Abstract
Objective
This study compared individual cognitive behavioral therapy (CBT) and a supportive child-centered therapy (CCT) for child anxiety disorders on rates of treatment response and recovery at post-treatment and one-year follow-up, as well as on real-world measures of emotional functioning.
Method
Youth (N= 133; ages 9–14) with anxiety disorders (generalized, separation, and/or social anxiety) were randomized using a 2:1 ratio to CBT (N = 90) or CCT (N = 43), which served as an active comparison. Treatment response and recovery at post-treatment and one-year follow-up were assessed by Independent Evaluators, and youth completed ecological momentary assessment (EMA) of daily emotions throughout treatment.
Results
The majority of youth in both CBT and CCT were classified as treatment responders (71.1% for CBT; 55.8% for CCT), but youth treated with CBT were significantly more likely to fully recover, no longer meeting diagnostic criteria for any of the targeted anxiety disorders and no longer showing residual symptoms (66.7% for CBT vs. 46.5% for CCT). Youth treated with CBT also reported significantly lower negative emotions associated with recent negative events experienced in daily life during the latter stages of treatment relative to youth treated with CCT. Furthermore, a significantly higher percentage of youth treated with CBT compared to CCT were in recovery at one-year follow-up (82.2% for CBT vs. 65.1% for CCT).
Conclusions
These findings indicate potential benefits of CBT above and beyond supportive therapy on the breadth, generalizability, and durability of treatment-related gains.
Keywords: child anxiety, cognitive behavioral therapy, active comparison, recovery, treatment response
Cognitive-behavioral therapy (CBT) for child anxiety has consistently been shown to be superior to wait-list control (Hollon & Beck, 2013; James, Soler, & Weatherall, 2005; Walkup et al., 2008), however, studies comparing individual CBT to active comparison treatments for child anxiety have produced mixed results, raising concerns about the specificity of the CBT effect on improvements in anxiety. Effectiveness trials for child anxiety detecting few differences in treatment outcomes for school- and community-based CBT and treatment-as-usual have increased these concerns (Barrington, Prior, Richardson, & Allen, 2005; Ginsburg, Becker, Drazdowski, & Tein, 2012; Southam-Gerow et al., 2010). Furthermore, there are still barriers to the dissemination and implementation of CBT in the community (Southam-Gerow, Rodríguez, Chorpita, & Daleiden, 2012). To inform decisions about the investment of resources in training and dissemination of CBT for child anxiety, it is important to determine whether CBT offers significant advantages over other treatments more readily available in the community for children who present with common anxiety disorders in youth, such as generalized anxiety disorder (GAD), social anxiety disorder (SocAD) and separation anxiety disorder (SAD). The present study addresses this question in the first large-scale randomized efficacy trial that compares individual CBT (I-CBT) to an active comparison treatment also delivered individually to children with these anxiety disorders. We focus on treatment for GAD, SocAD, and SAD because these disorders are prevalent in youth, have a similar presentation, frequently co-occur, and respond to the same treatments (Albano, Chorpita, & Barlow, 1996; Kendall et al., 2010).
Only a few studies have compared I-CBT to individualized active comparison treatments for these child anxiety disorders (Khanna & Kendall, 2010; Last, Hansen, & Franco, 1998; Silverman et al., 1999). In an early report, Last et al. (1998) found no differences in the efficacy of I-CBT compared to education and support in the treatment of anxiety-based school refusal in a sample comprised largely of youth with social and separation anxiety. Similarly, Silverman et al. (1999) found no differences in treatment efficacy for I-CBT compared to education and support for treating children with phobic disorders, including social phobia, simple phobia and agoraphobia. However, the active comparison treatment groups in these studies were small, perhaps leaving the studies underpowered to detect differences.
Two more recent larger studies compared I-CBT to active comparison, but the active comparison conditions were geared toward alternative forms of CBT (computerized CBT and family-based CBT). As part of a study testing the efficacy of computer-assisted CBT, Khanna and Kendall (2010) compared individual (non-computerized) CBT to a comparison treatment that included attention and support from a therapist along with non-therapeutic computer games. They found that youth who received individual CBT were less likely to meet criteria for a primary anxiety diagnosis at post-treatment and had lower clinician severity ratings and higher ratings of global functioning at post-treatment relative to the comparison treatment, although there were no differences in child report of anxiety symptoms. Similarly, in a study comparing I-CBT to family-based CBT and family-based education and support, Kendall et al. (2008) found greater effects of I-CBT compared to the family-based education/support condition on diagnostic outcomes at post-treatment and 1-year follow-up, but no condition differences in child or parent-reported anxiety severity at either time point. These studies are promising in suggesting that I-CBT might have a specific advantage over education and support on diagnostic outcomes, but because the active comparisons were delivered in computerized or family format, it is still not clear whether I-CBT is superior to active comparison treatment delivered individually to the child in a face-to-face only format, as is typical in the community. Furthermore, in both of these studies, group differences were found in ratings made by clinical evaluators, but there were no differences detected in child or parent reports of anxiety at post-treatment. For these reasons, there is a need for an efficacy trial comparing individual CBT to an active comparison, non-CBT, individual treatment to help clarify discrepant findings.
These previous studies compared I-CBT to psychoeducation and support in order to control for nonspecific ingredients of psychotherapy such as attention. However, it is unclear the extent to which education/support is similar to the types of treatments that anxious youth typically receive in the community. In their research on trauma-focused CBT, Cohen and Mannarino developed Child-Centered Therapy (CCT), an active comparison intervention for children and adolescents that draws on principles from client-centered therapy, an approach that is widely used in the community (Cohen, Deblinger, Mannarino, & Steer, 2004). CCT has previously been implemented as an active comparison condition for two trials testing the efficacy of trauma-focused CBT for youth with PTSD (Cohen et al., 2004; Cohen, Mannarino, & Iyengar, 2011; Cohen, Mannarino, & Knudsen, 2005). In these studies, children in both CBT and CCT improved from pre- to post-treatment, but CBT showed superiority over CCT in magnitude of treatment gains, rates of clinical remission, and treatment response at 1-year. In the present study, we adapted CCT for use in GAD, SAD, and SocAD to examine whether CBT offers specific advantages over an intervention that includes a strong emphasis on nonspecific psychotherapeutic ingredients, but no CBT content or psychoeducation. CCT places an emphasis on core non-specific therapeutic ingredients such as active listening, reflection, accurate empathy, and encouragement to talk about feelings, but does not include directive problem solving, psychoeducation about anxiety or coping skills, or exposure.
