Abstract
Background
The goal of this study was to compare early postoperative outcomes and actuarial-free survival between patients who underwent repair of acute Type A aortic dissection with axillary or femoral artery cannulation.
Methods
A total of 305 patients from five academic medical centers underwent acute Type A aortic dissection repair via axillary (n = 107) or femoral (n = 198) artery cannulation between January 2000 and December 2010. Major morbidity, operative mortality, and 5-year actuarial survival were compared between groups. Multivariate logistic regression was used to determine predictors of operative mortality, and Cox regression hazard ratios were calculated to determine predictors of long-term mortality.
Results
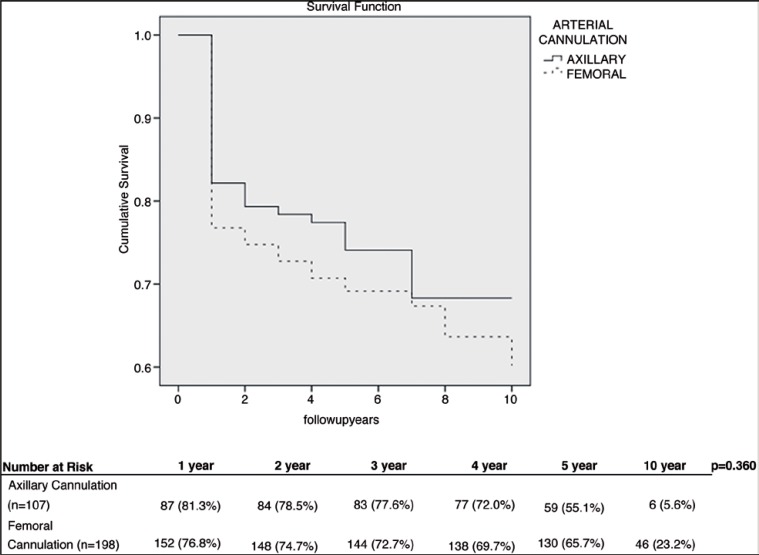
Operative mortality was not influenced by cannulation site (16% for axillary cannulation vs. 19% for femoral cannulation, p = 0.64). In multivariate logistic regression analysis, hemodynamic instability (p < 0.001) and prolonged cardiopulmonary bypass time (>200 min; p = 0.05) emerged as independent predictors of operative mortality. Stroke rates were comparable between the two techniques (14% for axillary and 17% for femoral cannulation, p = 0.52). Five-year actuarial survival was comparable between the groups (55.1% for axillary and 65.7% for femoral cannulation, p = 0.36). In Cox regression analysis, predictors of long-term mortality were: age (p < 0.001), stroke (p < 0.001), prolonged cardiopulmonary bypass time (p = 0.001), hemodynamic instability (p = 0.002), and renal failure (p = 0.001).
Conclusions
The outcomes of femoral versus axillary arterial cannulation in patients with acute Type A aortic dissection are comparable. The choice of arterial cannulation site should be individualized based on different patient risk profiles.
Keywords: Aortic dissection, Outcomes, Axillary cannulation, Femoral cammulation, Aorta, Dissection
Introduction
Acute Type A aortic dissection is a cardiovascular emergency with a risk of serious postoperative morbidities and death [1-6]. Surgical repair requires a nondiseased arterial cannulation site for cardiopulmonary bypass (CPB); the most commonly used sites are the right axillary and common femoral arteries [7, 8]. Improvements in surgical technique have led to decreases in operative mortality and adverse clinical outcomes in the modern era, which have been accompanied by a shift in cannulation site from the femoral artery to the axillary artery [1, 9, 10].
There is still considerable debate regarding the optimal cannulation site for maximizing long-term survival [2, 6, 11-15]. It has been hypothesized that cannulation of the femoral artery reverses flow in the thoracoabdominal aorta, which increases the risk of brain or organ malperfusion in those undergoing Type A aortic dissection repair [13, 16]. A recent meta-analysis found central cannulation, including the axillary artery, to be superior to peripheral cannulation of the femoral artery in the short term [17].
Our study sought to evaluate whether patients repaired with axillary artery cannulation have better clinical outcomes and long-term actuarial survival following acute Type A aortic dissection compared to patients repaired with femoral artery cannulation.
