Abstract
Introduction
Preventive resin restorations (PRR) are the conservative choice for the most common carious lesions in children. Thus, new age flowable resin composites with higher filler content are readily used. The aim of this study was to evaluate the microshear bond strength and microleakage of two flowable resin composites containing different percentages of nano zinc oxide (NZnO) particles, which have proven to have antimicrobial properties.
Methods
This experimental in-vitro study was carried out in the Dental Material Research Center of Babol University of Medical Sciences in 2015. One nanohybrid and one nanofill flowable resin composite were chosen and modified with the incorporation of 1% and 3% Wt NZnO particles. Six groups (n=10, 0%, 1%, and 3%) of resin composite sticks on dental enamel (2×2mm) were prepared to be placed in the microtensile tester. The microshear bond strength magnitude (MPa) was recorded at the point of failure. A class I box (3×0.8×1 mm) was prepared on 60 premolars and filled using the resin composites (6 groups, n=10). The specimens were immersed in a 5% basic fuschin solution and sectioned bucco-lingually to view the microleakage using a stereomicroscope. One-way ANOVA and Tukey tests for microshear and Wilcoxon and Kruskal–Wallis tests for microleakage were used to analyze the data in the IBM SPSS Statistics version 22 software.
Results
The bond strength of the 3% clearfill group significantly decreased while no significant change occurred in the bond strength in other groups. The Z-350 group had significantly lower microleakage as nanoparticles increased. No significant difference was observed in the clearfill group.
Conclusion
Up to 3% Wt incorporation of NZnO particles will not diversely alter the bond strength, but it will be beneficial in providing antimicrobial effects with lower microleakage rates.
Keywords: Dental leakage, Flowable composite, Nanoparticles, Shear strength, Zinc oxide
1. Introduction
Dental caries is still a common challenge to overcome in children. Occlusal pits and fissures are usually the most common trigger point for demineralization. Research has indicated that almost 90% of the caries in the permanent dentition of children occur in the pits and fissures and two-thirds of carious lesions are confined exclusively to the occlusal surfaces (1). An accepted and approved technique for restoring the caries of occlusal pits and fissures and preventing the further development of the caries in the adjacent pits and fissures is the preventive resin restoration technique (2–5). This technique is widely practiced due to being non-invasive (5). A wide range of resin composites is available for resin restorations, including flowable fissure sealant resins, flowable resin composites, hybrid and microfilled resin composites, and highly viscous and packable resin composites, each with special advantages and disadvantages (6). New age flowable resin composites are used for restoring cervical lesions, deciduous teeth, and other small lesions in non-stress bearing areas, as well as PRRs and fissure sealants (7, 8). What might be a slight drawback of the light-cured resin composites used for PRRs is polymerization shrinkage, causing occasional gaps along the bonded interface (9). Bacteria, molecules, liquids, and ions can penetrate through these gaps in a phenomenon called microleakage (10), resulting in dental sensitivity, recurrent caries, pulpal pathosis, and ultimately restoration failure (11). The most common reason for PRR failures, as detailed in the literature, is microleakage (2, 12, 13). One study calculated the rate of failure for these restorations at 20% (14). Although the contributing factors for caries and the preventive measures are all known, recurrent and secondary caries still account for the major part of resin restoration replacements (15, 16). Different methods and compositions have been investigated to prevent plaque accumulation on resin composite restorations. One successful method was the addition of nano zinc oxide (NZnO) particles to resin composite, due to its antimicrobial properties against streptococcus mutans (17, 18). The higher the percentage of the NZnO, the more antimicrobial effects it proved to provide. Furthermore, despite the decreasing rate of the antimicrobial properties of the composite after one month, it was still measured to be higher than the control group (19). In another study. the addition of 10% NZnO particles to a light-cured resin composite caused a 80% reduction of the microorganisms in the plaque accumulated on the restoration surface (20). High bond strength and the absence of microleakage are desirable properties of an ideal resin composite. If a resin composite was to have such properties plus special antimicrobial effects, it would greatly contribute to resin restoration qualities and enhance health services in the bigger picture. As the superior antimicrobial properties of resin composites containing NZnO particles have been proven, the aim of this study was to evaluate the microshear bond strength and microleakage of two flowable resin composites containing different percentages of NZnO particles.