A potential limitation of most extant child anxiety psychotherapy trials is a focus on the loss of the youth’s primary anxiety disorder rather than more complete measures of recovery, such as the absence of all study entry anxiety disorders and/or the absence of significant symptomatology at post-treatment (Caporino et al., 2013; Ginsburg, Becker, Keeton, & et al., 2014; Ginsburg et al., 2011). Considering post-treatment diagnosis of secondary anxiety disorders is important in studies of GAD, SAD, and SocAD because of high rates of comorbidity among these disorders (Costello, Egger, & Angold, 2005). For example, although a child might no longer meet clinical criteria for GAD, her pre-treatment diagnosis, she might still struggle with clinically-meaningful social anxiety at post-treatment. It is also important to determine whether youth have fully recovered from anxiety disorder, as indicated not only by the absence of anxiety diagnoses, but also by a return to symptom levels within the normal range (Herbert et al., 2009; Liber et al., 2010). This is important because residual symptoms constitute a likely risk factor for recurrence and development of future internalizing disorders.
Finally, although one of the primary goals of CBT treatment is to improve children's ability to cope with emotions as they go about their day-to-day life (Southam-Gerow & Kendall, 2002), RCTs for child anxiety have relied primarily on traditional measures such as severity ratings, thus there is little information about how CBT, or other treatments for child anxiety, impact daily emotional functioning. Ecological Momentary Assessment (EMA) is a methodology for using sampling devices in real-time to assess emotions and behaviors in the natural social contexts in which problems manifest themselves (Hormuth, 1986). EMA can provide information about how treated youth manage to cope with daily fears and anxieties in developmentally relevant domains, such as school, friendships, and family interactions. EMA methods have been useful in characterizing the emotional dynamics of child anxiety (Tan et al., 2012), but little is known about how treatment of child anxiety influences daily emotional dynamics. Previous research demonstrates that CBT treatment for adolescent depression is associated with reductions in global negative emotion during daily life (Silk et al. 2011), but this has not been investigated in child anxiety. In the present study, we leveraged EMA methods to examine whether treatment for child anxiety results in similar changes in negative emotions experienced in naturalistic settings, and importantly, whether such changes differed for youth who receive CBT compared to an active comparison treatment. We focused on negative emotions as the primary target for anxiety treatment.
The present study addresses these gaps in the literature using data from a randomized trial comparing individual CBT and CCT for children with GAD, SAD, and SocAD. Our primary goals were to examine whether CBT and CCT differed in terms of treatment response and rates of full recovery at post-treatment and 1-year follow-up and to assess differential impact on day-to-day negative emotions measured in daily life. We hypothesized that youth treated with CBT, compared to CCT, would show higher rates of treatment response and recovery at post-treatment and 1-year follow-up, and reduced peak and current negative emotions in daily life assessed via EMA at post-treatment.
Method
Participants
Participants (N = 133) aged 9–14 years (M = 10.96, SD = 1.47) were recruited through community advertisements (84%) or referrals from pediatricians, school counselors, or mental health professionals (16%) from a metropolitan Midwestern American city. Participants (56% female) were 89% Caucasian, 4% African-American, 2% Hispanic, and 5% Biracial. Anxious youth (ANX) were required to meet DSM-IV (American Psychiatric Association, 1994) criteria for current GAD (N = 94), SAD (N = 34), and/or SocAD (N = 29). Among anxious youth, 52 were diagnosed with multiple anxiety disorders and 36 had other comorbid disorders including Tourette or Tics (N = 5), Major Depressive Disorder (N= 1), Attention Deficit Hyperactivity Disorder, Inattentive Only Subtype (N = 5) and Oppositional Defiant Disorder (N = 3). Table 1 outlines participant characteristics by treatment group.
Table 1.
Baseline Characteristics of Participants by Treatment Condition
| CBT | CCT | |
|---|---|---|
| Demographic characteristics | ||
| Age (years) -- Mean (SD) | 10.943 (1.395) |
10.981 (1.633) |
| Sex -- no. (%) | ||
| Female | 50 (55.6%) | 24 (55.8%) |
| Race or ethnic group -- no. (%) | ||
| White | 81 (90.0%) | 38 (88.4%) |
| Black | 2 (2.2%) | 3 (7%) |
| Hispanic | 1 (1.1%) | 1 (2.3%) |
| Bi-racial | 6 (6.7%) | 1 (2.3%) |
| Family socioeconomic status -- Mean (SD) | ||
| Approximate Family Income | 94,155 (80,145) |
78,632 (43,666) |
| Clinical characteristics | ||
| Primary diagnosis of anxiety disorder -- no. (%) | ||
| Separation anxiety disorder only | 15 (16.7%) | 7 (16.3%) |
| Social anxiety disorder only | 11 (12.2%) | 5 (11.6%) |
| Generalized anxiety only | 49 (54.4%) | 24 (55.8%) |
| Separation and social anxiety disorders | 0 | 1 (2.3%) |
| Separation and generalized anxiety disorders | 7 (7.8%) | 2 (4.7%) |
| Social and generalized anxiety disorders | 8 (8.9%) | 3 (7.0%) |
| Separation, social, and generalized anxiety disorders | 0 | 1 (2.3%) |
| Anxiety Severity -- Mean (SD) | ||
| PARS 6-item Total Score | 16.78 (4.512) |
15.37 (4.577) |
| Daily Negative Affect -- Mean (SD) | ||
| Current Negative Affect | 1.341 (.335) |
1.235 (.254) |
| Peak Negative Affect | 2.254 (.620) |
2.238 (.601) |
Note:
CBT = cognitive behavioral therapy; CCT = child-centered therapy; PARS = Pediatric Anxiety Rating Scale; SD = standard deviation
Exclusion criteria included an IQ below 70 as assessed by the Wechsler Abbreviated Scale of Intelligence (Psychological Corporation, 1999), use of psychoactive medications, acute suicidality or risk for harm to self or others, and, because the larger study included a functional magnetic resonance imaging (fMRI) scan, presence of metal braces or other metal objects in the body. Diagnostic exclusion criteria included a current primary diagnosis of major depressive disorder (MDD), a current diagnosis of obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), conduct disorder, substance abuse or dependence, and ADHD combined type or predominantly hyperactive-impulsive type. Anxious youth were also excluded if they had evidence of an autism spectrum disorder or a lifetime diagnosis of bipolar disorder, psychotic depression, schizophrenia, or schizoaffective disorder. Youth with oppositional defiant disorder, adjustment disorders, tic or movement disorders, ADHD inattentive only subtype, and past history of depression, OCD, or PTSD were permitted to participate in the study.
Procedure
Study procedures were approved by the University’s Institutional Review Board. Following a brief phone screen, participants were scheduled for an intake assessment during which an Independent Evaluator (IE) administered a structured diagnostic interview and rating scales/questionnaires to the child and his/her primary caregiver. Active, signed primary caregiver consent and youth assent were obtained for all participants after a detailed study explanation. Following the intake assessment, youth completed 5 days of Ecological Momentary Assessment (EMA) to assess pre-treatment emotional functioning in daily life. EMA was repeated after every 4th treatment session and at the end of treatment. Psychiatric interviews, questionnaires, and rating scales were also re-administered at post-treatment and 1-year follow-up by an IE unaware of treatment assignment condition. Although not the focus of the present report, youth also completed a larger neurobehavioral assessment battery at pre-and post-treatment that included behavioral observation, sleep actigraphy, electroencephalography, eyetracking, and functional magnetic resonance imaging assessments. All participants were monetarily compensated for their time and effort.
