Abstract
Objective
To evaluate the utility of clinical history, radiographic and physical exam findings in the diagnosis of symptomatic meniscal tear (SMT) in patients over age 45, in whom concomitant osteoarthritis is prevalent.
Methods
In a cross-sectional study of patients from two orthopedic surgeons’ clinics we assessed clinical history, physical examination and radiographic findings in patients over 45 with knee pain. The orthopedic surgeons rated their confidence that subjects’ symptoms were due to MT; we defined the diagnosis of SMT as at least 70% confidence. We used logistic regression to identify factors independently associated with diagnosis of SMT and we used the regression results to construct an index of the likelihood of SMT.
Results
In 174 participants, six findings were associated independently with the expert clinician having ≥70% confidence that symptoms were due to MT: localized pain, ability to fully bend the knee, pain duration <1 year, lack of varus alignment, lack of pes planus, and absence of joint space narrowing on radiographs. The index identified a low risk group with 3% likelihood of SMT.
Conclusion
While clinicians traditionally rely upon mechanical symptoms in this diagnostic setting, our findings did not support the conclusion that mechanical symptoms were associated with the expert’s confidence that symptoms were due to MT. An index that includes history of localized pain, full flexion, duration <1 year, pes planus, varus alignment, and joint space narrowing can be used to stratify patients according to their risk of SMT and it identifies a subgroup with very low risk.
Keywords: meniscal tear, knee osteoarthritis
INTRODUCTION
Meniscal tears are frequently associated with knee symptoms and functional limitations. The menisci are semilunar-shaped cartilaginous structures in the knee joint that provide load transmission, shock absorption and joint stability.1,2 Tears in the menisci disrupt these functions and are associated with articular cartilage damage.3–7 Meniscal tears can be classified as degenerative or traumatic, with degenerative tears typically occurring in patients over 45.7,8 While approximately one-third of middle-aged and older adults have evidence of meniscal tear on magnetic resonance imaging (MRI), the great majority of these tears are asymptomatic.8 Similarly, while up to 80% of adults with knee osteoarthritis (OA) have imaging evidence of meniscal tear, patients with OA and meniscal tear do not differ in the severity of knee symptoms from those with OA and no tear.4
Given that many individuals with evidence of meniscal tear on MRI are asymptomatic, clinicians rely heavily upon the history and physical examination to identify patients whose symptoms can be attributed to the meniscal tear. In particular, clinicians typically elicit a history of mechanical symptoms including locking, clicking, popping, localized pain, and giving way. In a prior retrospective study, we found that these mechanical symptoms had modest diagnostic value in the diagnosis of symptomatic meniscal tear, and that the diagnostic value depends in part upon the clarity with which these mechanical symptoms are elicited.9 The diagnostic value of the physical exam has been assessed in younger patients, with studies suggesting that joint line tenderness, McMurray’s maneuver and Apley’s maneuver are the most useful physical findings.10,11 However, there has been limited study of the utility of the clinical history and physical exam in the diagnosis of a symptomatic meniscal tear in older individuals, in whom osteoarthritis is prevalent and poses another potential source of knee pain. To address this research gap, we evaluated the value of history and physical exam findings in the recognition of symptomatic meniscal tears in a sample of patients over the age of 45 reporting knee pain.
METHODS
Design
We performed a cross-sectional study of subjects greater than 45 years old to examine associations between findings on a standardized clinical history, physical examination, and radiographic findings and the likelihood of symptomatic meniscal tear (SMT), defined on the basis of the impression of an expert clinician.
Patient Sample
Patients were recruited from the clinics of two academic orthopedic surgeons at Brigham and Women’s Hospital in Boston, MA. Patients presenting to the clinic with knee pain were considered eligible if they were older than 45 years old, spoke English, and presented with unilateral knee pain. Patients who underwent knee surgery within the prior 5 years, had a prior total knee arthroplasty (TKA), presented with bilateral knee complaints, or had a prior visit to the same clinician within the past year were excluded from the study.
