SUMMARY
The human Ureaplasma species are the most frequently isolated microorganisms from the amniotic fluid and placentae of women who deliver preterm and are also associated with spontaneous abortions or miscarriages, neonatal respiratory diseases, and chorioamnionitis. Despite the fact that these microorganisms have been habitually found within placentae of pregnancies with chorioamnionitis, the role of Ureaplasma species as a causative agent has not been satisfactorily explained. There is also controversy surrounding their role in disease, particularly as not all women infected with Ureaplasma spp. develop chorioamnionitis. In this review, we provide evidence that Ureaplasma spp. are associated with diseases of pregnancy and discuss recent findings which demonstrate that Ureaplasma spp. are associated with chorioamnionitis, regardless of gestational age at the time of delivery. Here, we also discuss the proposed major virulence factors of Ureaplasma spp., with a focus on the multiple-banded antigen (MBA), which may facilitate modulation/alteration of the host immune response and potentially explain why only subpopulations of infected women experience adverse pregnancy outcomes. The information presented within this review confirms that Ureaplasma spp. are not simply “innocent bystanders” in disease and highlights that these microorganisms are an often underestimated pathogen of pregnancy.
KEYWORDS: amniotic fluid, chorioamnionitis, multiple-banded antigen, neonate/fetus, pregnancy, Ureaplasma, virulence factors
INTRODUCTION
Chorioamnionitis refers to inflammation of the fetal membranes, which comprise the chorion and amnion. Although the chorioamnion is anatomically part of the placenta, it is derived from the zygote and is considered to be of fetal origin (see “Development, Structure, and Function of the Chorioamnion” below). The chorioamnion is also in contact with the decidua, a tissue of maternal origin, and together these form the maternal/fetal interface. Chorioamnionitis frequently occurs in parallel with microbial infection of the chorioamnion and amniotic fluid (1–3); however, it may also occur in the absence of demonstrable microorganisms (i.e., “sterile inflammation” [2, 4], which will not be discussed in this review). The clinical signs of chorioamnionitis include fever, uterine fundal tenderness, maternal tachycardia (>100 beats/minute), fetal tachycardia (>160 beats/minute), and purulent or foul-smelling amniotic fluid (5). However, it is becoming increasingly apparent that a large proportion of chorioamnionitis cases are subclinical and are not diagnosed until retrospective analysis of the placenta (6) (see “Diagnosis of Chorioamnionitis” below). Upon histological examination, acute chorioamnionitis is defined as diffuse influx of neutrophils into the chorioamnion/decidua, and the severity of the maternal and fetal immune response can be classified according to published standards (7). Chronic chorioamnionitis is less well defined but has been characterized by an infiltration of maternally derived mononuclear cells, usually macrophages and T lymphocytes, into the chorioamnion or chorionic plate (the fetal surface of the placenta that directly connects to the uterine wall, where the chorionic villi are formed) (7, 8).
Since amniotic fluid, but not the placenta, is accessible prior to delivery in women at risk for preterm labor, most clinical studies have correlated intra-amniotic infection or inflammation rather than chorioamnionitis with preterm labor/delivery. However, intra-amniotic infection, defined as microorganisms detected in the amniotic fluid (9), may not always be concordant with retrospective diagnosis of histological chorioamnionitis. Recently, a National Institutes of Health workshop recommended that the term “chorioamnionitis” be replaced with “intrauterine infection or inflammation or both” (abbreviated as “Triple I” and characterized as being either proven or suspected) or isolated maternal fever (10). For the purposes of this review, we have used the terms chorioamnionitis and intra-amniotic infection according to their traditional definitions, as described above.
Development, Structure, and Function of the Chorioamnion
The amnion develops from the ectoderm of the embryo 8 days after conception and surrounds the developing embryo to form an amniotic sac, which contains amniotic fluid. As the amniotic sac expands due to fetal growth and the production of amniotic fluid, the amnion makes contact with the chorion, which lines the decidua of the uterine wall, to form the chorioamnion at 10 to 12 weeks of gestation (11). The avascular chorioamniotic membranes persist until term in healthy pregnancies and perform critical barrier and container functions (12). The amnion comprises five layers: (i) a cuboidal epithelium, which is in contact with the amniotic fluid; (ii) an acellular basement membrane; (iii) a compact layer; (iv) a mesenchymal cell layer; and (v) a spongy layer, which is in contact with the chorion (13). The amniotic epithelial cells and mesenchymal cells possess stem cell and immunomodulatory properties and have shown promising results for use in regenerative medicine (14). The chorion comprises four layers: (i) a cellular, fibroblast layer; (ii) a reticular layer; (iii) a pseudobasement membrane; and (iv) a trophoblast layer (13).
Diagnosis of Chorioamnionitis
The diagnosis of chorioamnionitis is currently based on clinical signs coupled with histological and microbiological analysis of the placenta after delivery of the newborn. Histologic grading of the placenta is considered the gold standard for the diagnosis of chorioamnionitis; however, this retrospective diagnosis is not useful in informing patient management throughout pregnancy, especially in the absence of clinical signs. Several studies have investigated the diagnostic value of amniotic fluid and maternal serum biomarkers for the detection of chorioamnionitis in pregnant women undergoing amniocentesis. Elevated inflammatory markers such as interleukin 6 (IL-6), IL-8, matrix metalloproteinase 8 (MMP-8), MMP-9, and monocyte chemotactic proteins within amniotic fluid are positive predictors of intra-amniotic inflammation and/or clinical chorioamnionitis (15–21); however, these markers may have poor positive predictive values for the detection of subclinical, histologic chorioamnionitis and may be variably expressed within the amniotic fluid and fetal membranes during chorioamnionitis (22–24). Recently, Liu et al. (25) reported that surface-enhanced laser desorption ionization–time of flight mass spectrometry (SELDI-TOF-MS) for the detection of human neutrophil defensin 1 (HNP-1) and HNP-2 and calgranulins A and C within amniotic fluid was highly accurate for the diagnosis of subclinical chorioamnionitis, but further studies with larger patient cohorts are required to validate these findings. Noninflammatory markers such as amniotic fluid lactate dehydrogenase and glucose were also recently investigated for the detection of histologic chorioamnionitis (26), but the diagnostic accuracy of these assays was low, suggesting that additional amniotic fluid biomarkers should be investigated for the diagnosis of chorioamnionitis.
CLINICAL PERSPECTIVES ON CHORIOAMNIONITIS AND ITS SIGNIFICANCE TO THE HEALTH OF THE PREGNANCY AND NEONATE
Clinical chorioamnionitis and histological chorioamnionitis affect 1 to 4% and 23.6% of term births (37 to 42 weeks of gestation), respectively (5, 27, 28). However, it has been well established that the frequency (29–31) and severity (31, 32) of chorioamnionitis are inversely related to gestational age at the time of delivery. In a study of 7,505 placentae from singleton pregnancies, Russell (29) reported that the frequency of chorioamnionitis in patients who delivered between 21 and 24 weeks of gestation was 94.4% (17/18 patients). More recently, Stoll et al. (30) demonstrated that histological chorioamnionitis was present in 70% (295/421) of pregnancies that delivered at 22 weeks of gestation. The frequency of histological chorioamnionitis was significantly higher in women who delivered after the spontaneous onset of labor than in those who had induction of labor at term or delivered via Caesarean section in the absence of labor (33, 34). Furthermore, the frequency of histological chorioamnionitis increases in patients with prolonged duration of labor (35) and premature rupture of membranes (36). Additional risk factors for chorioamnionitis include multiple digital examinations, nulliparity, bacterial vaginosis, alcohol and tobacco use, group B Streptococcus colonization, meconium-stained amniotic fluid, and epidural anesthesia (36–39).
Chorioamnionitis: a Major Predictor of Preterm Birth
Preterm birth, defined as delivery at <37 weeks of gestation, is the leading cause of neonatal death worldwide (40). In addition, complications arising from preterm birth are a leading cause of death in children under the age of 5, second only to pneumonia (41). Microbiological studies have demonstrated that intrauterine infection may be responsible for 25 to 40% of preterm births (42); however, this is likely to be underreported due to difficulties in detecting fastidious microorganisms using conventional culture methods. Histological chorioamnionitis complicates 40 to 70% of all preterm births (5), suggesting that chorioamnionitis may be an important, and potentially preventable, antecedent of preterm birth.
Parturition in Normal Pregnancy versus Chorioamnionitis
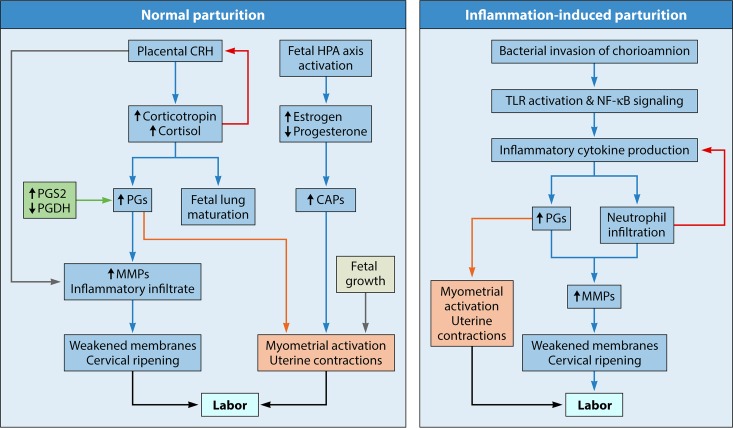
Figure 1 compares the key events that occur during normal parturition and inflammation-induced preterm delivery. The normal initiation of parturition in humans is a complex process that involves fetal hypothalamic-pituitary-adrenal (HPA) axis activation and increased placental synthesis of corticotropin-releasing hormone (CRH) (Fig. 1). Maternal CRH plasma levels increase throughout the duration of pregnancy and peak at term (43). Increased CRH levels drive the production of corticotropin and cortisol in the mother and fetus, which promotes fetal lung maturation and prostaglandin (PG) synthesis (e.g., PGE2 and PGF2α) within the amnion (44). PG production is enhanced by the concomitant downregulation of prostaglandin dehydrogenase (PGDH) within the chorion (45) and the production of prostaglandin-endoperoxide synthase 2 (PGS2, formerly cyclo-oxygenase 2) (46). Both CRH and PGE2 stimulate the release of MMPs (47, 48) (e.g., MMP-2 and MMP-9), which weaken the chorioamnion and facilitate membrane rupture and cervical ripening. In parallel, activation of the fetal HPA axis and uterine stretching caused by fetal growth lead to the upregulation of contraction-associated proteins and myometrial activation (44). Progesterone withdrawal coupled with increased estrogen production is also a key feature of parturition and further promotes uterine contractility (49–51).
FIG 1.
Comparison of key events involved in normal parturition and inflammation-induced parturition. Normal parturition is initiated by the increased placental synthesis of CRH at term, which causes the production of cortisol. Cortisol induces the production of prostaglandin E2 and prostaglandin F2α and works in a positive-feedback loop to further stimulate placental CRH production. Prostaglandins induce the production of matrix metalloproteases, which facilitate membrane rupture and cervical remodeling. In concert, activation of the fetal HPA axis leads to a functional progesterone withdrawal and production of contraction-associated proteins, which cause myometrial activation and uterine contractility. During chorioamnionitis, inflammatory cytokines and chemokines produced in response to microbial invasion of the chorioamnion and/or amniotic fluid stimulate prostaglandin production and neutrophil infiltration, leading to the synthesis of matrix metalloproteases and subsequent membrane weakening. Recognition of pathogen-associated molecular patterns by pattern recognition receptors (such as TLRs) is critical for the initiation of inflammation-induced parturition. CAPs, contraction-associated proteins; CRH, corticotropin-releasing hormone; HPA, hypothalamic-pituitary-adrenal; MMPs, matrix metalloproteases; NF-κB, nuclear factor kappa B; PGDH, prostaglandin dehydrogenase; PGs, prostaglandins; PGS2, prostaglandin-endoperoxide synthase 2; TLR, Toll-like receptor. The direction of the arrows within boxes represents either an increase or a decrease in expression.
In patients with chorioamnionitis, parturition may be accelerated by a maternal and/or fetal inflammatory response, which is thought to be mediated by Toll-like receptor (TLR) signaling (Fig. 1). A recent prospective study of human pregnancies demonstrated that the expression of TLR-1 and TLR-2 was significantly increased in chorion obtained from preterm deliveries with histological chorioamnionitis compared to chorion from preterm deliveries without histological chorioamnionitis (52). Similar results were reported in separate studies by Moço et al. (53) and Kim et al. (54), suggesting that the upregulation of TLRs plays an important role in the pathogenesis of chorioamnionitis.
Bacterial endotoxins, such as lipopolysaccharide (LPS) (55), and live microorganisms (56) have been shown to upregulate placental/chorioamnion TLRs, which are expressed by amnion epithelial cells, decidual cells, intermediate trophoblasts in the chorion, macrophages, and neutrophils (54). In vitro studies have demonstrated that human primary amnion epithelial cells express functional TLR-2, TLR-4, TLR-5, and TLR-6 and that stimulation with TLR-5 and TLR-2/6 agonists leads to activation of nuclear factor kappa B signaling and the production of proinflammatory cytokines, MMP-9, and PGS2 (57). These findings are consistent with human studies and animal models of chorioamnionitis/intrauterine infection, which demonstrate an increase in IL-1β and IL-6 (58, 59), IL-8 (52), tumor necrosis factor alpha (TNF-α) (60), monocyte chemotactic proteins (61), and granulocyte colony-stimulating factor (G-CSF) (62) in preterm fetal membranes, amniotic fluid, and/or cord blood. These inflammatory cytokines and chemokines stimulate PG production (63, 64) and neutrophil infiltration and the release of MMPs (65), thus leading to cervical ripening and weakening/rupture of the fetal membranes. Indeed, the levels of MMPs (66) and PGs (56, 67) are significantly increased within the amniotic fluid and fetal membranes during chorioamnionitis.
Neonatal Sequelae of Chorioamnionitis
During chorioamnionitis, the fetus may be directly exposed to microorganisms and inflammatory mediators within infected amniotic fluid. The fetus inspires, swallows, and is bathed in amniotic fluid; therefore, the fetal lungs (68, 69), gastrointestinal tract (70, 71), and skin (72) are primary sites of inflammation-mediated injury. Exposure to inflammatory mediators may also occur via the placental-fetal circulation, resulting in immunomodulation within the fetal blood (73–75), lymphoid tissues (76–78), and distant organs such as the brain (79, 80). The systemic response of the fetus to chorioamnionitis, termed the fetal inflammatory response syndrome (FIRS), is a severe inflammatory condition that is characterized by elevated inflammatory cytokines within fetal plasma, particularly IL-6 (81, 82), and increased fetal plasma white blood cell counts (83). FIRS is associated with multiorgan injury and with severe neonatal morbidity and mortality (82). The fetal immune response to chorioamnionitis has been reviewed in detail elsewhere (84, 85).
In human studies, chorioamnionitis has been associated with neonatal death (27, 86), early-onset neonatal sepsis (86–88), intrauterine growth restriction (89), poor neonatal growth (90), neurologic impairment/injury (91, 92), intraventricular hemorrhage (86), bronchopulmonary dysplasia (93–95), patent ductus arteriosus (86, 89, 93, 96), retinopathy of prematurity (89, 97, 98), cardiovascular abnormalities (99, 100), necrotizing enterocolitis (101, 102), and dermatitis (103). However, low gestational age is often a significant contributing factor (104–106), and therefore, it is difficult to attribute these sequelae solely to chorioamnionitis. Nonetheless, when controlling for gestational age in a multivariable analysis, a recent study of 3,082 extremely preterm infants (<27 weeks of gestation) demonstrated that fetal exposure to histological chorioamnionitis and clinical chorioamnionitis was associated with an increased risk of cognitive impairment at 18 to 22 months of corrected age compared to infants exposed to no chorioamnionitis or histological chorioamnionitis alone (107). When adjusting for gestational age, other studies have confirmed that chorioamnionitis is an independent risk factor for early-onset neonatal sepsis (108, 109), bronchopulmonary dysplasia (95), adverse neurodevelopmental outcome at 3 years (110), and necrotizing enterocolitis (108). Interestingly, the severity of chorioamnionitis has been shown to correlate with an increased frequency of chronic lung disease and necrotizing enterocolitis (111) but has an inverse relationship with the development of respiratory distress syndrome (112).
HOST DEFENSES AND PATHWAYS OF MICROBIAL INVASION OF THE CHORIOAMNION AND AMNIOTIC FLUID
Traditionally, the normal intrauterine environment is considered to be a sterile site with the chorioamnion representing the major physical and immunological barrier to the developing fetus. The chorioamnion expresses TLRs, which detect pathogen-associated molecular patterns and signal to coordinate cellular immune responses. The chorioamnion also secretes numerous natural antimicrobial peptides and defensins to protect against microbial invasion (113). In vitro, human chorion and amnion from healthy pregnancies that delivered at term inhibited the growth of a wide range of pathogenic bacteria, including group B Streptococcus, group A Streptococcus, Staphylococcus aureus, and Staphylococcus saprophyticus (114). Parthasarathy et al. also reported that human fetal membranes possess strong antimicrobial effects against Escherichia coli, Shigella spp., and the fungal pathogens Aspergillus niger and Aspergillus nidulans (115). Nonetheless, a wide range of microbes are capable of invading the fetal membranes and amniotic cavity and causing chorioamnionitis. Specific routes by which microorganisms are thought to access the upper genital tract during pregnancy include (i) retrograde spread from the peritoneal cavity (via the Fallopian tubes), (ii) hematogenous dissemination via the placenta and maternal blood supply, (iii) iatrogenic contamination at the time of invasive medical procedures (such as chorionic villus sampling or amniocentesis), and (iv) ascending invasive infections from the lower genital tract (42). While other studies have suggested that bacteria (specifically, Ureaplasma spp.) may also gain access to the upper genital tract attached to spermatozoa (116, 117), the most widely accepted route is that microorganisms originating from the lower genital tract ascend through the cervix into the choriodecidual space and cross the chorioamnion membrane, thereby reaching the amniotic fluid and fetus (118).
Recent deep-sequencing studies have demonstrated that the placental parenchyma harbors a unique microbiome comprising nonpathogenic bacteria from the Firmicutes, Tenericutes, Proteobacteria, and Fusobacteria phyla, with distinct similarities to the adult oral microbiota (119). Furthermore, whole-genome shotgun sequencing of placental membranes (fetal chorion and/or villous placental membranes) from term deliveries without chorioamnionitis demonstrated the presence of a diverse range of bacteria, including Enterobacter spp., E. coli, Acinetobacter lwoffii, Acinetobacter johnsonii, and Lactobacillus crispatus (120). These findings redefine our understanding of the placental microenvironment and challenge the view that the fetus exists normally within a sterile compartment. It is therefore possible that the commensal microorganisms of the placental parenchyma and fetal membranes represent a previously unrecognized source of bacteria, which, under certain conditions, may initiate an inflammatory response leading to chorioamnionitis. This may also be important for the establishment of the fetal/neonate microbiota (119) and normal immune development of the fetus (121).
CAUSATIVE AGENTS OF CHORIOAMNIONITIS
A range of microorganisms, including bacteria, viruses, and (less frequently) yeast and fungi, have been implicated in chorioamnionitis. The bacterial pathogens that are most frequently isolated in cases of chorioamnionitis include the human Ureaplasma species (Ureaplasma parvum and Ureaplasma urealyticum), Fusobacterium spp., Streptococcus spp., and, less frequently, Gardnerella spp., Mycoplasma spp., and Bacteroides spp. (1, 62, 120, 122–124). Other studies have identified that the sexually transmitted pathogens Chlamydia trachomatis and Neisseria gonorrhoeae, along with the uropathogen E. coli and yeast Candida spp., are also infrequently associated with chorioamnionitis (122, 125–128). Viral etiologies of chorioamnionitis include adenovirus, cytomegalovirus, enterovirus, and, less frequently, respiratory syncytial virus and Epstein-Barr virus (129–132). Of the microorganisms associated with chorioamnionitis, the human Ureaplasma spp. are consistently identified as the most common microorganisms within the amniotic fluid and placentae of women with chorioamnionitis (1, 62, 123, 133, 134), funisitis (120, 135, 136), and preterm birth (1, 137).
THE HUMAN UREAPLASMA SPP.
The human Ureaplasma spp. were first discovered in 1954 in agar cultures of urethral exudates from male patients with nongonococcal urethritis (138). Due to their small colony size (5 to 20 μm) and their resemblance to the human Mycoplasma spp., Ureaplasma spp. were initially identified as tiny-form pleuropneuomonia-like organisms and referred to as T-mycoplasmas (138). However, Ureaplasma can be distinguished from Mycoplasma spp. (139) by the presence of a urease enzyme, which hydrolyzes urea to produce 95% of its energy requirements. The hydrolysis of urea produces ammonia, which leads to an increase in proton electrochemical potential and de novo ATP synthesis (140). The production of ammonia is a distinguishing feature for the identification of Ureaplasma spp. in culture, and these tiny bacteria are detected not by turbidity within broth but by an alkaline shift and pH indicator color change in both broth and agar culture media (141, 142). Due to this distinctive urease activity, the Ureaplasma spp. were reclassified into their own genus within the Mycoplasmataceae family in 1974 (139). As members of the class Mollicutes, Ureaplasma spp. do not possess a cell wall and are surrounded only by a plasma membrane. Due to this lack of structural integrity, the Ureaplasma spp. are pleomorphic, and individual organisms can range in size from 100 nm to 1 μm (143). As such, the Ureaplasma spp. are considered to be among the smallest self-replicating microorganisms.
Taxonomic Classification
The human Ureaplasma spp. are divided into two species, which contain at least 14 serovars: U. parvum (serovars 1, 3, 6, and 14) and U. urealyticum (serovars 2, 4, 5, and 7 to 13) (144). U. parvum possesses a smaller genome (0.75 to 0.78 Mbp) than U. urealyticum (0.84 to 0.95 Mbp) (145), and these two species can also be distinguished based on restriction fragment length polymorphisms, DNA-DNA hybridization, multilocus sequence typing, and sequences of 16S rRNA, multiple-banded antigen (mba), and urease genes (146–151). While this taxonomic classification was formally accepted in 2002, it has not been universally adopted within the literature, and often the 14 serovars are still erroneously referred to as U. urealyticum.
Several methods for serotyping Ureaplasma spp. have been described, including growth inhibition tests (152, 153), immunoperoxidase tests (154), enzyme-linked immunosorbent assays (155, 156), and colony indirect epi-immunofluorescence (157), which utilize rabbit antisera. These tests performed poorly due to a lack of standardized reagents and the presence of multiple cross-reactions between serovars. These approaches also poorly discriminate clinical samples containing more than one Ureaplasma serovar. Therefore, serotyping of Ureaplasma for diagnostic and epidemiological purposes has historically been technically challenging. Molecular biology-based typing methods based on sequencing of the upstream region of the mba gene (151), conventional PCR of mba (158–160), and random amplified polymorphic DNA PCR (158) have also been described. However, these methods do not fully discriminate all 14 Ureaplasma serovars. In addition, the mba gene was recently shown to be part of a phase-variable gene superfamily (145), suggesting that its use as a diagnostic target may be limited.
