Abstract
Studies suggest that individuals with schizophrenia have smaller social networks and less satisfying relationships. However, much is still unknown about the typical quantity and quality of social relationships in young adults during the ultra high-risk (UHR) period. Investigating these relationships holds significant importance for improving understanding of etiological processes, mapping the social environment, and highlighting treatment targets in a critical period. A total of 85 participants (44 UHR and 41 healthy controls) completed measures examining the participants’ social relationships, social support, and loneliness. Mean differences between the UHR and healthy control participants and associations between social relationships and symptoms and functioning were examined. Results indicated significant differences between groups on several indices. Specifically, the UHR youth reported fewer close friends, less diverse social networks, less perceived social support, poorer relationship quality with family and friends, and more loneliness. Notably, within the UHR group, being lonely and having fewer and worse quality relationships was associated with greater symptom severity and lower overall functioning. This study suggests that youth at high-risk of developing psychosis have fewer and poorer quality social relationships. Interventions that focus on increasing the quantity and quality of young adults’ social networks may be beneficial for this population.
Keywords: Negative Symptoms, Positive Symptoms, Psychosis, Social Networks, Social Support
1. Introduction
Deficits in social functioning have been observed in people with schizophrenia for over 100 years and are thought to be a hallmark of the disorder (Hooley, 2010). For example, people with psychosis are six times more likely to never marry (MacCabe et al., 2009) and have smaller social networks than healthy controls (Goldberg et al., 2003). In addition, severity of positive symptoms has been associated with fewer and less satisfying social relationships and high levels of loneliness in people with schizophrenia (Angell and Test, 2002). However, although a significant literature exists describing social functioning deficits in people with schizophrenia, relatively few studies have described the quantity and quality of social relationships of at-risk individuals during the ultra high-risk (UHR) period immediately preceding the onset of psychosis. The current study aimed to examine differences in the social relationships of UHR young adults and age matched healthy controls and the association between social relationships and symptom severity.
Studies of individuals with elevated schizotypy traits, schizotypal personality disorder (SPD), and first episode psychosis have shown some differences in social relationship quantity and quality (for a full review see Gayer-Anderson and Morgan, 2013). Individuals with high levels of negative schizotypal symptoms reported poorer quality relationships with family members and social relationships in general (Cohen and Iii, 2009). In another study, compared to age matched controls, adults with SPD were found to have fewer friends and be more likely to be single and living alone or with their parents (Dickey et al., 2005).
Similarly, individuals who have recently experienced their first episode of psychosis are more passive, withdrawn, and isolated than would be expected for individuals their age (Moller and Husby, 2003) and have fewer friends and confidants than age-matched controls (Erickson et al., 1989). In a sample of Swedish army members, premorbid assessments showed that preferring to socialize in small groups, having fewer than two friends, and not having a girlfriend were associated with an increased risk of developing schizophrenia (Malmberg et al., 1998). Another study of individuals with first episode psychosis found that many individuals reported poor perceived social support and feeling lonely several days a week (Sündermann et al., 2014). Many of these individuals did not have even one confidant, which was associated with being more susceptible to loneliness.
Past studies also suggest that social support is associated with symptom course and functioning for individuals with psychotic disorders. Studies have found associations between low levels of social support and high levels of both negative (Pruessner et al., 2011) and positive symptoms (Norman et al., 2005). Lower levels of social support have also been found to predict higher frequency of hospitalizations (Norman et al., 2005) and availability of friends and family predicts hospital stay length and psychotic symptom severity (Hultman et al., 1996).
Social functioning and social support levels are associated with general functioning and well-being in people who are at risk or have experienced their first episode of psychosis. For example, poorer social functioning is associated with poorer overall quality of life (Domínguez-Martínez et al., 2015) and a lower level of social support is associated with poorer general functioning (Pruessner et al., 2011). In a sample of individuals with early psychosis, low levels of social support initially and one year later were associated five years later with lower Global Assessment of Functioning (GAF) scores, fewer weeks of full-time employment, and more weeks receiving disability support (Norman et al., 2012).
Studies examining social relationships in individuals in the UHR period have also found lower levels of social support and more reported social isolation. For example, in a sample of 30 UHR young adults compared to 30 controls, UHR individuals reported lower levels of social support on self-report measures (Pruessner et al., 2011). Another study found that in a sample of 62 UHR youth, most participants had high levels of social isolation regardless of whether they had predominantly negative or positive symptoms, although no control group was included in the study (Cornblatt et al., 2003). Our group found that in a distinct sample of high-risk youth (comprised of adolescents meeting criteria for SPD) the high-risk youth reported significantly more frequent social interaction using the Internet and reported fewer interactions with “real-life” friends than non-psychiatric controls (Mittal et al., 2007).