Data Collection Procedures
Patients who provided informed consent to participate met with a research assistant, who administered a questionnaire and performed a standardized musculoskeletal physical exam. Research assistants were trained in the physical examination by an expert clinician. The attending orthopedic surgeon, who was blinded to the findings of the standardized history and physical exam, rated his confidence that the patient’s symptoms were due to meniscal tear and provided a primary clinical diagnosis for the patient’s symptoms. Enrolled subjects who also had radiographs available via the electronic medical record were included in our analytic cohort.
Patient Questionnaire and Physical Exam
We obtained information on mechanical symptoms (e.g. catching, locking, swelling, giving way) with Likert responses that captured the frequency and severity of these symptoms within the preceding three months.9 The questionnaire also included weight, height, and demographic information, including age, sex, and race/ethnicity.
Data recorded during the physical exam included varus or valgus knee alignment, pes planus or cavus, and location of knee pain or tenderness. Additionally, the research assistant administered several provocative tests, such as the McMurray maneuver, Apley compression and Waldron tests.12–16 The protocols used to perform and evaluate these physical examination maneuvers are provided in the Appendix.
A research staff member trained in knee radiographic assessment documented radiographic information, including osteophytes and joint space narrowing (JSN) on a 4-point scale (0–3, with 0 denoting normal and 3 the most severe findings) according to the Osteoarthritis Research Society International (OARSI) guidelines.17 Osteophytes were evaluated in four compartments: lateral femoral, medial femoral, lateral tibial, medial tibial. JSN was recorded for the lateral and medial aspects. Along with individual osteophyte and JSN scores, we calculated a Kellgren–Lawrence (KL) grade and OARSI Summary Score for each subject with radiographs available.
Physician Assessment
After evaluating the patient clinically in the office visit, the orthopedist indicated his confidence that the patient’s symptoms were due to a meniscal tear. The surgeon endorsed a level of confidence from 0% (certain that the patient’s symptoms were not due to a meniscal tear) to 100% (certain that the patient’s symptoms were due to a meniscal tear). The surgeon then indicated the primary diagnosis he thought was responsible for the patient’s symptoms. The surgeon chose from a list of possible primary diagnoses that included symptomatic meniscal tear, patellofemoral OA, tricompartmental or tibiofemoral OA, symptomatic meniscal tear AND OA, rheumatoid arthritis, patellofemoral syndrome, symptomatic anterior cruciate or medial collateral ligament tear, or other.
Statistical Analyses
We defined the primary outcome as the physician’s confidence that the patient’s symptoms were due to meniscal tear, which we dichotomized at 70%. We chose this threshold both because it is clinically sensible and because the distribution of confidence scores revealed a cluster at 70% and greater. The secondary outcome was the expert clinician’s impression of the primary diagnosis of SMT. We performed bivariate analyses of the associations of history, physical examination, and radiographic findings with this primary outcome. History, physical exam, and radiographic findings associated with the primary outcome in bivariate analyses (at p < 0.05; or odds ratio (OR) > 1.5 or OR < 0.67) were advanced to multivariate logistic regression models. Findings associated in the model (at p < 0.05; OR > 1.5 or OR < 0.67) with physician confidence that symptoms were due to SMT were included in an additive index. Based on the results of the logistic regression model, we assigned weights for factors included in the additive index roughly proportional to the adjusted odds ratios. We then calculated the proportion of subjects with particular index scores for whom the expert clinician indicated ≥70% confidence that the symptoms were due to meniscal tear.
We tested the robustness of the regression model by performing 30 separate models of random sub-samples of 160 (~92%) of the 174 subjects. These models yielded a distribution of 30 parameter estimates for each of the predictor variables. We examined the 95% CI of these parameter estimates.
We performed a set of sensitivity analyses using the secondary outcome: diagnosis of SMT by the expert clinician. We examined the proportion of patients assigned as SMT by clinicians in each additive index score category.
