Introduction
Studying the performance of medical students with disabilities requires a better understanding of the prevalence and categories of disabilities represented.1–4 It remains unclear how many medical students have disabilities; prior estimates are out-of-date and psychological, learning, and chronic health disabilities have not been evaluated.5 This study assessed the prevalence of all disabilities and the accommodations in use at allopathic medical schools in the United States.
Methods
Between December 2014 and February 2016 an electronic, web-based survey was sent to institutionally designated disability administrators at eligible allopathic medical schools who have a federally mandated duty to assist qualified students with disabilities. Eligible schools were identified through a registry maintained by the Association of American Medical Colleges (AAMC); new schools and those with probationary accreditation or on probation were excluded. Participation was maximized through direct emails to disability administrators, AAMC outreach to Students Affairs deans at eligible schools encouraging participation, and phone calls to non-responding schools after 6 and 9 months.
The survey was designed by experts in medical school disability administration based on provisions of the Americans with Disabilities Act and prior research. The survey was pilot tested by 5 schools and refined. The survey assessed the following domains: (1) total number of self-disclosed/registered students with disabilities receiving accommodations, (2) demographic characteristics of students with disabilities, (3) categories of disabilities, and (4) approved accommodations. Disability categories included: attention deficit hyperactivity disorder (ADHD), learning disability, psychological disability (adjustment disorder, anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder, bipolar disorder, depressive disorder, eating disorder, cognitive disorder, autism spectrum disorder, schizophrenia, other psychotic disorders), deaf and hard of hearing, visual impairment, mobility disability, chronic health, and other functional impairment.
Survey results were linked to the AAMC’s Organizational Characteristics Database, which provided additional information about regional, ownership, and financial characteristics of medical schools. Descriptive statistics were used to summarize survey results. The study was deemed exempt by the University of California, San Francisco Institutional Review Board because school-level data were analyzed in a de-identified manner.
Results
One hundred forty-five schools were identified; 12 were excluded. Of the 133 eligible schools, 91 completed the survey (68.4%) and 89 reported complete data and were included in the analysis. Most schools were located in the south (32.6%) and were publicly owned (57.3%) (Table). Responding schools were similar to non-responding schools on geographic region, public-versus-private ownership, community-based status, research intensity, and financial relationship with the parent university.
Table 1.
Characteristics of Students with Disabilities and Participating Medical Schoolsa
| Students (N=1547) | ||
|---|---|---|
| Student characteristics | No. | Percent |
| Students receiving accommodations | 1512 | 97.7 |
| Type of disability | ||
| Attention Deficit Hyperactivity Disorder | 522 | 33.7 |
| Learning disability | 333 | 21.5 |
| Psychological disabilityb | 310 | 20.0 |
| Deaf or hard of hearing | 34 | 2.2 |
| Visual impairment | 46 | 3.0 |
| Mobility disability | 39 | 2.5 |
| Chronic health issue | 202 | 13.1 |
| Other functional impairmentc | 61 | 3.9 |
| School characteristicsd | Schools (N=89) | |
| Public ownership (vs. private ownership) | 51 | 57.3 |
| School region | ||
| Central | 20 | 22.5 |
| Northeast | 26 | 29.2 |
| Southern | 29 | 32.6 |
| Western | 14 | 15.7 |
| Financially integrated with parent university (vs. other)e | 75 | 84.3 |
| Community-based school (vs. not)f | 14 | 15.7 |
Data are reported for 89 of 91 responding schools (97.8%) that reported complete data for disability type. Gender information (not shown in table) was complete for 86 of 91 responding schools (94.5%); among these schools, 648 (43.3%) students with disabilities were male and 849 were female (56.7%).
Psychological disabilities included the following: adjustment disorder, anxiety disorder, obsessive-compulsive disorder, post traumatic stress disorder, bipolar disorder, depression, eating disorder, cognitive disorder, schizophrenia or other psychotic disorder, and other psychological disability.
Other functional impairment included non-mental health related disorders that do not fall into one of the prescribed categories of disability, but that result in a functional impairment for the student and render them eligible for accommodations and protection under the Americans with Disabilities Act; an example would be loss of a limb resulting in the need for assistive technology but that does not cause mobility issues or chronic health issues.
