Abstract
Lower extremity (LE) amputation patients who use prostheses have gait asymmetries and altered limb loading and movement strategies when ambulating. Subsequent secondary conditions are believed to be associated with gait deviations and lead to long-term complications that impact function and quality of life as a result. The purpose of this study was to systematically review the literature to determine the strength of evidence supporting gait training interventions and to formulate evidence statements to guide practice and research related to therapeutic gait training for lower extremity amputees. A systematic review of three databases was conducted followed by evaluation of evidence and synthesis of empirical evidence statements (EES). Eighteen manuscripts were included in the review, which covered two areas of gait training interventions: 1) overground and 2) treadmill-based. Eight EESs were synthesized. Four addressed overground gait training, one covered treadmill training, and three statements addressed both forms of therapy. Due to the gait asymmetries, altered biomechanics, and related secondary consequences associated with LE amputation, gait training interventions are needed along with study of their efficacy. Overground training with verbal or other auditory, manual, and psychological awareness interventions was found to be effective at improving gait. Similarly, treadmill-based training was found to be effective: 1) as a supplement to overground training; 2) independently when augmented with visual feedback and/or body weight support; or 3) as part of a home exercise plan. Gait training approaches studied improved multiple areas of gait, including sagittal and coronal biomechanics, spatiotemporal measures, and distance walked.
Keywords: Amputee, Physical therapy, Prosthesis, Rehabilitation, Therapeutic exercise, Trans-femoral, Transtibial, Treadmill
Introduction
In 2005, there were 1.6 million Americans with limb amputation(s) (1-3). Annually, 185,000 people experience upper or lower extremity (LE) limb loss for many reasons, including diabetic and vascular complications, trauma, and malignancy (1). Lower limb amputations represent ≈86% of all limb amputations, and ≈357,000 individuals experienced amputation at the transfemoral level (2). Ninety-five percent of transfemoral amputations (TFA) are attributable to vascular disease, and the remaining five percent are due to trauma, malignancy, and congenital limb deficiencies (2). Further, non-white males, specifically African Americans, Hispanics, and Native Americans, have increased risk of LE amputation (1,3). From 1979 to 1996, there were reportedly 70% more TFA patients and 46% more transtibial amputations (TTA) in males than females (4). Moreover, those older than 65 years of age experience 6.5 and 2.7 times the number of TFAs and TTAs, respectively, compared to those younger than 65 (4). By 2050, the number of Americans with amputations is expected to increase from 1.6 million to 3.6 million (1,3).
An individual with LE amputation may face increased mortality and morbidity rates, decreased quality of life, and impaired function (5). Impaired function may include gait problems such as movement asymmetry (6). Amputee gait impairments have been objectively documented in multiple domains, including spatiotemporal and biomechanical parameters as well as in terms of bioenergetics (7-9). Gait parameters potentially altered in LE amputees include changes in magnitude and symmetry of forces and joint moments, event duration, and others (6). These deviations may contribute to decreased balance and increased metabolic costs as well as more insidious chronic issues, potentially including degenerative joint disease for example (6). TFA patients are impaired relative to non-amputees due to the lack of muscles controlling their knees. TFA patients depend on a prosthetic knee joint that, despite technological advancements and functional improvements, limits function to some degree (10). The TFA gait pattern is described as having shorter stance and longer swing phases on the prosthetic side. Additionally, their gait speed and ability to change speed are also impaired (7,11). Gait patterns of LE amputees may also include lateral trunk flexion toward the prosthetic side secondary to weak hip abductors or decreased balance caused by socket instability and discomfort. Moreover, the TFA gait pattern may also include vaulting to assure prosthetic limb clearance during swing phase. The abnormalities of lateral trunk flexion and forces from vaulting may be contributing factors in the development of back pain, osteoarthritis, or other chronic overuse conditions (5,6,12,13). As previously mentioned, LE amputee gait impairments also include significantly increased ambulatory energy requirements, which may impact overall activity and participation (8,12,14).
Interventions to mitigate gait deviations and improve quality of life for LE amputees include prescribing the proper componentry and participating in physical therapy for gait training. For example, to manage TFA patients with gait deviations, an appropriate prosthesis needs to be prescribed. This includes the choice of socket type (15); knee type, such as non-microprocessor or microprocessor knee systems (MPK); and foot type to maximally benefit user lifestyle, budget, function, and quality of life. If patients frequently ascend and descend stairs in their homes and at work for instance, then perhaps an MPK that facilitates stair ambulation should be considered (16-18). There are numerous factors to consider when formulating the prosthetic prescription, including patient age, medical history, activity level, goals (e.g., functional, occupational, recreational, etc.), amputation length and level, strength, environments (e.g. home, work, recreational, etc.), aesthetic preference, and more. In addition to proper componentry, participation in physical therapy, including therapeutic exercise, neuromuscular re-education, and gait training, is beneficial for LE amputees to improve function and quality of life. Specifically, gait training reportedly improves spatiotemporal parameters, joint kinematics, and bioenergetic efficiency during gait for LE amputees (16,17,19). The purpose of this study was to systematically review the literature to determine the strength of evidence supporting gait training interventions and to formulate evidence statements to guide practice and research related to therapeutic gait training for LE amputees.
Methods
A multidisciplinary review team planned methodology in accordance with that used previously in prosthetic research (8) in addition to standards established by the Prisma Statement (20,21). Reviewers had graduate education or professional healthcare training in physical therapy or prosthetics. The team met on three occasions and outlined search methodology to include multiple databases and key search terms (primary and secondary) that would assure identification of available evidence to address gait training interventions for those with LE amputation. Search methodology was based upon a broad view of LE amputations with regard to gait training intervention. Preliminary test searches were conducted and outcomes previewed at pre-search meetings to assure adequate inclusion of key articles in terms of both quantity and quality within the topic of interest. The search statement was planned to be sensitive to include patients with LE amputation and gait training interventions. The search term sets sought to combine all levels of LE amputation with all forms of clinical gait training. Complete search term sets are listed in Table 1.