Following the release of full genome sequences of Ureaplasma American Type Culture Collection (ATCC) strains, Xiao et al. designed 14 separate monoplex real-time PCR assays, which successfully typed all 14 ATCC type strains without cross-reactivity between serovars (161). However, when these real-time PCRs were used to type clinical human Ureaplasma isolates, 6% of isolates failed to amplify and could not be typed according to any of the known 14 serovars (162). Whole-genome shotgun sequencing of a selection of these isolates revealed that the gene targets for real-time PCR were completely absent or had been significantly modified, such that one of the primers was unable to bind. Even more intriguing was that following filtering and subculture of single Ureaplasma colonies isolated from samples thought to contain mixtures of multiple serovars, several isolates continued to express loci from more than one serovar. DNA sequencing revealed that these isolates were in fact hybrids or genetic mosaics that carried multiple serovar markers. Screening of 271 clinical samples initially believed to contain multiple serovar mixtures demonstrated that 75 (28%) were hybrids, which carried markers of up to 4 different serovars (162). These data, in combination with recent comparative genome sequencing studies, demonstrate that there is extensive evidence of horizontal gene transfer (HGT) in Ureaplasma spp., suggesting that typing these microorganisms into defined serovar groups may be of limited value for diagnostic purposes (162) and that Ureaplasma organisms exist as quasispecies (145). On the other hand, it is possible that there are more-stable gene targets that have yet to be identified, which could be utilized for the discrimination of Ureaplasma serovars or pathogenic versus commensal subtypes. Large-scale comparative genome sequencing studies are required to clarify this issue.
Ureaplasma spp. Are Commensals of the Female Lower Genital Tract
Ureaplasma can be isolated from the mucosal surfaces of the vagina or cervix from 40 to 80% of sexually active females (163). U. parvum is isolated more frequently from the lower genital tract of females than U. urealyticum (158, 159, 164–166), and serovar 3 is the most common serovar isolated from females in the United States and Australia (116, 158, 163). Ureaplasma colonization of the female lower genital tract has been associated with numerous factors, including ethnicity (particularly African-American, Central/West African, and Indigenous Australian women) (123, 167, 168), age (most prevalent in the 14- to 25-year age group; carriage declines with increasing age) (165, 167), the number of recent sexual partners (123, 168), the use of nonbarrier contraceptives (123), level of education (167), age of first sexual intercourse (123), and intrauterine devices (167, 169). Ureaplasma spp. are considered to be commensal organisms within the female lower genital tract due to (i) their high prevalence and (ii) studies demonstrating no differences in the rates of endocervical Ureaplasma colonization between women of reproductive age with and those without symptoms of genital infection (165, 166). However, others have reported that Ureaplasma spp. can cause lower urogenital tract infections, such as symptomatic vaginitis (170, 171), cervicitis (172), bacterial vaginosis (173), pelvic infections (174, 175), and urinary tract infections (176–178).
Lower Genital Tract Ureaplasma Colonization Association with Chorioamnionitis and Adverse Pregnancy Outcomes
It has been proposed that the presence of Ureaplasma spp. in the female lower genital tract may be a risk factor for chorioamnionitis and adverse pregnancy outcomes, such as preterm birth (179–184). A prospective study of 2,471 women attending an antenatal clinic demonstrated that Ureaplasma spp. were isolated from vaginal swabs from 52/97 women (53.6%) who delivered preterm and that vaginal Ureaplasma colonization was an independent risk factor for preterm birth (odds ratio, 1.64; confidence interval, 1.08 to 2.48; P = 0.02). Despite this statistical association, it should be noted that, in the same study, Ureaplasma was also isolated from the lower genital tract of 783/1,891 women (41.1%) who delivered at term. Similarly, Kataoka et al. (179) demonstrated that U. parvum was detected in 16/21 women (76.2%) who delivered preterm and also in 440/856 women (51.4%) who delivered at term (P = 0.024). Other authors have reported equally high carriage rates in women who deliver at term, and the majority of studies conclude that lower genital tract Ureaplasma colonization is not a significant predictor of preterm birth or chorioamnionitis (185–190).
Ureaplasma Can Cause Ascending Asymptomatic Infections of the Upper Genital Tract
Although Ureaplasma spp. are (in most instances) considered to be commensals within the lower genital tract, these microorganisms are capable of causing ascending asymptomatic infections of the upper genital tract. A recent study of fertile and infertile women undergoing diagnostic laparoscopy (who had no symptoms of genital tract infection) demonstrated that lower genital tract Ureaplasma colonization can lead to asymptomatic infection of the pouch of Douglas (191). Furthermore, Ureaplasma spp. have been isolated from the endometrium and Fallopian tubes of nonpregnant women in the absence of clinical symptoms or abnormal pathology (192, 193). While it was historically thought that the Ureaplasma spp. were of low virulence and that their presence in the upper genital tract might be of little consequence, there is now increasing evidence that these microorganisms are not simply innocent bystanders. The presence of Ureaplasma spp. in the upper genital tract of nonpregnant women suggests that these microorganisms may infect the embryo at the time of implantation (163). Moreover, they are capable of inducing chorioamnionitis, which can adversely affect the health of the pregnancy and neonate. Here, we discuss the role of the human Ureaplasma spp. as causative agents of chorioamnionitis.
UREAPLASMA SPP. AS ETIOLOGICAL AGENTS OF CHORIOAMNIONITIS
The first study to identify an association between Ureaplasma spp. and chorioamnionitis was published in 1975 and identified a link between carriage of Ureaplasma spp. in the lower genital tract and an increased incidence of chorioamnionitis (194). While the majority of studies since have demonstrated that lower genital tract colonization with Ureaplasma is not predictive of adverse outcomes during pregnancy, the role of Ureaplasma spp. in chorioamnionitis has remained controversial. Attempts to correlate infection with Ureaplasma spp. with the presence of chorioamnionitis have been made by a variety of studies and utilizing amniotic fluid, cord blood, or placental samples. These studies have demonstrated that Ureaplasma spp. are habitually found in placentae with chorioamnionitis (Table 1). Despite the fact that up to 100% of placentae infected with Ureaplasma spp. have evidence of histological chorioamnionitis (Table 1), a causative role for these microorganisms has not been satisfactorily explained and is complicated by a number of factors.
TABLE 1.
Incidence of Ureaplasma infection, polymicrobial infections, and chorioamnionitis in women delivering preterm, late preterm, or at termg
| Author(s) of reference (yr) | Reference no. | GA (wk) | Specimen type | n | Incidence, no. positive/no. total (%) |
|||
|---|---|---|---|---|---|---|---|---|
| Ureaplasma infection | Polymicrobial infection |
Ureaplasma spp. |
||||||
| With chorioamnionitis | Without chorioamnionitis | |||||||
| Viscardi et al. (2008) | 222 | <33 | S/CSF | 313 | 74/313 (23.6) | —a | 30/46 (65.0) | 16/46 (35.0) |
| Hassanein et al. (2012) | 310 | <35 | CB | 30 | 13/30 (43.3) | No polymicrobial infections | 7/13 (53.8) | 6/13 (46.2) |
| Gray et al. (1992) | 311 | <28 | AF | 2,461 | 8/2,461 (0.4) | —b | 8/8 (100.0) | 0/8 (0.0) |
| Yoon et al. (1998) | 60 | ≤36 | AF | 120 | 25/120 (20.8) | 11/120 (9.0) | 5/25 (20.0) | |
| Yoon et al. (2003) | 312 | ≤35 | AF | 252 | 23/252 (9.1) | —c | ||
| Park et al. (2013) | 136 | <34 | AF | 56 | 35/56 (62.5) | 7/56 (12.5) | 26/47 (55.31)f | 0/3 (0.0) |
| Kacerovsky et al. (2014) | 16 | 24–36 | AF | 124 | 26/124 (21.0) | 5/124 (4.0)d | ||
| Romero et al. (2015) | 313 | ≤35 | AF | 59 | 6/24 (25.0) | 10/24 (41.7) | 3/6 (50.0) | 2/6 (33.3)f |
| Stepan et al. (2016) | 314 | 24–34 | AF | 122 | 33/122 (27.0) | 8/122 (6.6) | 29/33 (87.9) | 4/33 (12.1) |
| Musilova et al. (2015) | 315 | 24–36 | AF | 166 | 40/166 (24.1) | 19/166 (11.4) | 26/40 (65.0) | 14/40 (35.0) |
| Stepan et al. (2016) | 316 | 24–36 | AF | 386 | 103/386 (26.7) | 32/386 (8.3) | 70/103 (68.0)f | 16/103 (15.5)f |
| Berger et al. (2009) | 317 | ≤33 | AF/PL | 114 | 32/114 (28.1) | —a | 11/25 (44.0)f | 14/25 (66.0)f |
| Hillier et al. (1988) | 1 | <37 | PL | 112 | 32/112 (28.6) | —c | 19/29 (65.5)f | 10/65 (15.4)f |
| Stein et al. (1994) | 318 | Any GA | PL | 182 | 21/182 (11.5) | —e | 11/16f | 5/16f |
| Van Marter et al. (2002) | 319 | <36 | PL | 206 | 58/155 (37.4) | —e | 51/77 (66.2) | 7/78 (9.0) |
| Miralles et al. (2005) | 320 | <33 | PL | 14 | 5/14 (35.7) | 5/14 (35.7) | 4/5 (80.0) | 1/5 (20.0) |
| Egawa et al. (2007) | 135 | <32 | PL | 83 | 4/83 (4.8) | 5/83 (6.0)b | 4/4 (100.0) | 0/4 (0.0) |
| Olomu et al. (2009) | 321 | <28 | PL | 866 | 52/866 (6.0) | 21/52 (40.4) | 34/52 (65.4) | 18/52 (34.6) |
| Kasper et al. (2010) | 202 | <34 | AF | 118 | 32/118 (27.1) | —a | 5/19 (26.3)f | 14/19 (73.7)f |
| Namba et al. (2010) | 134 | ≤32 | PL | 151 | 63/151 (41.7) | 13/151 (8.6) | 52/63 (82.5) | 11/63 (17.5) |
| Roberts et al. (2012) | 4 | >37 | PL | 195 | 2/195 (1.0) | 1/195 (0.5) | 0/2 (0.0) | 2/2 (100.0) |
| Kundsin et al. (1984) | 322 | Various | PL | 801 | 156/801 (19.5) | 18/801 (2.2)b | 32/53 (60.4)f | 21/53 (39.6) |
| Sweeney et al. (2016) | 62 | >32 | PL | 535 | 42/535 (7.9) | 4/57 (7.0) | 26/38 (68.4) | 12/38 (31.6) |
| Cox et al. (2016) | 133 | <37 | PL | 57 | 13/57 (22.8) | 9/24 (37.5) | 4/33 (12.1) | |
Only Ureaplasma spp. were tested for within the study.
Only genital mycoplasmas (Ureaplasma spp. and Mycoplasma hominis) were tested for within this study.
Study states that >1 organism may have been isolated, but prevalence of polymicrobial infections not stated.
Only Ureaplasma spp., Mycoplasma hominis, and Chlamydia trachomatis tested for within this study.
No comment on polymicrobial infections.
Not all placentae in study were tested.
The incidence of chorioamnionitis in Ureaplasma-infected women is frequently high, indicating that these microbes are associated with chorioamnionitis. Abbreviations: AF, amniotic fluid; CB, cord blood; CSF, cerebrospinal fluid; GA, gestational age; PL, placenta; S, serum.
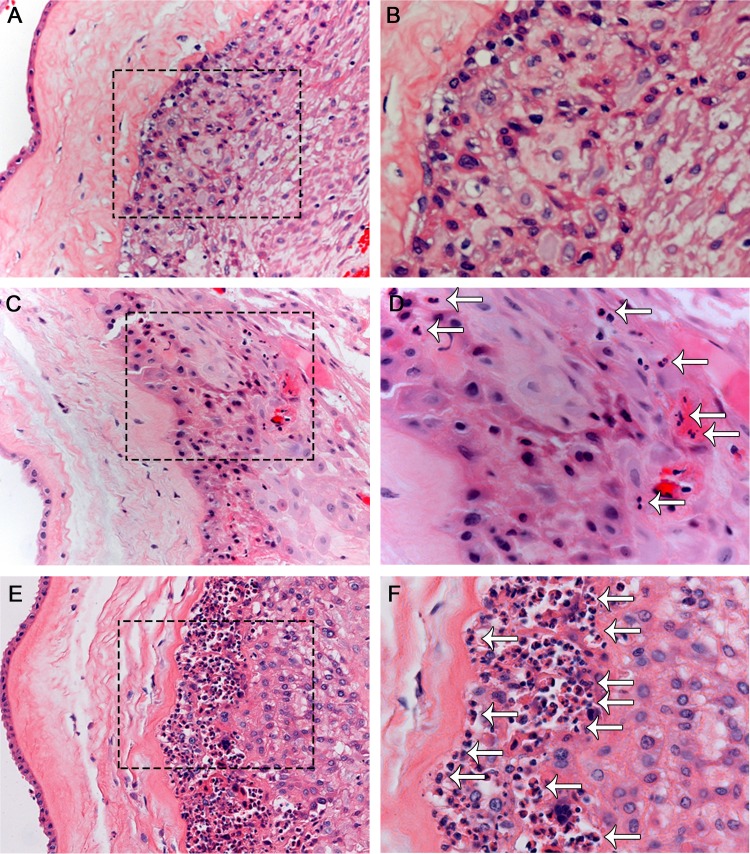
A factor which complicates the role of Ureaplasma spp. in chorioamnionitis is that not all women who are infected with these microorganisms develop chorioamnionitis or experience adverse pregnancy outcomes. Gerber et al. tested the amniotic fluid from 254 asymptomatic pregnant women at 15 to 17 weeks of gestation by PCR and detected Ureaplasma spp. in 29/254 (11.4%) subjects (137). Significantly, this study identified that 24% of women infected/colonized with Ureaplasma spp. delivered preterm, compared to 4.4% of women who were not infected with Ureaplasma spp. However, this study failed to comment on the vast majority (76%) of women in the study who were infected/colonized with Ureaplasma who went on to deliver at term with no apparent adverse outcomes. Similarly, Horowitz et al. detected intra-amniotic Ureaplasma infections in six pregnant women (2.8%), but only three (50%) of these women experienced preterm birth (195). Numerous studies have identified that the severity of upper genital tract Ureaplasma infection/inflammation in pregnant women is highly variable. Some studies have demonstrated that there may be immunological evidence of severe inflammation (196, 197), while in others there may be only moderate inflammation (198), or there may be no correlation between infection with Ureaplasma spp. and inflammation (199) (Fig. 2).
FIG 2.
Differences in the presence of chorioamnionitis in Ureaplasma-infected women. Hematoxylin-and-eosin-stained chorioamnion tissue demonstrates that some women whose placentae are colonized with Ureaplasma spp. have no evidence of chorioamnionitis (A and B), while other women have mild/moderate (C and D) or severe (E and F) evidence of inflammation (demonstrated by neutrophil influx [arrows]) within their chorioamnion, despite high numbers of Ureaplasma spp. present within the tissue. Images are shown at ×200 (A, C, and E) and ×400 (B, D, and F) total magnifications; boxed areas in panels A, C, and E are shown in panels B, D, and F, respectively.
Although it remains unclear why some women infected with Ureaplasma spp. experience adverse pregnancy outcomes while others do not, some researchers have attributed these differences in sequelae to the virulence of the infecting serovar (200), the bacterial load present (201, 202), or genetic background/ethnicity (203, 204). However, these findings are not always consistent, with a recent study by our group demonstrating no correlation between the numbers of Ureaplasma present within placentae, the species/serovar present, or the ethnicity of women infected with Ureaplasma and the incidence or severity of histological chorioamnionitis (62). Furthermore, animal model studies in which Ureaplasma infections have been established with the same strain and dose of U. parvum resulted in divergent inflammatory responses within the chorioamnion (59, 205, 206) and within other genital tract tissues (207), suggesting that the development or magnitude of host immune responses may contribute to the severity of chorioamnionitis. Indeed, we have demonstrated that the human Ureaplasma spp. can undergo immune evasive behavior in vivo by varying the expression of their surface-exposed antigens and that the severity of chorioamnionitis is inversely related to the number of antigenically distinct subtypes detected within amniotic fluid (reviewed in detail below). Therefore, we hypothesize that the ability of some Ureaplasma strains to hide from the immune system may be an important predictor of outcomes and may potentially explain why some women do not develop chorioamnionitis despite high bacterial loads within the amniotic fluid and chorioamnion.
Table 1 summarizes human studies which have investigated the role of Ureaplasma spp. in chorioamnionitis. These studies showed that the rates of Ureaplasma-associated inflammation within the chorioamnion may vary between 0 and 100%, further highlighting the diversity of histological chorioamnionitis and why it is so difficult to confirm the role of these microorganisms as causative agents of chorioamnionitis. Additionally, the pathogenic role of Ureaplasma spp. is often unclear as the majority of these infections are clinically silent. Ureaplasma infections of the chorioamnion can persist asymptomatically for up to 2 months in humans (208), and Ureaplasma-infected placentae cannot be distinguished macroscopically from normal placentae (although there may be histological evidence of chorioamnionitis that is detected following delivery). Due to the predominantly asymptomatic nature of Ureaplasma infections, coupled with the fastidious growth requirements of these microorganisms, pregnant women are not routinely screened for Ureaplasma spp., and therefore, these tiny bacteria are not always suspected (and are, therefore, likely to be underreported) as causative agents of chorioamnionitis.
One of the major reasons why the role of Ureaplasma spp. in chorioamnionitis has remained unconfirmed is due to the polymicrobial nature of chorioamnionitis (5, 209). The majority of studies investigating chorioamnionitis focus specifically on very preterm (<28 weeks) and early preterm (28 to 32 weeks) pregnancies, and these studies have demonstrated that up to 67% of amniotic fluid or placental samples with chorioamnionitis contained at least two detectable microorganisms (often Ureaplasma spp. and another microorganism) (Table 1). Because of this, researchers have not been able to confidently claim that Ureaplasma spp. are true etiological agents of chorioamnionitis. However, a recent study by our research group demonstrated that infections within late preterm (32 to 36 weeks) and term (≥37 weeks) placentae typically harbored only a single microorganism (90.5%) and that the presence of Ureaplasma spp. alone was significantly associated with histological chorioamnionitis, at any gestational age (62). Further investigations confirmed the finding that placental infections with Ureaplasma spp. are strongly associated with chorioamnionitis, using whole-genome shotgun sequencing of late preterm and term placentae (120). Similarly, another study has reported that preterm placentae infected with Ureaplasma spp. alone are independently associated with inflammation of the chorioamnion membranes. This study demonstrated that there were no differences in the incidence of chorioamnionitis in placentae infected with Ureaplasma spp. and other microorganisms compared to placentae infected with Ureaplasma spp. alone (210). Taken together, these recent data not only suggest that Ureaplasma spp. are likely to be a key etiological agent of chorioamnionitis in the absence of other microorganisms but also support a causal role for Ureaplasma in chorioamnionitis throughout pregnancy.
ANIMAL MODELS HAVE HELPED TO ELUCIDATE THE PATHOGENESIS OF UREAPLASMA CHORIOAMNIONITIS
Studies in experimental animal models have confirmed that Ureaplasma spp. can cause chorioamnionitis and fetal inflammation following intrauterine inoculation. Using a nonhuman primate model, Novy et al. (211) inoculated 107 CFU of U. parvum serovar 1 into the amniotic fluid of pregnant rhesus macaques at day 132 to 147 of gestation (term = 155 to 172 days) via an indwelling catheter. Intra-amniotic U. parvum caused a significant influx of leukocytes into the amniotic fluid and significant increases in the amniotic fluid levels of (i) TNF-α, IL-1β, IL-1ra, IL-6, and IL-8; (ii) PGE2 and PGF2α; and (iii) latent (92-kDa) and active (83-kDa) MMP-9 compared with preinoculation baseline values. A progressive increase in uterine activity was also observed following U. parvum intra-amniotic inoculation, and the mean inoculation-to-labor onset period was significantly reduced in U. parvum-infected animals compared to those inoculated with sterile medium or saline. Histological examination of fetal membranes revealed acute chorioamnionitis that was characterized by edematous thickening of the chorioamnion, neutrophil infiltration, denudation of amnion epithelial cells, and necrosis and microabscess formation in chorion trophoblast cells (211). Similarly, intra-amniotic injection of U. parvum serovar 1 into the amniotic cavity of pregnant baboons at day 122 to 123 of gestation (term is 185 days) resulted in elevated levels of amniotic fluid IL-6 and IL-8 at the time of preterm delivery (125 days) and histological evidence of acute chorioamnionitis (212). In contrast, more-recent studies in rhesus macaques demonstrated that despite the presence of high numbers (3.9 × 107 CFU/ml) of U. parvum serovar 1 within the amniotic fluid, no chorioamnionitis was detected after acute durations (3 days and 7 days) of infection (213).
While nonhuman primate models exhibit the closest resemblance to humans with respect to gestational length, uterine anatomy, and parturition, experimental intrauterine infection causes preterm delivery (211, 214), and therefore, it is only possible to study acute chorioamnionitis in these models. In contrast, sheep do not experience inflammation-induced preterm birth, as intra-amniotic infection/inflammation does not cause significant activation of the fetal HPA axis, cortisol production, and subsequent progesterone withdrawal, which are required for the initiation of labor in many species (215–217). This enables the study of chronic, asymptomatic intrauterine infection and chorioamnionitis, which is not possible using other animal models. In addition, fetal sheep are similar in size to human fetuses, which enables instrumentation of the ewe and fetus (217), and thus makes the ovine model very useful for the study of fetal development and neonatal outcomes following chorioamnionitis exposure.
We have demonstrated that human U. parvum clinical isolates injected into the amniotic cavity of pregnant sheep at 55 days (term is 150 days) can chronically colonize the amniotic fluid and fetus (59, 205, 215, 218). Following an intra-amniotic injection of 2 × 104 CFU of U. parvum serovar 6 at 55 days of gestation, temporal analysis demonstrated that the peak of amniotic fluid infection occurred between 87 days and 101 days of gestation and that the number of CFU per milliliter remained high (approximately 107 CFU/ml) until the time of surgical delivery at 140 days (59). These data demonstrate that Ureaplasma can chronically colonize the amniotic fluid for at least 85 days and suggest that amniotic fluid, a rich source of urea, can support the long-term growth of these microorganisms. We further demonstrated that U. parvum was consistently isolated from the chorioamnion and fetal lung following chronic intra-amniotic infection (205, 215, 218–220) and was also isolated from the umbilical cord and other fetal tissues, including cerebrospinal fluid, gut, kidney, liver, and spleen (205). These findings are consistent with human studies that have reported that Ureaplasma spp. may systemically infect the fetus, leading to neonatal morbidity and mortality (221–228).