Youth were randomized to treatment following pre-treatment assessments. Restricted randomization was used to balance participants across conditions by age and sex. Because the primary goal of the larger study was to investigate mechanisms involved in CBT treatment response, a 2:1 ratio was used for assignment to CBT vs. CCT. Treatment was delivered by seven M.A. and doctoral level therapists, with all therapists delivering both interventions to control for therapist characteristics. There were no significant differences in the relative proportion of CBT to CCT cases treated by each therapist (χ2 = 6.93, p = .327). Both protocols followed manuals and included 14 sessions with the child and two parent sessions, as well as parental consultation throughout treatment. Therapists for both treatments were trained by experts in each protocol and participated in weekly supervision with expert therapists.
Additionally, approximately 16% of tapes were rated for treatment integrity and fidelity by the expert therapists using standardized checklists to indicate whether appropriate content was covered. The use of any CBT components in CCT would have resulted in lower treatment integrity and fidelity scores on the CCT checklist, which assesses the extent to which the therapist remains nondirective and lets the child take the lead. Similarly, while CBT therapists were permitted to use general psychotherapy skills emphasized in CCT, such as empathy and active listening, if they used only these skills they would have received low scores on the CBT checklist, which assesses active structuring of the session and use of specific CBT components such as cognitive restructuring, coping modeling, role-play, exposures, and active problem-solving. Ratings indicated 98% fidelity for CBT and 99% fidelity for CCT.
Following the post-treatment assessment, anxious youth with sleep difficulties were given the opportunity to participate in a 6–8 session behavioral sleep enhancement intervention (Dahl et al., 2009) offered in the same clinic but delivered by a different clinician. Fifty (38.2%) youth participated in the sleep intervention. The sleep intervention focused on improving sleep-wake regulation and sleep habits within a motivational interviewing framework. There were no significant differences in rates of enrollment in the sleep intervention for youth who received CBT vs. CCT (χ2 = .16, p = .691). Participants were not prevented from seeking additional treatment from the community if desired during the follow-up. 15% of participants reported having obtained other additional services for an emotional or behavioral health problem during the 1-year follow-up, including additional psychotherapy (N =13 [CBT=5, family therapy=3, other = 5]) and/or medication (N = 4 [SSRI = 2, other = 2]). Rates of utilization of subsequent mental health services did not differ significantly for CBT (N = 7, 13%) vs. CCT (N = 6, 27%; χ2 = 2.49, p = .115). Enrollment vs. non-enrollment in the sleep intervention and additional community treatment were examined in exploratory analyses of 1-year treatment outcome, as described below.
CBT intervention
CBT was delivered using the Coping Cat therapist manual (Kendall & Hedtke, 2006a) and child workbook (Kendall & Hedtke, 2006b). The first 8 sessions focused on anxiety-management skills such as identifying somatic cues of anxious arousal, identifying anxious “self-talk” and developing coping “self-talk,” problem solving to cope with the anxiety-provoking situation, and using self-evaluation and self-reward. Progressive muscle relaxation, coping modeling, and role-play are provided. In the second 8 sessions, the therapist guides the child through a hierarchy of exposure tasks to increasingly anxiety-provoking situations. Throughout, children are encouraged to practice at home through homework assignments. Sessions 4 and 9 are held with parents. During these sessions, therapists introduce parents to the CBT model and obtain information from parents about primary concerns and goals. Parents are not treated as co-clients, but are consultants to the child’s treatment and are asked to provide some collaboration and assistance in planning exposure tasks and homework.
CCT intervention
Child-Centered Therapy (CCT; Cohen et al., 2004; Cohen et al., 2005) is a manualized nondirective, supportive psychotherapy based on humanistic principles such as unconditional positive regard, empathy, and therapist genuineness. The techniques employed in CCT include active listening, reflection, accurate empathy, and encouragement to talk about feelings. CCT was developed to be analogous to typical supportive psychotherapy that anxious children and adolescents receive in the community. Cohen et al. (2004) found that although CBT was more effective than CCT in the treatment of children with PTSD, CCT was also associated with a significant decrease in PTSD symptoms at post-treatment. Child and parent satisfaction with treatment have been shown to be equivalent for CCT and CBT treatment (Cohen & Mannarino, 1998). As the original CCT manual (Cohen et al., 2004) focused on anxious youth with PTSD, we adapted the manual to be suitable for youth with GAD, SAD, and/or SocAD. In order to parallel the structure of CBT, CCT was also delivered in 16 sessions, with parents included in sessions 4 and 9.
Structured diagnostic interviews
On their first visit, each youth and his or her parent(s) were interviewed using the Schedule for Affective Disorders and Schizophrenia in School-Age Children—Present and Lifetime version (K-SADS-PL, Kaufman, Birmaher, Brent, & Rao, 1997). Although a larger number of child anxiety trials have relied on the Anxiety Disorders Interview Schedule for Children (Silverman & Albano, 1996), the ADIS-C and K-SADS are both based on DSM criteria, have strong psychometric properties, and have similar structure and content. Parents and youth were interviewed separately, with Independent Evaluators (IE’s) integrating data from both informants to determine the final diagnosis. All interviews were carried out by trained BA- and MA-level IE’s. The results of the interview were presented at a consensus case conference with a child psychiatrist, who reviewed the findings and preliminary diagnosis and provided a final diagnosis based on DSM-IV (American Psychiatric Association, 1994) criteria. Inter-rater reliability between interviewers was calculated for 16% of interviews. Reliability for anxiety diagnoses was high (Kappa = .97). The K-SADS was administered again at 1-year follow-up, along with the Supplemental Services module from the Anxiety Disorders Interview Schedule for Children (Silverman & Albano, 1996) to determine rates of follow-up service utilization.
Anxiety Symptoms
Anxiety severity was rated by an IE on the Pediatric Anxiety Rating Scale (PARS) (RUPP Study Group, 2002). A total score was computed by summing six items assessing anxiety severity, frequency, distress, avoidance, and interference during the previous week (α = .76). Inter-rater reliability for the PARS total score based on 27% of interviews was high (ICC = .82). The following primary outcome indicators were calculated using clinical interview and symptom rating scales at post-treatment: (a) treatment response, defined as a 35% reduction in PARS from pre- to post-treatment, and (b) recovery, defined as an absence of SAD, GAD, and SocAD diagnoses and a PARS clinical severity score ≤10. Decisions regarding cut-offs for defining treatment response and recovery were informed by research establishing guidelines for operationalizing treatment outcome from the PARS (Caporino et al., 2013). The same indicators were also calculated using clinical interview and PARS scores from 1-year follow-up assessments. For secondary analyses, we also obtained child- and parent-report of anxious symptomatology using the Screen for Childhood Anxiety and Related Disorders (Birmaher et al., 1997). Internal consistency was high for parent (α = .92) and child report (α = .92).