Table 1. Search Term Sets and Databases.
| Database | MEDLINE | CINAHL | Web of Science |
|---|---|---|---|
| General Search Term Set | Gait[mesh] OR gait[tiab] OR gait[ot] OR stride[tiab] OR stride[ot] OR treadmill* OR walk*[tiab] OR running OR step[tiab] OR steps[tiab] OR stair* OR ramp[tiab] OR ambulat* OR balance[tiab] OR balance[ot] OR climb* OR slope OR “functional training” | (MH “Walking+”) OR gait OR step OR walk OR running OR stair* OR (MH “Stair Climbing”) OR ramp OR ambulat* OR balance OR climb* OR slope OR (MH “Functional Training”) | Gait OR stride OR treadmill* OR walk* OR running OR step OR steps OR stair*OR ramp OR ambulat* OR balance OR climb* OR slope OR “functional training” |
| Amput* String | (((((“Lower
Extremity”[Mesh] OR lower
extrem*[TIAB] OR lower extrem*[OT] OR
lower limb*[TIAB] OR lower limb*[OT]
OR leg[TIAB] OR leg[OT] OR legs[TIAB]
OR legs[OT] OR hip[TIAB] OR hip[OT] OR
hips[TIAB] OR hips[OT] OR
thigh*[TIAB] OR thigh*[OT] OR
foot[TIAB] OR foot[OT] OR feet[TIAB]
OR feet[OT] OR “Knee Joint”[Mesh] OR
knee[TIAB] OR knee[OT] OR knees[TIAB]
OR knees[OT] OR “Ankle Joint”[Mesh] OR
ankle*[TIAB] OR ankle*[OT] OR
“Femur”[Mesh] OR femur*[TIAB]
OR femur*[OT] OR transfemoral[TIAB] OR
transfemoral[OT] OR transfemoral[TIAB] OR
transfemoral[OT] OR “Tibia”[Mesh] OR
tibia*[TIAB] OR tibia*[OT] OR
transtibial[TIAB] OR transtibial[OT] OR
trans-tibial[TIAB] OR trans-tibial[OT] OR
transpelvic[TIAB] OR transpelvic[OT] OR
trans-pelvic[TIAB] OR trans-pelvic[OT] OR
syme's[TIAB] OR syme's[OT] OR
symes[TIAB] OR
symes[OT]))) AND ((“Amputation”[Mesh] OR amput*[TIAB] OR amput*[OT] OR disarticulat*[TIAB] OR disarticulat*[OT] OR hemipelvectom*[TIAB] OR hemipelvectom*[OT] OR “Amputees”[Mesh] OR “Amputation Stumps”[Mesh] OR “Artificial Limbs”[Mesh] OR artificial limb*[TIAB] OR artificial limb*[OT] OR “Amputation, Traumatic”[Mesh] OR “Prostheses and lmplants”[Mesh:noexp] OR residual limb*[TIAB] OR residual limb*[OT] OR limb loss*[TIAB] OR limb loss*[OT] OR prosthe*[TIAB] OR prosthe*[OT] OR stump*[TIAB] OR stump*[OT])))) |
((MH “Lower Extremity+”) OR (Tl
lower extrem* OR AB lower extrem*) OR (Tl lower limb* OR AB
lower limb*) OR (Tl leg OR AB leg) OR (Tl legs OR AB legs) OR (Tl hip OR AB
hip) OR (Tl hips OR AB hips) OR (Tl foot OR AB foot) OR (Tl feet OR AB feet) OR (MH
“Knee Joint+”) OR (Tl knee OR AB knee) OR (Tl knees OR AB
knees) OR (MH “Ankle Joint”) OR (Tl ankle* OR AB
ankle*) OR (MH “Femur+”) OR (Tl femur* OR AB
femur*) OR (Tl transfemoral OR AB transfemoral) OR (Tl trans-femoral OR AB
trans-femoral) OR (MH “Tibia”) OR (Tl tibia* OR AB
tibia*) OR (Tl transtibial OR AB transtibial) OR (Tl trans-tibial OR AB
trans-tibial) OR (Tl transpelvic OR AB transpelvic) OR (Tl trans-pelvic OR AB
trans-pelvic) OR (Tl syme's OR AB syme's) OR (Tl symes OR AB symes) OR
(Tl thigh* OR AB thigh*)) AND ((MH “Amputation+”) OR (Tl amput* OR AB amput*) OR (Tl disarticulat* OR AB disarticulat*) OR (Tl hemipelvectom* OR AB hemipelvectom*) OR (MH “Amputees”) OR (MH “Amputation, Traumatic”) OR (MH “Limb Prosthesis”) OR (Tl prosthe* OR AB prosthe*) OR (Tl artificial limb* OR AB artificial limb*) OR (Tl limb loss OR AB limb loss) OR (Tl residual limb* OR AB residual limb*) OR (Tl stump* OR AB stump*) OR (MH “Prostheses and Implants”)) |
(Lower AND (extremit* OR limb*)) OR leg OR
legs OR hip OR hips OR foot OR feet OR thigh* OR knee OR knees OR
ankle* OR femur OR transfemoral OR trans-femoral OR tibia* OR
transtibial OR trans-tibial OR transpelvic OR transpelvic OR syme's OR
symes AND amput* OR disarticulat* OR hemipelvectom* OR artificial Limb* OR residual limb* OR prosthe* OR stump* |
On December 15, 2014, the following databases were searched: 1.) MEDLINE (Pubmed), 2.) the Cumulative Index to Nursing and Allied Health Literature (CINAHL)(Ovid), and 3.) Web of Science. The following date limits were implemented as part of the database search parameters: 2000 Jan 1 to 2014 Dec 14. One month after the initial search, the search was repeated by a pair of separate information scientists.
Article Screening
Resulting references were exported to EndNote (vX6, Thompson, CA, USA) reference management software. Duplicate references were eliminated. Remaining articles were preliminarily sorted by article type. Exclusion criteria were selected to eliminate manuscripts that did not include gait training for adults with LE amputation who used prostheses. Foreign language articles were eliminated relative to prohibitive costs associated with translation. Manuscripts were screened for exclusion using the following initial criteria within EndNote:
Foreign language (i.e., non-English language)
Non-human subject (i.e., materials science, finite element studies)
Pediatric studies
Following the EndNote search using the aforementioned exclusion criteria, remaining intervention articles were divided up equally between reviewers. Each article was assigned a primary and secondary reviewer. The reviewers independently screened references according to inclusion/exclusion criteria and classified them as either: 1) pertinent, 2) not pertinent or 3) uncertain pertinence. Full-text articles were reviewed for all citations classified as pertinent or uncertain pertinence. Disagreement regarding citations of uncertain pertinence were resolved by discussion at weekly follow-up meetings with the two other reviewers. Review of full-text articles and associated discussion led to group consensus and ultimate inclusion/exclusion. Exclusion criteria applied during the EndNote search were applied at this stage of screening. Inclusion criteria applied were:
Peer-reviewed manuscript
Gait training intervention for LE Amputees
Published within the aforementioned timeline
Quality Assessment
Evaluation of Internal and External Validity
Methodological quality of included publications was independently assessed by two reviewers according to the American Academy of Orthotists and Prosthetists (AAOP) State-of-the-Science Evidence Report Guidelines protocol (22). The AAOP Study Design Classification Scale was used to describe the design type of included studies (22). The State of the Science Conference (SSC) Quality Assessment Form was used to rate the methodological quality of studies classified as experimental (E1 to E5) or observational (O1 to O6) (22). The form identifies 18 potential threats to internal validity, with the first four threats not applicable for study classifications E3 to E5 and the first five threats not applicable for classifications O1 to O6. Threats to validity were evaluated and tabulated. The internal and external validity of each study was then subjectively rated as “high,” “moderate,” or “low” based on the quantity and importance of threats present. For internal validity, 0 to 3 threats was rated “high,” 4 to 6 threats as “moderate,” and 7 to 13 or 14 threats as “low.” For external validity, the form identifies eight threats. For this study, 0 to 2 threats to external validity was rated “high,” 3 to 5 threats as “moderate,” and 6 to 8 threats as “low.” Each study was then given an overall quality of evidence of “high,” “moderate,” or “low” as outlined by the AAOP State-of-the-Science Evidence Report Guidelines (22).
