Abstract
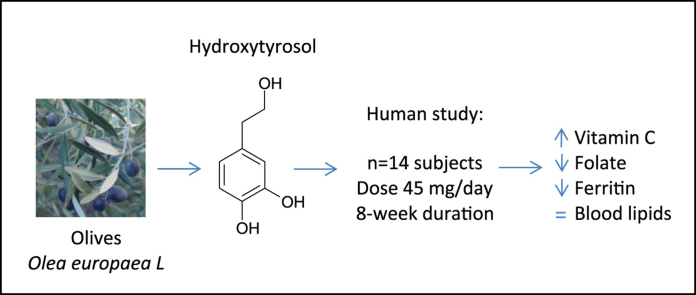
Hydroxytyrosol (HT) is a main phenolic component of olive oil. In this study, we investigated the safety and effects produced by HT purified (99.5%) from olive mill waste. HT was administered at a daily dosage of 45 mg for 8 weeks to volunteers with mild hyperlipidemia (n=14). We measured markers of cardiovascular disease risk, enzyme markers of several clinical conditions, hematology, antioxidant parameters, vitamins and minerals at baseline (T0), 4 weeks (T4) and 8 weeks (T8). The values obtained at T4 and T8 were compared with baseline. We found that the HT dose administered was safe and mostly did not influence markers of cardiovascular disease, blood lipids, inflammatory markers, liver or kidney functions and the electrolyte balance. Serum iron levels remained constant but a significant (P<0.05) decrease in ferritin at T4 and T8 was found. Serum folate and red blood cell folate levels were also reduced at T4 and T8. Finally, vitamin C increased by two-fold at T4 and T8 compared with levels at baseline. These results indicate a physiologically relevant antioxidant function for HT through increasing endogenous vitamin C levels.
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; CPK, creatine phosphokinase; CRP, ultrasensitive C-reactive protein; GGT, Gamma glutamyl transferase; HDL-C, high-density lipoprotein cholesterol; HCT, hematocrit; Hcy, homocysteine; ICAM, intercellular cell adhesion molecule 1; LD, lactate dehydrogenase; LDL-C, low-density lipoprotein cholesterol; Lpa, lipoprotein a; MCH, mean corpuscular hemoglobin; MCV, mean corpuscular volume; MCHC, mean corpuscular hemoglobin concentration; MDA, malondialdehyde; ox-LDL, oxidized LDL; TAC, total antioxidant capacity; TC, total cholesterol; TG, triacylglycerols; VCAM, vascular cell adhesion molecule 1
Keywords: Hydroxytyrosol, Polyphenolics, Olive oil, Antioxidant, Human study, Vitamin c
Graphical abstract
1. Introduction
Hydroxytyrosol (3,4-dihydroxyphenyl-ethanol, HT) is one of the main phenolic components of virgin olive oil and olive mill waste [1] that has demonstrated the strongest reactive oxygen species (ROS) scavenging properties in vivo and vitro among all the olive oil polyphenols [1], [2]. HT is the only phenolic compound that has received a European Food Safety Authority (EFSA) health claim approval. According with EFSA, the consumption of olive oil polyphenols contributes to the protection of blood lipids from oxidative damage [3, and references therein]. This claim refers mainly to the effects of HT and its derivatives (e.g. oleuropein complex and tyrosol) on the protection of low-density lipoproteins (LDL) from oxidation. As oxidative modification of LDL plays a central role in the development of cardiovascular disease (CVD), natural antioxidants are a main target for the nutraceutical industry and several HT preparations are commercially available.
Apart from LDL protection, several human studies have indicated other possible beneficial effects of olive oil phenolic compounds, including antioxidant effects in plasma [2], [4], [5], antithrombotic effects [4], [6], increased HDL-cholesterol [7], inhibition of platelet aggregation [8], [9], reduction of inflammatory markers and reduction of blood pressure [10]. These studies have all been carried out with polyphenols administered in olive oil, or with olive polyphenol extracts of complex origin, where other components (e.g. fatty acids, terpenoids) may also have a role.
In a previous study carried out in our laboratory, we showed that supplementation with 4 mg/Kg of pure HT improved blood lipids, the antioxidant status and reduced the size of atherosclerotic lesions in a rabbit model of diet-induced atherosclerosis [11]. We also purified large amounts of HT from olive mill waste aimed to produce an almost pure (99.5%) water-soluble pharmacological formulation and characterised its absorption profile in humans [12]. So far, no chronic studies reporting effects of pure HT in human volunteers have been published. In this study, we investigated the safety and health effects of a daily dose of 45 mg of HT administered for 8 weeks in markers of CVD risk, enzyme markers of several clinical conditions, hematology, antioxidant markers, vitamins and minerals.
2. Materials and methods
2.1. Subjects and study design
Fourteen healthy volunteers (11 men and 3 women) who were resident in Granada (Spain) participated in the study. The subjects were recruited from volunteers who responded to an advertisement about dietary intervention studies. We advertised for subjects preferably with borderline high levels of total cholesterol, as defined by the National Cholesterol Education Program-Adult Treatment Panel III (total blood cholesterol values between 200 and 239 mg/dL), not suffering from other cardiovascular risk factor. The subjects were given a physical examination and their medical history was consulted before they were included in the study. The subjects were not suffering from any chronic or metabolic disease, had no medical history of gastrointestinal, liver or kidney disease and were not taking any medication or antioxidant supplement. The Ethical Committee of Virgen de las Nieves Hospital Foundation approved the study. Informed written consent was obtained from the volunteers. The study was conducted in accordance with The Code of Ethics of the World Medical Association (Helsinki Declaration, Fortaleza revision 2013), following the EEC Good Clinical Practice guidelines (document 111/3976/88 of July 1990) and current Spanish law, which regulates clinical research in humans (Royal Decree 561/1993 regarding clinical trials). Sample size for before-after study (Paired T-test) was calculated using α (two-tailed) =0.05. The study was designed to have 80% power to detect an effect size of a 15 mg/dL difference in mean blood cholesterol using variance estimates from our previous cholesterol lowering studies.
