3) | 6 (22.2) | 6 (17.1) |
| Restricted ability to work | 9 (7.4) | 31 (66.0) | 17 (63.0) | 11 (31.4) |
| Unable to work | 0 (0.0) | 4 (8.5) | 2 (7.4) | 13 (37.1) |
| Cannot say | 0 (0.0) | 1 (2.1) | 1 (3.7) | 3 (8.6) |
| Missing information | 2 (1.7) | 1 (2.1) | 1 (3.7) | 2 (5.7) |
| Labour market trajectory | ||||
| Stable | 33 (27.3) | 8 (17.0) | 1 (3.7) | 1 (2.9) |
| Broken | 22 (18.2) | 12 (25.5) | 6 (22.2) | 11 (31.4) |
| Blocked (entry failed) | 14 (11.6) | 10 (21.3) | 6 (22.2) | 10 (28.6) |
| Unstable (only short contracts) | 52 (43.0) | 17 (36.2) | 14 (51.9) | 11 (31.4) |
| Other | 0 (0) | 0 (0) | 0 (0) | 2 (5.7) |
| Observed problems in social functioning | ||||
| Yesa | 16 (13.2) | 11 (23.4) | 15 (55.6) | 22 (62.9) |
| No | 105 (86.8) | 34 (72.3) | 11 (40.7) | 12 (34.3) |
| Missing information | 0 (0) | 2 (4.3) | 1 (3.7) | 1 (2.9) |
| Participant’s self-rated motivation to work or study (0–10, 0 = poor, 10 = good) | ||||
| Preference | ||||
| 0–7 | 10 (8.3) | 12 (25.5) | 12 (44.4) | 16 (45.7) |
| 8–10 | 100 (82.6) | 28 (59.6) | 13 (48.1) | 11 (31.4) |
| Missing information | 11 (9.1) | 7 (14.9) | 2 (7.4) | 8 (22.9) |
| Competence | ||||
| 0–7 | 12 (9.9) | 20 (42.6) | 19 (70.4) | 19 (54.3) |
| 8–10 | 98 (81.0) | 20 (42.6) | 6 (22.2) | 8 (22.9) |
| Missing information | 11 (9.1) | 7 (14.9) | 2 (7.4) | 8 (22.9) |
| Opportunities | ||||
| 0–7 | 61 (50.4) | 29 (61.7) | 23 (85.2) | 24 (68.6) |
| 8–10 | 49 (40.5) | 11 (23.4) | 2 (7.4) | 3 (8.6) |
| Missing information | 11 (9.1) | 7 (14.9) | 2 (7.4) | 8 (22.9) |
| Total | 121 (100) | 47 (100) | 27 (100) | 35 (100) |
At least one of the following: sparse network, avoidance of social contact, poor housing, inability to take care of own financial tasks.
Table 4.
Sensitivity and specificity scores and their 95% confidence intervals (CI) for the non-medical covariates in detecting inability to work in the open labour market (indicated as able to work in the transitional labour market only or unable to any work).
| Sensitivity % | 95% CI | Specificity % | 95% CI | |
|---|---|---|---|---|
| Supervisor’s view of work performance: less than satisfactory | 70.0 | (56.8–81.2) | 83.8 | (77.4–89.1) |
| Participant’s self-rating: work ability restricted/unable to work/cannot say | 79.3 | (66.6–88.8) | 72.3 | (64.8–78.9) |
| Labour market trajectory not stable (broken/blocked/unstable) | 96.7 | (88.7–99.6) | 24.3 | (18.0–31.4) |
| Observed problems in social functioning* | 61.0 | (47.4–73.5) | 83.2 | (76.7–88.6) |
| Low self-rated preference to work or to study (0–7/0–10) | 52.9 | (38.5–67.1) | 84.8 | (78.0–90.1) |
| Low self-rated perceived competence to work or to study (0–7/0–10) | 72.5 | (58.3–84.1) | 78.1 | (70.7–84.5) |
| Low self-rated perceived opportunities to work or to study (0–7/0–10) | 90.2 | (78.6–96.7) | 39.7 | (31.9–48.0) |
At least one of the following: sparse network, avoidance of social contacts, poor housing, inability to take care of own financial tasks.