Following the quality assessment of each study, key data (e.g., demographic, anthropometric, outcomes, etc.) were extracted to assist in describing the studied subjects, interventions, and their relative effects. Overall ratings from the AAOP State-of-the-Science Evidence Report Guidelines were used to assign the level of confidence for the developed empirical evidence statements (EES) described in the following section.
Empirical Evidence Statements
Based on results from the included publications, EESs were developed that described study findings related to gait training interventions for LE amputees. Reviewers rated the level of confidence of each EES as “high,” “moderate,” “low,” or “insufficient” based on the number of publications contributing to the statement, the methodological quality of those studies, and whether the contributing findings were confirmatory or conflicting as similarly outlined by others (23). These levels of evidence were somewhat adjustable in accordance with study quality, effect size, and other factors.
Analysis
Data pooling (i.e., meta-analyses) was conducted when homogeneous data were available. When data pooling was possible, mean difference with 95% confidence interval was calculated and significance determined a priori to be p ≤ 0.05 (24).
Sorting by Topic
Following procedures for screening and eligibility determination, full-text articles were sorted by reviewers into sub-topical areas.
Results
Literature Search, Sub-topics, and Study Designs
The search yielded 11,118 total manuscripts (Figure 1). Following screening, 11,100 manuscripts were eliminated, leaving 18 articles that met eligibility criteria. The 18 remaining articles, published from 2001 to 2014, were divided into two topical areas:
Figure 1.
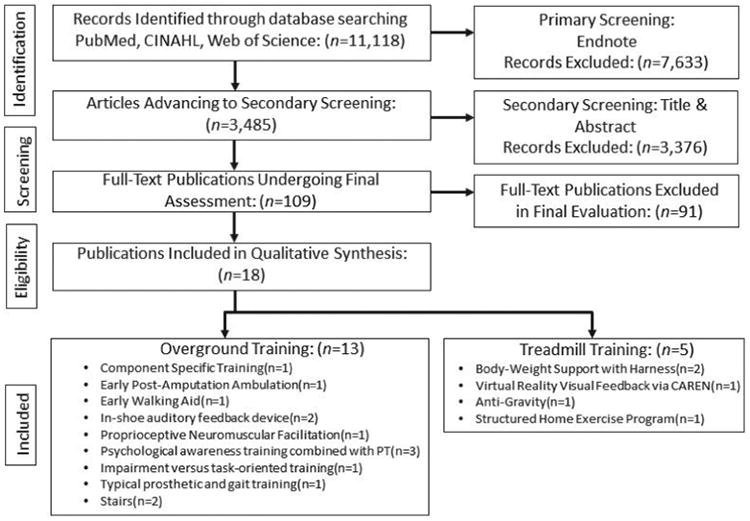
Study flow diagram.
The two most represented journals were Prosthetics and Orthotics International (six publications) and the Journal of Prosthetics and Orthotics (three publications). All other journals had a single publication, and the group included a dissertation.
In terms of study design (22), the case study was most represented (n = 5). There were 11 experimental studies and two expert opinion manuscripts (Table 2). None of the included studies had an economic analytic component.
Table 2. Distribution of Included Studies by Study Design.
| Study Design | Number of Publications |
|---|---|
| Meta-Analysis (S1) | 0 |
| Systematic Review (S2) | 0 |
| Randomized Control Trial (E1) | 3 |
| Controlled Trial (E2) | 1 |
| Interrupted Time Series Trial (E3) | 3 |
| Single Subject Trial (E4) | 0 |
| Controlled Before and After Trial (E5) | 4 |
| Cohort Study (O1) | 0 |
| Case-Control Study (O2) | 0 |
| Cross Sectional Study (O3) | 0 |
| Qualitative Study (O4) | 0 |
| Case Series (O5) | 0 |
| Case Study (O6) | 5 |
| Group Consensus (X1) | 0 |
| Expert Opinion (X2) | 2 |
|
| |
| Total | 18 |
Funding
Eight of the 18 included studies (40%) were unfunded. Local government supported four (20%) of the studies. Industry and the U.S. National Institutes of Health each funded 10% of this research. The remaining studies were sponsored by a university, a hospital system, a non-profit organization, or the U.S. Department of Defense. Bias risk from a research funding perspective was considered low given that only 10% of the research was funded by industry, with the majority being either unfunded or government sponsored.
Study Demographics, Interventions, and Outcome Measures
Conclusions from this systematic review are drawn from 229 subjects (Table 3). Some subjects represent single projects in multiple manuscripts (11,27,28). A total of 145 persons with lower limb amputation served as experimental subjects. Their mean (interquartile range (IQR), range) age, height, and mass were: 48.2 years (29.5, 31 to 85), 1.7 m (0.04, 1.7 to 1.8), and 80.6 kg (10.3, 67.4 to 99.3). There were 66 amputees who served as control subjects. Their mean (IQR, range) age, height, and body mass were: 48.7 years (27.8, 28 to 66), 1.7 m (0.03, 1.7 to 1.76), and 73.2 kg (5.4, 68 to 82). Eighteen lower limb amputee subjects served as their own controls in cross-over design studies. Finally, an additional 18 non-amputees served as controls with a mean age of 35.8 years, height of 1.7 m, and mass of 72.5 kg. The etiology for amputation was comparable between traumatic and dysvascular cases and included some malignancy cases. In terms of level of amputation, 57% of the sample had TFA level amputation, 21% had TTA, 21% were mixed lower extremity samples, and 1% were bilaterally involved. Time since amputation was 5.9 years (9.2, 0.3 to 25.5). The median (mean, IQR, range) sample size was n = 9 (14, 20, 1 to 50).