The volunteers were instructed not to consume olive oil, olives or olive-derived products and to refrain from alcohol consumption for at least 14 days prior to the beginning of the study. The subjects and their partners attended a dietary counselling session on general aspects of food composition, food processing, adequate portions, the effects of alcohol consumption, and the beneficial effects of the Mediterranean diet. The subjects were also advised not to eat fast food or precooked meals and to avoid smoky places or to reduce or stop smoking. The subjects were asked not to change their physical activity pattern during the entire duration of the study. Dietary intake was assessed at baseline and at week 7 of the study with a 7-d self-administered food-frequency questionnaire. Subjects were requested to fill in a food diary according to instructions from the principal investigator, where they recorded all food consumption during the week. Once the subjects completed the first week of the study, they were asked to use the food diaries as a reference to repeat the intake of the same foods registered in the diaries, during the remaining weeks of the study. Spanish food composition tables [13] were used to estimate dietary intake.
The HT supplement was administered in the morning between 10 and 12 a.m., as a single oral dose of 45 mg in 40 mL of sterile saline in a Falcon tube. The supplement was prepared daily and transported on ice to the subject's location where it was administered. On Fridays, the subjects received the oral dose and two other doses in an ice box for the weekend days. Compliance with consumption of the HT supplement at weekend days was ensured by collecting the empty containers. The subjects consumed the HT supplement every day for 8 weeks.
Peripheral blood (120 mL) was drawn from each volunteer at baseline (T0) and at times 4 weeks (T4) and 8 weeks (T8) of the study. Anthropometric data (height, weight and body mass index), systolic and diastolic blood pressure were monitored at each visit. The blood extractions were made by qualified personnel under medical supervision. Plasma was obtained by centrifugation at 1600×g for 10 min at 4 °C, and immediately frozen at –80 °C. For analysis of hematology parameters, blood was withdrawn in EDTA-containing vacutainers (S-Monovette, Sarstedt, Germany) and was sent to the laboratory. 24-h urine was collected in acid-washed containers the day before and on the test day itself. Urine aliquots were obtained and frozen at −80 °C until used.
2.2. Preparation of the HT supplement
The HT administered to the volunteers was obtained by the Process Engineering Department of Puleva Biotech SA, Granada (Spain). HT was purified from an olive mill waste water extract using food grade solvents, preparative chromatography and further desiccation. The HT obtained was a white powder soluble in water with a purity of 99.5% (see reference 12 for details). The HT used for analytical determinations was synthesised by reducing 3,4-dihydroxyphenylacetic acid with LiAlH4 in tetrahydrofuran under refluxing for 4 h. The reaction product was purified by chromatography on silica gel with CHCl3:MeOH (7:1) as the eluting solvent. The identity of the HT obtained was verified by 1H nuclear magnetic resonance and gas chromatography-mass spectrometry (GC–MS). The purity of the HT obtained using this method was 99%. The HT purified was dissolved in sterile saline and stored at −80 °C until use. The concentrations of HT in the aqueous solutions used in the study were measured by high performance liquid chromatography (HPLC) as described in [14].
2.3. Analytical determinations
The biochemistry parameters glucose, total cholesterol (TC), LDL-cholesterol (LDL-C), HDL-cholesterol (HDL-C), triacylglycerols (TG), total protein, albumin, liver enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma glutamyl transferase (GGT), direct and indirect bilirubin, alkaline phosphatase (ALP), lactate dehydrogenase (LD), creatine phosphokinase (CPK), amylase, urea, creatinine, uric acid, lipoprotein (a) (Lp(a)), vitamins A, C, D, E, B6, B12, ferritin, transferrin, iron, calcium, phosphorous, chloride, sodium and potassium, were measured in serum by a routine laboratory at Reference Laboratory (Barcelona, Spain), with certified quality which follows the UNE-EN ISO 15189:2007 directives. Vitamin C was measured by HPLC [15]. Urine analysis was also carried out at Reference Laboratory. Hematology analysis was carried out in Lara Laboratories (Granada, Spain) using an automatic hematology analyser (Beckman Coulter, USA).
Total fasting plasma homocysteine concentration was measured by high-performance liquid chromatography with fluorescence detection [16]. The serum total antioxidant capacity (TAC) was determined as described in [17], using TROLOX as standard. Plasma malondialdehyde (MDA) concentrations were measured using a HPLC separation described in [18] that is based on the thiobarbituric acid reaction and reverse-phase separation with fluorescence detection. Vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) were measured with commercial enzyme-linked immunosorbent assay kits from Biosource International (Camarillo, California, USA) according to the manufacturer's instructions. Oxidized LDL (ox-LDL) in plasma was quantified using an ELISA kit using the monoclonal antibody mAb-4E6 (Mercodia AB, Sweden).
2.4. Statistical analyses
All the data are expressed as means±standard error of the mean (SEM) and differences of P<0.05 were considered significant. Normality was assessed by the Kolmogorov-Smirnov test. The longitudinal effect of the HT supplement at the various time points of the study was analysed by one-way repeated-measures ANOVA followed by Tamhane's T2 posthoc test for not assumed equal variances. For the non-Gaussian variables, Wilcoxon test was performed to assess differences. The data were analysed using SPSS statistical software version 23.0; SPSS Chicago, USA).
