Abstract
Purpose
The study investigated the capability of clinical findings, temperature, C-reactive protein (CRP), and white blood cell (WBC) count to discern patients with acute colonic diverticulitis from all other patients admitted with acute abdominal pain.
Methods
The probability of acute diverticulitis was assessed by the examining doctor, using a scale from 0 (zero probability) to 10 (100 % probability). Receiver operating characteristic (ROC) curves were used to assess the clinical diagnostic accuracy of acute colonic diverticulitis in patients admitted with acute abdominal pain.
Results
Of 833 patients admitted with acute abdominal pain, 95 had acute colonic diverticulitis. ROC curve analysis gave an area under the ROC curve (AUC) of 0.95 (CI 0.92 to 0.97) for ages <65 years, AUC = 0.86 (CI 0.78 to 0.93) in older patients. Separate analysis showed an AUC = 0.83 (CI 0.80 to 0.86) of CRP alone. White blood cell count and temperature were almost useless to discriminate acute colonic diverticulitis from other types of acute abdominal pain, AUC = 0.59 (CI 0.53 to 0.65) for white blood cell count and AUC = 0.57 (0.50 to 0.63) for temperature, respectively.
Conclusion
This prospective study demonstrates that standard clinical evaluation by non-specialist doctors based on history, physical examination, and initial blood tests on admission provides a high degree of diagnostic precision in patients with acute colonic diverticulitis.
Keywords: Acute colonic diverticulitis, Clinical diagnostic accuracy, Receiver operating characteristic curve, C-reactive protein, White blood cell count, Temperature
Introduction
As the incidence and admission rates of acute colonic diverticulitis are rising in the Western world, the burden on healthcare systems increases [1–4]. The recurrence rate is high, ranging from 6 to 25 % in the subsequent years after the first episode [2, 5], causing repeated consultation and treatment in the primary healthcare and potential hospital readmission. Patients with uncomplicated acute diverticulitis do not necessarily require hospital admission and may be treated on an out-patient basis. Thus, differentiated treatment guidelines of evidence-based clinical care pathways would be effective for the patient and cost saving for the healthcare system [6, 7].
During recent decades, a significant change in both diagnostics and treatment of acute colonic diverticulitis has evolved. As a supplement to clinical evaluation, computed tomography (CT) scans verify and determine stage of acute colonic diverticulitis, improving the decision-making in non-operative and operative management [8, 9]. CT scan is a cost-effective way to diagnose acute abdominal conditions; however, radiation exposure is a concern [10]. Patients with uncomplicated colonic diverticulitis are treated conservatively, and the role of antibiotics is disputable [11, 12]. Radiological drainage of localized abscesses has been introduced [13], and surgical intervention has changed from major open procedures to more conservative laparoscopic procedures in selected cases [14].
The rate of complicated acute colonic diverticulitis is highest during the primary admission, and the majority of readmitted patients have uncomplicated disease [2, 15]. A repeated CT scan may be omitted in patients with clinical recurrent disease and a previously documented history of diverticulitis, especially with C-reactive protein (CRP) <50 mg/mL [16]. A clinical diagnosis of uncomplicated diverticulitis, which comprises the majority of these patients [8, 12], remains of major importance in the management of this condition in an out-patient setting [17].
The main aim of the present prospective study was to assess the accuracy of clinical diagnosis in acute colonic diverticulitis, based on history, physical examination, and initial blood tests on admission to hospital in patients with acute abdominal pain, using a receiver operating characteristic curve (ROC) analysis. The secondary aim was to examine the diagnostic accuracy of temperature, CRP, and white blood cell (WBC) count alone in the diagnosis of acute colonic diverticulitis in patients admitted with acute abdominal pain.
Methods
Between November 2011 and March 2014, all patients older than 18 years, who were admitted to the Department of Surgery at Levanger Hospital with acute abdominal pain with a duration of less than 1 week, were invited to participate in the study. The hospital, located in Mid-Norway, is a first-line hospital serving the population of ten municipalities in North-Trondelag County, which had 94,174 inhabitants in 2012.
After admission, 833 patients gave written consent to participate and were included in the study; 477 (57 %) were women, and 537 (64 %) were below 65 years of age.
Based on anamnestic history, primary clinical examination, temperature and the results of initial blood tests (CRP and WBC), and before the results of any radiological examinations were available; the non-specialist doctors (usually pre-registrar house officers) in the emergency department scored the probability of acute colonic diverticulitis for the particular patient. A specific form, based on a categorized score from 0 (zero probability) to 10 (100 % probability) was used. In all, 107 different non-specialist doctors were involved in the scoring, 20 of these examined 50 % of the included patients.