Table 3. Extracted Study Data.
| Author (Yr) | N | Treatment (Independent Variables) | Treatment Duration | Conclusions |
|---|---|---|---|---|
| Agrawal et al. (2013) | 10 | SACH, SAFE, Talux, Proprio; Foot type specific training | 1-4 h × 10-14 d accommodation period/foot | SEW improved in K2 amputees trained to use K3 prosthetic feet. |
| Barnett et al. (2009) | 15 | Pneumatic Post-Amputation Aid; Amputee Mobility Aide | Individual need; Rehab duration 78.1 ± 25.3 (40–126) d | Gait adaptation occurred w/ functional prosthesis. Unclear benefit at d/c after using either EWA. |
| Black et al. (2006)‡ | 1 | 50-60% BWSTT at 1.0-1.6m ph | 2×/wk × 8 sessions × 4.5 wks | Partial BWSTT improved speed & gait pattern. |
| Darter et al. (2013)‡ | 8 | 30 min home-based TM training | 3×/wk × 8 wks | Home TM training improved TFA gait. Consider use after initial rehab. |
| Darter et al. (2011)‡ | 1 | Visual feedback via CAREN VR system & verbal PT feedback | 12 × 30 min sessions × 3 wks | 12 sessions w/ real-time feedback improved TFA gait. Clinically important changes in biomechanics & VO2. |
| Isakov et al. (2006) | 42 | In-shoe BW measurement w/ audio feedback; PT feedback for FWB | 4 × 30 m in sessions × 14 d | Pts improved WB thru PL w/ auditory feedback device. |
| Lamberg et al. (2014)*‡ | 8 | BWSTT (30% BWS), gradually ↓ by 5% intervals; TM w/out support | 12 × 30 min sessions; 3×/wk | TM training maximizing walk time improved function years post-amputation regardless of training mode. |
| Mikami et al. (2014)‡ | 1 | Anti-gravity TM training | 20-40 min; 3×/wk × 2 wks | Anti-gravity TM useful for TTA rehab. |
| Sjodahl et al. (2001) | 9 | Psychological awareness training & PT | 1×/wk × 10 mos (range 7-14) | Combined psychological & PT improved TFA gait. |
| Sjodahl et al. (2002) | 27 | Training improved gait speed, pattern, symmetry. Intact knee flex/loading differed from reference side. | ||
| Sjodahl et al. (2003) | 27 | Pts w/ >2 y prosthetic use improved gait (emphasized prox. muscle strength & stability; balance & coord. | ||
| Yang et al. (2012) | 3 | In-shoe audio feedback device | 6 × 30 min sessions × 3 wks | LEAFS improved trunk sway & gait symmetry. |
| Cole et al. (2003) | 1 | Typical gait training pgm w/verbal tactile cues, varying surfaces | 12 sessions | Gait training improves functional independence & community integration. |
| Faucher et al. (2005) | 1 | WB & amb on post-op day 1 | 10d | Trauma teams should remain aware of this option. |
| Highsmith et al. (2012) | 19 | Reciprocal stair descent training for stance yielding knees | NR | Training may improve stumble recovery, STS & loading response. |
| Hyland et al. (2009)* | 22 | Grps: Impairment vs. Task Oriented | 10d | Both strategies equally improve TTA mobility. Function improved in 10 d protocol. |
| Yigiter et al. (2002) | 50 | PNF; Traditional training | 30 min/d ×10 sessions | PNF improved LEA balance, weight acceptance & gait. |
| Highsmith et al. (2014) | 20 | Genium knee stair ascent/ramp training | NR | Ramp/stair training may improve overall function & safety. |
High overall quality score. All other studies were Moderate quality.
Denotes a treadmill training study.
All other studies used overground gait training. BWSTT: body weight supported treadmill training. BWS: body weight support. BW: body weight. NR: not reported. EWA: early walk aid. FWB: full weight bearing. LEA: lower extremity amputee. MPH: miles/hour. TM: treadmill. CAREN: computer assisted rehabilitation environment. WB: weight bearing. PT: physical therapy. Amb: ambulation. LEAFs: lower extremity feedback system. Grp: group. PNF: proprioceptive neuromuscular facilitation. SEW: symmetry of external work. SSWS: self-selected walking speed. STS: sit to stand. TTA: transtibial amputee.
Outcome measures assessed included symmetry of external work, spatiotemporal measures, biomechanical and bioenergetic outcomes, level of assist with functional tasks (i.e., sit to stand, stair climbing ability), walking test performance, ambulatory weight bearing, clinical performance measures (i.e., timed up and go test), perceptive measures (i.e., Activities-specific Balance Confidence Scale, general self-efficacy scale), and performance against patient goals. Due to the varied levels of amputation, methods of data collection, training, and other factors, aggregation of data and meta-analysis were not possible.
Internal and External Validity
Threats to internal validity included lack of intervention blinding, inadequate reporting of eligibility criteria, and failure to include statistical analyses (i.e., expert opinions, editorials) (Table 4). Ten studies had low, six had moderate, and two had high internal validity. Conversely, sixteen studies had high and two had moderate external validity according to the AAOP rating tool (Table 5).
Table 4. Internal Validity Assessment of Included Manuscripts.
| Year | Author | Study Classification | Control group used | Randomization | Groups comparable at baseline | Similar group treatment | Comparison Group appropriate | Interventions blinded | Inclusion criteria appropriate | Exclusion criteria appropriate | Addresses fatigue & learning | Accommodation & washout | Attrition explained & <20% | Attrition equal | Outcome measures reliable | Proper statistical analysis | Effect size reported | Statistical significance | Statistical power adequate | Free from conflicts of interest | Total # threats | Overall assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | Sjodahl et al. | E5 | • | • | • | • | • | • | 8 | Low | ||||||||||||
| 2002 | Sjodahl et al. | E5 | • | • | • | • | • | • | • | • | • | 5 | Mod | |||||||||
| 2002 | Yigiter et al. | E1 | • | • | • | • | • | • | • | • | • | • | • | • | • | 4 | Mod | |||||
| 2003 | Sjodahl et al. | E5 | • | • | • | • | • | • | • | • | • | • | 4 | Mod | ||||||||
| 2003 | Cole et al. | O6 | • | • | • | • | • | 7 | Low | |||||||||||||
| 2005 | Faucher et al. | O6 | • | • | • | • | • | 7 | Low | |||||||||||||
| 2006 | Black et al. | O6 | • | • | • | • | 9 | Low | ||||||||||||||
| 2006 | Isakov et al. | E1 | • | • | • | • | • | • | • | 1 | Low | |||||||||||
| 2009 | Barnett et al. | E3 | • | • | • | • | • | • | • | • | • | • | • | 5 | Mod | |||||||
| 2009 | Hyland et al. | E1 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 2 | High | |||
| 2011 | Darter et al. | O6 | • | • | • | • | • | • | 7 | Low | ||||||||||||
| 2012 | Yang et al. | E5 | • | • | • | 11 | Low | |||||||||||||||
| 2012 | Highsmith et al. | X2 | • | • | 11 | Low | ||||||||||||||||
| 2013 | Agrawal et al. | E3 | • | • | • | • | • | • | • | • | • | • | • | 3 | Mod | |||||||
| 2013 | Darter et al. | E3 | • | • | • | • | • | • | • | • | • | • | 4 | Mod | ||||||||
| 2014 | Lamberg et al. | E2 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 2 | High | |||
| 2014 | Mikami et al. | O6 | • | • | • | 6 | Low | |||||||||||||||
| 2014 | Highsmith et al. | X2 | • | • | • | 1 | Low |
Boxes that are blacked out are not applicable for the specific study design and thus do not count as threats to validity. A dot in the box indicates the criteria was identified by reviewers whereas a blank box represents a criteria not identified
Table 5. External Validity Assessment of Included Manuscripts.