3. Results
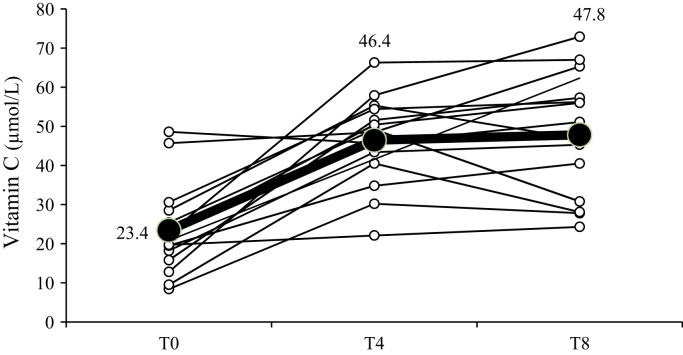
The HT supplement used in the study was well tolerated, compliance was good and the fourteen subjects completed the 8-week study. Nutritional and lifestyle habits showed no differences during the study. No significant changes were found in the intake of nutrients assessed at baseline and at week 7 of the experimental period (not shown). The subjects had a mean age of 34.1 y (range: 25–42), and a mean body mass index (BMI) at baseline of 25.97 kg/m2 (range: 20.2–29.5 kg/m2). No differences were found in anthropometric parameters, such as weight or BMI at the times of the study. Systolic and diastolic blood pressure values remained within normal values through the study period (Table 1). Table 2 shows the serum concentration of a selection of cardiovascular disease risk markers, liver enzymes, parameters of oxidation and enzyme markers of several clinical conditions. All enzyme values were within the range of normality. We only observed a modest but significant reduction in LD and an increase in the levels of CPK. Hematology parameters measured in whole blood (Table 3) showed a modest but significant increase in mean corpuscular volume (MCV) at times T4 and T8, and decreases in mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) at T4. A 10% increase in hematocrit (HCT) was detected at T4 and a non-significant increasing trend at T8. The parameters measured in 24-h urine did not change throughout the study (Table 4). Table 5 shows the vitamins and minerals measured in the subjects at the times of the study. A reduction in the concentration of serum folate was found at T8 together with reductions in RBC folate at times T4 and T8. Ferritin levels were also reduced at T4 and T8 whilst transferrin showed increasing trends at those times (non-significant). The serum levels of iron remained unchanged during the study period. Finally, the serum concentration of vitamin C increased by two-fold at T4 and T8 compared with levels at baseline. Fig. 1 shows the individual and average changes of the serum Vitamin C concentrations of the 14 subjects that participated in the study.
Table 1.
Anthropometric parameters and blood pressure of the subjects at the times of the study.
| Parameter | T0 | T4 | T8 |
|---|---|---|---|
| Weight | 80.07±4.83 | 79.99±4.70 | 80.11±4.76 |
| Height | 1.75±0.02 | 1.75±0.02 | 1.75±0.02 |
| BMI | 25.97±1.18 | 25.95±1.14 | 26.00±1.17 |
| Systolic blood pressure | 122.86±3.84 | 118.46±3.60 | 126.43±4.24 |
| Diastolic blood pressure | 76.79±2.60 | 80.00±2.53 | 83.21±2.95 |
Data are means±SEM. BMI, body mass index.
Table 2.
Biochemical parameters measured in serum at the times of the study.
| Parameter | T0 | T4 | T8 |
|---|---|---|---|
| Glucose (mg/dL) | 93.9±2.72 | 93.9±3.11 | 98.8±3.42 |
| TC (mg/dL) | 235±7.74 | 242±9.37 | 246±9.44 |
| LDL-C | 151±8.19 | 155±8.13 | 162±9.10 |
| TG (mg/dL) | 139±26.1 | 145±22.0 | 126±25.8 |
| HDL-C (mg/dL) | 56.0±4.25 | 57.3±3.52 | 58.7±4.51 |
| TC/HDL-C | 4.39±0.24 | 4.37±0.23 | 4.40±0.26 |
| Total proteins (g/L) | 72.9±1.15 | 77.4±1.44 | 75.0±1.37 |
| Albumin (g/L) | 48.2±1.16 | 47.3±1.08 | 43.5±0.68 |
| ALT (UI/L) | 23.5±1.73 | 23.6±1.80 | 24.7±1.80 |
| AST (UI/L) | 24.1±3.57 | 26.6±4.36 | 26.1±3.12 |
| GGT (U/L) | 49.4±12.9 | 48.4±11.6 | 52.1±11.9 |
| Total bilirubin (mg/dL) | 0.77±0.06 | 0.81±0.08 | 0.83±0.08 |
| Direct bilirubin (mg/dL) | 0.25±0.01 | 0.25±0.02 | 0.29±0.03 |
| Indirect bilirubin (mg/dL) | 0.52±0.05 | 0.56±0.06 | 0.57±0.07 |
| ALP (UI/L) | 146±8.45 | 157±9.57 | 152±7.80 |
| LD (UI/L) | 291±7.73 | 273±9.72* | 267±11.86* |
| CPK (U/L) | 96.1±7.54 | 114.6±15.2 | 124.1±10.4* |
| Amylase (U/L) | 53.3±3.50 | 55.7±3.79 | 53.9±3.31 |
| Urea (mg/dL) | 32.8±2.41 | 32.6±1.50 | 31.4±1.72 |
| Creatinine (mg/dL) | 1.17±0.04 | 1.16±0.04 | 1.14±0.04 |
| Uric acid (mg/dL) | 5.94±0.33 | 5.05±0.34 | 6.16±0.61 |
| CRP (mg/dL) | 3.32±0.44 | 3.40±0.27 | 2.40±0.10 |
| Lp (a) (mg/dL) | 24.3±5.74 | 23.48±5.42 | 24.22±6.90 |
| Hcy (µM) | 17.1±0.60 | 16.2± 0.54 | 16.6±0.60 |
| VCAM (µg/L) | 203±43 | 188±31.7 | 193±29.9 |
| ICAM (µg/L) | 187±24.2 | 202±23.8 | 166±21.2 |
| ox-LDL | 90.4±3.01 | ND | 88.3±4.61 |
| TAC (µM Trolox) | 2.83±0.09 | 2.90±0.09 | 2.86±0.06 |
| MDA (µmol/L) | 0.45±0.12 | 0.47±0.08 | 0.57±0.12 |
Data are means±SEM. *, significantly different from T0, †, significantly different from T4 (P<0.05).
ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; CPK, creatine phosphokinase; CRP, ultrasensitive C-reactive protein; GGT, Gamma glutamyl transferase; HDL-C, high-density lipoprotein cholesterol; Hcy, homocysteine; ICAM, intercellular cell adhesion molecule 1; LD, lactate dehydrogenase; LDL-C, low-density lipoprotein cholesterol; Lp(a), lipoprotein a; MDA, malondialdehyde; ox-LDL, oxidized LDL; TAC, total antioxidant capacity; TC, total cholesterol; TG, triacylglycerols; VCAM, vascular cell adhesion molecule 1.