The final diagnosis in all patients included in the study was based on the diagnosis at discharge and supplementary radiologic or endoscopic examinations as part of an ambulatory follow-up. Acute non-specific abdominal pain (NSAP) was defined as acute abdominal or pelvic pain without any obvious pathology if routine investigations, which included imaging and blood tests, did not reveal pathology and if the patient responded to non-specific treatment [18].
Acute colonic diverticulitis was confirmed by CT scan before discharge in 83 of 95 patients. Five patients with recurrent acute colonic diverticulitis had a recent CT verifying acute colonic diverticulitis, and five had their diagnosis confirmed by an ambulant CT scan or colonoscopy after discharge. Discharge diagnosis based on clinical examination and laboratory tests only occurred twice; the patients were aged 77 and 81 years.
In the study period, an unknown number of patients admitted with acute abdominal pain refused inclusion. Review of data from the hospital’s patient administrative system and patient records revealed a total of 168 patients admitted with acute colonic diverticulitis as discharge diagnosis in the relevant time period; of these, 95 (57 %) were included in the study. There were no statistical differences in gender, age, subtype of acute colonic diverticulitis, or length of hospital stay between patients included and those not included in the study, as shown in Table 1.
Table 1.
Characteristics of patients with acute colonic diverticulitis included in the study compared with those not included
| Patients included in the study (n = 95) | Patients not included in the study (n = 73) | Total (n = 168) | p value | |
|---|---|---|---|---|
| Male | 34 (36) | 21 (29) | 55 (33) | 0.34b |
| Age (years)a | 61 (28–90) | 66 (28–92) | 62 (28–92) | 0.29c |
| Hospital stay (days)a | 2 (0–19) | 2 (1–59) | 2 (0–59) | 0.045c |
| Uncomplicated diverticulitis | 80 (84) | 60 (82) | 140 (83) | 0.54d |
| Hinchey 1–2 | 10 (11) | 5 (7) | 15 (9) | 0.54d |
| Bowel obstruction (acute operation) | 0 | 2 (3) | 2 (1) | 0.54d |
| Hinchey 3 | 2 (2) | 5 (7) | 7 (4) | 0.54d |
| Hinchey 4 | 3 (3) | 1 (1) | 4 (2) | 0.54d |
Values in parentheses are percentages, unless indicated otherwise
aValues are median (range)
bZ-pooled exact test
cWilcoxon test
dCochran-Armitage Trend test
Statistical analysis
Proportions were compared using the unconditional z-pooled exact test. The medians of two samples were compared using the Wilcoxon test. The diagnostic accuracy of the clinical score was tested using ROC curves, including the area under the curve (AUC). An AUC value of 0.5 shows no predictive ability for the test in question, whereas a value of 1.0 indicates perfect discrimination [19]. Strength of discrimination has been classified as the following: AUC = 0.5 denotes no discrimination, AUC = 0.7–0.79 corresponds to acceptable strength of discrimination, AUC = 0.8–0.89 corresponds to excellent discrimination strength, and AUC = 0.9–1.0 corresponds to outstanding discrimination strength [20].
Two basic measures (sensitivity and specificity) of diagnostic accuracy were used [21] calculated from ROC curve analysis and expressed in percentage.
Two-sided p values <0.05 were considered significant. Ninety-five percent confidence intervals (CI) were reported where relevant. Medians are reported with range (minimum to maximum) where relevant.
The analyses were performed using SPSS 22 (SPSS Inc., Chicago, IL, USA), STATA 13 (Stata Corp LP, College Station, TX, USA), and StatXact 9 (Cytel Inc., Cambridge, MA, USA).
Ethics
The Regional Committee for Medical and Health Research Ethics (REC) gave permission for the study (2011/1782/REK midt). Only patients who gave written consent were included in the study.
Results
The study included 833 patients admitted with acute abdominal pain. The final diagnosis in relation to age is shown in Table 2. Overall, NSAP was the most frequent diagnosis, in 23 % of the patients, and acute colonic diverticulitis was the third most common diagnosis, in 11 % of the patients. Among patients younger than 65 years, NSAP was the most frequent diagnosis, while acute colonic diverticulitis was fourth in frequency. Among patients older than 65 years, acute biliary disease was the most frequent diagnosis, and acute colonic diverticulitis was third in frequency.
Table 2.