The superiors agreed on 89.3% of cases with good work ability. Surprisingly, six workers received good superiors’ ratings but were considered unable to work. The workers’ self-ratings of good work ability and the multidimensional assessment agreed in 90% of the cases. For six workers with self-reported good work ability, applying for retirement was recommended. These participants were unaware of their impairments due to serious psychiatric disorders, mental disablement after a stroke, developmental disturbance or long-term alcohol abuse. Among those fit for the transitional labour market only, self-rated work ability was good in six (22.2%) cases.
Evaluated as diagnostic tools, the superiors’ observations of poor performance at work were sensitive (70.0%) and specific (83.8%) in relation to the physician’s conclusion on being unable to work in the open labour market. The participants’ self-ratings of poor work ability were even more sensitive (79.3%), yet less specific (72.3%).
Stable careers with less than 1 year of unemployment before the Project were strikingly rare among those judged unable to work in the open labour market. In this municipality with high unemployment rate, even those with good work ability seldom had stable labour market trajectories (27.3%) or perceived their job opportunities as good (40.5%). Correspondingly, other than stable labour market trajectory appeared as a very sensitive (96.7%), but unspecific (24.3%) predictor of not being able to work.
Problems in social functioning were rare among those with good work ability but highly prevalent among those unable to work. In detecting poor work ability, the specificity of observed social problems was as high as 84.8%.
Of the motivational dimensions, self-rated poor competence to work or to study presented with better diagnostic relevance (sensitivity; 72.5%, specificity: 78.1%) in detecting work disability than did the perceptions of poor preference and opportunities to work or to study.
Discussion
We were surprised that only half of the jobseekers were readily able to work. They all had been expected to start working if only work was available. However, half of them had minor or major unmet needs for health care, rehabilitation or other advice. For one in six, a disability pension was recommended.
Applying the new multidimensional work ability assessment, we found diseases and impairments, especially psychiatric, which had remained unrecognised in the health care and other services. Without systematic screening of contextual and functioning-related history and performance at work, the conventional health-centred practices for assessing work ability may miss potential for supporting RTW. The routinely performed categorisation of the participant’s social history and labour market trajectory and detailed future motivation were helpful in focusing and scaling the problems and creating plans. The superiors’ observations of performance at work appeared useful, often providing illustrative examples. Assessing the work ability of a jobseeker is a challenge. Some have never had paid work, to which their abilities should be compared. Moreover, the participants did not necessarily self-recognise their disabling impairments. Although client-centredness is important, the physicians cannot solely rely on self-ratings of work ability.
Our study is limited to an observational design where confounding factors cannot be ruled out. Recruiting a control group or comparing different assessment methods, blinding the assessments, or testing for inter-rater variability between the two physicians was not possible in our study setting in the Full-Employment Project. Nevertheless, the routinely collected information concerning the non-medical aspects of the ICF in addition to the normal medical examination may have provided additional diagnostic cues for the physician and enhanced the creating of context-sensitive plans. The accuracy of our multidimensional model has received external support, as a high percentage of those classified unable to work (n ork5) have been granted disability pension: 27 applications accepted (77.1%), 3 not approved (8.6%) and for 5 the decision was not available as of 31 August 2014 (14.4%). The Finnish pension system is presented in Ref.[23]
Our study adds to the evidence indicating that the unemployed have unmet needs for health care [7–10] and for support to RTW.[24] Refraining from seeking help and distrust of medical services are potential explanations for this.[25] Social support may improve the accessibility of health care.[8] In this case, the Project employer’s referral probably encouraged participation in the work ability assessment because “everybody else was taking part as well”.[26] The health care systems should recognise the fact that some unemployed people abstain from seeking care.[8]
To the best of our knowledge, there are no previous community-level reports on clinical work ability assessments among the unemployed. We accept that our results do not universally apply in terms of numbers. As the unemployment rate is high in Paltamo, the proportion of disabled individuals among the jobseekers could be even larger in areas with low unemployment rate.[5] The low educational level among our sample may in turn have increased the work disability figures through less opportunities for getting jobs that could be adaptable to disabilities.[5] Nevertheless, the structures of health care, rehabilitation, social work and labour services are alike across the nation and also widely in line with those in many developed countries. Therefore, our results showing the high prevalence of work disabilities and unmet needs for care and rehabilitation among the jobseekers reflect the inadequacy of the current service patterns. We suggest that improving context sensitivity could help in optimising the services.
