Abstract
There is not a clear clinical recommendation for the determination of prosthetic candidacy. Guidelines do not delineate which member(s) of the multidisciplinary team are responsible for prosthetic candidacy decisions and which factors will best predict a positive outcome. Also not clearly addressed is a patient-centered decision-making role. In a previous systematic review (SR), Sansam et al. reported on the prediction of walking ability following lower limb amputation using literature up to 2007. The search strategy was designed from the previous Sansam SR as an update of previously valuable predictive factors of prosthetic candidacy. An electronic literature search was executed from August 8, 2007, to December 31, 2015, using MEDLINE (Pubmed), Embase, The Cumulative Index to Nursing and Allied Health Literature (CINAHL) (Ovid), and Cochrane. A total of 319 studies were identified through the electronic search. Of these, 298 were eliminated, leaving a total of 21 for full evaluation. Conclusions from this updated study are drawn from a total recruited sample (n) of 15,207 subjects. A total of 12,410 subjects completed the respective studies (18% attrition). This updated study increases the size of the original Sansam et al. report by including 137% more subjects for a total of 21,490 between the two articles Etiology, physical fitness, pre-amputation living status, amputation level, age, physical fitness, and comorbidities are included as moderate to strongly supported predictive factors of prosthetic candidacy. These factors are supported in an earlier literature review and should be strongly considered in a complete history and physical examination by a multidisciplinary team. Predictive factors should be part of the patient’s healthcare record.
Keywords: Amputee, Physical therapy, Prosthesis, Rehabilitation, Functional level, Prosthetic candidacy
INTRODUCTION
Guidelines for amputee rehabilitation are available nationally and internationally (1–4). However, there is not a clear clinical recommendation for the determination of prosthetic candidacy. Moreover, while multidisciplinary decision support is recognized in the aforementioned guidelines, the guidelines do not delineate which member(s) of the multidisciplinary team are responsible for prosthetic candidacy decisions nor which factors will best predict a positive outcome. Also not clearly addressed is a patient-centered decision-making role, which is crucial to any clinical decision process.
In a systematic review (SR), Sansam et al. reported on the prediction of walking ability following lower extremity amputation (LEA) (5). Conclusions of that SR were that adequately powered prospective studies reporting predictive ability of factors measured before the onset of rehabilitation could accurately estimate an individual’s walking potential (5). Prospective reports could establish clinic practice guidelines (CPG) for predicting prosthetic candidacy and functional level. Further, predictive factors that are modifiable through preemptive therapies could be explored further to establish whether targeting these factors would lead to improvements in walking outcome. Lastly, Sansam et al. reported there was mixed heterogeneity of methods and outcome measures used in comparing predictive factors (5). Investigation of predictive factors is needed to estimate walking potential more accurately, targeting modifiable factors to optimize outcome after LEA. Ultimately, this would help establish much needed CPGs (5). All factors should be considered when determining walking capacity, as not walking following amputation could lead to physical deterioration and comorbidities and be detrimental to overall health (6,7).
The quality of rehabilitation studies has improved in the last decade (8). Sansam et al.’s SR included literature up to August 2007. There have been many changes and proposed changes to health care regarding LEA, particularly in the U.S. These changes may have initiated more contemporary reports of predicting walking ability. Therefore, the purpose of this SR is to establish factors to predict walking ability with a prosthesis following LEA. This review is an extension and update using similar methods from a previous SR to help establish a wider, more current base of evidence regarding walking ability following lower limb amputation.
METHODS
Search Strategy for Extension of Previous Sansam et al. Systematic Review
An electronic literature search was executed from August 1, 2007, to December 31, 2015, using MEDLINE (Pubmed), Embase, The Cumulative Index to Nursing and Allied Health Literature (CINAHL) (Ovid), and Cochrane and using the following keywords in the title or abstract:
Amput* AND ambulat* OR mobil* OR walk* AND predict* OR prognos* OR probability
Manuscripts were selected or eliminated based on the following criteria:
- Inclusion criteria:
- Adult subjects with unilateral or bilateral lower limb amputation
- Published after August 1, 2007
- Examined the relationship between predictive variables recorded prior to amputee rehabilitation and measures of walking ability following rehabilitation
- Studies using health outcomes with a mobility component, such as the Functional Independence Measure
- English language
- Observational, retrospective studies if predictor variables were available
- Randomized clinical trials
- Exclusion criteria:
- Non-adult
- Prosthetic device or rehabilitation interventions studies
- Animal studies
- Case reports and series
- Letters, editorials, conference proceedings
- Manuscripts from developing nations
Two authors independently assessed selected papers for content, quality, and critical appraisal. Similar to the original Sansam et al. SR, a standardized checklist was used to extract each report’s methods, population, outcome measures, and predictive factors (5). Additionally, the UK National Service Framework for Long-term Conditions (3,9) was used to assess the quality of each study, as it allows assessment of quality in non-randomized cohort studies. The reports and data extracted were verified by at least two independent authors who agreed on final scoring and data extraction. The International Classification of Functioning, Disability and Health (4) was used to present the predictive factors identified from these studies. Following study evaluation and data extraction, factors predictive of walking ability following LEA were aggregated and compared narratively with the findings of the original Sansam et al. SR.
RESULTS
Number of Identified Studies
A total of 319 unique studies were identified through the electronic search. Of these, 298 were eliminated, leaving a total of 21 for full evaluation (Figure 1).
Figure 1.