The aim of the current study to conduct a descriptive examination of the social relationships of UHR individuals is important and informative for several reasons. Research on typical development has shown that adolescence is an important time for the development and maturation of social relationships at behavioral and neurological levels (Blakemore, 2008). During adolescence and young-adulthood, individuals’ social networks change substantially and they begin to spend less time with parents and more with peers and begin to form romantic relationships (Collins, 2003; Friedlmeier and Granqvist, 2006). Studies have found that social support from a variety of different sources during adolescence is especially tied to well-being and functioning, including academic adjustment, self-esteem, and depressive and anxiety symptoms (Rueger et al., 2009). In addition, negative perceptions of relationships with peers and family members have been found to be related to behavioral problems and emotional dysfunction during adolescence (Garnefski and Diekstra, 1996).
UHR individuals may be especially vulnerable to either developing poor social relationships or experiencing negative effects of having poor social support. Some studies have even found that social impairment is an important predictive marker of psychosis. For example, Cannon et al. (2008) found that social impairment was one of five unique predictors of conversion to psychosis in an UHR sample. Similarly, Cornblatt et al. (2007) found that compared to role functioning, poor social functioning was stable up to 2.5 years after a baseline assessment of a sample of UHR individuals and was predictive of later conversion. In addition to understanding which individuals are at the most risk for conversion, social relationships are also necessary for understanding the course and severity of symptoms in UHR youth.
Social relationships are also important because of their potential interaction with stress as proposed by the stress-buffering model (Cohen and Wills, 1985). The stress-buffering model proposes that social relationships are protective against stressful life events. Palmier-Claus et al., (2012) found that compared to controls, UHR individuals and those with psychotic disorders reported greater social stress and general levels of perceived stress, which was associated with more severe hallucinations and delusions. In addition, decreases in stressful maternal criticism have been found to predict improvement in subthreshold psychotic symptoms (O’Brien et al., 2015).
In summary, research has begun to examine social relationships and their associations with symptom severity and functioning in UHR youth with promising results. However, no study to date has used a variety of social measures to examine the social networks, social support, loneliness levels, and symptom severity of UHR youth and controls during the critical period of adolescence. Therefore, the current study aims to provide a broad descriptive view of the social relationships of UHR youth thus laying the groundwork for future studies designed to more specifically examine the mechanisms underlying the connection between relationships and symptoms and develop novel treatments and interventions. Specifically, the study aimed to evaluate potential differences between UHR individuals and controls in number of close friends, social network diversity, perceived social support, quality of relationships with family and friends, and loneliness. Based on findings from past studies of individuals with psychosis, we hypothesized that compared to healthy controls, UHR participants would report significantly fewer close friends (Dickey et al., 2005), less social network diversity (Goldberg et al., 2003), less perceived social support (Pruessner et al., 2011), poorer quality relationships with family and friends (Cohen and Iii, 2009), and more loneliness (Sündermann et al., 2014).
In addition, there is some preliminary evidence that poorer social relationship functioning is associated with more severe symptoms in UHR individuals and those with recent onset psychosis (Cornblatt et al., 2003; Pruessner et al., 2011). As a result, a second aim of the study was to examine the association between social relationships and symptoms, based on the hypothesis that fewer close friends, less social network diversity, less perceived social support, poorer quality relationships, and more loneliness would be associated with higher levels of positive and negative symptoms and lower overall functioning.
Further, we were also interested in testing whether two specific negative symptoms that are theoretically significant to social behavior – social anhedonia (Blanchard et al., 1998) and avolition (Strauss et al., 2013) – were associated with number of close friends, social network diversity, social support, quality of relationships, and loneliness in UHR individuals. Social anhedonia (enjoyment of social activities) and avolition (lack of motivation to engage in activities) were examined because they may be especially relevant to social functioning and relationships. We examined these negative symptoms separately because they measure related but distinct constructs from the other variables in the study.
Last, we have clinically observed that UHR youth often report interacting socially with others and yet still feel lonely and unsupported. This suggests that UHR youth may not be benefiting from social contact as much as other people. As a result, since adolescence is traditionally when peers begin playing an increasingly important role in social networks, we were interested in empirically testing the degree to which the association between number of close friends and loneliness differed for UHR youth relative to an age-matched non-psychiatric control group. We hypothesized that the association between number of friends and loneliness would be stronger for controls than for UHR individuals (i.e., compared to controls, UHR youth would report higher levels of loneliness independent of the number of friends they reported).
2. Methods
2.1 Participants
Participants were 44 UHR and 41 healthy control young adults who were recruited to the Adolescent Development and Preventative Treatment (ADAPT) research program (see Table 1 for demographic characteristics). The majority of the sample (65%) identified as White and approximately 18% of participants identified as Central/South American, 10% Asian, 5% interracial, 2% Black, and 1% Native American; 23% of the sample identified as Hispanic.
Table 1.
Participant Characteristics
| Controls | Ultra High Risk | X2 or t | p | |
|---|---|---|---|---|
| Gender | ||||
| Male | 15(37%) | 26 (59%) | ||
| Female | 26(63%) | 18 (41%) | −2.10 | .04 |
| Total | 41 | 44 | ||
| Age | ||||
| Mean Years (SD) | 19.20(2.56) | 19.17(1.73) | −0.07 | .94 |
| Parent Education | ||||
| Mean Years (SD) | 15.54 | 15.52 | −0.51 | .98 |
Control and UHR participants were recruited via email, newspaper advertisements, and Craigslist. UHR participants were also recruited using techniques that targeted clinical populations, specifically psychologists, psychiatrists, high school counselors, college counseling centers, psychiatric hospitals, and community-mental health centers. Advertising included using in-person presentations, phone calls, and regular mailers. In addition, recruitment utilized a bus advertisement campaign in Boulder, Aurora, and Denver as well as presentations for community mental health events.