How should work ability be assessed? It is difficult for specialised insurance physicians,[13] and for the unemployed citizens, it is the task of general practitioners.[27] Respecting the multidimensional nature of functioning and work ability in the ICF framework, the biomechanical measures and positivist approach only apply to the aspect of bodily functions. To create a holistic interpretation of work ability, the physician needs the skills and practical means to assess and categorise also the personal and contextual aspects of functioning.
Our work ability assessment model is an example of the ICF framework, adoptable in the primary health care setting. The general practitioners deal with several problems per consultation, necessitating good timing, ordering priorities and context sensitivity.[28] Individual care plans enable proactive, holistic and tailored care to chronically ill patients.[29] Although aiming to understand an individual’s work ability may be time-consuming, we found that the categorisations of the labour market trajectories, social functioning, work performance and the aspects of motivation were useful tools for the physician in interpreting the overall work ability. Through better understanding of personal goals and contextual factors, these categorisations might have even been time-saving when planning actions to support RTW. There is a great deal of contextual information already available for the physician who conducts work ability assessments, waiting to be systematically used for better and more accurate practice. Although a change in thinking is needed, when a physician starts from functioning-oriented information before conventional medical examinations, relatively simple alterations to the assessment practices are required. Clearly, further development research is needed to evaluate and advance the potential of this multidimensional approach of work ability assessment in primary health care and rehabilitation practices.
Ethical approval
The Ethics Committee at Northern Ostrobothnia Hospital district approved the study (293§ 106/2012), conducted in accordance with the Helsinki declaration. Written informed consent was obtained from all participants.
Disclosure statement
Raija Kerätär is the chair of the board of the company Oorninki. Jouko Soukainen is the vice-chair of the Oorninki board.
Funding
This work was supported by the Finnish Cultural Foundation from the Pehr August and Saga Stenius fund.
References
- 1.Roelfs CJ, Shor E, Davidson KW, et al. . Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med. 2011;72:840–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eliason M, Storrie D.. Job loss is bad for your health – Swedish evidence on cause-specific hospitalization following involuntary job loss. Soc Sci Med. 2009;68:1396–1406. [DOI] [PubMed] [Google Scholar]
- 3.Paul KI, Moser K.. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74:264–282. [Google Scholar]
- 4.Ala-Mursula L, Buxton JL, Ek E, et al. . Long-term unemployment is associated with short telomeres in 31-year-old men: an observational study in the Northern Finland Birth Cohort 1966. PLoS One. 2013;8:e80094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holland P, Burström B, Whitehead M, et al. . How do macro-level context and policies affect the employment chances of chronically ill and disabled people? Part I: the impact of recession and deindustrialization. Int J Health Serv. 2011;41:395–413. [DOI] [PubMed] [Google Scholar]
- 6.Virtanen P, Janlert U, Hammarstrom A. Suboptimal health as a predictor of non-permanent employment in middle age: a 12-year follow-up study of the Northern Swedish Cohort. Int Arch Occup Environ Health. 2013;86:139–145. [DOI] [PubMed] [Google Scholar]
- 7.Virtanen P, Kivimaki M, Vahtera J.. Employment status and differences in the one-year coverage of physician visits: different needs or unequal access to services? BMC Health Serv Res. 2006;6:123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Åhs A, Burell G, Westerling R. Care or not care-that is the question: predictors of healthcare utilisation in relation to employment status. Int J Behav Med. 2012;19:29–38. [DOI] [PubMed] [Google Scholar]
- 9.Nelson CH, Park J.. The nature and correlates of unmet health care needs in Ontario, Canada. Soc Sci Med. 2006;62:2291–2300. [DOI] [PubMed] [Google Scholar]
- 10.Virtanen P. Unemployment, re-employment and the use of primary health care services. Scand J Prim Health Care. 1993;11:228–233. [DOI] [PubMed] [Google Scholar]