Both chronic and acute intrauterine Ureaplasma infections were capable of causing histological chorioamnionitis in pregnant sheep (59, 205, 206, 218, 219). Intra-amniotic U. parvum infection was also associated with increased expression of IL-1β, IL-6, and IL-8 mRNA within the chorioamnion (59, 219) and an influx of neutrophils, monocytes/macrophages, and lymphocytes (59, 205, 218), compared to medium (vehicle) controls. Generally, the severity of chorioamnionitis correlated with increased duration of intra-amniotic Ureaplasma exposure (206); however, variability in the severity of inflammation was a notable feature of these sheep studies (205, 206), consistent with findings from human pathological investigations. Despite 100% of chorioamnion samples being infected with U. parvum, the severity of chorioamnionitis ranged from moderate (characterized by inflammatory cell infiltrate, fibrosis, scarring, sloughing of the amnion epithelium, and disruption of the normal tissue architecture) to no histological evidence of chorioamnionitis (205). The severity of chorioamnionitis was not related to the bacterial load within the chorioamnion at the time of delivery, the inoculating serovar, or the initial dose of U. parvum (205).
In an attempt to explain the differences in severity of Ureaplasma chorioamnionitis and address whether some Ureaplasma isolates are inherently more virulent than others, we infected the amniotic cavity of pregnant sheep with clonal U. parvum serovar 6 isolates (59), derived from placental isolates, which had caused severe histological chorioamnionitis (virulent strain-derived strain) or no chorioamnionitis (avirulent strain-derived strain) in a previous ovine study (205). Regardless of the inoculating clonal strain, moderate to severe chorioamnionitis was observed in experimentally infected animals and there were no differences in the chorioamnion expression of TLR-1, TLR-2, TLR-6, IL-1β, IL-6, IL-8, IL-10, and TNF-α between animals infected with the avirulent strain-derived strain and those infected with the virulent strain-derived strain. Similarly, there were no differences in the numbers of U. parvum isolated from the amniotic fluid, chorioamnion, cord, or fetal lung at 140 days (59). In the same study, we demonstrated that only a subpopulation of infected ewes from each group generated a serum IgG response to intrauterine U. parvum infection. When cytokine expression was compared between animals with and without anti-Ureaplasma serum IgG, the expression of IL-1β, IL-6, and IL-8 was significantly increased in the chorioamnion of anti-Ureaplasma IgG+ animals. In addition, maternal anti-Ureaplasma serum IgG was associated with a significant increase in meconium-stained amniotic fluid (59). These findings are also consistent with human studies that have demonstrated that patients with anti-Ureaplasma antibodies are at a higher risk for adverse pregnancy and neonatal outcomes than are those who do not develop a humoral immune response (229, 230). Taken together, this suggests that Ureaplasma strains are not likely to be inherently virulent or avirulent but that the host response to infection may affect the pathogenesis of chorioamnionitis.
The Immune Response to Ureaplasma Chorioamnionitis: Harmful or Helpful?
Studies in BALB/c and C57BL/6 mice have provided unique insights into the potentially harmful immune responses that may occur during Ureaplasma chorioamnionitis. BALB/c mice typically display a Th1/M1-dominant immune profile, whereas the immune profile of C57BL/6 mice is consistent with a Th2/M2 bias (203). These differences have enabled researchers to examine the immunopathogenic role of a skewed Th1/M1 or Th2/M2 response in Ureaplasma chorioamnionitis. In a model of experimental intrauterine infection, von Chamier et al. injected 107 CFU of U. parvum into the uterine horns of pregnant BALB/c and C57BL/6 mice at 14 days (203). Examination of the fetal membranes at 72 h postinfection demonstrated that C57BL/6 mice exhibited mild-moderate chorioamnionitis, whereas BALB/c mice displayed severe necrotizing chorioamnionitis and extensive neutrophil infiltration. These differences could not be attributed to differences in bacterial load; however, the placental expression levels of cytokines and calgranulins were markedly different between the strains (203). In a separate study, it was demonstrated that intrauterine U. parvum infection increased the expression of TLR2 and CD14 on neutrophils in BALB/c but not C57BL/6 mice (56). TLR/CD14-mediated signaling triggered by bacterial lipoproteins has been shown to extend the survival of apoptotic neutrophils in infected tissues, thereby increasing the duration of inflammation (231). It is therefore possible that TLR2/CD14 signaling plays a role in the extensive neutrophil infiltration and severe chorioamnionitis observed in BALB/c mice. Interestingly, increased levels of soluble CD14 are also observed in the amniotic fluid of women with intrauterine Ureaplasma infection (232), suggesting that CD14 signaling may be an important area for future research. Combined, these studies demonstrate that the host immune response may be a key factor that modulates the pathogenesis of acute Ureaplasma chorioamnionitis. Further studies using genetically modified/knockout mouse lines may significantly improve our understanding of protective versus pathogenic immune responses to intrauterine Ureaplasma infection.
Immune Effects of Ureaplasma spp. on the Fetus
Animal model studies from our research group have investigated the fetal immune responses to U. parvum exposure during gestation. In a series of experiments in pregnant sheep, it was demonstrated that chronic (69 days), but not acute (7 days), in utero infections with U. parvum suppressed innate immune responses in fetal sheep. Fetuses were challenged with E. coli LPS 2 days prior to delivery, and the fetuses that were chronically exposed to intra-amniotic Ureaplasma spp. demonstrated significant decreases in pro- and anti-inflammatory cytokine expression, as well as fewer CD3+ T lymphocytes and myeloperoxidase+ cells within the fetal lung, compared to the fetuses that were intra-amniotically exposed to sterile culture medium (vehicle). Blood monocytes obtained from these same animals also had a significantly decreased response to LPS in vitro (121), demonstrating that fetal exposure to U. parvum in utero can markedly alter the neonatal immune responses following delivery. Similarly, chronic exposure to U. parvum alone (with no LPS challenge) was sufficient to augment the presence of transforming growth factor beta (TGF-β) within the fetal lung, which may also contribute to the development of lung pathologies, such as bronchopulmonary dysplasia (233).
In both rhesus macaque and sheep models, intra-amniotic U. parvum infections decreased the populations of CD4+ FOXP3+ regulatory T cells (Tregs) in the preterm fetus, in both the thymus and the periphery (213, 234). Furthermore, a gamma interferon response was seen in Tregs exposed to U. parvum during gestation, and this response was absent in Tregs of fetuses exposed to control (medium) intra-amniotic injections. Since it is well established that Tregs are potent anti-inflammatory T cells (235), these results suggest the existence of a subset of Tregs that can develop a Th1 phenotype early in life and suggest that this response may be increased in the presence of inflammation (e.g., chorioamnionitis).
MANIPULATION OF HOST CELLS BY UREAPLASMA SPP.
Compared to other Mycoplasma spp., the cytadherence of Ureaplasma has not been investigated in detail. In vitro studies have demonstrated that Ureaplasma spp. are adherent to erythrocytes (236), placental endothelial cells (237), and human epithelial cells (238); however, the adhesion mechanisms are unknown. Pretreatment of HeLa cells and erythrocytes with neuraminidase significantly reduced ureaplasmal adherence (238), suggesting that Ureaplasma may bind to receptors containing sialic acid. In contrast, the adhesion of Ureaplasma to spermatozoa is thought to be mediated by sulfogalactoglycerolipid, which is expressed by the mammalian male germ cell membrane (239).
The human Ureaplasma spp. have been shown to alter/manipulate host cells in several ways. Allam et al. reported that U. parvum significantly increased filamin A phosphorylation at serine 2152 in human benign prostate cells and altered its intracellular distribution (240). Filamin A is an actin-binding protein that regulates the cytoskeleton and is involved in antimicrobial signaling pathways (241). Further investigation into the upstream and downstream signaling events may therefore reveal novel insights into Ureaplasma-host interactions. In endothelial cells isolated from normal and preeclamptic placentae, U. urealyticum significantly reduced cell viability, altered the expression of heat shock protein 70, and significantly increased the intracellular concentration of calcium and iron. It was suggested that these events occurred as part of the cellular stress response to infection and may indicate that cells are progressing toward apoptosis (237). Additional studies have demonstrated that U. urealyticum induces apoptosis in other cell types, including human lung epithelial cells (A549) and THP-1-derived macrophages (242). Ureaplasma-infected cells demonstrated an altered morphology and underwent DNA fragmentation and translocation of phosphatidylserine to the outside surface of the cell (as determined by annexin V staining and flow cytometry) (242). Ureaplasma spp. further manipulate host cells by suppressing innate host defense pathways. A recent study demonstrated that Ureaplasma infection decreased the expression of antimicrobial peptide genes in THP-1 cells in vitro, in association with a significant decrease in histone H3K9 acetylation (243). These findings suggest that Ureaplasma may downregulate antimicrobial/host defense genes via epigenetic modifications (243), which may be an important factor contributing to the ability of these microorganisms to cause persistent infections. Further studies using a combination of ex vivo and in vivo approaches are required to elucidate the host-pathogen interactions that occur during Ureaplasma chorioamnionitis.
UREAPLASMA VIRULENCE FACTORS
While Ureaplasma spp. were traditionally portrayed as microorganisms of low virulence, they are now recognized as the cause of serious disease. As such, Ureaplasma spp. have evolved specific virulence mechanisms that contribute to their survival and disease pathogenesis. Five proposed virulence factors have been identified: the multiple-banded antigen (MBA), phospholipases A and C, IgA protease, and the urease gene of Ureaplasma spp. Genetic manipulation of these microorganisms has remained elusive, and thus definitive roles for these proposed virulence factors have not been determined. Furthermore, recent genome sequencing studies have questioned the presence of some of these proposed virulence factors.
Multiple-Banded Antigen (MBA)
The MBA was first described by Watson et al. (244) and has since been identified as one of the major virulence factors of the human Ureaplasma spp. The mba gene, which encodes the MBA protein, contains no homology to any other known prokaryotes and is unique to Ureaplasma spp. (245). The MBA protein is the major antigen that is recognized by the host during infection and elicits the production of cytokines by activating nuclear factor kappa B via TLR-1, -2, and -6 (246–248). The MBA protein consists of three major domains: a typical prokaryotic signal peptide, an N-terminal transmembrane domain that is conserved among all 14 serovars of Ureaplasma spp., and a C-terminal (surface-exposed) variable domain that is composed of multiple repeating units, with both serovar-specific and cross-reactive epitopes (249, 250). The C-terminal region of the MBA has been shown to alter by switching on/off the gene (antigenic phase variation) and more commonly to vary in size (antigenic size variation) (59, 205, 249–252). U. urealyticum serovar 13 is the only Ureaplasma serovar that does not contain any tandem repeat units in the C-terminal variable domain of mba (145).
While some studies demonstrated differences in the size of the MBA protein (giving rise to the name of the protein itself as the multiple-banded antigen) (244, 252), the first study to characterize MBA size variation demonstrated that differences in the size of the MBA protein directly correlated with the number of tandem repeating units within the mba gene (149, 253). More recently, Knox et al. identified mba/MBA size variation in vivo using an ovine model (205). Pregnant ewes were chronically infected for 69 days with a nonclonal U. parvum isolate, and the size of mba/MBA was assessed. This study demonstrated that the number of mba/MBA size variants was inversely correlated with the severity of inflammation within the chorioamnion: when >9 mba/MBA size variants were identified, there was little or no chorioamnionitis; however, when <5 mba/MBA size variants were identified, there was severe histological chorioamnionitis (205). Other ovine studies have identified that variation in the size of the mba/MBA was not seen after 3 days of intra-amniotic infection, while some slight variation was seen after 7 days of infection (206) and significant mba/MBA size variation was seen after 69 days of chronic intra-amniotic U. parvum infection (59, 205, 206). Dando et al. (59) also demonstrated the ability of Ureaplasma spp. to vary their mba/MBA size throughout the course of gestation and suggested that size variation of mba/MBA (presumably by slipped-strand mispairing) may be a mechanism by which Ureaplasma spp. evade host immune recognition, allowing chronic asymptomatic infections to develop (59).
More recently, we have demonstrated for the first time that Ureaplasma clinical isolates from human placentae were also able to vary the size of their mba/MBA (E. L. Sweeney, S. Meawad, S. G. Kallapur, C. A. Chougnet, T. Gisslen, S. Stephenson, A. H. Jobe, and C. L. Knox, unpublished data). Clinical isolates that varied the size of their mba/MBA were associated with a reduced incidence of histological chorioamnionitis and significantly lower levels of the cord blood cytokines G-CSF and IL-8. In contrast, Ureaplasma spp. isolated from placentae that demonstrated no mba/MBA size variation were associated with severe histological chorioamnionitis and elevated cord blood cytokines. Further in vitro investigations using recombinant MBA (rMBA) proteins of differing sizes (i.e., different numbers of tandem repeat units) and human macrophage cell lines demonstrated immune responses that varied depending on the size of the rMBA. These results were confirmed by Western blot analysis; the expression of nuclear factor kappa B fragment p65 (an activator of transcription) varied when stimulated with the different-size rMBA proteins (Sweeney et al., unpublished). Combined, these results confirm the ability of Ureaplasma spp. to vary their surface-exposed MBAs in vivo and confirm that this variation is associated with the modulation of the host immune response both in vivo and in vitro.
Other studies have also demonstrated that mba/MBA can undergo phase (on/off-switching) variation. Three studies have identified that selective antibody pressure directed against the MBA can result in the generation of MBA-negative variants (Ureaplasma isolates that do not express their MBA protein) in serial passage experiments (59, 251, 254). In these studies, MBA-negative Ureaplasma isolates were detected following two to three serial passages in culture medium containing MBA-specific antibodies (59, 251). More recently, phase variation of the MBA occurred in the absence of any selective (antibody) pressures (255), indicating that this antigen is capable of rapid phase variation. Zimmerman et al. (254) hypothesized that the expression of the mba gene (locus UU375) is alternated with expression of an adjacent locus (UU376), which encodes a Ureaplasma-specific conserved hypothetical protein. Utilizing polyclonal rabbit antisera generated against the conserved (N-terminal, nonrepetitive) regions of MBA and UU376, these authors identified that antibody treatment led to the emergence of escape variants, which expressed the protein that had not been the target of selective pressure. Following this, it was hypothesized that DNA inversion events—presumably occurring at short inversion sequences—were responsible for the switching-on/off expression of these genes (254). Zimmerman and colleagues further investigated the role of DNA inversion sites within the Ureaplasma genome and demonstrated experimentally that the mba paralogues UU171 and UU172 and the orthologue UU144 were also involved in site-specific DNA inversion/recombination (256). Furthermore, it was shown that the XerC tyrosine recombinase gene of U. parvum is the most likely mediator of these DNA inversion events (257). Subsequent experimental investigation into the ability of XerC to process the recombination event proved successful, indicating that this tyrosine recombinase is able to induce DNA inversion events (258), representing the first evidence of a mechanism which may govern antigenic phase variation in Ureaplasma spp.
In a separate series of investigations, whole-genome sequencing was carried out on Ureaplasma ATCC strains and a range of clinical isolates and revealed the presence of multiple additional tandem repeat domains within the mba locus of all Ureaplasma isolates tested (145). Remarkably, it was shown that mba was part of a large gene superfamily, comprising 183 genes in U. parvum and U. urealyticum and 22 gene subfamilies. This study also identified the presence of putative recombination sites surrounding tandem repeating domains, consistent with the theory that Ureaplasma spp. may undergo significant antigenic phase and size variation, dependent on which sequences within the genome are expressed. While there is convincing molecular evidence that the mba gene is part of a complex phase-variable system, it should be noted that, to the best of our knowledge, MBA-negative Ureaplasma variants have not been isolated from human clinical material or experimental animal studies. Rather, there is significant evidence of MBA size variation in vivo.
Phospholipases A and C
The pathogenesis of phospholipases results from the production of membrane-destabilizing compounds and degradation of the host cell membrane phospholipids (259). Endogenous phospholipase A1, A2, and C activity has been previously identified in U. parvum serovar 3 and U. urealyticum serovars 4 and 8 (260–262). These phospholipases demonstrated higher activity in Ureaplasma during their exponential growth phase, suggesting that the Ureaplasma phospholipases were membrane bound and were not being secreted (261). It was further identified that phospholipase A2 activity was 3-fold higher in U. urealyticum serovar 8 than in U. urealyticum serovar 4 and U. parvum serovar 3 (260). However, subsequent whole-genome sequencing of U. parvum serovar 3 could not identify any genes of significant similarity to any known sequences of phospholipase A1, A2, or C (245). These findings indicated that Ureaplasma may encode phospholipases that are evolutionarily distinct from other phospholipase genes or that these phospholipases may not exist within Ureaplasma spp. Interestingly, more recent studies by the same research group revealed that whole-genome sequencing of the 14 Ureaplasma serovars and four Ureaplasma clinical isolates was again unable to detect any phospholipase A1, A2, or C genes; however, a phospholipase D domain-containing protein was identified in all Ureaplasma spp. (145). These researchers further investigated the presence/activity of these enzymes experimentally and were unable to detect any significant phospholipase C or D activity in U. parvum serovar 3 and U. urealyticum serovar 8 (145). Further investigations into the presence and activity of phospholipases within Ureaplasma spp. are required to elucidate if these enzymes are potential virulence factors of these organisms.
Immunoglobulin A (IgA) Protease
One of the primary defense mechanisms of the mammalian immune system is the production of IgA at mucosal sites (263), and the ability of an organism to degrade IgA antibodies allows the microorganism to evade this host defense mechanism. Robertson et al. published the first evidence of an IgA protease in U. urealyticum that was capable of cleaving IgA1 (264). While it was subsequently determined that all 14 Ureaplasma serovars possess an IgA protease with proteolytic activity against IgA1 (but no proteolytic activity against IgA2, IgG, or IgM antibodies) (265, 266), more recent evidence has questioned the presence of an IgA protease in Ureaplasma spp. Initial genome sequencing studies of U. parvum serovar 3 were unable to identify any genes with similarity to known IgA proteases (245), and more recent whole-genome analyses were unable to identify any IgA protease genes within the 14 Ureaplasma serovars, nor were they found to be present in any of the Ureaplasma clinical isolates tested (145). Recently, an IgG binding protein and IgG serine protease were identified within Mycoplasma mycoides subsp. capri. This study provided evidence that both U. parvum and U. urealyticum contain genes that encode an IgG binding protein and an IgG serine protease within their genomes (267). Based on these recent findings, further studies are warranted to determine if these IgG binding/IgG protease genes are active in cleaving IgG and therefore may be a previously unrecognized virulence factor of the human Ureaplasma spp.
Urease
The ability of Ureaplasma spp. to hydrolyze urea was first identified in 1966, and the production of ATP via this mechanism appears to be unique within Ureaplasma (141, 268). The urease enzyme is a key virulence factor of many ureolytic bacteria, and the ureaplasmal urease gene cluster has a genetic organization similar to that of E. coli, Proteus mirabilis, Klebsiella pneumoniae, and Klebsiella aerogenes (269). The urease complex constitutes a major component of the ureaplasmal cytoplasm (270), and Takebe et al. demonstrated that the urease of U. urealyticum serovar 8 was responsible for urolithiasis in humans (271). The Ureaplasma urease has a significantly higher specific activity than other bacterial ureases (272) and was responsible for lethal toxicity in mice following intravenous injection (273). Interestingly, the Ureaplasma spp. are some of the few bacterial species which encode a urease enzyme but lack the ability to assimilate ammonia into glutamine or glutamate (274), potentially explaining the very high intracellular ammonia concentration of these microorganisms (140).
Our recent studies suggest that Ureaplasma infection, and a subsequent increase in ammonia due to urease metabolism, can alter the pH of amniotic fluid and fetal lung fluid in an ovine model (206). This study also identified that the increased pH within the fetal lung was associated with lung damage, even in the absence of inflammatory responses, and provides the first evidence that increased pH in vivo may be due to Ureaplasma infections. Other studies have demonstrated that Ureaplasma infections can result in hyperammonemia (275). Clinical reports describe that patients who underwent lung transplantation and subsequently developed hyperammonemia (abnormally high levels of ammonia within the blood) were found to be infected with Ureaplasma spp. within their blood or bronchoalveolar lavage fluid. When these patients received antibiotic treatment to eradicate the Ureaplasma spp., their syndromes resolved, and only one relapse was identified, in a patient colonized with an antimicrobial-resistant Ureaplasma strain (275). Taken together, these findings suggest that the activity of the Ureaplasma urease enzyme can result in an alkaline environment in both fetal and adult lungs and also within amniotic fluid.
HORIZONTAL GENE TRANSFER (HGT) AND THE ABILITY OF UREAPLASMA SPP. TO RAPIDLY ADAPT TO HOST MICROENVIRONMENTS
HGT is an important mechanism used by microorganisms to acquire genetic material. Although Ureaplasma spp. maintain minimal genomes that have undergone significant degenerative evolution (245), recent evidence has identified that HGT is likely to occur within these microorganisms and may be an important determinant of virulence. As previously discussed, the identification of genetic hybrids (162) suggests that the Ureaplasma spp. may be genetically promiscuous. Comparative genome sequencing studies have provided further evidence of this and identified integrase-recombinase genes, transposases, and phage-related proteins in Ureaplasma genomes (145), which are highly indicative of HGT events. Interestingly, U. urealyticum genomes generally contained a higher number of these genes, suggesting that this species may be more capable of acquiring genes horizontally than U. parvum (145).
Early attempts to define the phylogeny of Mycoplasma suggested that Mycoplasma spp. with the smallest genomes have high mutation rates and undergo rapid evolution (276, 277). Dando et al. provided evidence of the ability of the human Ureaplasma spp. to rapidly adapt to their microenvironment in a sheep model of intrauterine infection (278). Following injection of a nonclonal U. parvum serovar 3 isolate into the amniotic fluid of pregnant sheep at 55 days, significant genetic variability within the 23S rRNA gene was detected between U. parvum isolated from the amniotic fluid and chorioamnion at the time of preterm surgical delivery (125 days). While U. parvum isolated from amniotic fluid showed 100% 23S rRNA domain V sequence homology to the original strain injected, highly polymorphic sequences (containing only 64 to 82% sequence homology to the inoculating strain) were detected within Ureaplasma isolates from the chorioamnion. Furthermore, chorioamnion Ureaplasma isolates demonstrated the presence of macrolide resistance genes, which were not evident in amniotic fluid isolates. While this study did not investigate the presence of potential genetic transfer elements flanking these variable gene sequences, these data support the concept that Ureaplasma spp. may undergo significant HGT in vivo. Furthermore, this study suggests that different anatomical sites (amniotic fluid versus chorioamnion) may select for different Ureaplasma subtypes within nonclonal populations and thus influence the sociomicrobiological structure of the bacterial population (278). Taken together, there is increasing evidence that Ureaplasma spp. undergo significant genetic variation, allowing them to diversify their populations, and this is likely to contribute to the overall pathogenicity of the Ureaplasma spp.