Methods
Patients
The Society of Thoracic Surgeons Databases at Beth Israel Deaconess Medical Center, Carolinas Medical Center, Missouri Baptist Medical Center, Meijer Heart and Vascular Institute, and University of Iowa Hospitals and Clinics were queried to identify all patients who underwent aortic dissection repair between January 2000 and December 2010. A total of 305 patients underwent repair for acute Type A aortic dissections, of which 107 repair procedures used axillary artery cannulation and 198 used femoral artery cannulation. Patients excluded were those who presented with Type A aortic dissection and did not have surgery, whose dissections were repaired using alternative sites of arterial cannulation, or whose axillary and femoral arteries were both used during repair. No serious complications specific to the femoral or axillary cannulation were reported. No crossover patients who started repair using one mode of cannulation and switched to the other were reported.
A preoperative diagnosis of aortic dissection was accomplished using computed tomography angiography or transesophageal echocardiography (TEE). The diagnosis was later confirmed at the time of operation. A database was created for entry of demographics, preoperative data, procedural data, and postoperative outcomes, which were prospectively entered by dedicated data-coordinating personnel. Long-term survival data were obtained from the Social Security Death Index, prior to censorship (http://www.genealogybank.com/gbnk/ssdi/). Follow-up was 97% complete.
Prior to this analysis, study approval from the Institutional Review Boards of each center was obtained. Consistent with the Health Insurance Portability and Accountability Act of 1996, patient confidentiality was consistently maintained.
Definitions
The Society of Thoracic Surgeons national cardiac surgery database definitions were used for this study. Acute Type A dissection was defined as any dissection that involved the ascending aorta with presentation within 2 weeks of symptom onset. Previous cerebrovascular accident was defined as a history of central neurologic deficit persisting for >24 h. Chronic renal insufficiency was defined as a serum creatinine value >2.0 mg/dL. Diabetes was defined as a history of diabetes mellitus, regardless of disease duration or need for oral agents or insulin. Recent myocardial infarction was defined as myocardial infarction occurring within 7 days. Depressed ejection fraction was defined as ejection fraction <40%. Hemodynamic instability was defined as hypotension (systolic blood pressure <80 mm Hg) or the presence of cardiac tamponade, shock, acute congestive heart failure, myocardial ischemia, and/or infarction. Prolonged ventilatory support was defined as postoperative pulmonary insufficiency requiring ventilatory support >24 h. Postoperative stroke was defined as any new major (Type I) neurologic deficit presenting in-hospital and persisting >72 h. Acute renal failure was defined as one or both of the following: (1) an increase in the serum creatinine to >2.0 mg/dL and/or a >two-fold increase in the most recent preoperative creatinine level or (2) a new requirement for dialysis, postoperatively. Operative mortality includes both (1) all deaths occurring during the hospitalization in which the operation was performed (even if death occurred after 30 days from the operation), and (2) those deaths occurring after discharge but within 30 days of the procedure.
Operative Technique
Intraoperatively, the diagnosis of Type A aortic dissection was confirmed by TEE for all patients. A median sternotomy was performed. CPB was instituted by arterial cannulation of the femoral or right axillary artery and venous cannulation of the right atrium. The axillary artery was cannulated by suturing an 8- or 10-mm graft whereas the femoral artery (with a good pulse) was accessed by cutdown and direct cannulation. The decision whether to clamp the ascending aorta was based on the individual surgeon’s decision. Cold blood cardioplegia administration was performed through an antegrade approach via the ostia of the coronary arteries and/or a retrograde approach through the coronary sinus, to ensure myocardial protection. The right superior pulmonary vein provided access for vent placement in the left ventricle. Restoration of the aortic root was accomplished by resection of the intimal tear followed by repair or resuspension of the aortic valve and replacement of the ascending aorta. After reaching the temperature range of 10°C to 20°C for deep hypothermic circulatory arrest or 21°C to 28°C for moderate hypothermic circulatory arrest, the aortic clamp was removed, and the aortic arch was examined. The distal anastomosis was then completed either using a hemiarch or clamp-on technique. Antegrade aortic perfusion was established. If the aortic valve and sinuses were normal, resuspension of the aortic valve was performed by placing three polypropelene pledgeted sutures at the three valve commisures along with replacement of the ascending aorta with a straight tube graft. If the aortic valve was structurally abnormal but the sinuses were normal, we performed aortic valve replacement with mechanical or tissue prosthesis and supracoronary aortic grafting. If the aortic valve and sinuses were abnormal due to dilation (>5 cm) or extension of the intimal tear to the valve, aortic root replacement (modified Bentall operation) with a tissue or mechanical valve-conduit was used. Teflon (polytetrafluoroethylene) strips were used to reinforce the proximal and distal anastomoses. In some patients, biological glue (BioGlue® surgical adhesive, Cryolife, Kennesaw, GA, USA) was used to better reapproximate the dissected layers.