RESULTS
Enrollment
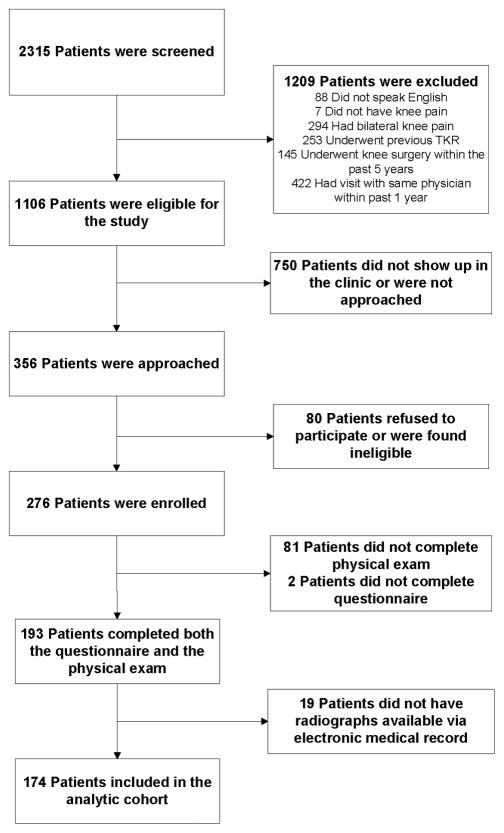
During the period of December 2011 through May 2014 we screened 2,315 patients aged 45 or greater seeing one of the orthopedic surgeons for knee pain. We excluded 1,209 patients upon reviewing the electronic medical record (Figure 1). Another 750 patients did not show up in clinic or were not approached by research coordinators, leaving 356 patients who were approached in the clinic. Of these, 79 (22%) refused and 276 agreed to participate; 193 (71%) of the 276 completed both the questionnaire and the physical examination and comprised the study sample. Of the 193 patients who completed the questionnaire and physical examination, 174 had radiographs available via the electronic medical record and were included in our final analytic cohort. Demographic characteristics were similar between subjects included in our analytic cohort and those excluded.
Figure 1.
This figure depicts the flow of subjects through screening and enrollment. 2,315 patients were assessed for eligibility, of whom 1,106 were deemed eligible for the study. Of the eligible patients who agreed to participate, 193 completed both the questionnaire and musculoskeletal exam. Of these, 19 did not have radiographs available for review, leaving 174 included in the analyses presented here.
Sample Characteristics
The mean age of participants was 63 (SD 9), with 63% of subjects greater than 60 years old. Forty percent were male, and one-third of subjects had body mass index greater than 30kg/m2. The subjects had moderate to severe knee pain and functional limitation with WOMAC Pain and Function scores of 36 (SD 19) and 34 (SD 21) respectively (0–100 scale, with 100 worst). On radiography, approximately 90% of subjects had evidence of JSN and 97% presented with an osteophyte in at least one compartment. Fifty-six percent of subjects with JSN had a maximum JSN score of 1, and 32% of those with an osteophyte had a maximum osteophyte score of 1, indicating mild JSN or osteophyte size.
Prevalence of symptomatic meniscal tear
The physician reported ≥70% confidence that symptoms were due to meniscal tear in 42 (24%) subjects and assigned 40 (23%) subjects a primary diagnosis of symptomatic meniscal tear. Another 24 (14%) subjects had primary diagnosis of symptomatic meniscal tear AND osteoarthritis. The expert physicians assigned 94 subjects (54%) a primary diagnosis of OA.
Bivariate associations between history, physical examination, radiographic findings and physician’s confidence in diagnosis of symptomatic meniscal tear (Table 1)
Table 1.