UHR individuals were included if they met criteria for a prodromal syndrome. Inclusion criteria included: (a) recent onset or escalation of moderate levels of attenuated positive symptoms (a score of 3–5 on at least one item from the Structured Interview for Prodromal Syndromes); or (b) the presence of a first-degree relative with a psychotic disorder such as schizophrenia, coupled with a decline in global functioning over the last 12 months (Miller et al., 1999). 93% of the sample met criteria for the study based on moderate attenuated positive symptoms and 7% based on genetic risk. Exclusion criteria for both groups included the presence of a neurological disorder, lifetime substance dependence, or a head injury. Additional exclusion criteria were the presence of a current or lifetime Axis I psychotic disorder (e.g., schizophrenia, schizoaffective disorder, schizophreniform) for the UHR participants, and the presence of any current Axis I disorder as determined by the SCID (e.g., depression, social phobia, alcohol or substance abuse or dependence) or a psychotic disorder in a 1st degree relative for the healthy controls. The protocol and informed consent procedures were approved by the university Institutional Review Board.
2.2 Instruments
Interviews
The Structured Interview for Prodromal Syndromes (SIPS; Miller et al., 1999) was administered to both UHR and healthy control participants to diagnose a prodromal syndrome and gauge positive and negative symptoms. For this study, all 5 categories of positive symptoms (unusual thoughts, suspiciousness, grandiose ideas, perceptual abnormalities, and disorganized symptoms) were summed to create a positive dimension composite score. As for the negative dimension, 5 out of the 6 symptoms (avolition, expressed emotion, experience of emotion, ideational richness, and occupational functioning) were summed. Social anhedonia was not used in the composite score because of construct overlap with the social relationship measures. Separate analyses were also run using social anhedonia and avolition as outcome measures. We used avolition as an outcome measure because it is theoretically related to social behavior but did not remove it from the negative symptoms dimension because the construct overlap with the social measures is smaller than with social anhedonia.
The Structured Clinical Interview for Axis-I DSM-IV Disorders (SCID; First et al., 1995) was also administered to rule out formal psychosis in UHR participants and any Axis I disorders in the healthy control participants. A Global Assessment of Functioning (GAF) score was also made by the assessor during the interview on a scale ranging from 1 to 100, based on each participant’s overall functioning across domains. This measure has excellent interrater reliability in adolescent populations (Schorre and Vandvik, 2004) and has been commonly used in studies of UHR adolescents and young adults (Pruessner et al., 2011). Training of interviewers (who were advanced doctoral students) was conducted over a 2-month period and interrater reliabilities exceed the minimum study criterion of Kappa ≥.80.
Self-Report Questionnaires
The number of close friends and social network diversity were measured using the Social Network Index (SNI). The measure is composed of questions examining 12 types of social relationships, such as relationship with a spouse or partner, children, parents, relatives, friends, or neighbors (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997). For this study, the variable number of close friends was calculated using one item from this measure. The question asked, “How many friends do you see or talk to at least once every 2 weeks?”. Social network diversity was calculated similarly to Cohen et al. (1997) by summing each participant’s reported number of types of social relationships that made up their social network. Items that were endorsed by less than 5% of the sample (including children and in-laws) were not included in the social network diversity variable. A table of the percentage of participants in the UHR and control groups who endorsed talking to at least one person every two weeks separately by type of social relationship can be found in the supplementary materials.
Perceived social support was measured using the Interpersonal Support Evaluation List-12 (ISEL:Cohen, Mermelstein, Kamarck, & Hoberman, 1985). Half of the items were reverse scored so that higher scores represented higher levels of support. All 12 items were then summed to create a composite score for overall social support. The full version of the scale has good reliability (Cohen & Hoberman, 1983; Cohen & Wills, 1985) and convergent and structural validity (Brookings & Bolton, 1988; Cohen & Hoberman, 1983). In the current sample the ISEL-12 had excellent internal consistency (α = .91).
The quality of participants’ relationship with family and friends was measured using the Support and Strain Scales (Walen and Lachman, 2000). The scales consist of 6 items measuring positive, supportive interactions and 6 items measuring negative, strained interactions with family members and separately for relationships with friends; items are rated on a 4-point scale from “not at all” to “a lot”. The 6 items from each scale were summed with higher scores indicating high support and strain. The measures had good internal consistency for Family Support (α = .88), Family Strain (α = .85) and Friend Strain (α = .81) and excellent internal consistency for Friend Support (α = .91) in the current sample.
Loneliness was measured using the UCLA Loneliness Scale, which is a 20-item measure (Russell, Peplau, & Ferguson, 1980). Items are answered on a 4-point scale from “I never feel this way” to “I always feel this way.” The scale has excellent internal consistency (Cronbach’s alpha = .97) in the current sample and high test-retest reliability over 1 year (r = .73), and convergent validity with other scales of loneliness in other samples (Russell, 1996).