Final diagnosis in patients admitted with acute abdominal pain, in relation to age
| Final diagnosis | < 65 years | 65 + years | Total |
|---|---|---|---|
| Non-specific abdominal pain | 146 (27.2) | 44 (14.9) | 190 (22.8) |
| Biliary disease, included acute cholecystitis | 66 (12.3) | 47 (15.9) | 113 (13.6) |
| Acute colonic diverticulitis | 55 (10.2) | 40 (13.5) | 95 (11.4) |
| Acute appendicitis | 59 (11.0) | 7 (2.4) | 66 (7.9) |
| Bowel obstruction | 36 (6.7) | 27 (9.1) | 63 (7.6) |
| Ureteral stones | 38 (7.1) | 14 (4.7) | 52 (6.2) |
| Constipation | 15 (2.8) | 22 (7.4) | 37 (4.4) |
| Urinary, except ureteral stones | 17 (3.2) | 17 (5.7) | 34 (4.1) |
| Acute pancreatitis | 16 (3.0) | 11 (3.7) | 27 (3.2) |
| Gynecological disorders | 14 (2.6) | 7 (2.4) | 21 (2.5) |
| Inflammatory bowel disease | 15 (2.8) | 3 (1.0) | 18 (2.2) |
| Gastrointestinal cancer | 4 (0.7) | 13 (4.4) | 17 (2.0) |
| Thoracic conditions, included pneumonia | 11 (2.0) | 3 (1.9) | 14 (1.7) |
| Acute gastroenteritis | 10 (1.9) | 4 (1.4) | 14 (1.7) |
| Incarcerated hernia | 2 (0.4) | 6 (2.0) | 8 (1.0) |
| Other specific acute abdominal conditions | 33 (6.1) | 31 (10.5) | 64 (7.7) |
| Total | 537 (100) | 296 (100) | 833 (100) |
Values in parentheses are percentages
Among included patients, 95 patients had a final diagnosis of acute colonic diverticulitis, including two with abscess and three with perforation and generalized peritonitis. The tentative diagnosis from the primary care physicians had been acute colonic diverticulitis in 49 patients, giving a sensitivity for this diagnosis of 52 %. The rest of the patients with a final diagnosis of acute colonic diverticulitis had been admitted from primary care physicians with the following diagnoses: NSAP (24 patients), acute appendicitis (6 patients), acute intestinal obstruction (6 patients), and other specified abdominal conditions (10 patients). In 19 patients admitted with a misdiagnosis of acute colonic diverticulitis, the final diagnosis was NSAP (7 patients), peptic ulcer (3 patients), acute appendicitis (2 patients), pancreatic cancer with metastases (1 patient), and other diagnoses in 6 patients. The proportion of patients correctly diagnosed by the primary care physicians with another diagnosis than diverticulitis was 719 out of total 738 patients, analog to a specificity of 97 %.
Table 3 shows the primary clinical scores, based on evaluation by non-specialist doctors in the emergency room, for patients with a final diagnosis of acute colonic diverticulitis. The percentages of patients with acute colonic diverticulitis increased smoothly from 1.6 % among patients with a score of zero to 100 % among those with the maximum score of 10.
Table 3.
Primary clinical evaluation score for final diagnosis of acute colonic diverticulitis by non-specialist doctors
| Non-specialist doctor’s clinical score | Diverticulitis diagnosis at discharge | Total | |
|---|---|---|---|
| No | Yes | ||
| 0 | 191 (98.4) | 3 (1.6) | 194 |
| 1 | 250 (98.8) | 3 (1.2) | 253 |
| 2 | 139 (97.9) | 3 (2.1) | 142 |
| 3 | 61 (89.7) | 7 (10.3) | 68 |
| 4 | 25 (78.1) | 7 (21.9) | 32 |
| 5 | 33 (78.6) | 9 (21.4) | 42 |
| 6 | 18 (62.1) | 11 (37.9) | 29 |
| 7 | 10 (45.4) | 12 (54.6) | 22 |
| 8 | 8 (26.7) | 22 (73.3) | 30 |
| 9 | 3 (20.0) | 12 (80.0) | 15 |
| 10 | 0 (0.0) | 6 (100.0) | 6 |
| Total | 738 (88.6) | 95 (11.4) | 833 |
Values in parentheses are percentages
p < 0.001 (Cochran-Armitage Trend test)
Table 4 shows the final diagnoses of all patients with clinical scores between 6 and 10. Two thirds of the patients with acute colonic diverticulitis (63/95) had high scores after the primary evaluation by the non-specialist doctors on admission.
Table 4.