Associations between clinical history, physical examination, and x-ray features of study participants and expert clinician’s confidence that the symptoms arise from meniscal tear
| Characteristic | Confidence ≥ 70% N=42 N (%) |
Confidence < 70% N=132 N (%) |
OR (95% CI) |
|---|---|---|---|
|
Demographics
| |||
| Age > 60 | 29 (69%) | 81 (61%) | 1.40 (0.67, 2.95) |
| Female sex | 26 (62%) | 72 (55%) | 1.35 (0.67, 2.76) |
| BMI < 30 | 35 (85%) | 75 (58%) | 4.28 (1.68, 10.88) |
|
| |||
|
Clinical Symptoms
| |||
| Duration of pain < 1 year | 40 (95%) | 84 (65%) | 10.95 (2.53, 47.39) |
| Localized pain to one spot | 20 (48%) | 34 (26%) | 2.54 (1.23, 5.22) |
| Grinding | 14 (34%) | 66 (51%) | 0.50 (0.24, 1.04) |
| Swelling | 28 (67%) | 91 (70%) | 0.86 (0.41, 1.80) |
| Can flex knee fully | 35 (88%) | 92 (70%) | 3.04 (1.11, 8.34) |
| Clicking | 8 (19%) | 41 (32%) | 0.50 (0.21, 1.17) |
| Locking | 9 (23%) | 35 (27%) | 0.80 (0.34, 1.84) |
| Catching | 12 (29%) | 40 (32%) | 0.90 (0.42, 1.94) |
| Popping | 18 (43%) | 53 (41%) | 1.09 (0.54, 2.20) |
| Giving Way | 25 (63%) | 78 (61%) | 1.05 (0.50, 2.18) |
|
| |||
|
Physical Examination
| |||
| Varus alignment | 5 (12%) | 35 (27%) | 0.36 (0.13, 0.99) |
| Pes planus | 6 (14%) | 60 (47%) | 0.19 (0.08, 0.49) |
| Medial joint line tenderness | 15 (36%) | 39 (30%) | 1.28 (0.62, 2.67) |
| Crepitus on Waldron test | 21 (54%) | 71 (64%) | 0.66 (0.31, 1.38) |
| Pain on McMurray Maneuver | 20 (48%) | 44 (34%) | 1.76 (0.87, 3.56) |
| Apley grind test | 5 (12%) | 12 (10%) | 1.31 (0.43, 3.96) |
|
| |||
|
X-Ray Findings
| |||
| Presence of osteophyte | 39 (93%) | 129 (98%) | 0.30 (0.06, 1.56) |
| Presence of joint space narrowing | 32 (76%) | 125 (95%) | 0.18 (0.06, 0.51) |
| KL Grade 0, 1 | 27 (64%) | 36 (27%) | 4.80 (2.29, 10.04) |
| OARSI Summary Score < 6 | 30 (71%) | 50 (38%) | 4.10 (1.92, 8.73) |
On history and clinical symptoms, the expert clinicians were more likely to indicate ≥70% confidence that the patient’s symptoms were due to meniscal tear in subjects with BMI < 30 kg/m2 than in those with BMI ≥ 30 kg/m2 (OR 4.28, 95% CI 1.68, 10.88). Pain duration less than one year (OR 10.95, 95% CI 2.53, 47.39), pain localized to one spot (OR 2.54, 95% CI 1.23, 5.22), and ability to fully flex the knee (OR 3.04, 95% CI 1.11, 8.34) were also associated with increased likelihood of clinicians’ indicating ≥70% confidence that symptoms were due to meniscal tear. Of note, we did not find clinically important or statistically significant associations between swelling, grinding, clicking, locking, catching, popping and giving way and the physician’s confidence that the symptoms were due to meniscal tear.
On physical examination, absence of varus alignment (OR 2.78, 95% CI 1.01, 7.69) and absence of pes planus (OR 5.26, 95% CI 2.04, 12.50) were associated with greater odds of ≥70% physician confidence in the diagnosis of SMT. (Note that we present the ORs associated with the absence of the finding in the text so that the ORs are all positive, for consistency and ease of interpretation).
The expert clinicians were more likely to indicate ≥70% confidence that the subject’s symptoms were due to meniscal tear in subjects with absence of JSN (OR 5.56 95% CI 1.96, 16.67), KL grade of 0 or 1 (OR 4.80, 95% CI 2.29, 10.04), and OARSI summary score < 6 (OR 4.10, 95% CI 1.92, 8.73). Presence of osteophytes was not associated with clinicians’ confidence that the symptoms were due to meniscal tear. As presence of JSN is a practical measure frequently used in a clinical setting, radiographic evidence of JSN, but not KL grade or OARSI summary score, progressed into the multivariate model.