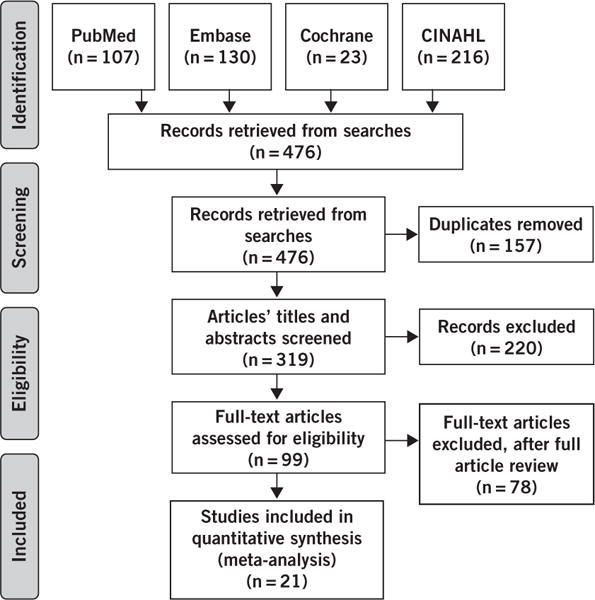
PRISMA 2009 flow diagram. Reprinted with permission from PLoS Medicine (Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting tems for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097), copyright 2009. For more information, visit www.prisma-statement.org.
Description of Sample
The original SR from Sansam et al. included a total (n) of 9,080 subjects (5). Conclusions from this updated study are drawn from a total recruited sample (n) of 15,207 subjects. A total of 12,410 subjects completed the respective studies (18% attrition). There was incomplete and inconsistent reporting of anthropometric, demographic, and etiologic data; of those studies sufficiently reporting this information, the lower extremity limb loss had the following distribution: 37% peripheral vascular disease (PVD), 27% trauma, 17% diabetic, 12% cancer, 6% infection, and 2% congenital. Three sub-groups of subjects were included: an experimental group of subjects with LEA, a control group of subjects with LEA, and another control group of otherwise healthy non-amputee controls. Within the experimental group of LEA patients, the subjects described had a mean age of 57.3 years (median 60.9 (interquartile range (IQR): 8.5); range: 48.1 to 69.8 years) and a mean body mass index (BMI) of 30.2 kg/m2 (median: 31.3 (IQR: 4); range: 27.6 to 31.6 kg/m2). Within the described control group of subjects with LEA, the reported etiology was typically PVD with comorbid diabetes mellitus. Their mean age was 61.8 years (median 66.7 (IQR: 11.8); range: 46.0 to 67.7 years) and mean BMI was 29.6 kg/m2 ± 6.3. Age and BMI were not different (p > 0.05) between experimental and control subjects with LEA. Finally, there was a smaller group of non-amputee, otherwise healthy control subjects described whose mean age was 49.0 years (median 59.2 years (IQR: 35.6); range: 26.1 to 61.7 years) and mean BMI was 25.7 kg/m2 (Table 1).
Table 1.
Diabetes Mellitus (DM), Cancer (CA), Infection (I), Peripheral Vascular Disease (PVD), Trauma (T), Congenital (CONG)
| First Author | Population | Total n | Walking Ability Measures | Results | Quality |
|---|---|---|---|---|---|
| Chin (10) | CA, I | 7 | Oxygen uptake | Older HDAs in good health & w/ low comorbidity prevalence able to successfully walk w/prosthesis in a community. Physical fitness of ≈60% VO2max necessary for older HAD patients to successfully walk. | Medium |
| Czerniecki (27) | PVD, DM | 199 | AMP, etiology | Rehab in CIRU improved mobility success for Veterans undergoing LEA for PVD or DM. No relation to differences in baseline mobility, demographic, psychosocial factors, or # rehab visits. | High |
| Erjavec (11) | PVD | 63 | FIM, 6MWT, Stress | Better exercise test performance relates to increased # patients fitted with prosthesis. Exercise test is good predictor of prosthetic fitting. | Medium |
| Erjavec (33) | PVD, DM, Τ | 160 | Arm Ergometer | TFA patients who reach the level of 30W or more in the exercise test with an arm ergometer are likely to be able to complete the 6MWT using a prosthesis. Simple ergometry may be useful for screening before prosthetic fitting. | High |
| Fortington (30) | PVD, NR | 831 | Healing, mortality, 2MWT, TUG, Step activity | Evidence supporting prognosis for prosthetic & non-prosthetic elderly mobility currently unavailable. | Medium |
| Gremeaux (24) | PVD, T, I, CA, CONG | 70 | Modified Houghton Scale, 2 groups: unlimited walking capacity (score=20) & incapacity to walk, regardless of severity (score <20) | 2MWT proposed as first-line clinical test. FRT indicated for specific assessment of balance disorders | Medium |
| Hamamura (17) | PVD, NR | 64 | Patients who could walk ≥ 100 m w/ at most 1 cane = “successful prosthetic users”; otherwise “failed users” | Minimal comorbidities, walking motivation & sound limb SLS ability are valuable factors contributing to successful prosthetic ambulation in geriatric LEA patients. Also, ≥50% VO2max is a valid initial guideline for physical fitness level required for successful prosthetic rehab. | High |
| Landry (26) | DM | 57 | TMA healing, ambulation, living status, survival | TMA healing predicts subsequent ambulatory status & should be pursued in patients with good rehab potential. | High |
| O’Neil (25) | PVD, T, CA | 37 | Frequency of prosthetic use, ability at DC | Memory & FAS verbal fluency correlate w/ more frequent prosthetic use. | Medium |
| Raya (32) | T, NR | 72 | 6MWT | Strong hip abduction strength strong predictor of; 6MWT score, ability to STS & cross obstacles | High |
| Stineman (22) | PVD, DM, Τ | 4727 | 1 y survival, Discharged home | Receiving inpatient rehab in 1 y of LEA associated w/ increased likelihood of 1 y survival & hospital discharge to home. | High |
| Stineman (21) | PVD, I, DM | 4357 | FIM | LEAs receiving specialized rehab can achieve 8.0 pt FIM motor increase vs. those receiving consultative rehab. One pt. FIM increase associated w/ avg decreased care from a 2nd person of 2.2–5.0min/d. | High |
| Sukow (23) | PVD | 3691 | Ambulating independently or w/ assistance & living at home at follow up. Assessed at DC & 1 y | LEA functional outcomes after LEB directly influenced by amp level. Possible to ID amps likely to achieve good functional outcomes based on pre-op patient characteristics. Can risk-stratify pts at time of LEB least likely to achieve good functional outcome when faced w/ subsequent LEA. | High |
| van Eijk(20) | PVD, DM, CA, I | 55 | SIGAM-WAP, TUG | Elderly patients referred to SNF for rehab have high probability of prosthetic use after TTA, w/out phantom pain; prosthetic candidates. | Medium |
