Abstract
Objective
To assess general practitioners’ (GPs’) information-seeking behaviour and perceived importance of sources of scientific medical information and to investigate associations with GP characteristics.
Design
A national cross-sectional survey was distributed electronically in December 2013.
Setting
Danish general practice.
Subjects
A population of 3440 GPs (corresponding to approximately 96% of all Danish GPs).
Main outcome measures
GPs’ use and perceived importance of information sources. Multilevel mixed-effects logit models were used to investigate associations with GP characteristics after adjusting for relevant covariates.
Results
A total of 1580 GPs (46.4%) responded to the questionnaire. GPs’ information-seeking behaviour is associated with gender, age and practice form. Single-handed GPs use their colleagues as an information source significantly less than GPs working in partnership practices and they do not use other sources more frequently. Compared with their younger colleagues, GPs aged above 44 years are less likely to seek information from colleagues, guidelines and websites, but more likely to seek information from medical journals. Male and female GPs seek information equally frequently. However, whereas male GPs are more likely than female GPs to find that pharmaceutical sales representative and non-refundable CME meetings are important, they are less likely to find that colleagues, refundable CME meetings, guidelines and websites are important.
Conclusion
Results from this study indicate that GP characteristics should be taken into consideration when disseminating scientific medical information, to ensure that patients receive medically updated, high-quality care.
KEY POINTS
Research indicates that information-seeking behaviour is associated with GP characteristics. Further insights could provide opportunities for targeting information dissemination strategies.
Single-handed GPs seek information from colleagues less frequently than GPs in partnerships and do not use other sources more frequently.
GPs aged above 44 years do not seek information as frequently as their younger colleagues and prefer other information sources.
Male and female GPs seek information equally frequently, but do not consider information sources equally important in keeping medically updated.
Keywords: Information seeking, general practitioners, variation, age, gender, practice form, quality of care, general practice, Denmark
Introduction
General practitioners (GPs) make decisions on how to treat the vast majority of all health-related problems in society, including who should be referred to more comprehensive investigations or treatments. GPs are expected to base these decisions on the best available scientific evidence in combination with clinical expertise and patients’ needs and wishes thus practicing “evidence-based medicine”.[1] This makes information seeking, defined as “the purposive seeking for information as a consequence of a need to satisfy some goal”, [2] a fundamental premise for all GPs delivering high-quality care. However, the knowledge base of medicine is changing rapidly and GPs need to draw on a wide range of information sources to adequately match medical knowledge to the individual patient.[3] In a busy everyday practice, the primary obstacles to information seeking are lack of time or lack of confidence that a relevant answer may be found.[4] GPs therefore prefer sources that are readily accessible, applicable to general practice, easy to use and have high quality.[5] Yet, information sources vary widely. To take an example, colleagues are often easier to access than journals, but perhaps not always as accurate.[6] Furthermore, information provided by pharmaceutical sales representatives or the like is accessible to all GPs but is potentially biased.[7]
Previous studies consistently find that colleagues and textbooks are the most frequently used information sources.[5,8,9] However, GPs in single-handed practices do not have the same access to colleagues as GPs working in partnership practices, and they might seek to compensate for this by using other sources more.
Furthermore, novel research reports an increase in the use of Internet websites and clinical practice guidelines;[10] yet, evidence suggests that GPs aged more than 50 years use the Internet significantly less than their younger colleagues.[11] Moreover, young physicians have repeatedly been shown to outperform their older colleagues on knowledge of and compliance with clinical guidelines on a variety of topics.[12–15] These findings suggest that information seeking varies with age, notably when information is sought in more recently developed information sources. However, little research has been devoted to investigating variation in information-seeking in more classic sources such as colleagues and textbooks, etc. Hence, there is a lack of knowledge of whether GPs in the older age groups seek less information (and why that may be), or if they simply prefer other information sources.
Variation in guideline adherence and knowledge has not only been reported between age groups, but also between genders. Thus, female physicians appear to do better than their male colleagues in terms of knowledge of and adherence to guidelines.[12,16,17] The question is if this difference applies only to guidelines, or if it is related to the use of other information sources as well, and whether potential discrepancies between genders can be explained by differences in the perceived importance of the information sources available.