2. Material and Methods
2.1. Resin composite preparation
This experimental in-vitro study was conducted in the Dental Material Research Center of Babol University of Medical Sciences in 2015. Two flowable resin composites were modified using NZnO particles in order to obtain the following desired compositions:
No added NZnO particles (the control group)
1% Wt NZnO containing resin composites
3% Wt NZnO containing resin composites
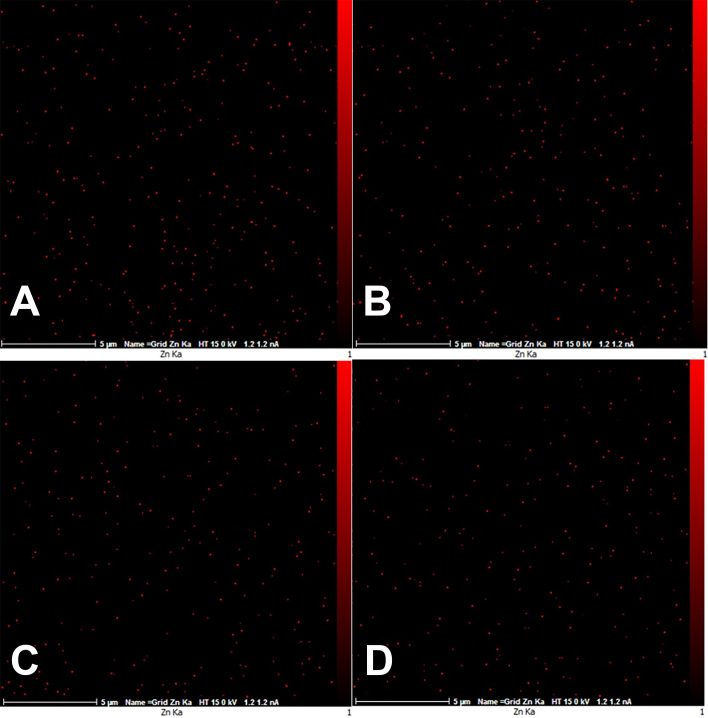
The materials used are described in Table 1. The nanoparticles were weighed using a digital scale with 0.0001 gr accuracy (A&D, USA). The mixing was carried out in a dark room using a spatula on a glass slab and placed over a vibrator for 15 minutes each. The resin composites were then returned to their opaque containers. Two specimens from each group were subjected to EDAX test for determining the homogenous diffusion of the resin particles within the resin matrix (Figure 1).
Table 1.
The materials used and their composition and manufacture
| Material | Composition | Manufacturer |
|---|---|---|
| Clearfill AP-X Flow | Nanohybrid resin composite, Bis-GMA, TEGDMA, 81% Wt barium glass and silica nano fillers | Kurary, Japan |
| Filtek Z-350 flowable | Nanofill resin composite, Bis-GMA, TEGDMA and Bis-EMA, 72% Wt silica, zirconia and zirconia/silica nanocluster fillers | 3M ESPE, USA |
| Nano Zinc Oxide | Mean diameter 20 nm, spherical crystal structure, 98% purity | US Nano, USA |
| Etch-rite Phosphoric Acid | 37% phosphoric acid | Pulpdent, USA |
| Clearfill SE bond | Two bottles, self-etch | Kurary, Japan |
Figure 1.
EDAX view showing the homogenous diffusion of NZnO particles, A: 3% Z-350, B: 3% clearfill, C: 1% Z-350, D: 1% clearfill
2.2. Microshear bond strength test
Thirty premolars, extracted for orthodontic reasons no longer than three months prior to the study and having no caries or cracks, were used to prepare specimens for the microshear bond strength (n=10 in six groups). They were kept in a 0.2% thymol solution for 24 hours and then in normal saline throughout the testing period, which was refreshed weekly. First, the roots were cut using a diamond disk (D&Z, Germany); then the crown was parted in half bucco-lingually. The buccal and lingual surfaces were ground to a flat level using silicon carbide sand paper (course), etched for 30 s, rinsed for another 30 s, and dried until the chalky white etched enamel was evident. The etched surfaces were bonded and light-cured for 20 s (LED VALO, Ultradent, USA) with 2300 mW/cm2 power. The power was calibrated using a radiometer before curing. A plastic cylindrical transparent mold was placed over the bonded surface of the enamel, and a 2 mm thickness resin composite was placed inside the mold and light cured for 40 s. The specimens were then placed and sectioned in the precision sectioning machine (Delta precision sectioning machine, Nemo, Mashhad, Iran) to sticks with a 2×2 mm surface area. To further enhance the accuracy of the measurements, the surface area of the sticks was measured in mm2 using a digital vernier caliper (Mitutoyo, Japan). These sticks were placed in a cantilever position in the microtensile tester (BISCO, USA). A wire loop was exacted around the interface of the enamel and resin composite and then pulled upwards at a speed of 0.5 mm/min until the failure occurred. The force magnitude at that point was registered in Newton, which was then divided by the surface area of each stick showing the microshear bond strength magnitude (MPa). The mode of failure was evaluated for each specimen using stereomicroscope (40× magnitude, HITACHI, S-4160, JAPAN) to determine the bond failure (adhesive, cohesive, or mixed). The mode of failure of the specimens was recorded using a stereomicroscope. The data acquired for the shear bond strength were analyzed using one-way ANOVA and Tukey tests.