TREATMENT OF UREAPLASMA CHORIOAMNIONITIS AND THERAPEUTIC CONSIDERATIONS
The major difficulty in treating chorioamnionitis is that a large proportion of cases are clinically asymptomatic and therefore are not diagnosed until retrospective analysis of the placenta and fetal membranes. This is particularly problematic for the human Ureaplasma spp., which can cause chronic, asymptomatic intrauterine infections that modulate the host immune response to prevent significant pathological events but are still associated with adverse outcomes. While antibiotics are recommended for women with preterm prelabor rupture of membranes (279) to prevent ascending invasive infections from the lower genital tract, the timing of administration may be too late to have beneficial effects against chronic Ureaplasma infections that were established in early/midgestation. It has been suggested that the administration of appropriate antibiotics before 22 weeks of gestation (or before inflammation and maternal-fetal damage occur) could significantly decrease the incidence of preterm birth (280). This is supported by a meta-analysis which demonstrated that the administration of macrolides and clindamycin during the second trimester of pregnancy was associated with a reduced risk of preterm delivery (281). However, due to concern about antibiotic resistance, widespread antimicrobial treatment is not recommended unless there is evidence of intra-amniotic infection. Culture and/or PCR detection of Ureaplasma spp. within amniotic fluid remains the gold standard for diagnosis; however, amniocentesis is an invasive procedure that is not routinely performed, and it is likely that high numbers of Ureaplasma infections during pregnancy remain undetected and therefore untreated.
An additional complicating factor for the treatment of Ureaplasma chorioamnionitis includes the often polymicrobial nature of this disease, which suggests that more than one antimicrobial agent may be required to successfully eradicate infection. Furthermore, treatment options for pregnant women are limited due to potential teratogenic and harmful effects associated with the use of some antimicrobials during pregnancy. Even fewer options are available for the treatment of intrauterine Ureaplasma infections, as these microorganisms are inherently resistant to beta-lactam and glycopeptide antibiotics (due to their lack of a cell wall), as well as trimethoprim and sulfonamides (as Ureaplasma spp. do not synthesize folic acid) (282). Antimicrobials that are potentially active against Ureaplasma include the tetracyclines, fluoroquinolones, and macrolides; however, resistance to these antimicrobial classes has also been well described (283–287).
Erythromycin, a 14-membered lactone ring macrolide, is the most common antibiotic used for the treatment of neonatal Ureaplasma infections and is routinely used in clinical obstetrics. Large randomized controls and meta-analyses have demonstrated that erythromycin administration for preterm prelabor rupture of membranes can reduce the risk of chorioamnionitis and neonatal morbidity and delay preterm birth (288–290). However, it is less clear if maternal erythromycin can eradicate existing human intrauterine infections due to conflicting reports within the literature (291–293). In pregnant sheep, maternal intramuscular erythromycin treatment (30 mg/kg of body weight/day for 4 days) failed to eradicate an erythromycin-susceptible strain of U. parvum from the amniotic fluid, chorioamnion, and fetal lung (218), presumably due to poor transplacental passage (218, 294–296). In a follow-up study, it was again demonstrated that intra-amniotic Ureaplasma infection was not eradicated following (i) single intra-amniotic and repeated maternal intramuscular erythromycin or (ii) single maternal intramuscular and repeated intra-amniotic erythromycin injections (297). These data suggest that erythromycin may not be beneficial for the treatment of intrauterine Ureaplasma infections.
Azithromycin is a 15-membered semisynthetic macrolide with superior tissue penetration, a prolonged half-life, and broader antimicrobial coverage than erythromycin (298). Azithromycin is well tolerated during pregnancy and achieves peak concentrations of 151 ± 46 ng/ml within human amniotic fluid and 2,130 ± 340 ng/ml within human placentae at 6 h postinjection, before rapidly declining (298). In pregnant sheep, a single intra-amniotic injection of azithromycin achieved therapeutic concentrations that were sustained for 48 h; however, there was poor maternal-fetal transfer (296). Despite this, a single maternal intravenous azithromycin injection or a single maternal intravenous azithromycin injection combined with an intra-amniotic azithromycin injection completely eradicated an established U. parvum infection from the amniotic fluid, chorioamnion, and fetal lung in pregnant sheep (299). Similarly, studies in rhesus macaques demonstrated that maternal intravenous azithromycin (25 mg/kg/day for 10 days) administered 6 to 8 days after intra-amniotic U. parvum inoculation successfully eradicated Ureaplasma from the amniotic fluid (300, 301). It should be noted that in both of these sheep (299) and monkey (301) studies, histological evidence of chorioamnionitis was still observed at the time of delivery, suggesting that azithromycin treatment alone is not sufficient to reduce/eliminate inflammation within the fetal membranes.
Recent research efforts have evaluated a new, broad-spectrum fluoroketolide, solithromycin, in pregnant sheep and demonstrated that a single maternal dose can deliver therapeutic concentrations to both the fetus and the amniotic fluid (302). The transplacental transfer of solithromycin was significantly higher than that reported for other macrolides, including azithromycin, and a maternal intravenous infusion resulted in sustained therapeutic concentrations within maternal plasma, fetal plasma, and amniotic fluid for >12 h (302). In vitro, solithromycin has potent activity against human clinical Ureaplasma isolates (303, 304), in addition to a range of other important pathogens (305–309). Both maternal intravenous solithromycin and maternal intravenous solithromycin combined with intra-amniotic solithromycin effectively eradicated U. parvum from the amniotic cavity of pregnant sheep but, similarly to azithromycin, failed to reduce inflammation of the chorioamnion and fetal lung (299). These findings suggest that solithromycin may not accumulate in high-enough concentrations to exert anti-inflammatory effects and that coadministration of immune modulators should be investigated. To date, solithromycin is the most potent antimicrobial for the treatment of genital mycoplasmas and has several pharmacokinetic advantages over older macrolides, suggesting that it may be useful for the treatment of intrauterine infections. Human studies are required to further examine the effectiveness and safety of solithromycin in pregnancy and chorioamnionitis.
CONCLUDING REMARKS AND FUTURE RESEARCH DIRECTIONS
In conclusion, the findings of both human and animal studies have now demonstrated that infection with Ureaplasma spp. alone can cause chorioamnionitis, demonstrating a true causal role for these microorganisms in disease. Furthermore, the ability of Ureaplasma spp. to vary the expression and size of their major surface-exposed antigen, the MBA, indicates that these pathogens have evolved specific virulence mechanisms to avoid immune detection by the host. Despite the lack of genetic manipulation studies, both animal and human research has now shown the involvement of the MBA in modulating the host response to chorioamnionitis, and our most recent study has demonstrated that recombinant MBA proteins of different sizes elicit different immune responses, potentially as a consequence of altered nuclear factor kappa B activation. We predict that this highly variable surface antigen expression facilitates immune evasion, enabling these microorganisms to cause chronic in utero infections, and further research is required to elucidate the mechanisms of antigenic variation in Ureaplasma spp. This may also assist in understanding the progression of disease during Ureaplasma infections and provide unique insights into the host-microbe interactions that occur in vivo. Furthermore, the development of genetic tools to create isogenic deletion mutants would enable researchers to assign definitive roles to proposed ureaplasmal virulence factors.
Due to the difficulties associated with identifying and diagnosing Ureaplasma infections and chorioamnionitis, additional research should be undertaken to identify biomarkers for the rapid diagnosis of Ureaplasma in order to detect subclinical infections and clinically silent chorioamnionitis. Due to the unique metabolism of the Ureaplasma spp., “omics” profiling of Ureaplasma-infected amniotic fluid may identify unique molecular signatures that could be used for diagnostic purposes, in combination with conventional Ureaplasma culture/PCR identification. This is a critical area of research that may lead to the improved identification and treatment of in utero inflammation, which will ultimately lead to improved maternal and neonatal outcomes. We also propose that amniotic fluid collected from pregnant women undergoing amniocentesis should be routinely tested for Ureaplasma spp., even in the absence of clinical signs/symptoms of chorioamnionitis. Additionally, further studies are required to identify effective and targeted therapies that eradicate intrauterine Ureaplasma infections and reduce inflammation. Continued research investigating the pharmacokinetics and anti-Ureaplasma activity of new-generation drugs, potentially in combination with immunomodulatory agents, may lead to the development of more effective treatment options for Ureaplasma chorioamnionitis.
Biographies
Emma L. Sweeney received her Ph.D. in 2015 from Queensland University of Technology (QUT), Australia. Her project investigated the presence and diversity of microorganisms, particularly the human Ureaplasma species, in adverse pregnancy outcomes with a focus on Ureaplasma pathogenesis in histological chorioamnionitis. Dr. Sweeney was subsequently appointed a postdoctoral research fellow at QUT, investigating the oral neonatal microbiome and how oral bacterial communities are regulated by reactive oxygen species that are produced when human breast milk and neonatal saliva combine. Dr. Sweeney has worked on the topic of Ureaplasma spp. for 6 years and hopes to continue research into the role of these minimalistic pathogens in human and animal infections and the host-microbe interactions that facilitate disease.
Samantha J. Dando received her Ph.D. in microbiology in 2012 from Queensland University of Technology, Australia, where she studied the pathogenesis of intrauterine Ureaplasma infections in an experimental ovine model. She has published seminal papers in this field, which have significantly improved our understanding of chronic, intra-amniotic ureaplasma infections. Dr. Dando subsequently undertook postdoctoral research at Griffith University, where she investigated the novel mechanisms by which Burkholderia pseudomallei can directly invade the central nervous system via the olfactory and trigeminal nerves within the nasal cavity. In her current position at Monash Biomedicine Discovery Institute, Monash University, Dr. Dando's research focuses on characterizing myeloid cell populations within various subcompartments of the eye and brain and how these cells respond to systemic inflammatory mediators. Dr. Dando also continues to be active in Ureaplasma research and is interested in the ability of these microorganisms to undergo antigenic variation and modulate the host immune response.

Suhas G. Kallapur received his bachelor in medicine (M.B.B.S.) and a doctorate in medicine (M.D.) from Bombay University, India. He then completed a residency in pediatrics at Wayne State University, Michigan, USA, followed by a fellowship in neonatal-perinatal medicine at Cincinnati Children's Hospital, Ohio, USA. He is currently a tenured Professor of Pediatrics at Cincinnati Children's Hospital, University of Cincinnati, and is a practicing neonatologist. Dr. Kallapur leads a laboratory, funded by NIH, the March of Dimes, and the Burroughs Wellcome Trust, whose main thrust since 2000 is to understand the pathogenesis of infection- or inflammation-mediated preterm birth. This condition is an important contributor to prematurity, which is a leading cause of infant mortality and morbidity worldwide. Ureaplasma species most commonly cause perinatal infections, and Dr. Kallapur has collaborated with coauthors and others to create sheep and rhesus macaque models of intrauterine infection and inflammation.

Christine L. Knox obtained her Ph.D. in 1998 from the Queensland University of Technology (QUT), where she pioneered the study at QUT of the Ureaplasma species and their role in adverse pregnancy outcomes. As an Associate Professor, she now leads the Reproductive Health Research Group at QUT and was the principal Ph.D. supervisor for Samantha Dando and Emma Sweeney, the joint first authors of this review. Funding from the National Institute of Health and the National Health and Medical Research Council, Australia, has enabled this group to further investigate the pathogenesis of Ureaplasma spp. in pregnant women delivering late preterm and at term and in an ovine model of intra-amniotic infection. Dr. Knox is an appointed member of the International Subcommittee for the Taxonomy of Mollicutes, and in 2016 she was the chair of the local organizing committee of the 21st Congress of the International Organization for Mycoplasmology.
REFERENCES
- 1.Hillier SL, Martius J, Krohn M, Kiviat N, Holmes KK, Eschenbach DA. 1988. A case-control study of chorioamnionic infection and histologic chorioamnionitis in prematurity. N Engl J Med 319:972–978. doi: 10.1056/NEJM198810133191503. [DOI] [PubMed] [Google Scholar]
- 2.Romero R, Miranda J, Kusanovic JP, Chaiworapongsa T, Chaemsaithong P, Martinez A, Gotsch F, Dong Z, Ahmed AI, Shaman M, Lannaman K, Yoon BH, Hassan SS, Kim CJ, Korzeniewski SJ, Yeo L, Kim YM. 2015. Clinical chorioamnionitis at term I: microbiology of the amniotic cavity using cultivation and molecular techniques. J Perinat Med 43:19–36. doi: 10.1515/jpm-2014-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romero R, Chaemsaithong P, Docheva N, Korzeniewski SJ, Kusanovic JP, Yoon BH, Kim JS, Chaiyasit N, Ahmed AI, Qureshi F, Jacques SM, Kim CJ, Hassan SS, Chaiworapongsa T, Yeo L, Kim YM. 2016. Clinical chorioamnionitis at term VI: acute chorioamnionitis and funisitis according to the presence or absence of microorganisms and inflammation in the amniotic cavity. J Perinat Med 44:33–51. doi: 10.1515/jpm-2015-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts DJ, Celi AC, Riley LE, Onderdonk AB, Boyd TK, Johnson LC, Lieberman E. 2012. Acute histologic chorioamnionitis at term: nearly always noninfectious. PLoS One 7:e31819. doi: 10.1371/journal.pone.0031819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tita AT, Andrews WW. 2010. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol 37:339–354. doi: 10.1016/j.clp.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horvath B, Lakatos F, Toth C, Bodecs T, Bodis J. 2014. Silent chorioamnionitis and associated pregnancy outcomes: a review of clinical data gathered over a 16-year period. J Perinat Med 42:441–447. doi: 10.1515/jpm-2013-0186. [DOI] [PubMed] [Google Scholar]
- 7.Redline RW, Faye-Petersen O, Heller D, Qureshi F, Savell V, Vogler C. 2003. Amniotic infection syndrome: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol 6:435–448. doi: 10.1007/s10024-003-7070-y. [DOI] [PubMed] [Google Scholar]
- 8.Kim CJ, Romero R, Kusanovic JP, Yoo W, Dong Z, Topping V, Gotsch F, Yoon BH, Chi JG, Kim JS. 2010. The frequency, clinical significance, and pathological features of chronic chorioamnionitis: a lesion associated with spontaneous preterm birth. Mod Pathol 23:1000–1011. doi: 10.1038/modpathol.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim YM. 2015. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol 213:S29–52. doi: 10.1016/j.ajog.2015.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, Silver RM, Raju TN. 2016. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol 127:426–436. doi: 10.1097/AOG.0000000000001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benirschke K, Burton GJ, Baergen RN. 2012. Anatomy and pathology of the placental membranes, p 249–307. In Benirschke K, Burton GJ, Baergen RN (ed), Pathology of the human placenta, 6th ed Springer, Heidelberg, Germany. [Google Scholar]
- 12.Calvin SE, Oyen ML. 2007. Microstructure and mechanics of the chorioamnion membrane with an emphasis on fracture properties. Ann N Y Acad Sci 1101:166–185. doi: 10.1196/annals.1389.009. [DOI] [PubMed] [Google Scholar]
- 13.Bourne GL. 1966. The anatomy of the human amnion and chorion. Proc R Soc Med 59:1127–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niknejad H, Yazdanpanah G, Ahmadiani A. 2016. Induction of apoptosis, stimulation of cell-cycle arrest and inhibition of angiogenesis make human amnion-derived cells promising sources for cell therapy of cancer. Cell Tissue Res 363:599–608. doi: 10.1007/s00441-016-2364-3. [DOI] [PubMed] [Google Scholar]
- 15.Chaemsaithong P, Romero R, Korzeniewski SJ, Martinez-Varea A, Dong Z, Yoon BH, Hassan SS, Chaiworapongsa T, Yeo L. 2016. A point of care test for interleukin-6 in amniotic fluid in preterm prelabor rupture of membranes: a step toward the early treatment of acute intra-amniotic inflammation/infection. J Matern Fetal Neonatal Med 29:360–367. doi: 10.3109/14767058.2015.1006621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kacerovsky M, Musilova I, Hornychova H, Kutova R, Pliskova L, Kostal M, Jacobsson B. 2014. Bedside assessment of amniotic fluid interleukin-6 in preterm prelabor rupture of membranes. Am J Obstet Gynecol 211:385.e1–385.e9. doi: 10.1016/j.ajog.2014.03.069. [DOI] [PubMed] [Google Scholar]
- 17.Romero R, Kadar N, Miranda J, Korzeniewski SJ, Schwartz AG, Chaemsaithong P, Rogers W, Soto E, Gotsch F, Yeo L, Hassan SS, Chaiworapongsa T. 2014. The diagnostic performance of the Mass Restricted (MR) score in the identification of microbial invasion of the amniotic cavity or intra-amniotic inflammation is not superior to amniotic fluid interleukin-6. J Matern Fetal Neonatal Med 27:757–769. doi: 10.3109/14767058.2013.844123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim KW, Romero R, Park HS, Park CW, Shim SS, Jun JK, Yoon BH. 2007. A rapid matrix metalloproteinase-8 bedside test for the detection of intraamniotic inflammation in women with preterm premature rupture of membranes. Am J Obstet Gynecol 197:292.e1–292.e5. [DOI] [PubMed] [Google Scholar]
- 19.Romero R, Chaemsaithong P, Korzeniewski SJ, Tarca AL, Bhatti G, Xu Z, Kusanovic JP, Dong Z, Docheva N, Martinez-Varea A, Yoon BH, Hassan SS, Chaiworapongsa T, Yeo L. 2016. Clinical chorioamnionitis at term II: the intra-amniotic inflammatory response. J Perinat Med 44:5–22. doi: 10.1515/jpm-2015-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim SM, Romero R, Park JW, Oh KJ, Jun JK, Yoon BH. 2015. The relationship between the intensity of intra-amniotic inflammation and the presence and severity of acute histologic chorioamnionitis in preterm gestation. J Matern Fetal Neonatal Med 28:1500–1509. doi: 10.3109/14767058.2014.961009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobsson B, Holst RM, Andersson B, Hagberg H. 2005. Monocyte chemotactic protein-2 and -3 in amniotic fluid: relationship to microbial invasion of the amniotic cavity, intra-amniotic inflammation and preterm delivery. Acta Obstet Gynecol Scand 84:566–571. doi: 10.1111/j.0001-6349.2005.00830.x. [DOI] [PubMed] [Google Scholar]
- 22.Oh KJ, Park KH, Kim SN, Jeong EH, Lee SY, Yoon HY. 2011. Predictive value of intra-amniotic and serum markers for inflammatory lesions of preterm placenta. Placenta 32:732–736. doi: 10.1016/j.placenta.2011.07.080. [DOI] [PubMed] [Google Scholar]