Multivariate associations between history, physical examination, radiographic findings and physician’s confidence in diagnosis of symptomatic meniscal tear
In the logistic regression model, six findings were associated with greater likelihood that the expert clinician indicated ≥70% confidence that pain was due to meniscal tear (Table 2). These included localized pain (OR 2.14, 95% CI 0.89, 5.19), ability to bend knee fully (OR 3.42, 95% CI 1.09, 10.71), duration of pain < 1 year (OR 10.46, 95% CI 1.89, 57.77), lack of varus alignment (OR 4.22, 95 % CI 1.30, 13.73), lack of pes planus (OR 5.90, 95% CI 1.90, 18.31), and lack of JSN on x-ray (OR 8.37, 95% CI 2.24, 31.36; Table 2). Other factors that had statistically significant bivariate associations with physician confidence in the diagnosis, such as obesity, dropped out of the multivariable model.
Table 2.
Logistic regression model of clinical, radiographic and physical examination features associated with physician confidence ≥70% in diagnosis of symptomatic meniscal tear
| Characteristic | Adjusted OR | 95% CI | Additive Index Value |
|---|---|---|---|
| Local vs. diffuse pain | 2.1 | 0.9 – 5.2 | 1 |
| Bending knee freely vs. with restriction | 3.4 | 1.1 – 10.7 | 1 |
| Duration of pain < 1 year | 10.5 | 1.9 – 57.8 | 4 |
| Absence of genu varum vs. varum | 4.2 | 1.3 – 13.7 | 2 |
| Absence of pes planus vs. planus | 5.9 | 1.9 – 18.3 | 2 |
| Absence of joint space narrowing vs. presence | 8.4 | 2.2 – 31.4 | 4 |
Additive Index
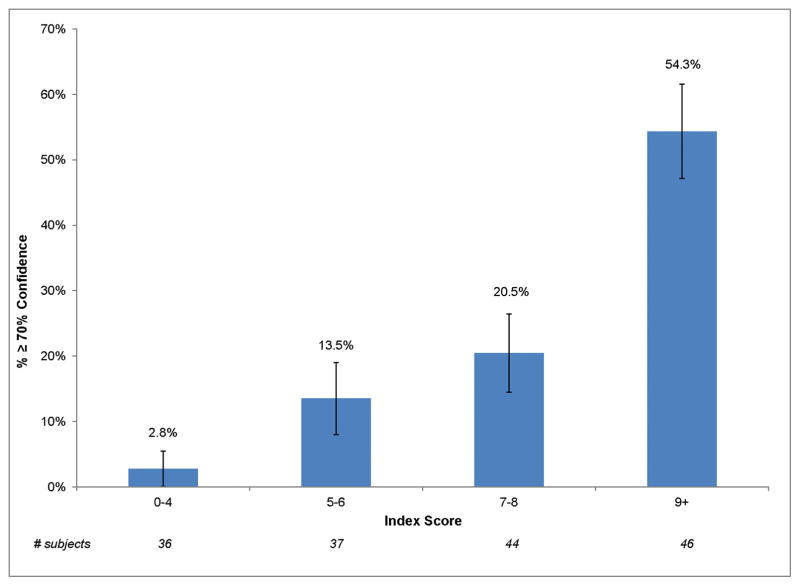
Based upon these regression results, we constructed an additive index of the likelihood of meniscal tear proportional to the adjusted OR. We assigned two findings a value of one point (localized pain and ability to fully bend knee), two a value of two points (lack of varus alignment and lack of pes planus), and two a value of four points (duration of pain < 1 year and lack radiographic evidence of JSN). Greater index scores were associated with increasing likelihood that the expert clinician had ≥70% confidence that symptoms were due to meniscal tear (Table 3, Figure 2). The data in Table 3 show that select history and physical examination findings identified a group of 36 subjects (22% of the sample) with very low (3%) risk of SMT and a group of 46 subjects (28% of the sample) with a risk of 54%.
Table 3.