| Wezenberg (28) | T, PVD | 58 | Oxygen uptake | Older adults amputated because of vascular deficiency had a lower aerobic capacity compared with able-bodied controls and traumatic amputees. Level of amputation not associated with VO2 peak. | High |
| Wezenberg (14) | T, PVD | 58 | ECG, BP, oxygen uptake, HR | Vascular LEA patients had lower walking ability vs traumatic LEA patients, which were similar to controls in oxygen uptake during exercise. | High |
| Wong (19) | DM | 151 | Ambulate w/ “success” at 1 y, Pre-op blood labs, Am Soc. Anesthes. status, Pedal pulses | TTA success rate 74%, w/ mortality rate 21% w/in 6 mos. 50% attained prosthetic mobility after 1 y. Infection & poor vascularity (i.e., popliteal pulse absence & low ABI) associated w/ poor clinical outcome. | High |
| Artwert (29) | PVD | 71 | PEQ, LCI, TUG | Functional use of a prosthesis 1y after TTA is related to RL quality. Tibial length of 12–15cm from the knee is correlated w/better functional outcomes than shorter tibial lengths. Surgical technique and RL length important for good functional outcome after TTA. | High |
| Gaunard (31) | Τ | 118 | CHAMP | Salvage the knee joint whenever possible. Intact knee joints increase the possibility of returning to high-level mobility activities following rehab. Rehab-related factors such as lower limb strength, standing and dynamic balance, and ability to displace the CoM over the base of support were all significantly related to ability to perform high-level mobility activities. | High |
| Linberg (12) | Τ | 215 | 6MWT | Characteristics such as age, height, weight, and waist circumference moderately affected 6MWT | High |
| Webster (18) | PVD, DM | 87 | Charlson comorbidity index, VA Large Health Survey, AUDIT-C, MSSS, PHQ-9, Phantom limb/stump pain, daily prosthetic use/ambulation, TAPES | Most individuals achieve successful prosthetic fitting by 1 y following a first major dysvascular LLA, TFAs were significantly less likely to achieve prosthetic fitting success at 1 y. TFA, increased age, major depressive episode, and history of dialysis were associated with significantly less prosthetic ambulation. Higher social support was associated with greater prosthetic ambulation. | High |
Summary of studies included in literature review. Using the UK National Service Framework for Long-term Conditions.(3, 4, 9) Articles were scored out of 10, with up to 2 points awarded for each of the following 5 items: Are the research question/aims and design clearly stated? Is the research design appropriate for the aims and objectives of the research? Are the methods clearly described? Is the data adequate to support the authors’ interpretations/conclusions? Are the results generalizable? Quality grade; ≤3 =poor, 4–6 = medium, ≥7= high quality. Factors considered important for predicting prosthetic use are supported by ≤3 references.
Settings, Study Designs, and Independent Variables
The predominant setting for these studies was the rehabilitation center. These were in varied organizations, including university medical centers, Veterans Administration hospitals, private sector hospitals, and skilled nursing facilities. In addition to these, data were also collected from military treatment facilities, trauma centers, private sector prosthetic practices, and university laboratories. Fifty percent of the included studies were prospective, 38% were retrospective, and 3% were SRs. Cohort and cross-sectional designs were the most common designs, and only two experimental studies were included. The predominant independent variable was LEA. In addition to this, prosthetic rehabilitation was commonly included as treatment.
Since the original Sansam et al. article, the following factors were each supported by a single reference: BMI, motivation, social support, smoking, and phantom limb condition. The following predictive factors were moderately supported (i.e., two references): independence in activities of daily living (ADL), time to rehabilitation, race, and vascular intervention. The following predictive factors were more strongly supported (i.e., three to five references): ability to stand on one leg, cognition and mood disturbance, gender, pre-amputation living status, and cause of amputation. Race, vascular intervention, and pre-amputation living status were newly identified in this report and not identified in the original Sansam et al. article. The most strongly supported factors (i.e., ≥6 references) emerging from the search when considering prosthetic candidacy were: amputation level, physical fitness, age, and comorbidities. There is increasing agreement that these identified predictive factors are important when contemplating prosthetic candidacy and walking ability.
Meta-analysis was not possible, as the studies of like outcome measures did not observe the same homogeneous patient characteristics; mainly, level, etiology, and mean ages were heterogeneous among these studies (10–14).
DISCUSSION
The purpose of this study was to extend the body of knowledge—using the same search strategy originally completed in the Sansam et al. article—of predicting walking ability following lower limb amputation. This SR identifies predictive factors of walking ability and updates the findings to include current literature. We hypothesized that most factors previously identified as important or predictive in determining prosthetic candidacy and walking ability would be reinforced and that new factors would potentially emerge as important in candidacy determinations. This hypothesis was confirmed, as all but five of the previous predictive factors were reported in the updated articles, with 15 of the same predictive characteristics from the original Sansam article recurring. Three new predictive factors were identified in this review that were not previously identified in the original Sansam review (Table 2).
Table 2.