Hence, there are good reasons to believe that GPs’ information-seeking behaviour is associated with GP characteristics. Further insight into this area may allow us to better target the dissemination of scientific research and its implementation into clinical practice. This is important because a fundamental precondition for delivering high-quality care is to keep up to date with the evidence and to use the information as an integrated part of daily patients care.
The objective of this study was to assess GPs’ information-seeking behaviour and perceived importance of medical information sources and to investigate any associations with GP characteristics.
Methods
Setting
There are two practice forms in Denmark: single-handed and partnership practices. Both can choose to work in collaboration, which implies having separate patient lists and separate economies, but sharing offices, personnel and/or clinical equipment. All Danish general practices are fully computerised with the Internet access and electronic communication with collaborators in primary and secondary healthcare.[18]
Besides the already established online medical information sources such as Medline and the Cochrane Library, Danish GPs have had online access to a “Doctors Handbook”, an online source of evidence-based medical information, since 2009.[19] Furthermore, updated information on drugs is available online only [20,21] and has been so since 2010. Participation in continuing medical education meetings and workshops (CME meetings) is voluntary according to the collective agreement between Danish GPs and Danish Regions. However, participation in CME meetings approved by the Organisation of General Practitioners in Denmark is remunerated by up to approximately 2000 Euro/year.
Study design and questionnaire
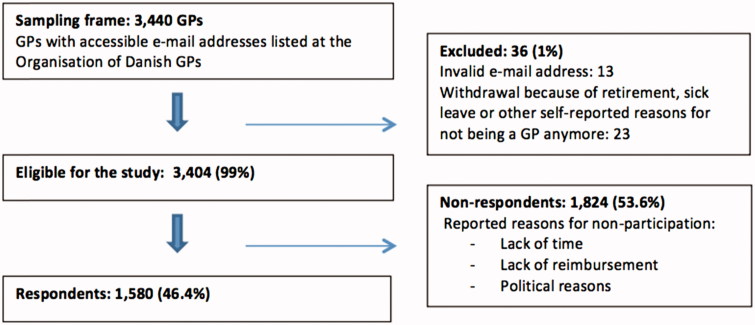
We conducted a cross-sectional survey assessing GPs’ information-seeking behaviour and perceived importance of information sources, as well as implementation activities in Danish general practices. The results reported here are from the first part of that survey. On 4 December 2013, questionnaires were distributed electronically to all GPs in Denmark who had an e-mail address registered at the Organisation of General Practitioners in Denmark (approximately 96% of all GPs in Denmark). A reminder was sent out on 7 January 2014, and the survey closed on 20 February 2014. Participation was voluntary and no financial compensation was given to responders. A flowchart of the study population is presented in Figure 1.
Figure 1.
Flowchart of the study population.
Before the questionnaire was sent out, it was tested in three steps comprising a pre-pilot study involving 14 respondents, a pilot study involving nine GPs and, finally, a qualitative pilot test inspired by “The three-step test interview” [22] that involved five GPs. Minor revisions were made before the questionnaire was distributed.
Measures included in the questionnaire
Information seeking: GPs were asked, “How often do you use the following information sources?” The sources were: GP colleagues, other medical specialists, medical books, medical journals, guidelines from the Danish College of General Practitioners (DCGP), drug information websites and medical websites. Response categories were as follows: daily, weekly, monthly, less frequently or “don’t know”.
Importance of the sources: GPs were asked to rate: “How important are the following sources for you at the moment in order to keep medically updated?” Answers were indicated on a four-point Likert response scale ranging from high importance to no importance of the same list of information sources as stated above. In addition, three information sources were added to this list: refundable CME meetings, non-refundable CME meetings and pharmaceutical sales representatives. These three sources were not included in the measures of frequency of use because they are not as readily accessible as the other sources in everyday clinical practice; nor are they applicable when GPs need to make specific clinical decisions.