All variables were tested for normality and only family support and friend support were significantly skewed. Both variables were transformed and results from all analyses were very similar when the transformed variables were used. To maintain consistency, results are reported for non-transformed variables.
2.3 Analysis
To test for differences between the UHR and control participants, a series of t-tests were conducted, comparing the means between groups on the social relationship measures. Regression analyses were conducted in the UHR sample to test for associations between social relationship variables and positive and negative symptoms and overall functioning using GAF scores. Last, to test whether the association between number of friends and loneliness depended on group (UHR or controls), a regression with an interaction term (Number of Friends × Group) was run, adjusting for the two component terms.
3. Results
There were no differences in demographic characteristics between UHR and control groups except for gender (Table 1): there was a higher percentage of males in the UHR group relative to the control group. All analyses were run with gender as a covariate. As this did not impact the direction or magnitude of the findings, results are presented without controlling for gender.
There were several significant mean differences in the social networks of the UHR and healthy control participants (Table 2). Relative to controls, the UHR participants reported having fewer close friends, less diverse social networks (having social contact with people from fewer different domains), less perceived social support, less supportive and more strained relationships with family members and friends, and higher levels of loneliness. For example, 58% of UHR participants reported having fewer than 3 close friends compared to only 29% of controls. In addition, 73% of controls reported definitely being able to find someone to have lunch with compared to 23% of UHR individuals. Last, 47% of the UHR youth reported sometimes or often feeling completely alone compared to only 10% of the controls.
Table 2.
Social Network, Social Support, Relationship Quality, and Loneliness in Control and UHR Groups
| Control | Ultra High Risk | t | d | |
|---|---|---|---|---|
| Social Network | ||||
| Number of Close Friends (SD) | 4.29(1.97) | 2.88(2.15) | 3.05** | .69 |
| Social Network Diversity (SD) | 5.84(2.06) | 4.56(1.60) | 3.04** | .70 |
| Social Support | ||||
| ISEL (SD) | 42.46(5.92) | 34.87(6.97) | 5.32*** | 1.19 |
| Relationship Quality | ||||
| Family Support (SD) | 16.95(2.54) | 13.26(4.52) | 4.55*** | 1.00 |
| Family Strain (SD) | 6.24(4.26) | 10.26(3.95) | −4.46*** | .99 |
| Friend Support (SD) | 17.15(3.33) | 13.81(4.04) | 4.07*** | .91 |
| Friend Strain (SD) | 4.48(2.71) | 6.26(3.52) | −2.57* | .57 |
| Loneliness | ||||
| UCLA (SD) | 8.83(10.57) | 29.70(14.88) | −7.26*** | 1.63 |
p < .05.
p < .01.
p < .001.
Regression analyses examining only the UHR participants revealed several significant associations between social networks variables and symptom severity and overall functioning (Table 3). More severe positive symptoms were associated with less family support, less friend support, and higher levels of loneliness. More severe negative symptoms were associated with less perceived social support, less friend support, and higher levels of loneliness (Table 3). Finally, poorer overall functioning was associated with having fewer close friends, less social network diversity, and higher levels of loneliness (Table 3).
Table 3.
Social Relationship Measures and Positive and Negative Symptoms and Overall Functioning in UHR Youth
| Positive Symptoms | Negative Symptoms | Functioning | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| B(SE) | df | t | r | B(SE) | df | t | r | B(SE) | df | t | r | |
| Social Network | ||||||||||||
| Number of Close Friends | −.50(.92) | 40 | −1.95^ | .29 | −.74(.42) | 41 | −1.75^ | .26 | 1.98(.98) | 41 | 2.03* | .30 |
| Social Network Diversity | −.14(.39) | 36 | −.35 | .06 | −.57(.59) | 37 | −.97 | .16 | 3.49(1.36) | 37 | 2.57* | .39 |
| Social Support | ||||||||||||
| ISEL | −.12(.08) | 38 | −1.422 | .22 | −.41(.12) | 32 | −3.38** | .51 | .53(.30) | 39 | 1.74^ | .27 |
| Relationship Quality | ||||||||||||
| Family Support | −.25(.12) | 41 | −2.12* | .31 | −.36(.19) | 42 | −1.80^ | .27 | .38(.47) | 42 | .79 | .12 |
| Family Strain | .28(.14) | 41 | 2.01^ | .30 | .063(.23) | 42 | .27 | .04 | −.19(.55) | 42 | −.36 | .05 |
| Friend Support | −.33(.14) | 39 | −2.44* | .36 | −.57(.21) | 40 | −2.68* | .39 | .53(.48) | 40 | 1.10 | .17 |
| Friend Strain | −.13(.17) | 39 | −.77 | .12 | −.21(.26) | 40 | −.81 | .13 | .11(.56) | 40 | .20 | .03 |
| Loneliness | ||||||||||||
| UCLA | .11(.04) | 38 | 2.95* | .43 | .20(.06) | 39 | 3.55** | .49 | −.39(.13) | 39 | −3.00** | .43 |
Note: Analyses include only UHR participants. Functioning was measured using the GAF score from the SCID-IV.
p < .10.
p < .05.
p < .01.
p < .001.