Association between index score and expert physician confidence in the diagnosis of symptomatic meniscal tear
| Confidence | Index Score N % |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Total | |
| < 70% | 2 100% |
15 100% |
8 89% |
10 100% |
9 100% |
23 82% |
19 95% |
16 67% |
14 50% |
5 56% |
1 50% |
1 25% |
0 0% |
123 |
| ≥ 70% | 0 0% |
0 0% |
1 11% |
0 0% |
0 0% |
5 18% |
1 5% |
8 33% |
14 50% |
4 44% |
1 50% |
3 75% |
3 100% |
40 |
| Total | 2 | 15 | 9 | 10 | 9 | 28 | 20 | 24 | 28 | 9 | 2 | 4 | 3 | 163 |
|
| ||||||||||||||
| Sensitivity | 1.00 | 1.00 | 1.00 | 0.98 | 0.98 | 0.98 | 0.85 | 0.83 | 0.63 | 0.28 | 0.18 | 0.15 | 0.08 | |
| Specificity | 0.00 | 0.02 | 0.14 | 0.20 | 0.28 | 0.36 | 0.54 | 0.70 | 0.83 | 0.94 | 0.98 | 0.99 | 1.00 | |
Footnote: Final model included 163 subjects from the analytic cohort who had responses to all six predictor variables included.
Figure 2.
The proportion of subjects in whom the expert clinician indicated ≥70% confidence in the diagnosis of symptomatic meniscal tear is shown for each index score category. Higher index scores were associated with a greater likelihood that the clinician had ≥70% confidence that the symptoms were due to meniscal tear.
To test the robustness of the multivariate model that gave rise to the index, we replicated the model thirty times randomly selecting partial data sets of 160 subjects from the full sample. In each of these models, the means of the parameter estimates (log OR) for each of the predictor variables shown in Table 2 did not change by more than 4%, supporting the robustness of the model.
Diagnosis of symptomatic meniscal tear (Table 4)
Table 4.
Sensitivity analysis: Patients’ risk of SMT as defined by additive index and physician’s diagnosis of SMT
| Index Score Range | Physician’s Diagnosis of SMT n (%) |
|
|---|---|---|
| No | Yes | |
| 0 – 4 | 33 (94%) | 2 (6%) |
| 5 – 6 | 24 (65%) | 13 (35%) |
| 7 – 8 | 29 (66%) | 15 (34%) |
| 9+ | 14 (30%) | 32 (70%) |
Footnote: Final model included 162 subjects from the analytic cohort who had responses to all six predictor variables and physician’s primary diagnosis documented. SMT, symptomatic meniscal tear.
The index was also effective in stratifying subjects according to the secondary outcome, the expert physician’s suspected primary diagnosis. Two (6%) patients out of 36 in the group with the lowest scores on the index (0–4) were assigned a diagnosis of SMT by clinicians, whereas 32 (70%) out of 46 in the group with the highest additive index scores (9+) were assigned an SMT diagnosis by clinicians.
DISCUSSION
Up to one-third to one-half of individuals greater than 45 years old have imaging evidence of meniscal tear.8 While the majority of these tears are asymptomatic, over 500,000 arthroscopic partial meniscectomies are performed annually in the US.18 The large number of surgical procedures performed for meniscal tear attests to the frequency with which the diagnosis of symptomatic meniscal tear is made and suggests that this diagnosis frequently leads to consideration of surgery. These observations and the conflicting results of randomized controlled trials of surgical therapy in patients with degenerative meniscal tear highlight the importance of making an accurate diagnosis of symptomatic meniscal tear.19–22
The sample of middle age and older subjects with knee pain in this study had an overall prevalence of symptomatic meniscal tear, as judged by an expert clinician, of 24%. The findings of this study suggest that the history, physical exam, and radiographic findings can indeed help in the diagnosis of symptomatic meniscal tear. The index derived from the most diagnostically valuable history, physical examination, and x-ray findings appears to identify a low risk group comprised of 22% of the sample with less than 5% risk that likely requires no further evaluation for symptomatic meniscal tear. The index also identified a higher risk group comprised of 28% of the sample with risk of 54% in whom further evaluation (e.g. with imaging tests) may help clinicians develop a firm diagnosis and contemplate invasive management with injections or surgery. Our secondary analyses, which used the clinicians’ stated primary diagnosis rather than their confidence in the diagnosis of symptomatic meniscal tear, produced similar results.