Table 3.
Hematology parameters measured in blood at the times of the study.
| Parameter | T0 | T4 | T8 |
|---|---|---|---|
| WBC /mL | 6642±310 | 6661±356 | 6285±430 |
| % Lymphs | 37.06±2.48 | 35.54±2.26 | 37.50±1.89 |
| % Monos | 5.37±0.24 | 4.00±0.30 | 3.79±0.26 |
| % Monos+Eos+Baso | 5.37±0.24 | 4.23±0.39 | 4.38±0.29 |
| Monos /mL | 359±27.2 | 277±37.6 | 250±32.4 |
| % Neu | 58.7±2.38 | 59.2±2.31 | 58.3±1.68 |
| RBC (×103/mL) | 4998±135 | 5271±123 | 5140±109 |
| Hgb (g/dL) | 15.4±0.35 | 15.9±0.36 | 15.7±0.37 |
| MCV, fL | 94.8±0.88 | 96.9±1.04** | 96.2±1.01* |
| MCH (pg/cell) | 30.9±0.35 | 30.2±0.27* | 30.8±0.30 |
| MCHC (g/dL) | 32.5±0.25 | 31.2±0.22* | 32.0±0.22 |
| RDW (%) | 14.2±0.38 | 14.2±0.38 | 14.2±0.38 |
| Platelets /mL | 225±11.4 | 215±20.5 | 234±14.6 |
| MPV (fl) | 11.9±0.25 | 11.8±0.27 | 11.9±0.19 |
| HCT (%) | 46.5±1.29 | 51.0±1.18* | 49.2±0.92 |
| ESR (1 h) | 7.71±1.26 | 7.92±1.24 | 6.43±1.03 |
| ESR (2 h) | 18.7±3.05 | 19.0±2.86 | 17.1±2.71 |
| Katz Index | 8.50±1.36 | 8.09±1.38 | 7.48±1.19 |
Data are means±SEM. * and **, significantly different from T0 (*, P<0.05; **, P<0.005).
Baso, basophils; Eos, eosinophils; ESR, erythrocyte sedimentation rate; HCT, hematocrit; Hgb, hemoglobin; Lymphs, lymphocytes; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; MCV, mean corpuscular volume; Monos, monocytes; MPV, mean platelet volume; Neu, neutrophils; RBC, red blood cells; RDW, red blood cell distribution width; WBC, white blood cells.
Table 4.
Parameters measured in 24-h urine at the times of the study.
| Parameter | T0 | T4 | T8 |
|---|---|---|---|
| Glucose (mg/24 h) | 196±43.0 | 264±25.1 | 154±12.0 |
| Urea (g/24 h) | 22.4±1.62 | 21.5±1.74 | 21.4±2.02 |
| Creatinine (mg/24 h) | 1960±160 | 1528±113 | 1837±156 |
| Uric acid (mg/dL) | 46.1±4.73 | 45.2±4.79 | 37.0±4.24 |
| Calcium (mg/24 h) | 226±29.1 | 203±23.8 | 250±30.7 |
| Phosphorous (mg/24 h) | 990±93.5 | ND | 1008±93.5 |
| Chloride (mmol/24 h) | 200±21.1 | 164±17.5 | 198±21.5 |
| Sodium (mEq/L/24 h) | 200±22.3 | 165±18.9 | 192±22.3 |
| Potassium (mEq/L/24 h) | 78.0±6.60 | 64.8±5.90 | 70.5±5.45 |
| Amylase (IU/L) | 159.7±16.9 | 144±16.7 | 131±11.8 |
| 8-Isoprostane (ng/mL) | 0.31±0.03 | ND | 0.26±0.06 |
Data are means±SEM.
Table 5.
Vitamins and minerals measured in the subjects at the times of the study.
| Parameter | T0 | T4 | T8 |
|---|---|---|---|
| Vitamin A (µg/mL) | 0.69±0.04 | 0.62±0.04 | 0.62±0.03 |
| 1,25-OH Vitamin D (pg/mL) | 45.8±2.94 | 40.1±2.75 | 41.4±2.09 |
| Vitamin B6 (µg/L) | 20.4±1.45 | 17.5±1.43 | 24.4±2.76 |
| Vitamin B12 (pg/mL) | 432±33.1 | 406±28.1 | 433±28.2 |
| Vitamin C (µmol/L) | 23.4±3.20 | 46.4±3.11** | 47.8±4.22** |
| Vitamin E (mg/L) | 7.52±0.58 | 7.54±0.66 | 7.32±0.35 |
| Serum folate (ng/mL) | 7.36±0.64 | 6.54±0.55 | 5.85±0.55* |
| RBC folate (ng/mL) | 451±38.3 | 282±28.1* | 320±36.9* |
| Ferritin (ng/mL) | 128±25.0 | 112±21.3* | 105±20.0* |
| Transferrin (mg/dL) | 287±13.1 | 296±15.9 | 293±13.9 |
| Iron (µg/dL) | 110±9.75 | 90.7±8.57 | 112±8.68 |
| Calcium (mg/dL) | 9.65±0.07 | 9.48±0.10 | 9.73±0.12 |
| phosphorous (mg/dL) | 3.23±0.12 | 3.45±0.11 | 3.47±0.13 |
| Sodium (mEq/L) | 140±0.52 | 139±0.64 | 138±0.76 |
| Potassium (mEq/L) | 4.52±0.07 | 4.45±0.07 | 4.29±0.08 |
| Chloride (mmol/L) | 104±0.56 | 102±0.86 | 101±0.41 |
Data are means±SEM. *, significantly different from T0 (P<0.05); **, significantly different from T0 (P<0.001).
Fig. 1.
Serum Vitamin C concentrations of the 14 participating subjects at baseline (T0), and after they had consumed 45 mg of HT daily for 4 weeks (T4) and 8 weeks (T8). Thin lines show vitamin C values of the individual subjects at the times of the study. The thick line shows average mean value changes.