Ecological Momentary Assessment (EMA) Protocol
A cellular phone methodology was used to obtain ecological momentary data on youths’ day-to-day emotional functioning using brief structured interviews. Before receiving answer-only cellular phones, youth underwent an orientation session where they were familiarized with the phone and interview questions. The EMA protocol consisted of a five-day block (Thursday to Monday) that was repeated after every 4th treatment session, resulting in a total of 70 calls. During each block, youth received two calls on weekdays and four calls on weekends, for a total of 14 calls per block (for details, see MASKED FOR REVIEW). The study included multiple school districts; thus, it was not feasible to acquire permission for in-school sampling. For each 5-day block, calls began Thursday after school and continued through the following Monday evening. This structure allowed us to sample the intervals of time when freedom and behavioral choice are most variable (after school and weekends). The blocks were repeated five times during the study: at pre-treatment, after session 4, after session 8, after session 12, and post-treatment. EMA data were not collected at one-year follow-up. Average call length was 6.21 minutes (SD = 2.27 minutes). EMA data were unavailable for one participant who reported having difficulty understanding the questions. Eighty-nine percent of scheduled calls were completed and call completion rates did not differ significantly between treatment conditions. Calls were random within pre-specified 3-hour time windows. Phone calls were conducted by trained research assistants who administered questions previously used to assess emotional functioning in the daily life of anxious and depressed youth (Silk et al. 2003; Silk et al., 2011). During each call, youth were asked to identify their momentary negative emotion at the time of the call. They were also asked to identify their most negative experience over the past hour, and to rate their peak affect in association with this experience. Examples include: “I was nervous that I didn't do well on my science test”, “My dad didn't tell me where he went and wasn't home and I didn't know where he was”, and “My friend ditched me to go over someone's house.” As demonstrated in previous research (e.g., Silk et al., 2003), a window of 1 hour maximizes the chances of assessing naturally-occurring emotional experiences while minimizing biases of retrospective recall. Although youth were not expected to experience a major negative emotional event in every 1-hour sampling interval, they were requested to identify a negative experience during each call, even if it was a minor event. Current and peak affect ratings were made using 4 items adapted from the Positive and Negative Affect Scale for Children rated on a scale from 1 (very slightly or not at all) to 5 (extremely) (PANAS-C; Laurent et al., 1999). Negative affect ratings were averaged across 4 items (upset, nervous, angry, sad).
Analytic Plan
For primary outcomes (i.e., response and recovery at post-treatment and 1-year follow-up), treatments were compared using logistic regression, with treatment condition entered as a predictor and youth’s baseline anxiety severity entered as a covariate (PARS 6-item score). For secondary analyses on SCARED scores, two linear regression models were used to compare treatments on these continuous measures. All analyses were conducted on an intent-to-treat (ITT) sample, using multiple imputation to estimate scores for attrited participants who did not complete post-treatment assessments. Missing value analysis, conducted with Little’s MCAR test, suggested that data were likely missing at random (χ2 = 214.130 p = .299). We therefore proceeded with a multiple imputation approach for replacing missing values by implementing fully conditional Markov Chain Monte Carlo (MCMC) modeling (Schafer & Schenker, 2000). The imputation model included child sex and age, parent education, treatment condition, and primary treatment outcome variables at each assessment point (i.e., KSADS diagnostic status, PARS scores). Using these variables, we generated 5 imputed datasets and obtained pooled estimates using Rubin’s established guidelines (Little & Rubin, 2002).
For EMA ratings of current and peak affect, linear multilevel models were used to determine predicted mean values at each assessment point and to test hypotheses with respect to condition and condition by time interactions. In each multilevel model, time (i.e., EMA assessment week, centered at baseline), and treatment condition (i.e., CCT/CBT) were included as fixed effects. All models included a random intercept and an AR1 (autoregressive) covariance structure was used to account for within-subject correlation over time.
Following these primary analyses, we conducted exploratory logistic regression analyses to examine whether any demographic (age, sex), clinical (anxiety subtype, baseline severity, comorbidity), or follow-up variables (enrollment in sleep intervention during follow-up, participation in community treatment during follow-up) were related to treatment outcome, either as non-specific predictors of treatment outcome (as evidenced by a main effect but no interaction with treatment condition), or moderators of treatment outcome (as evidenced by an interaction with treatment condition). Because of their exploratory nature, these analyses were conducted only for youth with complete data.
Results
Treatment and Study Attrition
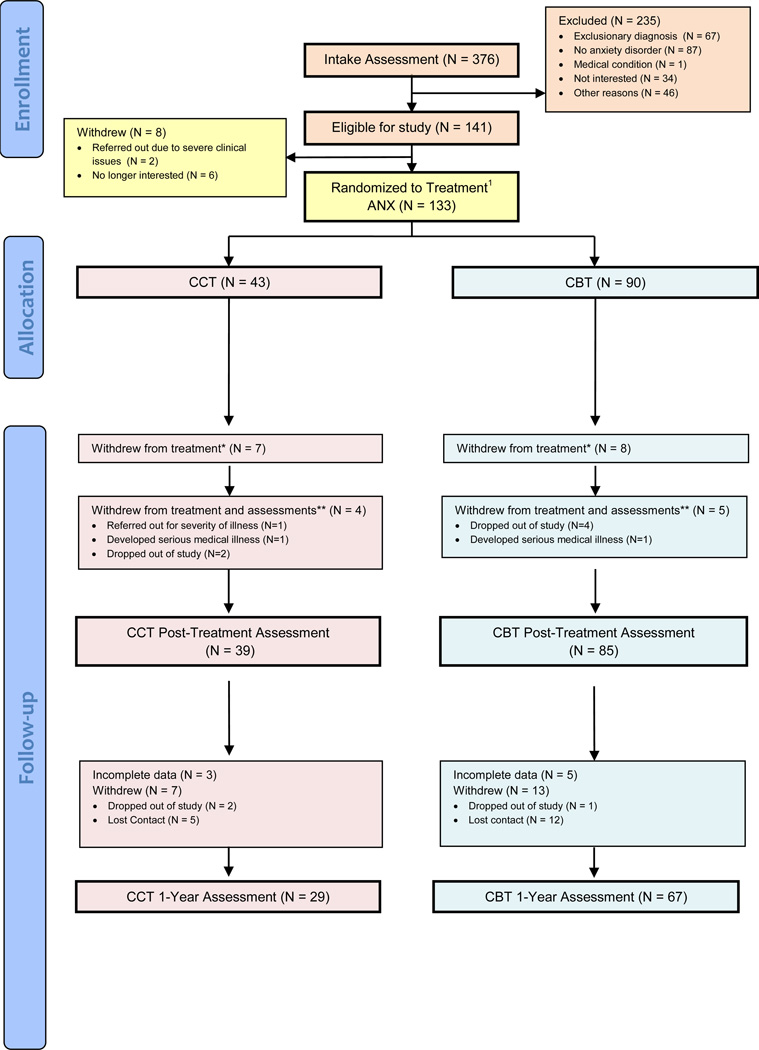
A total of 376 potentially-eligible anxious youth completed an intake assessment with an independent evaluator (Figure 1). Of these, 141 met eligibility criteria and were enrolled in the study. Before randomization, 2 youth were referred out (one for suicidality and one due to custody complications) and 6 withdrew because they were no longer interested. Two additional participants were erroneously randomized, i.e., did not meet study inclusion/exclusion criteria, and were therefore excluded from all analyses. This resulted in the randomization of 133 eligible participants to either 16 sessions of individual CBT or CCT.