However, our findings also warn that the traditional emphasis on the value of “mechanical symptoms” – clicking, catching, popping, giving way, swelling – in the diagnosis of symptomatic meniscal tear may have limited utility in middle aged and older patients with knee pain. Our data suggest that in this population a history of localized (as opposed to diffuse) knee pain lasting less than one year favored the diagnosis of symptomatic meniscal tear; whereas, findings of pes planus, varus deformity, and lack of full knee flexion as well as severity of joint space narrowing suggested alternative diagnoses (generally osteoarthritis). Our prior study, which demonstrated a role for mechanical symptoms in the diagnosis of symptomatic meniscal tear had a younger population (mean age 52), perhaps accounting for the difference in findings regarding the value of meniscal symptoms in the diagnosis of meniscal tear.9
We acknowledge several limitations. There is no gold standard for the diagnosis of symptomatic meniscal tear. In particular, while it is tempting to invoke an objective criterion, such as evidence of tear on MRI scan, ample data suggest that many tears seen on MRI are asymptomatic 4,5,8 In the absence of a gold standard, an expert clinician’s opinion is frequently used as the best approach to making the diagnosis, which has been employed in several prior research studies.23–28 This study was conducted in a single referral center and involved just two orthopedic practices. Further research involving a greater number of expert clinicians and practices would enhance generalizability. The diagnosis of meniscal tear was made by one physician in the course of clinical care. We recognize that consensus by two or more clinical experts could increase the reliability of the diagnosis of symptomatic meniscal tear. Research coordinators were carefully trained to conduct the physical examination; however, no formal reliability testing was conducted. Although subjects were generally seen by the research coordinator first, a few subjects were evaluated by the physician prior to the research coordinator which could influence the subject’s responses. However, in all instances, clinicians were blind to the results of the history and physical examination, and therefore, their diagnoses were not influenced by research findings.
These findings have important clinical implications. Knee pain is among the most common presenting complaints to primary care physicians, and knee OA affects over 10% of adults.29–32 Many of these adults with OA have structural evidence of meniscal tear; thus, the determination of whether the patient’s symptoms are related to the meniscal tear remains a key challenge in the management of adults with knee pain. Our findings suggest that the traditional battery of meniscal symptoms may have limited utility in the diagnosis of symptomatic meniscal tear in a middle age and older population. Our findings also identify a low risk group (<5% risk) in whom further evaluation for meniscal tear may not be justified; reducing the utilization of additional diagnostic imaging and surgical intervention in this low risk group could lessen the economic burden of this diagnosis. We further identify patients with moderate risk (~50% risk), in whom presumptive non-operative treatment and diagnostic testing for meniscal tear may be reasonable, and patients who appear to have a high likelihood of symptomatic meniscal tear in whom discussion of surgical intervention could be practical. Further research is required to confirm these findings in independent samples and to determine whether the use of the diagnostic index improves outcomes of care.
Supplementary Material
SIGNIFICANCE AND INNOVATION.
Localized pain, ability to bend the knee fully, duration of pain < 1 year, lack of varus alignment, lack of pes planus, and lack of joint space narrowing on x-ray are associated with higher likelihood of expert physician diagnosis of meniscal tear.
Commonly elicited mechanical symptoms may have limited utility in the diagnosis of symptomatic meniscal tear in a middle age and older population.
We identify a low risk group in whom further diagnostic evaluation for meniscal tear may not be necessary and a moderate risk group in whom additional testing for meniscal tear appears justified.
Acknowledgments
Contributions:
Obtaining of funding: Katz, Losina
Conception and design: Katz, Donnell-Fink, Losina
Provision of study patients: Martin, Wright
Collection and assembly of data: Smith
Analysis and interpretation of the data: Katz, Smith, Yang, Losina
Drafting of the article: Katz, Smith
Critical revision of the article for important intellectual content: All authors
Final approval of the article: All authors
Funding Source: NIH/NIAMS K24 AR057827, P60 AR047782
Footnotes
Competing interest statement: Dr. Wright reports receiving consulting fees and royalties from DePuy Orthopedics, a Johnson & Johnson Company. The remaining authors have no conflicts to report.