Variables
The outcome variables were GPs’ reported use of different sources of information as well as the perceived importance of the various information sources. GP characteristics were used as explanatory variables. Practice form was divided into single-handed, partnership or collaborative practices based on questionnaire answers given by the GPs. Information on age and gender was obtained from the registers of the Organisation of General Practitioners in Denmark.
Statistical analysis
In order to compare the characteristics of the most frequent users with those of the less frequent users, answers were dichotomised into frequent use: yes/no. The median-split approach was applied to ensure an equal distribution between the two groups. Regarding perceived importance, a source was defined as being important to the respondent if the answers “high importance” or “some importance” were given. The answer “don’t know” was considered “not frequently used” or “not important” in the analyses.
Multilevel mixed-effects logit models were used to investigate associations between GP characteristics, and frequent use of information sources and perceived importance of the sources, respectively. Robust cluster estimation was used to account for possible clustering within practices. Both unadjusted and adjusted odds ratios (ORs) were calculated. Adjustments were made for the covariates: gender, age and practice form as presented in Tables 3 and 4, and in addition but not reported herein: status as training practice (yes/no) and GP workload (<37/37–45/>45 h/week). Adjusted ORs were used for the primary analysis and are presented with 95% confidence intervals in the tables. p Values <0.05 were considered statistically significant.
Table 3.
Associations between frequent use of information sources and GP characteristics.
| Interpersonal sources |
Printed sources |
Online sourcesc |
|||||
|---|---|---|---|---|---|---|---|
| GP colleaguesa | Other medical specialistsb | Medical booksb | Medical journalsb | DCGP guidelinesb | Drug information websitesa | Medical websitesa | |
| OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | |
| Gender | |||||||
| Female | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Male | 0.77 (0.58–1.01) | 0.83 (0.66–1.05) | 1.29 (1.04–1.61)d | 1.27 (0.98–1.63) | 0.86 (0.68–1.08) | 1.19 (0.94–1.51) | 0.94 (0.73–1.23) |
| Age | |||||||
| <45 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 45–54 | 0.56 (0.38–0.81)d | 0.68 (0.49–0.93)d | 1.15 (0.85–1.54) | 1.65 (1.19–2.28)d | 0.65 (0.48–0.90)d | 0.46 (0.33–0.64)e | 0.56 (0.38–0.82)d |
| 55–64 | 0.52 (0.36–0.75)e | 0.47 (0.34–0.64)e | 1.18 (0.88–1.57) | 2.55 (1.83–3.55)e | 0.64 (0.47–0.87)d | 0.25 (0.18–0.36)e | 0.31 (0.21–0.45)e |
| ≥65 | 0.74 (0.41–1.36) | 0.30 (0.18–0.50)e | 0.79 (0.49–1.25) | 2.17 (1.27–3.70)d | 0.55 (0.34–0.89)d | 0.13 (0.07–0.23)e | 0.11 (0.06–0.21)e |
| Practice form | |||||||
| Single-handed | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Partnership | 17.68 (9.72–32.15)e | 1.23 (0.88–1.71) | 0.79 (0.58–1.08) | 1.20 (0.83–1.71) | 1.36 (0.98–1.88) | 1.20 (0.87–1.67) | 1.04 (0.72–1.51) |
| Collaborative | 17.22 (8.70–34.08)e | 1.30 (0.84–2.01) | 0.89 (0.59–1.35) | 0.97 (0.60–1.55) | 0.96 (0.62–1.47) | 1.05 (0.68–1.64) | 1.01 (0.62–1.64) |
| N= | 1407 | 1407 | 1406 | 1406 | 1406 | 1406 | 1406 |
Frequent use defined as daily use.
Frequent use defined as daily or weekly use.
Online sources are defined as only being available online whereas printed sources can exist both in print and online.
Adjusted for gender, age, practice form, workload and status as training practice.
p value <0.05.
p value <0.001.
Table 4.