2.3. Microleakage test
Sixty premolars with similar properties as the previous test were used to evaluate the microleakage of the modified resin composites. A 1 mm deep class I box was prepared in the occlusal part of the teeth using a diamond bur (D&Z, Germany) with all dimensions within the enamel (3×0.8×1 mm). One bur was used to prepare only six teeth. All the boxes were subjected to etching and bonding, as mentioned earlier, and were then filled with resin composites in six different study groups (n=10). The prepared teeth were thermocycled for 1500 cycles (5°C–55°C, 30 s in each bath, Nemo thermocycling machine, Mashhad, Iran). All dental surfaces were then covered using nail polish up to 1 mm around the restoration junction and the apical foramen was sealed using sticky wax. The teeth were immersed in a 5% basic fuschin solution for 24 hours at 37°C to allow the infusion of the solution through any possible gaps or faults. The teeth were then rinsed and sectioned bucco-lingually and examined with a stereomicroscope (40× magnitude). The dye penetration amounts were registered using the ranking described by Rego et al. and Youssef et al. (21, 22):
0- No penetration
1- Occlusal one third in only one wall (buccal/lingual)
2- Occlusal one third in both walls
3- Middle one third in only one wall
4- Middle one third in both walls
5- Pulpal one third in only one wall
6- Pulpal one third in both walls
7- Complete penetration from in both walls and the involvement of the pulpal floor
The qualitative data for the microleakage test was analyzed using Wilcoxon and Kruskal–Wallis tests. All the statistical tests were analyzed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA). The mean difference was considered significant at the 0.05 level.
3. Results
The mean shear bond strength for the tested groups is shown in Table 2. In the Z-350 group, the higher the amount of nano fillers, the more force was required to fracture the specimens. Despite the increase of the bond strength for the Z-350 group, it was not statistically significant (p=0.63). Bond strength was observed to be otherwise for the clearfill group as it decreased with the addition of nanoparticles. The addition of 1% NZnO particles to clearfill was acceptable as the bond strength was still within the insignificant range from the control group, whereas adding 3% NZnO particles significantly decreased the bond strength (p=0.017). No significant difference was observed in the mode of failure, and it was seen to be mostly mixed. Only one specimen in the Z-350 3% group was seen to fracture from the adhesive point. The clearfill 3% group was all fractured in a mixed way (Table 2).
Table 2.
Mean shear bond strength for Z-350 and clearfill resin composite groups
| Resin composite | Groups (% Wt NZnO); n=10 | Mean | Mode of Failure (%) | ||
|---|---|---|---|---|---|
| Adhesive | Cohesive | Mixed | |||
| Z-350 | 0 | 10.92a | 0 a | 20 a | 80 a |
| 1 | 11.51a | 0 a | 30 a | 70 a | |
| 3 | 12.28a | 10 a | 10 a | 80 a | |
| Clearfill | 0 | 11.55a | 0 a | 10 a | 90 a |
| 1 | 9.55ab | 0 a | 30 a | 70 a | |
| 3 | 8.26b | 0 a | 0 a | 100 a | |
Note. The different superscript letters indicate the significance for each resin composite separately
Table 3 displays the number of teeth with each score for the microleakage. The Z-350 group had significantly lower microleakage scores (score 0) as the nanoparticle percentage increased (p=0.02). Evidently, in the 3% group, no microleakage was observed, and all the specimens got a score 0. In the clearfill group, no significant difference was observed (p=0.86), and more than half of the specimens in all of the tested groups got a 0 score for microleakage.
Table 3.