| Year | Author | Study Classification | Sample adequately described | Sample representative | Outcomes adequately described | Outcomes valid for the study | Intervention adequately described | Findings clinically significant | Conclusion placed in literary context |
Findings support conclusions | Number of Threats |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | Sjodahl et al. | E5 | • | • | • | • | • | • | • | 2 | |
| 2002 | Sjodahl et al. | E5 | • | • | • | • | • | • | • | • | 0 |
| 2002 | Yigiter et al. | E1 | • | • | • | • | • | • | • | • | 0 |
| 2003 | Sjodahl et al. | E5 | • | • | • | • | • | • | • | • | 0 |
| 2003 | Cole et al. | O6 | • | • | • | • | • | 3 | |||
| 2005 | Faucher et al. | O6 | • | • | • | • | • | • | 2 | ||
| 2006 | Black et al. | O6 | • | • | • | • | • | • | 2 | ||
| 2006 | Isakov et al. | E1 | • | • | • | • | • | • | • | 1 | |
| 2009 | Barnett et al. | E3 | • | • | • | • | • | • | 2 | ||
| 2009 | Hyland et al. | E1 | • | • | • | • | • | • | • | • | 0 |
| 2011 | Darter et al. | O6 | • | • | • | • | • | • | 2 | ||
| 2012 | Yang et al. | E5 | • | • | • | • | • | • | 2 | ||
| 2012 | Highsmith et al. | X2 | • | • | • | • | 4* | ||||
| 2013 | Agrawal et al. | E3 | • | • | • | • | • | • | • | • | 0 |
| 2013 | Darter et al. | E3 | • | • | • | • | • | • | • | • | 0 |
| 2014 | Lamberg et al. | E2 | • | • | • | • | • | • | • | • | 0 |
| 2014 | Mikami et al. | O6 | • | • | • | • | • | • | • | 1 | |
| 2014 | Highsmith et al. | X2 | • | • | • | • | 4* |
All manuscripts had high external validity except those noted with (*) which had moderate external validity. The three manuscripts by Sjodahl et al. represent a single project and are thus counted as a single “manuscript” for the purposes of this review and analysis. A dot in the box indicates the criteria was identified by reviewers whereas a blank box represents a criteria not identified.
Evidence Statements
Eight EESs were synthesized from the results within the two topical areas previously identified (Table 6). One of the statements was supported by a single study, resulting in an insufficient level of confidence. Four statements had two to four studies supporting their synthesis, resulting in low confidence. One statement was supported by four studies, yielding moderate confidence, and two statements were supported by sufficient evidence to provide high confidence. Four statements address overground gait training exclusively, one statement addresses treadmill gait training exclusively, and three statements address both overground and treadmill gait training.
Table 6. Evidence Statements, Levels of Evidence and Overall Confidence.
| Evidence Statement | Level of Evidence | Overall Confidence | |
|---|---|---|---|
| 1.† | Integration of psychological awareness training with a typical gait training program is effective at improving frontal and sagittal plane joint kinematics in unilateral transfemoral amputees. | Moderate (×2*)11,28 | Low |
| 2.† | Integration of an in-shoe, auditory feedback device into a typical gait training program is effective at improving involved-side loading in lower limb amputees. | Low (×2)6,26 | Low |
| 3.†‡ | Therapeutic overground or treadmill based gait training under skilled supervision is effective to improve spatiotemporal gait parameters in transfemoral and transtibial amputees. | Low (×5), Moderate (×3), High (×2)6,11,12,26,27,31-35 | High |
| 4.‡ | Following lower extremity amputation, bioenergetic efficiency of gait may be improved with treadmill based gait training augmented either by reduced loading, real-time visual feedback, or a structured home-based program. | Low (×2), Moderate (×1)12,33,36 | Low |
| 5.†‡ | Lower limb amputee gait training protocols including typical gait and prosthetic training procedures with verbal and tactile cues, ambulation on post-op day 1, and treadmill training with body weight unloading are effective to increase ambulatory distance with reduced assistance. | Low (×4)29,30,34,36 | Low |
| 6.† | Gait training utilizing verbal and manual cues to practice gait components prior to whole task initiation is an effective strategy to improve overground ambulation and stair negotiation in lower limb amputees. | Low (×3), High (×1)16,17,29,31 | Moderate |
| 7.† | Combining prosthetic component specific gait training with appropriate prosthetic foot prescription can promote higher external work symmetry in limited and unlimited community ambulating unilateral transtibial amputees. | Moderate (×1)37 | Insufficient |
| 8.†‡ | Therapeutic gait training programs under skilled supervision, that maximize time spent performing ambulatory activities beyond current functional daily walking, are safe and effective at improving walking function in lower limb amputees. | Low (×10), Moderate (×6), High (×2)6,11,12,16,17,19,26-37 | High |
Denotes overground gait training.
Denotes treadmill gait training.
Same study.
Discussion
The purpose of this study was to systematically review the literature to determine the current strength of evidence regarding different gait training methods for lower limb amputees and to formulate evidence statements to guide current practice and future research related to gait training for persons with lower limb amputation. This search revealed limited literature on the subject, which is consistent with a recently published systematic review that identified eight studies investigating the effectiveness of exercise programs to improve gait performance in lower limb amputees (37). The difference in the number of studies may be due to the other review (37) limiting included articles to one-group cohort, pre- to post-test studies, two-group case-control trials, and control trials, whereas this review included all publications, including expert opinions. Though publications are limited, our literature review supported our hypothesis that multiple gait training modalities are effective to improve overall gait quality in lower limb amputees. Generally, gait training was described in two major categories: traditional overground and treadmill-based training. Beyond this, the evidence supports general themes with regard to benefits of therapeutic gait training.