Univariate Analysis
Univariate comparisons of preoperative, operative, and postoperative variables were performed between patients repaired with axillary artery cannulation (n = 107) and those repaired with femoral artery cannulation (n = 198). Normal distributions of continuous variables were assessed using Kolmognov-Smirnov tests. Continuous variables were tested using either Student’s t tests or Mann-Whitney tests, while categorical variables were assessed by chi-square or Fisher exact tests, depending on the data distribution. All tests were two-sided, and p < 0.05 was considered statistically significant.
Multivariate Analysis
A multivariable, stepwise, forward logistic regression analysis was conducted to determine independent predictors of operative mortality. The criterion for a variable entry into the logistic model was a univariate probability level of p < 0.1. The quality of the fit of the logistic model was tested with the Hosmer-Lemeshow goodness-of-fit test.
Survival Analysis
Kaplan-Meier univariate unadjusted survival estimates were calculated and compared using a log-rank test for patients repaired with axillary artery cannulation versus patients repaired with femoral artery cannulation. Cox regression hazard ratios were calculated to determine the predictors of long-term mortality. All analyses were conducted using SPSS statistical software Version 21 (IBM Corp, Armonk, NY, USA).
Results
Preoperative Characteristics
Preoperative characteristics are summarized in Table 1. The axillary cannulation group was more likely to undergo repair in the modern surgical era compared to the femoral cannulation group (p < 0.001) and had a lower number of patients with instability compared to the femoral cannulation group (p = 0.009). There was also a difference in the New York Heart Association class distribution (p < 0.001). There was no other significant difference between patients repaired with axillary or femoral artery cannulation.
Table 1.
Preoperative patient characteristics.
| Variablea | Axillary Cannulation | Femoral Cannulation | p |
|---|---|---|---|
| (n = 107) | (n = 198) | ||
| Age, years | 58 (23-87) | 61 (19-83) | 0.951 |
| Modern surgical era (2006–2010) | 81 (75.7%) | 95 (48.0%) | <0.001 |
| Diabetes | 7 (6.5%) | 17 (8.6%) | 0.658 |
| Hypertension | 86 (80.4%) | 146 (73.7%) | 0.209 |
| Ejection fraction | 60 (15-75) | 60 (25-80) | 0.883 |
| COPD | 8 (7.5%) | 17 (8.6%) | 0.717 |
| Creatinine | 1.1 (0.5-3.1) | 1.1 (.4-12.5) | 0.265 |
| Female gender | 34 (31.8%) | 61 (30.8%) | 0.897 |
| Arrhythmias | 7 (6.5%) | 23 (11.6%) | 0.226 |
| NYHA class | 0.000 | ||
| I | 10 (9.3%) | 15 (7.6%) | |
| II | 48 (44.9%) | 42 (21.2%) | |
| III | 12 (11.2%) | 55 (27.8%) | |
| IV | 37 (34.6%) | 86 (43.4%) | |
| History of stroke | 5 (4.7%) | 21 (10.6%) | 0.088 |
| History of cerebrovascular accident | 4 (3.7%) | 16 (8.1%) | 0.224 |
| Hemodynamic instability | 7 (6.5%) | 34 (17.2%) | 0.009 |
| EF < 40 | 4 (3.7%) | 9 (4.5%) | 1.000 |
Continuous data are shown as medians (ranges), and categorical data are shown as percentages.
