Abstract
Background
The first autochthonous Chikungunya virus transmission in Colombia was reported in September 2014. Three months later, every town in the Caribbean region was affected, including the bordering towns of Ovejas and Corozal, in the department of Sucre. The objective of the study was to analyze and compare the temporal dynamics of the outbreak of Chikungunya in two towns of the department of Sucre.
Methods
Households with suspicious cases with clinical symptomatology for Chikungunya were enrolled. In each house an epidemiological questionnaire was applied to collect economic and social information and methods for vector control.
Results
The study analyzed data collected between 09/01/2014 and 01/31/2015; 458 families in Corozal and 516 families in Ovejas were identified with Chikungunya cases. Estimated attack rates were 10,621 cases and 1640 cases per 100,000 inhabitants, in Ovejas and Corozal, respectively. The 75-day survival curve was 27.2% lower (0.632, CI = 0.614–0.651) in Ovejas than in Corozal (0.904, CI = 0.891–0.917). After 120 days, both curves showed a stable horizontal slope, close to a survival probability of 0.54, indicating the end of the epidemic period. The log-rank test (X 2 = 94.6, 1fd, p-value = 0.000) showed the improved survival of Chikungunya in the town of Corozal. The relative risk between the two towns was 0.863 (CI = 0.809–0.921; p-value < 0.001).
Conclusions
The dynamics of the temporal distribution of CHIKV could be influenced by socioeconomic and preventable risk factors. Poor socioeconomic conditions such as the lack and poor efficiency of water supply and waste collection services could be determining factors in the proliferation of CHIKV. The survival analysis proved to be a suitable method for studying the presentation of CHIKV and can be applied to other prevalent vector-borne diseases such as the ZIKA and Dengue.
Keywords: Kaplan meier estimate, Environment and public health, Comparative study, Infectious disease vector, Health economics, Culicidae, Risk management, Demography
Background
Chikungunya virus (CHIKV) is an alphavirus of the Togaviridae family, the etiologic agent of an acute febrile illness that presents with myalgia, rash and severe joint pain, which can be debilitating and persist for months or years [1, 2]. CHIKV generates an excess morbidity that overloads the public health systems [3, 4].
The arrival of CHIKV into the Americas is fairly recent, and the first autochthonous transmission was reported in December 2013 in the island of St. Martin [5, 6]. Currently in the Americas, transmission of the Asian genotype CHIKV [7–9] and East-Central-South African (ECSA) genotype [10] has been reported. According to reports of suspected and confirmed cases of CHIKV in America, the Pan American Health Organization [11] reported more than one million cases in the year 2014. In 2015, 666,311 cases were reported, 54% of which (359,728 cases) were reported in Colombia [12]. In 2016, until epidemiological week #28, 9% of 195,628 reported cases were from Colombia (17.898 cases) [13]. The real burden of disease is underestimated; and an important percentage of underreporting of cases is probably due to the nonattendance of sick people to health centers [14].
In Colombia, the first case of autochthonous transmission of CHIKV took place in September of 2014 in the town of Mahates, Bolivar [15]. Three months later, by epidemiological week #53, 96,687 cases had been reported, 66,118 (68.4%) of which belonged to the Caribbean region and 13,464 (13.9%) were from the department of Sucre. Of the eight probable deaths reports due to CHIKV, two were reported in the department of Sucre, one in Corozal and another in the town of Sincelejo [16]. The spread of the disease can be attributed to the mobilization of people (with viremia or in incubation period) into nearby geographical areas; the towns near main roads have been systematically affected.
The high susceptibility of the Colombian population to CHIKV and the high prevalence of Aedes aegypti have generated a complex epidemiological framework [17], a large number of cases are still being reported with the concomitant high economic and social impact, albeit a marked underreporting trend. The combination of Dengue, Chikungunya and Zika virus complicates the public health problem in the Colombian population where problems due to poverty, poor basic sanitation and poor vector control persist.