- 23.Bhat G, Peltier MR, Syed TA, Drobek CO, Saade G, Menon R. 2013. Fetal membrane biomarker network diversity and disease functions induced by intra-amniotic pathogens. Am J Reprod Immunol 69:124–133. doi: 10.1111/aji.12047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gervasi MT, Romero R, Bracalente G, Erez O, Dong Z, Hassan SS, Yeo L, Yoon BH, Chaiworapongsa T. 2012. Midtrimester amniotic fluid concentrations of interleukin-6 and interferon-gamma-inducible protein-10: evidence for heterogeneity of intra-amniotic inflammation and associations with spontaneous early (<32 weeks) and late (>32 weeks) preterm delivery. J Perinat Med 40:329–343. doi: 10.1515/jpm-2012-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y, Liu Y, Du C, Zhang R, Feng Z, Zhang J. 2016. Diagnostic value of amniotic fluid inflammatory biomarkers for subclinical chorioamnionitis. Int J Gynaecol Obstet 134:160–164. doi: 10.1016/j.ijgo.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Myntti T, Rahkonen L, Tikkanen M, Patari-Sampo A, Paavonen J, Stefanovic V. 2016. Amniotic fluid rapid biomarkers are associated with intra-amniotic infection in preterm pregnancies regardless of the membrane status. J Perinatol 36:606–611. doi: 10.1038/jp.2016.59. [DOI] [PubMed] [Google Scholar]
- 27.Malloy MH. 2014. Chorioamnionitis: epidemiology of newborn management and outcome United States 2008. J Perinatol 34:611–615. doi: 10.1038/jp.2014.81. [DOI] [PubMed] [Google Scholar]
- 28.Mi Lee S, Romero R, Lee KA, Jin Yang H, Joon Oh K, Park CW, Yoon BH. 2011. The frequency and risk factors of funisitis and histologic chorioamnionitis in pregnant women at term who delivered after the spontaneous onset of labor. J Matern Fetal Neonatal Med 24:37–42. doi: 10.3109/14767058.2010.482622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Russell P. 1979. Inflammatory lesions of the human placenta: clinical significance of acute chorioamnionitis. Am J Diagn Gynecol Obstet 2:127–137. [Google Scholar]
- 30.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sanchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID III, Watterberg KL, Saha S, Das A, Higgins RD. 2010. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126:443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mueller-Heubach E, Rubinstein DN, Schwarz SS. 1990. Histologic chorioamnionitis and preterm delivery in different patient populations. Obstet Gynecol 75:622–626. [PubMed] [Google Scholar]
- 32.Torricelli M, Voltolini C, Toti P, Vellucci FL, Conti N, Cannoni A, Moncini I, Occhini R, Severi FM, Petraglia F. 2014. Histologic chorioamnionitis: different histologic features at different gestational ages. J Matern Fetal Neonatal Med 27:910–913. doi: 10.3109/14767058.2013.846313. [DOI] [PubMed] [Google Scholar]
- 33.Seong HS, Lee SE, Kang JH, Romero R, Yoon BH. 2008. The frequency of microbial invasion of the amniotic cavity and histologic chorioamnionitis in women at term with intact membranes in the presence or absence of labor. Am J Obstet Gynecol 199:375.e1–375.e5. doi: 10.1016/j.ajog.2008.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park HS, Romero R, Lee SM, Park CW, Jun JK, Yoon BH. 2010. Histologic chorioamnionitis is more common after spontaneous labor than after induced labor at term. Placenta 31:792–795. doi: 10.1016/j.placenta.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. 2014. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol 124:57–67. doi: 10.1097/AOG.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rickert VI, Wiemann CM, Hankins GD, McKee JM, Berenson AB. 1998. Prevalence and risk factors of chorioamnionitis among adolescents. Obstet Gynecol 92:254–257. doi: 10.1016/S0029-7844(98)00135-5. [DOI] [PubMed] [Google Scholar]
- 37.Seaward PG, Hannah ME, Myhr TL, Farine D, Ohlsson A, Wang EE, Haque K, Weston JA, Hewson SA, Ohel G, Hodnett ED. 1997. International Multicentre Term Prelabor Rupture of Membranes Study: evaluation of predictors of clinical chorioamnionitis and postpartum fever in patients with prelabor rupture of membranes at term. Am J Obstet Gynecol 177:1024–1029. doi: 10.1016/S0002-9378(97)70007-3. [DOI] [PubMed] [Google Scholar]
- 38.Denney JM, Culhane JF. 2009. Bacterial vaginosis: a problematic infection from both a perinatal and neonatal perspective. Semin Fetal Neonatal Med 14:200–203. doi: 10.1016/j.siny.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 39.Anderson BL, Simhan HN, Simons KM, Wiesenfeld HC. 2007. Untreated asymptomatic group B streptococcal bacteriuria early in pregnancy and chorioamnionitis at delivery. Am J Obstet Gynecol 196:524.e1–524.e5. [DOI] [PubMed] [Google Scholar]
- 40.Howson CP, Kinney MV, McDougall L, Lawn JE. 2013. Born too soon: preterm birth matters. Reprod Health 10(Suppl 1):S1. doi: 10.1186/1742-4755-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE. 2012. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 42.Goldenberg RL, Hauth JC, Andrews WW. 2000. Intrauterine infection and preterm delivery. N Engl J Med 342:1500–1507. doi: 10.1056/NEJM200005183422007. [DOI] [PubMed] [Google Scholar]
- 43.Goland RS, Wardlaw SL, Blum M, Tropper PJ, Stark RI. 1988. Biologically active corticotropin-releasing hormone in maternal and fetal plasma during pregnancy. Am J Obstet Gynecol 159:884–890. doi: 10.1016/S0002-9378(88)80162-5. [DOI] [PubMed] [Google Scholar]
- 44.Smith R. 2007. Parturition. N Engl J Med 356:271–283. doi: 10.1056/NEJMra061360. [DOI] [PubMed] [Google Scholar]
- 45.Johnson RF, Mitchell CM, Clifton V, Zakar T. 2004. Regulation of 15-hydroxyprostaglandin dehydrogenase (PGDH) gene activity, messenger ribonucleic acid processing, and protein abundance in the human chorion in late gestation and labor. J Clin Endocrinol Metab 89:5639–5648. doi: 10.1210/jc.2004-0540. [DOI] [PubMed] [Google Scholar]
- 46.Phillips RJ, Al-Zamil H, Hunt LP, Fortier MA, Lopez Bernal A. 2011. Genes for prostaglandin synthesis, transport and inactivation are differentially expressed in human uterine tissues, and the prostaglandin F synthase AKR1B1 is induced in myometrial cells by inflammatory cytokines. Mol Hum Reprod 17:1–13. doi: 10.1093/molehr/gaq057. [DOI] [PubMed] [Google Scholar]
- 47.Li W, Challis JR. 2005. Corticotropin-releasing hormone and urocortin induce secretion of matrix metalloproteinase-9 (MMP-9) without change in tissue inhibitors of MMP-1 by cultured cells from human placenta and fetal membranes. J Clin Endocrinol Metab 90:6569–6574. doi: 10.1210/jc.2005-1445. [DOI] [PubMed] [Google Scholar]
- 48.Ulug U, Goldman S, Ben-Shlomo I, Shalev E. 2001. Matrix metalloproteinase (MMP)-2 and MMP-9 and their inhibitor, TIMP-1, in human term decidua and fetal membranes: the effect of prostaglandin F(2alpha) and indomethacin. Mol Hum Reprod 7:1187–1193. doi: 10.1093/molehr/7.12.1187. [DOI] [PubMed] [Google Scholar]
- 49.Xie N, Liu L, Li Y, Yu C, Lam S, Shynlova O, Gleave M, Challis JR, Lye S, Dong X. 2012. Expression and function of myometrial PSF suggest a role in progesterone withdrawal and the initiation of labor. Mol Endocrinol 26:1370–1379. doi: 10.1210/me.2012-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nadeem L, Shynlova O, Matysiak-Zablocki E, Mesiano S, Dong X, Lye S. 2016. Molecular evidence of functional progesterone withdrawal in human myometrium. Nat Commun 7:11565. doi: 10.1038/ncomms11565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maiti K, Paul JW, Read M, Chan EC, Riley SC, Nahar P, Smith R. 2011. G-1-activated membrane estrogen receptors mediate increased contractility of the human myometrium. Endocrinology 152:2448–2455. doi: 10.1210/en.2010-0979. [DOI] [PubMed] [Google Scholar]
- 52.Waring GJ, Robson SC, Bulmer JN, Tyson-Capper AJ. 2015. Inflammatory signalling in fetal membranes: increased expression levels of TLR 1 in the presence of preterm histological chorioamnionitis. PLoS One 10:e0124298. doi: 10.1371/journal.pone.0124298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moço NP, Martin LF, Pereira AC, Polettini J, Peracoli JC, Coelho KI, da Silva MG. 2013. Gene expression and protein localization of TLR-1, -2, -4 and -6 in amniochorion membranes of pregnancies complicated by histologic chorioamnionitis. Eur J Obstet Gynecol Reprod Biol 171:12–17. doi: 10.1016/j.ejogrb.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 54.Kim YM, Romero R, Chaiworapongsa T, Kim GJ, Kim MR, Kuivaniemi H, Tromp G, Espinoza J, Bujold E, Abrahams VM, Mor G. 2004. Toll-like receptor-2 and -4 in the chorioamniotic membranes in spontaneous labor at term and in preterm parturition that are associated with chorioamnionitis. Am J Obstet Gynecol 191:1346–1355. doi: 10.1016/j.ajog.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 55.Holmlund U, Cebers G, Dahlfors AR, Sandstedt B, Bremme K, Ekstrom ES, Scheynius A. 2002. Expression and regulation of the pattern recognition receptors Toll-like receptor-2 and Toll-like receptor-4 in the human placenta. Immunology 107:145–151. doi: 10.1046/j.1365-2567.2002.01491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Allam AB, von Chamier M, Brown MB, Reyes L. 2014. Immune profiling of BALB/C and C57BL/6 mice reveals a correlation between Ureaplasma parvum-induced fetal inflammatory response syndrome-like pathology and increased placental expression of TLR2 and CD14. Am J Reprod Immunol 71:241–251. doi: 10.1111/aji.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gillaux C, Mehats C, Vaiman D, Cabrol D, Breuiller-Fouche M. 2011. Functional screening of TLRs in human amniotic epithelial cells. J Immunol 187:2766–2774. doi: 10.4049/jimmunol.1100217. [DOI] [PubMed] [Google Scholar]
- 58.Marconi C, de Andrade Ramos BR, Peracoli JC, Donders GG, da Silva MG. 2011. Amniotic fluid interleukin-1 beta and interleukin-6, but not interleukin-8 correlate with microbial invasion of the amniotic cavity in preterm labor. Am J Reprod Immunol 65:549–556. doi: 10.1111/j.1600-0897.2010.00940.x. [DOI] [PubMed] [Google Scholar]
- 59.Dando SJ, Nitsos I, Kallapur SG, Newnham JP, Polglase GR, Pillow JJ, Jobe AH, Timms P, Knox CL. 2012. The role of the multiple banded antigen of Ureaplasma parvum in intra-amniotic infection: major virulence factor or decoy? PLoS One 7:e29856. doi: 10.1371/journal.pone.0029856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yoon BH, Romero R, Park JS, Chang JW, Kim YA, Kim JC, Kim KS. 1998. Microbial invasion of the amniotic cavity with Ureaplasma urealyticum is associated with a robust host response in fetal, amniotic, and maternal compartments. Am J Obstet Gynecol 179:1254–1260. doi: 10.1016/S0002-9378(98)70142-5. [DOI] [PubMed] [Google Scholar]
- 61.Holst RM, Laurini R, Jacobsson B, Samuelsson E, Savman K, Doverhag C, Wennerholm UB, Hagberg H. 2007. Expression of cytokines and chemokines in cervical and amniotic fluid: relationship to histological chorioamnionitis. J Matern Fetal Neonatal Med 20:885–893. doi: 10.1080/14767050701752601. [DOI] [PubMed] [Google Scholar]
- 62.Sweeney EL, Kallapur SG, Gisslen T, Lambers DS, Chougnet CA, Stephenson SA, Jobe AH, Knox CL. 2016. Placental infection with Ureaplasma species is associated with histologic chorioamnionitis and adverse outcomes in moderately preterm and late-preterm infants. J Infect Dis 213:1340–1347. doi: 10.1093/infdis/jiv587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Romero R, Mazor M, Wu YK, Avila C, Oyarzun E, Mitchell MD. 1989. Bacterial endotoxin and tumor necrosis factor stimulate prostaglandin production by human decidua. Prostaglandins Leukot Essent Fatty Acids 37:183–186. doi: 10.1016/0952-3278(89)90083-5. [DOI] [PubMed] [Google Scholar]
- 64.Norwitz ER, Lopez Bernal A, Starkey PM. 1992. Tumor necrosis factor-alpha selectively stimulates prostaglandin F2 alpha production by macrophages in human term decidua. Am J Obstet Gynecol 167:815–820. doi: 10.1016/S0002-9378(11)91595-6. [DOI] [PubMed] [Google Scholar]
- 65.Sadowsky DW, Adams KM, Gravett MG, Witkin SS, Novy MJ. 2006. Preterm labor is induced by intraamniotic infusions of interleukin-1beta and tumor necrosis factor-alpha but not by interleukin-6 or interleukin-8 in a nonhuman primate model. Am J Obstet Gynecol 195:1578–1589. doi: 10.1016/j.ajog.2006.06.072. [DOI] [PubMed] [Google Scholar]
- 66.Maymon E, Romero R, Pacora P, Gomez R, Athayde N, Edwin S, Yoon BH. 2000. Human neutrophil collagenase (matrix metalloproteinase 8) in parturition, premature rupture of the membranes, and intrauterine infection. Am J Obstet Gynecol 183:94–99. doi: 10.1067/mob.2000.105344. [DOI] [PubMed] [Google Scholar]
- 67.Park JY, Romero R, Lee J, Chaemsaithong P, Chaiyasit N, Yoon BH. 2016. An elevated amniotic fluid prostaglandin F2alpha concentration is associated with intra-amniotic inflammation/infection, and clinical and histologic chorioamnionitis, as well as impending preterm delivery in patients with preterm labor and intact membranes. J Matern Fetal Neonatal Med 29:2563–2572. doi: 10.3109/14767058.2015.1094794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schmidt AF, Kannan PS, Kemp MW, Kramer BW, Newnham JP, Jobe AH, Kallapur SG. 2014. Intra-amniotic LPS modulates expression of antimicrobial peptides in the fetal sheep lung. Pediatr Res 76:441–447. doi: 10.1038/pr.2014.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Collins JJ, Kuypers E, Nitsos I, Pillow JJ, Polglase GR, Kemp MW, Newnham JP, Cleutjens JP, Frints SG, Kallapur SG, Jobe AH, Kramer BW. 2012. LPS-induced chorioamnionitis and antenatal corticosteroids modulate Shh signaling in the ovine fetal lung. Am J Physiol Lung Cell Mol Physiol 303:L778–L787. doi: 10.1152/ajplung.00280.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wolfs TG, Kramer BW, Thuijls G, Kemp MW, Saito M, Willems MG, Senthamarai-Kannan P, Newnham JP, Jobe AH, Kallapur SG. 2014. Chorioamnionitis-induced fetal gut injury is mediated by direct gut exposure of inflammatory mediators or by lung inflammation. Am J Physiol Gastrointest Liver Physiol 306:G382–G393. doi: 10.1152/ajpgi.00260.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nikiforou M, Kemp MW, van Gorp RH, Saito M, Newnham JP, Reynaert NL, Janssen LE, Jobe AH, Kallapur SG, Kramer BW, Wolfs TG. 2016. Selective IL-1alpha exposure to the fetal gut, lung, and chorioamnion/skin causes intestinal inflammatory and developmental changes in fetal sheep. Lab Invest 96:69–80. doi: 10.1038/labinvest.2015.127. [DOI] [PubMed] [Google Scholar]
- 72.Zhang L, Saito M, Jobe A, Kallapur SG, Newnham JP, Cox T, Kramer B, Yang H, Kemp MW. 2012. Intra-amniotic administration of E. coli lipopolysaccharides causes sustained inflammation of the fetal skin in sheep. Reprod Sci 19:1181–1189. doi: 10.1177/1933719112446079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Howman RA, Charles AK, Jacques A, Doherty DA, Simmer K, Strunk T, Richmond PC, Cole CH, Burgner DP. 2012. Inflammatory and haematological markers in the maternal, umbilical cord and infant circulation in histological chorioamnionitis. PLoS One 7:e51836. doi: 10.1371/journal.pone.0051836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zanardo V, Peruzzetto C, Trevisanuto D, Cavallin F, Vedovato S, Straface G, Chiarelli S. 2012. Relationship between the neonatal white blood cell count and histologic chorioamnionitis in preterm newborns. J Matern Fetal Neonatal Med 25:2769–2772. doi: 10.3109/14767058.2012.712562. [DOI] [PubMed] [Google Scholar]
- 75.Rueda CM, Wells CB, Gisslen T, Jobe AH, Kallapur SG, Chougnet CA. 2015. Effect of chorioamnionitis on regulatory T cells in moderate/late preterm neonates. Hum Immunol 76:65–73. doi: 10.1016/j.humimm.2014.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Melville JM, Bischof RJ, Meeusen EN, Westover AJ, Moss TJ. 2012. Changes in fetal thymic immune cell populations in a sheep model of intrauterine inflammation. Reprod Sci 19:740–747. doi: 10.1177/1933719111432873. [DOI] [PubMed] [Google Scholar]
- 77.Kuypers E, Willems MG, Jellema RK, Kemp MW, Newnham JP, Delhaas T, Kallapur SG, Jobe AH, Wolfs TG, Kramer BW. 2015. Responses of the spleen to intraamniotic lipopolysaccharide exposure in fetal sheep. Pediatr Res 77:29–35. doi: 10.1038/pr.2014.152. [DOI] [PubMed] [Google Scholar]
- 78.Collins JJ, Kallapur SG, Knox CL, Nitsos I, Polglase GR, Pillow JJ, Kuypers E, Newnham JP, Jobe AH, Kramer BW. 2010. Inflammation in fetal sheep from intra-amniotic injection of Ureaplasma parvum. Am J Physiol Lung Cell Mol Physiol 299:L852–L860. doi: 10.1152/ajplung.00183.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Strackx E, Sparnaaij MA, Vlassaks E, Jellema R, Kuypers E, Vles JS, Kramer BW, Gavilanes AW. 2015. Lipopolysaccharide-induced chorioamnionitis causes acute inflammatory changes in the ovine central nervous system. CNS Neurol Disord Drug Targets 14:77–84. doi: 10.2174/1871527314666150116120029. [DOI] [PubMed] [Google Scholar]
- 80.Kuypers E, Jellema RK, Ophelders DR, Dudink J, Nikiforou M, Wolfs TG, Nitsos I, Pillow JJ, Polglase GR, Kemp MW, Saito M, Newnham JP, Jobe AH, Kallapur SG, Kramer BW. 2013. Effects of intra-amniotic lipopolysaccharide and maternal betamethasone on brain inflammation in fetal sheep. PLoS One 8:e81644. doi: 10.1371/journal.pone.0081644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Madsen-Bouterse SA, Romero R, Tarca AL, Kusanovic JP, Espinoza J, Kim CJ, Kim JS, Edwin SS, Gomez R, Draghici S. 2010. The transcriptome of the fetal inflammatory response syndrome. Am J Reprod Immunol 63:73–92. doi: 10.1111/j.1600-0897.2009.00791.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. 1998. The fetal inflammatory response syndrome. Am J Obstet Gynecol 179:194–202. doi: 10.1016/S0002-9378(98)70272-8. [DOI] [PubMed] [Google Scholar]
- 83.Romero R, Savasan ZA, Chaiworapongsa T, Berry SM, Kusanovic JP, Hassan SS, Yoon BH, Edwin S, Mazor M. 2011. Hematologic profile of the fetus with systemic inflammatory response syndrome. J Perinat Med 40:19–32. doi: 10.1515/JPM.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kallapur SG, Presicce P, Rueda CM, Jobe AH, Chougnet CA. 2014. Fetal immune response to chorioamnionitis. Semin Reprod Med 32:56–67. doi: 10.1055/s-0033-1361823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gantert M, Been JV, Gavilanes AW, Garnier Y, Zimmermann LJ, Kramer BW. 2010. Chorioamnionitis: a multiorgan disease of the fetus? J Perinatol 30(Suppl):S21–S30. doi: 10.1038/jp.2010.96. [DOI] [PubMed] [Google Scholar]
- 86.Arayici S, Kadioglu Simsek G, Oncel MY, Eras Z, Canpolat FE, Oguz SS, Uras N, Zergeroglu S, Dilmen U. 2014. The effect of histological chorioamnionitis on the short-term outcome of preterm infants ≤32 weeks: a single-center study. J Matern Fetal Neonatal Med 27:1129–1133. doi: 10.3109/14767058.2013.850668. [DOI] [PubMed] [Google Scholar]
- 87.Arora P, Bagga R, Kalra J, Kumar P, Radhika S, Gautam V. 2015. Mean gestation at delivery and histological chorioamnionitis correlates with early-onset neonatal sepsis following expectant management in pPROM. J Obstet Gynaecol 35:235–240. doi: 10.3109/01443615.2014.958143. [DOI] [PubMed] [Google Scholar]
- 88.Stimac M, Juretic E, Vukelic V, Matasic NP, Kos M, Babic D. 2014. Effect of chorioamnionitis on mortality, early onset neonatal sepsis and bronchopulmonary dysplasia in preterm neonates with birth weight of <1,500 grams. Coll Antropol 38:167–171. [PubMed] [Google Scholar]
- 89.Moscuzza F, Belcari F, Nardini V, Bartoli A, Domenici C, Cuttano A, Ghirri P, Boldrini A. 2011. Correlation between placental histopathology and fetal/neonatal outcome: chorioamnionitis and funisitis are associated to intraventricular haemorrage and retinopathy of prematurity in preterm newborns. Gynecol Endocrinol 27:319–323. doi: 10.3109/09513590.2010.487619. [DOI] [PubMed] [Google Scholar]
- 90.Mestan K, Yu Y, Matoba N, Cerda S, Demmin B, Pearson C, Ortiz K, Wang X. 2010. Placental inflammatory response is associated with poor neonatal growth: preterm birth cohort study. Pediatrics 125:e891–e898. doi: 10.1542/peds.2009-0313. [DOI] [PubMed] [Google Scholar]
- 91.Lu HY, Zhang Q, Wang QX, Lu JY. 2016. Contribution of histologic chorioamnionitis and fetal inflammatory response syndrome to increased risk of brain injury in infants with preterm premature rupture of membranes. Pediatr Neurol 61:94–98.e1. doi: 10.1016/j.pediatrneurol.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 92.Korzeniewski SJ, Romero R, Cortez J, Pappas A, Schwartz AG, Kim CJ, Kim JS, Kim YM, Yoon BH, Chaiworapongsa T, Hassan SS. 2014. A “multi-hit” model of neonatal white matter injury: cumulative contributions of chronic placental inflammation, acute fetal inflammation and postnatal inflammatory events. J Perinat Med 42:731–743. doi: 10.1515/jpm-2014-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Perrone S, Toti P, Toti MS, Badii S, Becucci E, Gatti MG, Marzocchi B, Picardi A, Buonocore G. 2012. Perinatal outcome and placental histological characteristics: a single-center study. J Matern Fetal Neonatal Med 25(Suppl 1):110–113. doi: 10.3109/14767058.2012.664344. [DOI] [PubMed] [Google Scholar]
- 94.Eriksson L, Haglund B, Odlind V, Altman M, Kieler H. 2014. Prenatal inflammatory risk factors for development of bronchopulmonary dysplasia. Pediatr Pulmonol 49:665–672. doi: 10.1002/ppul.22881. [DOI] [PubMed] [Google Scholar]
- 95.Hartling L, Liang Y, Lacaze-Masmonteil T. 2012. Chorioamnionitis as a risk factor for bronchopulmonary dysplasia: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 97:F8–F17. doi: 10.1136/adc.2010.210187. [DOI] [PubMed] [Google Scholar]