COPD = chronic obstructive pulmonary disease; EF = ejection fraction; NYHA = New York Heart Association.
Operative Characteristics
Operative characteristics of patients who underwent repair for acute Type A aortic dissection with axillary cannulation or femoral cannulation are presented in Table 2. Patients in the axillary cannulation group more frequently had a prolonged CPB time, defined as >200 min, compared to the femoral cannulation group (p = 0.002). The type of cerebral perfusion used also differed between the groups, with antegrade cerebral perfusion used more commonly in axillary cannulation patients (p < 0.001). The hemiarch technique was used less frequently in patients with axillary cannulation compared to patients with femoral cannulation (p = 0.004).
Table 2.
Operative patient characteristics.
| Variablea | Axillary Cannulation | Femoral Cannulation | p |
|---|---|---|---|
| (n = 107) | (n = 198) | ||
| CPB time > 200 min | 60 (56.1%) | 74 (37.4%) | 0.002 |
| CPB time, min | 218 (5-430) | 182 (31-684) | 0.098 |
| Circulatory arrest time, min | 22.5 (0-71) | 25 (0-146) | 0.194 |
| Cerebral perfusion | <0.001 | ||
| None | 41 (38.3%) | 133 (67.2%) | |
| Antegrade | 55 (51.4%) | 23 (11.6%) | |
| Retrograde | 11 (10.3%) | 42 (21.2%) | |
| Temperature | 18 (10-27) | 18 (8-32) | 0.552 |
| Aortic valve procedure | 0.083 | ||
| Nothing | 37 (34.6%) | 53 (26.8%) | |
| Replacement | 9 (8.4%) | 14 (7.1%) | |
| Resuspension | 35 (32.7%) | 95 (48%) | |
| Bentall | 26 (24.3%) | 36 (18.2%) | |
| Hemiarch technique | 52 (48.6%) | 130 (65.7%) | 0.004 |
| Total arch replacement | 14 (13.1%) | 14 (7.1%) | 0.097 |
| Bioglue/Felt Strip | 0.298 | ||
| Bioglue | 52 (48.6%) | 84 (42.4%) | |
| Felt strip | 28 (26.2%) | 69 (34.8%) | |
| Both | 27 (25.2%) | 45 (22.7%) |
Continuous data are shown as medians (ranges), and categorical data are shown as percentages.
CPB = cardiopulmonary bypass.
Postoperative Characteristics
Postoperative characteristics are depicted in Table 3. Hemorrhage-related re-exploration was more frequent in the femoral cannulation group compared to the axillary cannulation group (p = 0.013).
Table 3.
Postoperative patient characteristics.
| Variablea | Axillary Cannulation | Femoral Cannulation | p |
|---|---|---|---|
| (n = 107) | (n = 198) | ||
| Prolonged ventilation | 51 (47.7%) | 87 (43.9%) | 0.549 |
| Acute renal failure | 22 (20.6%) | 39 (19.7%) | 0.881 |
| Hemodialysis | 8 (7.5%) | 18 (9.1%) | 0.675 |
| Hemorrhage-related re-exploration | 9 (8.4%) | 39 (19.7%) | 0.013 |
| Cardiac arrest | 7 (6.5%) | 22 (11.1%) | 0.225 |
| Stroke | 15 (14%) | 34 (17.2%) | 0.517 |
| Atrial fibrillation | 22 (20.6%) | 42 (21.2%) | 1.000 |
| Hospital length of stay (days) | 9 (0-99) | 11 (0-86) | 0.291 |
| Operative mortality | 17 (16%) | 37 (18.7%) | 0.638 |
Continuous data are shown as medians (ranges), and categorical data are shown as percentages.
Multivariate Analysis
In multivariate logistic regression analysis, hemodynamic instability (odds ratio [OR] = 23.8, 95% confidence interval [CI] = 0.067-0.316, p < 0.001) and prolonged CPB time (OR = 3.8, 95% CI = 0.261-1.002, p = 0.051) emerged as independent predictors of operative mortality. Cannulation site was not found to be an independent predictor of mortality.