Funding, Subjects, and Outcomes
A high number of these studies were unfunded. This is not surprising, as it is less common for commercial parties to have an interest in sponsoring the development or study of new gait therapies. This is likely because gait training therapies commonly represent services rather than products. Therefore, packaging gait training services for a profit is difficult. The highest amount of funding in this review was from local government, which may likely be connected to academia by way of investigators' academic affiliations. This is especially surprising given that federal sponsors, such as the U.S. National Institutes of Health, have a mission to apply knowledge to enhance health, lengthen life, and reduce disability. This body of work demonstrates that gait training reduces disability. Clearly, more federal funding is needed to further enhance this body of gait training research in lower limb amputees.
Subjects in the included studies tended to be community ambulators of approximately 48 years of age who had lost their limbs to either trauma or vascular disease. Additionally, the cohort had a higher presence of transfemoral limb loss than other levels. These characteristics are a bit different than commonly cited epidemiologic studies, which describe most U.S. amputees as considerably older than 40 years and having lost their limbs to vascular disease, most likely at the transtibial level (1,38). These differences are not surprising given that transfemoral amputees may have greater impairment than more distal levels of amputation thus justifying heightened interest in gait training. Further, given that most subjects were community ambulators, it is feasible that the age and etiology would shift lower and toward trauma, respectively.
In terms of outcome measures, spatiotemporal, biomechanical, and bioenergetic measures are common and logical assessments to determine objectively if gait is improving following therapy. Problematically, these tend to be more research laboratory tools and less clinically oriented. Therefore, inclusion of observational gait scales and perceptive and functional measures may facilitate improved translation into the clinical setting.
Overground Gait Training
Of the articles included in this review, 13 included some form of overground gait training. Multiple therapeutic gait interventions, including in-shoe auditory feedback (6,26), verbal and tactile cues (16,17,25,29,31), PNF (19), component specific training (16,17,25), early weight-bearing (30), early walking aids (32), part or whole task training (31), and combined PT and psychological awareness training (11,27,28), were identified in our literature review.
Sufficient evidence provided moderate confidence that gait training focused on practicing components of gait, while utilizing verbal and manual cues, prior to initiating the task as a whole was an effective strategy to improve overground ambulation and stair negotiation. Superiority of part task versus whole task training has long been debated (39-41). Here, it seems there is merit in both approaches. For instance, Highsmith et al. advocated one scenario where breaking down the subparts of a complex skill (i.e., stair ascent) enabled whole task mastery (17). Conversely, adding treadmill training as part of a home exercise plan incorporates whole task training that has also proved effective (33). This evidence statement is based on one randomized control trial (31), one case study (29), and two expert opinions (16,17).
Treadmill-Based Gait Training
Improved bioenergetic efficiency was the most prevalent finding for treadmill-based gait training that differed from traditional overground gait training (12,33,36). Lower limb amputees demonstrate a less efficient gait pattern as observed by higher O2 cost, which becomes more pronounced with higher level of amputation or bilateral involvement (42). This can lead to other gait implications, such as reduced self-selected walking speed, reliance on an assistive device, or gait deviations, as the amputee attempts to reduce energy expenditure while ambulating, therefore emphasizing the importance of improving bioenergetic efficiency for this population. Our findings support a low level of evidence that demonstrates improved bioenergetic efficiency was observed following a supervised treadmill training program that included a structured home exercise program, anti-gravity training system, or a virtual reality system that provides real-time visual feedback. Two out of the three articles to support this statement were case studies (12,36), making current evidence to support this statement low. Also, the finding that treadmill training is the superior gait training modality to improve bioenergetic efficiency is misleading, as none of the studies that included traditional overground gait training methods measured energy consumption or expenditure as a primary outcome measure. This is most likely explained by the convenience of measuring O2 consumption and gas exchange while participants are relatively fixed on a treadmill versus collecting this data while they ambulate over ground. Even so, it is unable to be determined at this time if improved bioenergetics can also be achieved with overground training methods or if this finding is limited to treadmill training. Therefore, future research is recommended.
Lamberg et al. compared the effects of body-weight support treadmill training versus treadmill training without body-weight support (35). They found that treadmill training with and without body-weight support is effective to improve six-minute walk test distance and timed up and go test time; increase treadmill speed; and improve spatiotemporal parameters for lower limb amputees with no significant differences found between groups. This study reflects similar findings in patients post-stroke as published in a recent Cochrane review, which concluded that treadmill training with or without body weight support is effective to improve walking speed and endurance (43). These findings have also been demonstrated in patients with Parkinson's disease (44), traumatic brain injury (45), and in some patients following orthopedic surgery (46). All of these studies demonstrated carryover to overground training. Beyond providing activity repetitions, the effectiveness of treadmill training may be partially attributed to the patients' ability to practice walking in a safe environment, especially when utilizing a harness system with or without body-weight support to minimize risk for falls, which improves the patients' confidence when attempting to ambulate at increased speeds.
General Statements
Due to the high variability of gait training methods identified in the literature, a clear pattern of the most beneficial method of gait training was not able to be identified. Conversely, the literature revealed a high level of evidence to support that any of the therapeutic gait training programs administered under skilled supervision that increases time spent performing ambulatory activities beyond the patient's current functional daily ambulation was effective at improving walking function in lower limb amputees (6,11,12,16,17,19,25-36). Most studies assessed spatiotemporal, joint kinematics, bioenergetic efficiency, outcome measures, level of assistance, or a combination of these to demonstrate improvements in gait. Subsequently, evidence statements were able to be formed. It is also important to note that adverse or safety issues were not reported in connection with the gait training methods studied.
Spatiotemporal Gait Parameters
Current literature supports a high level of evidence that therapeutic gait training methods, including early ambulation with a walking aid (32); in-shoe auditory feedback devices (6,26); psychological awareness training (11); or treadmill training with or without body-weight support (34,35), or as a part of a structured home exercise plan, are effective to reduce spatiotemporal gait deviations. Lower limb amputees demonstrate impaired spatiotemporal gait parameters, including decreased prosthetic limb stance phase duration, decreased intact limb step length, decreased cadence, and decreased self-selected walking speed compared to a healthy population (7,47). Changes in spatiotemporal gait parameters can lead to reduced energy efficiency (42) and increased joint stress of intact limb and trunk. Ephraim et al. reported that approximately 63% and 49% of amputees experienced back pain or pain of their intact limb, respectively (48). Also, reduced self-selected walking can make participation in functional and recreational activities difficult and lead to reduced safety when ambulating in the community, such as being able to cross the street in an appropriate amount of time (37). This reinforces the importance of reducing spatiotemporal gait impairments to improve functional mobility, increase safety, and increase amputees' ability to participate in their typical functional and recreational activities.