Knowledge and follow up regarding the evolution of outbreaks and the identification of causal factors can contribute to the implementation of more effective measures against the disease. Statistical methods such as the survival analysis can be used to understand the temporal variation of any event of interest in public health [18]; including, the temporal dynamics of infectious diseases transmitted by vectors.
The objective of the study was to analyze the temporal evolution between 2014 and 2015 of an epidemic outbreak of Chikungunya in two neighbouring towns in the Caribbean region of Colombia.
Methods
Type of study, area and population
A retrospective study was conducted to describe and analyze the demographic, socioeconomic and epidemiological characteristics of the population in two neighbouring towns affected by an outbreak of Chikungunya. The study area included the urban area of the town of Corozal and Ovejas, in the department of Sucre, Colombia (Fig. 1). The towns of Ovejas and Corozal are separated by 22 km; they have average temperatures of 28 °C and an altitude of 265 and 174 m above sea level, respectively. The areas were selected because of their proximity and because both showed a CHIKV outbreak emergent at the end of 2014. In addition, both are relatively near the town of Mahates, where it likely appeared to the first autochthonous case of this disease in the country [8, 15]. In 2015, the urban population in Ovejas and in Corozal was estimated at 11,947 and 51,157 inhabitants, respectively [19].
Fig. 1.
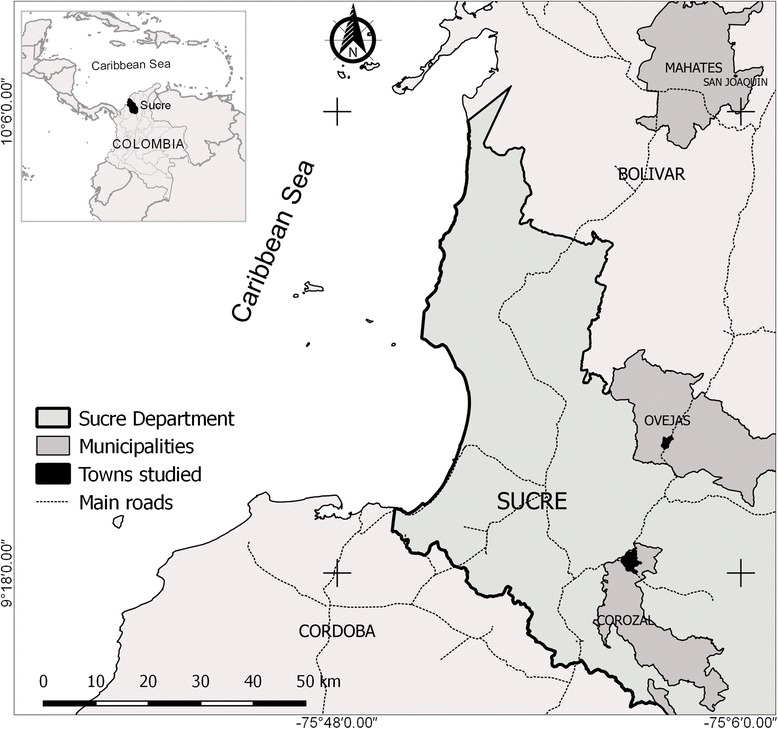
Study area in the towns of Corozal and Ovejas, in the department of Sucre, Colombia
We performed convenience sampling in the two chosen populations, selecting the areas of low socioeconomic level and with environmental conditions favourable to mosquito proliferation, which include proximity to water reservoirs and the accumulation of wastes. In each selected site, households were selected if any of its members had Chikungunya in the previous months and their story matched with the definition for a clinical suspect case from the Colombian National Institute of Health [20].
An epidemiological questionnaire was applied on 01/31/2015 in each selected household. The relevant aspects in the questionnaire included: characteristics of the house, composition of the household, family income, medical care and health expenses due to Chikungunya; public utilities available and predisposing factors associated with the disease; preventive measures to reduce the proliferation and bites of mosquitoes. Potential cases were questioned regarding the beginning of the symptoms of the disease and other clinical aspects.