4. Discussion
In this study we investigated, for the first time, the chronic effects (eight weeks) produced by the intake of pure HT administered as a supplement in an aqueous solution. Our hypothesis was that the intake of HT in the context of a balanced diet would improve blood lipids values in mildly hyperlipidaemic subjects. For this reason we recruited volunteers with borderline high levels of total cholesterol, who were not taking cholesterol lowering drugs but who also did not have other cardiovascular risk factors.
The HT administered in our study is equivalent to about 30 g of olive fruit or 10–15 olives from variety rich in polyphenols [19]. However, the dose is well above the nutritional amounts of HT present in virgin olive oil. According to EFSA, 5 mg of hydroxytyrosol and its derivatives (e.g. oleuropein complex and tyrosol), provided by moderate amounts of olive oil, can be easily consumed in the context of a balanced diet, although the concentration of some olive oils may be too low to achieve this intake [3]. However, the HT dose administered in our study is much lower than the estimated intake of polyphenols in the diet from foods like coffee (200 mg/day) [20] or 100 g of apples (141 mg) [21].
We found that in healthy subjects with borderline high levels of cholesterol, the HT dose administered was safe and did not influence markers of cardiovascular disease, blood lipids, inflammatory markers, liver or kidney functions and the electrolyte balance. Some minor changes were detected in biochemical parameters analysed in serum like a decrease in LD or an increase in CPK enzymes, but their values were kept within the normal range and the changes have little clinical relevance.
We previously demonstrated that pure HT was able to reduce blood triacylglycerols, total and LDL-cholesterol and to increase HDL-cholesterol, in a diet-induced model of atherosclerosis performed in hypercholesterolemic rabbits [11]. Other studies using animal models have also shown reductions in total and LDL-cholesterol by olive oil polyphenol extracts or purified HT [22], [23]. The effects of olive oil polyphenols on blood lipids are somehow controversial. Seven studies have investigated in humans the chronic effects (for a period of time of at least 3 weeks) produced by olive oil polyphenol consumption in blood lipids, as a primary or secondary outcome. Five studies were carried out with olive oils [7], [24], [25], [26], [27], one with olive oil polyphenol-enriched sunflower oil [28] and one study with a supplement of a polyphenol extract obtained from olives [29].
The studies with polyphenols administered in olive oil showed increases in HDL-cholesterol [7], [24], reductions in triacylglycerols, total and LDL-cholesterol and increases in HDL-cholesterol [26] or reported no effects at all [27], [28]. One study showed that the reduction in triacylglycerols and total cholesterol produced by the administered olive oils were independent of their polyphenol content [25]. Indeed, olive oil contains other components such as fatty acids (mainly oleic acid), which can modulate blood lipids levels. These other components may contribute to the discrepancy of results. The supplement study, performed with a complex mixture of olive oil polyphenols, administered much higher doses (250 mg/day) to postmenopausal women with osteopenia and obtained reductions in total and LDL-Cholesterol [29]. Related to this, two other supplement studies with similar amounts of polyphenols, but obtained from olive leaves, administered to borderline hypertensive subjects also observed total and LDL-cholesterol reductions [30], [31].
Our study used purified HT (99.5%) to eliminate the effects of fatty acids, or other possible cholesterol-lowering compounds present in olives or olive oil, but showed no effect on blood lipids. Since the cholesterol reductions in other studies were observed at much higher doses of polyphenols (200–400 mg per day), we speculate whether the 45 mg dose in our study was too low, or if the extracts used in other studies could contain cholesterol-lowering compounds other than HT. A recent short study administering 25 mg of HT extract for 7 days also failed to record significant effects on a variety of surrogate markers of cardiovascular disease such as lipid profile, inflammation or oxidation markers [32], although the 7-d duration of the trial was probably too short to detect effect on blood lipids.
We also aimed to investigate the possible deleterious effects produced by the chronic intake of HT. HT has been described to possess iron-chelation properties [33] but, strikingly, the influence of HT on iron status has not been investigated so far. Serum iron concentration is widely used for the diagnosis of iron status and deficiency. However, serum ferritin is directly proportional to the total iron stores in the body and is a much more sensitive and reliable test for demonstration of iron deficiency. Transferrin is the iron transport protein in serum. In our study, the serum levels of iron, ferritin and transferrin were normal, however, the gradual significant decrease obtained in ferritin and the increasing trend observed for transferring could be associated with an increased risk for developing iron deficiency. In relation to this, low values of MCHC are often seen in conditions of iron deficiency anemia (described elsewhere). The significant decreases in MCHC and MCH observed at T4 in our study may also suggest risk of iron loss.
However, reducing iron stores might not be entirely negative. Body iron stores (ferritin) have been associated with increased risk of CVD [34], [35] while depletion may be a cardioprotective mechanism [36], [37]. But this is highly controversial because iron deficiency too has been associated with increased cardiovascular risk [38].
We also observed a significant decrease in serum folate and in RBC folate, albeit within the physiological range. Folate deficiency is associated with macrocytosis (RBC larger than normal). These may as well explain the increase in MCV obtained from the hematology analysis, which is a measure of the size of the average RBC.
This decrease in folate has never been reported in previous olive oil polyphenol chronic trials but has been described in other human studies administering polyphenols [39]. The decrease could be explained by the fact that some polyphenols inhibit intestinal folate uptake [40] or influence the activity of dihydrofolate reductase which is an enzyme necessary for maintaining intracellular pools of tetrahydrofolate [41], [42].
The increase in HCT detected at T4 and the increasing trend at T8 is interesting and deserves further investigation. Other two studies, using much higher amounts of olive oil polyphenols, detected reductions in the concentration of HCT [31] or no changes [29].
The subjects showed low levels of vitamin C at baseline (ranging from 8.4 to 48.6 µmol/L). Intake of the HT supplement increased the serum concentration of vitamin C by 2-fold at T4 (P<0.001), and the levels were sustained for the following 4 weeks (T8).