Associations between perceived importancea of information sources and GP characteristics.
| Interpersonal sources |
Printed sources |
Online sourcesb |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GP colleagues | Othermedical specialists | RefundableCME meetings | Non-refundableCME meetings | Pharmaceuticalrepresentatives | Medical books | Medical journals | DCGP guidelines | Drug informationwebsites | Medical websites | |
| OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | OR adj. (95%CI) | |
| Gender | ||||||||||
| Female | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Male | 0.45 (0.33–0.63)d | 0.76 (0.58–0.98)c | 0.32 (0.19–0.52)d | 1.36 (1.06–1.73)c | 1.57 (1.12–2.21)c | 1.18 (0.92–1.51) | 0.88 (0.67–1.15) | 0.30 (0.17–0.54)d | 0.57 (0.39–0.83)c | 0.66 (0.38–1.14) |
| Age | ||||||||||
| <45 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 45–54 | 1.03 (0.67–1.58) | 0.99 (0.69–1.42) | 1.10 (0.61–1.98) | 1.30 (0.93–1.82) | 1.03 (0.62–1.70) | 1.42 (1.03–1.95)c | 1.74 (1.22–2.47)c | 0.69 (0.34–1.38) | 0.80 (0.43–1.51) | 0.31 (0.09–1.01) |
| 55–64 | 1.05 (0.70–1.57) | 0.75 (0.54–1.05) | 1.38 (0.79–2.43) | 1.36 (0.98–1.88) | 1.81 (1.14–2.88)c | 1.77 (1.29–2.42)d | 2.13 (1.50–3.02)d | 0.75 (0.39–1.44) | 0.36 (0.20–0.62)d | 0.12 (0.04–0.37)d |
| ≥65 | 0.83 (0.47–1.48) | 0.63 (0.38–1.04) | 1.13 (0.52–2.45) | 1.09 (0.65–1.82) | 1.92 (0.98–3.78) | 1.96 (1.15–3.34)c | 2.80 (1.52–5.16)c | 0.64 (0.26–1.57) | 0.20 (0.10–0.39)d | 0.05 (0.01–0.20)d |
| Practice form | ||||||||||
| Single-handed | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Partnership | 2.11 (1.45–3.09)d | 0.81 (0.56–1.17) | 1.29 (0.75–2.19) | 0.79 (0.57–1.09) | 0.66 (0.42–1.03) | 0.69 (0.47–0.99)c | 0.98 (0.66–1.44) | 1.91 (1.02–3.58)c | 1.01 (0.64–1.59) | 0.92 (0.47–1.81) |
| Collaborative | 3.40 (1.84–6.26)d | 0.79 (0.49–1.26) | 1.04 (0.52–2.06) | 0.66 (0.42–1.04) | 0.94 (0.53–1.67) | 0.71 (0.44–1.15) | 1.10 (0.65–1.87) | 0.75 (0.35–1.58) | 1.72 (0.88–3.38) | 0.96 (0.40–2.31) |
| N= | 1392 | 1392 | 1392 | 1392 | 1392 | 1392 | 1392 | 1392 | 1392 | 1392 |
Perceived importance defined as “high importance” or “some importance” according to the answers given in the questionnaire.
Online sources are defined as only being available online whereas printed sources can exist both in print and online.
Adjusted for gender, age, practice form, workload and status as training practice.
p value <0.05.
p value <0.001.
STATA release 13.0 (StataCorp, College Station, TX) was used for all statistical analyses.
Results
Study population
A total of 1580 GPs responded (46%) and 1383 (41%) GPs answered all questions in the questionnaire. Women were slightly overrepresented among the respondents as were GPs in the two youngest age groups and GPs working in partnership practices. The characteristics of the study population are presented in Table 1.
Table 1.