- 96.Park HW, Choi YS, Kim KS, Kim SN. 2015. Chorioamnionitis and patent ductus arteriosus: a systematic review and meta-analysis. PLoS One 10:e0138114. doi: 10.1371/journal.pone.0138114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chen ML, Allred EN, Hecht JL, Onderdonk A, VanderVeen D, Wallace DK, Leviton A, Dammann O. 2011. Placenta microbiology and histology and the risk for severe retinopathy of prematurity. Invest Ophthalmol Vis Sci 52:7052–7058. doi: 10.1167/iovs.11-7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Woo SJ, Park KH, Jung HJ, Kim S, Choe G, Ahn J, Park KH. 2012. Effects of maternal and placental inflammation on retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 250:915–923. doi: 10.1007/s00417-011-1648-2. [DOI] [PubMed] [Google Scholar]
- 99.Romero R, Espinoza J, Goncalves LF, Gomez R, Medina L, Silva M, Chaiworapongsa T, Yoon BH, Ghezzi F, Lee W, Treadwell M, Berry SM, Maymon E, Mazor M, DeVore G. 2004. Fetal cardiac dysfunction in preterm premature rupture of membranes. J Matern Fetal Neonatal Med 16:146–157. doi: 10.1080/14767050400009279. [DOI] [PubMed] [Google Scholar]
- 100.Yanowitz TD, Jordan JA, Gilmour CH, Towbin R, Bowen A, Roberts JM, Brozanski BS. 2002. Hemodynamic disturbances in premature infants born after chorioamnionitis: association with cord blood cytokine concentrations. Pediatr Res 51:310–316. doi: 10.1203/00006450-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 101.Moore SW, Arnold M, Wright C. 2013. Necrotizing enterocolitis and the placenta—a key etiological link. J Pediatr Surg 48:359–362. doi: 10.1016/j.jpedsurg.2012.11.020. [DOI] [PubMed] [Google Scholar]
- 102.Been JV, Lievense S, Zimmermann LJ, Kramer BW, Wolfs TG. 2013. Chorioamnionitis as a risk factor for necrotizing enterocolitis: a systematic review and meta-analysis. J Pediatr 162:236–242.e232. doi: 10.1016/j.jpeds.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 103.Kim YM, Romero R, Chaiworapongsa T, Espinoza J, Mor G, Kim CJ. 2006. Dermatitis as a component of the fetal inflammatory response syndrome is associated with activation of Toll-like receptors in epidermal keratinocytes. Histopathology 49:506–514. doi: 10.1111/j.1365-2559.2006.02542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lee Y, Kim HJ, Choi SJ, Oh SY, Kim JS, Roh CR, Kim JH. 2015. Is there a stepwise increase in neonatal morbidities according to histological stage (or grade) of acute chorioamnionitis and funisitis?: effect of gestational age at delivery. J Perinat Med 43:259–267. doi: 10.1515/jpm-2014-0035. [DOI] [PubMed] [Google Scholar]
- 105.Hendson L, Russell L, Robertson CM, Liang Y, Chen Y, Abdalla A, Lacaze-Masmonteil T. 2011. Neonatal and neurodevelopmental outcomes of very low birth weight infants with histologic chorioamnionitis. J Pediatr 158:397–402. doi: 10.1016/j.jpeds.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 106.Gisslen T, Alvarez M, Wells C, Soo MT, Lambers DS, Knox CL, Meinzen-Derr JK, Chougnet CA, Jobe AH, Kallapur SG. 23 March 2016. Fetal inflammation associated with minimal acute morbidity in moderate/late preterm infants. Arch Dis Child Fetal Neonatal Ed doi: 10.1136/archdischild-2015-308518. [DOI] [PubMed] [Google Scholar]
- 107.Pappas A, Kendrick DE, Shankaran S, Stoll BJ, Bell EF, Laptook AR, Walsh MC, Das A, Hale EC, Newman NS, Higgins RD. 2014. Chorioamnionitis and early childhood outcomes among extremely low-gestational-age neonates. JAMA Pediatr 168:137–147. doi: 10.1001/jamapediatrics.2013.4248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Garcia-Munoz Rodrigo F, Galan Henriquez G, Figueras Aloy J, Garcia-Alix Perez A. 2014. Outcomes of very-low-birth-weight infants exposed to maternal clinical chorioamnionitis: a multicentre study. Neonatology 106:229–234. doi: 10.1159/000363127. [DOI] [PubMed] [Google Scholar]
- 109.Botet F, Figueras J, Carbonell-Estrany X, Arca G, The Castrillo Study Group. 2010. Effect of maternal clinical chorioamnionitis on neonatal morbidity in very-low birthweight infants: a case-control study. J Perinat Med 38:269–273. doi: 10.1515/JPM.2010.029. [DOI] [PubMed] [Google Scholar]
- 110.Soraisham AS, Trevenen C, Wood S, Singhal N, Sauve R. 2013. Histological chorioamnionitis and neurodevelopmental outcome in preterm infants. J Perinatol 33:70–75. doi: 10.1038/jp.2012.49. [DOI] [PubMed] [Google Scholar]
- 111.Yamada N, Sato Y, Moriguchi-Goto S, Yamashita A, Kodama Y, Sameshima H, Asada Y. 2015. Histological severity of fetal inflammation is useful in predicting neonatal outcome. Placenta 36:1490–1493. doi: 10.1016/j.placenta.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 112.Sato M, Nishimaki S, Yokota S, Seki K, Horiguchi H, An H, Ishida F, Fujita S, Ao K, Yatake H. 2011. Severity of chorioamnionitis and neonatal outcome. J Obstet Gynaecol Res 37:1313–1319. doi: 10.1111/j.1447-0756.2010.01519.x. [DOI] [PubMed] [Google Scholar]
- 113.King AE, Kelly RW, Sallenave JM, Bocking AD, Challis JR. 2007. Innate immune defences in the human uterus during pregnancy. Placenta 28:1099–1106. doi: 10.1016/j.placenta.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 114.Kjaergaard N, Hein M, Hyttel L, Helmig RB, Schonheyder HC, Uldbjerg N, Madsen H. 2001. Antibacterial properties of human amnion and chorion in vitro. Eur J Obstet Gynecol Reprod Biol 94:224–229. doi: 10.1016/S0301-2115(00)00345-6. [DOI] [PubMed] [Google Scholar]
- 115.Parthasarathy M, Sasikala R, Gunasekaran P, Raja J. 2014. Antimicrobial activity of human amniotic and chorionic membranes. J Acad Ind Res 2:545–547. [Google Scholar]
- 116.Knox CL, Allan JA, Allan JM, Edirisinghe WR, Stenzel D, Lawrence FA, Purdie DM, Timms P. 2003. Ureaplasma parvum and Ureaplasma urealyticum are detected in semen after washing before assisted reproductive technology procedures. Fertil Steril 80:921–929. doi: 10.1016/S0015-0282(03)01125-7. [DOI] [PubMed] [Google Scholar]
- 117.Quinn PA, Li HC, Th'ng C, Dunn M, Butany J. 1993. Serological response to Ureaplasma urealyticum in the neonate. Clin Infect Dis 17(Suppl 1):S136–S143. doi: 10.1093/clinids/17.Supplement_1.S136. [DOI] [PubMed] [Google Scholar]
- 118.Kim MJ, Romero R, Gervasi MT, Kim JS, Yoo W, Lee DC, Mittal P, Erez O, Kusanovic JP, Hassan SS, Kim CJ. 2009. Widespread microbial invasion of the chorioamniotic membranes is a consequence and not a cause of intra-amniotic infection. Lab Invest 89:924–936. doi: 10.1038/labinvest.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. 2014. The placenta harbors a unique microbiome. Sci Transl Med 6:237ra65. doi: 10.1126/scitranslmed.3008599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Prince AL, Ma J, Kannan PS, Alvarez M, Gisslen T, Harris RA, Sweeney EL, Knox CL, Lambers DS, Jobe AH, Chougnet CA, Kallapur SG, Aagaard KM. 2016. The placental membrane microbiome is altered among subjects with spontaneous preterm birth with and without chorioamnionitis. Am J Obstet Gynecol 214:627.e1–627.e16. doi: 10.1016/j.ajog.2016.01.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kallapur SG, Kramer BW, Knox CL, Berry CA, Collins JJ, Kemp MW, Nitsos I, Polglase GR, Robinson J, Hillman NH, Newnham JP, Chougnet C, Jobe AH. 2011. Chronic fetal exposure to Ureaplasma parvum suppresses innate immune responses in sheep. J Immunol 187:2688–2695. doi: 10.4049/jimmunol.1100779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.DiGiulio DB, Romero R, Amogan HP, Kusanovic JP, Bik EM, Gotsch F, Kim CJ, Erez O, Edwin S, Relman DA. 2008. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One 3:e3056. doi: 10.1371/journal.pone.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Knox CL, Cave DG, Farrell DJ, Eastment HT, Timms P. 1997. The role of Ureaplasma urealyticum in adverse pregnancy outcome. Aust N Z J Obstet Gynaecol 37:45–51. doi: 10.1111/j.1479-828X.1997.tb02216.x. [DOI] [PubMed] [Google Scholar]
- 124.Kundsin RB, Leviton A, Allred EN, Poulin SA. 1996. Ureaplasma urealyticum infection of the placenta in pregnancies that ended prematurely. Obstet Gynecol 87:122–127. doi: 10.1016/0029-7844(95)00376-2. [DOI] [PubMed] [Google Scholar]
- 125.Iwatani S, Mizobuchi M, Sofue T, Tanaka S, Sakai H, Yoshimoto S, Nakao H. 2014. Neonatal leukemoid reaction associated with Candida albicans chorioamnionitis. Pediatr Int 56:277–279. doi: 10.1111/ped.12259. [DOI] [PubMed] [Google Scholar]
- 126.Ljubin-Sternak S, Mestrovic T. 2014. Chlamydia trachomatis and genital mycoplasmas: pathogens with an impact on human reproductive health. J Pathog 2014:183167. doi: 10.1155/2014/183167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Montelongo EM, Blue NR, Lee RH. 2015. Placenta accreta in a woman with Escherichia coli chorioamnionitis with intact membranes. Case Rep Obstet Gynecol 2015:121864. doi: 10.1155/2015/121864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rours GI, de Krijger RR, Ott A, Willemse HF, de Groot R, Zimmermann LJ, Kornelisse RF, Verbrugh HA, Verkooijen RP. 2011. Chlamydia trachomatis and placental inflammation in early preterm delivery. Eur J Epidemiol 26:421–428. doi: 10.1007/s10654-011-9569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wenstrom KD, Andrews WW, Bowles NE, Towbin JA, Hauth JC, Goldenberg RL. 1998. Intrauterine viral infection at the time of second trimester genetic amniocentesis. Obstet Gynecol 92:420–424. doi: 10.1016/S0029-7844(98)00210-5. [DOI] [PubMed] [Google Scholar]
- 130.Miller JL, Harman C, Weiner C, Baschat AA. 2009. Perinatal outcomes after second trimester detection of amniotic fluid viral genome in asymptomatic patients. J Perinat Med 37:140–143. doi: 10.1515/JPM.2009.027. [DOI] [PubMed] [Google Scholar]
- 131.Reddy UM, Baschat AA, Zlatnik MG, Towbin JA, Harman CR, Weiner CP. 2005. Detection of viral deoxyribonucleic acid in amniotic fluid: association with fetal malformation and pregnancy abnormalities. Fetal Diagn Ther 20:203–207. doi: 10.1159/000083906. [DOI] [PubMed] [Google Scholar]
- 132.Baschat AA, Towbin J, Bowles NE, Harman CR, Weiner CP. 2003. Prevalence of viral DNA in amniotic fluid of low-risk pregnancies in the second trimester. J Matern Fetal Neonatal Med 13:381–384. doi: 10.1080/jmf.13.6.381.384. [DOI] [PubMed] [Google Scholar]
- 133.Cox C, Saxena N, Watt AP, Gannon C, McKenna JP, Fairley DJ, Sweet D, Shields MD, S LC, Coyle PV. 2016. The common vaginal commensal bacterium Ureaplasma parvum is associated with chorioamnionitis in extreme preterm labor. J Matern Fetal Neonatal Med 29:3646–3651. doi: 10.3109/14767058.2016.1140734. [DOI] [PubMed] [Google Scholar]
- 134.Namba F, Hasegawa T, Nakayama M, Hamanaka T, Yamashita T, Nakahira K, Kimoto A, Nozaki M, Nishihara M, Mimura K, Yamada M, Kitajima H, Suehara N, Yanagihara I. 2010. Placental features of chorioamnionitis colonized with Ureaplasma species in preterm delivery. Pediatr Res 67:166–172. doi: 10.1203/PDR.0b013e3181c6e58e. [DOI] [PubMed] [Google Scholar]
- 135.Egawa T, Morioka I, Morisawa T, Yokoyama N, Nakao H, Ohashi M, Matsuo M. 2007. Ureaplasma urealyticum and Mycoplasma hominis presence in umbilical cord is associated with pathogenesis of funisitis. Kobe J Med Sci 53:241–249. [PubMed] [Google Scholar]
- 136.Park CW, Yoon BH, Park JS, Jun JK. 2013. A fetal and an intra-amniotic inflammatory response is more severe in preterm labor than in preterm PROM in the context of funisitis: unexpected observation in human gestations. PLoS One 8:e62521. doi: 10.1371/journal.pone.0062521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gerber S, Vial Y, Hohlfeld P, Witkin SS. 2003. Detection of Ureaplasma urealyticum in second-trimester amniotic fluid by polymerase chain reaction correlates with subsequent preterm labor and delivery. J Infect Dis 187:518–521. doi: 10.1086/368205. [DOI] [PubMed] [Google Scholar]
- 138.Shepard MC. 1954. The recovery of pleuropneumonia-like organisms from Negro men with and without nongonococcal urethritis. Am J Syph Gonorrhea Vener Dis 38:113–124. [PubMed] [Google Scholar]
- 139.Shepard MC, Lunceford CD, Ford DK, Purcell RH, Taylor-Robinson D, Razin S, Black FT. 1974. Ureaplasma urealyticum gen. nov., sp. nov.: proposed nomenclature for the human T (T-strain) mycoplasmas. Int J Syst Bacteriol 24:160–171. doi: 10.1099/00207713-24-2-160. [DOI] [Google Scholar]
- 140.Smith DG, Russell WC, Ingledew WJ, Thirkell D. 1993. Hydrolysis of urea by Ureaplasma urealyticum generates a transmembrane potential with resultant ATP synthesis. J Bacteriol 175:3253–3258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shepard MC, Lunceford CD. 1976. Differential agar medium (A7) for identification of Ureaplasma urealyticum (human T mycoplasmas) in primary cultures of clinical material. J Clin Microbiol 3:613–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tully JG. 1983. Cloning and filtration techniques for mycoplasmas, p 173–177. In Razin S. (ed), Methods in mycoplasmology, vol 1 Academic Press, Inc, New York, NY. [Google Scholar]
- 143.Shepard MC, Masover GK. 1979. Special features of the ureaplasmas, p 452–494. In Barile MF, Razin S (ed), The mycoplasmas, vol 1 Academic Press, Inc, New York, NY. [Google Scholar]
- 144.Robertson JA, Stemke GW, Davis JW Jr, Harasawa R, Thirkell D, Kong F, Shepard MC, Ford DK. 2002. Proposal of Ureaplasma parvum sp. nov. and emended description of Ureaplasma urealyticum (Shepard et al. 1974) Robertson et al. 2001. Int J Syst Evol Microbiol 52:587–597. doi: 10.1099/00207713-52-2-587. [DOI] [PubMed] [Google Scholar]
- 145.Paralanov V, Lu J, Duffy LB, Crabb DM, Shrivastava S, Methe BA, Inman J, Yooseph S, Xiao L, Cassell GH, Waites KB, Glass JI. 2012. Comparative genome analysis of 19 Ureaplasma urealyticum and Ureaplasma parvum strains. BMC Microbiol 12:88. doi: 10.1186/1471-2180-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Christiansen C, Black FT, Freundt EA. 1981. Hybridization experiments with deoxyribonucleic acid from Ureaplasma urealyticum serovars I to VIII. Int J Syst Bacteriol 31:259–262. doi: 10.1099/00207713-31-3-259. [DOI] [Google Scholar]
- 147.Razin S, Harasawa R, Barile MF. 1983. Cleavage patterns of the mycoplasma chromosome, obtained by using restriction endonucleases, as indicators of genetic relatedness among strains. Int J Syst Bacteriol 33:201–206. doi: 10.1099/00207713-33-2-201. [DOI] [Google Scholar]
- 148.Kong F, James G, Ma Z, Gordon S, Bin W, Gilbert GL. 1999. Phylogenetic analysis of Ureaplasma urealyticum—support for the establishment of a new species, Ureaplasma parvum. Int J Syst Bacteriol 49:1879–1889. doi: 10.1099/00207713-49-4-1879. [DOI] [PubMed] [Google Scholar]
- 149.Teng LJ, Zheng X, Glass JI, Watson HL, Tsai J, Cassell GH. 1994. Ureaplasma urealyticum biovar specificity and diversity are encoded in multiple-banded antigen gene. J Clin Microbiol 32:1464–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang J, Kong Y, Feng Y, Huang J, Song T, Ruan Z, Song J, Jiang Y, Yu Y, Xie X. 2014. Development of a multilocus sequence typing scheme for Ureaplasma. Eur J Clin Microbiol Infect Dis 33:537–544. doi: 10.1007/s10096-013-1981-y. [DOI] [PubMed] [Google Scholar]
- 151.Knox CL, Giffard P, Timms P. 1998. The phylogeny of Ureaplasma urealyticum based on the mba gene fragment. Int J Syst Bacteriol 48:1323–1331. doi: 10.1099/00207713-48-4-1323. [DOI] [PubMed] [Google Scholar]
- 152.Black FT. 1973. Modifications of the growth inhibition test and its application to human T-mycoplasmas. Appl Microbiol 25:528–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Shepard MC, Lunceford CD. 1978. Serological typing of Ureaplasma urealyticum isolates from urethritis patients by an agar growth inhibition method. J Clin Microbiol 8:566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Quinn PA, Arshoff LU, Li HC. 1981. Serotyping of Ureaplasma urealyticum by immunoperoxidase assay. J Clin Microbiol 13:670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Turunen H, Leinikki P, Jansson E. 1982. Serological characterisation of Ureaplasma urealyticum strains by enzyme-linked immunosorbent assay (ELISA). J Clin Pathol 35:439–443. doi: 10.1136/jcp.35.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Echahidi F, Muyldermans G, Lauwers S, Naessens A. 2001. Development of an enzyme-linked immunosorbent assay for serotyping Ureaplasma urealyticum strains using monoclonal antibodies. Clin Diagn Lab Immunol 8:52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Stemke GW, Robertson JA. 1981. Modified colony indirect epifluorescence test for serotyping Ureaplasma urealyticum and an adaptation to detect common antigenic specificity. J Clin Microbiol 14:582–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Knox CL, Timms P. 1998. Comparison of PCR, nested PCR, and random amplified polymorphic DNA PCR for detection and typing of Ureaplasma urealyticum in specimens from pregnant women. J Clin Microbiol 36:3032–3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kong F, Ma Z, James G, Gordon S, Gilbert GL. 2000. Species identification and subtyping of Ureaplasma parvum and Ureaplasma urealyticum using PCR-based assays. J Clin Microbiol 38:1175–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kong F, Ma Z, James G, Gordon S, Gilbert GL. 2000. Molecular genotyping of human Ureaplasma species based on multiple-banded antigen (MBA) gene sequences. Int J Syst Evol Microbiol 50:1921–1929. doi: 10.1099/00207713-50-5-1921. [DOI] [PubMed] [Google Scholar]
- 161.Xiao L, Glass JI, Paralanov V, Yooseph S, Cassell GH, Duffy LB, Waites KB. 2010. Detection and characterization of human Ureaplasma species and serovars by real-time PCR. J Clin Microbiol 48:2715–2723. doi: 10.1128/JCM.01877-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Xiao L, Paralanov V, Glass JI, Duffy LB, Robertson JA, Cassell GH, Chen Y, Waites KB. 2011. Extensive horizontal gene transfer in ureaplasmas from humans questions the utility of serotyping for diagnostic purposes. J Clin Microbiol 49:2818–2826. doi: 10.1128/JCM.00637-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Cassell GH, Waites KB, Watson HL, Crouse DT, Harasawa R. 1993. Ureaplasma urealyticum intrauterine infection: role in prematurity and disease in newborns. Clin Microbiol Rev 6:69–87. doi: 10.1128/CMR.6.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Vancutsem E, Faron G, Foulon W, Naessens A. 2015. Genital tract colonization with Ureaplasma spp. and its association with abnormal vaginal flora. J Med Microbiol 64:654–656. doi: 10.1099/jmm.0.000071. [DOI] [PubMed] [Google Scholar]
- 165.Marovt M, Kese D, Kotar T, Kmet N, Miljkovic J, Soba B, Maticic M. 2015. Ureaplasma parvum and Ureaplasma urealyticum detected with the same frequency among women with and without symptoms of urogenital tract infection. Eur J Clin Microbiol Infect Dis 34:1237–1245. doi: 10.1007/s10096-015-2351-8. [DOI] [PubMed] [Google Scholar]
- 166.Hunjak B, Sabol I, Vojnovic G, Fistonic I, Erceg AB, Persic Z, Grce M. 2014. Ureaplasma urealyticum and Ureaplasma parvum in women of reproductive age. Arch Gynecol Obstet 289:407–412. doi: 10.1007/s00404-013-2980-z. [DOI] [PubMed] [Google Scholar]
- 167.Tibaldi C, Cappello N, Latino MA, Masuelli G, Marini S, Benedetto C. 2009. Vaginal and endocervical microorganisms in symptomatic and asymptomatic non-pregnant females: risk factors and rates of occurrence. Clin Microbiol Infect 15:670–679. doi: 10.1111/j.1469-0691.2009.02842.x. [DOI] [PubMed] [Google Scholar]
- 168.McCormack WM. 1986. Ureaplasma urealyticum: ecologic niche and epidemiologic considerations. Pediatr Infect Dis 5:S232–S233. doi: 10.1097/00006454-198611010-00004. [DOI] [PubMed] [Google Scholar]
- 169.Kaliterna V, Kucisec-Tepes N, Pejkovic L, Zavorovic S, Petrovic S, Barisic Z. 2011. An intrauterine device as a possible cause of change in the microbial flora of the female genital system. J Obstet Gynaecol Res 37:1035–1040. doi: 10.1111/j.1447-0756.2010.01480.x. [DOI] [PubMed] [Google Scholar]
- 170.De Francesco MA, Negrini R, Pinsi G, Peroni L, Manca N. 2009. Detection of Ureaplasma biovars and polymerase chain reaction-based subtyping of Ureaplasma parvum in women with or without symptoms of genital infections. Eur J Clin Microbiol Infect Dis 28:641–646. doi: 10.1007/s10096-008-0687-z. [DOI] [PubMed] [Google Scholar]
- 171.Zdrodowska-Stefanow B, Klosowska WM, Ostaszewska-Puchalska I, Bulhak-Koziol V, Kotowicz B. 2006. Ureaplasma urealyticum and Mycoplasma hominis infection in women with urogenital diseases. Adv Med Sci 51:250–253. [PubMed] [Google Scholar]
- 172.Liu L, Cao G, Zhao Z, Zhao F, Huang Y. 2014. High bacterial loads of Ureaplasma may be associated with non-specific cervicitis. Scand J Infect Dis 46:637–641. doi: 10.3109/00365548.2014.922696. [DOI] [PubMed] [Google Scholar]