Final diagnosis in patients with acute abdominal pain and a high clinical score (6 to 10) for suspicion of acute colonic diverticulitis
| Final diagnosis | Number of patients |
|---|---|
| Acute colonic diverticulitis | 63 |
| Non-specific abdominal pain | 10 |
| Constipation | 4 |
| Acute appendicitis | 3 |
| Inflammatory bowel disease | 3 |
| Urinary, except ureteral stones | 3 |
| Ureteral stones | 2 |
| Gynecological disorders | 2 |
| Peptic ulcer | 2 |
| Diverticulosis (without inflammation) | 2 |
| Biliary disease | 1 |
| Bowel obstruction | 1 |
| Acute gastroenteritis | 1 |
| Bowel perforation | 1 |
| Retroperitoneal metastases (seminoma) | 1 |
| SIRS, unknown origin | 1 |
| Osteomyelitis of left greater trochanter | 1 |
| Torsion of an epiploic appendage | 1 |
| Total | 102 |
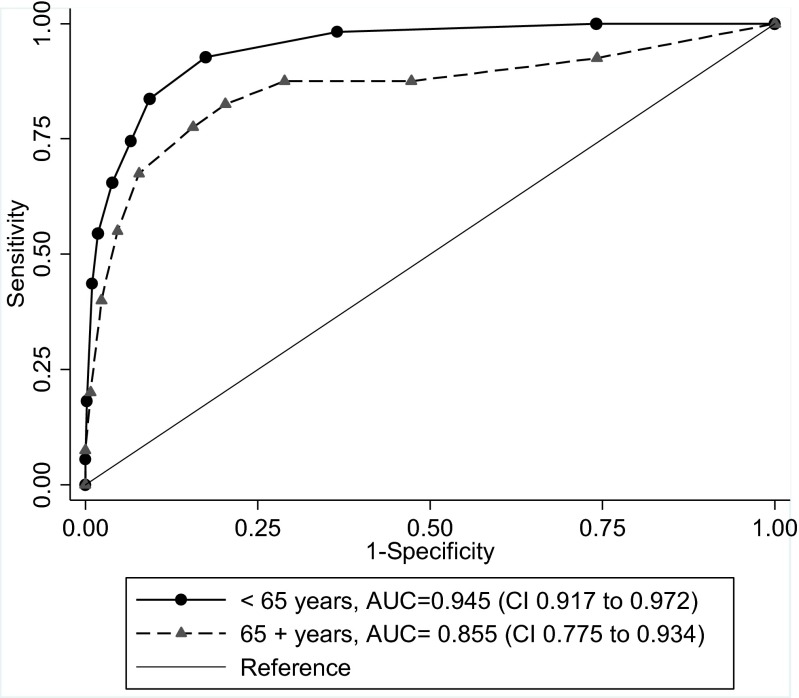
The diagnostic accuracy of the initial clinical score
Figure 1 illustrates the ROC curve analysis used to assess the diagnostic performance of the initial clinical scores given on admission. The initial diagnostic performance ranged from excellent to outstanding discrimination, with an AUC of 0.95 (CI 0.92 to 0.97) in patients younger than 65 years and 0.86 (CI 0.78 to 0.93) in patients aged 65 years or older. The AUC was significantly higher among younger than it was among older patients (p = 0.036). When we chose a cutoff value of 6 on the scale from 0 to 10 in patients younger than 65 years, ROC curve analysis resulted in a sensitivity of 65 % and a specificity of 96 %. In patients 65 years and older, a cutoff value of 6 resulted in a sensitivity of 68 % and specificity of 92 %.
Fig. 1.