Study populationa.
| Respondents |
Non-respondents |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Female | 772 | 48.9 | 803 | 43.2 |
| Male | 808 | 51.1 | 1,057 | 56.8 |
| Age | ||||
| <45 | 350 | 22.2 | 380 | 20.4 |
| 45–54 | 483 | 30.6 | 517 | 27.8 |
| 55–64 | 622 | 39.4 | 737 | 39.6 |
| ≥65 | 125 | 7.9 | 225 | 12.1 |
| Practice form | ||||
| Single-handed | 462 | 29.2 | 621 | 33.4 |
| Partnership | 1,118 | 70.8 | 1,239 | 66.6 |
Based on the Organisation of General Practitioners’ registers. Note that collaborative practice is not included as it is a self-reported variable and therefore only available in the survey data.
Frequent use of information sources
Three sources were used daily by 50% or more of the respondents: medical websites, drug information websites and conference with GP colleagues. These three sources were also the most frequent sources reported used on a daily or weekly basis (Table 2).
Table 2.
GPs’ Use and perceived importance of information sources.
| Use |
Perceived |
|||||
|---|---|---|---|---|---|---|
| Daily |
Daily/Weekly |
importance |
||||
| N | % | N | % | N | % | |
| Interpersonal sources | ||||||
| GP colleagues | 703 | 50% | 1055 | 75% | 1149 | 83% |
| Other medical specialists | 69 | 5% | 661 | 47% | 1047 | 75% |
| Refundable CME meetings | n.a | n.a | 1261 | 91% | ||
| Non-refundable CME meetings | n.a | n.a | 415 | 32% | ||
| Pharmaceutical representatives | n.a | n.a | 238 | 17% | ||
| Printed sources | ||||||
| Medical books | 197 | 14% | 727 | 52% | 934 | 67% |
| Medical journals | 74 | 5% | 1000 | 71% | 1067 | 77% |
| DCGP guidelines | 183 | 13% | 799 | 57% | 1252 | 90% |
| Online sources | ||||||
| Drug information websites | 729 | 52% | 1,044 | 74% | 1236 | 89% |
| Medical websites | 875 | 62% | 1286 | 91% | 1304 | 94% |
n.a.: not applicable, not included in the questionnaire.
Perceived importance of information sources
Most important were the following: medical websites, refundable CME meetings and DCGP guidelines. With the exception of non-refundable CME meetings and pharmaceutical sales representatives, all of the other sources were perceived as being important by a majority of GPs (Table 2).
Associations between frequent use of information sources and GP characteristics(Table 3)
Compared with their younger colleagues, GPs aged more than 44 years were more likely to seek information from medical journals and significantly less likely to seek information frequently from colleagues and other medical specialists, DCGP guidelines and websites.
GPs working in partnerships or collaborative practices were significantly more likely to seek information from GP colleagues than were single-handed GPs. Furthermore, while there was a non-statistically significant tendency towards female GPs to seek information from interpersonal sources more frequently than male GPs (GP colleagues: OR: 0.77 (CI: 0.58–1.01); other specialists: OR: 0.83 (CI: 0.66–1.05)), male GPs were found to be significantly more likely to seek information from medical books than female GPs.
Associations between the perceived importance of information sources and GP characteristics (Table 4)
While the frequency of use differed little between genders, male GPs were significantly less likely than their female colleagues to perceive almost all of the sources as being important. However, they were more likely to perceive pharmaceutical sales representatives and non-refundable CME meetings as being important. A similar though non-statistically significant trend was found for practice forms as GPs working in a partnership found that pharmaceutical representatives and non-refundable CME meetings were less important than single-handed GPs did (OR: 0.66 (CI: 0.42–1.03) and OR: 0.79 (CI: 0.57–1.09), respectively). Furthermore, compared with single-handed GPs, GPs in partnership practices found that medical books were significantly less important and that guidelines were significantly more important. Regarding age groups, the differences in perceived importance did not entirely reflect the differences found in frequencies of use either, as DCGP guidelines, other medical specialists and GP colleagues were less frequently used by GPs aged more than 44 years, but not perceived as being less important. Nonetheless, the perceived importance reflected the frequency of use for websites and medical journals.
Discussion
Statement of principal findings
Medical websites were used weekly by 91% of the GPs and were thus the most frequently used information source. The second most frequently used information source was conferences with GP colleagues (75%), closely followed by drug information websites (74%). All of the investigated sources were rated as important by a majority of the GPs (range 67–94%), albeit with a few exceptions: pharmaceutical sales representatives (17%) and non-refundable CME-meetings (32%).