- 173.Povlsen K, Thorsen P, Lind I. 2001. Relationship of Ureaplasma urealyticum biovars to the presence or absence of bacterial vaginosis in pregnant women and to the time of delivery. Eur J Clin Microbiol Infect Dis 20:65–67. doi: 10.1007/PL00011237. [DOI] [PubMed] [Google Scholar]
- 174.Plummer DC, Garland SM, Gilbert GL. 1987. Bacteraemia and pelvic infection in women due to Ureaplasma urealyticum and Mycoplasma hominis. Med J Aust 146:135–137. [DOI] [PubMed] [Google Scholar]
- 175.Kelly VN, Garland SM, Gilbert GL. 1987. Isolation of genital mycoplasmas from the blood of neonates and women with pelvic infection using conventional SPS-free blood culture media. Pathology 19:277–280. doi: 10.3109/00313028709066563. [DOI] [PubMed] [Google Scholar]
- 176.Latthe PM, Toozs-Hobson P, Gray J. 2008. Mycoplasma and ureaplasma colonisation in women with lower urinary tract symptoms. J Obstet Gynaecol 28:519–521. doi: 10.1080/01443610802097690. [DOI] [PubMed] [Google Scholar]
- 177.Baka S, Kouskouni E, Antonopoulou S, Sioutis D, Papakonstantinou M, Hassiakos D, Logothetis E, Liapis A. 2009. Prevalence of Ureaplasma urealyticum and Mycoplasma hominis in women with chronic urinary symptoms. Urology 74:62–66. doi: 10.1016/j.urology.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 178.Gilbert GL, Garland SM, Fairley KF, McDowall DM. 1986. Bacteriuria due to ureaplasmas and other fastidious organisms during pregnancy: prevalence and significance. Pediatr Infect Dis 5:S239–S243. doi: 10.1097/00006454-198611010-00007. [DOI] [PubMed] [Google Scholar]
- 179.Kataoka S, Yamada T, Chou K, Nishida R, Morikawa M, Minami M, Yamada H, Sakuragi N, Minakami H. 2006. Association between preterm birth and vaginal colonization by mycoplasmas in early pregnancy. J Clin Microbiol 44:51–55. doi: 10.1128/JCM.44.1.51-55.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gonzalez Bosquet E, Gene A, Ferrer I, Borras M, Lailla JM. 2006. Value of endocervical Ureaplasma species colonization as a marker of preterm delivery. Gynecol Obstet Invest 61:119–123. doi: 10.1159/000089457. [DOI] [PubMed] [Google Scholar]
- 181.Kafetzis DA, Skevaki CL, Skouteri V, Gavrili S, Peppa K, Kostalos C, Petrochilou V, Michalas S. 2004. Maternal genital colonization with Ureaplasma urealyticum promotes preterm delivery: association of the respiratory colonization of premature infants with chronic lung disease and increased mortality. Clin Infect Dis 39:1113–1122. doi: 10.1086/424505. [DOI] [PubMed] [Google Scholar]
- 182.Abele-Horn M, Scholz M, Wolff C, Kolben M. 2000. High-density vaginal Ureaplasma urealyticum colonization as a risk factor for chorioamnionitis and preterm delivery. Acta Obstet Gynecol Scand 79:973–978. doi: 10.1034/j.1600-0412.2000.079011973.x. [DOI] [PubMed] [Google Scholar]
- 183.Kwak DW, Hwang HS, Kwon JY, Park YW, Kim YH. 2014. Co-infection with vaginal Ureaplasma urealyticum and Mycoplasma hominis increases adverse pregnancy outcomes in patients with preterm labor or preterm premature rupture of membranes. J Matern Fetal Neonatal Med 27:333–337. doi: 10.3109/14767058.2013.818124. [DOI] [PubMed] [Google Scholar]
- 184.DiGiulio DB, Callahan BJ, McMurdie PJ, Costello EK, Lyell DJ, Robaczewska A, Sun CL, Goltsman DS, Wong RJ, Shaw G, Stevenson DK, Holmes SP, Relman DA. 2015. Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci U S A 112:11060–11065. doi: 10.1073/pnas.1502875112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Choi SJ, Park SD, Jang IH, Uh Y, Lee A. 2012. The prevalence of vaginal microorganisms in pregnant women with preterm labor and preterm birth. Ann Lab Med 32:194–200. doi: 10.3343/alm.2012.32.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Carey JC, Blackwelder WC, Nugent RP, Matteson MA, Rao AV, Eschenbach DA, Lee ML, Rettig PJ, Regan JA, Geromanos KL, Martin DH, Pastorek JG, Gibbs RS, Lipscomb KA. 1991. Antepartum cultures for Ureaplasma urealyticum are not useful in predicting pregnancy outcome. The Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol 164:728–733. [DOI] [PubMed] [Google Scholar]
- 187.Kwak DW, Cho HY, Kwon JY, Park YW, Kim YH. 2015. Usefulness of maternal serum C-reactive protein with vaginal Ureaplasma urealyticum as a marker for prediction of imminent preterm delivery and chorioamnionitis in patients with preterm labor or preterm premature rupture of membranes. J Perinat Med 43:409–415. doi: 10.1515/jpm-2014-0142. [DOI] [PubMed] [Google Scholar]
- 188.Donders GG, Van Calsteren K, Bellen G, Reybrouck R, Van den Bosch T, Riphagen I, Van Lierde S. 2009. Predictive value for preterm birth of abnormal vaginal flora, bacterial vaginosis and aerobic vaginitis during the first trimester of pregnancy. BJOG 116:1315–1324. doi: 10.1111/j.1471-0528.2009.02237.x. [DOI] [PubMed] [Google Scholar]
- 189.Vogel I, Thorsen P, Hogan VK, Schieve LA, Jacobsson B, Ferre CD. 2006. The joint effect of vaginal Ureaplasma urealyticum and bacterial vaginosis on adverse pregnancy outcomes. Acta Obstet Gynecol Scand 85:778–785. doi: 10.1080/00016340500442423. [DOI] [PubMed] [Google Scholar]
- 190.Lee SE, Romero R, Kim EC, Yoon BH. 2009. A high Nugent score but not a positive culture for genital mycoplasmas is a risk factor for spontaneous preterm birth. J Matern Fetal Neonatal Med 22:212–217. doi: 10.1080/14767050802616994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kasprzykowska U, Elias J, Elias M, Maczynska B, Sobieszczanska BM. 2014. Colonization of the lower urogenital tract with Ureaplasma parvum can cause asymptomatic infection of the upper reproductive system in women: a preliminary study. Arch Gynecol Obstet 289:1129–1134. doi: 10.1007/s00404-013-3102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Taylor-Robinson D, Jensen JS, Svenstrup H, Stacey CM. 2012. Difficulties experienced in defining the microbial cause of pelvic inflammatory disease. Int J STD AIDS 23:18–24. doi: 10.1258/ijsa.2011.011066. [DOI] [PubMed] [Google Scholar]
- 193.Cassell GH, Younger JB, Brown MB, Blackwell RE, Davis JK, Marriott P, Stagno S. 1983. Microbiologic study of infertile women at the time of diagnostic laparoscopy. Association of Ureaplasma urealyticum with a defined subpopulation. N Engl J Med 308:502–505. [DOI] [PubMed] [Google Scholar]
- 194.Shurin PA, Alpert S, Bernard Rosner BA, Driscoll SG, Lee YH. 1975. Chorioamnionitis and colonization of the newborn infant with genital mycoplasmas. N Engl J Med 293:5–8. doi: 10.1056/NEJM197507032930102. [DOI] [PubMed] [Google Scholar]
- 195.Horowitz S, Mazor M, Romero R, Horowitz J, Glezerman M. 1995. Infection of the amniotic cavity with Ureaplasma urealyticum in the midtrimester of pregnancy. J Reprod Med 40:375–379. [PubMed] [Google Scholar]
- 196.Holst RM, Mattsby-Baltzer I, Wennerholm UB, Hagberg H, Jacobsson B. 2005. Interleukin-6 and interleukin-8 in cervical fluid in a population of Swedish women in preterm labor: relationship to microbial invasion of the amniotic fluid, intra-amniotic inflammation, and preterm delivery. Acta Obstet Gynecol Scand 84:551–557. doi: 10.1111/j.0001-6349.2005.00708.x. [DOI] [PubMed] [Google Scholar]
- 197.Witt A, Berger A, Gruber CJ, Petricevic L, Apfalter P, Husslein P. 2005. IL-8 concentrations in maternal serum, amniotic fluid and cord blood in relation to different pathogens within the amniotic cavity. J Perinat Med 33:22–26. [DOI] [PubMed] [Google Scholar]
- 198.Menon R, Peltier MR, Eckardt J, Fortunato SJ. 2009. Diversity in cytokine response to bacteria associated with preterm birth by fetal membranes. Am J Obstet Gynecol 201:306.e1–306.e6. doi: 10.1016/j.ajog.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 199.Perni SC, Vardhana S, Korneeva I, Tuttle SL, Paraskevas LR, Chasen ST, Kalish RB, Witkin SS. 2004. Mycoplasma hominis and Ureaplasma urealyticum in midtrimester amniotic fluid: association with amniotic fluid cytokine levels and pregnancy outcome. Am J Obstet Gynecol 191:1382–1386. doi: 10.1016/j.ajog.2004.05.070. [DOI] [PubMed] [Google Scholar]
- 200.Naessens A, Foulon W, Breynaert J, Lauwers S. 1988. Serotypes of Ureaplasma urealyticum isolated from normal pregnant women and patients with pregnancy complications. J Clin Microbiol 26:319–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Jacobsson B, Aaltonen R, Rantakokko-Jalava K, Morken NH, Alanen A. 2009. Quantification of Ureaplasma urealyticum DNA in the amniotic fluid from patients in PTL and pPROM and its relation to inflammatory cytokine levels. Acta Obstet Gynecol Scand 88:63–70. doi: 10.1080/00016340802572646. [DOI] [PubMed] [Google Scholar]
- 202.Kasper DC, Mechtler TP, Reischer GH, Witt A, Langgartner M, Pollak A, Herkner KR, Berger A. 2010. The bacterial load of Ureaplasma parvum in amniotic fluid is correlated with an increased intrauterine inflammatory response. Diagn Microbiol Infect Dis 67:117–121. doi: 10.1016/j.diagmicrobio.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 203.von Chamier M, Allam A, Brown MB, Reinhard MK, Reyes L. 2012. Host genetic background impacts disease outcome during intrauterine infection with Ureaplasma parvum. PLoS One 7:e44047. doi: 10.1371/journal.pone.0044047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Menon R, Williams SM, Fortunato SJ. 2007. Amniotic fluid interleukin-1beta and interleukin-8 concentrations: racial disparity in preterm birth. Reprod Sci 14:253–259. doi: 10.1177/1933719107301336. [DOI] [PubMed] [Google Scholar]
- 205.Knox CL, Dando SJ, Nitsos I, Kallapur SG, Jobe AH, Payton D, Moss TJ, Newnham JP. 2010. The severity of chorioamnionitis in pregnant sheep is associated with in vivo variation of the surface-exposed multiple-banded antigen/gene of Ureaplasma parvum. Biol Reprod 83:415–426. doi: 10.1095/biolreprod.109.083121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Robinson JW, Dando SJ, Nitsos I, Newnham J, Polglase GR, Kallapur SG, Pillow JJ, Kramer BW, Jobe AH, Payton D, Knox CL. 2013. Ureaplasma parvum serovar 3 multiple banded antigen size variation after chronic intra-amniotic infection/colonization. PLoS One 8:e62746. doi: 10.1371/journal.pone.0062746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Reyes L, Reinhard M, Brown MB. 2009. Different inflammatory responses are associated with Ureaplasma parvum-induced UTI and urolith formation. BMC Infect Dis 9:9. doi: 10.1186/1471-2334-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Cassell GH, Davis RO, Waites KB, Brown MB, Marriott PA, Stagno S, Davis JK. 1983. Isolation of Mycoplasma hominis and Ureaplasma urealyticum from amniotic fluid at 16–20 weeks of gestation: potential effect on outcome of pregnancy. Sex Transm Dis 10:294–302. [PubMed] [Google Scholar]
- 209.Czikk MJ, McCarthy FP, Murphy KE. 2011. Chorioamnionitis: from pathogenesis to treatment. Clin Microbiol Infect 17:1304–1311. doi: 10.1111/j.1469-0691.2011.03574.x. [DOI] [PubMed] [Google Scholar]
- 210.Stirling KM, Hussain N, Sanders MM, Campbell W. 2016. Association between maternal genital mycoplasma colonization and histologic chorioamnionitis in preterm births. J Neonatal Perinatal Med 9:201–209. doi: 10.3233/NPM-16915059. [DOI] [PubMed] [Google Scholar]
- 211.Novy MJ, Duffy L, Axthelm MK, Sadowsky DW, Witkin SS, Gravett MG, Cassell GH, Waites KB. 2009. Ureaplasma parvum or Mycoplasma hominis as sole pathogens cause chorioamnionitis, preterm delivery, and fetal pneumonia in rhesus macaques. Reprod Sci 16:56–70. doi: 10.1177/1933719108325508. [DOI] [PubMed] [Google Scholar]
- 212.Yoder BA, Coalson JJ, Winter VT, Siler-Khodr T, Duffy LB, Cassell GH. 2003. Effects of antenatal colonization with Ureaplasma urealyticum on pulmonary disease in the immature baboon. Pediatr Res 54:797–807. doi: 10.1203/01.PDR.0000091284.84322.16. [DOI] [PubMed] [Google Scholar]
- 213.Senthamaraikannan P, Presicce P, Rueda CM, Maneenil G, Schmidt AF, Miller LA, Waites KB, Jobe AH, Kallapur SG, Chougnet CA. 2016. Intra-amniotic Ureaplasma parvum induced maternal and fetal inflammation and immune responses in rhesus macaque. J Infect Dis 214:1597–1604. doi: 10.1093/infdis/jiw408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Gravett MG, Witkin SS, Haluska GJ, Edwards JL, Cook MJ, Novy MJ. 1994. An experimental model for intraamniotic infection and preterm labor in rhesus monkeys. Am J Obstet Gynecol 171:1660–1667. doi: 10.1016/0002-9378(94)90418-9. [DOI] [PubMed] [Google Scholar]
- 215.Moss TJ, Nitsos I, Ikegami M, Jobe AH, Newnham JP. 2005. Experimental intrauterine ureaplasma infection in sheep. Am J Obstet Gynecol 192:1179–1186. doi: 10.1016/j.ajog.2004.11.063. [DOI] [PubMed] [Google Scholar]
- 216.Nitsos I, Moss TJ, Cock ML, Harding R, Newnham JP. 2002. Fetal responses to intra-amniotic endotoxin in sheep. J Soc Gynecol Invest 9:80–85. doi: 10.1016/S1071-5576(01)00155-1. [DOI] [PubMed] [Google Scholar]
- 217.Mitchell BF, Taggart MJ. 2009. Are animal models relevant to key aspects of human parturition? Am J Physiol Regul Integr Comp Physiol 297:R525–R545. doi: 10.1152/ajpregu.00153.2009. [DOI] [PubMed] [Google Scholar]
- 218.Dando SJ, Nitsos I, Newnham JP, Jobe AH, Moss TJ, Knox CL. 2010. Maternal administration of erythromycin fails to eradicate intrauterine ureaplasma infection in an ovine model. Biol Reprod 83:616–622. doi: 10.1095/biolreprod.110.084954. [DOI] [PubMed] [Google Scholar]
- 219.Moss TJ, Knox CL, Kallapur SG, Nitsos I, Theodoropoulos C, Newnham JP, Ikegami M, Jobe AH. 2008. Experimental amniotic fluid infection in sheep: effects of Ureaplasma parvum serovars 3 and 6 on preterm or term fetal sheep. Am J Obstet Gynecol 198:122.e1–122.e8. doi: 10.1016/j.ajog.2007.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Polglase GR, Dalton RG, Nitsos I, Knox CL, Pillow JJ, Jobe AH, Moss TJ, Newnham JP, Kallapur SG. 2010. Pulmonary vascular and alveolar development in preterm lambs chronically colonized with Ureaplasma parvum. Am J Physiol Lung Cell Mol Physiol 299:L232–L241. doi: 10.1152/ajplung.00369.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Goldenberg RL, Andrews WW, Goepfert AR, Faye-Petersen O, Cliver SP, Carlo WA, Hauth JC. 2008. The Alabama Preterm Birth Study: umbilical cord blood Ureaplasma urealyticum and Mycoplasma hominis cultures in very preterm newborn infants. Am J Obstet Gynecol 198:43.e1–43.e5. doi: 10.1016/j.ajog.2007.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Viscardi RM, Hashmi N, Gross GW, Sun CC, Rodriguez A, Fairchild KD. 2008. Incidence of invasive ureaplasma in VLBW infants: relationship to severe intraventricular hemorrhage. J Perinatol 28:759–765. doi: 10.1038/jp.2008.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Colaizy TT, Morris CD, Lapidus J, Sklar RS, Pillers DA. 2007. Detection of ureaplasma DNA in endotracheal samples is associated with bronchopulmonary dysplasia after adjustment for multiple risk factors. Pediatr Res 61:578–583. doi: 10.1203/pdr.0b013e318045be03. [DOI] [PubMed] [Google Scholar]
- 224.Kotecha S, Hodge R, Schaber JA, Miralles R, Silverman M, Grant WD. 2004. Pulmonary Ureaplasma urealyticum is associated with the development of acute lung inflammation and chronic lung disease in preterm infants. Pediatr Res 55:61–68. doi: 10.1203/01.PDR.0000100757.38675.50. [DOI] [PubMed] [Google Scholar]
- 225.Fonseca LT, Silveira RC, Procianoy RS. 2011. Ureaplasma bacteremia in very low birth weight infants in Brazil. Pediatr Infect Dis J 30:1052–1055. doi: 10.1097/INF.0b013e31822a8662. [DOI] [PubMed] [Google Scholar]
- 226.Quinn PA, Gillan JE, Markestad T, St John MA, Daneman A, Lie KI, Li HC, Czegledy-Nagy E, Klein A. 1985. Intrauterine infection with Ureaplasma urealyticum as a cause of fatal neonatal pneumonia. Pediatr Infect Dis 4:538–543. doi: 10.1097/00006454-198509000-00020. [DOI] [PubMed] [Google Scholar]
- 227.Madan E, Meyer MP, Amortegui AJ. 1988. Isolation of genital mycoplasmas and Chlamydia trachomatis in stillborn and neonatal autopsy material. Arch Pathol Lab Med 112:749–751. [PubMed] [Google Scholar]
- 228.Ollikainen J, Hiekkaniemi H, Korppi M, Katila ML, Heinonen K. 1993. Ureaplasma urealyticum cultured from brain tissue of preterm twins who died of intraventricular hemorrhage. Scand J Infect Dis 25:529–531. doi: 10.3109/00365549309008538. [DOI] [PubMed] [Google Scholar]
- 229.Quinn PA. 1986. Evidence of an immune response to Ureaplasma urealyticum in perinatal morbidity and mortality. Pediatr Infect Dis 5:S282–287. doi: 10.1097/00006454-198611010-00018. [DOI] [PubMed] [Google Scholar]
- 230.Horowitz S, Mazor M, Horowitz J, Porath A, Glezerman M. 1995. Antibodies to Ureaplasma urealyticum in women with intraamniotic infection and adverse pregnancy outcome. Acta Obstet Gynecol Scand 74:132–136. doi: 10.3109/00016349509008922. [DOI] [PubMed] [Google Scholar]
- 231.Power CP, Wang JH, Manning B, Kell MR, Aherne NJ, Wu QD, Redmond HP. 2004. Bacterial lipoprotein delays apoptosis in human neutrophils through inhibition of caspase-3 activity: regulatory roles for CD14 and TLR-2. J Immunol 173:5229–5237. doi: 10.4049/jimmunol.173.8.5229. [DOI] [PubMed] [Google Scholar]
- 232.Espinoza J, Chaiworapongsa T, Romero R, Gomez R, Kim JC, Yoshimatsu J, Edwin S, Rathnasabapathy C, Yoon BH. 2002. Evidence of participation of soluble CD14 in the host response to microbial invasion of the amniotic cavity and intra-amniotic inflammation in term and preterm gestations. J Matern Fetal Neonatal Med 12:304–312. doi: 10.1080/jmf.12.5.304.312. [DOI] [PubMed] [Google Scholar]
- 233.Collins JJ, Kallapur SG, Knox CL, Kemp MW, Kuypers E, Zimmermann LJ, Newnham JP, Jobe AH, Kramer BW. 2013. Repeated intrauterine exposures to inflammatory stimuli attenuated transforming growth factor-beta signaling in the ovine fetal lung. Neonatology 104:49–55. doi: 10.1159/000350548. [DOI] [PubMed] [Google Scholar]
- 234.Wolfs TG, Kallapur SG, Knox CL, Thuijls G, Nitsos I, Polglase GR, Collins JJ, Kroon E, Spierings J, Shroyer NF, Newnham JP, Jobe AH, Kramer BW. 2013. Antenatal ureaplasma infection impairs development of the fetal ovine gut in an IL-1-dependent manner. Mucosal Immunol 6:547–556. doi: 10.1038/mi.2012.97. [DOI] [PubMed] [Google Scholar]
- 235.Josefowicz SZ, Lu LF, Rudensky AY. 2012. Regulatory T cells: mechanisms of differentiation and function. Annu Rev Immunol 30:531–564. doi: 10.1146/annurev.immunol.25.022106.141623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Saada AB, Terespolski Y, Adoni A, Kahane I. 1991. Adherence of Ureaplasma urealyticum to human erythrocytes. Infect Immun 59:467–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Padmini E, Uthra V. 2012. Role of Ureaplasma urealyticum in altering the endothelial metal concentration during preeclampsia. Placenta 33:304–311. doi: 10.1016/j.placenta.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 238.Smith DG, Russell WC, Thirkell D. 1994. Adherence of Ureaplasma urealyticum to human epithelial cells. Microbiology 140:2893–2898. doi: 10.1099/00221287-140-10-2893. [DOI] [PubMed] [Google Scholar]
- 239.Lingwood CA, Quinn PA, Wilansky S, Nutikka A, Ruhnke HL, Miller RB. 1990. Common sulfoglycolipid receptor for mycoplasmas involved in animal and human infertility. Biol Reprod 43:694–697. doi: 10.1095/biolreprod43.4.694. [DOI] [PubMed] [Google Scholar]
- 240.Allam AB, Alvarez S, Brown MB, Reyes L. 2011. Ureaplasma parvum infection alters filamin A dynamics in host cells. BMC Infect Dis 11:101. doi: 10.1186/1471-2334-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Malathi K, Siddiqui MA, Dayal S, Naji M, Ezelle HJ, Zeng C, Zhou A, Hassel BA. 2014. RNase L interacts with filamin A to regulate actin dynamics and barrier function for viral entry. mBio 5:e02012-14. doi: 10.1128/mBio.02012-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Li YH, Chen M, Brauner A, Zheng C, Skov Jensen J, Tullus K. 2002. Ureaplasma urealyticum induces apoptosis in human lung epithelial cells and macrophages. Biol Neonate 82:166–173. doi: 10.1159/000063616. [DOI] [PubMed] [Google Scholar]
- 243.Xiao L, Crabb DM, Dai Y, Chen Y, Waites KB, Atkinson TP. 2014. Suppression of antimicrobial peptide expression by Ureaplasma species. Infect Immun 82:1657–1665. doi: 10.1128/IAI.01231-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Watson HL, Blalock DK, Cassell GH. 1990. Variable antigens of Ureaplasma urealyticum containing both serovar-specific and serovar-cross-reactive epitopes. Infect Immun 58:3679–3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Glass JI, Lefkowitz EJ, Glass JS, Heiner CR, Chen EY, Cassell GH. 2000. The complete sequence of the mucosal pathogen Ureaplasma urealyticum. Nature 407:757–762. doi: 10.1038/35037619. [DOI] [PubMed] [Google Scholar]
- 246.Triantafilou M, De Glanville B, Aboklaish AF, Spiller OB, Kotecha S, Triantafilou K. 2013. Synergic activation of toll-like receptor (TLR) 2/6 and 9 in response to Ureaplasma parvum & urealyticum in human amniotic epithelial cells. PLoS One 8:e61199. doi: 10.1371/journal.pone.0061199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Shimizu T, Kida Y, Kuwano K. 2008. Ureaplasma parvum lipoproteins, including MB antigen, activate NF-kappa B through TLR1, TLR2 and TLR6. Microbiology 154:1318–1325. doi: 10.1099/mic.0.2007/016212-0. [DOI] [PubMed] [Google Scholar]