Data analysis
Data was collected in a spreadsheet using Microsoft Excel®. Frequencies, summary statistics and other descriptive analyses were calculated for the variables under study using the statistical software EpiInfo™, version 7.2.0.1. A p-value < 0.05 was considered statistically significant. Rates of incidence, epidemic curves and survival curves were calculated to analyze the temporal evolution of the outbreak of Chikungunya in the two neighbouring towns affected. Survival analysis used the Kaplan-Meier model [21], which is a non-parametric, analytical and graphic technique that estimates the probability of survival by the maximum likelihood method; the response variable is the time of survival or time-to-event, corresponding to the time elapsed since the initial moment until the occurrence of a certain event; when the event of interest is not observed it is defined as censoring.
In this study the epidemiological event was the presence of clinically suspected cases of Chikungunya and the survival (time-to-event) time was the time it took people to get sick from the appearance of the first case of Chikungunya in the two towns. The Kaplan-Meier estimator was applied using the Survival Analysis package in the statistical software R.
For the survival analysis an additional database was built in which each affected individual living in the houses was characterized according to his/her status for censoring, time of disease and town to which he/she belongs. Individuals who were not ill were considered to be censored data. The log-rank test was used to compare the curves of Chikungunya survival in the towns of Ovejas and Corozal; this test calculate the Chi-square for each time of each event in each group, adds the results and compare between them [18]. In addition, and through contingency tables assessed the possible association between socioeconomic factors and preventive measures that could explain the differences between the survival curves of the two towns.
Results
Affected population and incidence of Chikungunya
The study analyzed data obtained between 09/01/2014 and 01/31/2015. The date of the beginning of the outbreak in the town of Corozal was on 09/05/2014 and in the town of Ovejas on 09/15/2014.
We reported 458 families affected by Chikungunya in Corozal including 1995 residents, of which 839 (42%) became ill. Similarly, we reported 516 families affected in Ovejas, identifying 2605 residents with high risk of exposure, of which 1269 (49%) became ill. An estimated relative risk of 0.863 (CI = 0.809–0.921; p-value <0.001) suggested a protective factor for Chikungunya for the inhabitants of Corozal in relation to the inhabitants of Ovejas.
The attack rate in Ovejas was estimated at 10,621 cases per 100,000 inhabitants, while in Corozal the attack rate was 1640 cases per 100,000 inhabitants (Table 1). Monthly incidence rates of Chikungunya (Table 1, Fig. 2) also showed a higher frequency of cases in Ovejas, which was noticeable during the months of September, October and November. In the months of December and January the incidences in the two towns were similar and descending, showing the end of the epidemic period.
Table 1.
Monthly and cumulative incidences rates of Chikungunya in towns of Ovejas and Corozal
| Ovejas | Corozal | |||||||
|---|---|---|---|---|---|---|---|---|
| Cases | Population | Rate/100000 inhabitans | Cases | Population | Rate/100000 inhabitans | |||
| Months | # | % | # | % | ||||
| September | 203 | 16.0 | 11947 | 1699.2 | 29 | 3.5 | 51157 | 56.7 |
| October | 530 | 41.8 | 11744 | 4512.9 | 82 | 9.8 | 51128 | 160.4 |
| November | 390 | 30.7 | 11214 | 3477.8 | 197 | 23.5 | 51046 | 385.9 |
| December | 137 | 10.8 | 10824 | 1265.7 | 461 | 54.9 | 50849 | 906.6 |
| January | 9 | 0.7 | 10687 | 84.2 | 70 | 8.3 | 50388 | 138.9 |
| Total | 1269 | 100 | 11947 | 10621.9 | 839 | 100 | 51157 | 1640.0 |
Fig. 2.
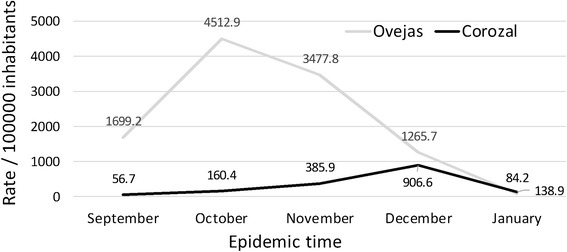
Monthly incidences rates of chikungunya in the towns of Corozal and Ovejas
The epidemic curves of Chikungunya in Corozal and Ovejas are shown in Fig. 3. A high rate of positioning and spread with high variation was observed in Ovejas, and a slow rate with greater stability in Corozal; the decline of the outbreak in the two towns was evidenced by the month of January. The duration of the epidemic in the two towns did not exceed 5 months.