We were also interested in evaluating the associations between the social variables and social anhedonia and avolition. Higher levels of social anhedonia were associated with fewer close friends, r(40) = −.43, p < .01, less social network diversity, r(36) = −.37, p < .05, less perceived social support, r(38) = −.41, p < .01, less friend support, r(39) = −.40, p < .01, and higher levels of loneliness, r(38) = .42, p < .01, but less friend strain, r(39) = −.31, p < .05; social anhedonia was not associated with family support or strain. Higher levels of avolition were associated with less perceived social support, r(38) = −.42, p < .01 and higher levels of loneliness, r(38) = .55, p < .001.
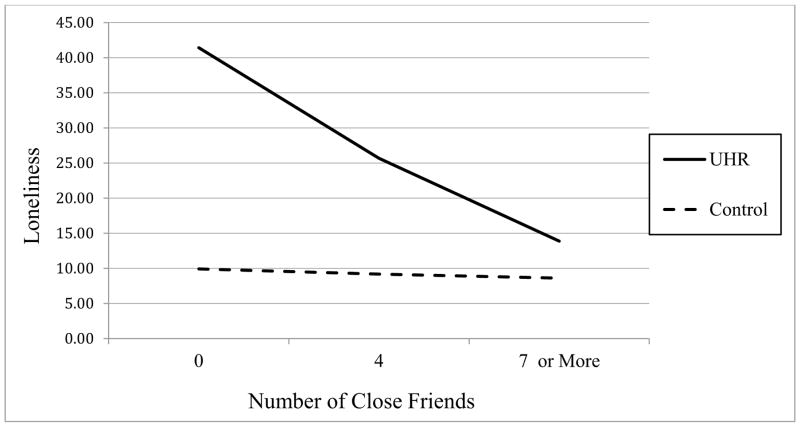
After adjusting for the component terms, the Number of Friends × Group interaction term was significantly associated with loneliness, t(74) = 2.86, p = .006. To evaluate the nature of this interaction, we plotted the predicted values of loneliness based on number of friends separately for UHR and control participants (see Figure 1). Analyses of simple slopes indicated that the number of friends was significantly and negatively associated with loneliness for the UHR group (B = −3.94, SE =.87, p < .001), whereas the number of friends was not significantly associated with loneliness in the control group (B = −.19 SE =.98, p = .85).
Figure 1.
Interaction Between Number of Close Friends and Condition Predicting Loneliness
4. Discussion
Results from this study of UHR adolescents and age-matched non-psychiatric controls provided support for our hypothesis that UHR participants have poorer social networks than healthy controls across a variety of measures. Specifically, relative to controls, UHR participants reported having fewer close friends and less diverse social networks, less availability of social support, less positive and more negative relationships with family members and friends, and higher levels of loneliness. The differences between the groups were quite striking for most of the social variables and demonstrated medium (i.e., d > .50) and large effect sizes (i.e., d > .80). In addition within the UHR sample, those with poorer social relationships had higher positive and negative symptoms and poorer overall functioning. Last, our exploratory analyses showed that social anhedonia and avolition were associated with a variety of social variables; specifically, less perceived social support and more loneliness. Interestingly, social anhedonia was associated with all of the social variables except family support and strain. Surprisingly, higher levels of social anhedonia was associated with less friend strain. Taken together, these findings provide an important and novel picture of the social relationships of UHR youth. This is the first study to our knowledge to evaluate so many aspects of the social relationships of UHR youth and demonstrates that UHR youth differ from controls not only in the size but also in the effectiveness of their social networks in providing support, availability of companionship, and protection from loneliness.
We also found that the strength of the negative association between number of close friends and loneliness depended on whether the participant was a UHR or a control young adult. Contrary to our hypothesis, UHR participants seemed to be more sensitive to the number of their friends, as number of friends was strongly associated with loneliness in UHR participants but was unrelated to loneliness for the controls. Controls reported very low levels of loneliness even when they had very few friends and UHR youth reported higher levels of loneliness even when they had many close friends compared to controls. This finding suggests that UHR youth may be more vulnerable to feeling lonely no matter how many friends they have, but are especially at risk if they have few close friends compared to healthy controls. In addition, for the UHR youth having even one or two friends was associated with lower levels of loneliness, although loneliness scores were never as low as controls.
The results of this study are consistent with past research on the social functioning of individuals with first episode psychosis (Erickson et al., 1989; Horan et al., 2006; Macdonald et al., 2000), UHR individuals (Cornblatt et al., 2003; Pruessner et al., 2011), and individuals with schizophrenia (Angell and Test, 2002; Goldberg et al., 2003). Specifically, people with schizophrenia have fewer and poorer quality social relationships than controls and those with the worst social networks have the most severe negative and positive symptoms and poorest quality of life (Bengtsson-tops and Hansson, 2001). Individuals who have experienced their first episode of psychosis tend to have fewer friends than controls (Erickson et al., 1989) and are more isolated and withdrawn than most individuals their age (Moller and Husby, 2003). Also consistent with past studies, the current study found that lower levels of social support were associated with higher levels of positive and negative symptoms (Domínguez-Martínez et al., 2015; Norman et al., 2005; Pruessner et al., 2011) and lower levels of functioning (Pruessner et al., 2011).