Age was the single most important factor in determining the use of information sources, whereas, in rating the sources by importance, gender proved to be the factor associated with most significant differences.
Strengths and weaknesses of the study
Register data and email addresses obtained from the Organisation of General Practitioners in Denmark made it possible to invite approximately 96% of all Danish GPs to participate in the survey and to acquire valid background information on both respondents and non-respondents (gender, age and practice form). This allowed for a qualified evaluation of the representativeness of the study population.
In total, 46% participated in the survey. This raises questions as to the generalisability of the results. If responding GPs are more engaged in information-seeking than non-respondents, there is a risk that the overall use and perceived importance are overestimated in the present study. Moreover, in the association analyses, age, gender and practice form were found to be explanatory factors related to information-seeking. Hence, non-response bias might also affect the results. However, as can be observed from Table 1, the difference between the characteristics of responders and non-responders was not very pronounced and extensive sampling ensured that much of the GP population was, indeed, covered.
Using self-reported data carry a risk of introducing recall and reporting errors. To reduce the risk of reporting errors it was emphasised to the GPs that all data handling would be strictly anonymous, and that the results were expected to benefit the on-going development of general practice.
We do not know whether GPs’ processes of care actually improve as a result of their information-seeking behaviour. However, quality of care measured as guideline adherence has previously been associated with age and gender, which is in line with our results on use and perceived importance of guidelines.
Future studies should focus on confirming reported information-seeking behaviour through observation, and on further assessing associations with quality of care.
Findings in relation to other studies
Although other studies also report an increase in the use of online sources,[10,23] the level of use found in this study is considerably higher than the levels previously reported. This may be part of a continuous move towards sources that are more accessible, well developed and easy to use. Moreover, since 2010, drug information websites have been the only available updated resource for drug information in Denmark.
It is well recognised that most of the information that GPs use when seeing patients is obtained from memory.[3] This introduces a risk that the information could be out of date or incorrect.[3] According to the present study, this risk may increase with increasing age as GPs aged more than 44 years less frequently consulted guidelines, drug information websites and medical websites, which, along with medical journals, have the prospects of bearing the most updated information. Furthermore, the first barrier to physicians’ adherence to guidelines is a lack of awareness of these guidelines,[24] and doctors in the youngest age groups have repeatedly been shown to have a better knowledge of guidelines and higher adherence to new recommendations than their older colleagues.[12–15] Younger doctors’ more frequent use of websites as an information source has also been reported elsewhere.[11,25] However, in the present study, GPs >44 years of age more often sought information from medical journals and found them to be more important in keeping medically updated. Medical journals represent a more detailed and unrefined type of knowledge than guidelines.[26] An explanation for these findings could therefore be that younger and more inexperienced GPs prefer explicit recommendations (third-generation knowledge), whereas more experienced GPs prefer the unrefined types of knowledge (first-generation knowledge). It is equally possible that older GPs prefer journals because they are more familiar to them than online sources of information. Also, GPs aged more than 44 years may not feel the same need as younger GPs for seeking the tacit knowledge provided by colleagues. It should not be forgotten, though, considering the frequency of use of information sources, that GPs in general only search for answers to about one third of all questions that arise during consultation,[8,27] and presumably inexperienced GPs generate more questions than experienced GPs. Hence, inexperienced GPs would naturally more frequently have a need for accessing readily accessible sources like for instance websites and GP colleagues. Nevertheless, the results may indicate the presence of competency traps in general practice, where experienced GPs favour their well-established routines instead of seeking new ones[28] and therefore do not update their medical knowledge to the same extent as young GPs.
We found that GPs in partnership practices have a 17 times higher OR of consulting frequently with GP colleagues than single-handed GPs. Although this difference appears high, it is intuitive. What is not clear is whether the twice as high OR of perceiving that colleagues are an important source, which was found for GPs working in partnership, is due to convenience or because they are believed to be authoritative.