Receiver operating characteristic (ROC) curves with corresponding area under the curve (AUC) for clinical scoring of acute colonic diverticulitis in patients below and above 65 years of age admitted with acute abdominal pain
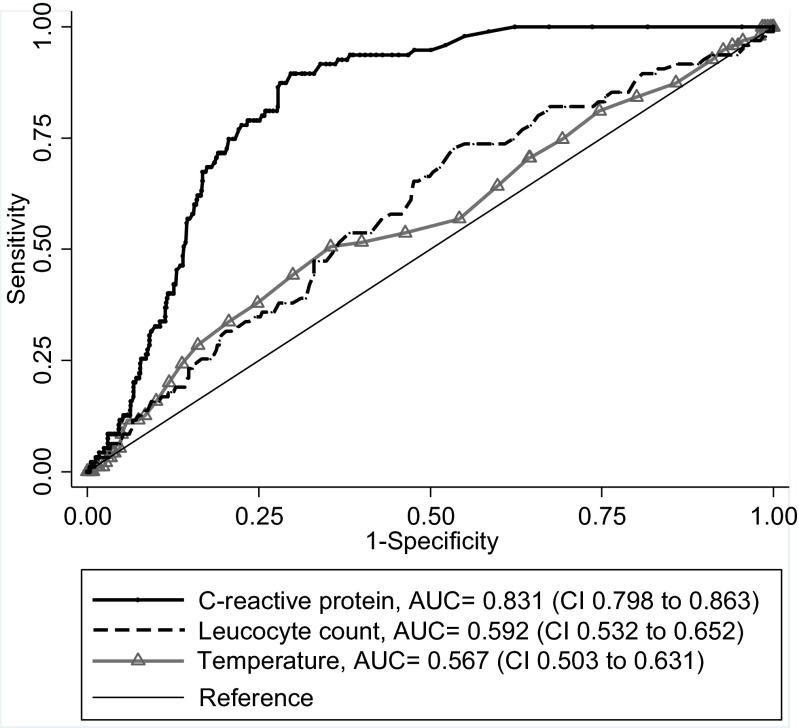
The diagnostic accuracy of temperature, WBC, and CRP
The diagnostic performance of temperature, CRP, and WBC on admission is illustrated in Fig. 2. This ROC curve analysis showed an excellent performance for C-reactive protein with an AUC of 0.83 (CI 0.80 to 0.86), while temperature and WBC had almost no discriminative power, with an AUC of 0.59 (CI 0.53 to 0.65) and 0.57 (CI 0.50 to 0.63), respectively.
Fig. 2.
Receiver operating characteristic (ROC) curves with corresponding area under the curve (AUC) for C-reactive protein, white blood cell count, and body temperature in predicting acute colonic diverticulitis in patients admitted with acute abdominal pain
Discussion
Main findings
This prospective series demonstrates that standard clinical evaluation, by non-specialist doctors, provides a high degree of diagnostic precision in patients with acute colonic diverticulitis. The diagnostic precision was slightly higher among patients younger than 65 years compared to those older. Furthermore, the analyses proved CRP to be the most valuable initial laboratory test in the differentiation of acute diverticulitis from other acute abdominal conditions.
Relation to other reports
Few reports have used ROC curve analysis to assess the clinical diagnostic performance in acute colonic diverticulitis [8, 32]; a categorical scoring system similar to the one presented here has never been used. In order to compare our findings with previous studies regarding sensitivity and specificity, we chose a cutoff value of 6 on the scale from 0 to 10. The resulting sensitivities and specificities were in accordance with previous studies that reported a sensitivity of 64–71 % and a specificity of 97–98 % when evaluating clinical diagnostics in acute colonic diverticulitis [8, 9, 22–25].
The clinical diagnostic sensitivity of acute colonic diverticulitis, based on examinations before admission to hospital by the primary care physicians, was 52 %. This was inferior to the results achieved by the non-specialist doctors in the hospital, but comparable to a previous study on diagnostic sensitivity of acute colonic diverticulitis in primary health care [24]. Various factors have impact on this finding: increased focus on patients with acute colonic diverticulitis, because of the study and the selection of patients admitted to a surgical department, advantage of the tentative diagnosis from the primary care physicians, and access to previous hospital records, body temperature, and blood tests in all included cases.
In the present study, the accuracy of the clinical diagnosis was slightly better in younger patients. The presentation of acute abdominal pain among elderly may be different from that seen in younger age groups. Elderly patients tend to have more vague and non-specific symptoms, broader alternatives of differential diagnosis, altered clinical signs that do not correlate with disease severity, higher incidence of comorbidity and multi-pharmacy, and communication difficulties because of hearing and cognitive impairment [26, 27]. This makes elderly patients more prone to misdiagnosis than younger patients [28].
ROC curve analysis to assess CRP in the diagnostics of acute colonic diverticulitis has previously been reported with an AUC ranging from 0.72 to 0.94 [8, 30–34], which is comparable to the present results. Furthermore, these studies confirm WBC count and body temperature to be without discriminative power in distinguishing diverticulitis from other patients with acute abdominal pain, with an AUC between 0.54 and 0.57 [8, 33].
Most previous studies have focused on these parameters in the differentiation between uncomplicated and complicated acute colonic diverticulitis [29, 32, 33]; also demonstrating that CRP, other than WBC count, was the most important biochemical marker.
Practical implication
This study confirms that a clinical diagnosis of acute colonic diverticulitis is achievable by non-specialist doctors at the emergency department and applies specifically to patients younger than 65 years with localized tenderness in the left lower quadrant and an elevated CRP.