Although the results of this study clearly link poor social relationships and worse symptom severity and functioning in UHR youth, it is impossible to make a conclusion about the directionality of this association. UHR youth with more symptoms and poorer overall functioning may have difficulty forming and maintaining social relationships, leading to poorer social functioning. Alternatively, poor quality social relationships may be stressful to UHR youth, increasing the likelihood of symptoms and resulting in poorer functioning. Because UHR youth report poorer social functioning relative to controls, they may be more susceptible to the adverse effects of stress as proposed by the stress-buffering model. This model proposes that social support reduces the negative consequences of stressful events that are damaging to health (Cohen and Wills, 1985). Social networks help reduce the physical and emotional consequences of stressful life events by providing emotional and instrumental support. In addition, high levels of perceived and actual social support reduce one’s negative appraisal, negative reaction, and physiological stress responses to current and potential future stressful events (Cohen and Wills, 1985). For UHR individuals, the stress-buffering hypothesis may serve as a helpful explanatory framework for understanding the associations between social functioning and symptom severity, given some preliminary evidence that social dysfunction may predate symptom presentation (Erickson et al., 1998; Horan et al., 2006) and that poor peer relationships are common in children who will later develop schizophrenia (Meyer et al., 2005). Social relationships may act as a protective factor against the stressful experience of the first manifestation of positive and negative symptoms during the UHR period. Future longitudinal studies should aim to more directly test this hypothesis by examining the chronology of the appearance of symptoms and social relationship problems and whether the association between stress and symptom severity and functioning is moderated by social relationship variables. In addition, future studies should also determine if associations between relationship variables and symptoms and functioning are mediated by anhedonia and avolition given that they were also associated with many of the relationship variables.
The results of this study suggest that UHR youth tend to have poor quality relationships, feel unsupported, and be lonely. As a result, improving social relationships may be an important target for intervention. Even if interventions that aim to increase the quantity and quality of social relationships do not improve symptoms, they may be highly beneficial in improving the quality of life of UHR youth. In addition, past studies provide evidence that relationship interventions can be beneficial in many domains. For example, investigations examining family interactions suggest that interventions to improve family relationships can be effective in reducing symptom severity and improving functioning (O’Brien et al., 2008). Harrop et al. (2014) also advocate for the development and implementation of friend interventions for UHR individuals. This recommendation is especially important given the few and poor quality friend relationships observed in this study and past findings that worse symptoms are often associated with higher proportions of providers and family members in UHR social networks compared to friends (Erickson et al., 1989; Macdonald et al., 2000).
The results of this study should be interpreted with a few limitations in mind. Specifically, the study design was correlational and not longitudinal, so the direction of causation cannot be determined. As a result, it is equally as plausible that symptoms and improve overall functioning lead to poor social relationships as that social relationships are protective and decrease symptom severity and overall functioning. Future studies should examine these variables in a longitudinal design. In addition, future longitudinal studies should investigate whether having fewer relationships is truly harmful or is in someway protective for UHR individuals who may be trying to reduce stress and stimulation during a vulnerable time period.
Another limitation of the study is the relatively small sample size. This may have resulted in several of the associations obtained from the regression analyses not reaching conventional levels of statistical significance despite their medium effect sizes. Additionally, people with any current Axis I disorders were excluded from the control group, and even though the sample did have a significant amount of variability in social network composition (see Table 2) and some lifetime disorders (3 with major depressive disorder, 1 with generalized anxiety disorder, 1 with alcohol abuse, and 1 with alcohol dependence), this exclusion criterion may have created a fairly high functioning control group. As a result, it would be informative for future studies to include a less tightly controlled control group and a clinical control group to compare individuals with similar comorbidities, such as depression, but without being at risk of developing psychosis.
In conclusion, the results of this study suggest that relative to the control group, UHR youth have poorer social networks and tend to feel unsupported and lonely. In addition, poorer functioning in social relationships was associated with higher symptom severity and poorer overall functioning. Future studies should continue to examine multiple aspects of social relationships to gain a more comprehensive picture of what is going awry for young adults at risk for developing psychosis and ways interventions can improve outcomes for these individuals.
Supplementary Material
Highlights.
UHR young adults have fewer and poorer social relationships and are lonelier.
Poorer social relationships associated with more positive and negative symptoms.
Poorer social relationships associated with poorer functioning.
Negative association between number of friends and loneliness in UHR and no association in controls.
Acknowledgments
This work was supported by National Institutes of Health Grants R01MH094650 and R21/R33MH103231.