Survival Analysis
Actuarial Kaplan-Meier survival estimates are presented in Figure 1. There was no difference in actuarial survival between those with axillary cannulation and femoral cannulation (p = 0.360). Table 4 depicts the Cox regression hazard ratios for the predictors of long-term mortality.
Figure 1.
Actuarial survival curves for patients who underwent axillary or femoral artery cannulation.
Table 4.
Predictors of long-term mortality.
| Variable | HR | 95% CI | p |
|---|---|---|---|
| Age | 21 | 1.024-1.062 | <0.001 |
| Stroke | 15 | 0.244-0.630 | <0.001 |
| CPB > 200 min | 11.8 | 0.315-0.728 | 0.001 |
| Hemodynamic instability | 9.3 | 0.266-0.750 | 0.002 |
| Renal failure | 8.4 | 0.326-0.806 | 0.004 |
CI = confidence interval; CPB = cardiopulmonary bypass; HR = hazard ratio.
Discussion
Our study compares the early and late postoperative outcomes for patients with axillary and femoral artery cannulation during repair of acute Type A aortic dissection. The axillary cannulation group more often had prolonged CPB time and less frequently used the hemiarch technique compared to the femoral cannulation group. No significant difference in stroke, operative mortality, or long-term survival was noted between the groups. Our results imply the arterial cannulation site for patients undergoing surgical repair of an acute Type A aortic dissection should be chosen on a case-by-case basis.
Principal Findings
Operative Mortality. The preferred arterial cannulation site for CPB during surgical repair of acute Type A aortic dissection has changed in the past few decades, and axillary cannulation has become more frequent [9, 18, 19]. However, which site offers the best operative and postoperative outcomes remains controversial [2, 6, 11-15]. Our study found no significant difference in operative mortality (p = 0.638) or stroke (p = 0.517) between the axillary artery and femoral artery cannulation groups. Previous studies also reported no significant difference in operative mortality between axillary and femoral cannulation [2, 15]. Specifically, Di Eusanio et al. [15] compared central cannulation and femoral cannulation in 473 patients undergoing aortic arch surgery and found similar rates of in-hospital death and permanent neurological damage between the groups. However, mixed results have generally been observed for operative mortality and neurological deficit based on cannulation strategy [10, 19, 20, 21-23]. Svensson et al. [18] reviewed 1,336 operations for complex cardiac problems that used CPB. Their results favored axillary cannulation due to a significant increased risk of hospital mortality in patients with femoral cannulation. On the other hand, Ayyash et al. [10] and Fusco et al. [20] found femoral cannulation to yield good clinical results with low adverse outcome and death rates. A possible explanation of the disparity in the conclusion of those studies may be the use of axillary cannulation in more recent years when improvements in the surgical technique and postoperative care may account for improved outcomes rather than cannulation site per se. In our study, axillary cannulation was more frequently used in the more recent years compared to the use of femoral arterial cannulation. Further, femoral cannulation patients had a higher risk profile such as higher incidence of hemodynamic instability that affects both the cannulation strategy (femoral cannulation allows for more expedient institution of CPB) and postoperative outcomes. In our study, hemodynamic instability on presentation and prolonged CPB time emerged as independent predictors of operative mortality, as previously reported [24].
Axillary cannulation patients more often had a prolonged CPB time compared to those who had femoral cannulation, possibly related to a higher frequency of complex cases in the axillary cannulation arm (e.g., aortic root replacements and total arch replacements). Fewer patients with axillary cannulation had hemiarch replacement compared to femoral artery patients, possibly because more patients in the axillary cannulation arm underwent creation of distal anastomosis with the cross-clamp on. Moreover, axillary cannulation patients had lower rates of hemodynamic instability and hemiarch replacement and a higher incidence of moderate hypothermia compared to those who had femoral cannulation, resulting in a higher rate of hemorrhage-related re-exploration.