The past decade appears to have seen a substantial decline in GPs’ reliance on the pharmaceutical industry as an important source for keeping medically updated.[10,29] However, a non-statistically significant trend was found that single-handed GPs are less sceptical towards the pharmaceutical industry than GPs working in partnership practice. Together with results from previous research showing that single-handed GPs see pharmaceutical representatives more frequently than GPs working in large partnerships,[30] these findings may imply that, regardless of practice form, GPs require professional discussions and that single-handed GPs have to rely on potentially biased sources [7] to a greater extent than GPs in partnership practices. However, it should be noted that only 17% of all GPs perceived pharmaceutical representatives as an important source of information.
Furthermore, the results of the present study show that male GPs value guidelines and other sources less than females do, which may contribute to explain previous research findings that female doctors are more inclined to adhere to recommendations than their male colleagues.[12,16,17] Surprisingly, no significant differences in the actual frequency of use in the present study were found to support these previous findings. This indicates that even though male and female GPs seek information to the same extent their perceptions of information sources affect their adherence to recommendations, which could have consequences for the quality of care provided.
Meaning of the study
Three areas deserve extra attention: First, GPs aged more than 44 years do not seek information from colleagues, guidelines, medical websites and drug information websites as frequently as their younger colleagues. Hence, they may be at a higher risk of overlooking new information, including recommendations. Also, today’s focus on developing guidelines and medical websites may not sufficiently consider the information needs of this group of GPs. Second, single-handed GPs may have a need to be provided with better opportunities for professional discussions in their everyday practice. Third, further research is needed regarding men’s and women’s different perceptions of the importance of different information sources and the potential association of these perceptions with the quality of care delivered.
Although these findings are based on data from a Danish population of GPs, it is likely that the results may be applicable to other Western countries, too.
Conclusions
GPs’ information-seeking behaviour appears to be evolving concurrently with the development of new information sources. The choice of source as well as the perception of its importance are associated with the GP’s age, gender and practice form. The results of the present study indicate that GP characteristics should be taken into consideration when disseminating scientific medical information to ensure that patients are provided with medically updated, high-quality care.
Acknowledgements
The authors wish to thank all of the GPs for participating in the survey. Also, we take this opportunity to extend our gratitude to secretary Merete Moll Lund for proofreading the manuscript and to Statistician Pia Veldt Larsen for assisting with the statistical analyses.
Ethical approval
The Danish Data Protection Agency approved this study (record no. 2012-41-0178). According to Danish legislation, no approval from the Regional Scientific Ethical Committees for Southern Denmark was required.
Disclosure statement
All authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Funding
Financial support for this study was provided in part by a grant from the independent charity The Health Foundation (2013B070).
References
- 1.Greenhalgh T, Howick J, Maskrey N. Evidence Based Medicine Renaissance G . Evidence based medicine: a movement in crisis? BMJ. 2014;348:g3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson TD. Human information behavior. Informing Sci. 2000;3:49–56. [Google Scholar]
- 3.Smith R. What clinical information do doctors need? BMJ. 1996;313:1062–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook DA, Sorensen KJ, Wilkinson JM, et al. Barriers and decisions when answering clinical questions at the point of care: a grounded theory study. JAMA Int Med. 2013;173:1962–1969. [DOI] [PubMed] [Google Scholar]
- 5.Dawes M, Sampson U.. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform. 2003;71:9–15. [DOI] [PubMed] [Google Scholar]