Fig. 3.
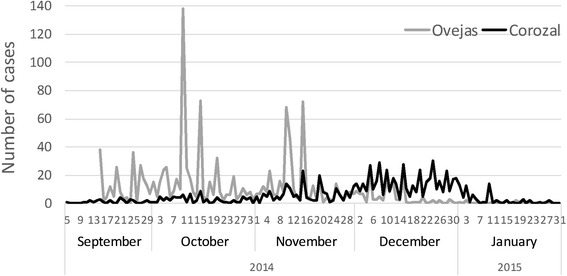
Epidemic curves of chikungunya in the towns of Corozal and Ovejas
Survival to Chikungunya infection
The survival curves generated by the Kaplan-Meier estimator for residents within affected households in the two towns are shown in Fig. 4. The survival curve with the total number of data sampled in two populations (Fig. 4a) showed by the middle of the study period (75 days), a survival probability of 0.75 (CI = 0.738–0.763) and at the end of period (150 days), the proportion fell to 0.54 (CI = 0.528–0.556). After 120 days, a stable horizontal slope was observed, indicating the end of the epidemic period.
Fig. 4.
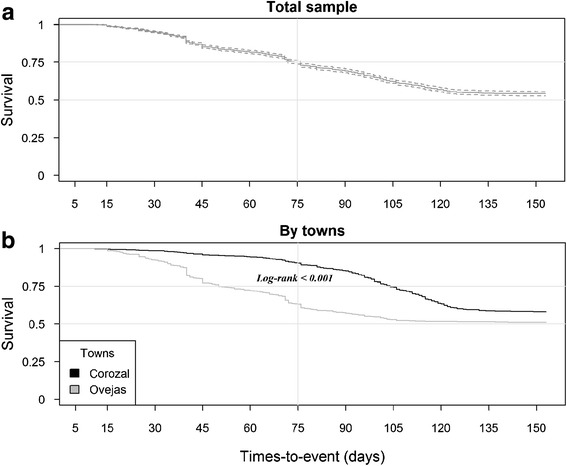
Survival curves for residents affected for chikungunya in Corozal and Ovejas. a Analysis of the total sample. b Comparative analysis between the towns
When comparing the data from the two populations (Fig. 4b), survival curves showed different features. At 75 days, a marked reduction in the survival in Ovejas was observed (0.632, CI = 0.614–0.651); in contrast with the trend observed in Corozal (0.904, CI = 0.891–0.917). However, at the end of the epidemic period the two curves stabilized their slopes, continuing horizontal, parallel and close to a probability of 0.54.
The log-rank test showed high level of statistical significance (X 2 = 94.6, 1fd, p-value = 0.000) between the two curves, evidencing a different survival evolution to Chikungunya among the two populations.
Socioeconomic factors and preventive measures
The results of the survey, which was applied to 516 households affected by Chikungunya in the town of Ovejas and 458 households affected in the town of Corozal are shown in Table 2. The table describes the number and the percentage of households with confirmation of the factors related to the disease, the application of preventive measures and the predisposing factors for proliferation and attack from vectors; Additionally, we present the measures of effect (risk ratio) of these variables for the two towns. High family income (> $USD 269, January/2015), mosquito fogging, mosquito repellent, garbage collection service, fibber cement roof and cement wall are all factors that demonstrated protection in dwellings studied of Corozal. In contrast, health expenditures, medical attention and stored water were variables that indicated risk in dwellings studied of Ovejas. For its part, the variables hospitalization, wire gauze windows, bed net and aqueduct supply were not determined to have significant differences between the two areas.
Table 2.