Actuarial Survival
Our study is among the few studies comparing actuarial survival for axillary versus femoral artery cannulation in patients undergoing repair for acute Type A aortic dissection. While there was no significant difference in long-term survival, patients who underwent femoral cannulation tended to have lower survival within the early postoperative period. This could be explained by the impact of surgical era and hemodynamic instability on long-term outcomes. Earlier surgical era and hemodynamic instability have been shown to significantly decrease short-term survival following dissection repair, but less so over a longer period of time [9, 25]. In our study, more patients who underwent femoral artery cannulation were repaired in the earlier surgical era and had a higher incidence of hemodynamic instability. This likely contributed to the poorer survival witnessed in the femoral cannulation group over the early postoperative period. Kamiya et al. [11] examined long-term survival in patients with either central or femoral cannulation for repair of acute Type A aortic dissection. Survival for central cannulation was 80 ± 5%, 66 ± 6%, and 40 ± 8% at 1, 5, and 10 years, respectively, and for femoral cannulation it was 73% ± 4%, 64 ± 4%, and 46 ± 5% at 1, 5, and 10 years, respectively [11]. The same trend was seen in our data with axillary cannulation initially having better survival, but after 5 years, the femoral cannulation group had better survival. However, actuarial survival failed to reach significance in either study. Wong et al. [23] also investigated actuarial survival for patients with axillary artery cannulation. At 1 and 3 years, the survival rates were 73 ± 5% and 64 ± 6%, respectively, compared to 81.3% and 77.6% in our patients.
Cox regression analysis identified statistically significant predictors of long-term mortality of age at time of surgery, postoperative stroke, CPB >200 min, hemodynamic instability, and postoperative renal failure (Table 4 ).
Clinical Implications
We conducted a multi-institutional observational study to assess the impact of arterial cannulation site on early and long-term outcomes following repair of acute Type A aortic dissection. We examined an unselected cohort of patients from five academic institutions and compared patients that underwent surgery for acute Type A aortic dissection with either axillary artery or femoral artery cannulation. The differences in operative mortality and stroke rates between the cannulation sites were not statistically significant. Cannulation site selection needs to be individualized. In unstable patients who require expedient institution of CPB, femoral arterial cannulation provides quick access, while axillary cannulation with antegrade cerebral perfusion and moderate hypothermia is more beneficial in stable patients, allowing for a shorter CPB time by decreasing the cooling and rewarming periods. Obesity and at times small axillary artery size may limit its use in a selected set of patients. Involvement of the artery in the dissection, atherosclerosis, and other factors must also be considered when choosing a site [8, 12, 26]. Difficulty advancing the cannula, extreme arterial line pressure, insufficient CPB flow, vessel stenosis, small vessel diameter, and arterial wall damage may require a switch from axillary to femoral cannulation [26]. Iliofemoral disease and the risk of atheroembolism due to retrograde aortic perfusion contraindicate the use of the femoral artery for cannulation [8].
Study Limitations
Inherent limitations of a retrospective multi-institution investigation inevitably affected our study. The small sample size did not allow propensity score matching of the two groups to risk adjust for preoperative characteristic imbalances. Bias may have also been introduced into the analysis since different surgeons from five different institutions performed the procedures. Further study of reoperations on the remaining dissected aorta, the causes of late mortality, and false lumen fate were outside the scope of our analysis. In future studies, these variables should be included to evaluate the long-term outcomes of acute Type A aortic dissection repair.
Conclusions
The arterial cannulation site (i.e., the axillary or femoral artery) was not significantly related to stroke or mortality rates. The arterial cannulation site for CPB during acute Type A aortic dissection repair should be individualized based on the patient’s presentation, anatomic consideration, risk profiles, and surgeon preference.
Conflict of Interest
The authors have no conflict of interest relevant to this publication.