- 6.Schaafsma F, Verbeek J, Hulshof C, et al. Caution required when relying on a colleague's advice; a comparison between professional advice and evidence from the literature. BMC Health Serv Res. 2005;5:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melander H, Ahlqvist-Rastad J, Meijer G, et al. Evidence b(i)ased medicine-selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applications. BMJ. 2003;326:1171–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Gonzalez AI, Dawes M, Sanchez-Mateos J, et al. Information needs and information-seeking behavior of primary care physicians. Ann Fam Med. 2007;5:345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coumou HC, Meijman FJ.. How do primary care physicians seek answers to clinical questions? A literature review. J Med Libr Assoc. 2006;94:55–60. [PMC free article] [PubMed] [Google Scholar]
- 10.Kosteniuk JG, Morgan DG, D'Arcy CK.. Use and perceptions of information among family physicians: sources considered accessible, relevant, and reliable. J Med Lib Assoc. 2013;101:32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernard E, Arnould M, Saint-Lary O, et al. Internet use for information seeking in clinical practice: a cross-sectional survey among French general practitioners. Int J Med Inform. 2012;81:493–499. [DOI] [PubMed] [Google Scholar]
- 12.Chauvel N, Le Vaillant M, Pelletier-Fleury N.. Variation in HbA1c prescription for patients with diabetes in French general practice: an observational study prior to the implementation of a P4P programme. Eur J Public Health. 2013;23:61–66. [DOI] [PubMed] [Google Scholar]
- 13.Choudhry NK, Fletcher RH, Soumerai SB.. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142:260–273. [DOI] [PubMed] [Google Scholar]
- 14.Van Hoecke H, Vandeplas G, Acke F, et al. Dissemination and implementation of the ARIA guidelines for allergic rhinitis in general practice. Int Arch Allergy Immunol. 2014;163:106–113. [DOI] [PubMed] [Google Scholar]
- 15.Doroodchi H, Abdolrasulnia M, Foster JA, et al. Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam Pract. 2008;9:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berthold HK, Gouni-Berthold I, Bestehorn KP, et al. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med. 2008;264:340–350. [DOI] [PubMed] [Google Scholar]
- 17.Kuo DZ, Robbins JM, Burns KH, et al. Individual and practice characteristics associated with physician provision of recommended care for children with special health care needs. Clin Pediatr (Phila). 2011;50:704–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pedersen KM, Andersen JS, Sondergaard J.. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25:S34–S38. [DOI] [PubMed] [Google Scholar]
- 19.Lægehåndbogen. About Lægehåndbogen; 2012. [updated 2012 Dec 1; cited 2016 Feb 15]. Available from: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/om-laegehaandbogen/in-english/.
- 20.Pro.medicin.dk ; 2016. [updated 2016 Jan 27; cited 2016 Feb 15]. Available from: http://pro.medicin.dk/Artikler/Artikel/52.
- 21.Institute for Rational Pharmacotherapy About IRF; 2012. [updated 2012 Jun 22; cited 2016 Feb 15]. Available from: http://www.irf.dk/en/about_irf/om_irf.htm.
- 22.Hak T, van der Veer K, Ommundsen R.. An application of the three‐step test‐interview (TSTI): a validation study of the Dutch and Norwegian versions of the ‘Illegal Aliens Scale’. Int J of Soc Res Methodol. 2006;9:215–227. [Google Scholar]
- 23.Bennett NL, Casebeer LL, Kristofco R, et al. Family physicians' information seeking behaviors: a survey comparison with other specialties. BMC Med Inform Decis Mak. 2005;5:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. [DOI] [PubMed] [Google Scholar]
- 25.Bynum SA, Malo TL, Lee JH, et al. HPV vaccine information-seeking behaviors among US physicians: government, media, or colleagues? Vaccine. 2011;29:5090–5093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: Time for a map? J Contin Educ Health Prof. 2006;26:13–24. [DOI] [PubMed] [Google Scholar]
- 27.Ely JW, Osheroff JA, Chambliss ML, et al. Answering physicians' clinical questions: obstacles and potential solutions. J Am Med Inform Assoc. 2005;12:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carroll JS, Edmondson AC.. Leading organisational learning in health care. Qual Saf Health Care. 2002;11:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nylenna M, Aasland OG.. Primary care physicians and their information-seeking behaviour. Scand J Prim Health Care. 2000;18:9–13. [DOI] [PubMed] [Google Scholar]
- 30.Watkins C, Moore L, Harvey I, et al. Characteristics of general practitioners who frequently see drug industry representatives: national cross sectional study. BMJ. 2003;326:1178–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]