Only one previous study has investigated the effects of olive oil polyphenols in plasma vitamin C [6]. In the study, the authors administered 12.5 or 25 mg of HT from a HT-concentrated extract obtained from olive oil wastewaters, to type I diabetes patients (n=5), for four days. In this case, the patients only showed a non-significant trend to increase levels of plasma vitamin C. Our study was carried out with more subjects, for a longer period of time and confirms their observation. These results indicate a physiologically relevant antioxidant function for dietary HT due to its vitamin C saving effect. This could also affect the cooperative action of vitamin C with vitamin E (the main antioxidant of LDL), as vitamin C acts regenerating alpha-tocopherol from alpha-tocopheryl radical [43]. It has been proposed that the hydrophilic properties of vitamin C facilitate their localization at the interface of the lipid bilayers in membranes, thereby producing effective inhibition of attack by free radicals in the aqueous phase, and effective repair of lipophilic antioxidants [44]. A previous study in humans carried out in our laboratory demonstrated absorption of the HT supplement and a transient but measurable association of HT with LDL particles [12], where it may act as a quencher of ROS. It has been demonstrated that HT and its derivatives protect LDL particles from oxidative damage [3], [45], using much lower amounts than the dose used in our study. Our results may suggest an additional indirect mechanism of protection of LDL oxidation through increasing endogenous vitamin C levels.
One limitation of our study was the lack of a control group consuming a placebo. This was not possible due to budget restrictions so we used a repeated measures design. Therefore we had to analyse the data for changes compared with baseline. Another limitation was that we did not measure HT in urine to assess compliance.
In conclusion, we aimed to investigate the hypolipidemic effects of HT in subjects with borderline high levels of cholesterol but found negligible effects on blood lipids, a reduction in body iron stores, a reduction in serum and RBC folate and a remarkable increase in vitamin C. More research is needed with a higher number of volunteers and different HT doses to confirm these results. The nutraceutical industry should take these findings into consideration and they should provoke discussion concerning the suitability of commercially available products in the form of olive oil antioxidant supplements.
Conflict of interest
EL-H states no conflict of interest; J.F. is an employee of Puleva Biotech SA, now Biosearch Life.
Acknowledgements
The authors wish to thank Puleva Biotech SA and the Spanish Ministry of Economy and Competitiveness (formerly Ministry of Science and Innovation) [the ERDF-cofinanced grant AGL2011-24428], for funding. The authors wish to thank Maria González-Santiago, Carlos Rodríguez and Antonio D. Valero for their valuable technical assistance, Dr Luis Perez for the purification of the HT used in the study, Alberto Zafra for his help with the HPLC and GC-MS analytical procedures, Dr Arjan Geerlings for fruitful discussions and Ruth Wilson for revising the manuscript.
This Manuscript is dedicated to the memory of Dr Antonio Zarzuelo, Professor of pharmacology of Granada University, a great mentor and friend.
References
- 1.Tripoli E., Giammanco M., Tabacchi G., Di Majo D., Giammanco S., La Guardia M. The phenolic compounds of olive oil: structure, biological activity and beneficial effects on human health. Nutr. Res. Rev. 2005;18:98–112. doi: 10.1079/NRR200495. [DOI] [PubMed] [Google Scholar]
- 2.Visioli F., Caruso D., Galli C., Viappiani S., Galli G., Sala A. Olive oils rich in natural catecholic phenols decrease isoprostane excretion in humans. Biochem. Biophys. Res Commun. 2000;278:797–799. doi: 10.1006/bbrc.2000.3879. [DOI] [PubMed] [Google Scholar]
- 3.EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA); Scientific Opinion on the substantiation of health claims related to polyphenols in olive and protection of LDL particles from oxidative damage (ID 1333, 1638, 1639, 1696, 2865), maintenance of normal blood HDL-cholesterol concentrations (ID 1639), maintenance of normal blood pressure (ID 3781), anti-inflammatory properties (ID 1882), contributes to the upper respiratory tract health (ID 3468), can help to maintain a normal function of gastrointestinal tract (3779), and contributes to body defences against external agents (ID 3467) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA Journal 2011;9(4):2033 [25 pp.]. doi:10.2903/j.efsa.2011.2033. Available online: 〈www.efsa.europa.eu/efsajournal〉
- 4.Visioli F., Caruso D., Grande S., Bosisio R., Villa M., Galli G., Sirtori C., Galli C. Virgin olive oil study (VOLOS): vasoprotective potential of extra virgin olive oil in mildly dyslipidemic patients. Eur. J. Nutr. 2004;6:1–7. doi: 10.1007/s00394-004-0504-0. [DOI] [PubMed] [Google Scholar]
- 5.Fito M., Gimeno E., Covas M.I., Miro E., Lopez-Sabater M.C., Farre M., Marrugat de I.T. J. postprandial and short-term effects of dietary virgin olive oil on oxidant/antioxidant status. Lipids. 2002;37:245–251. doi: 10.1007/s11745-002-0887-1. [DOI] [PubMed] [Google Scholar]
- 6.Leger C.L., Carbonneau M.A., Michel F., Mas E., Monnier L., Cristol J.P., Descomps B. A thromboxane effect of a hydroxytyrosol-rich olive oil wastewater extract in patients with uncomplicated type I diabetes. Eur. J. Clin. Nutr. 2005;59:727–730. doi: 10.1038/sj.ejcn.1602133. [DOI] [PubMed] [Google Scholar]