Households in the towns of Ovejas and Corozal and its association with the epidemic of Chikungunya
| Variables | COROZAL | OVEJAS | Risk ratio | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | Lower | Upper | |||
| High family income | 165 | 34.2 | 105 | 20.3 | 0.713 | 0.628 | 0.808 | 0.000 |
| Health expenditures | 351 | 72.8 | 504 | 97.7 | 2.232 | 2.031 | 2.452 | 0.000 |
| Medical attention | 291 | 60.4 | 363 | 70.4 | 1.248 | 1.098 | 1.418 | 0.001 |
| Hospitalization | 60 | 12.5 | 52 | 10.1 | 0.889 | 0.738 | 1.071 | 0.236 |
| Mosquito fogging | 221 | 45.9 | 0 | 0.0 | 0.336 | 0.304 | 0.371 | 0.000 |
| Mosquito repellent | 113 | 23.4 | 87 | 16.9 | 0.818 | 0.710 | 0.944 | 0.009 |
| Mosquito net | 10 | 2.1 | 19 | 3.7 | 1.413 | 0.852 | 2.343 | 0.131 |
| Wire gauze | 6 | 1.2 | 7 | 1.4 | 1.047 | 0.580 | 1.890 | 0.876 |
| Aqueduct network | 482 | 100.0 | 516 | 100.0 | - - - | - - - | - - - | - - - |
| Stored water | 255 | 52.9 | 512 | 99.2 | 2.956 | 2.670 | 3.272 | 0.000 |
| Garbage Service | 482 | 100.0 | 283 | 54.8 | 0.000 | Undefined | 0.000 | |
| Fiber cement roof | 401 | 83.2 | 232 | 45.0 | 0.350 | 0.287 | 0.428 | 0.000 |
| Cement wall | 450 | 93.4 | 423 | 82.0 | 0.497 | 0.366 | 0.674 | 0.000 |
Discussion
This is the first socioeconomic and demographic study that compared two populations in the Colombian Caribbean that have been severely affected by the chikungunya virus. In a previous study in 2014 that included both rural and urban areas, the department of Sucre was reported to have the second highest incidence of CHIKV in Colombia, with 14,741 cases and an attack rate of 1748 cases/100,000 inhabitants. Within Sucre, Ovejas had ranked second with a cumulative incidence of 4659 cases/100,000 inhabitants and Corozal had the sixth position with a cumulative rate of 2179 cases/100,000 inhabitants [22].
While the present study was exclusively focused on the urban area of the town of Ovejas and Corozal, the presentation of the disease followed the expected trend reported by the previous study [22]. Still, the attack rate by CHIKV in Ovejas (10,621/100,000 inhabitants) was 10 times higher than that observed in Corozal (1640/100,000 inhabitants). This could be evidence of serious problems in populated areas, including the urbanization of Aedes aegypti [23] and poor public health control measures. The attack rate by CHIKV in both cities was high, despite the fact that the outbreak took place in a dry season influenced by the el Niño phenomenon.
A higher frequency of occurrence, higher variability and higher speed of accommodation and spread of the virus was observed in Ovejas when comparing the two epidemic curves. Therefore, it can be asserted that the evolution of the epidemic process was different in the two urban areas. Additionally, the significance obtained from the log-rank test showed a better evolution in survival to CHIKV in Corozal; at 75 days the survival rate was 27.2% higher than that observed in Ovejas. Furthermore, the relative risk represented a protection factor for the inhabitants of Corozal, exhibiting 1.16 times less likely of contracting Chikungunya in comparison with the inhabitants of Ovejas.
Despite the differences in variability, incidence and survival analysis in the two towns, the decrease of the outbreak of Chikungunya took place approximately at 120 days, as it was observed both in the joint estimation of survival and in the separate estimate in the two towns. Previous studies conducted by the National Health Institute of Colombia showed a similar presentation [24, 25].
Socioeconomic factors and preventive measures are determinant in the rate of installation and spread of infectious diseases [26]. When the causal agent, vector and climatic conditions are similar between neighbouring communities, the differences in the evolution of the epidemic process can only be explained by their different socioeconomic conditions and their preventive measures.