Figure 1. Consort Diagram.
1Two participants were originally erroneously randomized to treatment, but did not meet inclusion/exclusion criteria for the study. These participants are included above as “ineligible”; *Subjects who withdrew from treatment continued to do follow-up assessments. **Subjects who withdrew from treatment and assessments did not do any follow-up assessments
As shown in Figure 1, 90 participants were randomized to CBT and 43 to CCT. Treatment groups did not differ significantly in age (F = .04, p = .835), gender (χ2 = .02, p = .967), race (χ2 = 2.68, p = .444), or family income (F = .01, p = .947). The number of completed sessions ranged from 1 to 16, with a mean of 14.35 sessions (SD = 3.76). As shown in Figure 1, 11 CCT participants and 13 CBT participants withdrew from treatment. Of these, 4 CCT participants and 5 CBT participants refused to complete follow-up assessments. Of these 9 study dropouts, two withdrew from the study due to the onset of serious medical conditions (acute brain injury and autoimmune disorder). At the 1-year follow-up, three additional participants withdrew from the study, 17 did not return for an assessment, and 8 had incomplete 1-year follow up data, resulting in complete 1-year follow-up data on N = 96 (72%). However, all randomized subjects were included in ITT analyses (N=133).
Preliminary Analyses
There were no treatment condition differences detected in number of completed sessions (MCCT = 14.21 [SD = 3.63]; MCBT = 14.42 [SD = 3.83], F(1,131) = 0.09, p = .761) or rates of treatment withdrawal (χ2 = 2.08, p = .211). In addition, one-way ANOVAs and χ2-tests indicated that there were no condition differences detected in demographic characteristics (all p’s > .204), clinician-evaluated anxiety severity (F(1,129) = 2.803, p = .097), or comorbidity of anxiety diagnoses (present/absent: χ2 = .691 p = .450). There were no differences found based on recruitment source (community versus referred) on any anxiety or treatment response measure at any time point in the study (all p’s > .22). Finally, we conducted chi square tests to examine whether treatment response or recovery rates differed as a function of therapist. These analyses were conducted across the entire sample as well as within each therapy group, and no therapist effects were detected at post or 1-year follow-up (all p’s > .15)
Condition Differences in Treatment Efficacy at Post-treatment
Our first goal was to examine whether treatment efficacy differed significantly for the two treatment conditions, CCT and CBT, controlling for baseline severity. Table 2 shows reductions in symptoms and associated tests of group differences across acute treatment as well as the follow-up period. Contrary to hypothesis, pooled results from the imputed datasets did not reveal statistically significant condition effects on categorical treatment response at post-treatment (В = .56, SE = .41, p = .176), with the majority of participants responding to both CCT (55.8%) and CBT (71.1%).
Table 2.
Primary Treatment Outcomes
| CBT Imputed | CCT Imputed |
Odds Ratio (95%CI) |
p- value |
|
|---|---|---|---|---|
| Response/Remission Rates for Categorical Outcomes -- N (%) | ||||
| Response (35% decrease in PARS 6-item score) | ||||
| Post-treatment | 64 (71.11%) | 24 (55.81%) | 1.75 (.78, 3.94) | .176 |
| 1-year Follow-up | 76 (84.44%) | 20 (69.77%) | 2.57 (1.01, 6.54) | .049 |
| Recovery (No social, separation, or generalized anxiety disorder diagnosis and PARS 6-item score ≤10) | ||||
| Post-treatment | 60 (66.67%) | 20 (46.51%) | 2.74 (1.05, 5.55) | .037 |
| 1-year Follow-up | 74 (82.22%) | 28 (65.12%) | 3.29 (1.22–8.12) | .010 |
Note:
p < .05,
p < .01,
p < .001;
CBT = cognitive behavioral therapy; CCT = child-centered therapy; PARS = Pediatric Anxiety Rating Scale
In contrast, youth in the two conditions did differ in rates of recovery at post-treatment (В = .88, SE = .42, p = .037). Specifically, 66.7% of youth who received CBT were in full recovery at post-treatment compared to 46.5% of youth who received CCT (Odds Ratio = 2.74).
Condition Differences at 1-year Follow-up
Our second goal was to examine whether CBT had longer-term benefits for anxious youth than CCT. As hypothesized, treatment groups differed in treatment response at 1-year follow-up, with 84.4% of youth who received CBT showing a 35% reduction in PARS scores from pre-treatment compared to 69.8% of youth who received CCT (β = .942, SE = .48, OR = 2.56, p = .049). A similar pattern was observed for recovery (β = 1.19, SE = .46, p = .010), with 82.2% of youth who received CBT compared to 65.1% of youth who received CCT reaching full recovery of anxiety one year following treatment (OR = 3.29).
Child and Parent Report of Anxiety
Secondary analyses of child- and parent-report of symptom severity on the SCARED failed to show a condition or condition X time effect in linear mixed models (p’s ≥ .22). Only time was a significant predictor of anxiety severity from baseline to one-year follow-up as assessed by child (BIC = 12782.19, F(16,834.389) = 1.457, p = .109) and parent (BIC = 13460.749, F(18, 988.015) = 1.194, p = .258).
Exploratory Analyses
Logistic regression analyses were used to explore whether any demographic (age, sex), clinical (anxiety subtype, comorbidity), or follow-up (enrollment versus non-enrollment in sleep intervention during follow-up, participation in community treatment during follow-up) variables predicted or moderated the effect of treatment condition on treatment outcome. There was a main effect of comorbidity (any comorbid DSM-IV diagnosis) on recovery at 1- year follow-up (χ2 = 17.88, p < .001). Specifically, youth with comorbidity were less likely to sustain full recovery at 1-year follow-up than youth without comorbidity, β = −1.39, SE = .69, Wald = 4.08, p = .044, OR = .25. We did not detect any other predictors or moderators of treatment response or recovery at post-treatment or 1-year follow-up.