- 248.Uchida K, Nakahira K, Mimura K, Shimizu T, De Seta F, Wakimoto T, Kawai Y, Nomiyama M, Kuwano K, Guaschino S, Yanagihara I. 2013. Effects of Ureaplasma parvum lipoprotein multiple-banded antigen on pregnancy outcome in mice. J Reprod Immunol 100:118–127. doi: 10.1016/j.jri.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 249.Zheng X, Teng LJ, Watson HL, Glass JI, Blanchard A, Cassell GH. 1995. Small repeating units within the Ureaplasma urealyticum MB antigen gene encode serovar specificity and are associated with antigen size variation. Infect Immun 63:891–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Zheng X, Lau K, Frazier M, Cassell GH, Watson HL. 1996. Epitope mapping of the variable repetitive region with the MB antigen of Ureaplasma urealyticum. Clin Diagn Lab Immunol 3:774–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Monecke S, Helbig JH, Jacobs E. 2003. Phase variation of the multiple banded protein in Ureaplasma urealyticum and Ureaplasma parvum. Int J Med Microbiol 293:203–211. doi: 10.1078/1438-4221-00239. [DOI] [PubMed] [Google Scholar]
- 252.Zheng X, Watson HL, Waites KB, Cassell GH. 1992. Serotype diversity and antigen variation among invasive isolates of Ureaplasma urealyticum from neonates. Infect Immun 60:3472–3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Zheng X, Teng LJ, Glass JI, Blanchard A, Cao Z, Kempf MC, Watson HL, Cassell GH. 1994. Size variation of a major serotype-specific antigen of Ureaplasma urealyticum. Ann N Y Acad Sci 730:299–301. doi: 10.1111/j.1749-6632.1994.tb44272.x. [DOI] [PubMed] [Google Scholar]
- 254.Zimmerman CU, Stiedl T, Rosengarten R, Spergser J. 2009. Alternate phase variation in expression of two major surface membrane proteins (MBA and UU376) of Ureaplasma parvum serovar 3. FEMS Microbiol Lett 292:187–193. doi: 10.1111/j.1574-6968.2009.01505.x. [DOI] [PubMed] [Google Scholar]
- 255.Zimmerman CU, Stiedl T, Spergser J, Rosengarten R. 2014. A simple agar plate preparation for effective transfer of ureaplasma colonies onto nitrocellulose membranes for colony immunoblotting. J Microbiol Methods 104:79–81. doi: 10.1016/j.mimet.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 256.Zimmerman CU, Rosengarten R, Spergser J. 2011. Ureaplasma antigenic variation beyond MBA phase variation: DNA inversions generating chimeric structures and switching in expression of the MBA N-terminal paralogue UU172. Mol Microbiol 79:663–676. doi: 10.1111/j.1365-2958.2010.07474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zimmerman CU, Rosengarten R, Spergser J. 2013. Interaction of the putative tyrosine recombinases RipX (UU145), XerC (UU222), and CodV (UU529) of Ureaplasma parvum serovar 3 with specific DNA. FEMS Microbiol Lett 340:55–64. doi: 10.1111/1574-6968.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Zimmerman CU, Herrmann R, Rosengarten R. 2015. XerC-mediated DNA inversion at the inverted repeats of the UU172-phase-variable element of Ureaplasma parvum serovar 3. Microbiol Res 170:263–269. doi: 10.1016/j.micres.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 259.Istivan TS, Coloe PJ. 2006. Phospholipase A in Gram-negative bacteria and its role in pathogenesis. Microbiology 152:1263–1274. doi: 10.1099/mic.0.28609-0. [DOI] [PubMed] [Google Scholar]
- 260.De Silva NS, Quinn PA. 1986. Endogenous activity of phospholipases A and C in Ureaplasma urealyticum. J Clin Microbiol 23:354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.De Silva NS, Quinn PA. 1991. Localization of endogenous activity of phospholipases A and C in Ureaplasma urealyticum. J Clin Microbiol 29:1498–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.DeSilva NS, Quinn PA. 1999. Characterization of phospholipase A1, A2, C activity in Ureaplasma urealyticum membranes. Mol Cell Biochem 201:159–167. doi: 10.1023/A:1007082507407. [DOI] [PubMed] [Google Scholar]
- 263.Janeway CA Jr, Travers P, Walport M, Schlomchik MJ. 2001. Immunobiology: the immune system in health and disease, 5th ed Garland Science, New York, NY. [Google Scholar]
- 264.Robertson JA, Stemler ME, Stemke GW. 1984. Immunoglobulin A protease activity of Ureaplasma urealyticum. J Clin Microbiol 19:255–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Kilian M, Brown MB, Brown TA, Freundt EA, Cassell GH. 1984. Immunoglobulin A1 protease activity in strains of Ureaplasma urealyticum. Acta Pathol Microbiol Immunol Scand B 92:61–64. [DOI] [PubMed] [Google Scholar]
- 266.Kilian M, Freundt EA. 1984. Exclusive occurrence of an extracellular protease capable of cleaving the hinge region of human immunoglobulin A1 in strains of Ureaplasma urealyticum. Isr J Med Sci 20:938–941. [PubMed] [Google Scholar]
- 267.Arfi Y, Minder L, Di Primo C, Le Roy A, Ebel C, Coquet L, Claverol S, Vashee S, Jores J, Blanchard A, Sirand-Pugnet P. 2016. MIB-MIP is a mycoplasma system that captures and cleaves immunoglobulin G. Proc Natl Acad Sci U S A 113:5406–5411. doi: 10.1073/pnas.1600546113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Purcell RH, Taylor-Robinson D, Wong D, Chanock RM. 1966. Color test for the measurement of antibody to T-strain mycoplasmas. J Bacteriol 92:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Neyrolles O, Ferris S, Behbahani N, Montagnier L, Blanchard A. 1996. Organization of Ureaplasma urealyticum urease gene cluster and expression in a suppressor strain of Escherichia coli. J Bacteriol 178:2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Blanchard A, Razin S, Kenny GE, Barile MF. 1988. Characteristics of Ureaplasma urealyticum urease. J Bacteriol 170:2692–2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Takebe S, Numata A, Kobashi K. 1984. Stone formation by Ureaplasma urealyticum in human urine and its prevention by urease inhibitors. J Clin Microbiol 20:869–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Mobley HL, Island MD, Hausinger RP. 1995. Molecular biology of microbial ureases. Microbiol Rev 59:451–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Ligon JV, Kenny GE. 1991. Virulence of ureaplasmal urease for mice. Infect Immun 59:1170–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Williams LE, Wernegreen JJ. 2010. Unprecedented loss of ammonia assimilation capability in a urease-encoding bacterial mutualist. BMC Genomics 11:687. doi: 10.1186/1471-2164-11-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Bharat A, Cunningham SA, Scott Budinger GR, Kreisel D, DeWet CJ, Gelman AE, Waites K, Crabb D, Xiao L, Bhorade S, Ambalavanan N, Dilling DF, Lowery EM, Astor T, Hachem R, Krupnick AS, DeCamp MM, Ison MG, Patel R. 2015. Disseminated ureaplasma infection as a cause of fatal hyperammonemia in humans. Sci Transl Med 7:284re3. doi: 10.1126/scitranslmed.aaa8419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Rogers MJ, Simmons J, Walker RT, Weisburg WG, Woese CR, Tanner RS, Robinson IM, Stahl DA, Olsen G, Leach RH, Maniloff J. 1985. Construction of the mycoplasma evolutionary tree from 5S rRNA sequence data. Proc Natl Acad Sci U S A 82:1160–1164. doi: 10.1073/pnas.82.4.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Woese CR, Stackebrandt E, Ludwig W. 1984. What are mycoplasmas: the relationship of tempo and mode in bacterial evolution. J Mol Evol 21:305–316. [DOI] [PubMed] [Google Scholar]
- 278.Dando SJ, Nitsos I, Polglase GR, Newnham JP, Jobe AH, Knox CL. 2014. Ureaplasma parvum undergoes selection in utero resulting in genetically diverse isolates colonizing the chorioamnion of fetal sheep. Biol Reprod 90:27. doi: 10.1095/biolreprod.113.113456. [DOI] [PubMed] [Google Scholar]
- 279.Yudin MH, van Schalkwyk J, Van Eyk N, Boucher M, Castillo E, Cormier B, Gruslin A, Money DM, Murphy K, Ogilvie G, Paquet C, Steenbeek A, Wong T, Gagnon R, Hudon L, Basso M, Bos H, Delisle MF, Farine D, Grabowska K, Menticoglou S, Mundle WR, Murphy-Kaulbeck LC, Ouellet A, Pressey T, Roggensack A. 2009. Antibiotic therapy in preterm premature rupture of the membranes. J Obstet Gynaecol Can 31:863–874. doi: 10.1016/S1701-2163(16)34305-5. [DOI] [PubMed] [Google Scholar]
- 280.Lamont RF, Jaggat AN. 2007. Emerging drug therapies for preventing spontaneous preterm labor and preterm birth. Expert Opin Invest Drugs 16:337–345. doi: 10.1517/13543784.16.3.337. [DOI] [PubMed] [Google Scholar]
- 281.Morency AM, Bujold E. 2007. The effect of second-trimester antibiotic therapy on the rate of preterm birth. J Obstet Gynaecol Can 29:35–44. doi: 10.1016/S1701-2163(16)32350-7. [DOI] [PubMed] [Google Scholar]
- 282.Waites KB, Katz B, Schelonka RL. 2005. Mycoplasmas and ureaplasmas as neonatal pathogens. Clin Microbiol Rev 18:757–789. doi: 10.1128/CMR.18.4.757-789.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Beeton ML, Chalker VJ, Jones LC, Maxwell NC, Spiller OB. 2015. Antibiotic resistance among clinical ureaplasma isolates recovered from neonates in England and Wales between 2007 and 2013. Antimicrob Agents Chemother 60:52–56. doi: 10.1128/AAC.00889-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Fernandez J, Karau MJ, Cunningham SA, Greenwood-Quaintance KE, Patel R. 2016. Antimicrobial susceptibility and clonality of clinical ureaplasma isolates in the United States. Antimicrob Agents Chemother 60:4793–4798. doi: 10.1128/AAC.00671-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Song J, Qiao Y, Kong Y, Ruan Z, Huang J, Song T, Zhang J, Xie X. 2015. Frequent topoisomerase IV mutations associated with fluoroquinolone resistance in Ureaplasma species. J Med Microbiol 64:1315–1320. doi: 10.1099/jmm.0.000153. [DOI] [PubMed] [Google Scholar]
- 286.Xiao L, Crabb DM, Duffy LB, Paralanov V, Glass JI, Waites KB. 2012. Chromosomal mutations responsible for fluoroquinolone resistance in Ureaplasma species in the United States. Antimicrob Agents Chemother 56:2780–2783. doi: 10.1128/AAC.06342-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Xiao L, Crabb DM, Duffy LB, Paralanov V, Glass JI, Hamilos DL, Waites KB. 2011. Mutations in ribosomal proteins and ribosomal RNA confer macrolide resistance in human Ureaplasma spp. Int J Antimicrob Agents 37:377–379. doi: 10.1016/j.ijantimicag.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 288.Kenyon SL, Taylor DJ, Tarnow-Mordi W. 2001. Broad-spectrum antibiotics for preterm, prelabour rupture of fetal membranes: the ORACLE I randomised trial. ORACLE Collaborative Group. Lancet 357:979–988. [DOI] [PubMed] [Google Scholar]
- 289.Kenyon S, Boulvain M, Neilson J. 2001. Antibiotics for preterm premature rupture of membranes. Cochrane Database Syst Rev 2001(4):CD001058. [DOI] [PubMed] [Google Scholar]
- 290.Kenyon S, Boulvain M, Neilson J. 2004. Antibiotics for preterm rupture of the membranes: a systematic review. Obstet Gynecol 104:1051–1057. doi: 10.1097/01.AOG.0000143268.36682.21. [DOI] [PubMed] [Google Scholar]
- 291.Gomez R, Romero R, Nien JK, Medina L, Carstens M, Kim YM, Espinoza J, Chaiworapongsa T, Gonzalez R, Iams JD, Rojas I. 2007. Antibiotic administration to patients with preterm premature rupture of membranes does not eradicate intra-amniotic infection. J Matern Fetal Neonatal Med 20:167–173. doi: 10.1080/14767050601135485. [DOI] [PubMed] [Google Scholar]
- 292.Mazor M, Chaim W, Horowitz S, Leiberman JR, Glezerman M. 1993. Successful treatment of preterm labour by eradication of Ureaplasma urealyticum with erythromycin. Arch Gynecol Obstet 253:215–218. doi: 10.1007/BF02766648. [DOI] [PubMed] [Google Scholar]
- 293.Berg TG, Philpot KL, Welsh MS, Sanger WG, Smith CV. 1999. Ureaplasma/mycoplasma-infected amniotic fluid: pregnancy outcome in treated and nontreated patients. J Perinatol 19:275–277. doi: 10.1038/sj.jp.7200185. [DOI] [PubMed] [Google Scholar]
- 294.Heikkinen T, Laine K, Neuvonen PJ, Ekblad U. 2000. The transplacental transfer of the macrolide antibiotics erythromycin, roxithromycin and azithromycin. BJOG 107:770–775. doi: 10.1111/j.1471-0528.2000.tb13339.x. [DOI] [PubMed] [Google Scholar]
- 295.Philipson A, Sabath LD, Charles D. 1973. Transplacental passage of erythromycin and clindamycin. N Engl J Med 288:1219–1221. doi: 10.1056/NEJM197306072882307. [DOI] [PubMed] [Google Scholar]
- 296.Keelan JA, Nitsos I, Saito M, Musk GC, Kemp MW, Timmins M, Li S, Yaegashi N, Newnham JP. 2011. Maternal-amniotic-fetal distribution of macrolide antibiotics following intravenous, intramuscular, and intraamniotic administration in late pregnant sheep. Am J Obstet Gynecol 204:546.e10–546.e17. doi: 10.1016/j.ajog.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 297.Kemp MW, Miura Y, Payne MS, Watts R, Megharaj S, Jobe AH, Kallapur SG, Saito M, Spiller OB, Keelan JA, Newnham JP. 2014. Repeated maternal intramuscular or intraamniotic erythromycin incompletely resolves intrauterine Ureaplasma parvum infection in a sheep model of pregnancy. Am J Obstet Gynecol 211:134.e1–134.e9. doi: 10.1016/j.ajog.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 298.Ramsey PS, Vaules MB, Vasdev GM, Andrews WW, Ramin KD. 2003. Maternal and transplacental pharmacokinetics of azithromycin. Am J Obstet Gynecol 188:714–718. doi: 10.1067/mob.2003.141. [DOI] [PubMed] [Google Scholar]
- 299.Miura Y, Payne MS, Keelan JA, Noe A, Carter S, Watts R, Spiller OB, Jobe AH, Kallapur SG, Saito M, Stock SJ, Newnham JP, Kemp MW. 2014. Maternal intravenous treatment with either azithromycin or solithromycin clears Ureaplasma parvum from the amniotic fluid in an ovine model of intrauterine infection. Antimicrob Agents Chemother 58:5413–5420. doi: 10.1128/AAC.03187-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Acosta EP, Grigsby PL, Larson KB, James AM, Long MC, Duffy LB, Waites KB, Novy MJ. 2014. Transplacental transfer of azithromycin and its use for eradicating intra-amniotic ureaplasma infection in a primate model. J Infect Dis 209:898–904. doi: 10.1093/infdis/jit578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Grigsby PL, Novy MJ, Sadowsky DW, Morgan TK, Long M, Acosta E, Duffy LB, Waites KB. 2012. Maternal azithromycin therapy for ureaplasma intraamniotic infection delays preterm delivery and reduces fetal lung injury in a primate model. Am J Obstet Gynecol 207:475.e1–475.e14. doi: 10.1016/j.ajog.2012.10.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Keelan JA, Kemp MW, Payne MS, Johnson D, Stock SJ, Saito M, Fernandes P, Newnham JP. 2014. Maternal administration of solithromycin, a new, potent, broad-spectrum fluoroketolide antibiotic, achieves fetal and intra-amniotic antimicrobial protection in a pregnant sheep model. Antimicrob Agents Chemother 58:447–454. doi: 10.1128/AAC.01743-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Furfaro LL, Spiller OB, Keelan JA, Payne MS. 2015. In vitro activity of solithromycin and its metabolites, CEM-214 and N-acetyl-CEM-101, against 100 clinical Ureaplasma spp. isolates compared with azithromycin. Int J Antimicrob Agents 46:319–324. doi: 10.1016/j.ijantimicag.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 304.Waites KB, Crabb DM, Duffy LB. 2009. Comparative in vitro susceptibilities of human mycoplasmas and ureaplasmas to a new investigational ketolide, CEM-101. Antimicrob Agents Chemother 53:2139–2141. doi: 10.1128/AAC.00090-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Farrell DJ, Flamm RK, Sader HS, Jones RN. 2016. Results from the Solithromycin International Surveillance Program (2014). Antimicrob Agents Chemother 60:3662–3668. doi: 10.1128/AAC.00185-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Putnam SD, Castanheira M, Moet GJ, Farrell DJ, Jones RN. 2010. CEM-101, a novel fluoroketolide: antimicrobial activity against a diverse collection of Gram-positive and Gram-negative bacteria. Diagn Microbiol Infect Dis 66:393–401. doi: 10.1016/j.diagmicrobio.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 307.Putnam SD, Sader HS, Farrell DJ, Biedenbach DJ, Castanheira M. 2011. Antimicrobial characterisation of solithromycin (CEM-101), a novel fluoroketolide: activity against staphylococci and enterococci. Int J Antimicrob Agents 37:39–45. doi: 10.1016/j.ijantimicag.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 308.Golparian D, Fernandes P, Ohnishi M, Jensen JS, Unemo M. 2012. In vitro activity of the new fluoroketolide solithromycin (CEM-101) against a large collection of clinical Neisseria gonorrhoeae isolates and international reference strains, including those with high-level antimicrobial resistance: potential treatment option for gonorrhea? Antimicrob Agents Chemother 56:2739–2742. doi: 10.1128/AAC.00036-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Rodgers W, Frazier AD, Champney WS. 2013. Solithromycin inhibition of protein synthesis and ribosome biogenesis in Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. Antimicrob Agents Chemother 57:1632–1637. doi: 10.1128/AAC.02316-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Hassanein SM, El-Farrash RA, Hafez HM, Hassanin OM, Abd El Rahman NA. 2012. Cord blood interleukin-6 and neonatal morbidities among preterm infants with PCR-positive Ureaplasma urealyticum. J Matern Fetal Neonatal Med 25:2106–2110. doi: 10.3109/14767058.2012.678435. [DOI] [PubMed] [Google Scholar]
- 311.Gray DJ, Robinson HB, Malone J, Thomson RB Jr. 1992. Adverse outcome in pregnancy following amniotic fluid isolation of Ureaplasma urealyticum. Prenat Diagn 12:111–117. doi: 10.1002/pd.1970120206. [DOI] [PubMed] [Google Scholar]
- 312.Yoon BH, Romero R, Moon J, Chaiworapongsa T, Espinoza J, Kim YM, Edwin S, Kim JC, Camacho N, Bujold E, Gomez R. 2003. Differences in the fetal interleukin-6 response to microbial invasion of the amniotic cavity between term and preterm gestation. J Matern Fetal Neonatal Med 13:32–38. doi: 10.1080/jmf.13.1.32.38. [DOI] [PubMed] [Google Scholar]
- 313.Romero R, Miranda J, Chaemsaithong P, Chaiworapongsa T, Kusanovic JP, Dong Z, Ahmed AI, Shaman M, Lannaman K, Yoon BH, Hassan SS, Kim CJ, Korzeniewski SJ, Yeo L, Kim YM. 2015. Sterile and microbial-associated intra-amniotic inflammation in preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med 28:1394–1409. doi: 10.3109/14767058.2014.958463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Stepan M, Cobo T, Maly J, Navratilova M, Musilova I, Hornychova H, Jacobsson B, Kacerovsky M. 2016. Neonatal outcomes in subgroups of women with preterm prelabor rupture of membranes before 34 weeks. J Matern Fetal Neonatal Med 29:2373–2377. doi: 10.3109/14767058.2015.1086329. [DOI] [PubMed] [Google Scholar]
- 315.Musilova I, Kutova R, Pliskova L, Stepan M, Menon R, Jacobsson B, Kacerovsky M. 2015. Intraamniotic inflammation in women with preterm prelabor rupture of membranes. PLoS One 10:e0133929. doi: 10.1371/journal.pone.0133929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Stepan M, Cobo T, Musilova I, Hornychova H, Jacobsson B, Kacerovsky M. 2016. Maternal serum c-reactive protein in women with preterm prelabor rupture of membranes. PLoS One 11:e0150217. doi: 10.1371/journal.pone.0150217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Berger A, Witt A, Haiden N, Kaider A, Klebermasz K, Fuiko R, Langgartner M, Pollak A. 2009. Intrauterine infection with Ureaplasma species is associated with adverse neuromotor outcome at 1 and 2 years adjusted age in preterm infants. J Perinat Med 37:72–78. doi: 10.1515/JPM.2009.016. [DOI] [PubMed] [Google Scholar]
- 318.Stein A, Boubli L, Blanc B, Raoult D. 1994. Genital mycoplasmas in placental infections. Infect Dis Obstet Gynecol 1:275–281. doi: 10.1155/S1064744994000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Van Marter LJ, Dammann O, Allred EN, Leviton A, Pagano M, Moore M, Martin C. 2002. Chorioamnionitis, mechanical ventilation, and postnatal sepsis as modulators of chronic lung disease in preterm infants. J Pediatr 140:171–176. doi: 10.1067/mpd.2002.121381. [DOI] [PubMed] [Google Scholar]
- 320.Miralles R, Hodge R, McParland PC, Field DJ, Bell SC, Taylor DJ, Grant WD, Kotecha S. 2005. Relationship between antenatal inflammation and antenatal infection identified by detection of microbial genes by polymerase chain reaction. Pediatr Res 57:570–577. doi: 10.1203/01.PDR.0000155944.48195.97. [DOI] [PubMed] [Google Scholar]
- 321.Olomu IN, Hecht JL, Onderdonk AO, Allred EN, Leviton A. 2009. Perinatal correlates of Ureaplasma urealyticum in placenta parenchyma of singleton pregnancies that end before 28 weeks of gestation. Pediatrics 123:1329–1336. doi: 10.1542/peds.2008-1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Kundsin RB, Driscoll SG, Monson RR, Yeh C, Biano SA, Cochran WD. 1984. Association of Ureaplasma urealyticum in the placenta with perinatal morbidity and mortality. N Engl J Med 310:941–945. doi: 10.1056/NEJM198404123101502. [DOI] [PubMed] [Google Scholar]