Conflicts of interest: Dr. Mittal is a consultant to Takeda. No other authors have any disclosures
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angell B, Test MA. The relationship of clinical factors and environmental opportunities to social functioning in young adults with schizophrenia. Schizophr Bull. 2002;28:259–271. doi: 10.1093/oxfordjournals.schbul.a006936. [DOI] [PubMed] [Google Scholar]
- Bengtsson-tops A, Hansson L. Quantitative and qualitative aspects of the social network in schizophrenia patients living in the community. Relationship to sociodemographic characteristics and clinical factors and subjective quality of life. Int J Soc Psychiatry. 2001;47:67–77. doi: 10.1177/002076400104700307. [DOI] [PubMed] [Google Scholar]
- Blakemore SJ. The social brain in adolescence. Nat Rev Neurosci. 2008;9:267–277. doi: 10.1038/nrn2353. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Mueser KT, Bellack AS, Journals PP. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Psychology. 1998:413–424. doi: 10.1093/oxfordjournals.schbul.a033336. [DOI] [PubMed] [Google Scholar]
- Brookings JB, Bolton B. Confirmatory factor analysis of the interpersonal support evaluation list. Am J Community Psychol. 1988;16:137–147. doi: 10.1007/BF00906076. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, TED Quality of life across the schizotypy spectrum: findings from a large nonclinical adult sample. Compr Psychiatry. 2009;50:408–414. doi: 10.1016/j.comppsych.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. JAMA. 1997;277:1940–1944. doi: 10.1001/jama.278.15.1231b. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13:99–125. doi: 10.1111/j.1559-1816.1983.tb02325.x. [DOI] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason Irwin G, Sarason Barbara R., editors. Social Support: Theory, Research and Applications. Springer; Netherlands: 1985. pp. 73–94. [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- Collins WA. More than Myth: The developmental significance of romantic relationships during adolescence. J Res Adolesc. 2003;13:1–24. doi: 10.1111/1532-7795.1301001. [DOI] [Google Scholar]
- Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, Cannon TD. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Lencz T, Smith CW, Correll CU, Auther AM, Nakayama E. The schizophrenia prodrome revisited: A neurodevelopmental perspective. Schizophr Bull. 2003;29:633–651. doi: 10.1093/oxfordjournals.schbul.a007036. [DOI] [PubMed] [Google Scholar]
- Dickey CC, Mccarley RW, Niznikiewicz MA, Voglmaier MM, Seidman LJ, Kim S, Shenton ME. Clinical, cognitive, and social characteristics of a sample of neuroleptic-naive persons with schizotypal personality disorder. 2005;78:297–308. doi: 10.1016/j.schres.2005.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domínguez-Martínez T, Kwapil TR, Barrantes-Vidal N. Subjective quality of life in at-risk mental state for psychosis patients: relationship with symptom severity and functional impairment. Early Interv Psychiatry. 2015;9:292–299. doi: 10.1111/eip.12111. [DOI] [PubMed] [Google Scholar]
- Erickson DH, Beiser M, Iacono WG. Social support predicts 5-year outcome in first-episode schizophrenia. J Abnorm Psychol. 1998;107:681–685. doi: 10.1037//0021-843x.107.4.681. doi.apa.org/journals/abn/107/4/681.pdf. [DOI] [PubMed] [Google Scholar]
- Erickson DH, Beiser M, Iacono WG, Fleming Ja, Lin TY. The role of social relationships in the course of first-episode schizophrenia and affective psychosis. Am J Psychiatry. 1989;146:1456–1461. doi: 10.1176/ajp.146.11.1456. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) American Psychiatric Press, Inc; Washington, DC: 1996. [Google Scholar]
- Friedlmeier W, Granqvist P. Attachment transfer among Swedish and German adolescents: A prospective longitudinal study. Pers Relatsh. 2006;13:261–279. doi: 10.1111/j.1475-6811.2006.00117.x. [DOI] [Google Scholar]
- Garnefski N, Diekstra RFW. Perceived social support from family, school, and peers: Relationship with emotional and behavioral problems among adolescents. Psychiatry. 1996;35:1657–1664. doi: 10.1097/00004583-199612000-00018. [DOI] [PubMed] [Google Scholar]
- Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol Psychiatr Sci. 2013;22:131–146. doi: 10.1017/S2045796012000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg RW, Rollins AL, Lehman AF. Social network correlates among people with psychiatric disabilities. Psychiatr Rehabil J. 2003;26:393–402. doi: 10.2975/26.2003.393.402. [DOI] [PubMed] [Google Scholar]
- Harrop C, Ellett L, Brand R, Lobban F. Friends interventions in psychosis: a narrative review and call to action. Early Interv Psychiatry. 2014 doi: 10.1111/eip.12172. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Social factors in schizophrenia. Curr Dir Psychol Sci. 2010;19:238–242. doi: 10.1177/0963721410377597. [DOI] [Google Scholar]
- Horan WP, Subotnik KL, Snyder KS, Nuechterlein KH. Do recent-onset schizophrenia patients experience a “social network crisis”? Psychiatry. 2006;69:115–129. doi: 10.1521/psyc.2006.69.2.115. [DOI] [PubMed] [Google Scholar]