Predictive Factors Investigated by Included Studies
| First Author | Cause of amputation (Etiology) |
Amputation Level | Stump factors and pain | Cognition/Mood Disturbance |
BMI -Height, weight | Physical Fitness | Motivation | Ability to Stand on 1 Leg (SLS) |
IADLs | Age | Comorbidities | Gender (sex) | Social support | Time to rehabilitation | Smoking | Pre-morbid living status | Race | Vascular intervention/ disease |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chin (10) | 1 | 1 | ||||||||||||||||
| Czerniecki (27) | 1 | |||||||||||||||||
| Erjavec (11) | 1 | |||||||||||||||||
| Erjavec (33) | 1 | |||||||||||||||||
| Fortington (30) | 1 | |||||||||||||||||
| Gremeaux (24) | 1 | 1 | 1 | |||||||||||||||
| Hamamura (17) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| Landry (26) | 1 | |||||||||||||||||
| O’Neil (25) | 1 | |||||||||||||||||
| Raya (32) | 1 | |||||||||||||||||
| Stineman (22) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| Stineman (21) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| Suckow (23) | 1 | 1 | ||||||||||||||||
| van Eijk (20) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| Wezenberg (28) | 1 | 1 | ||||||||||||||||
| Wezenberg (14) | 1 | 1 | ||||||||||||||||
| Wong (19) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| Artwert (29) | ||||||||||||||||||
| Gaunard (31) | 1 | 1 | 1 | |||||||||||||||
| Linberg (12) | 1 | 1 | 1 | |||||||||||||||
| Webster (18) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| Total | 3 | 13 | 1 | 3 | 1 | 5 | 1 | 3 | 2 | 10 | 6 | 4 | 1 | 2 | 1 | 4 | 2 | 2 |
Predictive factors in common with Sansam et al, and this systematic review are grey color filled. Predictive factors identified in studies in the Sansam et al. article, but not found in studies included in this extension are: pre-rehab motor function, employment and sport, hemiparesis, psychological factors, and self-efficacy.(5) Predictive factors exclusive to this review are white color filled.
This literature review spans the seven years (2007–2015, 21 studies) following the original Sansam et al. article, whereas the original search included 57 years of literature (1950–2007, 57 studies). This updated study increases the size of the original Sansam et al. report by including 137% more subjects for a total of 21,490 between the two articles. However, the authors caution that, due to poor reporting, it is not clear at times if patients are repeat counted in multiple publications. Nevertheless, in terms of prosthetic studies, this is a considerably large study relative to other SRs, which tend to include much smaller samples. For example, a recent comprehensive SR of microprocessor knees based conclusions on 625 subjects (15). The patients in this SR had predominantly lost their lower extremities due to PVD, which is consistent with epidemiologic data (16). Therefore, it is plausible that the results of this SR would have high generalizability to clinical practice. Given the predominant setting was the rehabilitation center or major medical centers, results may be particularly relevant within these types of settings.
Predictive Factors in a Single Study in This Literature Review
BMI
Linberg et al. found demographics (i.e., height, weight) did not affect the six-minute walk test (6MWT) (12). This is consistent with previous reports in finding that, when adjusting for medical comorbidities, age, and sex, BMI was not a significant predictor of walking ability (5).
Motivation
Hamamura et al., in a high quality study, found significance in motivation as a predictive factor for successful prosthetic ambulation among geriatric subjects (17). This is consistent with a previous report finding a statistically significant association between patient “motivation” and the ability to learn to walk with a prosthesis (5).
Social Support
Webster et al. identified greater levels of baseline social support were associated with more hours of prosthetic walking and identified a need to build in social support structures for patients that have limitations in this regard (18). Greater perceived social support as a predictor of higher mobility was not a well-supported predictive factor in previous studies (5).
Smoking
Wong et al. reported smoking was associated with significantly poorer outcomes in diabetic transtibial amputation (TTA) patients (19). Czerniecki et al. reported smoking status and reported a likely relationship between smoking and a more proximal level amputation, which is discussed later. Although smoking is implicated in the etiology of many amputations, Sansam et al. reported that it is unlikely to have a significant impact on mobility outcome (5).
Stump Factors and Pain
van Eijk et al., in a medium quality article, reported that the presence of phantom pain was significantly associated with the ability to use a prosthesis (20). Phantom limb pain specifically was not reported as a predictive factor outcome measure in previous studies.
Predictive Factors Supported with Two References in This Literature Review
Independence in Activities of Daily Living
van Eijk et al., in a medium quality article, reported preoperative Barthel Index (BI) as a measure of one’s ability to perform basic ADLs. It is reported as evaluation of the functional status at baseline. In addition, the preoperative BI was estimated based on history taking and was significantly positively associated with prosthetic use (20). Further, BI was a significant indicator of the ability to complete the Timed Up and Go (TUG) test. However, Wong et al., in a high quality study, found no correlation between independence in ADLs and outcome in TTA patients (19). This is inconsistent with the previous report of dependency for self-care prior to amputation as an independent negative predictor of walking ability up to 18 years after surgery. A significant association between post-operative ADLs and walking ability after rehabilitation with a prosthesis has also been described (5). Therefore, it seems the preponderance of evidence suggests that independence in completion of ADLs is a factor worth considering when determining prosthetic candidacy.
Time to Rehabilitation
Stineman et al., in two separate high quality studies, reported that patients who had early rehabilitation initially made higher motor gains than those individuals who had later rehabilitation (21). Additionally, patients who received acute postoperative inpatient rehabilitation, compared to those with no evidence of inpatient rehabilitation, had an increased likelihood of one-year survival and home discharge. Prosthetic limb procurement did not differ significantly between groups (22). Sansam et al. found a shorter time interval between surgery and admission for rehabilitation is related to better walking potential. Similarly, the length of time taken from surgery to fitting for a prosthesis is significantly associated with outcome, with those waiting longer having poorer walking ability at one year (5).