School characteristics are from the Association of American Medical College’s (AAMC) Organizational Characteristics Database.
Financial integration with parent university refers to a medical school for which budget and financing are subject to parent university authorization. This is in comparison to free-standing medical schools or those that are financially autonomous.
A community-based medical school relies on community hospitals or clinical facilities to achieve their educational mission rather than a traditional academic medical center hospital and received full accreditation in 1972 or later (after the "community-based" movement in medical education).
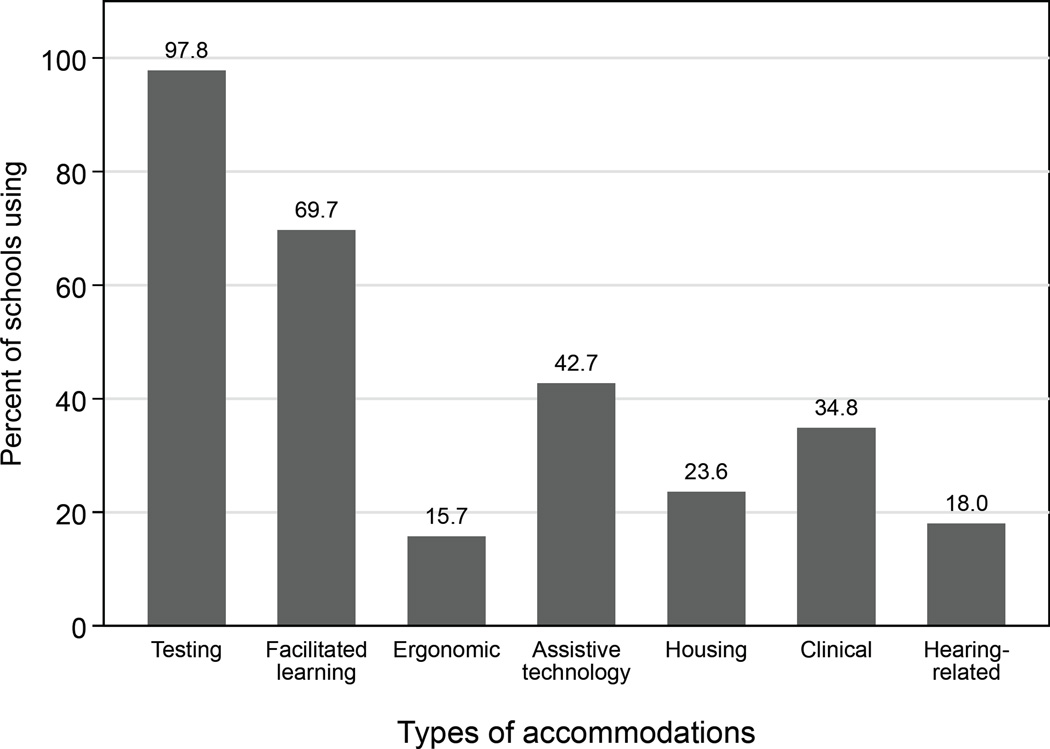
Respondents identified 1,547 students with disabilities (43/3% male), representing 2.7% of the total enrollment and ranging from 0% to 12%. Of these students, 97.7% received accommodations (Table). ADHD was the most common disability (33.7%), followed by learning disabilities (21.5%) and psychological disabilities (20.0%). Mobility and sensory disabilities were less common. School-based testing accommodations were most frequently used (97.8%); clinical accommodations were less frequent (Figure).
Figure 1. Types of Accommodations Used by US Allopathic Medical Schools.
Testing refers to extra time used for school-based exams (including time and a half and double time), use of low distraction or private environments, and testing breaks. Facilitated learning refers to flexible attendance, note takers, Live Scribe Pen, recorded lectures, and preferential seating. Ergonomic refers to ergonomic evaluation and equipment. Assistive technology refers to textbooks in alternate formats, text-to-speech, speech-to-text computer programs. Housing refers to living accommodations such as single room housing, release from housing, assistance animal (e.g., therapy dogs), service animal, and reserved parking. Clinical refers to clinical placement, deferred clinical year, leave of absence, and release from overnight call. Hearing-related refers to use of transcriptionist, Communication Access Real-time Translation (CART), sign language interpreter, specialized phone, and specialized pager.