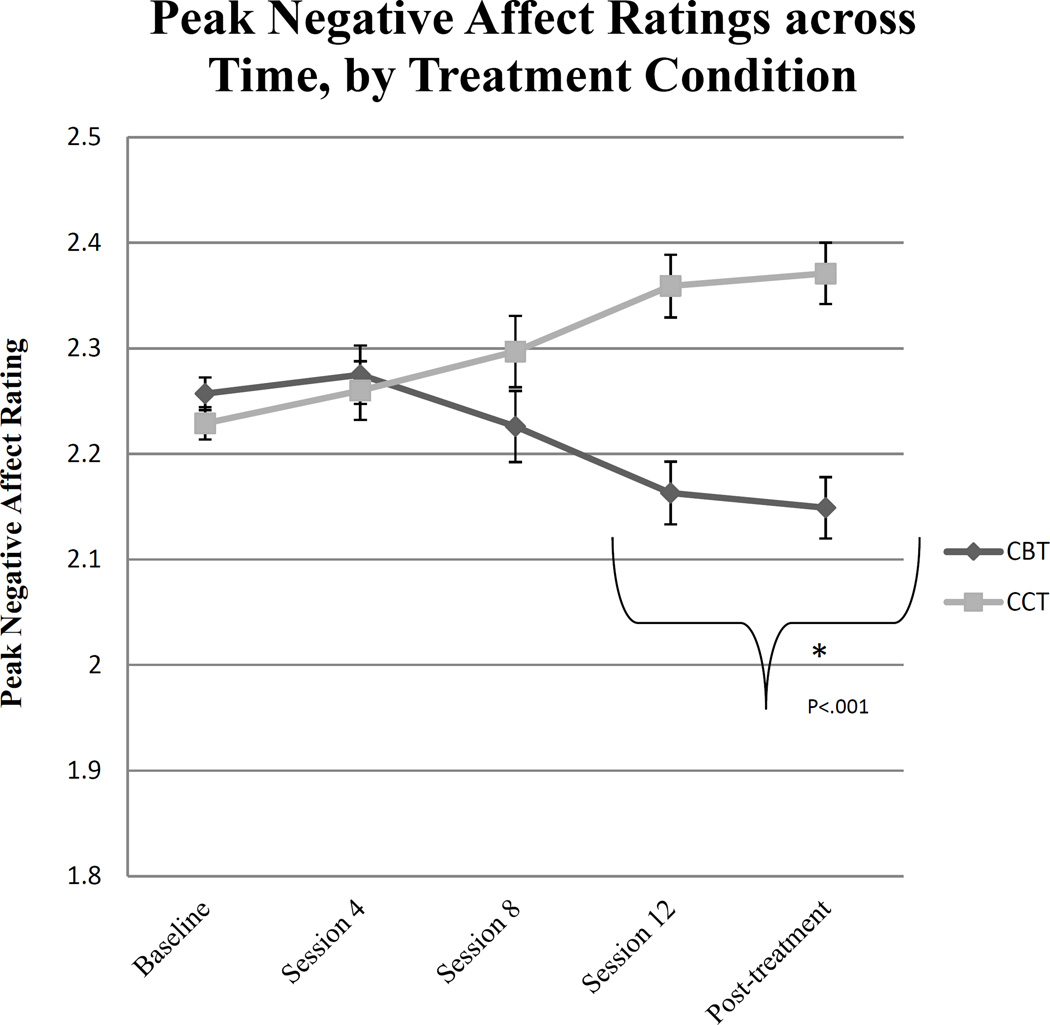
Association of Treatment Condition with Emotional Functioning in Daily Life
Contrary to expectations, there was no evidence in linear mixed effects models of a time by condition interaction effect in predicting youth’s current negative affect at the moment of the call (F(1,132.164) =.770, p =.382, BIC = 10390.63). However, there was a significant time (session) by condition interaction effect in predicting peak negative affect ratings in the hour preceding the call (F(4,1923) =5.612, p < .001, BIC = 12455.432). A follow-up mixed effects model showed that only youth in CBT reported significant reductions in peak negative affect over the course of treatment (F(4,1324.432) = 4.734, p < .001). Moreover, as shown in Figure 2, youth in the CBT condition reported significantly lower levels of peak negative affect than youth in the CCT during the latter part of treatment, after the incorporation of exposure into CBT (assessed at session 12 and post-treatment), t(1697.307) = 4.44, p < .001. In contrast, the two conditions did not appear to differ on reports of peak negative affect from baseline through session 8 (t(136.238) = .082, p = .935).
Figure 2.
Peak Negative Affect Ratings across Time, by Treatment Condition. Post-hoc contrast tests indicate that youth in cognitive behavioral therapy (CBT) reported lower levels of peak negative affect relative to youth in child-centered therapy (CCT) following Session 8, specifically, across the sampling weeks that occurred after the introduction of exposure in CBT (Session 12 and Post-treatment), t(1697.307) = 4.44, p < .001; Cohen’s d = .19. No group differences were observed in ratings of peak negative affect before the introduction of exposure in CBT (Baseline, Session 4, and Session 8), t(136.238) = .082, p = .935, Cohen’s d = .02. Error bars represent the standard error group differences in Peak negative affect at each time point.
Discussion
In the present study, the majority of youth responded positively to both CBT and CCT at post-treatment; however, there were three distinct advantages of CBT over the active comparison. First, youth treated with CBT were significantly more likely to reach full recovery of all targeted anxiety diagnoses and symptom normalization following acute treatment compared to youth treated with CCT. Second, a significantly higher percentage of youth treated with CBT compared to CCT were in full recovery at 1-year follow-up. Third, youth treated with CBT reported significantly lower negative emotions associated with negative or anxiety-provoking events in experience-sampling measures of daily life in the second half of treatment relative to youth treated with CCT. These findings suggest potential specific benefits of CBT above and beyond supportive psychotherapy on the breadth, generalizability, and durability of treatment-related gains.
Findings on whether CBT for child anxiety differs from another active treatment on acute treatment response have been somewhat inconsistent in previous efficacy trials (Brahmbhatt, White, & Barch, 2010; Khanna & Kendall, 2010; Silverman et al., 1999), particularly when comparing interventions delivered to children individually. Our findings may help to explain some of these inconsistencies by suggesting that the acute benefits of individual CBT over active comparison for child anxiety may only emerge when using more stringent measures of treatment response, such as absence of anxiety diagnosis and residual symptomatology (Khanna & Kendall, 2010). The present results indicate that although CBT and CCT both resulted in a significant reduction in anxious symptomatology for the majority of youth, those treated with CBT were more likely to fully recover (62% for CBT vs. 47% for CCT), no longer meeting diagnostic criteria for any of the targeted anxiety disorders (GAD, SAD, and or SocAD) or reporting clinically significant residual symptoms. Although the association between partial recovery and longer-term outcomes for child anxiety are only beginning to be investigated (Ginsburg et al., 2014), partial recovery is a risk factor for future recurrence in other internalizing disorders such as depression (Emslie et al., 2008). Thus, youth who do not reach full recovery may be more likely to experience a recurrence of anxiety disorder and require further treatment in the future.