Role of the Funding Source: The study sponsor had no role in the design of the study; collection, analysis or interpretation of the data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
References
- 1.Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34:252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noble J, Turner PG. The function, pathology, and surgery of the meniscus. Clin Orthop Relat Res. 1986:62–68. [PubMed] [Google Scholar]
- 3.Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–2187. doi: 10.1002/art.11088. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9. doi: 10.2106/00004623-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Boden SD, Davis DO, Dina TS, Stoller DW, Brown SD, Vailas JC, et al. A prospective and blinded investigation of magnetic resonance imaging of the knee. Abnormal findings in asymptomatic subjects. Clin Orthop Relat Res. 1992:177–185. [PubMed] [Google Scholar]
- 6.Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B, Hodler J. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol. 2003;181:635–641. doi: 10.2214/ajr.181.3.1810635. [DOI] [PubMed] [Google Scholar]
- 7.Poehling GG, Ruch DS, Chabon SJ. The landscape of meniscal injuries. Clin Sports Med. 1990;9:539–549. [PubMed] [Google Scholar]
- 8.Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niu NN, Losina E, Martin SD, Wright J, Solomon DH, Katz JN. Development and preliminary validation of a meniscal symptom index. Arthritis Care Res (Hoboken) 2011;63:208–215. doi: 10.1002/acr.20354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eren OT. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy. 2003;19:850–854. doi: 10.1016/s0749-8063(03)00736-9. [DOI] [PubMed] [Google Scholar]
- 11.Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy. 1989;5:184–186. doi: 10.1016/0749-8063(89)90168-0. [DOI] [PubMed] [Google Scholar]
- 12.McMurray TP. The Semilunar Cartilages. Br J Surg. 1942;29:407–414. [Google Scholar]
- 13.Apley AG. The diagnosis of meniscus injuries; some new clinical methods. J Bone Joint Surg Am. 1947;29:78–84. [PubMed] [Google Scholar]
- 14.Waldron V. A test for chondromalacia patellae. Orthop Rev. 1983:12. [Google Scholar]
- 15.Selfe J, Harper L, Pedersen I, Breen-Turner J, Waring J. Four Outcome Measures for Patellofemoral Joint Problems. Physiotherapy. 87:507–515. [Google Scholar]
- 16.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 17.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368:1675–1684. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrlin SV, Wange PO, Lapidus G, Hallander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21:358–364. doi: 10.1007/s00167-012-1960-3. [DOI] [PubMed] [Google Scholar]
- 21.Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515–2524. doi: 10.1056/NEJMoa1305189. [DOI] [PubMed] [Google Scholar]
- 22.Yim JH, Seon JK, Song EK, Choi JI, Kim MC, Lee KB, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41:1565–1570. doi: 10.1177/0363546513488518. [DOI] [PubMed] [Google Scholar]
- 23.Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears. Int Orthop. 2007;31:57–60. doi: 10.1007/s00264-006-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 25.Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236–1241. doi: 10.1002/art.1780380910. [DOI] [PubMed] [Google Scholar]
- 26.Feinstein A. Clinical epidemiology: the architecture of clinical reearch. Philadelphia: WB Saunders; 1985. [Google Scholar]
- 27.Katz MI. Angle classification revisited. 1: Is current use reliable? Am J Orthod Dentofacial Orthop. 1992;102:173–179. doi: 10.1016/0889-5406(92)70030-E. [DOI] [PubMed] [Google Scholar]
- 28.Katz MI. Angle classification revisited 2: a modified Angle classification. Am J Orthod Dentofacial Orthop. 1992;102:277–284. doi: 10.1016/S0889-5406(05)81064-9. [DOI] [PubMed] [Google Scholar]
- 29.Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med. 2003;139:575–588. doi: 10.7326/0003-4819-139-7-200310070-00010. [DOI] [PubMed] [Google Scholar]
- 30.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jinks C, Lewis M, Ong BN, Croft P. A brief screening tool for knee pain in primary care. 1. Validity and reliability. Rheumatology (Oxford) 2001;40:528–536. doi: 10.1093/rheumatology/40.5.528. [DOI] [PubMed] [Google Scholar]
- 32.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.