Previous studies report other criteria as significant in the selection of patients suitable for out-patient diagnosis and treatment such as a CRP cutoff value between 150 and 200 mg/L, absence of vomiting, significant fever and signs of generalized peritonitis, absence of compromised immune status, and significant comorbidities. Of additional importance is a close follow-up and the possibility of a secondary evaluation if symptoms worsen [8, 31–37]. The diagnosis would be even more strengthened in patients who have recurrent symptoms, with colonic diverticular disease verified on a pervious CT scan.
Out-patient treatment would include oral analgesics, with or without oral antibiotics. Follow-up, including clinical examination and CRP with the possibility of ambulant CT scan on day 4 and referral to follow-up endoscopy or CT colonography after 6 weeks of improvement, has been suggested [38].
This evidence should form the basis for a clinical care pathway. A structural approach, involving both the primary and secondary healthcare system, would increase the quality of treatment, define an appropriate level of treatment for the individual patient, and reduce the increasing rates of admission to hospital among patients with acute colonic diverticulitis.
Weakness of the study
Not all patients admitted to hospital because of acute abdominal pain in the study period were included in this study. There were no statistical differences in gender, age, subtype of acute colonic diverticulitis, or hospital stay when comparing patients included or not, as shown in Table 1. The included patients seem to be a representative selection of all patients admitted with acute abdominal pain, although a more complete inclusion would have increased the precision of the findings.
Another limitation is the probable selection bias based on the hospital doctors’ awareness of the study. However, the percentage of patients with acute colonic diverticulitis in relation to other types of acute abdomen conditions generally matches other studies [39].
Strengths of the study
The present prospective study is the first to use a fine graded categorized clinical score and subsequent ROC curve analysis in the evaluation of clinical diagnostic accuracy in patients with acute colonic diverticulitis. The advantage of ROC curve analysis in the present study was the possibility to consider the complete spectrum of the observed results, not only the mean or dichotomous variable denoting “yes or no.”
The study highlights that non-specialist doctors, usually in their first year of a clinical career, were able to clinically diagnose acute colonic diverticulitis in patients with acute abdominal pain with a high degree of accuracy. This reflects the possibility of a similar standardized approach applied in the out-patient setting, reducing the need for further referral to hospitals, especially in cases of suspected uncomplicated acute colonic diverticulitis.
Conclusion
This prospective study demonstrates that standard clinical evaluation by non-specialist doctors based on history, physical examination, and initial blood tests on admission provides a high degree of diagnostic precision in patients with acute colonic diverticulitis.
Furthermore, the analyses proved CRP to be a valuable initial laboratory test in the differentiation of acute colonic diverticulitis from other acute abdominal conditions.
Compliance with ethical standards
The Regional Committee for Medical and Health Research Ethics (REC) gave permission for the study (2011/1782/REK midt). Only patients who gave written consent were included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Anand N. Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol. 2011;17(12):1600–1605. doi: 10.3748/wjg.v17.i12.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jamal Talabani A, Endreseth BH, Edna TH. Major increase in admission- and incidence rates of acute colonic diverticulitis. Int J Color Dis. 2014;29(8):937–945. doi: 10.1007/s00384-014-1888-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warner E, Crighton EJ, Moineddin R, Mamdani M, Upshur R. Fourteen-year study of hospital admissions for diverticular disease in Ontario. Can J Gastroenterol. 2007;21(2):97–99. doi: 10.1155/2007/943460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papagrigoriadis S, Koreli A, Husain A. Impact of diverticular disease on hospital costs and activity. Color Dis. 2004;6(2):81–84. doi: 10.1111/j.1463-1318.2004.00532.x. [DOI] [PubMed] [Google Scholar]