Race
In two high quality studies, race was reported as not significant in affecting the outcome of TTA patients or being a predictive factor (18,19). Race was not reported as a predictive factor outcome measure in previous studies.
Vascular Intervention
In a high quality study, Suckow et al. reported it is possible, based on preoperative patient characteristics, to identify patients undergoing lower extremity bypass surgery who are most or least likely to achieve good functional outcomes even if a major amputation is ultimately required. These findings may assist in patient education and surgical decision making in patients who are poor candidates for lower extremity bypass (23). Wong et al. found indicators of poor vascularity, such as absence of popliteal pulse and low Ankle Brachial Index (ABI), were significantly associated with poor clinical outcomes (19). Vascular intervention was not reported as a predictive factor outcome measure in previous studies.
Predictive Factors Supported with Three to Five References in This Literature Review
Ability to Stand on One Leg
In a medium quality study, Grameaux et al. identified the one-leg balance test as appropriate for early evaluation in the immediate follow-up of the amputation in order to establish a prognosis for success in prosthetic ambulation (24). Hamamura et al., in a high quality study, identified the patient’s ability to stand on one leg on the non-amputated limb as one of the most valuable factors contributing to successful prosthetic ambulation in geriatric amputees, reporting significance in successful prosthetic walkers (17). van Eijk et al., in a medium quality article, reported that one-leg balance was significantly positively associated with prosthetic use (20). These reports are consistent with previous reports identifying the ability to stand on one leg as indicative of better walking potential after unilateral lower limb amputation (5).
Cognition and Mood Disturbance
Webster et al. reported, in a study of high quality, that management of depression and promotion of social support may have a positive effect on prosthetic use (18). O’Neill et al., in a report of medium quality, concluded that identified cognitive deficits may indicate augmented rehabilitation or provision of alternative mobility rehabilitation (25). Stineman et al. reported ADL function and mobility (physical functioning) using gains in motor FIM™ scores achieved by rehabilitation discharge. Psychosis was associated with lower motor FIM™ gains, but no direct correlation between psychosis and prosthetic candidacy was reported (21). In the previous Sansam et al. article, cognitive ability was consistently found to be a significant predictor of walking ability following rehabilitation, with a superior outcome reported in those with better cognitive ability (5).
Gender
Four high quality studies found no association between gender and walking ability following lower limb amputation, suggesting it is not a predictive determinant (19–22). Previous studies also found no consistent association with gender (5).
Pre-Amputation Living Status
Several reports in this literature review collected data on factors related to living status, such as marital status and independence. However, none of them reported correlations on living status being a predictive characteristic of walking ability following lower extremity amputation (18,21,22,26).
Cause of Amputation
Some authors reported cause of amputation as a factor in prosthetic candidacy; however, there was no association of cause as a predictive characteristic of walking candidacy (11,21,27). Hamamura et al. reported on cause of amputation, yet no significant difference between the two groups (successful and unsuccessful ambulators) was observed (17). Wezenberg et al. found that the presence of an amputation as a result of vascular deficiency was significantly associated with a lower VO2 peak of 29.1%, whereas a traumatic amputation was not significantly associated with a difference in VO2 peak compared with controls. Having a vascular amputation was associated with a 26.4% decrease in VO2 peak compared with having an amputation because of trauma (28). In a second later article, Wezenberg et al. found traumatic amputees walked at the same VO2 as able-bodied controls but did so at a lower walking speed. Vascular amputees walked at an even slower speed with a substantially higher VO2. Both amputee groups chose a walking speed that was lower than the most efficient walking speed. Consideration of peak aerobic capacity is an important factor when aiming to improve walking ability in amputees (14). Finally, peak aerobic capacity is an important determinant for walking ability. Sansam et al. also reported an association between the cause of amputation and walking potential in five studies, with subjects undergoing an amputation for dysvascularity achieving a poorer outcome than those due to trauma or other non-vascular causes (5).
Predictive Factors Previously Reported Supported With Six or More References in This Literature Review
Amputation Level
Artwert et al., in a high quality article, reported that functional use of a prosthesis in TTA patients is related to residual-limb quality in general as well as for specific bony aspects of the residual limb. A tibial length of 12 to 15 cm from the knee joint line correlated with a better functional outcome than shorter tibial lengths. Surgical technique and attention to the residual limb length ensures a more likely good functional outcome after TTA (29). In a high quality article, Suckow et al. reported TTA and transfemoral amputee (TFA) patients were equally likely to ambulate independently or with assistance (within groups) at hospital discharge. Between groups, however, there were significant differences based on level of amputation. Patients who underwent a minor amputation were more likely to ambulate with or without assistance but less so than patients who did not have an amputation after lower extremity bypass (23). Linberg et al., in a high quality article, reported a significant difference in 6MWT performance between bilateral TTA patients and TFA patients, with bilateral TTA patients walking further (12). Chin et al. reported, in a medium quality study, solely on the hip disarticulation amputee (HDA), where older HDA patients in good physical condition and with a low prevalence of comorbidities were able to successfully walk with a prosthesis in a community setting (10). Czerniecki et al. reported the rates of success were similar: 35%, 31%, and 33% of amputees with transmetatarsal (TM), TTA, and TFA, respectively, achieved mobility success when seen in a comprehensive inpatient rehabilitation unit (27). Fortington et al. reported poorer performance by people with a TFA versus TTA. Slower five-meter walk tests and fewer steps taken per day were reported one year after amputation. One year after discharge, people with TFA or TTA increased the number of steps taken per day from 570 steps at discharge to 1314 steps and were able to maintain this level in the second year (30). Grameaux et al. did not find a statistically significant worse result in bioenergetic efficiency after TFA but did find a reduction in walking speed. Only when age was taken into account in a multiple regression model did the impact of the level of amputation become statistically significant (24). Hamamura et al. reported, in a high quality study, no significant difference between the successful and unsuccessful ambulator groups when considering amputation level (17). Guanard et al., in a high quality article, reported on the importance of an intact knee joint for providing the TTA patient with the ability to return to high-level mobility activities following rehabilitation (31). Stineman et al. reported ADLs and mobility (physical functioning) using gains in motor FIM™ scores achieved by rehabilitation discharge. TFA was associated with lower motor FIM™ gains, but no direct correlation between amputation level and prosthetic candidacy was reported. There was no statistically significant difference in prosthetic limb procurement for the group who received impatient rehabilitation compared to the group who did not (21). van Eijk et al., in a medium quality article, reported amputation level (low versus high) was significantly positively associated with prosthetic use (20). Further, van Eijk et al. found level as a predictor for ability to complete the TUG test. Webster et al., in a high quality article, reported TFA patients were significantly less likely to achieve prosthetic fitting success at one year (18). Wezenberg et al. reported that the level of amputation was not associated with VO2 peak (28). Sansam et al. previously found that the majority of studies reported better walking ability and greater ability to achieve ADLs after distal and unilateral amputations compared with more proximal or bilateral amputations. At this time, it seems the preponderance of evidence suggests that level of amputation is a factor in determining prosthetic ability but not a preclusion from candidacy. Finally, having more intact joints (i.e., having an intact knee compared with not having it) is consistent with a higher potential level of function in TTA patients. Moreover, the longer the transtibial residual limb, the greater potential there is for increased functional level. It is noteworthy, however, that having a long TTA is not requisite for achieving community ambulation, as those with HDA can achieve community ambulation as well.