Because the epidemiological questionnaire assessed the socioeconomic aspects and prevention against Chikungunya in the surveyed households and it specifies the time until the presentation of the event, no additional information is available in the residents to be associated through the Cox proportional hazards model that are normally applied in conjunction with the survival analysis [27]. However, public health aspects studied in households were able to identify either protective factors or risk factors for Chikungunya in the two towns that could be related with the best or worst epidemiological presentation of Chikungunya in the studied populations.
The two towns had water supply service; however, all the studied houses in Ovejas and the half houses in Corozal, they often stored water in tanks, a consequence of the intermittence or irregular water supply by aqueduct service. From a preventive point of view, the higher rate of storage water in tanks, the higher accumulation of wastes, the low frequency of applied insecticide spray and the low use of repellents by people in the urban area of Ovejas, produced the favourable conditions for the proliferation of mosquitoes and for the transmission of Chikungunya. Additionally, the deficient structural housing conditions allows for easier entry of mosquitoes. Finally, the high number of families with low income in Ovejas is a fundamental factor associated with a high health vulnerability.
Overall, better sanitary conditions were observed in Corozal than in Ovejas. These results agree with the official socioeconomic characterization defined by the National Administrative Statistics State of Colombia [19] through which the urban and rural area of Corozal shows better socioeconomic conditions than the municipality of Ovejas.
Conclusions
The dynamics of the temporal distribution of CHIKV is influenced by socioeconomic and preventives factors. Precarious socioeconomic conditions, such as inefficient water supply and waste collection services, may be determining factors in the proliferation of CHIKV. The survival analysis proved to be an appropriate method to analyze the temporal presentation of CHIKV and can be applied to other infectious diseases transmitted by vectors with a similar performance, as is the case of the Dengue and ZIKA arboviruses. The timely intervention of outbreaks with an analysis such as the one presented in this study, may be a useful tool for an efficient response towards the control of the epidemic outbreaks that may occur in the future.
Acknowledgements
To the municipal health town of Ovejas (Dr. Miladis Lambrano), to the public health department of Sucre (Dr. Manolo Olivares) and to the staff of the Biological Tropical Research Institute (IIBT), of Universidad de Cordoba, especially to Jose Aponte, Hector Contreras, Yeneiris Villero, Vanesa Tique and Samia Barrera. To the University of Cordoba, Colombia. To Dr. Carlos Sanchez MD, for his gramar and style corrections of the manuscript.
Funding
Corporacion Universitaria del Caribe - CECAR, small funding grant: “Epidemic surveillance and perception of the illness of the Chikungunya virus in the social context of the inhabitants of the municipalities of Corozal and Ovejas, Sucre”. Code: AM50501010303009. University of Cordoba, sustainability agenda of research groups code: FMV-01-16.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Authors’ contributions
SM, GA, NM, LG and MOP conceived and designed the study; MOP, NM and SM conducted data management and analysis; MOP, NM, SM and GA wrote the manuscript. All the authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethics committee of the Tropical Biological Research Institute, and took into account technical, scientific, ethics and administrative standards for health research stipulated by the Ministry of Health of Colombia according to resolution No. 008430/1993 [28] and the international Ethics standards of Helsinki [29]. The purpose of the study was explained to individuals who participated on a voluntary interview the basis of the work, participants signed an informed consent and confidentiality was kept at all the time.
Contributor Information
Misael Oviedo-Pastrana, Email: mpastrana@outlook.com.
Nelson Méndez, Email: nemendez15@gmail.com.
Salim Mattar, Phone: (094) 756 9027, Email: mattarsalim@hotmail.com.
Germán Arrieta, Email: arrietager@yahoo.es.
Luty Gomezcaceres, Email: luty.gomezcaceres@cecar.edu.com.