Joint Kinematics and Loading
Two studies were identified, resulting in low level confidence to support improved frontal and sagittal plane joint kinematics when psychological awareness training was integrated into a typical gait training program (11,28). Two additional studies supported use of an auditory feedback device to improve involved side loading (6,26). In patients with lower limb amputation, joint loading in gait and in functional activities is known to be altered and possibly connected with long term secondary consequences (13,49). Therefore, gait training interventions to mitigate these sequelae are needed.
Limitations
Aggregation of data and meta-analyses were not possible due to the high variability in interventions administered and studied, levels of amputation, etiologies, and selection of outcome measures. Numerous text resources provide gait training intervention concepts; however, they are not peer-reviewed and therefore were not included in this review.
Conclusion
Due to the gait asymmetries, altered biomechanics, and related secondary consequences associated with lower extremity amputation, gait training interventions are needed. Eight evidence statements were synthesized over two general areas of gait training therapy: overground and treadmill training. Overground training with verbal or other auditory, manual, and psychological awareness interventions was found to be effective at improving gait. Similarly, treadmill-based training was found to be effective: 1) as a supplement to overground training; 2) independently when augmented with visual feedback and/or body weight support; or 3) as one part of a home exercise plan. Gait training approaches studied improved multiple areas of gait, including sagittal and coronal biomechanics, spatiotemporal measures, and distance walked. No adverse or safety events were reported in connection with the studied interventions.
Acknowledgments
Contents of this manuscript represent the opinions of the authors and not necessarily those of the U.S. Department of Defense, U.S. Department of the Army, U.S. Department of Veterans Affairs, or any academic or health care institution. Authors declare no conflicts of interest. This project was partially funded by the National Institutes of Health Scholars in Patient Oriented Research (SPOR) grant (1K30RR22270).
References
- 1.Zeigler-Graham K, Mackenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Dillingham TR, Pezzin LE, Mackenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95:875–83. doi: 10.1097/00007611-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Varma P, Stineman MG, Dillingham TR. Epidemiology of limb loss. Phys Med Rehabil Clin N Am. 2014;25:1–8. doi: 10.1016/j.pmr.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feinglass J, Brown JL, LoSasso A. Rates of lower-extremity amputation and arterial reconstruction in the United States, 1979 to 1996. Am J Public Health. 1999;89:1222–7. doi: 10.2105/ajph.89.8.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sauter CN, Pezzin LE, Dillingham TR. Functional outcomes of persons who underwent dysvascular lower extremity amputations. Am J Phys Med Rehabil. 2013;92:287–96. doi: 10.1097/PHM.0b013e31827d620d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang L, Dyer PS, Carson RJ, Webster JB, Bo Foreman K, Bamberg SJM. Utilization of a lower extremity ambulatory feedback system to reduce gait asymmetry in transtibial amputation gait. Gait Posture. 2012;36:631–4. doi: 10.1016/j.gaitpost.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Highsmith MJ, Schulz BW, Hart-Hughes S, Latlief GA, Phillips SL. Differences in the spatiotemporal parameters of transtibial and transfemoral amputee gait. J Prosthet Orthot. 2010;22:26–30. [Google Scholar]
- 8.Highsmith MJ, Kahle JT, Bongiorni DR, Sutton BS, Groer S, Kaufman KR. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int. 2010;34:362–77. doi: 10.3109/03093646.2010.520054. [DOI] [PubMed] [Google Scholar]
- 9.Lura DJ, Wernke MM, Carey SL, Kahle JT, Miro RM, Highsmith MJ. Differences in knee flexion between the Genium and C-Leg microprocessor knees while walking on level ground and ramps. Clin Biomech (Bristol, Avon) 2015;30:175–81. doi: 10.1016/j.clinbiomech.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Highsmith MJ, Kahle JT, Lura DJ, Dubey RV, Carey SL, Quillen WS, Mengelkoch LJ. Short and mid-distance walking and posturography with a novel microprocessor knee. Technol Innov. 2014;15:359–68. [Google Scholar]
- 11.Sjodahl C, Jarnlo GB, Soderberg B, Persson BM. Kinematic and kinetic gait analysis in the sagittal plane of transfemoral amputees before and after special gait re-education. Prosthet Orthot Int. 2002;26:101–12. doi: 10.1080/03093640208726632. [DOI] [PubMed] [Google Scholar]
- 12.Darter BJ, Wilken JM. Gait training with virtual reality-based real-time feedback: improving gait performance following transfemoral amputation. Phys Ther. 2011;91:1385–94. doi: 10.2522/ptj.20100360. [DOI] [PubMed] [Google Scholar]
- 13.Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45:15–29. doi: 10.1682/jrrd.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- 14.Mengelkoch LJ, Kahle JT, Highsmith MJ. Energy costs & performance of transtibial amputees & non-amputees during walking & running. Int J Sports Med. 2014;35:1223–8. doi: 10.1055/s-0034-1382056. [DOI] [PubMed] [Google Scholar]
- 15.Kahle JT, Highsmith MJ. Transfemoral interfaces with vacuum assisted suspension comparison of gait, balance, and subjective analysis: ischial containment versus brimless. Gait Posture. 2014;40:315–20. doi: 10.1016/j.gaitpost.2014.04.206. [DOI] [PubMed] [Google Scholar]
- 16.Highsmith MJ, Kahle JT, Lewandowski AL, Kim SH, Mengelkoch LJ. A method for training step-over-step stair descent gait with stance yielding prosthetic knees. J Prosthet Orthot. 2012;24:10–5. [Google Scholar]
- 17.Highsmith MJ, Kahle JT, Lura DJ, Lewandowski AL, Quillen WS, Kim SH. Stair ascent and ramp gait training with the Genium knee. Technol Innov. 2014;15:349–58. [Google Scholar]
- 18.Bellmann M, Schmalz T, Ludwigs E, Blumentritt S. Stair ascent with an innovative microprocessor-controlled exoprosthetic knee joint. Biomed Tech. 2012;57:435–44. doi: 10.1515/bmt-2011-0029. [DOI] [PubMed] [Google Scholar]