Physical Fitness
Raya et al., in a high quality article, reported hip strength and balance were significant factors impacting 6MWT scores in individuals with LLA. The 6MWT can identify impairments of the musculoskeletal system that can affect ambulation ability such as weakness in the muscles that support ambulation (32). Chin et al. reported that when older HDA patients are in good physical condition, they are successfully able to walk with a prosthesis in a community setting (10). Hamamura et al. found, in a high quality article, that the successful ambulatory group had a significantly higher VO2 max compared with the failure group (17). van Eijk et al., in a medium quality article, reported that functional ambulation (Functional Ambulation Catagories (FAC) score, which measures the independency of gait) was significantly positively associated with prosthetic use (20). Guanard et al., in a high quality article, reported rehabilitation-related factors, such as lower limb strength, standing and dynamic balance, and ability to displace the center of mass over the base of support, were all significantly related to ability to perform high-level mobility activities (31.) Sansam et al. previously reported that two medium to high quality studies with the same first author have looked at physical fitness and its relationship to walking ability following unilateral above knee amputation. Both studies concluded that a %VO2 max of at least 50% could be regarded as a guideline value for the level of fitness required for successful ambulation with an above-knee prosthesis. This provides agreement that fitness parameters, particularly cardiorespiratory fitness, can be an important factor in determining prosthetic candidacy and success.
Age
Erjavec et al. found that age was a key determining predictive factor in combination with the results of the exercise stress test, a 6MWT at admission, the FIM™ at admission, and consideration of gender, allowing the successful discrimination between patients who were fit with a prosthesis and those who were not (11). Grameaux et al. reported a statistically significant worse result in bioenergetic efficiency related to age when taken into account with amputation level (24). Hamamura et al. reported, in a high quality study, no significant difference between the successful and unsuccessful ambulator groups when considering age (17). Webster et al., in a high quality article, reported that increased age was associated with significantly less prosthetic ambulation (18). Stineman et al. reported ADL function and mobility (physical functioning) using gains in motor FIM™ scores achieved by rehabilitation discharge. Advanced age was associated with lower motor FIM™ gains, but no direct correlation between age and prosthetic candidacy was reported (21). Wong et al., in a high quality article, reported that age was not a significant predictive factor in affecting the outcome in TTA patients (19). van Eijk et al., in a medium quality article, reported that age was not significantly associated with prosthetic use (20). Sansam et al. previously reported that, in most studies, older age at the time of amputation had an adverse effect on walking potential, with six studies reporting a much stronger dependence of walking ability on age than on comorbidity. There is disagreement on the extent to which age is a factor in determining prosthetic candidacy or success. The majority of the studies, including the higher quality evidence, suggests that age does have a role in prosthetic and functional determinations but that it should not restrict candidacy.
Comorbidities
Chin et al. reported that, when there is a low prevalence of commodities, older HDA patients were able to successfully walk with a prosthesis in a community setting (10). Hamamura et al. reported a significant difference between the successful and unsuccessful ambulator groups in the number of comorbidities, with fewer comorbidities having a positive effect (17). Webster et al., in a high quality article, reported that a history of dialysis was associated with significantly less prosthetic ambulation (18). Wong et al., in a high quality article, reported that amputation due to diabetes, high total white count, erythrocyte sedimentation rate, C-reactive protein, urea, creatinine, neutrophils, absence of pulses, low ABI, and Toe Brachial Index were significantly associated with poor clinical outcomes in TTA patients (19). van Eijk et al., in a medium quality article, reported multimorbidity was not significantly associated with prosthetic use (20). Sansam et al. previously reported that the effect of comorbid conditions on walking outcome is not clear. In the majority of studies investigating the role of comorbidities, the conclusions have been drawn from secondary analyses or in conjunction with other factors. At this time, the majority of the evidence is unclear on the extent to which multiple comorbidities impacts prosthetic candidacy and use. However, some studies clearly demonstrate a negative effect of comorbidities on successful outcomes and a positive effect of fewer comorbidities on successful outcomes. Moreover, no studies have shown positive outcomes associated with the presence of comorbidities.