References
- 1.Sasaki Y, Manda S, Sato T, Maeda T, Miyazaki T, Nakanishi K, Urita Y. Chikungunya virus infection presenting with persistent arthralgia without fever. J Gen Fam Med. 2015;16:204–207. doi: 10.14442/jgfm.16.3_204. [DOI] [Google Scholar]
- 2.Larrieu S, Pouderoux N, Pistone T, Filleul L, Receveur M-C, Sissoko D, Ezzedine K, Malvy D. Factors associated with persistence of arthralgia among chikungunya virus-infected travellers: report of 42 French cases. J Clin Virol. 2010;47:85–88. doi: 10.1016/j.jcv.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Seyler T, Hutin Y, Ramanchandran V, Ramakrishnan R, Manickam P, Murhekar M. Estimating the burden of disease and the economic cost attributable to chikungunya, Andhra Pradesh, India, 2005–2006. Trans R Soc Trop Med Hyg. 2010;104:133–138. doi: 10.1016/j.trstmh.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 4.Rougeron V, Sam I-C, Caron M, Nkoghe D, Leroy E, Roques P. Chikungunya, a paradigm of neglected tropical disease that emerged to be a new health global risk. J Clin Virol. 2015;64:144–152. doi: 10.1016/j.jcv.2014.08.032. [DOI] [PubMed] [Google Scholar]
- 5.Leparc-Goffart I, Nougairede A, Cassadou S, Prat C, de Lamballerie X. Chikungunya in the Americas. Lancet. 2014;383:514. doi: 10.1016/S0140-6736(14)60185-9. [DOI] [PubMed] [Google Scholar]
- 6.Lancet Chikungunya—coming to America. Lancet. 2014;383:488. doi: 10.1016/S0140-6736(14)60167-7. [DOI] [PubMed] [Google Scholar]
- 7.Gay N, Rousset D, Huc P, Matheus S, Ledrans M, Rosine J, Cassadou S, Noel H: Seroprevalence of Asian Lineage Chikungunya Virus Infection on Saint Martin Island, 7 Months After the Emergence. Am J Trop Med Hyg. 2013;2016(94):393–396. doi: 10.4269/ajtmh.15-0308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattar S, Miranda J, Pinzon H, Tique V, Bolanos A, Aponte J, Arrieta G, Gonzalez M, Barrios K, Contreras H, et al. Outbreak of chikungunya virus in the north Caribbean area of Colombia: clinical presentation and phylogenetic analysis. J Infect Dev Ctries. 2015;9:1126–1132. doi: 10.3855/jidc.6670. [DOI] [PubMed] [Google Scholar]
- 9.Lanciotti RS, Lambert AJ. Phylogenetic analysis of chikungunya virus strains circulating in the Western hemisphere. Am J Trop Med Hyg. 2016;94:800–803. doi: 10.4269/ajtmh.15-0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nunes MRT, Faria NR, de Vasconcelos JM, Golding N, Kraemer MUG, de Oliveira LF, Azevedo RSS, da Silva DEA, da Silva EVP, da Silva SP, et al. Emergence and potential for spread of Chikungunya virus in Brazil. BMC Med. 2015;13:102. doi: 10.1186/s12916-015-0348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.OPS/OMS. Chikungunya: Datos estadísticos. Washington, D.C. 20037, United States of America. 2016. http://www.paho.org/hq/index.php?option=com_topics&view=readall&cid=5932&Itemid=40931&lang=es. Accessed 1 Aug 2016.
- 12.Instituto Nacional de Salud (Colombia). Boletín Epidemiológico semanal; Semana epidemiológica número 52 de 2015. http://www.ins.gov.co/boletin-epidemiologico/Boletn%20Epidemiolgico/2015%20Boletin%20epidemiologico%20Semana%2052.pdf. Accessed 1 Aug 2016.
- 13.Instituto Nacional de Salud (Colombia). Boletín Epidemiológico semanal; Semana epidemiológica número 28 de 2016. http://www.ins.gov.co/boletin-epidemiologico/Boletn%20Epidemiolgico/2016%20Bolet%C3%ADn%20epidemiol%C3%B3gico%20semana%2028.pdf. Accessed 1 Aug 2016.