Findings with regard to 1-year treatment outcomes were also more marked when examining condition differences in rates of full recovery, with CBT youth nearly 5 times more likely to be in recovery one year after treatment than youth treated with CCT. This finding suggests that the benefits of CBT over an active comparison may be more detectable over time. These findings are consistent with data from previous trials demonstrating that the effects of CBT for child anxiety are durable over time (Ginsburg et al., 2014; Kendall, Safford, Flannery-Schroeder, & Webb, 2004), but results from the present study extend this research by showing that this durability may be at least partially attributable to the specific active ingredients of CBT.
A primary goal of treatments for child anxiety is to improve children's ability to manage day-to-day negative emotions (Hudson, 2005; Southam-Gerow & Kendall, 2002), but previous research has not investigated the extent to which this is accomplished. In the present study, we examined changes in the experience of negative emotions in daily life across the course of treatment. Findings indicate that children treated with CBT and CCT did not differ in their current levels of negative affect when sampled at random points in time. However, they did differ in peak negative emotions, with youth treated with CBT reporting lower levels of peak negative affect in response to negative events in the hour leading up to the call than youth in CCT during the latter part of treatment. It is important to note that, although treatment groups differed significantly in peak levels of negative affect over the past hour toward the end of treatment, the absolute magnitude of this difference was small. This is consistent with previous EMA reports demonstrating that both community and clinical samples of youth generally report low intensity and limited ranges of negative emotion (Schneiders et al., 2007; Silk et al., 2011; Silk, Steinberg, & Morris, 2003; Weinstein, Mermelstein, Hedeker, Hankin, & Flay, 2006). For example Silk et al. 2011 found that a difference of only two tenths of a point in EMA negative affect ratings differentiated currently depressed youth from healthy controls. Therefore, although the magnitude of the difference warrants caution, we believe these findings may point to clinically meaningful differences in the quality of daily mood as a function of treatment type.
Additional research will be needed to establish mechanisms through which skills learned in CBT generalize to daily life. Reduced peak negative emotion could be a function of decreased emotional reactivity to daily fears and stressors and/or improved ability to regulate these negative emotions as a function of treatment. For example, it may be that the use of exposure tasks to encourage skills practice during in vivo situations that simulate real-world anxiety provoking scenarios promotes better transfer of these skills to the real world. In line with this possibility, it is notable that the group difference in peak negative emotions only emerges after the introduction of the exposure component of therapy in CBT treatment. This is consistent with one trial reporting that significant changes associated with CBT for child anxiety were not apparent until after the introduction of exposures (Kendall et al., 1997), and with findings that exposure is a key element of successful cognitive-behavioral treatment of child anxiety (Tiwari, Kendall, Hoff, Harrison, & Fizur, 2013). Our findings suggest that it may be the exposure component of CBT which differentiates CBT most clearly from supportive therapy, at least in terms of generalizability to daily negative emotion. In line with this observation, recent efforts have focused on shortening CBT treatment for child anxiety by decreasing the proportion of time spent in the educational preparatory phase (Crawley et al., 2013; Gryczkowski et al., 2013).
Exploratory analyses suggested that, although comorbidity did not influence acute treatment response, full recovery rates one year after treatment were lower for anxious youth with comorbid psychiatric diagnoses relative to youth without comorbid diagnoses, regardless of which intervention they received. This result stands in contrast to a meta-analysis of earlier studies that failed to find support for comorbidity as a predictor or moderator of treatment outcomes for child anxiety (Ollendick, Jarrett, Grills-Taquechel, Hovey, & Wolff, 2008). However, the majority of these studies examined treatment response rather than full recovery. It may be that comorbid diagnoses need to be addressed in order to facilitate more complete recovery.
Potential limitations merit mention. First, the follow-up was only one year. It will be important to examine whether differences in treatment response for CBT vs. active comparison hold over a longer duration. Second, because this was a naturalistic follow-up period, youth in both treatment arms were free to engage in additional interventions, including both community treatment and a behavioral sleep intervention delivered in the clinic. Third, we focused on psychological therapy: findings may not generalize to treatments combined with medication. Fourth, as in previous studies (Kendall et al., 2008; Khanna & Kendall, 2010), differences in treatment response were not consistent when examining parent- and child-reports of symptom severity. This may be due to parents’ and children’s ratings being susceptible to social desirability. Fifth, the sample was primarily Caucasian and middle class, limiting generalization to more diverse samples. Another limitation to generalizability is the fact that youth were excluded from this study if they met criteria for more severe comorbid diagnoses that could influence response to treatment, such as autism spectrum disorder, thus, results may not generalize to all youth with anxiety disorders. It should also be noted that interventions were delivered in an academic medical setting with high quality conditions for treatment delivery, such as frequent therapist supervision, trained therapists, and low caseloads. Additionally, the intervention was delivered as part of a larger study that included frequent assessments that carried opportunities for support and attention from research staff. Effectiveness trials would be needed to determine whether the benefits of individual CBT over child-centered-psychotherapy would be found in community settings. Finally, this trial was part of a larger study designed to investigate mechanisms of treatment response. Although a full investigation of these mechanisms is beyond the scope of the present paper, future analyses will focus on how neurobiological, social, and sleep-related factors might moderate or mediate response to treatment.
Despite these limitations, this study has several strengths, such as the use of a large sample of clinically anxious youth, inclusion of an active comparison treatment known to have positive effects in other samples of anxious youth (Cohen et al., 2005), and use of EMA to examine daily emotional functioning as an additional outcome. Findings regarding the generalizability of treatment response to daily life suggest that, although modest, CBT conveys some benefit for the management of daily negative emotions relative to an active comparison. Superior recovery rates at post-treatment and 1-year for CBT compared to CCT suggest that investment of resources in training and disseminating CBT interventions for child anxiety might have payoff in long-term health outcomes, potentially resulting in reduced expenses associated with the recurrence and/or incomplete remission of anxiety.