Limitations
Several publications in this review were written by the same or similar author teams. Further, the study topics are also commonly related. The study samples vary slightly at times among these seemingly related publications, making it difficult to be able to sum total number of subjects. Caution is advised related to the interpretation of the results of total sample size.
CONCLUSION
In this literature review, body mass index, motivation, gender, and smoking are among the factors with minimal support to assist in determining candidacy for a prosthesis. Moderately supported factors for prosthetic candidacy included cognition/mood disturbance, etiology, physical fitness, ability to stand on one leg, and pre-amputation living status. The most strongly supported factors for considering prosthetic candidacy were amputation level, age, physical fitness, and comorbidities. These factors are mostly supported in an earlier literature review and should be strongly considered in a complete history and physical examination by a multidisciplinary team. Predictive factor data is likely available in a complete patient health record. Prosthetic candidacy and functional level determinations could be predicted prior to prosthetic prescription based on a comprehensive review of the aforementioned factors. Additionally, these factors seem to remain important later in rehabilitation when determining the appropriate prosthetic prescription and functional level potential. Prosthetic over-prescription is preferred to under-prescription because the cost of a less active and less healthy patient, limited by technologies and therapies that adversely impacts their function and mobility, far outweighs the cost of a higher level prosthesis.
Acknowledgments
Authors would like to acknowledge Tyler Klenow, MSOP, CPT-ACSM, for his contributions to the project. Contents of this manuscript represent the opinions of the authors and not necessarily those of the U.S. Department of Defense, U.S. Department of the Army, U.S. Department of Veterans Affairs, or any academic or health care institution. This project was funded by the AOPA RFP 04012015 and the National Institutes of Health Scholars in Patient Oriented Research (SPOR) grant 1K30RR22270.
Footnotes
Authors declare no conflicts of interest.
References
- 1.CARF International. CMS DMEPOS accreditation program standards manual with survey preparation questions. 3rd. Washington, (DC): CARF International; 2011. [Google Scholar]
- 2.CARF International. Medical rehabilitation program descriptions. Washington, (DC): CARF International; 2013. [Google Scholar]
- 3.Royal College of Physicians, National Council for Palliative Care, British Society of Rehabilitation Medicine. Long-term neurological conditions: management at the interface between neurology, rehabilitation and palliative care. London (UK): RCP; 2008. (Concise Guidance to Good Practice series, No 10). [Google Scholar]
- 4.[WHO] World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva (Switzerland): WHO; 2001. [Google Scholar]
- 5.Sansam K, Neumann V, O’Connor R, Bhakta B. Predicting walking ability following lower limb amputation: a systematic review of the literature. J Rehabil Med. 2009;41(8):593–603. doi: 10.2340/16501977-0393. [DOI] [PubMed] [Google Scholar]
- 6.Dobson A, El-Gamil A, Shimer M, DaVanzo JE. Economic value of prosthetic services among Medicare beneficiaries: a claims-based retrospective cohort study. Mil Med. 2016;181(2 Suppl):18–24. doi: 10.7205/MILMED-D-15-00545. [DOI] [PubMed] [Google Scholar]
- 7.Samuelsson KA, Toytari O, Salminen AL, Brandt A. Effects of lower limb prosthesis on activity, participation, and quality of life: a systematic review. Prosthet Orthot Int. 2012;36(2):145–58. doi: 10.1177/0309364611432794. [DOI] [PubMed] [Google Scholar]
- 8.Cunningham BP, Harmsen S, Kweon C, Patterson J, Waldrop R, McLaren A, McLemore R. Have levels of evidence improved the quality of orthopaedic research? Clin Orthop Relat Res. 2013;471(11):3679–86. doi: 10.1007/s11999-013-3159-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health Long-term Conditions NSF Team. The national service framework for long-term conditions. London (UK): Department of Health; 2005. p. 88. Annex 2 research and evidence. [Google Scholar]
- 10.Chin T, Kuroda R, Akisue T, Iguchi T, Kurosaka M. Energy consumption during prosthetic walking and physical fitness in older hip disarticulation amputees. J Rehabil Res Dev. 2012;49(8):1255–60. doi: 10.1682/jrrd.2011.04.0067. [DOI] [PubMed] [Google Scholar]
- 11.Erjavec T, Presern-Strukelj M, Burger H. The diagnostic importance of exercise testing in developing appropriate rehabilitation programmes for patients following transfemoral amputation. Eur J Phys Rehabil Med. 2008;44(2):133–9. [PubMed] [Google Scholar]
- 12.Linberg AA, Roach KE, Campbell SM, Stoneman PD, Gaunaurd IA, Raya MA, Gomez-Orozco C, Gailey RS. Comparison of 6-minute walk test performance between male Active Duty soldiers and servicemembers with and without traumatic lower-limb loss. J Rehabil Res Dev. 2013;50(7):931–40. doi: 10.1682/JRRD.2012.05.0098. [DOI] [PubMed] [Google Scholar]
- 13.Raya MA, Gailey RS, Fiebert IM, Roach KE. Impairment variables predicting activity limitation in individuals with lower limb amputation. Prosthet Orthot Int. 2010;34(1):73–84. doi: 10.3109/03093640903585008. [DOI] [PubMed] [Google Scholar]