References
- 1.Ramanath VS, Oh JK, Sundt TM III, Eagle KA. Acute aortic syndromes and thoracic aortic aneurysm. Mayo Clin Proc. 2009;84:465-481. DOI: 10.1016/S0025-6196(11)60566-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Etz CD, von Apern K, da Rocha E, Silva J, Girrbach FF, Leontyev S, Luehr M, et al. . Impact of perfusion strategy on outcome after repair for acute type A aortic dissection. Ann Thorac Surg. 2014;97:78-85. DOI: 10.1016/j.athoracsur.2013.07.034 [DOI] [PubMed] [Google Scholar]
- 3.Shimazaki Y, Watanabe T, Takahashi T, Minowa T, Inui K, Uchida T, et al. . Minimized mortality and neurological complications in surgery for chronic arch aneurysm: axillary artery cannulation, selective cerebral perfusion, and replacement of the ascending and total arch aorta. J Card Surg. 2004;19:338-342. DOI: 10.1111/j.0886-0440.2004.4092_11.x [DOI] [PubMed] [Google Scholar]
- 4.Rylski B, Urbanski PP, Siepe M, Beyersdorf F, Bachet J, Gleason TG, et al. . Operative techniques in patients with type A dissection complicated by cerebral malperfusion. Eur J Cardiothorac Surg. 2014;46:156-166. DOI: 10.1093/ejcts/ezu251 [DOI] [PubMed] [Google Scholar]
- 5.Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. . The International Registry of Acute Aortic Dissection (IRAD) – New insights into an old disease. JAMA. 2000;283:897-903. DOI: 10.1001/jama.283.7.897 [DOI] [PubMed] [Google Scholar]
- 6.Calvaruso D, Voisine P, Mohammadi S, Dumont E, Dagenais F. Axillary artery cannulation. Multimed Man Cardiothorac Surg. 2012;2012:mms004 DOI: 10.1093/mmcts/mms004 [DOI] [PubMed] [Google Scholar]
- 7.Neri E, Massetti M, Capannini G, Carone E, Tucci E, Diciolla F, et al. . Axillary artery cannulation in type A aortic dissection operations. J Thorac Cardiovasc Surg. 1999;118:324-329. DOI: 10.1016/S0022-5223(99)70223-0 [DOI] [PubMed] [Google Scholar]
- 8.Kokotsakis J, Lazopoulos G, Milonakis M, Athanasiadis G, Skouteli E, Bastounis E. Right axillary artery cannulation for surgical management of the hostile ascending aorta. Tex Heart Inst J. 2005;32:189-193. PMID: [PMC free article] [PubMed] [Google Scholar]
- 9.Conway BD, Stamou SC, Kouchoukos NT, Lobdell KW, Khabbaz K, Patzelt LH, et al. . Effects of hemodynamic instability on early outcomes and late survival following repair of acute type A aortic dissection. AORTA (Stamford). 2014;2:22-27. DOI: 10.12945/j.aorta.2014.13-055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayyash B, Tranquilli M, Elefteriades JA. Femoral artery cannulation for thoracic aortic surgery: safe under transesophageal echocardiographic control. J Thorac Cardiovasc Surg. 2011;142:1478-1481. DOI: 10.1016/j.jtcvs.2011.04.005 [DOI] [PubMed] [Google Scholar]
- 11.Kamiya H, Kallenbach K, Haimer D, Ozsös M, Ilg K, Lichtenberg A, et al. . Comparison of ascending aorta versus femoral artery cannulation for acute aortic dissection type A. Circulation. 2009;120:S282-S286. DOI: 10.1161/CIRCULATIONAHA.108.844480 [DOI] [PubMed] [Google Scholar]
- 12.Schachner T, Nagiller J, Zimmer A, Laufer G, Bonatti J. Technical problems and complications of axillary artery cannulation. Eur J Cardiothorac Surg. 2005;27:634-637. DOI: 10.1016/j.ejcts.2004.12.042 [DOI] [PubMed] [Google Scholar]
- 13.Tiwari KK, Murzi M, Bevilacqua S, Glauber M. Which cannulation (ascending aortic cannulation or peripheral arterial cannulation) is better for acute type A aortic dissection surgery? Interact Cardiovasc Thorac Surg. 2010;10:797-802. DOI: 10.1510/icvts.2009.230409 [DOI] [PubMed] [Google Scholar]