References
- Albano A, Chorpita B, Barlow D. Anxiety Disorders. In: Mash E, Barkley R, editors. Child Psychopathology. New York: The Guilford Press; 1996. pp. 196–241. [Google Scholar]
- American Psychological Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Barrington J, Prior M, Richardson M, Allen K. Effectiveness of CBT versus standard treatment for childhood anxiety disorders in a community clinic setting. Behaviour Change. 2005;22(1):29. [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brahmbhatt SB, White DA, Barch DM. Developmental differences in sustained and transient activity underlying working memory. Brain Research. 2010;1354:140–151. doi: 10.1016/j.brainres.2010.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporino NE, Brodman DM, Kendall PC, Albano AM, Sherrill J, Piacentini J. Defining treatment response and remission in child anxiety: Signal Detection analysis using the Pediatric Anxiety Rating Scale. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(1):57–67. doi: 10.1016/j.jaac.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(4):393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Interventions for sexually abused children: Initial treatment outcome findings. Child Maltreatment. 1998;3(1):17–26. [Google Scholar]
- Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: a randomized controlled trial. Archives of pediatrics & adolescent medicine. 2011;165(1):16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse & Neglect. 2005;29(2):135–145. doi: 10.1016/j.chiabu.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Crawley SA, Kendall PC, Benjamin CL, Brodman DM, Wei C, Beidas RS. Brief cognitive-behavioral therapy for anxious youth: feasibility and initial outcomes. Cognitive and Behavioral Practice. 2013;20(2):123–133. doi: 10.1016/j.cbpra.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl RE, Harvey A, Forbes EE, McMakin DL, Milbert MM, Trubnick L. Sleeping Tigers: Treatment for sleep problems in young people. Unpublished treatment manual. Pittsburgh, PA: University of Pittsburgh; 2009. [Google Scholar]
- Emslie GJ, Kennard BD, Mayes TL, Nightingale-Teresi J, Carmody T, Hughes CW. Fluoxetine versus placebo in preventing relapse of major depression in children and adolescents. Am J Psychiatry. 2008;165(4):459–467. doi: 10.1176/appi.ajp.2007.07091453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Becker EM, Keeton CP, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71(3):310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Becker KD, Drazdowski TK, Tein JY. Treating anxiety disorders in inner city schools: Results from a pilot randomized controlled trial comparing CBT and usual care. Child & Youth Care Forum. 2012;41(1):1–19. doi: 10.1007/s10566-011-9156-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM. Remission after acute treatment in children and adolescents with anxiety disorders: Findings from the CAMS. Journal of consulting and clinical psychology. 2011;79(6):806–813. doi: 10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczkowski MR, Tiede MS, Dammann JE, Jacobsen AB, Hale LR, Whiteside SP. The timing of exposure in clinic-based treatment for childhood anxiety disorders. Behavior Modification. 2013;37:113–127. doi: 10.1177/0145445512456546. [DOI] [PubMed] [Google Scholar]
- Herbert JD, Gaudiano BA, Rheingold AA, Moitra E, Myers VH, Dalrymple KL. Cognitive behavior therapy for generalized social anxiety disorder in adolescents: A randomized controlled trial. Journal of Anxiety Disorders. 2009;23(2):167–177. doi: 10.1016/j.janxdis.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon S, Beck AT. Cognitive and cognitive-behavioral therapies. In: Lambert M, editor. Handbook of Psychotherapy and Behavior Change. New York: Wiley; 2013. pp. 393–442. [Google Scholar]
- Hormuth SE. The sampling of experiences in situ. Journal of Personality. 1986;54(1):262–293. [Google Scholar]
- Hudson JL. Mechanisms of change in cognitive behavioral therapy for anxious youth. Clinical Psychology: Science and Practice. 2005;12(2):161–165. [Google Scholar]
- James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. The Cochrane Database of Systematic Reviews. 2005 doi: 10.1002/14651858.CD004690.pub2. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-(K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24(3):360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clincal trial. Journal of consulting and clinical psychology. 1997;65(3):366. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke K. Cognitive-behavioral therapy for anxious children: Therapist manual. Ardmore, PA: Workbook Publishing; 2006a. [Google Scholar]
- Kendall PC, Hedtke K. The Coping Cat Workbook. Ardmore, PA: Workbook Publishing; 2006b. [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. Journal of consulting and clinical psychology. 2008;76(2):282. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: Outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. Journal of Consulting and Clinical Psychology. 2004;72(2):276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. Journal of consulting and clinical psychology. 2010;78(5):737. doi: 10.1037/a0019739. [DOI] [PubMed] [Google Scholar]
- Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(4):404–411. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- Liber J, van Widenfelt B, van der Leeden A, Goedhart A, Utens E, Treffers P. The Relation of severity and comorbidity to treatment outcome with cognitive behavioral therapy for childhood anxiety disorders. J Abnorm Child Psychol. 2010;38(5):683–694. doi: 10.1007/s10802-010-9394-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff JC. Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clin Psychol Rev. 2008;28(8):1447–1471. 683–694. doi: 10.1016/j.cpr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Psychological Corporation. Wechsler Abbreviated Scale of Intelligence (WASI) manual. San Antonio, TX: Author; 1999. [Google Scholar]
- RUPP Study Group. The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Schneiders J, Nicolson NA, Berkhof J, Feron FJ, deVries MW, van Os J. Mood in daily contexts: Relationship with risk in early adolescence. Journal of Research on Adolescence. 2007;17(4):697–722. [Google Scholar]
- Silk JS, Forbes EE, Whalen DJ, Jakubcak JL, Thompson WK, Ryan ND. Understanding daily emotional and social dynamics in depressed youth: a Cell-phone ecological momentary assessment study. Journal of Experimental Child Psychology. 2011;110:241–257. doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents' emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Dev. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children (DSM-IV) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A Randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67(5):675. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC. Emotion regulation and understanding: Implications for child psychopathology and therapy. Clin Psychol Rev. 2002;22(2):189–222. doi: 10.1016/s0272-7358(01)00087-3. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Rodríguez A, Chorpita BF, Daleiden EL. Dissemination and implementation of evidence based treatments for youth: Challenges and recommendations. Professional Psychology: Research and Practice. 2012;43(5):527–534. [Google Scholar]
- Southam-Gerow MA, Weisz JR, Chu BC, McLeod BD, Gordis EB, Connor-Smith JK. Does cognitive behavioral therapy for youth anxiety outperform usual care in community clinics? An initial effectiveness test. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):1043–1052. doi: 10.1016/j.jaac.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan PZ, Forbes EE, Dahl RE, Ryan ND, Siegle GJ, Ladouceur CD. Emotional reactivity and regulation in anxious and non-anxious youth: a Cell-phone ecological momentary assessment study. Journal of Child Psychology & Psychiatry. 2012;53(2):197–206. doi: 10.1111/j.1469-7610.2011.02469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari S, Kendall PC, Hoff AL, Harrison JP, Fizur P. Characteristics of exposure sessions as predictors of treatment response in anxious youth. Journal of Clinical Child & Adolescent Psychology. 2013;42:34–43. doi: 10.1080/15374416.2012.738454. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein SM, Mermelstein RJ, Hedeker D, Hankin BL, Flay BR. The time-varying influences of peer and family support on adolescent daily positive and negative affect. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):420–430. doi: 10.1207/s15374424jccp3503_7. [DOI] [PMC free article] [PubMed] [Google Scholar]