- 14.Wezenberg D, van der Woude LH, Faber WX, de Haan A, Houdijk H. Relation between aerobic capacity and walking ability in older adults with a lower-limb amputation. Arch Phys Med Rehabil. 2013;94(9):1714–20. doi: 10.1016/j.apmr.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Highsmith MJ, Kahle JT, Bongiorni DR, Sutton BS, Groer S, Kaufman KR. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int. 2010;34(4):362–77. doi: 10.3109/03093646.2010.520054. [DOI] [PubMed] [Google Scholar]
- 16.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Hamamura S, Chin T, Kuroda R, Akisue T, Iguchi T, Kohno H, Kitagawa A, Tsumura N, Kurosaka M. Factors affecting prosthetic rehabilitation outcomes in amputees of age 60 years and over. J Int Med Res. 2009;37(6):1921–7. doi: 10.1177/147323000903700630. [DOI] [PubMed] [Google Scholar]
- 18.Webster JB, Hakimi KN, Williams RM, Turner AP, Norvell DC, Czerniecki JM. Prosthetic fitting, use, and satisfaction following lower-limb amputation: a prospective study. J Rehabil Res Dev. 2012;49(10):1493–504. doi: 10.1682/jrrd.2012.01.0001. [DOI] [PubMed] [Google Scholar]
- 19.Wong KL, Nather A, Liang S, Chang Z, Wong TT, Lim CT. Clinical outcomes of below knee amputations in diabetic foot patients. Ann Acad Med Singapore. 2013;42(8):388–94. [PubMed] [Google Scholar]
- 20.van Eijk MS, van der Linde H, Buijck B, Geurts A, Zuidema S, Koopmans R. Predicting prosthetic use in elderly patients after major lower limb amputation. Prosthet Orthot Int. 2012;36(1):45–52. doi: 10.1177/0309364611430885. [DOI] [PubMed] [Google Scholar]
- 21.Stineman MG, Kwong PL, Xie D, Kurichi JE, Ripley DC, Brooks DM, Bidelspach DE, Bates BE. Prognostic differences for functional recovery after major lower limb amputation: effects of the timing and type of inpatient rehabilitation services in the Veterans Health Administration. PM R. 2010;2(4):232–43. doi: 10.1016/j.pmrj.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stineman MG, Kwong PL, Kurichi JE, Prvu-Bettger JA, Vogel WB, Maislin G, Bates BE, Reker DM. The effectiveness of inpatient rehabilitation in the acute postoperative phase of care after transtibial or transfemoral amputation: study of an integrated health care delivery system. ArchPhys Med Rehabil. 2008;89(10):1863–72. doi: 10.1016/j.apmr.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suckow BD, Goodney PP, Cambria RA, Bertges DJ, Eldrup-Jorgensen J, Indes JE, Schanzer A, Stone DH, Kraiss LW, Cronenwett JL, Vascular Study Group of New England Predicting functional status following amputation after lower extremity bypass. Ann Vasc Surg. 2012;26(1):67–78. doi: 10.1016/j.avsg.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gremeaux V, Damak S, Troisgros O, Feki A, Laroche D, Perennou D, Benaim C, Casillas JM. Selecting a test for the clinical assessment of balance and walking capacity at the definitive fitting state after unilateral amputation: a comparative study. Prosthet Orthot Int. 2012;36(4):415–22. doi: 10.1177/0309364612437904. [DOI] [PubMed] [Google Scholar]
- 25.O’Neill BF, Evans JJ. Memory and executive function predict mobility rehabilitation outcome after lower-limb amputation. Disabil Rehabil. 2009;31(13):1083–91. doi: 10.1080/09638280802509579. [DOI] [PubMed] [Google Scholar]
- 26.Landry GJ, Silverman DA, Liem TK, Mitchell EL, Moneta GL. Predictors of healing and functional outcome following transmetatarsal amputations. Arch Surg. 2011;146(9):1005–9. doi: 10.1001/archsurg.2011.206. [DOI] [PubMed] [Google Scholar]
- 27.Czerniecki JM, Turner AP, Williams RM, Hakimi KN, Norvell DC. The effect of rehabilitation in a comprehensive inpatient rehabilitation unit on mobility outcome after dysvascular lower extremity amputation. Arch Phys Med Rehabil. 2012;93(8):1384–91. doi: 10.1016/j.apmr.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wezenberg D, de Haan A, Faber WX, Slootman HJ, van der Woude LH, Houdijk H. Peak oxygen consumption in older adults with a lower limb amputation. Arch Phys Med Rehabil. 2012;93(11):1924–9. doi: 10.1016/j.apmr.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 29.Arwert HJ, van Doorn-Loogman MH, Koning J, Terburg M, Rol M, Roebroeck ME. Residual-limb quality and functional mobility 1 year after transtibial amputation caused by vascular insufficiency. J Rehabil Res Dev. 2007;44(5):717–22. doi: 10.1682/jrrd.2006.05.0047. [DOI] [PubMed] [Google Scholar]
- 30.Fortington LV, Rommers GM, Geertzen JH, Postema K, Dijkstra PU. Mobility in elderly people with a lower limb amputation: a systematic review. JAm Med Dir Assoc. 2012;13(4):319–25. doi: 10.1016/j.jamda.2010.12.097. [DOI] [PubMed] [Google Scholar]
- 31.Gaunaurd IA, Roach KE, Raya MA, Hooper R, Linberg AA, Laferrier JZ, Campbell SM, Scoville C, Gailey RS. Factors related to high-level mobility in male servicemembers with traumatic lower-limb loss. J Rehabil Res Dev. 2013;50(7):969–84. doi: 10.1682/JRRD.2013.02.0035. [DOI] [PubMed] [Google Scholar]
- 32.Raya MA, Gailey RS, Gaunaurd IA, Ganyard H, Knapp-Wood J, McDonough K, Palmisano T. Amputee mobility predictor-bilateral: a performance-based measure of mobility for people with bilateral lower-limb loss. J Rehabil Res Dev. 2013;50(7):961–8. doi: 10.1682/JRRD.2012.05.0097. [DOI] [PubMed] [Google Scholar]
- 33.Erjavec T, Vidmar G, Burger H. Exercise testing as a screening measure for ability to walk with a prosthesis after transfemoral amputation due to peripheral vascular disease. Disabil Rehabil. 2014;36:1148–55. doi: 10.3109/09638288.2013.833307. [DOI] [PubMed] [Google Scholar]