- 7.Marrugat J., Covas M.I., Fito M., Schroder H., Miro-Casas E., Gimeno E., Lopez-Sabater M.C., de la Torre R., Farre M., SOLOS Investigators Effects of differing phenolic content in dietary olive oils on lipids and LDL oxidation-a randomized controlled trial. Eur. J. Nutr. 2004;43:140–147. doi: 10.1007/s00394-004-0452-8. [DOI] [PubMed] [Google Scholar]
- 8.Petroni A., Blasevich M., Salami M., Papini N., Montedoro G.F., Galli C. Inhibition of platelet aggregation and eicosanoid production by phenolic components of olive oil. Thromb. Res. 1995;78:151–160. doi: 10.1016/0049-3848(95)00043-7. [DOI] [PubMed] [Google Scholar]
- 9.Dell'Agli M., Maschi O., Galli G.V., Fagnani R., Dal Cero E., Caruso D., Bosisio E. Inhibition of platelet aggregation by olive oil phenols via cAMP-phosphodiesterase. Br. J. Nutr. 2008;99:945–951. doi: 10.1017/S0007114507837470. [DOI] [PubMed] [Google Scholar]
- 10.Moreno-Luna R., Muñoz-Hernandez R., Miranda M.L., Costa A.F., Jimenez-Jimenez L., Vallejo-Vaz A.J., Muriana F.J., Villar J., Stiefel P. Olive oil polyphenols decrease blood pressure and improve endothelial function in young women with mild hypertension. Am. J. Hypertens. 2012;25:1299–1304. doi: 10.1038/ajh.2012.128. [DOI] [PubMed] [Google Scholar]
- 11.González-Santiago M., Martín-Bautista E., Carrero J.J., Fonollá J., Baró L., Bartolomé M.V., Gil-Loyzaga P., López-Huertas E. One-month administration of hydroxytyrosol, a phenolic antioxidant present in olive oil, to hyperlipemic rabbits improves blood lipid profile, antioxidant status and reduces atherosclerosis development. Atherosclerosis. 2006;188:35–42. doi: 10.1016/j.atherosclerosis.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 12.González-Santiago M., Fonollá J., Lopez-Huertas E. Human absorption of a supplement containing purified hydroxytyrosol, a natural antioxidant from olive oil, and evidence for its transient association with low-density lipoproteins. Pharm. Res. 2010;61:364–370. doi: 10.1016/j.phrs.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 13.Mataix J., Mañas M., Llopis J., Martinez-Victoria E. Universidad de Granada; Granada, Spain: 1998. Tabla de composición de alimentos españoles. [Google Scholar]
- 14.Brenes M., García A., García P., Rios J.J., Garrido A. Phenolic compounds in Spanish olive oils. J. Agric. Food Chem. 1999;47:3535–3540. doi: 10.1021/jf990009o. [DOI] [PubMed] [Google Scholar]
- 15.Foot E.A., Fry I.D., Starkey B.J. Measurement of plasma and urinary ascorbic acid by high performance liquid chromatography (HPLC) Ann. Clin. Biochem. 1987;24 (Supplement: S1-225) [Google Scholar]
- 16.Araki A., Sako Y. Determination of free and total homocysteine in human plasma by high-performance liquid chromatography with fluorescence detection. J. Chromatogr. 1987;422:43–52. doi: 10.1016/0378-4347(87)80438-3. [DOI] [PubMed] [Google Scholar]
- 17.Miller J.N., Rice-Evans C., Davies M.J., Gopinathan V., Milner A. A novel method for measuring antioxidant capacity and its application to monitoring the antioxidant status in premature neonates. Clin. Sci. 1993;84:407–412. doi: 10.1042/cs0840407. [DOI] [PubMed] [Google Scholar]
- 18.Fukunaga K., Yoshida M., Nakazono N. A simple, rapid, highly sensitive and reproducible quantification method for plasma malondialdehyde by highperformance liquid chromatography. Biomed. Chromatogr. 1998;12:300–303. doi: 10.1002/(SICI)1099-0801(199809/10)12:5<300::AID-BMC751>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 19.Romero C., Brenes M., Yousfi K., García P., García A., Garrido A. Effect of cultivar and processing method on the contents of polyphenols in table olives. J. Agric. Food Chem. 2004;52:479–484. doi: 10.1021/jf030525l. [DOI] [PubMed] [Google Scholar]
- 20.Radtke J., Linseisen J., Wolfram G. Phenolic acid intake of adults in a Bavarian subgroup of the national food consumption survey. Z. Ernahr. 1998;37:190–197. doi: 10.1007/s003940050016. [DOI] [PubMed] [Google Scholar]
- 21.Williamson G., Holst B. Dietary reference intake (DRI) value for dietary polyphenols: are we heading in the right direction? Br. J. Nutr. 2008;99(Suppl. 3):S55–S58. doi: 10.1017/S0007114508006867. [DOI] [PubMed] [Google Scholar]
- 22.Fki I., Bouaziz M., Sahnoun Z., Sayadi S. Antioxidant effect of phenolic compounds extracted from Chemlali olive cultivar in hypercholesterolemic rats. Bioorg. Med. Chem. 2005;13:5362–5370. doi: 10.1016/j.bmc.2005.05.036. [DOI] [PubMed] [Google Scholar]
- 23.Fki I., Sahnoun Z., Sayadi S. Hypocholesterolemic effects of phenolic extracts and purified hydroxytyrosol recovered from olive mill wastewater in rats fed a cholesterol-rich diet. J. Agric. Food Chem. 2007;55:624–631. doi: 10.1021/jf0623586. [DOI] [PubMed] [Google Scholar]
- 24.Covas M.I., Nyyssönen K., Poulsen H.E., Kaikkonen J., Zunft H.J., Kiesewetter H., Gaddi A., de la Torre R., Mursu J., Bäumler H., Nascetti S., Salonen J.T., Fitó M., Virtanen J., Marrugat J., EUROLIVE Study Group The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann. Intern. Med. 2006;145:333–341. doi: 10.7326/0003-4819-145-5-200609050-00006. [DOI] [PubMed] [Google Scholar]
- 25.Machowetz A., Gruendel S., Garcia A.L., Harsch I., Covas M.I., Zunft H.J., Koebnick C. Effect of olive oil consumption on serum resistin concentrations in healthy men. Horm. Metab. Res. 2008;40:697–701. doi: 10.1055/s-2008-1078728. [DOI] [PubMed] [Google Scholar]