Number of teeth with each microleakage score
| Resin composite | Groups (% Wt NZnO); n=10 | Microleakage (scores) | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 5 | ||
| Z-350 | 0 | 5 | 3 | 0 | 2 | 0 |
| 1 | 8 | 2 | 0 | 0 | 0 | |
| 3 | 10 | 0 | 0 | 0 | 0 | |
| Clearfill | 0 | 6 | 3 | 1 | 0 | 0 |
| 1 | 7 | 2 | 0 | 0 | 1 | |
| 3 | 7 | 2 | 1 | 0 | 0 | |
4. Discussion
The aim of this study was to evaluate the microshear bond strength and microleakage of the two flowable resin composites containing different percentages of NZnO particles. The analysis of the acquired data in the present study suggested that the addition of 3% NZnO particles to the clearfill resin composite significantly decreased the microshear bond strength while in the Z-350 group a slight increase—although not significant—was evident. The presence of NZnO particles contrastively altered the strength of the two resin composites, which might be due to the different composition of each of the composites. Despite the insignificant statistical analysis, the microshear bond strength of the Z-350 group with NZnO particles increased, which supports previous studies (17, 23–25). However the strength required to debond the resin composite in Tavassoli et al.’s study was higher, even in the control group (30 Mega Pascal vs. 10 Mega Pascal) (17). The reason could stem from the differences of the test methods used in the two studies. In the latter study, a plastic tube was utilized to build the cylindrical composite on the tooth surface. Meanwhile, in the present study, after the placement of the resin composite on the tooth surface, the specimens where subjected to the precision sectioning machine, thereby facing extra stress during the sectioning step, which could have affected the specimens’ bond strength. Using a mold to build the composite cylinder on the tooth surface has the disadvantage of a larger-than-needed area of etching and bonding, which might not be covered with the resin composite. The method of the present study provides more similar conditions for the specimens, either the control or the test groups, and diminishes the confounding factors. Another notable factor could be the utilization of different bonding agents. The resin bonding used in Tavassoli et al.’s study was a 5th-generation bonding versus the two-bottle 6th-generation resin bonding of the present study. However, the mixed mode of failure noticed in almost all of the specimens diminishes the role of the bonding agent. It also is a good indicator of the stress-bearing area during the force application, which would be the bonded interface and not within either of the substrates.
In the clearfill group, a significant decrease of the bond strength was observed by adding 3% NZnO particles. Clearfill is a nanohybrid resin composite, containing high nano filler particles (81%). Because these particles have a higher surface-to-volume ratio, the addition of the NZnO particles could alter the existing balance of the filler-resin matrix, thereby lowering the available resin per volume unit, to infiltrate the resin bonding (26, 27). What should be kept in mind is the prior role of the NZnO particles as an antimicrobial agent. Although it could be an additional benefit to have increased bond strength, it is also acceptable to have results just similar to those of the control group, meaning that the incorporation of the nanoparticles will not adversely affect the properties of the resin composite. For the microleakage test, the alteration of the Z-350 resin composite composition with NZnO particles significantly scaled down the infusion of the dye solution. Surprisingly, in the 3% group, none of the specimens had any microleakage. Benetti et al. concluded that the better marginal integrity is related to a higher modulus of elasticity (28). This matter supports the findings of this study, showing that the better marginal integrity is related to higher bond strength. The specimens were randomly assigned to six groups for the microleakage test, but it would still be wise to keep in mind that the enamel structure is different from one another; thus, the difference in the microleakage test results could be explained by the probable structural faults of some of the specimens. In the clearfill group, no significant microleakage difference was observed between the groups. Ultimately, only 15 of the 60 microleakage specimens had evident microleakage, which were mostly limited to the occlusal one third (score 1). Using the dye penetration technique in vitro is considered the gold standard for microleakage rather than the techniques used in the oral cavity (29). The proteins of the saliva may seal the marginal gap of a resin restoration in the oral cavity; in addition, the penetration of dye seems to be better than that of bacteria and its byproducts. These could be some of the many factors inducing dye penetration as a better way to test the microleakage. Overall, the insertion of nanoparticles increased the microshear bond strength and decreased the microleakage in the Z-350 group. These findings indicate that the properties of this specific resin composite would be enhanced if up to 3% Wt NZnO particles are included in the fillers. Yet the findings are adverse for the clearfill group, which might be based on the filler size and percent weight difference of these two resin composites. Despite the beneficial antimicrobial property of this specific nanoparticle in higher percentages, previous studies have suggested that incorporating more than 3% NZnO might adversely affect the bond strength of the resin composite (17, 18, 24). Thus, this modification is only advised up to 3% Wt. One matter to mention is the comfortable isolation of the work area in this in vitro study, whereas the same conditions might not be achievable in vivo. Furthermore, seeing as how the two resin composites had different property changes, when nanoparticles were added, the investigation of other flowable resin composites—especially with a higher filler amount—in conjunction with NZnO particles is suggested.