- 14.Méndez N, Causil L, Contreras H, Bolanos A, Aponte J, Mattar S, Calderón A, Alvis N, Arrieta G. Encuesta epidemiológica sobre el virus del chikunguña en Ovejas, Sucre. Biomedica. 2015;35:110–111. [Google Scholar]
- 15.Martínez M, Gómez S. Chikungunya en Colombia, el inicio de la transmisión autóctona, 2014. IQUEN. 2014;19(18):260–279. [Google Scholar]
- 16.Instituto Nacional de Salud (Colombia). Boletín Epidemiológico semanal; Semana epidemiológica número 53 de 2014. http://www.ins.gov.co/boletin-epidemiologico/Boletn%20Epidemiolgico/2014%20Boletin%20epidemiologico%20semana%2053.pdf. Accessed 26 Apr 2016.
- 17.Ministerio de Salud y Protección Social (Colombia). Plan nacional de respuesta frente a la introducción del virus Chikungunya en Colombia. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ET/PLAN%20NACIONAL%20DE%20RESPUESTA%20CHIKUNGUNYA%20COLOMBIA%202014.pdf. Accessed 26 Apr 2016.
- 18.Rich JT, Neely JG, Paniello RC, Voelker CC, Nussenbaum B, Wang EW. A practical guide to understanding Kaplan-Meier curves. Otolaryngol Head Neck Surg. 2010;143:331–336. doi: 10.1016/j.otohns.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DANE. Censo general 2005, Informe de Conyuntura Económica. Colombia. http://www.dane.gov.co/files/icer/2004/sucre/t2.pdf. Accessed 30 Apr 2016.
- 20.Instituto Nacional de Salud (Colombia). Lineamientos de vigilancia en salud pública, entomológica y de laboratorio ante la transmisión autóctona del virus Chikungunya Fase II. http://www.ins.gov.co/lineas-de-accion/Subdireccion-Vigilancia/informacion-epidemiologica/Lineamientos/Lineamientos%20de%20vigilancia%20chikungunya%202014.pdf. Accessed 26 Apr 2016.
- 21.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 22.Rodriguez-Morales AJ, Cárdenas-Giraldo EV, Montoya-Arias CP, Guerrero-Matituy EA, Bedoya-Arias JE, Ramírez-Jaramillo V, Villamil-Gómez WE. Mapping chikungunya fever in municipalities of one coastal department of Colombia (Sucre) using geographic information system (GIS) during 2014 outbreak: Implications for travel advice. Travel Med Infect Dis. 2015;13:256. doi: 10.1016/j.tmaid.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Horwood P, Buchy P. Chikungunya. Rev Sci Tech. 2015;34:479–489. doi: 10.20506/rst.34.2.2373. [DOI] [PubMed] [Google Scholar]
- 24.Campo A, Martínez M, Benavides M, Constanza N. Brote de chikungunya en el municipio de San Juan Nepomuceno, Bolivar, Colombia. Informe Quincenal Epidemiológico Nacional. 2014;20:1–20. [Google Scholar]
- 25.Castillo J, Walteros D, Herrera N, Cochero S. Brote fiebre por virus Chikungunya en Ovejas, Sucre, septiembre de 2014. Informe Quincenal Epidemiológico Nacional. 2015;20:205–218. [Google Scholar]
- 26.Fritzell C, Raude J, Adde A, Dusfour I, Quenel P, Flamand C. Knowledge, attitude and practices of vector-borne disease prevention during the emergence of a New arbovirus: implications for the control of chikungunya virus in French Guiana. PLOS Negl Trop Dis. 2016;10:e0005081. doi: 10.1371/journal.pntd.0005081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stel VS, Dekker FW, Tripepi G, Zoccali C, Jager KJ. Survival analysis II: Cox regression. Nephron Clin Pract. 2011;119:c255–c260. doi: 10.1159/000328916. [DOI] [PubMed] [Google Scholar]
- 28.República de Colombia, Ministerio de Salud. Resolución N° 008430 del 4 de octubre del 1993. Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud.
- 29.World Medical Association. WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects. 2016. http://www.wma.net/en/30publications/10policies/b3/index.html. Accessed 4 Aug 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.