Discussion
This study identified a higher prevalence of disability among students in US allopathic medical schools—2.7%—than prior studies (0.3% to 0.6%).3,5 These results underscore the limitations of studying isolated subtypes of disabilities (ie, only mobility impairments), which may underestimate this population.6 The preponderance of students with ADHD, learning disabilities, and psychological disabilities suggests that these disability subtypes should be included in future research efforts, such as studies assessing the performance of appropriately accommodated students.
Schools reported incomplete student demographic data, precluding analysis. Also, students who did not self-disclose were not captured, nor was severity of disability—however, medical documentation is required for disability registration. Given the stigma surrounding psychological disabilities, it is plausible that these disabilities were underrepresented. Schools responding to the survey may not be representative of all allopathic medical schools and may not generalize to osteopathic schools. Finally, these prevalence estimates rely on the accuracy of the data reported by schools; however, schools are under a federal mandate to document communication and decision-making regarding students with disabilities, supporting the accuracy of these data.
Acknowledgments
The authors thank Matthew Smith, PhD (Feinberg School of Medicine: Northwestern University), for help with survey development and recruitment; Jayme Bograd (Association for American Medical Colleges) and the Association for American Medical Colleges GSA Group for their help with recruitment; Neera Jain, CRC, MS (University of California, San Francisco) for contributions to the construction of the database and data collection; Judith Wentz, MA (University of California, San Francisco) for assisting with data collection and data checking; and Lauren Nicholas, PhD (Johns Hopkins University) for suggestions on the manuscript. The authors are indebted to disability administrators from the responding medical schools for their attention to detail and time commitment to completing the survey. No compensation was provided for any of the persons involved.
Funding/Support: Dr. Herzer is supported by Medical Scientist Training Program grant T32GM007309-41 from the National Institute of General Medical Sciences and the National Institute on Aging Grant R36AG051727.
Role of the Funders/Sponsors: The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author Contributions: Drs. Meeks and Herzer had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Meeks.
Acquisition, analysis, or interpretation of data: Meeks, Herzer.
Drafting of the manuscript: Meeks, Herzer.
Critical revision of the manuscript for important intellectual content: Meeks, Herzer.
Statistical analysis: Herzer.
Obtained funding: Meeks, Herzer.
Administrative, technical, or material support: Meeks.
Study supervision: Meeks, Herzer.
Conflict of Interest Disclosures: All authors have no potential conflicts of interest to disclose.
REFERENCES
- 1.Zazove P, Case B, Moreland C, et al. US medical schools' compliance with the Americans with Disabilities Act: findings from a national study. Acad Med. 2016 doi: 10.1097/ACM.0000000000001087. [DOI] [PubMed] [Google Scholar]
- 2.Teherani A, Papadakis MA. Clinical performance of medical students with protected disabilities. JAMA. 2013;310(21):2309–2311. doi: 10.1001/jama.2013.283198. [DOI] [PubMed] [Google Scholar]
- 3.Searcy CA, Dowd KW, Hughes MG, Baldwin S, Pigg T. Association of MCAT scores obtained with standard vs extra administration time with medical school admission, medical student performance, and time to graduation. JAMA. 2015;313(22):2253–2262. doi: 10.1001/jama.2015.5511. [DOI] [PubMed] [Google Scholar]
- 4.Gostin LO. The Americans with Disabilities Act at 25: the highest expression of American values. JAMA. 2015;313(22):2231–2235. doi: 10.1001/jama.2015.6405. [DOI] [PubMed] [Google Scholar]
- 5.Eickmeyer SM, Do KD, Kirschner KL, Curry RH. North American medical schools’ experience with and approaches to the needs of students with physical and sensory disabilities. Acad Med. 2012;87(5):567–573. doi: 10.1097/ACM.0b013e31824dd129. [DOI] [PubMed] [Google Scholar]