- 14.Lee HK, Kim GJ, Cho JY, Lee JT, Park I, Lee YO. Comparison of the outcomes between axillary and femoral artery cannulation for acute type a aortic dissection. Korean J Thorac Cardiovasc Surg. 2012;45:85-90. DOI: 10.5090/kjtcs.2012.45.2.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Eusanio M, Pantaleo A, Petridis FD, Folesani G, Cefarelli M, Berretta P, et al. . Impact of different cannulation strategies on in-hospital outcomes of aortic arch surgery: a propensity-score analysis. Ann Thorac Surg. 2013;96:1656-1663. DOI: 10.1016/j.athoracsur.2013.06.081 [DOI] [PubMed] [Google Scholar]
- 16.Gulbins H, Pritisanac A, Ennker J. Axillary versus femoral cannulation for aortic surgery: enough evidence for a general recommendation? Ann Thorac Surg. 2007;83:1219-1224. DOI: 10.1016/j.athoracsur.2006.10.068 [DOI] [PubMed] [Google Scholar]
- 17.Benedetto U, Raja SG, Amrani M, Pepper JR, Zeinah M, Tonelli E, et al. . The impact of arterial cannulation strategy on operative outcomes in aortic surgery: evidence from a comprehensive meta-analysis of comparative studies on 4476 patients. J Thorac Cardiovasc Surg. 2014;148:2936-2943. DOI: 10.1016/j.jtcvs.2014.05.082 [DOI] [PubMed] [Google Scholar]
- 18.Svensson LG, Blackstone EH, Rajeswaran J, Sabik JF III, Lytle BW, Gonzalez-Stawinski G, et al. . Does the arterial cannulation site for circulatory arrest influence stroke risk? Ann Thorac Surg. 2004;78:1274-1284. DOI: 10.1016/j.athoracsur.2004.04.063 [DOI] [PubMed] [Google Scholar]
- 19.Shimokawa T, Takanashi S, Ozawa N, Itoh T. Management of intraoperative malperfusion syndrome using femoral artery cannulation for repair of acute type A aortic dissection. Ann Thorac Surg. 2008;85:1619-1624. DOI: 10.1016/j.athoracsur.2008.01.048 [DOI] [PubMed] [Google Scholar]
- 20.Fusco DS, Shaw RK, Tranquilli M, Kopf GS, Elefteriades JA. Femoral cannulation is safe for type A dissection repair. Ann Thorac Surg. 2004;78:1285-1289. DOI: 10.1016/j.athoracsur.2004.04.072 [DOI] [PubMed] [Google Scholar]
- 21.Moizumi Y, Motoyoshi N, Sakuma K, Yoshida S. Axillary artery cannulation improves operative results for acute type A aortic dissection. Ann Thorac Surg. 2005;80:77-83. DOI: 10.1016/j.athoracsur.2005.01.058 [DOI] [PubMed] [Google Scholar]
- 22.Yavuz S, Göncü MT, Türk T. Axillary artery cannulation for arterial inflow in patients with acute dissection of the ascending aorta. Eur J Cardiothorac Surg. 2002;22:313-315. DOI: 10.1016/S1010-7940(02)00249-X [DOI] [PubMed] [Google Scholar]
- 23.Wong DR, Coselli JS, Palmero L, Bozinovski J, Carter SA, Murariu D, et al. . Axillary artery cannulation in surgery for acute or subacute ascending aortic dissections. Ann Thorac Surg. 2010;90:731-737. DOI: 10.1016/j.athoracsur.2010.04.059 [DOI] [PubMed] [Google Scholar]
- 24.Stamou SC, Hagberg RC, Khabbaz KR, Stiegel MR, Reames MK, Skipper E, et al. . Is advanced age a contraindication for emergent repair of acute type A aortic dissection? Interact Cardiovasc Thorac Surg. 2010;10:539-544. DOI: 10.1510/icvts.2009.222984 [DOI] [PubMed] [Google Scholar]
- 25.Strauch JT, Spielvogel D, Lauten A, Lansman SL, McMurty K, Bodian CA, et al. . Axillary artery cannulation: routine use in ascending aorta and aortic arch replacement. Ann Thorac Surg. 2004;78:103-108. DOI: 10.1016/j.athoracsur.2004.01.035 [DOI] [PubMed] [Google Scholar]
- 26.Schachner T, Vertacnik K, Laufer G, Bonatti J. Axillary artery cannulation in surgery of the ascending aorta and the aortic arch. Eur J Cardiothorac Surg. 2002;22:445-447. DOI: 10.1016/S1010-7940(02)00365-2 [DOI] [PubMed] [Google Scholar]