- 5.Martellucci J, Tonelli P, Valeri A. Long-term results of treatment of acute diverticulitis: still lessons to be learned? Updat Surg. 2013;65(2):125–130. doi: 10.1007/s13304-012-0194-8. [DOI] [PubMed] [Google Scholar]
- 6.Unlü C, de Korte N, Daniels L, Consten EC, Cuesta MA, Gerhards MF, van Geloven AA, van der Zaag ES, van der Hoeven JA, Klicks R, et al. A multicenter randomized clinical trial investigating the cost-effectiveness of treatment strategies with or without antibiotics for uncomplicated acute diverticulitis (DIABOLO trial) BMC Surg. 2010;20:10–23. doi: 10.1186/1471-2482-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tursi A. Efficacy, safety, and applicability of outpatient treatment for diverticulitis. Drug Healthc Patient Saf. 2014;6:29–36. doi: 10.2147/DHPS.S61277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laméris W, van Randen A, van Gulik TM, Busch OR, Winkelhagen J, Bossuyt PM, Stoker J, Boermeester MA (2010) A clinical decision rule to establish the diagnosis of acute diverticulitis at the emergency department. Dis Colon rectum 53(6):896–904 [DOI] [PubMed]
- 9.Andeweg CS, Mulder IM, Felt-Bersma RJ, Verbon A, van der Wilt GJ, van Goor H, Lange JF, Stoker J, Boermeester MA, Bleichrodt RP, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30(4–6):278–292. doi: 10.1159/000354035. [DOI] [PubMed] [Google Scholar]
- 10.Brenner DJ. Should we be concerned about the rapid increase in CT usage? Rev Environ Health. 2010;25(1):63–68. doi: 10.1515/REVEH.2010.25.1.63. [DOI] [PubMed] [Google Scholar]
- 11.Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K, AVOD Study Group Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. BJS. 2012;99(4):532–539. doi: 10.1002/bjs.8688. [DOI] [PubMed] [Google Scholar]
- 12.Isacson D, Andreasson K, Nikberg M, Smedh K, Chabok A. No antibiotics in acute uncomplicated diverticulitis: does it works? Scand J Gastroenterol. 2014;49(12):1441–1446. doi: 10.3109/00365521.2014.968861. [DOI] [PubMed] [Google Scholar]
- 13.Singh B, May K, Coltart I, Moore NR, Cunningham C. The long-term results of percutaneous drainage of diverticular abscess. Ann R Coll Surg Engl. 2008;90(4):297–301. doi: 10.1308/003588408X285928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thornell A, Angenete E, Bisgaard T, Bock D, Burcharth J, Heath J, Pommergaard HC, Rosenberg J, Stilling N, Skullman S, Haglind E. Laparoscopic lavage for perforated diverticulitis with purulent peritonitis: a randomized trial. Ann Intern Med. 2016;164(3):137–145. doi: 10.7326/M15-1210. [DOI] [PubMed] [Google Scholar]
- 15.Ritz JP, Lehmann KS, Frericks B, Stroux A, Buhr HJ, Holmer C. Outcome of patients with acute sigmoid diverticulitis: multivariate analysis of risk factors for free perforation. Surgery. 2011;149(5):606–613. doi: 10.1016/j.surg.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Nizri E, Spring S, Ben-Yehuda A, Khatib M, Klausner J, Greenberg R. C-reactive protein as a marker of complicated diverticulitisin patients on anti-inflammatory medications. Tech Coloproctol. 2014;18(2):145–149. doi: 10.1007/s10151-013-1044-5. [DOI] [PubMed] [Google Scholar]
- 17.Isacson D, Thorisson A, Andreasson K, Nikberg M, Smedh K, Chabok A. Outpatient, non-antibiotic management in acute uncomplicated diverticulitis, a prospective study. Int J Color Dis. 2015;30(9):1229–1234. doi: 10.1007/s00384-015-2258-y. [DOI] [PubMed] [Google Scholar]
- 18.Gerhardt RT, Nelson BK, Keenan S, Kernan L, MacKersie A, Lane MS. Derivation of clinical guideline for the assessment of nonspecific abdominal pain: the guideline for abdominal pain in the ED setting (GAPEDS) phase-1 study. Am J Emerg Med. 2005;23(6):709–717. doi: 10.1016/j.ajem.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Søreide K, Kørner H, Søreide JA. Diagnostic accuracy and receiver-operating characteristics curve analysis in surgical research and decision making. Ann Surg. 2011;253(1):27–34. doi: 10.1097/SLA.0b013e318204a892. [DOI] [PubMed] [Google Scholar]