- 19.Yiğiter K, Sener G, Erbahçeci F, Bayar K, Ulger OG, Akdoğan S. A comparison of traditional prosthetic training versus proprioceptive neuromuscular facilitation resistive gait training with trans-femoral amputees. Prosthet Orthot Int. 2002;31:258–70. doi: 10.1080/03093640208726650. [DOI] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hafner B. State of the Science Evidence Report Guidelines. Washington (DC): American Academy of Orthotists & Prosthetists; 2008. [Google Scholar]
- 23.Carey SL, Lura DJ, Highsmith MJ. Differences in myoelectric and body-powered upper-limb prostheses: systematic literature review. J Rehabil Res Dev. 2015;52:247–62. doi: 10.1682/JRRD.2014.08.0192. [DOI] [PubMed] [Google Scholar]
- 24.Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5:52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agrawal V, Gailey R, O'Toole C, Gaunaurd I, Finnieston A. Influence of gait training and prosthetic foot category on external work symmetry during unilateral transtibial amputee gait. Prosthet Orthot Int. 2013;37(5):396–403. doi: 10.1177/0309364612473501. [DOI] [PubMed] [Google Scholar]
- 26.Isakov E. Gait rehabilitation: a new biofeed-back device for monitoring and enhancing weight-bearing over the affected lower limb. Eura Medicophys. 2007;43:21–6. [PubMed] [Google Scholar]
- 27.Sjodahl C, Jarnlo GB, Persson BM. Gait improvement in unilateral transfemoral amputees by a combined psychological and physiotherapeutic treatment. J Rehabil Med. 2001;33:114–8. doi: 10.1080/165019701750165934. [DOI] [PubMed] [Google Scholar]
- 28.Sjodahl C, Jarnlo GB, Soderberg B, Persson BM. Pelvic motion in trans-femoral amputees in the frontal and transverse plane before and after special gait re-education. Prosthet Orthot Int. 2003;27:227–37. doi: 10.1080/03093640308726686. [DOI] [PubMed] [Google Scholar]
- 29.Cole ES. Training elders with transfemoral amputations. Top Geriatr Rehabil. 2003;19(3):183–190. [Google Scholar]
- 30.Faucher LD, Shurr DG. Ambulation on postoperative day 1 after bilateral transtibial amputations: a case report and literature review. J Prosthet Orthot. 2005;17:47–9. [Google Scholar]
- 31.Hyland NW. A comparative analysis of two gait training approaches for individuals with trans-tibial amputation [dissertation] South Orange, (NJ): Seton Hall University; 2009. [Google Scholar]
- 32.Barnett C, Vanicek N, Polman RC, Hancock A, Brown B, Smith L, Chetter I. Kinematic gait adaptations in unilateral transtibial amputees during rehabilitation. Prosthet Orthot Int. 2009;33:135–47. doi: 10.1080/03093640902751762. [DOI] [PubMed] [Google Scholar]
- 33.Darter BJ, Nielsen DH, Yack HJ, Janz KF. Home-based treadmill training to improve gait performance in persons with a chronic transfemoral amputation. Arch Phys Med Rehabil. 2013;94:2440–7. doi: 10.1016/j.apmr.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Black M, Seale J. Prosthetic gait training following bilateral transfemoral amputation using body weight supported treadmill training. A case report. J Neurol Phys Ther. 2006;30:215–6. [Google Scholar]
- 35.Lamberg EM, Muratori LM, Streb R, Werner M, Penna J. Harness-supported versus conventional treadmill training for people with lower-limb amputation: a preliminary report. J Prosthet Orthot. 2014;26:93–8. [Google Scholar]
- 36.Mikami Y, Fukuhara K, Kawae T, Kimura H, Ochi M. The effect of anti-gravity treadmill training for prosthetic rehabilitation of a case with below-knee amputation. Prosthet Orthot Int. 2015;39:502–6. doi: 10.1177/0309364614532866. [DOI] [PubMed] [Google Scholar]
- 37.Wong CK, Ehrlich JE, Ersing JC, Maroldi NJ, Stevenson CE, Varca MJ. Exercise programs to improve gait performance in people with lower limb amputation: a systematic review. Prosthet Orthot Int. 2016;40:8–17. doi: 10.1177/0309364614546926. [DOI] [PubMed] [Google Scholar]
- 38.Ephraim PL, Dillingham TR, Sector M, Pezzin LE, Mackenzie EJ. Epidemiology of limb loss and congenital limb deficiency: a review of the literature. Arch Phys Med Rehabil. 2003;84:747–61. doi: 10.1016/s0003-9993(02)04932-8. [DOI] [PubMed] [Google Scholar]
- 39.Cunningham D. Task analysis and part versus whole learning methods. ETR & D. 1971;19:365–98. [Google Scholar]
- 40.Gopher D, Weil M, Siegel D. Practice under changing priorities: an approach to the training of complex skills. Acta Psychol (Amst) 1989;71:147–77. [Google Scholar]
- 41.Naylor JC, Briggs GE. Effects of task complexity and task organization on the relative efficiency of part and whole training methods. J Exp Psychol. 1963;65:217–24. doi: 10.1037/h0041060. [DOI] [PubMed] [Google Scholar]
- 42.Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9:207–31. doi: 10.1016/s0966-6362(99)00009-0. [DOI] [PubMed] [Google Scholar]
- 43.Mehrholz J, Pohl M, Elsner B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst Rev. 2014:CD002840. doi: 10.1002/14651858.CD002840.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miyai I, Fujimoto Y, Yamamoto H, Ueda Y, Saito T, Nozaki S, Kang J. Long-term effect of body weight-supported treadmill training in Parkinson's disease: a randomized controlled trial. Arch Phys Med Rehabil. 2002;83:1370–3. doi: 10.1053/apmr.2002.34603. [DOI] [PubMed] [Google Scholar]
- 45.Brown TH, Mount J, Rouland BL, Kautz KA, Barnes RM, Kim J. Body weight-supported treadmill training versus conventional gait training for people with chronic traumatic brain injury. J Head Trauma Rehabil. 2005;20:402–15. doi: 10.1097/00001199-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Hesse S, Werner C, Seibel H, von Frankenberg S, Kappel EM, Kirker S, Käding M. Treadmill training with partial body-weight support after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2003;84:1767–73. doi: 10.1016/s0003-9993(03)00434-9. [DOI] [PubMed] [Google Scholar]
- 47.Skinner HB, Effeney DJ. Gait analysis in amputees. Am J Phys Med. 1985;64:82–9. [PubMed] [Google Scholar]
- 48.Ephraim PL, Wegener ST, MacKenzie EJ, Dillingham TR, Pezzin LE. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch Phys Med Rehabil. 2005;86:1910–9. doi: 10.1016/j.apmr.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 49.Highsmith MJ, Kahle JT, Carey SL, Lura DJ, Dubey RV, Csavina KR, Quillen WS. Kinetic asymmetry in transfemoral amputees while performing sit to stand and stand to sit movements. Gait Posture. 2011;34:86–91. doi: 10.1016/j.gaitpost.2011.03.018. [DOI] [PubMed] [Google Scholar]