- 11.International Classification of Impairment, Disabilities and Handicaps. Geneva: World Health Organization; 1980. [Google Scholar]
- 12.International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization; 2001. [Google Scholar]
- 13.Slebus FG, Sluiter JK, Kuijer PPFM, et al. . Work-ability evaluation: a piece of cake or a hard nut to crack? Disabil Rehabil. 2007;29:1295–1300. [DOI] [PubMed] [Google Scholar]
- 14.Claussen B. A clinical follow up of unemployed II: sociomedical evaluations as predictors of re-employment. Scand J Prim Health Care. 1993;11:234–240. [DOI] [PubMed] [Google Scholar]
- 15.Dekkers-Sánchez PM, Wind H, Sluiter JK, et al. . What factors are most relevant to the assessment of work ability of employees on long-term sick leave? The physicians’ perspective. Int Arch Occup Environ Health. 2013;86:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geyh S, Peter C, Müller R, et al. . The personal factors of the International Classification of Functioning, Disability and Health in the literature – a systematic review and content analysis. Disabil Rehabil. 2011;33:1089–1102. [DOI] [PubMed] [Google Scholar]
- 17.Schwegler U, Peter C, Trezzini B, et al. . Toward transparent documentation in medical work capacity evaluations: identifying personal factors in medical reports on Swiss disability claimants with chronic widespread pain. Int J Rehab Res. 2013;36:298–307. [DOI] [PubMed] [Google Scholar]
- 18.Spanjer J, Krol B, Brouwer S, Groothof JW.. Sources of variation in work disability assessment. Work. 2010;37:405–411. [DOI] [PubMed] [Google Scholar]
- 19.Kerätär R, Taanila A, Härkäpää K, et al. . Sairauslähtöisestä työ-ja toimintakyvyn arvioinnista monialaiseen arviointimalliin [From the disease-based assessment of work ability and functional capacity to a multidimensional assessment model] English summary. Duodecim. 2014;130:495–502. [PubMed] [Google Scholar]
- 20.Statistics Finland [Internet]. 2013. [cited 2014 Jun 29]. Available from: http://www.tilastokeskus.fi/til/vrm.html [Google Scholar]
- 21.Sepponen K, Vilen T, Kiviniemi L. Työttömyyden pitkittyminen on monen tekijän summa. Tutkimus pitkäaikaistyöttömyyteen johtavista tekijöistä ja työmarkkinoille kuntouttamisesta [Prolonged unemployment is a sum of several factors. A study of underlying factors of long term unemployment and return to work] [Internet]. 2012. [cited 2014 Jul 20]. Available from: http://www.theseus.fi/bitstream/handle/10024/47372/oamk_tkjulkaisu_50.pdf?sequence=1 [Google Scholar]
- 22.Berglind H, Gerner U.. Motivation and return to work among the long-term sicklisted: an action theory perspective. Disabil Rehabil. 2002;24:719–726. [DOI] [PubMed] [Google Scholar]
- 23.Finnish Centre for Pensions: Finnish Pension System [Internet] [cited 2016 Apr 19]. Available from: http://www.etk.fi/en/the-pension-system-2/the-pension-system/pension-benefits/
- 24.Niiranen K, Hakulinen H, Huuskonen MS, et al. . Työttömän työelämävalmiuksien tukeminen viranomaisverkostossa [Supporting basic skills in the labour market among the unemployed by authoritative network] English summary. Sos Laaketiet Aikak. 2011;48:38–52. [Google Scholar]
- 25.Westin M, Åhs A, Persson KB, et al. . A large proportion of Swedish citizens refrain from seeking medical care – lack of confidence in the medical services a plausible explanation? Health Policy. 2004;68:333–344. [DOI] [PubMed] [Google Scholar]
- 26.Kokko R, Nenonen T, Martelin T, Koskinen S. Työllisyys, terveys ja hyvinvointi – Paltamon työllistämismallin vaikutusten arviointitutkimus 2009–13. Hankkeen loppuraportti [Employment, Health, and Well-Being. The Paltamo Employment Project Evaluation Study 2009–13. Final Report] English summary. Report 18/2013. Helsinki: National Institute for Health and Welfare (THL); 2013. p. 124–131. [Google Scholar]
- 27.Wynne-Jones G, Mallen CD, Main CJ, et al. . What do GPs feel about sickness certification? A systematic search and narrative review. Scand J Prim Health Care. 2010;28:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.What do patients bring up in consultations? An observational study in general practice. Scand J Prim Health Care. 2010;33:206–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Individual care plans for chronically ill patients within primary care in the Netherlands: dissemination and associations with patient characteristics and patient-perceived quality of care. Scand J Prim Health Care. 2015;33:100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]