- 20.Hosmer DW, Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. Hoboken: Wiley; 2013. [Google Scholar]
- 21.Zhou X-H, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine. Hoboken: Wiley; 2011. [Google Scholar]
- 22.Toorenvliet BR, Bakker RF, Breslau PJ, Merkus JW, Hamming JF. Colonic diverticulitis: a prospective analysis of diagnostic accuracy and clinical decision-making. Color Dis. 2010;12(3):179–186. doi: 10.1111/j.1463-1318.2009.01778.x. [DOI] [PubMed] [Google Scholar]
- 23.Andeweg CS, Wegdam JA, Groenewoud J, van der Wilt GJ, van Goor H, Bleichrodt RP. Toward an evidence-based step up approach in diagnosing diverticulitis. Scand J Gastroenterol. 2014;49(7):775–784. doi: 10.3109/00365521.2014.908475. [DOI] [PubMed] [Google Scholar]
- 24.Laurell H, Hansson LE, Gunnarsson U. Impact of clinical experience and diagnostic performance in patients with acute abdominal pain. Gastroenterol Res Pract. 2015;2015:1–7. doi: 10.1155/2015/590346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laurell H, Hansson LE, Gunnarsson U. Acute diverticulitis—clinical presentation and differential diagnostics. Color Dis. 2007;9(6):496–501. doi: 10.1111/j.1463-1318.2006.01162.x. [DOI] [PubMed] [Google Scholar]
- 26.Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537–1544. [PubMed] [Google Scholar]
- 27.Chang C-C, Wang S-S. Acute abdominal pain in the elderly. Int J Gerontolog. 2007;1(2):77–82. doi: 10.1016/S1873-9598(08)70026-7. [DOI] [Google Scholar]
- 28.Laurell H, Hansson LE, Gunnarsson U. Acute abdominal pain among elderly patients. Gerontology. 2006;52(6):339–344. doi: 10.1159/000094982. [DOI] [PubMed] [Google Scholar]
- 29.Tursi A. Biomarkers in diverticular diseases of the colon. Dig Dis. 2012;30(1):12–18. doi: 10.1159/000335695. [DOI] [PubMed] [Google Scholar]
- 30.Mäkelä JT, Klintrup K, Takala H, Rautio T. The role of C-reactive protein in prediction of the severity of acute diverticulitis in an emergency unit. Scand J Gastroenterolog. 2015;50(5):536–541. doi: 10.3109/00365521.2014.999350. [DOI] [PubMed] [Google Scholar]
- 31.Kechagias A, Rautio T, Kechagias G, Mäkelä J. The role of C-reactive protein in the prediction of the clinical severity of acute diverticulitis. Am Surg. 2014;80(4):391–395. [PubMed] [Google Scholar]
- 32.Andeweg CS, Knobben L, Hendriks JC, Bleichrodt RP, van Goor H. How to diagnose acute left-sided colonic diverticulitis. Proposal to clinical scoring system. Ann Surg. 2011;253(5):940–946. doi: 10.1097/SLA.0b013e3182113614. [DOI] [PubMed] [Google Scholar]
- 33.van de Wall BJ, Draaisma WA, van der Kaaij RT, Consten EC, Wiezer MJ, Broeders IA. The value of inflammation markers and body temperature in acute diverticulitis. Color Dis. 2013;15(5):621–626. doi: 10.1111/codi.12072. [DOI] [PubMed] [Google Scholar]
- 34.Käser SA, Fankhauser G, Glauser PM, Toia D, Maurer CA. Diagnostic value of inflammation markers in predicting perforation in acute sigmoid diverticulitis. Wolrd J Surg. 2010;34(11):2717–2722. doi: 10.1007/s00268-010-0726-7. [DOI] [PubMed] [Google Scholar]
- 35.Tan JP, Barazanchi AW, Singh PP, Hill AG, Maccormick AD. Predictors of acute diverticulitis severity: a systematic review. Int J Surg. 2016;26:43–52. doi: 10.1016/j.ijsu.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Mizuki A, Nagata H, Tatemichi M, Kaneda S, Tsukada N, Ishii H, Hibi T. The out-patient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol Ther. 2005;21(7):889–897. doi: 10.1111/j.1365-2036.2005.02422.x. [DOI] [PubMed] [Google Scholar]
- 37.Mäkelä JT, Klintrup K, Rautio T. The role of low CRP values in the prediction of the development of acute diverticulitis. Int J Color Dis. 2016;31(1):23–27. doi: 10.1007/s00384-015-2410-8. [DOI] [PubMed] [Google Scholar]
- 38.Jackson JD, Hammond T. Systematic review: outpatient management of acute uncomplicated diverticulitis. Int J Color Dis. 2014;29(7):775–781. doi: 10.1007/s00384-014-1900-4. [DOI] [PubMed] [Google Scholar]
- 39.Laméris W, van Randen A, van Es HW, van Heesewijk JP, van Ramshorst B, Bouma WH, ten Hove W, van Leeuwen MS, van Keulen EM, Dijkgraaf MG, Bossuyt PM, Boermeester MA, Stoker J, OPTIMA study group (2009) Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ 338 [DOI] [PMC free article] [PubMed]