- Hultman CM, Ohlund LS, Wieselgren IM, Ohman a, Ost LG. Electrodermal activity and social network as predictors of outcome of episodes in schizophrenia. J Abnorm Psychol. 1996;105:626–636. doi: 10.1037//0021-843x.105.4.626. [DOI] [PubMed] [Google Scholar]
- MacCabe JH, Koupil I, Leon DA. Lifetime reproductive output over two generations in patients with psychosis and their unaffected siblings: the Uppsala 1915–1929 Birth Cohort Multigenerational Study. Psychol Med. 2009;39:1667–1676. doi: 10.1017/s0033291709005431. [DOI] [PubMed] [Google Scholar]
- Macdonald EM, Hayes RL, Baglioni aJ. The quantity and quality of the social networks of young people with early psychosis compared with closely matched controls. Schizophr Res. 2000;46:25–30. doi: 10.1016/S0920-9964(00)00024-4. [DOI] [PubMed] [Google Scholar]
- Malmberg A, Lewis G, David A, Allebeck P. Premorbid adjustment and personality in people with schizophrenia. Br J Psychiatry. 1998;172:308–313. doi: 10.1192/bjp.172.4.308. [DOI] [PubMed] [Google Scholar]
- Meyer SE, Bearden CE, Lux SR, Gordon JL, Johnson JK, O’Brien MP, Niendam TA, Loewy RL, Ventura J, Cannon TD. The psychosis prodrome in adolescent patients viewed through the lens of DSM-IV. J Child Adolesc Psychopharmacol. 2005;15:434–51. doi: 10.1089/cap.2005.15.434. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Woods SW, Stein K, Driesen N, Corcoran CM, Hoffman R, Davidson L. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70:273–287. doi: 10.1023/a:1022034115078. [DOI] [PubMed] [Google Scholar]
- Mittal VA, Tessner KD, Walker EF. Elevated social Internet use and schizotypal personality disorder in adolescents. Schizophr Res. 2007;94:50–57. doi: 10.1016/j.schres.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moller P, Husby R. The initial prodrome in schizophrenia: Searching for naturalistic core dimensions of experience and behavior. Schizophr Bull. 2003;26:217–232. doi: 10.1093/oxfordjournals.schbul.a033442. [DOI] [PubMed] [Google Scholar]
- Norman RMG, Malla AK, Manchanda R, Harricharan R, Takhar J, Northcott S. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. 2005;80:227–234. doi: 10.1016/j.schres.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Norman RMG, Windell D, Manchanda R, Harricharan R, Northcott S. Social support and functional outcomes in an early intervention program. Schizophr Res. 2012;140:37–40. doi: 10.1016/j.schres.2012.07.003. [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, Cannon TD. Decreases in perceived maternal criticism predict improvement in subthreshold psychotic symptoms in a randomized trial of family-focused therapy for individuals at clinical high risk for psychosis. J Fam Psychol. 2015;29:945–51. doi: 10.1037/fam0000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Zinberg JL, Bearden CE, Lopez SR, Kopelowicz A, Daley M, Cannon TD, Bertrando B. Parent attitudes and parent adolescent interaction in families of youth at risk for psychosis and with recent-onset psychotic symptoms. Early Interv Psychiatry. 2008;2:268–76. doi: 10.1111/j.1751-7893.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Palmier-Claus JE, Dunn G, Lewis SW. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42:1003–1012. doi: 10.1017/S0033291711001929. [DOI] [PubMed] [Google Scholar]
- Pruessner M, Iyer SN, Faridi K, Joober R, Malla AK. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res. 2011;129:29–35. doi: 10.1016/j.schres.2011.03.022. [DOI] [PubMed] [Google Scholar]
- Rueger SY, Malecki CK, Demaray MK. Relationship between multiple sources of perceived social support and psychological and academic adjustment in early adolescence: Comparisons across gender. J Youth Adolesc. 2009;39:47–61. doi: 10.1007/s10964-008-9368-6. [DOI] [PubMed] [Google Scholar]
- Russell D. UCLA loneliness scale version 3 (description of measure) J Pers Soc Psychol. 1996;39:3–4. [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: Concurrent and discriminate validity evidence. J Pers Soc Psychol. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Schorre BEH, Vandvik IH. Global assessment of psychosocial functioning in child and adolescent psychiatry: A review of three unidimensional scales (CGAS, GAF, GAPD) Eur Child Adolesc Psychiatry. 2004;13:273–286. doi: 10.1007/s00787-004-0390-2. [DOI] [PubMed] [Google Scholar]
- Strauss GP, Horan WP, Kirkpatrick B, Fischer BA, Keller WR, Miski P, Buchanan RW, Green MF, Carpenter WT. Deconstructing negative symptoms of schizophrenia: Avolition-apathy and diminished expression clusters predict clinical presentation and functional outcome. J Psychiatr Res. 2013;47:783–790. doi: 10.1016/j.jpsychires.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sündermann O, Onwumere J, Kane F, Morgan C, Kuipers E. Social networks and support in first-episode psychosis: exploring the role of loneliness and anxiety. Soc Psychiatry Psychiatr Epidemiol. 2014;49:359–366. doi: 10.1007/s00127-013-0754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen HR, Lachman ME. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. J Soc Pers Relat. 2000;17:5–30. doi: 10.1177/0265407500171001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.