- 26.Oliveras-López M.J., Molina J.J., Mir M.V., Rey E.F., Martín F., de la Serrana H.L. Extra virgin olive oil (EVOO) consumption and antioxidant status in healthy institutionalized elderly humans. Arch. Gerontol. Geriatr. 2013;57:234–242. doi: 10.1016/j.archger.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 27.S. Martín-Peláez, J. Mosele, N. Pizarro, M. Farràs, R. de la Torre, I. Subirana, F. Pérez-Cano, O. Castañer, R. Solà, S. Fernandez-Castillejo, S. Heredia, M. Farré, M. Motilva, M. Fitó Effect of virgin olive oil and thyme phenolic compounds on blood lipid profile: implications of human gut microbiota. Eur. J. Nutr. 2015; November 5, published online. doi: 10.1007/s00394-015-1063-2 [DOI] [PubMed]
- 28.Vázquez-Velasco M.1, Esperanza Díaz L., Lucas R., Gómez-Martínez S., Bastida S., Marcos A., Sánchez-Muniz F.J. Effects of hydroxytyrosol-enriched sunflower oil consumption on CVD risk factors. Br. J. Nutr. 2011;105:1448–1452. doi: 10.1017/S0007114510005015. (Epub 2010 Dec 8) [DOI] [PubMed] [Google Scholar]
- 29.Filip R., Possemiers S., Heyerick A., Pinheiro I., Raszewski G., Davicco M.J., Coxam V. Twelve-month consumption of a polyphenol extract from olive (Olea europaea) in a double blind, randomized trial increases serum total osteocalcin levels and improves serum lipid profiles in postmenopausal women with osteopenia. J. Nutr. Health Aging. 2015;19:77–86. doi: 10.1007/s12603-014-0480-x. [DOI] [PubMed] [Google Scholar]
- 30.Perrinjaquet-Moccetti T., Busjahn A., Schmidlin C., Schmidt A., Bradl B., Aydogan C. Food supplementation with an olive (Olea europaea L.) leaf extract reduces blood pressure in borderline hypertensive monozygotic twins. Phytother. Res. 2008;22:1239–1242. doi: 10.1002/ptr.2455. [DOI] [PubMed] [Google Scholar]
- 31.Susalit E., Agus N., Effendi I., Tjandrawinata R.R., Nofiarny D., Perrinjaquet-Moccetti T., Verbruggen M. Olive (Olea europaea) leaf extract effective in patients with stage-1 hypertension: comparison with Captopril. Phytomedicine. 2011;18:251–258. doi: 10.1016/j.phymed.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 32.Crespo M.C., Tomé-Carneiro J., Burgos-Ramos E., Loria Kohen V., Espinosa M.I., Herranz J., Visioli F. One-week administration of hydroxytyrosol to humans does not activate Phase II enzymes. Pharm. Res. 2015;95–96:132–137. doi: 10.1016/j.phrs.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 33.Andjelkovic M., Van Camp J., Bruno De Meulenaer B., Depaemelaere G., Socaciu C., Verloo M., Verhe R. Iron-chelation properties of phenolic acids bearing catechol and galloyl groups. Food Chem. 2006;98:23. [Google Scholar]
- 34.Salonen J.T., Nyyssönen K., Korpela H., Tuomilehto J., Seppänen R., Salonen R. High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation. 1992;86:803–811. doi: 10.1161/01.cir.86.3.803. [DOI] [PubMed] [Google Scholar]
- 35.Hunnicutt J., He K., Xun P. Dietary iron intake and body iron stores are associated with risk of coronary heart disease in a meta-analysis of prospective cohort studies. J. Nutr. 2014;144:359–366. doi: 10.3945/jn.113.185124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lapice E., Masulli M., Vaccaro O. Iron deficiency and cardiovascular disease: an updated review of the evidence. Curr. Atheroscler. Rep. 2013;15:358. doi: 10.1007/s11883-013-0358-0. [DOI] [PubMed] [Google Scholar]
- 37.Ouyang P., Gottlieb S.H., Culotta V.L., Navas-Acien A. EDTA chelation therapy to reduce cardiovascular events in persons with diabetes. Curr. Cardiol. Rep. 2015;17:96. doi: 10.1007/s11886-015-0656-y. [DOI] [PubMed] [Google Scholar]
- 38.Franchini M., Targher G., Montagnana M., Lippi G. Iron and thrombosis. Ann. Hematol. 2008;87:167–173. doi: 10.1007/s00277-007-0416-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiva-Blanch G., Urpi-Sarda M., Ros E., Valderas-Martinez P., Casas R., Arranz S., Guillén M., Lamuela-Raventós R.M., Llorach R., Andres-Lacueva C., Estruch R. Clin. Nutr. 2013;32:200–206. doi: 10.1016/j.clnu.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 40.Lemos C., Peters G.J., Jansen G., Martel F., Calhau C. Modulation of folate uptake in cultured human colon adenocarcinoma Caco-2 cells by dietary compounds. Eur. J. Nutr. 2007;46:329–336. doi: 10.1007/s00394-007-0670-y. [DOI] [PubMed] [Google Scholar]
- 41.Navarro-Perán E., Cabezas-Herrera J., García-Cánovas F., Durrant M.C., Thorneley R.N., Rodríguez-López J.N. The antifolate activity of tea catechins. Cancer Res. 2005;65:2059–2064. doi: 10.1158/0008-5472.CAN-04-3469. [DOI] [PubMed] [Google Scholar]
- 42.Sánchez-del-Campo L., Sáez-Ayala M., Chazarra S., Cabezas-Herrera J., Rodríguez-López J.N. Binding of natural and synthetic polyphenols to human dihydrofolate reductase. Int J. Mol. Sci. 2009;10:5398–5410. doi: 10.3390/ijms10125398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Halliwell B., Gutteridge J.M.C. Free Radicals in Biology and Medicine. 5th ed. Oxford University Press; Oxford: 2015. [Google Scholar]
- 44.Laranjinha J., Cadenas E. Redox cycles of caffeic acid, alpha-tocopherol, and ascorbate: implications for protection of low density lipoproteins against oxidation. Life. 1999;48:57–65. doi: 10.1080/713803474. [DOI] [PubMed] [Google Scholar]
- 45.Covas M.I., de la Torre K., Farré-Albaladejo M., Kaikkonen J., Fitó M., López-Sabater C., Pujadas-Bastardes M.A., Joglar J., Weinbrenner T., Lamuela-Raventós R.M., de la Torre R. Postprandial LDL phenolic content and LDL oxidation are modulated by olive oil phenolic compounds in humans. Free Radic. Biol. Med. 2006;40:608–616. doi: 10.1016/j.freeradbiomed.2005.09.027. [DOI] [PubMed] [Google Scholar]