5. Study limitations
The present study was limited by the number of specimens. Because dental tissues differ in structure and surface properties, an increased number of specimens would lower the effect of this compromising factor. In addition, the results should be compared with other studies only cautiously as bond strength tests can have very different results due to various substrates, specimen preparation, and storage and loading methods. Unfortunately, no unique standardization for bond strength tests exists among the research.
6. Conclusions
As the results indicate, the addition of 3% NZnO particles to the clearfill resin composite significantly decreased the microshear bond strength while in the Z-350 group a slight increase—although not significant—was evident. The presence of NZnO particles lowered the microleakage chance in the Z-350 groups, but no significant change was observed in the clearfill group. Keeping in mind the antimicrobial properties of NZnO particles, it can be concluded that the incorporation of up to 3% Wt of this filler in flowable resin composites will not adversely alter the bond strength or microleakage of the resin composite; indeed, in some cases it might even result in better properties. It would be wise to investigate the incorporation of this nanoparticle in other flowable resin composites with different filler sizes and percent weights, testing the effect in order to obtain an antimicrobial flowable resin composite with optimum properties.
Acknowledgments
The present paper is a summary of the postgraduate thesis with grant number 3261 of the corresponding author. The author would like to thank the Dental Material Research Center of Babol University of Medical Sciences for the time and material supplements for the laboratory procedures.
Footnotes
iThenticate screening: June 04, 2016, English editing: August 04, 2016, Quality control: September 24, 2016
Conflict of Interest:
There is no conflict of interest to be declared.
Authors' contributions:
All authors contributed to this project and article equally. All authors read and approved the final manuscript.
References
- 1.JR P. missouri, editor, editor. Pediatric dentistry infancy trough adolescence. 5th ed. Elsevier; 2013. p. 469. [Google Scholar]
- 2.Fuks AB, Grajover R, Eidelman E. Assessment of marginal leakage of class II amalgam-sealant restorations. ASDC j dent child. 1986;53(5):343–5. [PubMed] [Google Scholar]
- 3.McComb D. Systematic review of conservative operative caries management strategies. J dent educ. 2001;65(10):1154–61. [PubMed] [Google Scholar]
- 4.Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B, et al. Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent mater. 2005;21(9):864–81. doi: 10.1016/j.dental.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Simonsen RJ. Preventive resin restorations and sealants in light of current evidence. Dent clin North Am. 2005;49(4):815–23. doi: 10.1016/j.cden.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Leinfelder KF. Posterior composite resins: the materials and their clinical performance. J Am Den Assoc. 1995;126(5):663–4. 7–8, 71–2. doi: 10.14219/jada.archive.1995.0247. [DOI] [PubMed] [Google Scholar]
- 7.Ronald L, Sakaguchi J, Powers M. Flowable composites. Craig’s restorative dental material. 13th ed. 2012. p. 181. [Google Scholar]
- 8.Autio-Gold J. Clinical Evaluation of a Medium-Filled Flowable Restorative Material as a Pit and Fissure Sealant. Oper Dent. 2002;27(4):325–9. [PubMed] [Google Scholar]
- 9.Yazici AR, Celik C, Ozgunaltay G. Microleakage of different resin composite types. Quintessence int. 2004;35(10):790–4. [PubMed] [Google Scholar]
- 10.Hilton TJ, Schwartz RS, Ferracane JL. Microleakage of four Class II resin composite insertion techniques at intraoral temperature. Quintessence int. 1997;28(2):135–44. [PubMed] [Google Scholar]
- 11.Franco EB, Gonzaga Lopes L, Lia Mondelli RF, da Silva e Souza MH, Jr, Pereira Lauris JR. Effect of the cavity configuration factor on the marginal microleakage of esthetic restorative materials. Am j dent. 2003;16(3):211–4. [PubMed] [Google Scholar]
- 12.Fuks AB, Shey Z. In vitro assessment of marginal leakage of combined amalgam-sealant restorations on occlusal surfaces of permanent posterior teeth. ASDC j dent child. 1983;50(6):425–9. [PubMed] [Google Scholar]
- 13.Kossa AP. Microleakage in a hybrid amalgam-composite restoration. Gen dent. 1987;35(4):289–91. [PubMed] [Google Scholar]
- 14.Sandres BJ, Feigal RJ, Avery DR. In: Dentistry for the Child and Adolescent. McDonald READ, Dean JA, editors. Mosby; 2011. p. 320. [Google Scholar]
- 15.McIntyre J. Placement and replacement of restorations by selected practitioners. Aust Dent J. 2005;50(3):81–9. [PubMed] [Google Scholar]
- 16.Major IA. Clinical diagnosis of recurrent caries. J Am Dent Assoc. 2005;136(10):1426–33. doi: 10.14219/jada.archive.2005.0057. [DOI] [PubMed] [Google Scholar]
- 17.Tavassoli S, Alaghemand H, Hamze F, Ahmadian Babaki F, Rajab-Nia R, Rezvani MB, et al. Antibacterial, physical and mechanical properties of flowable resin composites containing zinc oxide nanoparticles. Dent mater. 2013;29(5):495–505. doi: 10.1016/j.dental.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Mirhashemi A, Bahador A, Kassaee MZ, Daryakenari GH, Ahmad-Akhoundi MS, Sodagar A, et al. Antimicrobial Effect of Nano-Zinc Oxide and Nano-Chitosan Particles in Dental Composite Used in Orthodontics. J Med Bacteriol. 2013;2(3–4):1–10. [Google Scholar]
- 19.Spencer CG, Campbell PM, Buschang PH, Cai J, Honeyman AL. Antimicrobial effects of zinc oxide in an orthodontic bonding agent. Angle Orthod. 2009;79(2):317–22. doi: 10.2319/011408-19.1. [DOI] [PubMed] [Google Scholar]
- 20.Aydin Sevinc B, Hanley L. Antibacterial activity of dental composites containing zinc oxide nanoparticles. J Biomed Mater Res B Appl Biomater. 2010;94(1):22–31. doi: 10.1002/jbm.b.31620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Microleakage evaluation of pit and fissure sealants done with different procedures, materials, and laser after invasive technique. J Clin Pediatr Dent. 1999;24:63–8. [PubMed] [Google Scholar]
- 22.Youssef MN, Youssef FA, Souza-Zaroni WC, Turbino ML, Vieira MM. Effect of enamel preparation method on in vitro marginal microleakage of a flowable composite used as pit and fissure sealant. Int j paediatr dent. 2006;16(5):342–7. doi: 10.1111/j.1365-263x.2006.00751.x. [DOI] [PubMed] [Google Scholar]
- 23.Vanajassun P, Nivedhitha MS, Nishad NT, Soman D. Effects of Zinc Oxide Nanoparticles in Combination with Conventional Glass Ionomer Cement: In vitro Study. Advance Human Biology. 2014;4(3):31–6. [Google Scholar]
- 24.Akhoundi MS, Sodagar A, Kasaei M. Effect of Nano-ZnO and Nano-Chitosan particles on shear bond strength of Dental Composite used in Orthodontics. 2013. In press. [Google Scholar]
- 25.Poosti M, Ramazanzadeh B, Zebarjad M, Javadzadeh P, Naderinasab M, Shakeri MT. Shear bond strength and antibacterial effects of orthodontic composite containing TiO2 nanoparticles. Eur J Orthod. 2013;35(5):676–9. doi: 10.1093/ejo/cjs073. [DOI] [PubMed] [Google Scholar]
- 26.JR P. missouri, editor, editor. Pediatric dentistry infancy trough adolescence. 5th ed. Elsevier; 2013. p. 471. [Google Scholar]
- 27.Sandres BJ, Feigal RJ, Avery DR. In: Dentistry for the Child and Adolescent. McDonald READ, Dean JA, editors. Mosby; 2011. [Google Scholar]
- 28.Benetti AR, Peutzfeldt A, Lussi A, Flury S. Resin composites: Modulus of elasticity and marginal quality. J dent. 2014;42(9):1185–92. doi: 10.1016/j.jdent.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J prosthet dent. 1991;65(3):436–42. doi: 10.1016/0022-3913(91)90239-s. [DOI] [PubMed] [Google Scholar]